Published online Apr 14, 2024. doi: 10.3748/wjg.v30.i14.2059
Peer-review started: January 2, 2024
First decision: January 30, 2024
Revised: February 9, 2024
Accepted: March 26, 2024
Article in press: March 26, 2024
Published online: April 14, 2024
Processing time: 101 Days and 6.5 Hours
Hemorrhage associated with varices at the site of choledochojejunostomy is an unusual, difficult to treat, and often fatal manifestation of portal hypertension. So far, no treatment guidelines have been established.
We reported three patients with jejunal varices at the site of choledochojejunostomy managed by endoscopic sclerotherapy with lauromacrogol/α-butyl cyanoacrylate injection at our institution between June 2021 and August 2023. We reviewed all patient records, clinical presentation, endoscopic findings and treatment, outcomes and follow-up. Three patients who underwent pancreaticoduodenectomy with a Whipple anastomosis were examined using conventional upper gastrointestinal endoscopy for suspected hemorrhage from the afferent jejunal loop. Varices with stigmata of recent hemorrhage or active he
We conclude that endoscopic sclerotherapy with lauromacrogol/α-butyl cyanoacrylate injection can be an easy, effective, safe and low-cost treatment option for jejunal varicose bleeding at the site of choledochojejunostomy.
Core Tip: This is the first series of case reports on endoscopic sclerotherapy for venous varices at the choledochojejunostomy, including videos. From the experiences of our center, endoscopic sclerotherapy with lauromacrogol/α-butyl cyanoacrylate injection may be considered as an easy, cost-effective and efficient treatment option for hemorrhage from venous varices at the choledochojejunostomy site. For patients without complications, underlying diseases, and significant organ dysfunction, as well as those who have undergone pancreaticoduodenectomy for benign diseases, endoscopic sclerotherapy tends to have better outcomes.
- Citation: Liu J, Wang P, Wang LM, Guo J, Zhong N. Outcomes of endoscopic sclerotherapy for jejunal varices at the site of choledochojejunostomy (with video): Three case reports. World J Gastroenterol 2024; 30(14): 2059-2067
- URL: https://www.wjgnet.com/1007-9327/full/v30/i14/2059.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i14.2059
The prevalence of gastrointestinal hemorrhage from ectopic varices is relatively low, ranging from 1% to 5%[1,2]. Bilioenteric anastomosis is an uncommonly affected site of ectopic variceal bleeding[3]. Hemorrhage associated with varices at the site of choledochojejunostomy is an unusual, difficult to treat, and often fatal manifestation of portal hypertension (PHT). The possible cause of hemorrhage from ruptured jejunal varices could be extrahepatic portal vein obstruction or stenosis at the site where choledochojejunostomy was previously carried out, which leads to the development of hepatopetal portal collaterals through the anastomosis and PHT[4,5].
Diagnosis of ectopic variceal hemorrhage at a bilioenteric anastomosis can be difficult because varices are located deep within the jejunal loop and factors such as postsurgical adhesions make early detection of the bleeding source more difficult[6]. Treatment of ectopic variceal hemorrhage at bilioenteric anastomoses can be challenging because of their hemodynamic complexity. So far, no treatment guidelines have been established, so it may require a multidisciplinary approach and depend on the patient’s conditions[7]. There are two treatment choices: Portal decompression and obliteration of the varices[8-11]. Endoscopic sclerotherapy has been reported as a minimally invasive therapeutic method for jejunal varices[12-14].
We report three patients with jejunal varices at the site of choledochojejunostomy managed by endoscopic sclerotherapy with lauromacrogol/α-butyl cyanoacrylate injection. We highlight the outcomes of endoscopic sclerotherapy for such rare causes of bleeding, and analyze the possible factors affecting treatment effectiveness.
Case 1: A 25-year-old woman was admitted to hospital because of hematemesis, melena and hematochezia for 1 wk (Table 1).
| Patient No. | Age (yr) | Sex | Primary disease | Duration from operation to admission | Injection mixture composition | Pre-Clipping | Carvedilol intake | Rebleeding |
| 1 | 25 | Female | Solid pseudopapillary tumor of pancreas | 29 months | Auromacrogol/α-butyl cyanoacrylate (5.0/0.5 mL) | No | No | No |
| 2 | 55 | Male | Cholangio; carcinoma | 14 months | Lauromacrogol/α-butyl cyanoacrylate (12/1 mL) | Yes | No | Yes |
| 3 | 68 | Male | Cholangio; carcinoma | 47 months | Lauromacrogol/α-butyl cyanoacrylate (30/3 mL) | No | Yes | No |
Case 2: A 55-year-old man was admitted to our hospital with hematochezia for 1 month and hematemesis for 12 d (Table 1).
Case 3: A 68-year-old man presented to our hospital with intermittent melena, dizziness and fatigue for 1 month (Table 1).
Case 1: Local laboratory tests showed a minimum hemoglobin level of 45 g/L, which necessitated blood transfusions for 8 months. The location of the bleeding could not be definitively identified by repeated gastroscopy and colonoscopy.
Case 2: Gastroscopy and angiography at the local hospital did not definitively identify the site of bleeding.
Case 3: Gastroscopy at the local hospital revealed esophageal and gastric varices, no signs of bleeding.
Case 1: The patient had undergone pancreaticoduodenectomy with a Whipple anastomosis for a solid pseudopapillary tumor of the pancreas 29 months prior to the current visit. Eighteen days after surgery, follow-up computed tomography (CT) revealed formation of thrombosis in the portal vein and superior mesenteric vein, and anticoagulation therapy was administered.
Case 2: He had undergone pancreaticoduodenectomy 14 months previously with a Whipple anastomosis for moderately to poorly differentiated adenocarcinoma of the bile duct. The portal vein and the right wall of the superior mesenteric vein were affected by tumor invasion and were partially resected during the operation.
Case 3: He had undergone pancreaticoduodenectomy with a Whipple-Braun anastomosis for moderately differentiated adenocarcinoma of the bile duct (pathological staging pT2N0) 47 months previously.
All the three patients denied any family history of genetic disease and malignant tumours.
Case 1: The vital sign were as follows: Blood pressure, 104/72 mmHg; heart rate, 104 beats per min.
Case 2: On physical examination, the vital sign were as follows: Blood pressure, 121/63 mmHg; heart rate, 83 beats per min. Furthermore, anemic appearance and right abdominal tenderness were detected.
Case 3: On physical examination, the vital sign were as follows: Blood pressure, 121/74 mmHg; heart rate, 75 beats per min.
Case 1: Hemoglobin: 77.0 g/L; white blood counts (WBC): 19.94 × 109/L; platelet (PLT): 97 × 109/L.
Case 2: After admission, laboratory assessments revealed that the patient had heart failure, kidney failure and severe internal environment disorder. Hemoglobin: 73.0 g/L; PLT: 98 × 109/L; blood urea nitrogen: 42.70 mmol/L; serum creatinine: 367 μmol/L; carbon dioxide combining power: 6.5 mmol/L; carbohydrate antigen 19-9: 42.85 U/mL.
Case 3: Hemoglobin: 84.0 g/L; WBC: 3.46 × 109/L; PLT: 104 × 109/L.
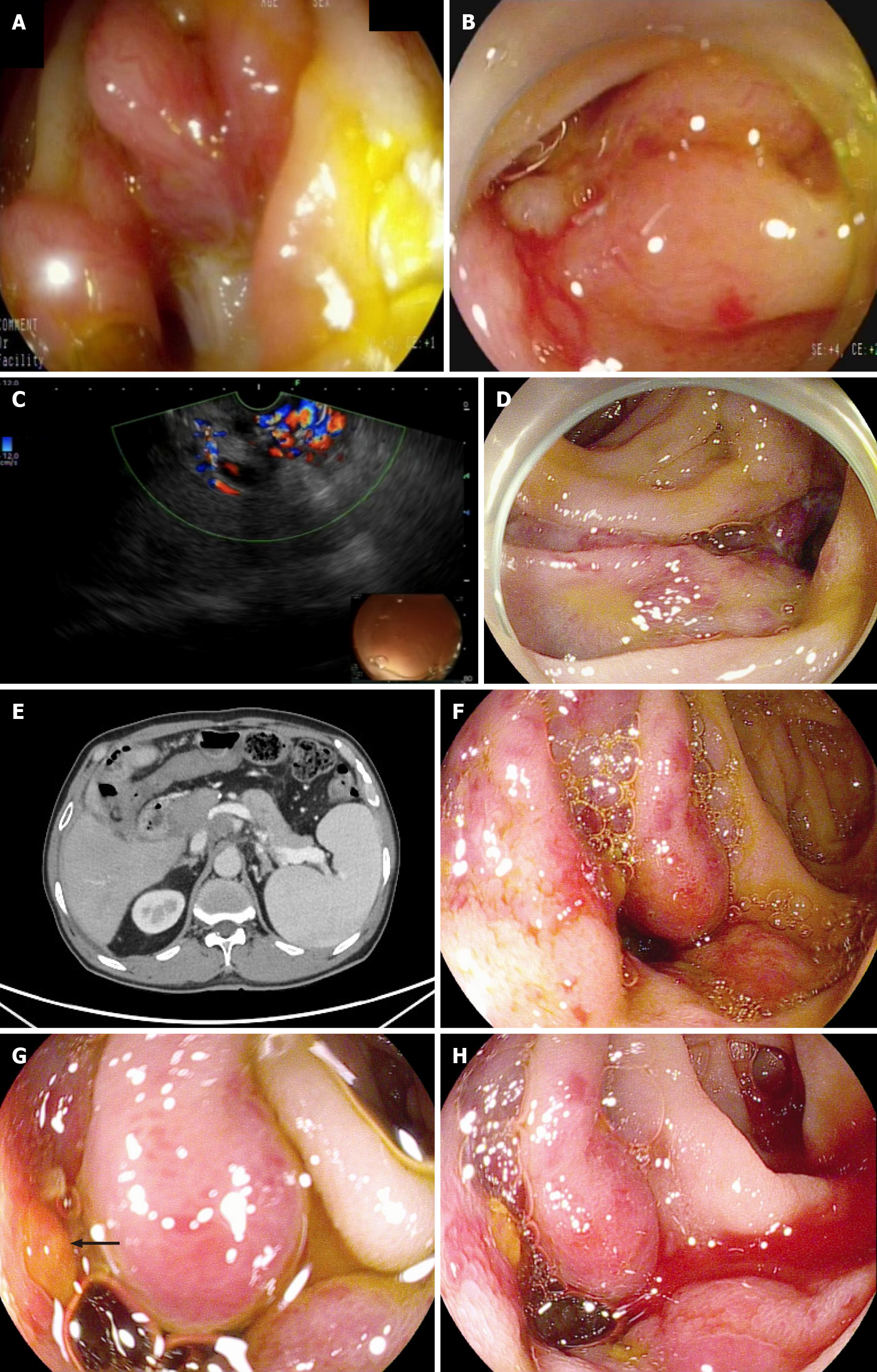
Case 1: After another episode of hematochezia, emergency gastroscopic examination the afferent loop revealed tortuous dilated blood vessels around the choledochojejunostomy site (Figure 1A), along with mucosal rupture (Figure 1B). Endoscopic ultrasonography confirmed the presence of numerous varicose veins near the choledochojejunostomy site, with abundant blood flow (Figure 1C).
Case 2: A nonenhanced abdominal CT scan revealed liver cirrhosis and PHT. With adequate adjustment of the internal environment and continuous renal replacement therapy, we performed emergency endoscopy on the afferent loop, which revealed a significant number of tortuous dilated varicose veins near the choledochojejunostomy site, along with several sites of active bleedings (Figure 1D).
Case 3: CT showed prehepatic PHT, suspicious tumor recurrence in the hepatic hilum area, and varices around the choledochojejunostomy site (Figure 1E). Gastroscopy and colonoscopy detected no particular bleeding point, and only detected nonbleeding signs of esophageal and gastric fundus varices. From these findings, his condition was suspected to be due to repeated rupturing of jejunal varices of the afferent loop, which had developed because of extrahepatic portal venous obstruction at the hepatic hilum area. Colonoscopy was undertaken to assess the possible varices around the choledochojejunostomy site at the afferent loop. There were three varicose veins visible with signs of erythema (Figure 1F) and thrombus head (Figure 1G), along with spontaneous bleeding (Figure 1H).
The final diagnosis of the three patients were jejunal varices at the site of choledochojejunostomy.
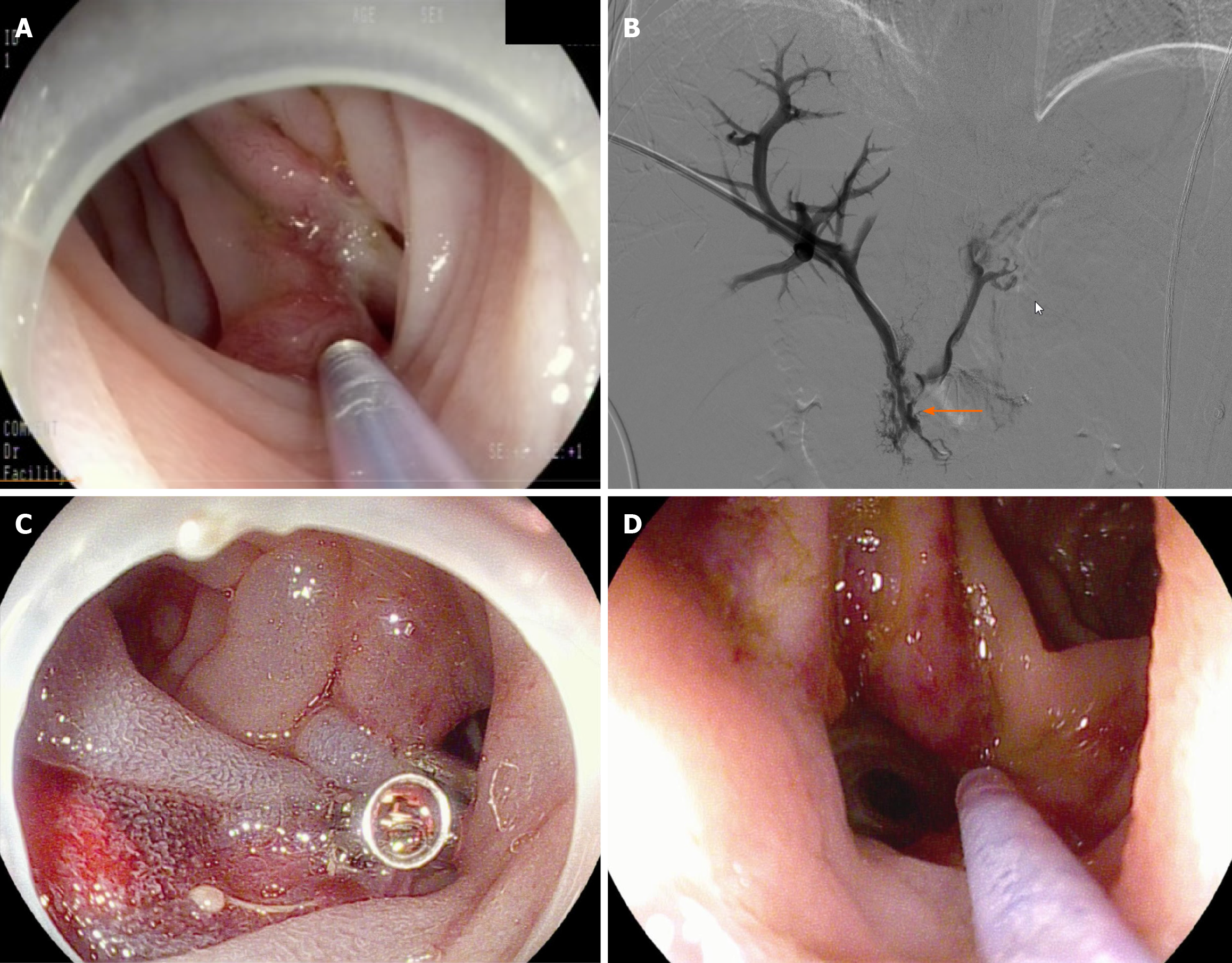
Injection sclerotherapy with lauromacrogol/α-butyl cyanoacrylate (5.0/0.5 mL) was carried out at the mucosal rupture (Figure 2A). Vascular angiography showed a patent portal vein and segmental occlusion of the superior mesenteric vein with old mural thrombus (arrow, Figure 2B). Therefore, balloon angioplasty of the superior mesenteric vein was not feasible. Considering the risk of bleeding, anticoagulant medication was not administered.
Hemostatic clips were used to close off the bleeding points. Subsequently, combined injection of lauromacrogol/α-butyl cyanoacrylate (12/1 mL) was administered to the varicose veins (Figure 2C).
Hemorrhage has remained stable for 27 months of follow-up.
Rebleeding occurred 1 month after endoscopic sclerotherapy, and despite two further endoscopic sclerotherapy procedures, repeated episodes of bleeding and multi-organ failure resulted in eventual death.
The patient developed moderate abdominal discomfort that disappeared within 2 d. He declined further examinations regarding tumor recurrence and was discharged with 6.25 mg carvedilol orally once daily after sclerotherapy to reduce portal vein pressure. One month later, the patient returned to the hospital for a follow-up examination. Enhanced CT revealed increased soft tissue density in the hepatic hilum, suggesting metastasis. There was also localized narrowing of the portal vein, with increased pressure on the right side of the narrowed segment. The peritoneum was thickened, and abdominal lymph nodes were enlarged (Figure 3A). The endoscopic follow-up revealed adhesive clumps and exudative ulcers near the choledochojejunostomy site, with no signs of bleeding (Figure 3B). The patient underwent endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) of the hepatic hilum mass, which was confirmed to be high-grade intraepithelial neoplasia, suggesting metastasis. However, the patient declined portal vein stenting intervention and was subsequently discharged. Two months after undergoing endoscopic sclerotherapy, a follow-up call revealed the patient had no further gastrointestinal bleeding and continued to take carvedilol consistently.
Anastomotic jejunal varices are a rare and often easily ignored cause of bleeding from the gastrointestinal tract and are typically diagnosed in patients with portal vein hypertension due to cirrhotic or extrahepatic PHT[15,16]. In some patients who have previously undergone cholangiojejunostomy, portal vein hypertension may occur as a result of extrahepatic portal venous stenosis or obstruction, leading to the development of hepatopetal portal collaterals through the anastomosis in the afferent loop[17]. Extrahepatic portal venous stenosis or obstruction can result from thrombophlebitis of the portal or superior mesenteric vein associated with an infection, compression or invasion of the portal vein by benign and malignant tumor, radiation-induced portal vein stenosis, thrombosis caused by portal stasis associated with hepatic cirrhosis, or surgical adhesions[18,19]. The most likely causes in our patients were as follows. Case 1 was considered to have a long-segment occlusion in the superior mesenteric vein due to an obsolete thrombus associated with potential infection. Case 2 had a tumor invading the right wall of the portal vein and superior mesenteric vein, leading to an intraoperative vascular wall resection. In case 3, it was believed to have resulted from local stenosis of the portal vein caused by recurrence of a tumor at the hepatic portal region, leading to portal vein hypertension on the right side of the stenotic segment.
Although the number of long-term survival cases after cholangiojejunostomy has increased, only a few have so far been reported. Despite the low incidence, jejunal varices should be considered in the differential diagnosis of digestive bleeding in patients with a history of pancreaticoduodenectomy. Clinical features for variceal bleeding are similar to those of typical varices. Depending on the bleeding rate, venous varices at the site of cholangiojejunostomy can present with hematemesis, melena or hematochezia. Based on previous reports, venous varices at the site of cholangiojejunostomy can lead to hemorrhagic shock, often requiring multiple blood transfusions during the treatment process. All three patients we reported received multiple blood transfusions during treatment.
Ectopic varices at the site of cholangiojejunostomy, which can trigger life-threatening bleeding, are usually overlooked in the differential diagnosis when hemorrhage occurs, owing to the length of small bowel, tortuosity and the intermittent nature of bleeding[3]. Enteroscopy can serve as an effective interventional diagnostic tool with therapeutic capabilities[14]. For patients who have undergone the Whipple procedure, experienced endoscopists can also reach the site of choledochojejunostomy using conventional gastroscopy and colonoscopy, and endoscopic treatment can also be performed. Capsule endoscopy cannot show the anastomosis because it is in the afferent limb[20].
Treatment of jejunal loop varices is difficult and has no definitive conclusion because of their hemodynamic complexity. Two treatment options are available: Obliteration of the varices (by endoscopic sclerotherapy or ligation, embolization using interventional radiology, surgery for re-anastomosis); and portal decompression (by portal venous dilatation and stent placement, splenectomy, and shunt operation)[9,21-26]. A multidisciplinary approach with the cooperation of endoscopists, interventional radiologists, and surgeons is critical for timely treatment of these patients[27]. The choice of treatment strategy depends on the patient’s overall condition, and the physician’s skill and equipment available at the institution. Norton et al[12]. used an algorithmic approach for treatment, and endoscopic therapy was recommended as the primary option. Embolization, surgical shunt or transjugular intrahepatic portosystemic shunt should be taken into consideration if the hemorrhage cannot be successfully controlled by endoscopic therapy and the portal vein is patent. Surgical ligation should be selected if the portal vein is obstructed. In summary, endoscopic therapy should be the first-choice management for ectopic variceal bleeding. Additionally, second or third rounds of treatment should be taken into consideration, because control of ectopic bleeding is sometimes difficult[5].
In case 1, vascular angiography showed patent portal vein blood flow, but the superior mesenteric vein was occluded due to chronic thrombosis, making balloon angioplasty with stent placement impossible. For case 2, the previous surgical records indicated that the primary tumor had a wide-ranging involvement, affecting the portal vein and superior mesenteric vein. The patient’s poor general physical condition and cardiac and renal functions led him ultimately to decide upon repeated endoscopic sclerotherapy as the treatment option. For case 3, CT confirmed the presence of a soft tissue mass in the hepatic hilum area, which encased and compressed the portal vein, resulting in significant narrowing. EUS-FNA was inclined towards a possible recurrence. However, the patient ultimately refused the placement of a portal vein stent.
Some factors may affect the clinical outcomes of endoscopic sclerotherapy for variceal bleeding at the site of cholangiojejunostomy. The severity of varices can affect the difficulty and success rate of treatment. More severe varices may require more treatment sessions or a greater amount of sclerosant, increasing the risk and complexity of the treatment. The overall condition of the patient can influence the risk and recovery of the procedure. Some patients may have failure of other organs that could increase the risk of treatment. The endoscopist’s expertise and skill can directly affect the success rate of treatment and the incidence of complications. Post-treatment follow-up and strategies to prevent recurrence are also crucial factors. From the prospective of pathophysiology, beta-blockers make sense in patients with ectopic varices[28]. Case 3 has been regularly taking carvedilol after sclerotherapy to reduce portal vein pressure; however, large-scale clinical data are still needed to evaluate the benefits of using carvedilol in patients with varices at the biliary-enteric anastomosis.
There were some limitations to the current study. First, the results were obtained retrospectively, and the number of cases was small. However, due to the short survival period caused by the underlying neoplastic disease and post-pancreaticoduodenectomy, as well as the low incidence of venous varices at the choledochojejunostomy site, there are a small number of reports of these patients. Further studies with larger sample size or prospective cohort studies are needed to confirm the safety and effectiveness. Second, all endoscopic sclerotherapeutic procedures were performed by an endoscopist at a single center. Therefore, it is difficult to generalize the current results. Despite these limitations, to our knowledge, this is the first series of case reports on endoscopic sclerotherapy for venous varices at the choledochojejunostomy site, including videos.
Endoscopic sclerotherapy with lauromacrogol/α-butyl cyanoacrylate injection may be considered as an easy, cost-effective and efficient treatment option for hemorrhage from venous varices at the choledochojejunostomy site in patients who have undergone pancreaticoduodenectomy. For patients without complications, underlying diseases, and significant organ dysfunction, as well as those who have undergone pancreaticoduodenectomy for benign diseases, endoscopic sclerotherapy tends to have better outcomes. The treatment of this rare cause of bleeding will increasingly require a multidisciplinary approach and personalized treatment choices in the future.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Salvadori M, Italy; Yoshida H, Japan S-Editor: Fan JR L-Editor: A P-Editor: Zheng XM
| 1. | Wilson SE, Stone RT, Christie JP, Passaro E Jr. Massive lower gastrointestinal bleeding from intestinal varices. Arch Surg. 1979;114:1158-1161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 63] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Sato T, Akaike J, Toyota J, Karino Y, Ohmura T. Clinicopathological features and treatment of ectopic varices with portal hypertension. Int J Hepatol. 2011;2011:960720. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 71] [Article Influence: 5.1] [Reference Citation Analysis (35)] |
| 3. | Watanabe N, Toyonaga A, Kojima S, Takashimizu S, Oho K, Kokubu S, Nakamura K, Hasumi A, Murashima N, Tajiri T. Current status of ectopic varices in Japan: Results of a survey by the Japan Society for Portal Hypertension. Hepatol Res. 2010;40:763-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 95] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 4. | Hiraoka K, Kondo S, Ambo Y, Hirano S, Omi M, Okushiba S, Katoh H. Portal venous dilatation and stenting for bleeding jejunal varices: report of two cases. Surg Today. 2001;31:1008-1011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Sasamoto A, Kamiya J, Nimura Y, Nagino M. Successful embolization therapy for bleeding from jejunal varices after choledochojejunostomy: report of a case. Surg Today. 2010;40:788-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Hekmat H, Al-toma A, Mallant MP, Mulder CJ, Jacobs MA. Endoscopic N-butyl-2-cyanoacrylate (Histoacryl) obliteration of jejunal varices by using the double balloon enteroscope. Gastrointest Endosc. 2007;65:350-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Wakasugi M, Tsujie M, Goda S, Ohnishi K, Koga C, Tei M, Kawabata R, Hasegawa J. Laparotomy-assisted transcatheter variceal embolization for bleeding jejunal varices formed at the site of choledochojejunostomy: Report of a case and review of the literature. Int J Surg Case Rep. 2020;77:554-559. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Sato T, Yasui O, Kurokawa T, Hashimoto M, Asanuma Y, Koyama K. Jejunal varix with extrahepatic portal obstruction treated by embolization using interventional radiology: report of a case. Surg Today. 2003;33:131-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Sakai M, Nakao A, Kaneko T, Takeda S, Inoue S, Yagi Y, Okochi O, Ota T, Ito S. Transhepatic portal venous angioplasty with stenting for bleeding jejunal varices. Hepatogastroenterology. 2005;52:749-752. [PubMed] |
| 10. | Sone M, Arai Y, Morita S, Tomimatsu H, Sugawara S, Ishii H, Takeuchi Y. Percutaneous creation of an extraanatomic splenoportal shunt in a patient with bleeding ectopic varices. J Vasc Interv Radiol. 2014;25:1301-1303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Abdalla AO, Abdallah MA, Calvo LA. Successful Treatment of a Case of Ectopic Jejunal Varices with Portal Venous Stenting. Am J Case Rep. 2019;20:948-952. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Norton ID, Andrews JC, Kamath PS. Management of ectopic varices. Hepatology. 1998;28:1154-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 254] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 13. | Prachayakul V, Aswakul P, Kachintorn U. Bleeding hepaticojejunostomy anastomotic varices successfully treated with Histoacryl injection, using single-balloon enteroscopy. Endoscopy. 2011;43 Suppl 2 UCTN:E153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Takashima K, Matsui S, Komeda Y, Nagai T, Toshiharu S, Kashida H, Kudo M. Endoscopic sclerotherapy under balloon-assisted enteroscopy for hemorrhagic jejunal varices after choledocho-jejunostomy. Endoscopy. 2020;52:E41-E42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Akhter NM, Haskal ZJ. Diagnosis and management of ectopic varices. Gastrointest Interv. 2012;1:3-10. [RCA] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 16. | Kastanakis M, Anyfantakis D, Katsougris N, Bobolakis E. Massive gastrointestinal bleeding due to isolated jejunal varices in a patient without portal hypertension. Int J Surg Case Rep. 2013;4:439-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Heiberger CJ, Mehta TI, Yim D. Jejunal varices: an unconsidered cause of recurrent gastrointestinal haemorrhage. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Moncure AC, Waltman AC, Vandersalm TJ, Linton RR, Levine FH, Abbott WM. Gastrointestinal hemorrhage from adhesion-related mesenteric varices. Ann Surg. 1976;183:24-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 77] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Sakurai K, Amano R, Yamamoto A, Nishida N, Matsutani S, Hirata K, Kimura K, Muguruma K, Toyokawa T, Kubo N, Tanaka H, Yashiro M, Ohira M, Hirakawa K. Portal vein stenting to treat portal vein stenosis in a patient with malignant tumor and gastrointestinal bleeding. Int Surg. 2014;99:91-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Ali S, Asad Ur Rahman, Navaneethan U. An Unusual Cause of Recurrent Gastrointestinal Bleeding After Whipple's Surgery. Gastroenterology. 2017;153:e1-e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Saeki Y, Ide K, Kakizawa H, Ishikawa M, Tashiro H, Ohdan H. Controlling the bleeding of jejunal varices formed at the site of choledochojejunostomy: report of 2 cases and a review of the literature. Surg Today. 2013;43:550-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Taniguchi H, Moriguchi M, Amaike H, Fuji N, Murayama Y, Kosuga T. Hemorrhage from varices in hepaticojejunostomy in the fifth and tenth year after surgery for hepatic hilar bile duct cancer: a case report. Cases J. 2008;1:59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Rezende-Neto JB, Petroianu A, Santana SK. Subtotal splenectomy and central splenorenal shunt for treatment of bleeding from Roux en Y jejunal loop varices secondary to portal hypertension. Dig Dis Sci. 2008;53:539-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Ota S, Suzuki S, Mitsuoka H, Unno N, Inagawa S, Takehara Y, Sakaguchi T, Konno H, Nakamura S. Effect of a portal venous stent for gastrointestinal hemorrhage from jejunal varices caused by portal hypertension after pancreatoduodenectomy. J Hepatobiliary Pancreat Surg. 2005;12:88-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 46] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 25. | Maeda N, Maruyama H, Higashimori A, Ominami M, Fukunaga S, Nagami Y, Fujiwara Y. Successful treatment using balloon-assisted enteroscopy for jejunal loop variceal bleeding after pancreaticoduodenectomy. Endoscopy. 2023;55:E536-E537. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 26. | Nasr S, Dahmani W, Jaziri H, Becheikh Y, Ameur WB, Elleuch N, Jmaa A. Massive hematochezia due to jejunal varices successfully treated with coil embolization. Clin Case Rep. 2022;10:e6339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 27. | Kohli DR, Levy MF, Smallfield GB. Laparotomy-Assisted Endoscopic Injection of Jejunal Varices for Overt Small Bowel Bleeding. ACG Case Rep J. 2017;4:e79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Biecker E. Portal hypertension and gastrointestinal bleeding: diagnosis, prevention and management. World J Gastroenterol. 2013;19:5035-5050. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 51] [Cited by in RCA: 61] [Article Influence: 5.1] [Reference Citation Analysis (0)] |