Published online Mar 21, 2024. doi: 10.3748/wjg.v30.i11.1475
Peer-review started: November 27, 2023
First decision: January 5, 2024
Revised: January 22, 2024
Accepted: February 27, 2024
Article in press: February 27, 2024
Published online: March 21, 2024
Processing time: 114 Days and 18.9 Hours
Acute pancreatitis (AP) is a leading cause of gastrointestinal-related hospitalizations in the United States, resulting in 300000 admissions per year with an estimated cost of over $2.6 billion annually. The severity of AP is determined by the presence of pancreatic complications and end-organ damage. While mode
Core Tip: In this editorial we review the outcomes of an emergency department (ED) pathway for patients with mild acute pancreatitis. The goal of the pathway is to reduce hospitalizations, prevent iatrogenic complications and reduce costs, without affecting readmission rates or mortality. We discuss the clinical course and outcomes of mild acute pancreatitis patients enrolled in the pathway who were successfully discharged from the ED compared to those who were admitted to the hospital, and identify predictors of successful ED discharge to select patients who can potentially be triaged to the pathway.
- Citation: Kothari DJ, Sheth SG. Innovative pathways allow safe discharge of mild acute pancreatitis from the emergency room. World J Gastroenterol 2024; 30(11): 1475-1479
- URL: https://www.wjgnet.com/1007-9327/full/v30/i11/1475.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i11.1475
Acute pancreatitis (AP) is an inflammatory condition of the pancreas caused by the activation of pancreatic enzymes resulting in digestion of the pancreatic parenchyma. Patients typically present with acute onset epigastric abdominal pain with nausea and vomiting[1]. Diagnosis of AP requires two of the following three criteria: (1) Classic abdominal pain; (2) serum amylase or lipase that is greater than three times the upper limit of normal; and/or (3) radiographic evidence of pancreatic inflammation. Further, severity of AP is determined by the presence of peripancreatic complications and/or end-organ damage (i.e., renal failure, respiratory failure or altered mental status)[2,3]. Studies report that patients with severe AP can have a mortality of nearly 30% during the hospitalization however account for less than 25% of all AP. Conversely, the majority of patients with AP have mild presentations and generally have a low mortality rate[1].
In the United States, the most common cause of AP is gallstones followed by alcohol use and contributes to nearly 300000 hospital admissions per year amounting to approximately $2.6 billion in aggregate costs per year[4]. Over the past two decades, the incidence of AP has increased amongst hospitalized patients with an estimated annual incidence ranging from 68 to 81 per 100000 persons[5]. Furthermore, despite the low mortality rate for patients with mild AP, traditionally, patients with mild AP are hospitalized with length of stay (LOS) of up to 3 d to 7 d[6-8]. Thus, patients with AP contribute to significant health care costs per year and opportunity exists to streamline care for patients with mild AP.
In an effort to reduce healthcare costs, Emergency Departments (ED) implement clinical pathways for common chief complaints and clinical conditions to streamline care. The goal of these pathways is to provide high-level care and identify those patients who need admission vs those who can be stabilized and safely discharged with outpatient management. Examples include chest pain with acute coronary syndromes, asthma, atrial fibrillation, seizures, congestive heart failure, hyperglycemia including diabetic ketoacidosis, and chronic obstructive pulmonary disease. In these scenarios, pathways include specialists that help direct care but also a direct transition to outpatient follow up. These pathways became the mainstay of therapy during the coronavirus disease 2019 pandemic when EDs were overcrowded and hospital beds were scarce. In these times, other conditions that were typically managed with admission were managed with ED stabilization and close outpatient follow up[9-16].
The traditional dogma for AP management includes hospital admission for fluid resuscitation, bowel rest, symptom management, and risk mitigation for recurrence (i.e., cholecystectomy for biliary pancreatitis and alcohol cessation resources for alcoholic pancreatitis)[1,2]. Over the decades, studies and guidelines advance this management to improve care and reduce hospital LOS. Specifically, the American Gastroenterological Association (AGA) guidelines for early management of AP published in 2018 specifically advocate for goal directed fluid resuscitation and oral solid diet within 24 h of presentation[17]. Streamlined protocols in AP are aimed at reducing LOS and health care costs[18-21]. Some studies have explored the effect of such pathways on patient outcomes including mortality, sepsis, and LOS[22-25]. One study using a combined paging alert and web-based clinical decision-making tool and demonstrated a reduction in LOS and included all patients with AP regardless of severity and local complications[25]. Finally, with greater support for judicious use of fluids, as published in Waterfall trial in 2022, there is greater evidence to support streamlined care[26].
Furthermore, a 2014 Turkish study demonstrated that patients with mild AP could be safely discharged from the ED with intensive in-home therapy without a difference in readmission rates and with lower charges[27]. Although a novel approach, most health systems are not able to provide intensive home care and thus these results are not generalizable to most. Further, this study eliminated alcoholic pancreatitis, an important etiology to consider for United States patients. Given the low mortality rates for mild AP and accurate prediction scoring systems to identify patients with mild AP, patients with low-risk AP could potentially be managed safely within the confines of the ED with close outpatient follow up.
In a study published in 2018, we developed a clinical pathway for patients with mild AP with the aim to determine the feasibility of managing these patients in the ED with discharge after stabilization rather than admission[28]. The clinical pathway isolated patients with the mildest form of AP by excluding those with confirmed moderately-severe or severe AP, patients with persistent systemic inflammatory response, severe hyperglycemia, evidence of cholangitis or choledocholithiasis, or with patients with severe comorbidities (such as heart failure with reduced ejection fraction or end-stage renal failure on hemodialysis or peritoneal dialysis). Patients enrolled in the ED observation pathway, received structured hydration and reassessment in 8 h increments. Improvement was defined as lower pain scores, nausea controlled by medications, presence of hunger, and stable vital signs. When improved, patients would receive a solid fat diet and with continued improvement would be discharged with primary care or gastroenterology (GI) follow up. Patients with biliary pancreatitis in the absence of cholangitis or choledocholithasis would have surgical follow up within 7 d of discharge to ensure close interval cholecystectomy. Patients who failed to improve would be admitted and follow standard of care.
In comparison to those admitted, we found that patients were typically younger, had lower prediction scores, and were more likely to have an idiopathic etiology for their pancreatitis. Patients in the observation pathway had a significantly lower LOS (22 h vs 87 h). In this study we also compared those patients in the observation pathway to a historical cohort of patients with similar presentations who would have met criteria for observation. In this comparison, patients’ LOS were significantly longer in the historical cohort (72 h vs 23 h) and significantly greater patient charges in the historical cohort. Importantly, there was no difference in 30 d readmission rates and there were no deaths in either cohort. These findings suggested that a robust ED-based clinical pathway could be safe for the mildest form of AP.
In follow-up, we published longer-term data using the same ED-based clinical pathway in 2021[29]. In this study, the patients enrolled in the observation pathway continued to have a lower LOS and significantly fewer patient charges than those admitted and compared to those of a historical cohort without differences in readmission and without any related deaths. Compared to the initial study that had direct oversight by the GI team, the follow up study demonstrated that the ED providers could use the clinical pathway autonomously suggesting the ease of implementation and generalizability to institutions without GI providers. Using the availability data, we found that older age, greater medical comorbidity, and biliary pancreatitis were predictors for admission rather than observation whereas patients with idiopathic pancreatitis were nearly eight times more likely to be observed[30].
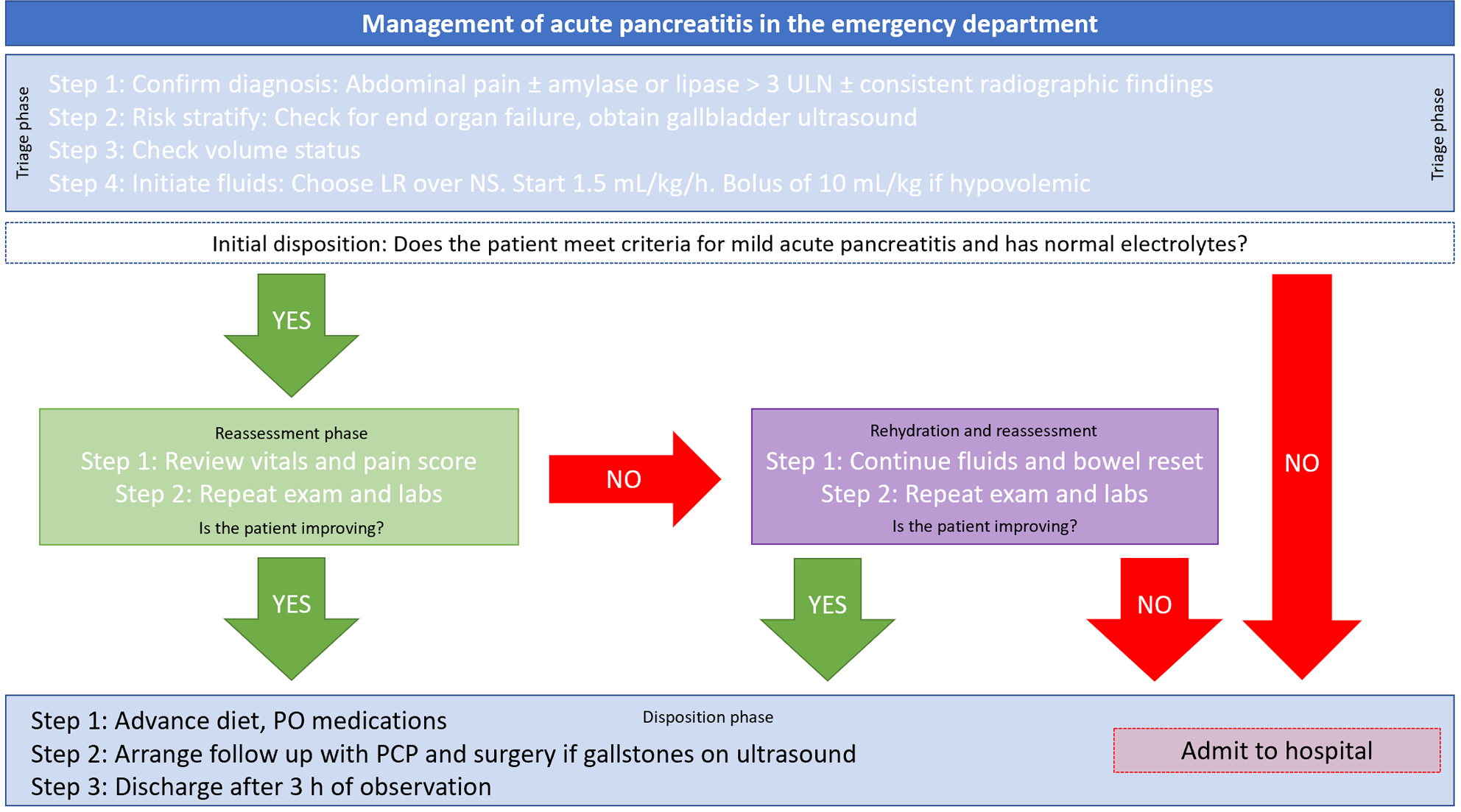
These studies demonstrate both the feasibility and durability of ED-based clinical observation pathways to support patients with mild AP using guideline based care while also providing safe discharge and avoiding unnecessary admission. In using such pathways, healthcare systems could reduce costs without compromising patient care or safety. In Figure 1, we provide a sample clinical decision tool as an example of a type of ED-based clinical pathway. In implementing such a pathway, we suggest assembling a group of stakeholders to include ED providers (physicians, midlevel providers, and nursing leadership), GI providers, hospital administrators and surgeons to sure that this pathway has support. Implicit in instituting such a pathway requires clear communication between the stakeholders to reduce risk of error and patient harm. In the studies we presented, we created a specific alert system to ensure that patients discharged from the ED on the pancreatitis pathway had adequate follow up with appropriated providers.
AP is an important contributor to healthcare burden in the United States and although some presentations are associated with a high mortality rate, the majority of patients have mild AP and thus a low mortality rate. As demonstrated by other clinical pathways for similarly morbid conditions such as asthma and atrial fibrillation, the mildest form of AP can safely manage in the ED with the implementation of guideline based clinical pathway.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Liu C, China S-Editor: Chen YL L-Editor: A P-Editor: Cai YX
| 1. | Forsmark CE, Vege SS, Wilcox CM. Acute Pancreatitis. N Engl J Med. 2016;375:1972-1981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 615] [Cited by in RCA: 553] [Article Influence: 61.4] [Reference Citation Analysis (0)] |
| 2. | Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, Tsiotos GG, Vege SS; Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4932] [Cited by in RCA: 4323] [Article Influence: 360.3] [Reference Citation Analysis (45)] |
| 3. | Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013;13:e1-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1080] [Cited by in RCA: 1037] [Article Influence: 86.4] [Reference Citation Analysis (6)] |
| 4. | Peery AF, Crockett SD, Murphy CC, Jensen ET, Kim HP, Egberg MD, Lund JL, Moon AM, Pate V, Barnes EL, Schlusser CL, Baron TH, Shaheen NJ, Sandler RS. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2021. Gastroenterology. 2022;162:621-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 475] [Article Influence: 158.3] [Reference Citation Analysis (1)] |
| 5. | Gapp J, Hall AG, Walters RW, Jahann D, Kassim T, Reddymasu S. Trends and Outcomes of Hospitalizations Related to Acute Pancreatitis: Epidemiology From 2001 to 2014 in the United States. Pancreas. 2019;48:548-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 79] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 6. | Kulvatunyou N, Watt J, Friese RS, Gries L, Green DJ, Joseph B, O'Keeffe T, Tang AL, Vercruysse G, Rhee P. Management of acute mild gallstone pancreatitis under acute care surgery: should patients be admitted to the surgery or medicine service? Am J Surg. 2014;208:981-7; discussion 986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Lariño-Noia J, Lindkvist B, Iglesias-García J, Seijo-Ríos S, Iglesias-Canle J, Domínguez-Muñoz JE. Early and/or immediately full caloric diet versus standard refeeding in mild acute pancreatitis: a randomized open-label trial. Pancreatology. 2014;14:167-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Cavallini G, Frulloni L, Bassi C, Gabbrielli A, Castoldi L, Costamagna G, De Rai P, Di Carlo V, Falconi M, Pezzilli R, Uomo G; ProInf-AISP Study Group. Prospective multicentre survey on acute pancreatitis in Italy (ProInf-AISP): results on 1005 patients. Dig Liver Dis. 2004;36:205-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 87] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 9. | Capp R, Sun B, Boatright D, Gross C. The impact of emergency department observation units on United States emergency department admission rates. J Hosp Med. 2015;10:738-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Baugh CW, Venkatesh AK, Bohan JS. Emergency department observation units: A clinical and financial benefit for hospitals. Health Care Manage Rev. 2011;36:28-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 97] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 11. | Bellew SD, Bremer ML, Kopecky SL, Lohse CM, Munger TM, Robelia PM, Smars PA. Impact of an Emergency Department Observation Unit Management Algorithm for Atrial Fibrillation. J Am Heart Assoc. 2016;5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Decker WW, Smars PA, Vaidyanathan L, Goyal DG, Boie ET, Stead LG, Packer DL, Meloy TD, Boggust AJ, Haro LH, Laudon DA, Lobl JK, Sadosty AT, Schears RM, Schiebel NE, Hodge DO, Shen WK. A prospective, randomized trial of an emergency department observation unit for acute onset atrial fibrillation. Ann Emerg Med. 2008;52:322-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 90] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 13. | Atzema CL, Austin PC, Miller E, Chong AS, Yun L, Dorian P. A population-based description of atrial fibrillation in the emergency department, 2002 to 2010. Ann Emerg Med. 2013;62:570-577.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 85] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 14. | Scribano PV, Wiley JF 2nd, Platt K. Use of an observation unit by a pediatric emergency department for common pediatric illnesses. Pediatr Emerg Care. 2001;17:321-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Grossman AM, Volz KA, Shapiro NI, Salem R, Sanchez LD, Smulowitz P, Grossman SA. Comparison of 1-Day Emergency Department Observation and Inpatient Ward for 1-Day Admissions in Syncope Patients. J Emerg Med. 2016;50:217-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Baugh CW, Liang LJ, Probst MA, Sun BC. National cost savings from observation unit management of syncope. Acad Emerg Med. 2015;22:934-941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Crockett SD, Wani S, Gardner TB, Falck-Ytter Y, Barkun AN; American Gastroenterological Association Institute Clinical Guidelines Committee. American Gastroenterological Association Institute Guideline on Initial Management of Acute Pancreatitis. Gastroenterology. 2018;154:1096-1101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 405] [Cited by in RCA: 559] [Article Influence: 79.9] [Reference Citation Analysis (0)] |
| 18. | Fagenholz PJ, Castillo CF, Harris NS, Pelletier AJ, Camargo CA Jr. Increasing United States hospital admissions for acute pancreatitis, 1988-2003. Ann Epidemiol. 2007;17:491-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 212] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 19. | Fagenholz PJ, Fernández-del Castillo C, Harris NS, Pelletier AJ, Camargo CA Jr. Direct medical costs of acute pancreatitis hospitalizations in the United States. Pancreas. 2007;35:302-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 218] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 20. | Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M; Early Goal-Directed Therapy Collaborative Group. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368-1377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6993] [Cited by in RCA: 6388] [Article Influence: 266.2] [Reference Citation Analysis (0)] |
| 21. | Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb SA, Beale RJ, Vincent JL, Moreno R; Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41:580-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4031] [Cited by in RCA: 3979] [Article Influence: 331.6] [Reference Citation Analysis (0)] |
| 22. | Reddy N, Wilcox CM, Tamhane A, Eloubeidi MA, Varadarajulu S. Protocol-based medical management of post-ERCP pancreatitis. J Gastroenterol Hepatol. 2008;23:385-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Mao EQ, Fei J, Peng YB, Huang J, Tang YQ, Zhang SD. Rapid hemodilution is associated with increased sepsis and mortality among patients with severe acute pancreatitis. Chin Med J (Engl). 2010;123:1639-1644. [PubMed] |
| 24. | Wu BU, Hwang JQ, Gardner TH, Repas K, Delee R, Yu S, Smith B, Banks PA, Conwell DL. Lactated Ringer's solution reduces systemic inflammation compared with saline in patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2011;9:710-717.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 339] [Article Influence: 24.2] [Reference Citation Analysis (1)] |
| 25. | Dimagno MJ, Wamsteker EJ, Rizk RS, Spaete JP, Gupta S, Sahay T, Costanzo J, Inadomi JM, Napolitano LM, Hyzy RC, Desmond JS. A combined paging alert and web-based instrument alters clinician behavior and shortens hospital length of stay in acute pancreatitis. Am J Gastroenterol. 2014;109:306-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 26. | de-Madaria E, Buxbaum JL, Maisonneuve P, García García de Paredes A, Zapater P, Guilabert L, Vaillo-Rocamora A, Rodríguez-Gandía MÁ, Donate-Ortega J, Lozada-Hernández EE, Collazo Moreno AJR, Lira-Aguilar A, Llovet LP, Mehta R, Tandel R, Navarro P, Sánchez-Pardo AM, Sánchez-Marin C, Cobreros M, Fernández-Cabrera I, Casals-Seoane F, Casas Deza D, Lauret-Braña E, Martí-Marqués E, Camacho-Montaño LM, Ubieto V, Ganuza M, Bolado F; ERICA Consortium. Aggressive or Moderate Fluid Resuscitation in Acute Pancreatitis. N Engl J Med. 2022;387:989-1000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 144] [Article Influence: 48.0] [Reference Citation Analysis (1)] |
| 27. | Ince AT, Senturk H, Singh VK, Yildiz K, Danalioğlu A, Cinar A, Uysal O, Kocaman O, Baysal B, Gürakar A. A randomized controlled trial of home monitoring versus hospitalization for mild non-alcoholic acute interstitial pancreatitis: a pilot study. Pancreatology. 2014;14:174-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 28. | Kothari D, Babineau M, Hall M, Freedman SD, Shapiro NI, Sheth SG. Preventing Hospitalization in Mild Acute Pancreatitis Using a Clinical Pathway in the Emergency Department. J Clin Gastroenterol. 2018;52:734-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 29. | Ahmed A, Kothari DJ, Wardlaw S, Freedman SD, Sheth SG. Reducing Hospitalization in Mild Acute Pancreatitis: Results of Long-term Follow-up. J Clin Gastroenterol. 2021;55:180-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 30. | Anderson K, Shah I, Yakah W, Cartelle AL, Zuberi SA, McHenry N, Horton L, Ahmed A, Freedman SD, Kothari DJ, Sheth SG. Prospective evaluation of an emergency department protocol to prevent hospitalization in mild acute pancreatitis: Outcomes and predictors of discharge. Pancreatology. 2023;23:299-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |