Published online May 28, 2024. doi: 10.3748/wjg.v30.i20.2677
Revised: January 10, 2024
Accepted: February 22, 2024
Published online: May 28, 2024
Processing time: 188 Days and 20.4 Hours
The coronavirus disease 2019 (COVID-19) pandemic disrupted healthcare in the United States.
To investigate COVID-19-related and non-COVID-19-related death and characteristics associated with excess death among inflammatory bowel disease (IBD) decedents.
We performed a register-based study using data from the National Vital Statistics System, which reports death data from over 99% of the United States population, from January 1, 2006 through December 31, 2021. IBD-related deaths among adults 25 years and older were stratified by age, sex, race/ethnicity, place of death, and primary cause of death. Predicted and actual age-standardized mortality rates (ASMRs) per 100000 persons were compared.
49782 IBD-related deaths occurred during the study period. Non-COVID-19-related deaths increased by 13.14% in 2020 and 18.12% in 2021 [2020 ASMR: 1.55 actual vs 1.37 predicted, 95% confidence interval (CI): 1.26-1.49; 2021 ASMR: 1.63 actual vs 1.38 predicted, 95%CI: 1.26-1.49]. In 2020, non-COVID-19-related mortality increased by 17.65% in ulcerative colitis (UC) patients between the ages of 25 and 65 and 36.36% in non-Hispanic black (NHB) Crohn’s disease (CD) patients. During the pandemic, deaths at home or on arrival and at medical facilities as well as deaths due to neoplasms also increased.
IBD patients suffered excess non-COVID-19-related death during the pandemic. Excess death was associated with younger age among UC patients, and with NHB race among CD patients. Increased death at home or on arrival and due to neoplasms suggests that delayed presentation and difficulty accessing healthcare may have led to increased IBD mortality.
Core Tip: The coronavirus disease 2019 (COVID-19) pandemic disrupted healthcare in the United States. Excess non-COVID-19-related mortality during the COVID-19 pandemic has been reported in several chronic conditions, including cardiovascular disease, alcohol use disorder, diabetes mellitus, and cirrhosis. We found that inflammatory bowel disease patients also experienced excess non-COVID-19-related mortality during the COVID-19 pandemic. Young ulcerative colitis patients and non-Hispanic black patients with Crohn’s disease were particularly affected, with 17.65% and 36.36% increase in non-COVID-19-related death in 2020, respectively.
- Citation: Rotondo-Trivette S, He XY, Samaan JS, Lv F, Truong E, Juels M, Nguyen A, Gao X, Zu J, Yeo YH, Ji FP, Melmed GY. Excess non-COVID-19-related mortality among inflammatory bowel disease decedents during the COVID-19 pandemic. World J Gastroenterol 2024; 30(20): 2677-2688
- URL: https://www.wjgnet.com/1007-9327/full/v30/i20/2677.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i20.2677
The coronavirus disease 2019 (COVID-19) pandemic led to devastating consequences for healthcare in the United States. COVID-19 has killed over 1 million individuals in the United States[1], with an estimated 180 excess deaths per 100000 individuals in 2020 and 2021[2]. The excess death observed since the start of the pandemic is not entirely attributed to COVID-19. From March to August 2020, 20% of excess deaths were due to non-COVID-19-related causes[3]. Previous studies have shown non-COVID-19-related excess mortality in chronic conditions such as cardiovascular disease, alcohol use disorder, diabetes mellitus, and cirrhosis[4-8].
Inflammatory bowel disease (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC), affects approximately 3 million adults in the United States, with a 123% increase in prevalence from 2007-2016[9,10]. Recent studies have shown that mortality rates among IBD patients are only modestly increased compared to the general population[11-13]. Additionally, after controlling for comorbidities, IBD patients are not at increased risk of COVID-19-related mortality despite the use of immunosuppressive medications[14]. It is also known that IBD patients have greater healthcare needs than the average population, including outpatient and emergency department visits, medication prescriptions, hospitalizations, and surgeries[9,11,15]. They also require more frequent cancer screening due to increased risk of colorectal cancer[16,17]. During the pandemic, IBD patients experienced a lack of adequate high-quality follow-up visits, decreased use of colonoscopies, and reduced surgical intervention[18,19]. The decreased healthcare utilization, in addition to job loss, financial stress, and mental health distress, may have made IBD patients more vulnerable to mortality during the pandemic[20-23]. As IBD patients do not normally have significantly different mortality rates than the general population but do use significantly more healthcare resources, they represent an important group for investigating excess mortality in the context of the pandemic’s impact on access to health services. In this study, we investigated whether there was excess death among IBD patients during the pandemic using nationally representative data from 2006 to 2021. We also investigated patient characteristics associated with mortality during the pandemic.
In this register-based study, data on IBD-related deaths from January 1, 2006 to December 31, 2021 among United States adults that were 25 years old and older was collected using the National Vital Statistics System (NVSS) database from the Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research website[24,25]. The NVSS database contains death data for more than 99% of decedents in the United States. Since data from NVSS is publicly available and de-identified, the study did not seek institutional review board approval. The study is compliant with the STROBE guidelines.
Diseases were categorized by the international classification of diseases (ICD-10) codes, including COVID-19 infection (U07.1), CD (K50), and UC (K51). IBD is associated with numerous complications and may not be perceived as the immediate cause of death. Therefore, we defined an IBD-related death as a decedent with CD or UC listed in any cause of death position. Similarly, we defined a COVID-19-related death as a decedent with COVID-19 infection listed in any cause of death position. Decedents were stratified by age (25-64 and ≥ 65 years), sex (male and female), and race/ethnicity [Hispanic, non-Hispanic white, and non-Hispanic black (NHB)]. We were unable to include stratification by race in 2021, as a new category of race (“multi-racial”) was introduced and resulted in sample sizes that were too small for analysis. We classified the location of death into mutually exclusive subgroups, including “death at home or on arrival”, “hospice facility”, “medical facility”, and “nursing home”. The corresponding ICD-10 codes for the top three immediate causes of death were K00-K92 for diseases of the digestive system, C00-D48 for neoplasms, and I00-I99 for diseases of the circulatory system. Beyond the top three causes of death, numbers of deaths were too small to maintain anonymity.
Crude mortality rates were calculated by dividing the number of annual IBD-related deaths by the total United States population of the corresponding year. Calculating age-standardized mortality rates (ASMRs) involves a series of steps using the direct standardization method. Initially, age-specific mortality rates are determined for various age groups. The 2010 United States Census Standard Population is then used as a reference to account for different age structures in populations. This population is divided into groups by decade, from 25 to 85+ years. For each group, the age-specific mortality rate is multiplied by the corresponding number of individuals in the standard population. These products are summed across all age groups, and the total is normalized to represent the mortality rate per 100000 persons.
We conducted predictive analyses to determine the predicted mortality rates in 2020 and 2021, according to the trend of ASMRs between 2006 and 2019, and compared the observed and predicted mortality rates. We tested various time series regression models, each suited to different aspects of data analysis, according to the data distribution. The auto-regressive integrated moving average model, known for its ability to handle non-stationary data through differencing, was a key component of our analysis. The auto-regressive moving average model, which is effective for stationary time series data, was also employed. Additionally, we utilized linear regression, a fundamental approach for modeling the relationship between a dependent variable and one or more independent variables. We also explored polynomial regression, which extends linear regression by considering the relationship between the independent variable and polynomial degrees of it, thus fitting non-linear data more effectively. The most appropriate model was then selected by referring to the model fit and the significance of the variables, ensuring the best representation of the underlying data patterns and relationships. For analyses that used the linear regression model, we used the ordinary least squares method to determine the predicted rates and the R square to determine the goodness of fit of each model. For data with non-linear distribution, we performed polynomial regression to predict the mortality rates during the pandemic (Supplementary Table 1). Statistically significant excess non-COVID-19-related death was defined as observed non-COVID-19-related ASMR greater than the upper limit of the predicted ASMR’s 95% confidence interval (CI). Subgroups with ≤ 20 deaths were excluded due to the concern of unreliable estimation. All analyses were performed using R 4.0.2 statistical software (data management) and PyCharm 3.9.0 (predictive analysis).
There were 49782 IBD-related deaths in the United States during the study period, including 40945 prior to the pandemic (2006 to 2019), and 8837 during the pandemic (2020 and 2021). During the pandemic, there were 783 (8.86%) COVID-19-related deaths and 8054 (91.14%) non-COVID-19-related deaths. Detailed demographics of decedents can be found in Table 1. The majority of IBD decedents were aged 65 years and above (69.13%), with 23122 males (46.45%), and 26660 females (53.55%). 90.48% were non-Hispanic white.
| Overall deaths (2006-2021) | Pre-pandemic deaths (2006-2019) | Pandemic deaths (2020-2021) | ||||
| Ulcerative colitis | Crohn’s disease | Ulcerative colitis | Crohn’s disease | Ulcerative colitis | Crohn’s disease | |
| Age (yr) | ||||||
| ≥ 65 | 15136 (77.45) | 19278 (63.75) | 12304 (77.01) | 15706 (62.90) | 2832 (79.39) | 3572 (67.78) |
| 25-64 | 4408 (22.55) | 10960 (36.25) | 3673 (22.99) | 9262 (37.10) | 735 (20.61) | 1698 (32.22) |
| Gender | ||||||
| Male | 9805 (50.17) | 13317 (44.04) | 8087 (50.62) | 10951 (43.86) | 1718 (48.16) | 2366 (44.90) |
| Female | 9739 (49.83) | 16921 (55.96) | 7890 (49.38) | 14017 (56.14) | 1849 (51.84) | 2904 (55.10) |
| Race/ethnicity (not including 2021) | ||||||
| Hispanic | 726 (4.10) | 732 (2.66) | 651 (4.07) | 651 (2.61) | 75 (4.37) | 81 (3.19) |
| Non-Hispanic white | 15740 (88.96) | 24661 (89.66) | 14249 (89.18) | 22448 (89.91) | 1491 (86.89) | 2213 (87.23) |
| Non-Hispanic black | 948 (5.36) | 1843 (6.70) | 841 (5.26) | 1627 (6.52) | 107 (6.24) | 216 (8.51) |
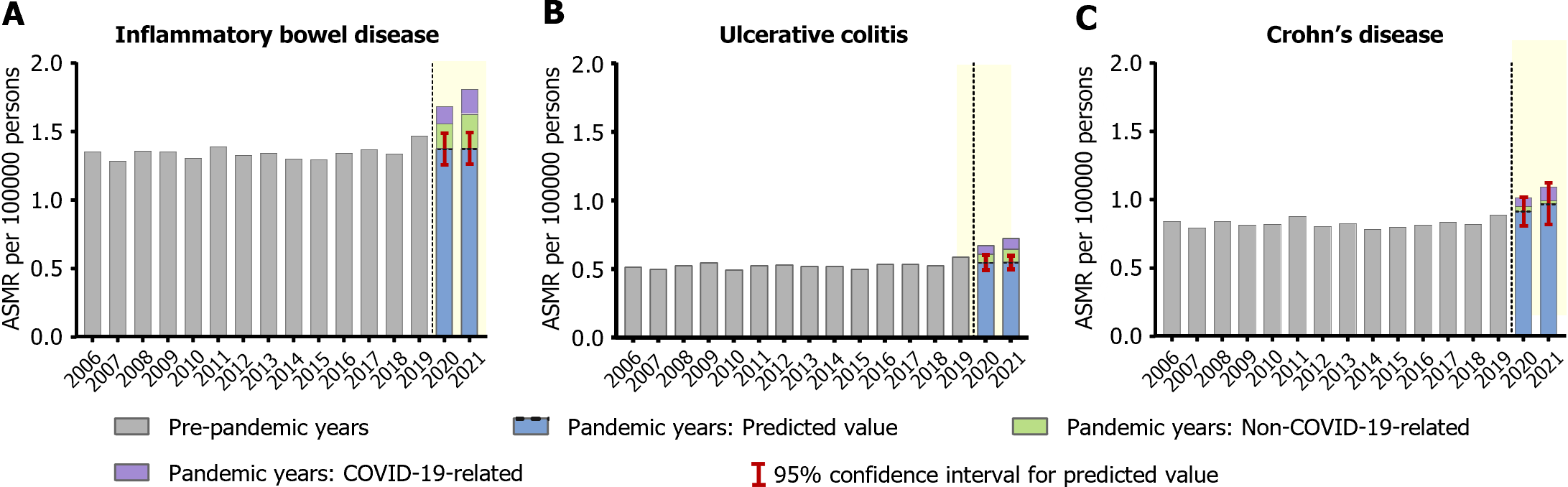
Mortality trends among CD, UC, and all IBD decedents from 2006 to 2021 are illustrated in Figure 1. In 2020 and 2021, non-COVID-19-related mortality among decedents with IBD was respectively 13.14% and 18.12% higher than predicted (2020 ASMR: 1.55 actual vs 1.37 predicted, 95%CI: 1.26-1.49; 2021 ASMR: 1.63 actual vs 1.38 predicted, 95%CI: 1.26-1.49). When stratified by disease type, this excess mortality was specifically noted among those with UC (2020: 10.91% increase, ASMR: 0.61 actual vs 0.55 predicted, 95%CI: 0.49-0.60; 2021: 18.18% increase, ASMR: 0.65 actual vs 0.55 predicted, 95%CI: 0.50-0.60). There was no significant increase in non-COVID-19-related or all-cause mortality among CD decedents compared to predicted in both 2020 and 2021. Detailed results can be found in Table 2.
| 2006 | 2019 | 2020 | 2021 | ||||||||
| Observed all-cause | Predicted (95%CI) | Observed non-COVID | Increase (%)1 | Observed all-cause | Predicted (95%CI) | Observed non-COVID | Increase (%)1 | ||||
| IBD | 1.35 | 1.47 | 1.68 | 1.37 (1.26-1.49) | 1.55 | 13.14 | 1.81 | 1.38 (1.26-1.49) | 1.63 | 18.12 | |
| UC | 0.51 | 0.59 | 0.68 | 0.55 (0.49-0.60) | 0.61 | 10.91 | 0.73 | 0.55 (0.50-0.60) | 0.65 | 18.18 | |
| CD | 0.84 | 0.89 | 1.01 | 0.91 (0.81-1.02) | 0.95 | 4.40 | 1.09 | 0.97 (0.82-1.12) | 0.99 | 2.06 | |
| Age | |||||||||||
| 25-64 yr | IBD | 0.53 | 0.59 | 0.68 | 0.61 (0.55-0.66) | 0.65 | 6.56 | 0.71 | 0.64 (0.57-0.72) | 0.64 | 0.00 |
| UC | 0.14 | 0.19 | 0.21 | 0.17 (0.15-0.19) | 0.20 | 17.65 | 0.21 | 0.17 (0.15-0.19) | 0.18 | 5.88 | |
| CD | 0.39 | 0.41 | 0.47 | 0.42 (0.37-0.47) | 0.46 | 9.52 | 0.50 | 0.45 (0.38-0.52) | 0.46 | 2.22 | |
| ≥ 65 yr | IBD | 4.69 | 5.03 | 5.76 | 4.95 (4.49-5.40) | 5.23 | 5.66 | 6.28 | 5.07 (4.54-5.60) | 5.67 | 11.83 |
| UC | 2.02 | 2.21 | 2.59 | 2.3 (2.01-2.58) | 2.31 | 0.43 | 2.81 | 2.45 (2.04-2.86) | 2.53 | 3.27 | |
| CD | 2.67 | 2.83 | 3.20 | 2.79 (2.46-3.12) | 2.95 | 5.73 | 3.48 | 2.87 (2.49-3.25) | 3.15 | 9.76 | |
| Sex | |||||||||||
| Female | IBD | 1.28 | 1.38 | 1.61 | 1.42 (1.24-1.61) | 1.48 | 4.23 | 1.76 | 1.51 (1.25-1.78) | 1.59 | 5.30 |
| UC | 0.43 | 0.50 | 0.60 | 0.53 (0.44-0.61) | 0.54 | 1.89 | 0.68 | 0.57 (0.44-0.70) | 0.60 | 5.26 | |
| CD | 0.85 | 0.88 | 1.02 | 0.9 (0.78-1.02) | 0.95 | 5.56 | 1.09 | 0.94 (0.76-1.12) | 0.99 | 5.32 | |
| Male | IBD | 1.44 | 1.58 | 1.76 | 1.63 (1.49-1.76) | 1.63 | 0.00 | 1.87 | 1.73 (1.54-1.92) | 1.68 | -2.89 |
| UC | 0.62 | 0.70 | 0.76 | 0.68 (0.62-0.75) | 0.70 | 2.94 | 0.78 | 0.7 (0.63-0.78) | 0.69 | -1.43 | |
| CD | 0.83 | 0.89 | 1.00 | 0.93 (0.83-1.04) | 0.94 | 1.08 | 1.10 | 1.01 (0.86-1.16) | 0.99 | -1.98 | |
| Race/ethnicity | |||||||||||
| Non-Hispanic white | UC | 0.57 | 0.68 | 0.79 | 0.71 (0.63-0.78) | 0.71 | 0.00 | N/A | N/A | N/A | N/A |
| CD | 0.96 | 1.08 | 1.22 | 1.12 (0.99-1.25) | 1.15 | 2.68 | N/A | N/A | N/A | N/A | |
| Non-Hispanic black | UC | 0.24 | 0.36 | 0.42 | 0.41 (0.29-0.52) | 0.39 | -4.88 | N/A | N/A | N/A | N/A |
| CD | 0.57 | 0.58 | 0.81 | 0.55 (0.41-0.70) | 0.75 | 36.36 | N/A | N/A | N/A | N/A | |
| Hispanic | UC | 0.36 | 0.23 | 0.30 | 0.23 (0.07-0.38) | 0.26 | 13.04 | N/A | N/A | N/A | N/A |
| CD | 0.22 | 0.24 | 0.30 | 0.27 (0.08-0.47) | 0.27 | 0.00 | N/A | N/A | N/A | N/A | |
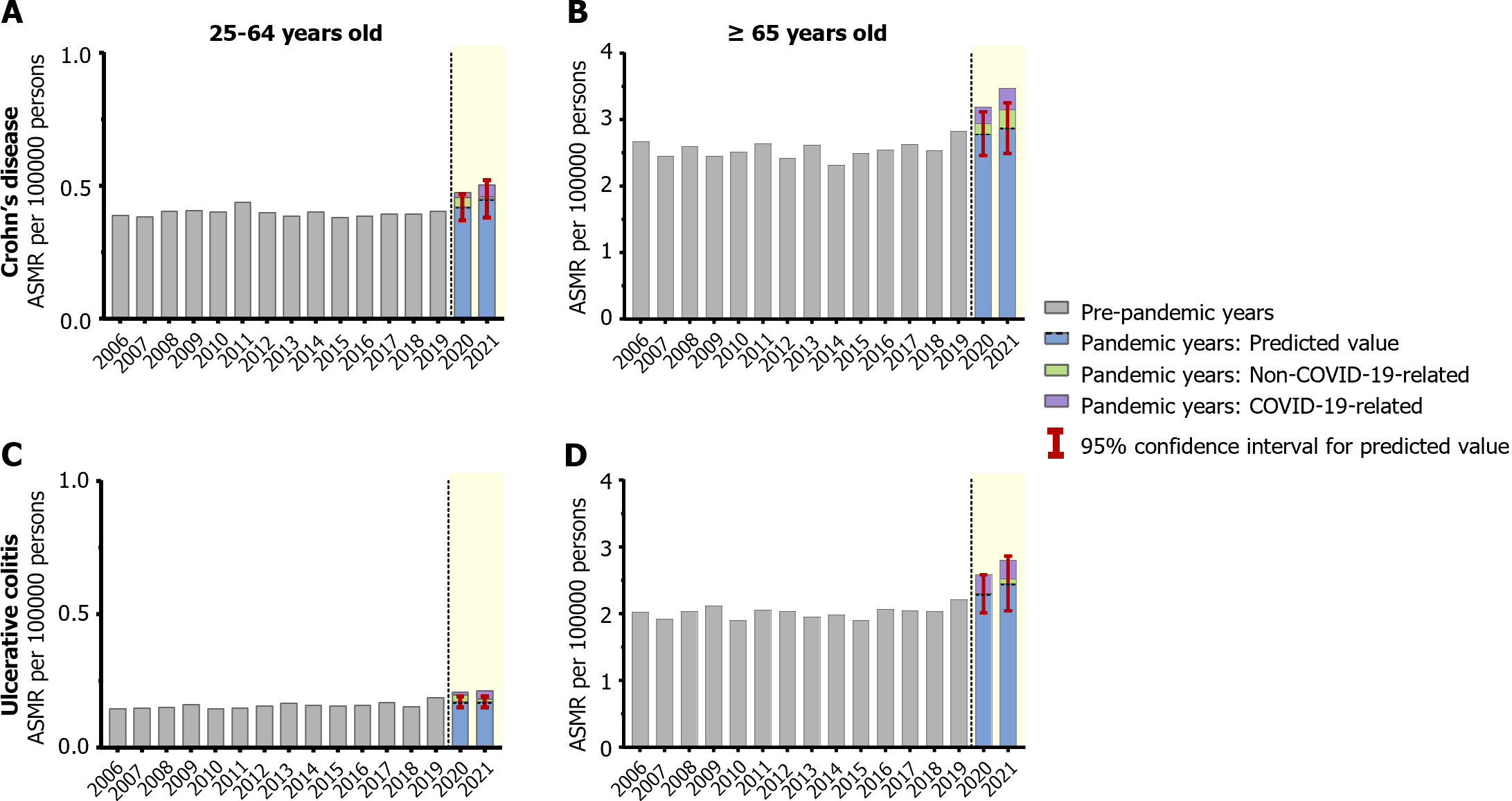
Mortality trends among CD and UC decedents from 2006 to 2021 stratified by age are shown in Figure 2. UC decedents aged 25-64 years demonstrated a 17.65% increase in non-COVID-19-related death during the pandemic (ASMR: 0.20 actual vs 0.17 predicted, 95%CI: 0.15-0.19) (Figure 2C). Detailed results can be found in Table 2.
Mortality trends among CD and UC decedents stratified by sex from 2006 to 2021 are shown in Supplementary Figure 1. Overall, no significant sex disparity was found among CD or UC decedents for excess non-COVID-19-related mortality, but males with UC had increased all-cause mortality in 2020 (2020 ASMR: 0.76 actual vs 0.68 predicted, 95%CI: 0.62-0.75). Most of the all-cause mortality for males was COVID-19-related. Detailed results can be found in Table 2.
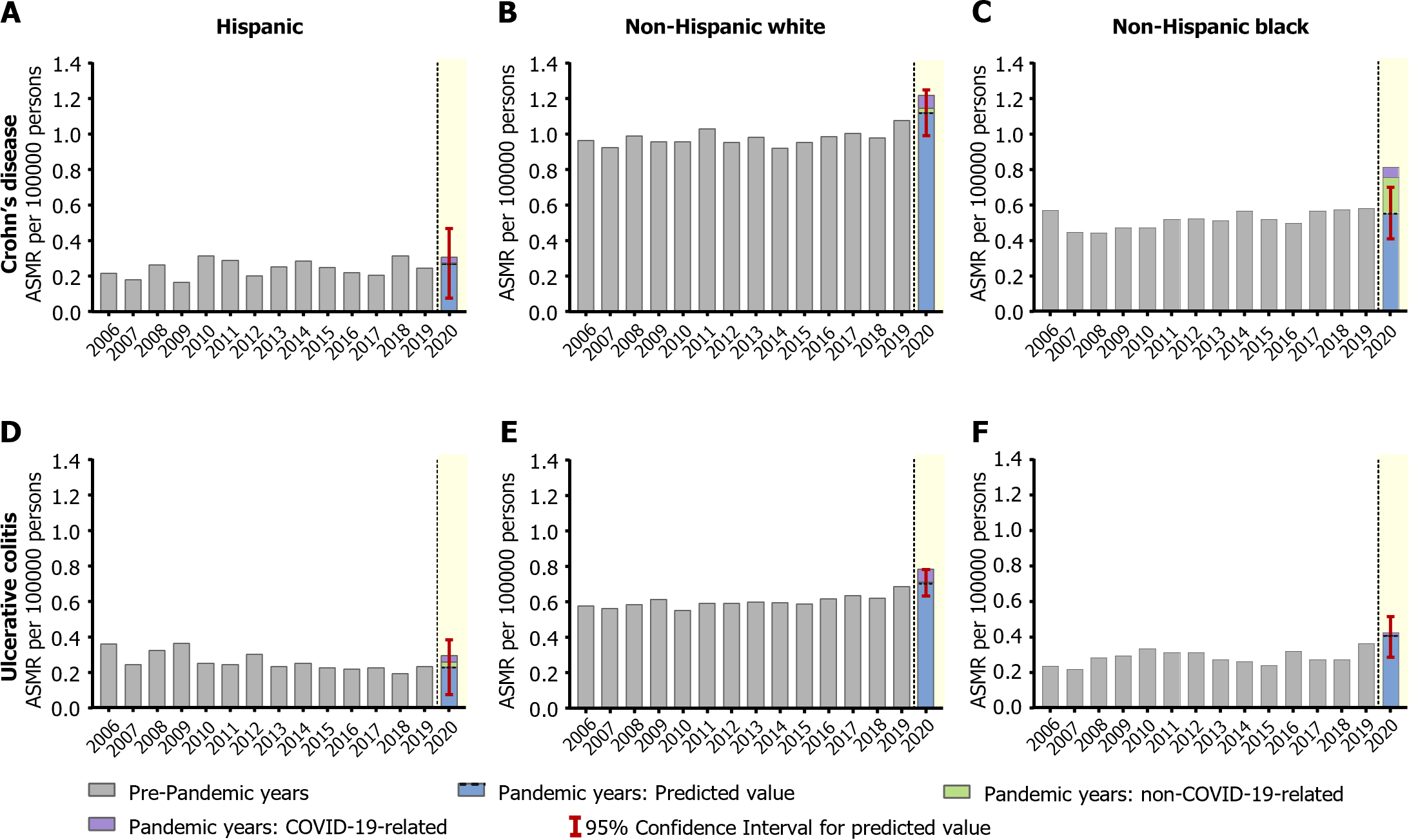
Mortality trends among CD and UC decedents stratified by race/ethnicity from 2006 to 2020 are shown in Figure 3. NHB CD decedents experienced a 36.36% increase in non-COVID-19-related mortality (2020 ASMR: 0.75 actual vs 0.55 predicted, 95%CI: 0.41-0.70) (Figure 3C). Non-Hispanic white UC decedents showed increased all-cause mortality in 2020 (2020 ASMR: 0.79 actual vs 0.71 predicted, 95%CI: 0.63-0.78) (Figure 3E). However, this was mainly COVID-19-related. Detailed results can be found in Table 2.
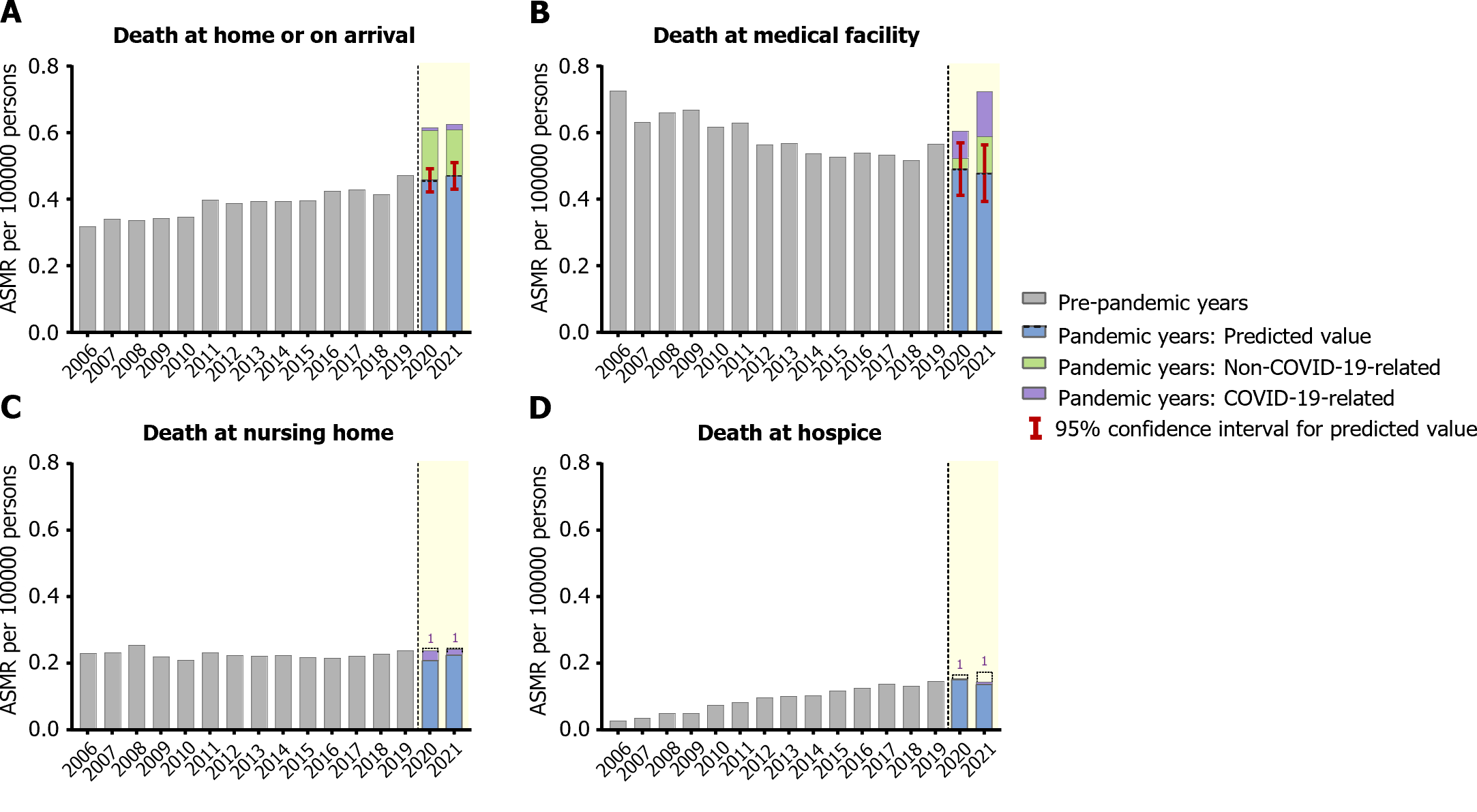
Figure 4 shows trends in IBD ASMR by location of death. Non-COVID-19-related IBD deaths at home or on arrival increased by 32.61% in 2020 and 29.79% in 2021 (2020 ASMR: 0.61 actual vs 0.46 predicted, 95%CI: 0.42-0.49, 2021 ASMR: 0.61 actual vs 0.47 predicted, 95%CI: 0.43-0.51). Non-COVID-19-related IBD deaths at medical facilities also increased by 22.92% in 2021 (2021 ASMR: 0.59 actual vs 0.48 predicted, 95%CI: 0.39-0.56). Additionally, non-COVID-19-related IBD deaths at hospice facilities decreased by 23.53% in 2021 (ASMR: 0.13 actual vs 0.17 predicted, 95%CI: 0.16-0.18) (Table 3).
| 2006 | 2019 | 2020 | 2021 | |||||||
| Observed all-cause | Predicted (95%CI) | Observed non-COVID | Increase (%)1 | Observed all-cause | Predicted (95%CI) | Observed non-COVID | Increase (%)1 | |||
| Home or on arrival | 0.32 | 0.47 | 0.62 | 0.46 (0.42-0.49) | 0.61 | 32.61 | 0.63 | 0.47 (0.43-0.51) | 0.61 | 29.79 |
| Medical facility | 0.73 | 0.56 | 0.60 | 0.49 (0.41-0.57) | 0.52 | 6.12 | 0.73 | 0.48 (0.39-0.56) | 0.59 | 22.92 |
| Nursing home | 0.23 | 0.24 | 0.24 | 0.24 (0.20-0.27) | 0.21 | -12.50 | 0.24 | 0.24 (0.20-0.28) | 0.22 | -8.33 |
| Hospice facility | 0.03 | 0.15 | 0.15 | 0.16 (0.14-0.17) | 0.15 | -6.25 | 0.14 | 0.17 (0.15-0.18) | 0.13 | -23.53 |
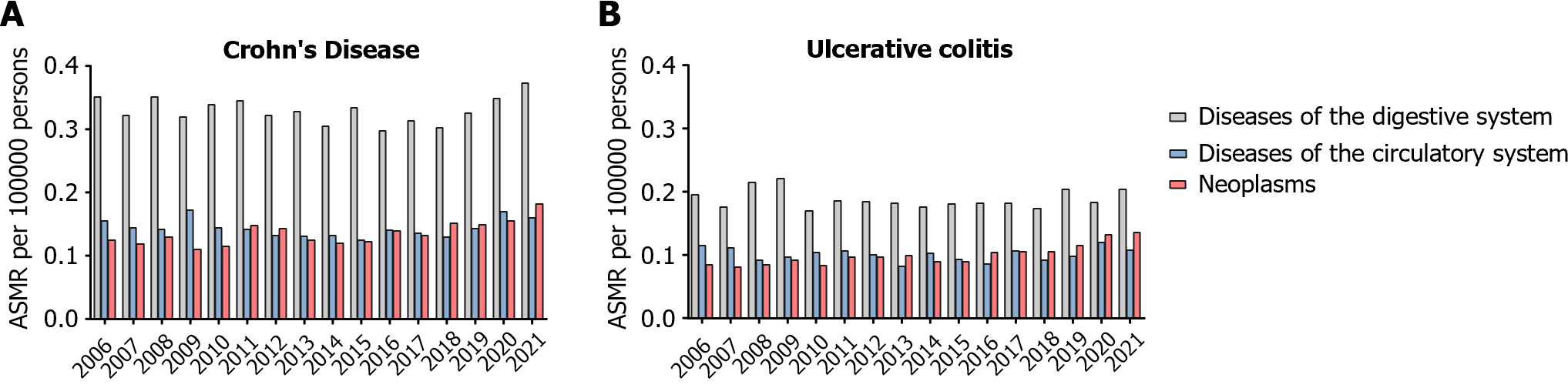
The top three primary causes of death for IBD decedents from 2006 to 2021 are shown in Figure 5. Diseases of the digestive system, circulatory system, and neoplasms consistently remained the top 3 leading causes of death in IBD decedents. Notably, the mortality rate from neoplasms reached an all-time high during the pandemic for both CD (2020 ASMR: 0.16; 2021 ASMR: 0.18) and UC (2020 ASMR: 0.13; 2021 ASMR: 0.14) decedents. Though, this increase was not higher than predicted (Supplementary Table 2). The top three primary causes of death for UC decedents aged 25-64 and for NHB CD decedents can also be found in Supplementary Figure 2.
We found higher-than-predicted non-COVID-19-related mortality rates among IBD patients during the pandemic using a large, nationally representative dataset, and identified key demographic characteristics associated with increased mortality rates. Furthermore, we found excess IBD-related mortality at home or on arrival, at medical facilities, and due to neoplasms increased during the pandemic. Taken together, our findings suggest that decreased access to healthcare may have influenced mortality among IBD patients during the pandemic.
Decreased access was likely initially due to mandated lockdowns, stay-at-home orders, and fear of contracting the virus. In fact, one study found that from the start of the pandemic to May 2020, utilization of all healthcare services decreased significantly, specifically with reductions in visits, diagnostics, and therapeutics[26]. Moreover, a retrospective analysis previously found that 2.8% of deaths at a tertiary care center during the pandemic were attributable to delayed presentation due to fear of coming to the hospital, and inadequate documentation of fear or delay in seeking care may have led to underestimation of its effect on mortality[27]. However, uncertainty surrounding COVID-19 continued well beyond the initial six months. The World Health Organization found that COVID-19 continued to disrupt essentially healthcare services in 90% of countries well into 2021[28]. However, this does not explain our findings of excess non-COVID-19-related death among UC but not CD decedents.
While it is not possible to know why only UC patients and not CD patients experienced excess non-COVID-19-related mortality due to a lack of data on potential causative factors, we speculate this may be related to differences in corticosteroid usage among these patients. Corticosteroid use at the time of COVID-19 infection is associated with worse COVID-19 outcomes in IBD patients[14]. Prolonged corticosteroid use in IBD patients is also associated with increased overall mortality compared to antitumor necrosis factor-α-directed therapy[29]. However, an analysis of United States claims data reported that 10%-24% of patients with UC had received corticosteroid treatment for more than three months of a 12-month study period[30]. Additionally, prior to the pandemic, CD patients were more likely to be started on biologic therapies than UC patients (19% vs 6%)[31]. At the start of the pandemic, expert recommendations initially suggested continuation but against initiation of biologics[32]. This likely led to further imbalance in use of biologic therapy among those with UC relative to CD, and thus potentially further exacerbated steroid use in UC patients.
UC patients aged 25-64 years, more specifically, experienced significant excess non-COVID-19-related mortality (17.65%) during the pandemic. We speculate that this could be due to mental and financial stressors which affected this age group more so than others[33,34]. A global survey found that people aged 18-35 years were more vulnerable to stress, depression, and anxiety compared to those > 36 years during the pandemic[35]. There was also an increase in unemployment among all ages, but especially among young adults[36].
When stratified by sex, there were no subgroups of IBD patients that were at particularly increased risk of non-COVID-19-related mortality. Only males with UC reached a significantly increased observed all-cause ASMR compared to predicted. However, this was mostly due to COVID-19-related ASMR. This finding is consistent with other studies that have shown that males have generally greater levels of excess mortality from COVID-19[37].
Stratification by race/ethnicity showed NHB CD decedents had significant excess non-COVID-19-related ASMR in 2020 (36.36%). The disproportionate impact of the pandemic on non-COVID-19-related and COVID-19-related mortality among black Americans has been well documented[38]. NHB CD patients may have more extensive inflammation than other races with CD and have higher hospitalization rates than NHB patients with UC. Additionally, NHB patients are less likely to be prescribed infliximab[39], which may have exacerbated steroid use in this subgroup during the pandemic and led to increased severity of their underlying CD leading to increased mortality as speculated above.
We also found significant excess non-COVID-19-related mortality at home or on arrival (2020: 32.61%; 2021: 29.79%) and in medical facilities (2021: 22.92%) among IBD decedents during the pandemic. This may suggest delayed presentation among IBD patients. Delays in presentation for other conditions, including acute myocardial ischemia and strokes, have been documented[40,41]. There was also decreased non-COVID-19-related ASMR at hospice facilities during the pandemic among IBD patients (2021: 23.53%). As patients eligible for hospice often have multiple comorbidities and are susceptible to severe COVID-19 infection, these patients may have experienced increased COVID-19-related mortality that therefore decreased the need for admission to hospice facilities. Moreover, fear of contracting COVID-19 may have led to decreased referrals to and utilization of hospice facilities[42].
On analysis of the top three primary causes of IBD-related death, neoplasms became an even more prominent cause of death in both CD and UC patients during the pandemic. This could have been due to delayed and disrupted cancer diagnosis and care during the pandemic as cancer service availability, including medical visits, surgeries, procedures, radiotherapy, and chemotherapy sessions, were reduced[43].
Our findings among IBD decedents are in line with prior studies that have similarly demonstrated excess non-COVID-19-related mortality during the pandemic among decedents with other chronic medical conditions, including cardiovascular disease, liver disease, diabetes mellitus and alcohol-use disorder[4,5,7,8]. These studies also used nationally representative mortality data and distinguished between excess all-cause and excess non-COVID-19-related mortality. Additionally, among liver disease and alcohol-use disorder related deaths, excess non-COVID-19-related mortality was similarly increased in younger patients compared to older patients and no differences were seen based on sex[5].
Our study has several important limitations. First, the cause of death from NVSS may be subject to erroneous documentation, possibly resulting in misclassification of COVID-19-related and non-COVID-19-related deaths among IBD decedents as well as possibly not capturing all truly IBD-related deaths. Especially early in the pandemic, reporting of COVID-19 infection as a cause of death was not reliable[44]. Additionally, reporting of cause of death may have been affected by the place of death, as it may have been more difficult to determine immediate cause of death for deaths at home/on arrival as opposed to deaths in a medical facility. Finally, we were unable to ascertain potentially confounding clinical factors such as medications, IBD disease activity, and nutritional status among decedents which could have contributed to mortality rates.
Despite these limitations, our study is strengthened by the long-term analysis of temporal trends based on comprehensive NVSS data, which comprises over 99% of annual death data across the United States. Additionally, mortality rates and causes of death among IBD patients remains extremely relevant to patients and is an important measurable outcome of disease. Future studies are necessary to better understand the underlying causes and to identify interventions that may prevent excess IBD death in future healthcare emergencies.
In conclusion, our study revealed a 15% increase in non-COVID-19-related ASMR among individuals with IBD during the COVID-19 pandemic. Specifically, 14% of excess mortality was related to UC, and 3% of excess mortality was related to CD in the United States. The surge in non-COVID-19-related ASMR during the pandemic was mostpronounced in younger UC patients and NHB CD patients. Due to the potential consequences of disrupted medical services, delayed diagnoses, and implementation of stay-at-home mandates, significant excess non-COVID-19-related mortality occurred at home or on arrival among IBD decedents during the pandemic. Our study highlights the need for more effective strategies to reduce excess mortality amongst IBD patients and other vulnerable subgroups in future health care crises.
Prior studies have shown that inflammatory bowel disease (IBD)-related mortality increased dramatically during the coronavirus disease 2019 (COVID-19) pandemic.
We aim to investigate the difference in excess mortality between COVID-19-related and non-COVID-19-related deaths in IBD-related decedents during the pandemic. We further explore disparities among subgroups within ulcerative colitis (UC) and Crohn’s disease (CD).
Utilizing Vital Statistics Online Data Portal of the National Vital Statistic System from January 1, 2006 through December 31, 2021, we focused on IBD-related decedents aged 25 years or older. We performed subgroup analyses including age, sex, race/ethnicity, place of death, and primary cause of death.
We used the direct model to calculate age-standardized mortality rates (ASMRs), with the 2010 United States Census Standard Population as the reference. Time series regression models predicted mortality rates in 2020 and 2021 based on trends from 2006 to 2019, estimating the pandemic’s impact on IBD-related mortality. The excess death was categorized into COVID-19-related and non-COVID-19-related.
A total of 49782 IBD-related deaths were documented during the study period. Non-COVID-19-related mortality among IBD decedents increased by 13.14% in 2020 and 18.12% in 2021. Notably, young UC patients and non-Hispanic black (NHB) CD patients increased at an unprecedented rate, 17.65% and 36.36%, respectively. Non-COVID-19-related deaths at home or on arrival at the hospital exhibited the most substantial upward trend during the pandemic, reaching 32.61% in 2020 and 29.79% in 2021.
Non-COVID-19-related ASMR for IBD-related deaths increased at alarming rates during the COVID-19 pandemic in the United States, particularly in younger age UC patients, and NHB CD patients.
Our findings have vital implications for public health strategies, emphasizing the need for enhanced surveillance of IBD patients. The research underscores the importance of placing greater attention on young UC and NHB CD patients during future healthcare crises. .
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
| 1. | CDC. Deaths by Week and State - Provisional Death Counts for COVID-19. [cited 10 August 2023]. Available from: https://www.cdc.gov/nchs/nvss/vsrr/covid19/index.htm. |
| 2. | COVID-19 Excess Mortality Collaborators. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020-21. Lancet. 2022;399:1513-1536. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 430] [Cited by in RCA: 960] [Article Influence: 320.0] [Reference Citation Analysis (2)] |
| 3. | Shiels MS, Almeida JS, García-Closas M, Albert PS, Freedman ND, Berrington de González A. Impact of Population Growth and Aging on Estimates of Excess U.S. Deaths During the COVID-19 Pandemic, March to August 2020. Ann Intern Med. 2021;174:437-443. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (1)] |
| 4. | Banerjee A, Chen S, Pasea L, Lai AG, Katsoulis M, Denaxas S, Nafilyan V, Williams B, Wong WK, Bakhai A, Khunti K, Pillay D, Noursadeghi M, Wu H, Pareek N, Bromage D, McDonagh TA, Byrne J, Teo JTH, Shah AM, Humberstone B, Tang LV, Shah ASV, Rubboli A, Guo Y, Hu Y, Sudlow CLM, Lip GYH, Hemingway H. Excess deaths in people with cardiovascular diseases during the COVID-19 pandemic. Eur J Prev Cardiol. 2021;28:1599-1609. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 101] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 5. | Yeo YH, He X, Ting PS, Zu J, Almario CV, Spiegel BMR, Ji F. Evaluation of Trends in Alcohol Use Disorder-Related Mortality in the US Before and During the COVID-19 Pandemic. JAMA Netw Open. 2022;5:e2210259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 46] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 6. | Zhao Y, Yeo YH, Samaan J, Lv F, He X, Gao N, Park J, Yang JD, Ayoub W, Odden MC, Ji F, Nguyen MH. Most excess years of potential life loss among individuals with cirrhosis during the pandemic were not related to COVID-19. Gut. 2023;72:1628-1630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Lv F, Gao X, Huang AH, Zu J, He X, Sun X, Liu J, Gao N, Jiao Y, Keane MG, Zhang L, Yeo YH, Wang Y, Ji F. Excess diabetes mellitus-related deaths during the COVID-19 pandemic in the United States. EClinicalMedicine. 2022;54:101671. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 28] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 8. | Gao X, Lv F, He X, Zhao Y, Liu Y, Zu J, Henry L, Wang J, Yeo YH, Ji F, Nguyen MH. Impact of the COVID-19 pandemic on liver disease-related mortality rates in the United States. J Hepatol. 2023;78:16-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 62] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 9. | Dahlhamer JM, Zammitti EP, Ward BW, Wheaton AG, Croft JB. Prevalence of Inflammatory Bowel Disease Among Adults Aged ≥18 Years - United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:1166-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 339] [Cited by in RCA: 477] [Article Influence: 53.0] [Reference Citation Analysis (0)] |
| 10. | Ye Y, Manne S, Treem WR, Bennett D. Prevalence of Inflammatory Bowel Disease in Pediatric and Adult Populations: Recent Estimates From Large National Databases in the United States, 2007-2016. Inflamm Bowel Dis. 2020;26:619-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 63] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 11. | Kassam Z, Belga S, Roifman I, Hirota S, Jijon H, Kaplan GG, Ghosh S, Beck PL. Inflammatory bowel disease cause-specific mortality: a primer for clinicians. Inflamm Bowel Dis. 2014;20:2483-2492. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 12. | Follin-Arbelet B, Cvancarova Småstuen M, Hovde Ø, Jelsness-Jørgensen LP, Moum B. Mortality in Patients with Inflammatory Bowel Disease: Results from 30 Years of Follow-up in a Norwegian Inception Cohort (the IBSEN study). J Crohns Colitis. 2023;17:497-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 13. | Jess T, Frisch M, Simonsen J. Trends in overall and cause-specific mortality among patients with inflammatory bowel disease from 1982 to 2010. Clin Gastroenterol Hepatol. 2013;11:43-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 135] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 14. | Singh S, Khan A, Chowdhry M, Bilal M, Kochhar GS, Clarke K. Risk of Severe Coronavirus Disease 2019 in Patients With Inflammatory Bowel Disease in the United States: A Multicenter Research Network Study. Gastroenterology. 2020;159:1575-1578.e4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 93] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 15. | Kappelman MD, Porter CQ, Galanko JA, Rifas-Shiman SL, Ollendorf DA, Sandler RS, Finkelstein JA. Utilization of healthcare resources by U.S. children and adults with inflammatory bowel disease. Inflamm Bowel Dis. 2011;17:62-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 107] [Cited by in RCA: 101] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 16. | Keller DS, Windsor A, Cohen R, Chand M. Colorectal cancer in inflammatory bowel disease: review of the evidence. Tech Coloproctol. 2019;23:3-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 174] [Article Influence: 29.0] [Reference Citation Analysis (0)] |
| 17. | Shah SC, Itzkowitz SH. Colorectal Cancer in Inflammatory Bowel Disease: Mechanisms and Management. Gastroenterology. 2022;162:715-730.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 445] [Article Influence: 148.3] [Reference Citation Analysis (0)] |
| 18. | Ungaro RC, Chou B, Mo J, Ursos L, Twardowski R, Candela N, Colombel JF. Impact of COVID-19 on Healthcare Resource Utilisation Among Patients with Inflammatory Bowel Disease in the USA. J Crohns Colitis. 2022;16:1405-1414. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Te Groen M, Derks MEW, Kuijpers CCHJ, Nagtegaal ID, Hoentjen F. Reduction in Inflammatory Bowel Disease Healthcare During the Coronavirus Disease 2019 Pandemic: A Nationwide Retrospective Cohort Study. Gastroenterology. 2021;160:935-937.e1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Roy CM, Bollman EB, Carson LM, Northrop AJ, Jackson EF, Moresky RT. Assessing the indirect effects of COVID-19 on healthcare delivery, utilization and health outcomes: a scoping review. Eur J Public Health. 2021;31:634-640. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 125] [Cited by in RCA: 122] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 21. | Falk G, Romero PD, Nicchitta IA, Nyhof EC. Unemployment rates during the COVID-19 pandemic. [cited 10 August 2023]. Available from: https://crsreports.congress.gov/product/pdf/R/R46554. |
| 22. | Rodrigues M, Silva R, Franco M. COVID-19: Financial Stress and Well-Being in Families. J Fam Issues. 2023;44:1254-1275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 23. | Faust JS, Shah SB, Du C, Li SX, Lin Z, Krumholz HM. Suicide Deaths During the COVID-19 Stay-at-Home Advisory in Massachusetts, March to May 2020. JAMA Netw Open. 2021;4:e2034273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 70] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 24. | CDC. CDC WONDER. [cited 10 August 2023]. Available from: https://wonder.cdc.gov. |
| 25. | CDC. National Center for Health Statistics. [cited 15 August 2023]. Available from: https://www.cdc.gov/nchs/index.htm. |
| 26. | Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, To EJ, Jones M, Kitchener E, Fox M, Johansson M, Lang E, Duggan A, Scott I, Albarqouni L. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. 2021;11:e045343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 748] [Cited by in RCA: 775] [Article Influence: 193.8] [Reference Citation Analysis (1)] |
| 27. | Bansal S, Roy M, Chatterjee T, Roy AK. Deaths due to delayed presentation to the hospital from fear of contracting COVID-19 during lockdown period: a tertiary care center experience. J Community Hosp Intern Med Perspect. 2021;11:299-301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 28. | World Health Organization. COVID-19 continues to disrupt essential health services in 90% of countries. [cited 15 August 2023]. Available from: https://www.who.int/news/item/23-04-2021-covid-19-continues-to-disrupt-essential-health-services-in-90-of-countries. |
| 29. | Lewis JD, Scott FI, Brensinger CM, Roy JA, Osterman MT, Mamtani R, Bewtra M, Chen L, Yun H, Xie F, Curtis JR. Increased Mortality Rates With Prolonged Corticosteroid Therapy When Compared With Antitumor Necrosis Factor-α-Directed Therapy for Inflammatory Bowel Disease. Am J Gastroenterol. 2018;113:405-417. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 118] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 30. | Rubin DT, Mody R, Davis KL, Wang CC. Real-world assessment of therapy changes, suboptimal treatment and associated costs in patients with ulcerative colitis or Crohn's disease. Aliment Pharmacol Ther. 2014;39:1143-1155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 31. | Siegel CA, Yang F, Eslava S, Cai Z. Treatment Pathways Leading to Biologic Therapies for Ulcerative Colitis and Crohn's Disease in the United States. Clin Transl Gastroenterol. 2020;11:e00128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 57] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 32. | Zingone F, Buda A, Savarino EV. Starting a Biologic Therapy in IBD Patients Amid COVID-19: Hold, Careful Monitoring, or Testing? J Crohns Colitis. 2020;14:1785. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 33. | Russ TC, Stamatakis E, Hamer M, Starr JM, Kivimäki M, Batty GD. Association between psychological distress and mortality: individual participant pooled analysis of 10 prospective cohort studies. BMJ. 2012;345:e4933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 364] [Cited by in RCA: 394] [Article Influence: 30.3] [Reference Citation Analysis (0)] |
| 34. | Mode NA, Evans MK, Zonderman AB. Race, Neighborhood Economic Status, Income Inequality and Mortality. PLoS One. 2016;11:e0154535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 62] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 35. | Varma P, Junge M, Meaklim H, Jackson ML. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Prog Neuropsychopharmacol Biol Psychiatry. 2021;109:110236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 236] [Cited by in RCA: 372] [Article Influence: 93.0] [Reference Citation Analysis (0)] |
| 36. | Moen P, Pedtke JH, Flood S. Disparate Disruptions: Intersectional COVID-19 Employment Effects by Age, Gender, Education, and Race/Ethnicity. Work Aging Retire. 2020;6:207-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 52] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 37. | Alwani M, Yassin A, Al-Zoubi RM, Aboumarzouk OM, Nettleship J, Kelly D, Al-Qudimat AR, Shabsigh R. Sex-based differences in severity and mortality in COVID-19. Rev Med Virol. 2021;31:e2223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 75] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 38. | Cronin CJ, Evans WN. Excess mortality from COVID and non-COVID causes in minority populations. Proc Natl Acad Sci U S A. 2021;118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 39. | Nguyen GC, LaVeist TA, Harris ML, Wang MH, Datta LW, Brant SR. Racial disparities in utilization of specialist care and medications in inflammatory bowel disease. Am J Gastroenterol. 2010;105:2202-2208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 104] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 40. | Aldujeli A, Hamadeh A, Briedis K, Tecson KM, Rutland J, Krivickas Z, Stiklioraitis S, Briede K, Aldujeili M, Unikas R, Zaliaduonyte D, Zaliunas R, Vallabhan RC, McCullough PA. Delays in Presentation in Patients With Acute Myocardial Infarction During the COVID-19 Pandemic. Cardiol Res. 2020;11:386-391. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 68] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 41. | Schirmer CM, Ringer AJ, Arthur AS, Binning MJ, Fox WC, James RF, Levitt MR, Tawk RG, Veznedaroglu E, Walker M, Spiotta AM; Endovascular Research Group (ENRG). Delayed presentation of acute ischemic strokes during the COVID-19 crisis. J Neurointerv Surg. 2020;12:639-642. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 111] [Cited by in RCA: 121] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 42. | Gergerich E, Mallonee J, Gherardi S, Kale-Cheever M, Duga F. Strengths and Struggles for Families Involved in Hospice Care During the COVID-19 Pandemic. J Soc Work End Life Palliat Care. 2021;17:198-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 43. | Riera R, Bagattini ÂM, Pacheco RL, Pachito DV, Roitberg F, Ilbawi A. Delays and Disruptions in Cancer Health Care Due to COVID-19 Pandemic: Systematic Review. JCO Glob Oncol. 2021;7:311-323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 114] [Cited by in RCA: 299] [Article Influence: 74.8] [Reference Citation Analysis (0)] |
| 44. | Iuliano AD, Chang HH, Patel NN, Threlkel R, Kniss K, Reich J, Steele M, Hall AJ, Fry AM, Reed C. Estimating under-recognized COVID-19 deaths, United States, march 2020-may 2021 using an excess mortality modelling approach. Lancet Reg Health Am. 2021;1:100019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |