Published online May 7, 2024. doi: 10.3748/wjg.v30.i17.2332
Peer-review started: January 3, 2024
First decision: January 16, 2024
Revised: February 13, 2024
Accepted: March 27, 2024
Article in press: March 27, 2024
Published online: May 7, 2024
Processing time: 122 Days and 17.3 Hours
Hemorrhoidal artery embolization (Emborrhoid) is a novel method for the treatment of severe hemorrhoidal bleeding. Despite having a technical success rate of 93%-100%, the clinical success ranges between 63% and 94%, with a rebleeding rate of 13.6%.
To evaluate the effectiveness of this procedure in reducing hemorrhoidal flow and hemorrhoidal bleeding.
This prospective observational pilot study was conducted at Division of General Surgery 1 and Tertiary Referral Pelvic Floor Center, Treviso Regional Hospital, Italy. In a 2 months period (February-March 2022), consecutive patients with hemorrhoidal bleeding scores (HBSs) ≥ 4, Goligher scores of II or III, failure of non-operative management, and a candidate for Emborrhoid were included. Endoanal ultrasound with eco-Doppler was performed preoperatively and 1 month after the procedure. The primary endpoint was to quantify the changes in arterial hemorrhoidal flow after treatment. The secondary endpoint was to evaluate the correlation between the flow changes and the HBS.
Eleven patients underwent Emborrhoid. The overall pretreatment mean systolic peak (MSP) was 14.66 cm/s. The highest MSP values were found in the anterior left lateral (17.82 cm/s at 1 o’clock and 15.88 cm/s at 3 o’clock) and in the posterior right lateral (14.62 cm/s at 7 o’clock and 16.71 cm/s at 9 o’clock) quadrants of the anal canal. After treatment, the overall MSP values were significantly reduced (P = 0.008) although the correlation between MSP and HBS changes was weak (P = 0.570). A statistical difference was found between distal embolization compared with proximal embolization (P = 0.047). However, the coil landing zone was not related to symptoms improvement (P = 1.000). A significant difference in MSP changes was also reported between patients with type 1 and type 2 superior rectal artery (SRA) anatomy (P = 0.040). No relationship between hemorrhoidal grades (P = 1.000), SRA anatomy (P = 1.000) and treatment outcomes was found.
The preliminary findings of this pilot study confirm that Emborrhoid was effective in reducing the arterial hemorrhoidal flow in hemorrhoidal disease. However, the correlation between the post-operative MSP and HBS changes was weak. Hemorrhoidal grade, SRA anatomy and type of embolization were not related to treatment outcomes.
Core Tip: This was a prospective observational pilot study seeking to evaluate the changes in the arterial hemorrhoidal flow after hemorrhoidal artery embolization, and the correlation between the mean systolic peak and the hemorrhoidal bleeding score changes. Embolization was effective in reducing the arterial hemorrhoidal flow in hemorrhoidal disease, however the correlation between flow and symptoms was weak.
- Citation: Tutino R, Stecca T, Farneti F, Massani M, Santoro GA. Transanal eco-Doppler evaluation after hemorrhoidal artery embolization. World J Gastroenterol 2024; 30(17): 2332-2342
- URL: https://www.wjgnet.com/1007-9327/full/v30/i17/2332.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i17.2332
The main vascular hemorrhoidal supply is provided by the superior rectal artery (SRA), which splits into three to five distal branches[1,2]. Panneau et al[3] described three patterns of arterial hemorrhoidal vascularization: (1) Type 1 consists of one or more dominant SRAs without hypertrophy of the middle rectal artery (MRA); (2) Type 2 includes unilateral hypertrophy of the SRA and hypertrophy of the contralateral MRA; (3) Type 3 includes bilateral hypertrophy of the MRA without hypertrophy of the SRA. Schuurman et al[4] found that vascularization of the corpus cavernosum recti and distal rectum is provided almost exclusively by branches of the SRA, and that the distal distribution is not limited to sectorial o’clock positions. By using endoanal duplex color, Ratto et al[5] showed that the hemorrhoidal arteries lie in the perirectal fat outside the rectal walls at 6.5 cm and 4.0 cm over the anorectal junction (ARJ) where they are located in the right and left lateral and in the right and left posterolateral sectors. No hemorrhoidal arteries were found in the right and left anterolateral sectors. From 3 cm at the lowest 2 cm above the ARJ, arteries move toward the submucosa and distribute circumferentially in each quadrant[6].
Symptomatic hemorrhoids are associated to destructive changes in the supporting connective tissue with downward displacement of normal anal cushions and to abnormal arterial supply to the anal canal with hyperperfusion, dilation and distortion of the hemorrhoidal plexus[7-9]. The hemorrhoidal bleeding score (HBS; range 0-9) has been proposed to evaluate the severity of this symptom[10].
In patients with early stage hemorrhoidal disease, if non-operative treatment fails, minimally invasive techniques including rubber band ligation, injection sclerotherapy, infrared coagulation, cryosurgery, and laser are proposed[11]. In advanced stages, traditional hemorrhoidectomy, stapled mucoprolapsectomy or transanal hemorrhoidal dearterialization (THD) are used to treat both the prolapse and the bleeding[12].
Hemorrhoidal artery embolization (Emborrhoid) is a novel method for the treatment of severe bleeding. Through the catheterization of the femoral or radial arteries and a selective angiogram of the inferior mesenteric artery, embolic agents are used to occlude the SRA branches[13]. Despite a technical success rate up to 93%-100%, clinical success was reported in 63%-94% of cases with a rebleeding rate of 13.6%. It was shown that in 24% of cases, rebleeding was due to the presence of a significant MRA[14]. There are no data in the literature that evaluated the changes in the hemorrhoidal arterial flow after embolization.
The primary endpoint of this study was to quantify the reduction in the blood supply occurring after Emborrhoid by using transanal eco-Doppler. The secondary endpoint was to evaluate the correlation between the flow reduction and the hemorrhoidal bleeding.
A prospective observational pilot study was conducted at the Division of General Surgery 1, Treviso Regional Hospital, Italy. In a 2-mo period (February-March 2022), consecutive patients who were candidates for hemorrhoidal artery embolization were included. The study was approved by the local Ethical Committee (No. 1286/CE Marca) and registered on clinicaltrials.gov (NCT05627999). All patients gave written informed consent.
Indications to the procedure were HBS ≥ 4, Goligher score II or III, more than 18 years of age, failure of non-operative management (lifestyle change, dietary modification, supplemental fibers, and over-the-counter treatment). Exclusion criteria were a Goligher score of IV, pregnancy, previous hemorrhoidal surgery, inflammatory bowel disease. Use of anticoagulants or anti-aggregants was not considered an exclusion criterion[15].
Patients underwent history and physical (proctological) examination and assessment of the Goligher and HBS scores by a single operator (RT) before and 1 mo after the procedure. Symptom improvement was defined a reduction of at least three points of the HBS score.
To measure the hemorrhoidal artery flow, transanal ultrasonography with eco-color Doppler was performed the same day of the procedure and at 1-mo follow-up at the Tertiary Referral Pelvic Floor Center, Treviso Regional Hospital, Italy by a single expert operator, who was blinded at the clinical findings. Data on SRA anatomy[3], type of embolization (distal or proximal) and the coil landing zone (distal vs proximal) were collected. Relationships between hemorrhoidal grade and treatment outcome, between changes in the mean arterial systolic peak (MSP) and the type of embolization (distal or proximal) and between the SRA anatomy[3], the coil landing zone (distal vs proximal) and treatment outcomes were analyzed. The correlation between changes in the MSP and the HBS score before and after treatment was also evaluated. Post-procedural complications were reported according to Clavien-Dindo classification[16].
Ultrasound was performed by using a Flexfocus 5000 (BK Medical, Herlev, Denmark) with an endocavitary transducer (3DX14L4-9038, BK Medical), 16 mm diameter, frequency range 4-14 MHz, focal range 3-60 mm, linear array with 65 mm acoustic surface and automatic three-dimensional acquisition. Before examination, patients were administered two enemas to flush the rectum and were placed in the left lateral position. Close contact of the transducer with the rectal mucosa was maintained while carefully avoiding excessive pressure on the rectal wall to minimize artifacts due to arterial compression. The same care was taken to maintain the transducer perpendicular to the examined structures in order to have a perpendicular angle of intersection between the Doppler beam and the vessels. Angle correction was used to adjust the angulation of the ultrasound beam and standardize the calculations of the velocity flow.
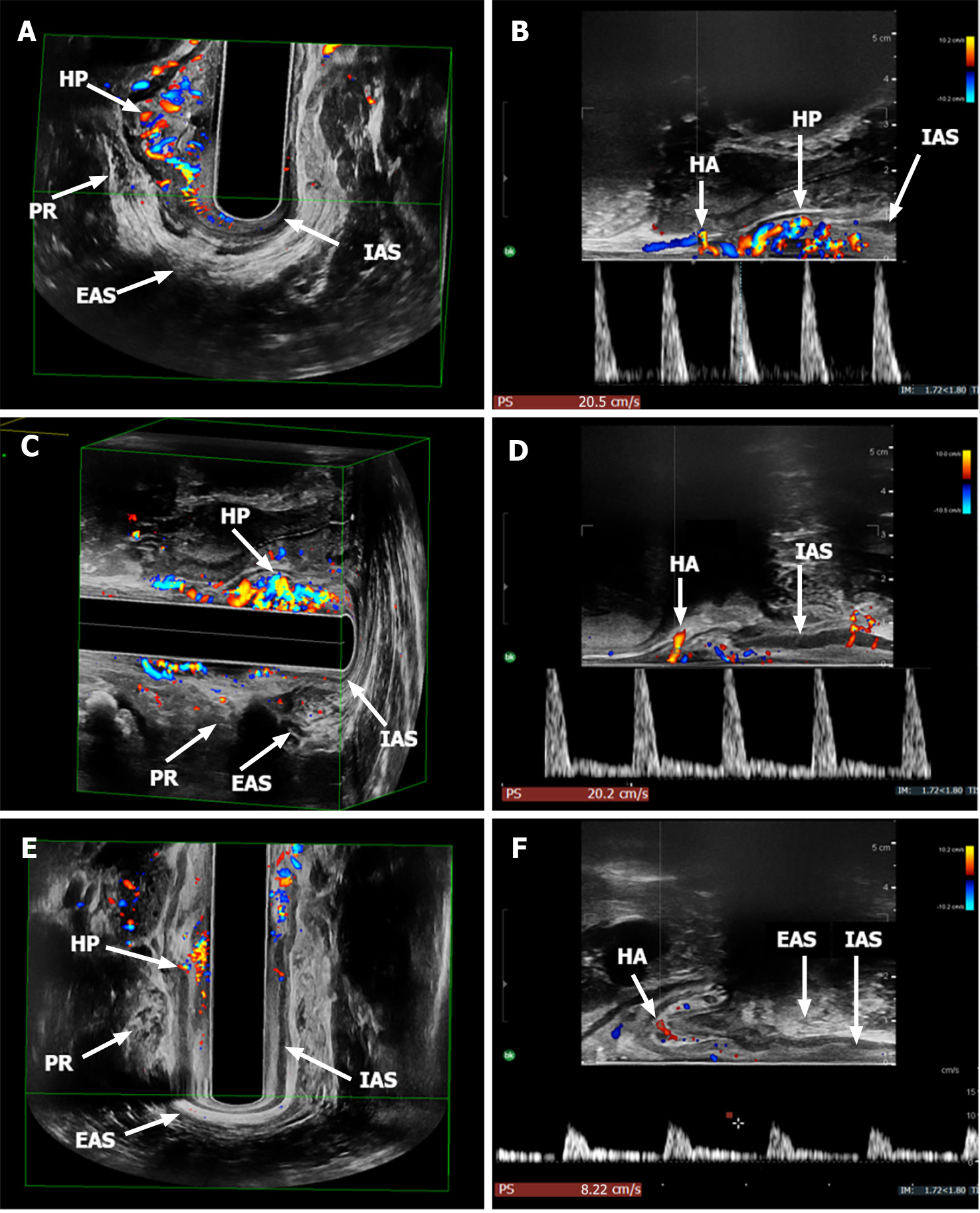
According to Ratto et al[5], the hemorrhoidal arterial flow was assessed in the 1, 3, 5, 6, 7, 9, 11, and 12 o’clock positions 2 cm above the ARJ, localized by ultrasound at the proximal edge of the puborectalis sling (Figure 1). Pulsed wave Doppler was used to measure the peak systolic velocity (cm/s), corresponding to the tallest peak in the spectrum window (Figure 2). For each investigated sector, pictures graphically displaying the flow velocity over time were obtained for reviewing after the examination.
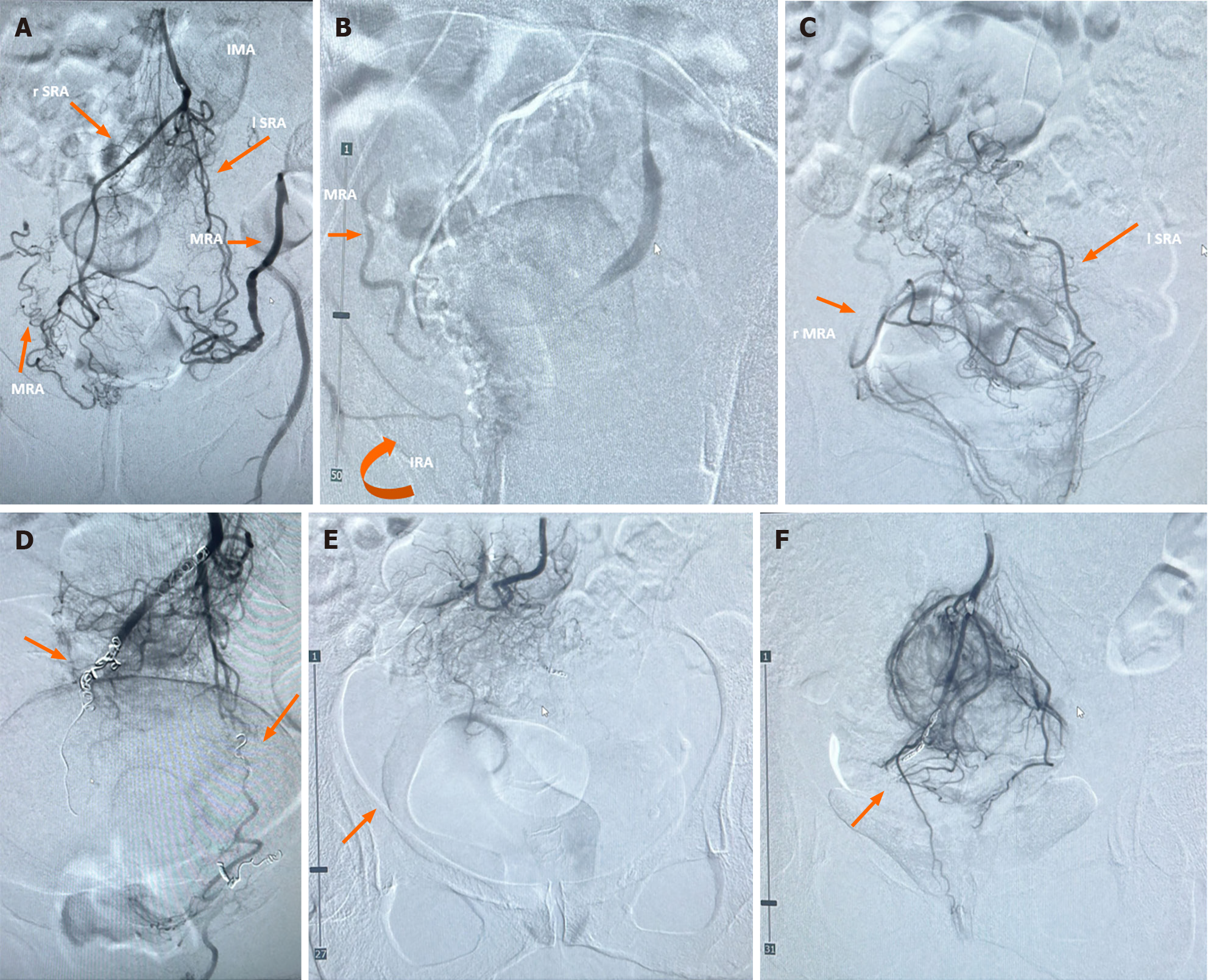
Embolization was performed as described by Vidal et al[1] under local anesthesia via the femoral or radial routes. No prophylactic antibiotic was given. The inferior mesenteric artery was catheterized using a 4 Fr Simmons catheter (Cordis Corp, Bridgewater, NJ, United States) and the SRAs were then catheterized with a microcatheter (Direxion HI-FLO; Boston Scientific, Marlborough, MA, United States) and a microwire (0.16-inch Fathom; Boston Scientific; Figure 3A-C). In distal embolization, each superior rectal branch was selectively embolized as distally as possible with 2–3 pushable coils, usually 3 mm in diameter (0.018 VortX; Boston Scientific). In proximal embolization, one or two coils, usually 4 mm in diameter (0.018 VortX; Boston Scientific) were deployed before the bifurcation into the main branch of the SRA. If a middle or inferior rectal artery anastomosis was observed on one or both sides of the hemorrhoidal plexus from the right or left internal iliac arteries, treatment was by selective catheterization of the distal branches of the SRA with a microcatheter and slow injection of a small amount of biocompatible, hydrophilic, non-resorbable microspheres (700 μm in diameter, acrylic polymer; Embosphere; Merit Medical, South Jordan, UT, United States) until the anastomosis was occluded. Then the distal branches of the SRA were embolized with pushable coils as previously described. Embolization was carried out until the angiographic endpoint of neither flow in the distal branches of the SRA or in the hemorrhoidal terminal branches (Figure 3D-F). At the end of the procedure, hemostasis of the femoral or radial arteries was achieved by manual compression. Patients were sent home the day after the procedure.
Descriptive data were analyzed using SPSS version 16 for Windows (SPSS Inc., Chicago, IL, United States). The results were reported as mean ± SD, median (range) and number (percentage) of patients. Overall and sectorial mean arterial systolic peaks were compared preoperatively and at 1-mo follow-up by using the Student t-test. Relationships between MSP changes, treatment outcomes and anatomical and technical details were analyzed by using the Student t-test and the chi-squared test. A P value of < 0.05 was considered statistically significant. The linear correlation between changes in MSP and changes in HBS was calculated using Pearson’s correlation coefficient.
Eleven patients, consisting of five women and six men with median of age 52.6 (range 28-75) years and who are candidates for Emborrhoid, were included in the study. Patient demographics and pre-treatment symptom severity are shown in Table 1. Three patients (27.3%) had Goligher grade 2, and eight patients (72.7%) had Goligher grade 3 hemorrhoids. Median HBS was 4 (range 4-6). No major comorbidities were reported. In a patient on oral anticoagulant therapy for chronic atrial fibrillation, the therapy was discontinued and replaced with low molecular weight heparin for the procedure.
| Patient | Age | Sex | Comorbidities | Anticoagulant therapy | Goligher score | Pre-treatment HBS |
| 1 | 56 | F | No comorbidities | No therapy | 3 | 5 |
| 2 | 43 | F | No comorbidities | No therapy | 3 | 6 |
| 3 | 75 | M | Atrial fibrillation | Warfarin | 3 | 4 |
| 4 | 54 | F | Hypothyroidism | No therapy | 2 | 5 |
| 5 | 62 | M | No comorbidities | No therapy | 3 | 6 |
| 6 | 53 | M | No comorbidities | No therapy | 3 | 3 |
| 7 | 46 | F | No comorbidities | No therapy | 2 | 4 |
| 8 | 46 | M | No comorbidities | No therapy | 3 | 3 |
| 9 | 63 | F | No comorbidities | No therapy | 3 | 4 |
| 10 | 55 | M | No comorbidities | No therapy | 2 | 5 |
| 11 | 28 | M | No comorbidities | No therapy | 3 | 3 |
The overall pre-treatment MSP was 14.66 cm/s (SD ± 1.93). Sectorial analysis showed that the highest values were found in the anterior left lateral (17.82 cm/s at 1 o’clock, 15.88 cm/s at 3 o’clock positions) and in the posterior right lateral (14.62 cm/s at 7 o’clock and 16.71 cm/s at 9 o’clock positions) quadrants of the anal canal. The lowest values were registered at 5 o’clock (13.03 cm/s) and 11 o’clock (12.74 cm/s) positions (Table 2, Figure 4A-D).
| Patient | 1 o’clock | 3 o’clock | 5 o’clock | 6 o’clock | 7 o’clock | 9 o’clock | 11 o’clock | 12 o’clock | ||||||||
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | |
| 1 | 9.61 | 13.10 | 5.12 | 5.44 | 9.50 | 6.19 | 20.50 | 14.90 | 15.00 | 9.93 | 7.47 | 10.80 | 20.10 | 17.40 | 6.62 | 13.00 |
| 2 | 20.40 | 5.12 | 24.91 | 16.10 | 15.90 | 8.11 | 24.90 | 13.10 | 10.90 | 6.62 | 15.40 | 14.90 | 6.50 | 8.11 | 10.40 | 20.50 |
| 3 | 17.00 | 19.90 | 10.70 | 17.00 | 13.70 | 19.40 | 8.86 | 8.97 | 15.80 | 12.40 | 8.97 | 22.60 | 12.00 | 14.40 | 20.00 | 14.90 |
| 4 | 13.10 | 20.40 | 18.50 | 20.40 | 16.19 | 7.36 | 6.19 | 6.83 | 12.00 | 9.61 | 19.40 | 15.80 | 13.00 | 8.00 | 21.00 | 24.90 |
| 5 | 25.40 | 25.20 | 16.90 | 10.60 | 6.62 | 7.58 | 8.65 | 8.00 | 13.60 | 10.60 | 26.40 | 20.20 | 19.40 | 14.10 | 15.00 | 7.47 |
| 6 | 20.50 | 14.50 | 15.50 | 8.43 | 8.11 | 13.00 | 7.79 | 9.39 | 13.20 | 8.22 | 12.80 | 14.30 | 7.36 | 13.70 | 10.10 | 5.87 |
| 7 | 17.70 | ND | 16.40 | ND | 8.22 | ND | 8.86 | ND | 19.40 | ND | 13.80 | ND | 8.11 | ND | 8.65 | ND |
| 8 | 17.40 | 20.40 | 15.60 | 13.60 | 8.11 | 8.65 | 12.70 | 8.22 | 15.50 | 7.79 | 25.00 | 15.70 | 20.50 | 15.30 | 15.50 | 8.00 |
| 9 | 24.00 | 20.40 | 25.00 | 6.51 | 8.00 | 6.40 | 15.70 | 8.22 | 11.20 | 12.20 | 18.60 | 14.30 | 11.00 | 19.00 | 16.20 | 8.86 |
| 10 | 5.90 | 14.10 | 13.00 | 13.00 | 20.00 | 11.60 | 7.79 | 7.79 | 8.22 | 8.97 | 10.00 | 4.38 | 12.70 | 8.00 | 5.70 | 5.87 |
| 11 | 25.00 | ND | 13.10 | ND | 29.00 | ND | 25.00 | ND | 26.00 | ND | 26.00 | ND | 9.50 | ND | 15.20 | ND |
| Mean | 17.82 | 17.01 | 15.88 | 12.34 | 13.03 | 9.81 | 13.36 | 9.49 | 14.62 | 9.59 | 16.71 | 14.77 | 12.74 | 13.11 | 13.12 | 12.15 |
The radial artery was catheterized in 7 patients and the femoral artery was catheterized in 4. Eight patients (72.7%) had type 1 SRA anatomy and three patients (27.3%) had type 2 SRA anatomy (Table 3). Embolization was performed distally in 8 patients (72.7%) and proximally in 3 patients (27.3%). In patients with type 2 SRA anatomy, the SRA/MRA anastomosis was also embolized (Table 3). The angiographic complete interruption of the blood flow in the distal branches of the SRA was achieved in all cases (technical success of the procedure 100%).
| Patient | SRA classification | Type of embolization | Pre-treatment MSP | Post-treatment MSP | Pre-treatment HBS | Post-treatment HBS |
| 1 | Type 1 | Distal (particles and coils) | 11.74 | 11.34 | 5 | 0 |
| 2 | Type 1 | Distal (particles and coils) | 16.16 | 11.57 | 6 | 0 |
| 3 | Type 2 | Proximal (particles and coils; coils in SRA/MRA anastomosis) | 13.38 | 16.20 | 4 | 4 |
| 4 | Type 1 | Proximal (particles and coils) | 14.92 | 14.16 | 5 | 0 |
| 5 | Type 1 | Distal (particles and coils) | 16.50 | 12.97 | 6 | 4 |
| 6 | Type 2 | Distal (particles and coils; particles and coils in SRA/MRA anastomosis) | 11.92 | 10.93 | 3 | 0 |
| 7 | Type 1 | Distal (particles and coils) | 12.64 | ND | 4 | ND |
| 8 | Type 1 | Distal (particles and coils) | 16.29 | 12.21 | 3 | 0 |
| 9 | Type 1 | Distal (particles distally; one coil proximal) | 16.21 | 11.99 | 4 | 4 |
| 10 | Type 1 | Distal (coils) | 10.41 | 9.21 | 5 | 3 |
| 11 | Type 2 | Proximal (particles and coils; particles and coils in SRA/MRA anastomosis) | 21.10 | ND | 3 | ND |
Four patients (36.4%) reported post-operative complications, including one patient C-D 1, two patients C-D 2 and one patient C-D 3b. Complications included acute urine retention, orchitis, radial artery thrombosis with deep brachial vein and superficial cephalic vein thrombosis. One patient reported severe hemorrhoidal bleeding requiring transfusions and an emergency excisional hemorrhoidectomy. In that case, it was not possible to perform the post-operative Doppler assessment.
After 1 mo, a follow-up evaluation was performed in 9 patients because 1 refused to repeat an endoanal ultrasound. All patients had persisting prolapse. Bleeding was absent or slight in 5 patients (55.5%, median HBS 1; Figure 4E and F) and persistent in 4 (44.5%, mean HBS 3.75; Figure 5A).
Overall post-treatment MSP was 12.29 cm/s (SD ± 2.68). The difference between pre- and post-treatment overall MSP was significant (P = 0.008) (Table 4, Figure 5B). Sectorial analyses showed that the MSP reduction was significant only at 7 o’clock (14.62 cm/s vs 9.59 cm/s; P = 0.008; Table 2). MSP was significantly reduced in patients treated by distal compared with proximal embolization [−2.52 cm/s (SD 1.70) vs 1.03 cm/s (SD 2.53); P = 0.047]. However, the coil landing zone was not associated with symptom improvement (P = 1.000). The difference in MSP change in patients with type 1 and type 2 SRA anatomy was significant [−2.54 cm/s (SD 1.68) vs 1.10 cm/s (SD 2.43); P = 0.040].
| Position | Pre-treatment MSP | Post-treatment MSP | P value |
| 1 o’clock | 17.82 | 17.01 | 0.993 |
| 3 o’clock | 15.88 | 12.34 | 0.158 |
| 5 o’clock | 13.03 | 9.81 | 0.314 |
| 6 o’clock | 13.36 | 9.49 | 0.077 |
| 7 o’clock | 14.62 | 9.59 | 0.008 |
| 9 o’clock | 16.71 | 14.77 | 0.604 |
| 11 o’clock | 12.74 | 13.11 | 0.708 |
| 12 o’clock | 13.12 | 12.15 | 0.592 |
| Overall | 14.66 | 12.29 | 0.008 |
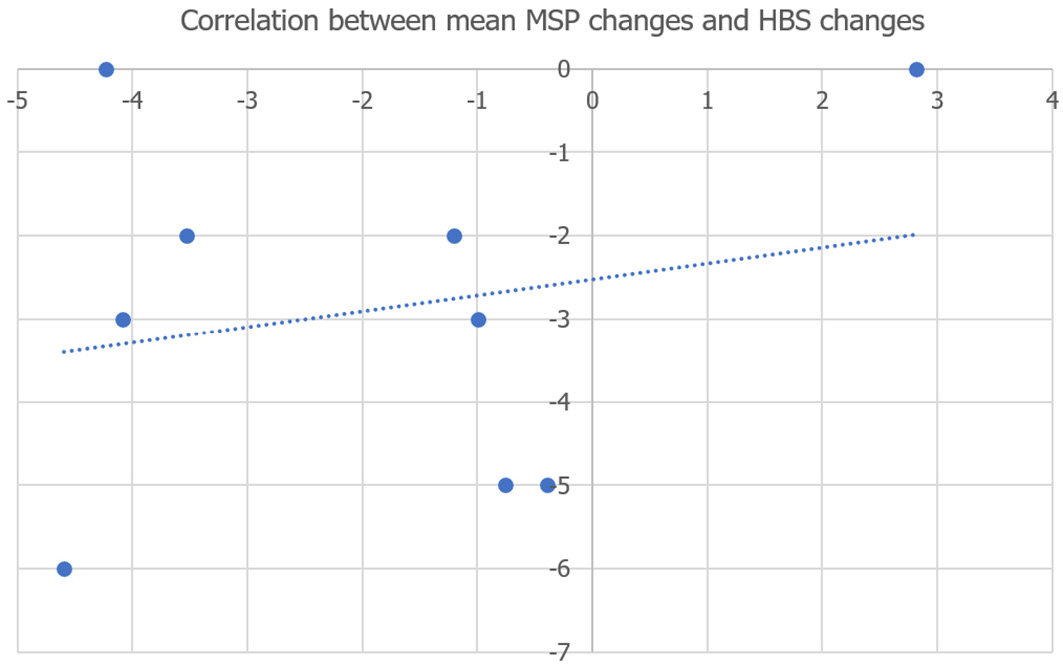
In 5 patients (55.5%) with HBS reductions ≥ 3, no significant difference was found between pre- (14.20 cm/s) and post-treatment (12.04 cm/s) MSP values (P = 0.07). The same was reported in 4 patients (44.5%) who complained of persisting bleeding and who showed no significant difference between pre- (14.12 cm/s) and post-treatment (12.59 cm/s) MSP values (P = 0.41). No relationship was found between hemorrhoidal grade and treatment outcome (P = 1.000) or between SRA anatomy and treatment outcome (P = 1.000). Pearson’s correlation analysis showed a weak positive correlation [rs (9) = 0.21, P = 0.57] between MSP and HBS changes, with a monotonic relationship, as assessed by visual inspection of the scatterplot (Figure 6).
Hemorrhoidal peak velocities were shown to be significantly different in a healthy control group and in patients with hemorrhoidal disease[17]. Doppler ultrasound-guided hemorrhoidal artery ligation (DHAL) and THD techniques have been proposed as minimally invasive modalities to treat hemorrhoidal bleeding by selective dearterialization[5,13]. A systematic review and meta-analysis showed an advantage of THD over traditional hemorrhoidectomy in terms of shorter operative time and reduced pain and complications[18]. However, this procedure is associated with a recurrence rate up to 40%[18,19]. A systematic review of the literature showed an overall recurrence rate of 17.5% after DHAL[20]. These data are different from those of Ratto et al[5] who reported a correlation between technical success and clinical success of the THD procedure at a 1-year follow-up. These findings may be due to the peripheral hemorrhoidal artery ligation used in their study[6].
Embolization with particles conceptually mirrors the DHAL and THD techniques[21]. Compared to those procedures, Emborrhoid has the advantage of identifying all the hemorrhoidal arterial branches to be occluded by arteriography, potentially improving therapeutic effectiveness[1]. This technique was initially performed in the 1990s in patients with disabling chronic rectal bleeding[22]. Currently, indications for the procedure include mild-to-severe hemorrhoidal bleeding, recurrence after hemorrhoidal surgery, coagulation disorders, and presence of high operative risk[13]. Embolization, avoiding anal manipulation, has also been proposed for patients with faucal incontinence and hemorr
Ratto et al[5] analyzed the effects of THD on the hemodynamic parameters of the hemorrhoidal arteries, finding a significant reduction in MSP values (post treatment 10.3 cm/s vs pretreatment 18.7 cm/s). However, the analysis was limited to patients who reported resolution of the bleeding after treatment. These results are consistent with those of our pilot study showing that the overall MSP of hemorrhoidal arteries was significantly reduced after Emborrhoid. The present study demonstrated that distal embolization resulted in a greater reduction in MSP values compared with proximal embolization. Sectorial analysis revealed that the reduction was significant in the right posterolateral quadrant. Similar results were reported by Zakharchenko et al[21] who measured the hemorrhoidal blood flow by ultrasound. They demonstrated a drop in the flow from 109.0 mL/min/100 g ± 1.2 mL/min/100 g (SD) to 60.2 mL/min/100 g ± 4.4 mL/min/100 g (SD) (P < 0.05) the day after embolization, and unchanged at 1 mo of follow-up. Patient satisfaction was 94% in grade 1-2 and 83% in grade 3 hemorrhoids. These investigators used 0.3 mm diameter non-lysing synthetic polyvinyl alcohol particles and standard metallic coils. No data were provided on the correlation between flow and symptoms.
Our findings demonstrate that the benefit of Emborrhoid was not associated with the hemorrhoidal, probably due to the small size of the study cohort. However, in a previous study, we reported that Emborrhoid was more effective in grade 2 than in grade 3 hemorrhoids, with 84% vs 50% of symptoms resolution, respectively at the 6 mo follow-up[15].
Particles over coils or a combination of both, as in our patients, were not superior in terms of clinical success in a comparative study by Moussa et al[24] with a longer follow-up period.
Our study findings included a weak, nonsignificant correlation between post-operative MSP and HBS changes in both asymptomatic patients and in cases with persistent bleeding. Consequently, our results do not confirm the hypothesis that hypervascularization of the branches of the SRA and severity of hemorrhoidal bleeding are correlated. This data could explain why the technical success of the procedure, defined as the absence of the flow in the branches of SRA and absence of opacification of the terminal branches in the projection of the hemorrhoids, has been reported up to 93%-100%. On the other hand, the clinical success, assessed by using composite scores for symptoms evaluation, quality of life, and satisfaction, ranged between 63.0% and 94.0%, with 13.6% of rebleeding[14]. Vidal et al[13] treated 14 patients with embolization, reporting 100% technical success and 72% clinical success (mean follow-up, 192 d). These data are consistent with the results of our study, with 100.0% technical success, 55.5% clinical success, and persistent bleeding in 44.5% of cases (mean HBS: 3.75). The difference between the technical success reported at the end of the procedure and the clinical success at 1-mo of follow-up could be due to a revascularization of the branches of the SRA or the MRA.
The type of SRA anatomy is crucial to the effectiveness of MSP changes. We demonstrated greater flow reduction in patients with type 1 SRA anatomy compared with those with type 2. Accordingly, patients with persistent or recurrent bleeding and no significant hemorrhoidal flow reduction at the follow-up eco-Doppler assessment may receive a second or third embolization. However, as described by Vidal et al[13], clinical success after repeated sessions was still not achieved in 28% of cases.
Post-operative complications after SRA embolization included fever, persistent bleeding, hematoma at the site of the puncture, tenesmus, hemorrhoidal thrombosis and pain. Eberspacher et al[25] reported a case of rectal ischemia resulting in rectal stenosis treated with bowel dilation. In our study, post-operative complications occurred in 36.4% of cases. The radial artery access, proposed to reduce the need for post-operative bed rest and offer patients a prompt return to normal activities[13,26], was complicated by a radial artery thrombosis.
Limitations of this study are the small sample-size and the short follow-up period. However, given the novelty of this technique, we decided to conduct a pilot study to preliminarily assess the effectiveness of the procedure. Our results in terms of moderate efficacy and weak correlation between symptoms and flow suggest a word of caution. In hemorrhoidal disease the increased arterial flow might not be the main cause of symptoms. Studies in a larger group of patients and with a longer follow-up are needed to draw definitive conclusion on long term effectiveness and recurrence rate.
The preliminary findings of this pilot study confirm that Emborrhoid was effective in reducing the arterial hemorrhoidal flow in hemorrhoidal disease. The MSP reduction was significant in type 1 SRA anatomy and in distal embolization. However, the correlation between post-operative changes in MSP values and HBS was weak and no relationship was found between hemorrhoidal grades, SRA anatomy, type of embolization, and treatment outcomes.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Guirola Ortíz JA, Spain S-Editor: Chen YL L-Editor: Filipodia P-Editor: Yu HG
| 1. | Vidal V, Louis G, Bartoli JM, Sielezneff I. Embolization of the hemorrhoidal arteries (the emborrhoid technique): a new concept and challenge for interventional radiology. Diagn Interv Imaging. 2014;95:307-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 2. | De Nardi P, Maggi G. Embolization of the superior rectal artery: another management option for hemorrhoids. Tech Coloproctol. 2021;25:1-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Panneau J, Mege D, Biseglie MD, Duclos J, Habert P, Vidal V, Tradi F. Emborrhoid: Rectal Artery Embolization for Hemorrhoid Disease. Semin Intervent Radiol. 2022;39:194-202. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Schuurman JP, Go PM, Bleys RL. Anatomical branches of the superior rectal artery in the distal rectum. Colorectal Dis. 2009;11:967-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 55] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 5. | Ratto C, Parello A, Donisi L, Litta F, Zaccone G, Doglietto GB. Assessment of haemorrhoidal artery network using colour duplex imaging and clinical implications. Br J Surg. 2012;99:112-118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (1)] |
| 6. | Parello A, Litta F, De Simone V, Campennì P, Orefice R, Marra AA, Goglia M, Santoro L, Santoliquido A, Ratto C. Haemorrhoidal haemodynamic changes in patients with haemorrhoids treated using Doppler-guided dearterialization. BJS Open. 2021;5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Thomson WH. The nature of haemorrhoids. Br J Surg. 1975;62:542-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 440] [Cited by in RCA: 328] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 8. | Sun WM, Peck RJ, Shorthouse AJ, Read NW. Haemorrhoids are associated not with hypertrophy of the internal anal sphincter, but with hypertension of the anal cushions. Br J Surg. 1992;79:592-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 34] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Stelzner F, Staubesand J, Machleidt H. [The corpus cavernosum recti--basis of internal hemorrhoids]. Langenbecks Arch Klin Chir Ver Dtsch Z Chir. 1962;299:302-312. [PubMed] |
| 10. | Moussa N, Sielezneff I, Sapoval M, Tradi F, Del Giudice C, Fathallah N, Pellerin O, Amouyal G, Pereira H, de Parades V, Vidal V. Embolization of the superior rectal arteries for chronic bleeding due to haemorrhoidal disease. Colorectal Dis. 2017;19:194-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 11. | Cocorullo G, Tutino R, Falco N, Licari L, Orlando G, Fontana T, Raspanti C, Salamone G, Scerrino G, Gallo G, Trompetto M, Gulotta G. The non-surgical management for hemorrhoidal disease. A systematic review. G Chir. 2017;38:5-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 12. | Tutino R, Salamone G, De Marco P, Cocorullo G, Gulotta G. Outpatient Treatment of Hemorrhoidal Disease: The Alternative Way to Treat Hemorrhoidal Disease in a Simple, Safe and Effective Manner. Rev Recent Clin Trials. 2021;16:5-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Vidal V, Sapoval M, Sielezneff Y, De Parades V, Tradi F, Louis G, Bartoli JM, Pellerin O. Emborrhoid: a new concept for the treatment of hemorrhoids with arterial embolization: the first 14 cases. Cardiovasc Intervent Radiol. 2015;38:72-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 14. | Talaie R, Torkian P, Moghadam AD, Tradi F, Vidal V, Sapoval M, Golzarian J. Hemorrhoid embolization: A review of current evidences. Diagn Interv Imaging. 2022;103:3-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 15. | Stecca T, Farneti F, Balestriero G, Barban M, Caratozzolo E, Zilio S, Massani M. Superior Rectal Artery Embolization for Symptomatic Grades 2 and 3 Hemorrhoidal Disease: 6-Month Follow-up among 43 Patients. J Vasc Interv Radiol. 2021;32:1348-1357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18532] [Cited by in RCA: 24805] [Article Influence: 1181.2] [Reference Citation Analysis (0)] |
| 17. | Aigner F, Gruber H, Conrad F, Eder J, Wedel T, Zelger B, Engelhardt V, Lametschwandtner A, Wienert V, Böhler U, Margreiter R, Fritsch H. Revised morphology and hemodynamics of the anorectal vascular plexus: impact on the course of hemorrhoidal disease. Int J Colorectal Dis. 2009;24:105-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 70] [Article Influence: 4.4] [Reference Citation Analysis (1)] |
| 18. | Simillis C, Thoukididou SN, Slesser AA, Rasheed S, Tan E, Tekkis PP. Systematic review and network meta-analysis comparing clinical outcomes and effectiveness of surgical treatments for haemorrhoids. Br J Surg. 2015;102:1603-1618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 130] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 19. | Fathallah N, Fels A, Benfredj P, Pommaret E, Beaussier H, de Parades V. Long-Term Efficacy of Artery Ligation with Mucopexy in Hemorrhoidal Disease: High Recurrence Rates but Most Patients Satisfied. J Gastrointest Surg. 2023;27:1936-1938. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 20. | Pucher PH, Sodergren MH, Lord AC, Darzi A, Ziprin P. Clinical outcome following Doppler-guided haemorrhoidal artery ligation: a systematic review. Colorectal Dis. 2013;15:e284-e294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 21. | Zakharchenko A, Kaitoukov Y, Vinnik Y, Tradi F, Sapoval M, Sielezneff I, Galkin E, Vidal V. Safety and efficacy of superior rectal artery embolization with particles and metallic coils for the treatment of hemorrhoids (Emborrhoid technique). Diagn Interv Imaging. 2016;97:1079-1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 22. | Tarazov PG. Arterial Embolization of Hemorrhoids. Cardiovasc Intervent Radiol. 2015;38:1055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 23. | Li YD, Xu JH, Lin JJ, Zhu WF. Excisional hemorrhoidal surgery and its effect on anal continence. World J Gastroenterol. 2012;18:4059-4063. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Moussa N, Bonnet B, Pereira H, Pechmajou L, Pellerin O, Abed A, Del Giudice C, Dean C, Bouda D, de Parades V, Fathallah N, Sapoval M. Mid-Term Results of Superior Rectal Artery and Coils for Hemorrhoidal Embolization with Particles Bleeding. Cardiovasc Intervent Radiol. 2020;43:1062-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 25. | Eberspacher C, Ficuccilli F, Tessieri L, D’Andrea V, Lauro A, Fralleone L, Mascagni D. Annoyed with Haemorrhoids? Risks of the Emborrhoid Technique. Dig Dis Sci. 2021;66:3725-3729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Iezzi R, Campenni P, Posa A, Parello A, Rodolfino E, Marra AA, Ratto C, Manfredi R. Outpatient Transradial Emborrhoid Technique: A Pilot Study. Cardiovasc Intervent Radiol. 2021;44:1300-1306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |