Published online Feb 28, 2023. doi: 10.3748/wjg.v29.i8.1289
Peer-review started: November 19, 2022
First decision: December 10, 2022
Revised: December 18, 2022
Accepted: February 15, 2023
Article in press: February 158, 2023
Published online: February 28, 2023
Processing time: 100 Days and 17.4 Hours
Colorectal cancer (CRC) is one of the most prevalent malignancies worldwide. Although most prevalent among older people, its incidence above 50 years old has been decreasing globally in the last decades, probably as a result of better screening. Paradoxically, its incidence in patients below 50 years old [early-onset CRC (EO-CRC)] has been increasing, for reasons not yet fully understood. EO-CRC’s increasing incidence is genre independent but shows racial disparities and has been described to occur worldwide. It follows a birth-cohort effect which probably reflects a change in exposure to CRC risk factors. Its incidence is predicted to double until 2030, which makes EO-CRC a serious public health issue. Both modifiable and non-modifiable risk factors have been identified - some are potential targets for preventive measures. EO-CRC is often diagnosed at advanced stages and histological features associated with poor prognosis have been described. EO-CRC presents some distinctive features: Microsatellite in-stability is common, but another subtype of tumours, both microsatellite and chromosome stable also seems relevant. There are no age-specific treatment protocols and studies on EO-CRC survival rates have shown conflicting data. Due to the higher germline pathological mutations found in EO-CRC patients, an accurate genetic risk evaluation should be performed. In this review, we summarize the current evidence on epidemiological, clinical, histopathological and molecular features of EO-CRC and discuss the contribution of genetics and lifestyle risk factors. We further comment on screening strategies and specific dimensions to consider when dealing with a younger cancer patient.
Core Tip: The incidence of early-onset colorectal cancer (EO-CRC) has been surprisingly increasing worldwide and it has become a public health issue. Its clinical, genetic, molecular and histological characteristics suggest that this may be a distinct entity, with a more aggressive behaviour. However, both genetic and environmental risk factors seem to contribute to this observed epidemiological shift in CRC incidence. More evidence is needed in order to clarify EO-CRC aetiology and to develop screening and management strategies.
- Citation: Saraiva MR, Rosa I, Claro I. Early-onset colorectal cancer: A review of current knowledge. World J Gastroenterol 2023; 29(8): 1289-1303
- URL: https://www.wjgnet.com/1007-9327/full/v29/i8/1289.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i8.1289
Colorectal cancer (CRC), the most common gastrointestinal cancer, is the third most common malignancy and the third leading cause of cancer-related death globally[1]. Once perceived as an elderlies’ disease, CRC incidence among the younger population [early-onset CRC (EO-CRC)] has been gaining more relevance. Recent epidemiological data show that, probably due to interventions on risk factors, screening programs implementation and better treatment[2], the incidence and mortality of CRC in patients older than 50 have been decreasing for the past decades[3]. On the contrary, from 1939, when the first case-reports of CRC in the young were published[4], the incidence of EO-CRC has been increasing and is expected to double by 2030[5].
Efforts have been made to characterize EO-CRC, questioning if this is a different entity from CRC in the older. As consensus is lacking, the authors review the existing knowledge, namely epidemiology, risk factors, clinical, molecular and genetic characteristics as well as treatment and overall survival (OS). EO-CRC has become a global health issue and there is a need to raise awareness for it, aiming at lowering the suspicion diagnostic threshold for symptomatic young patients.
CRC belongs to the top 3 of the most prevalent cancers worldwide, representing, in 2020, 10% of the global cancer incidence and 9.4% of all cancer-related deaths[1,6]. Globally, both CRC incidence and mortality have been decreasing in the last decades[3,5], which is consistently associated to screening programs implementation, thus allowing the detection and removal of adenomatous polyps and consequently interrupting the adenoma-carcinoma sequence[7]. In fact, the inflection time point when CRC incidence began to decrease occurred in the 1990s, coincident with the adoption and diffusion of colonoscopy for screening of average-risk CRC patients in several countries[8].
CRC incidence follows a heterogeneous geographical distribution. The highest incidences have been reported to occur in China, United States of America and Japan. Studies suggest that Human Development Index (HDI) is positively correlated with CRC incidence[9], meaning that countries with high HDI have a CRC incidence about 4-folds higher than low HDI countries. Currently, developed countries show a stabilizing or declining incidence rate whereas developing countries have an increasing incidence rate. The later is probably related to the increase in exposure to CRC risk factors[1], reflecting the adoption of a western lifestyle that accompanies economic transition[10].
Current data implies that CRC is going through an epidemiological change. In fact, based on data from the United States Surveillance, Epidemiology, and End Results program, Galloway et al[11] concluded that, although CRC incidence is decreasing by 3.1% per year among people above 50 years old, the incidence of EO-CRC is increasing by 1.4% per year. EO-CRC patients currently account for a percentage that ranges from 0.4% to as high as 35.6% with a median of 7% between the considered reports - such high values should be interpreted carefully as they may reflect institutional biases due to cancer centres that probably receive a high referral of EO-CRC patients[12]. Undoubtedly, CRC has become an increasingly more common diagnosis in younger patients.
One problem potentially leading to controversial research results is the lack of an agreed definition of EO-CRC patients. Some authors use a cut-off of 40 years old[12,13], but most reports in the literature apply a 50 years old limit[10,14,15], this later being consistent with the Amsterdam criteria, that identify patients more likely to have an hereditary predisposition for CRC[16]; 50 years old also coincides with the starting age of most screening programs in the general risk population.
Most studies found no significant difference in gender distribution in CRC[12,17] and the available evidence on EO-CRC prevalence found it to be independent of gender as well[13]. Racial disparities in EO-CRC incidence have however been described, namely with a higher proportion of Black patients, who also have a worse OS rate[18] - the same occurs for CRC in general in the United States[19]. A recent study, that suggested that the EO-CRC incidence has increased in all racial groups, reported the most elevated rise in Non-Hispanic White People. However, the overall incidence of EO-CRC in the United States remains higher for African Americans[20]. In an Israeli study, racial differences were also found, with the highest EO-CRC incidence in the Arabic population[21].
The reasons for the increased incidence of EO-CRC are not fully understood. Some authors suggest that the common use of colonoscopy is responsible for a proportion of the detected CRCs in young adults. This may have happened as a consequence of the diffusion of colonoscopy as a screening method as well as of an increased endoscopic capacity and efficiency, which may have unintentionally lowered the threshold for performing colonoscopy in younger patients[22].
Another important factor to consider when reflecting about EO-CRC incidence is the globally described existence of a strong birth-cohort effect. This is considered to occur when age-specific incidence rates vary by generation as a result of changes in people’s exposure to factors associated to disease risk. This is the opposite concept of period effect, when incidence varies at the same time for all generations[23].
A report based on the incidence of CRC in people from 20 European countries, aged 20 to 49 years old and including data from 1990 to 2016, elucidates on this effect. It showed that the CRC incidence for people aged 30-39 years old started to increase exactly 10 years earlier than in the 40-49 years old group and that, although the CRC incidence also increased for 20-29 years old patients, the study period (> 1980) did not cover the time inflection for that group. This suggests that the turning point possibly occurred before 1990. Additionally, the biggest incidence rise occurred in patients 20-39 years[24], which is consistent with results from an American study[5].
This recent rise in EO-CRC has been observed globally. A report including data from 20 European countries found that EO-CRC incidence has raised significantly in 14 of them, in 5 of them was stable and decreased only in Italy[24]. Another study about EO-CRC incidence among 36 countries from 5 continents reported that EO-CRC incidence was stable in 14 countries, decreased in 3 countries (Austria, Italy and Lithuania) and increased in 19 countries. From these 19 countries, 9 presented an isolated increase in EO-CRC incidence rate - in 5 of them CRC incidence was declining in the older population and in the remaining 4 countries it was stable[17].
Additionally, authors concluded that the most rapid increase in EO-CRC happened in countries where incidence rates were already the highest, such as South Korea[10]. This may be justified by the modernization process that occurred earlier in South Korea in comparison with other Asian countries and the consequently rapid dietary transition that took place following the Korean war[25]. The obesity increase that has been occurring worldwide, both for adults and children, may also play an important role, particularly because Asian countries have been experiencing some of the largest relative increases in body mass indexes[26].
In terms of future predictions, it is expected that the incidence rate for EO-CRC will double by 2030, while in older patients incidence it will probably decline by more than one-third. Meaning that, compared to 2010, when only 4.8% of all colon and 9.5% of all rectal cancers were diagnosed in younger patients, by 2030 they will sum up to 10.9% of all colon and 22.9% of all rectal cancers[5]. These findings explain why EO-CRC is clearly becoming an important public health issue.
CRC is a very heterogeneous disease that results from an interaction between genetic and environmental factors. The majority of CRCs are sporadic (70%), a small proportion of cases are caused by inherited syndromes (5%) and the remaining (25%) have an associated hereditary component, which has not yet been well established and is known as familial CRC[27]. Based on current knowledge, both modifiable and non-modifiable factors may also contribute to EO-CRC.
There is substantial controversy about results from studies concerning risk factors for CRC, and for EO-CRC in particular, especially concerning preventable risk factors. The majority of data about CRC risk factors is based on older age cohorts’ evidence and mainly represents mid- to late-life exposures. But when it comes to EO-CRC, early-life exposures may have a predominant role[28].
One of the most consensual risk factors for CRC is excess body weight. This has been associated with an increased risk for CRC[29] and has become more relevant since obesity prevalence has increased in the last decades[30], paralleling the tendency of EO-CRC[31]. In fact, recent data show that obesity is responsible for a 20% higher risk of EO-CRC[32].
Early-age exposures and weight are also suggested to influence CRC risk. A meta-analysis concluded that higher body fatness at an early age is associated with a higher risk of colon cancer in men and women, the same not applying to rectal cancer[33]. This correlation is probably explained by the effect of proinflammatory cytokines produced by the adipose tissue and by the chronic exposure to hyperinsulinemia and insulin-like growth factor 1 (IGF-I), that may contribute to carcinogenesis[34].
Another consistently associated risk factor for CRC is diabetes mellitus, with an increased relative risk of 30%[35]. In fact, a Swedish study concluded that a diabetic patient reaches the 10-year cumulative risk for CRC that justifies the general screening program 5 years earlier than a non-diabetic patient[36]. Its impact on EO-CRC has already been proved as well[37].
Both alcohol[38] and tobacco[39] are independent risk factors for CRC. A recent study also showed their contribution to EO-CRC, particularly when concomitantly present[40,41]. The protective role of physical activity has been described in different studies that demonstrated an inverse relationship between physical activity and risk of colon cancer. This probably happens due to decreased inflammation, reduced intestinal transit time, decreased IGF-I levels, reduced hyperinsulinemia and modulated immune function, that come with physical activity[42].
Conflicting data exists regarding the role of dyslipidaemia in CRC risk. While some studies suggest a protective one[43], others associate it to a higher risk[44]. The association between diet and CRC has been extensively studied. Some of the proposed elements associated to a higher risk of CRC are processed and red meat[45-47] and sugar sweetened beverages[48] - these are believed to influence gut immune response and inflammation[49]. On the contrary, a diet rich in fiber, dairy, fruits, vegetables[45], fish, beta-carotene, vitamin C, vitamin E, vitamin D and folate has shown a protective effect[41,50].
Aspirin and nonsteroidal anti-inflammatory drugs also exert a dose-dependent protective effect for CRC, through inhibition of the cyclooxygenase pathway[51]. Some of these interactions may account for the older onset/EO-CRC findings[41]. The importance of including fiber in the diet is mainly due to the production of short chain fatty acids during fiber fermentation. These have anti-inflammatory and anti-tumor properties[52] and their levels are inversely related with CRC occurrence[53].
The Western diet, typically rich in red and processed meat and poor in fiber, may be implicated on some of the differences found in incidence among populations[49]. Currently, the increasing incidence of EO-CRC is mostly observed in high-income economies or countries transitioning to a high-income economy and thus adopting Westernized lifestyle habits such as a western diet, weight excess and less activity level - all these may contribute to the increase in EO-CRC[10].
Microbiota has been recently proposed to also play a role in CRC pathogenesis. After comparing the colonic bacterial flora of populations considered to be at high and low risk for CRC[54], differences in microbiota composition were described - this may be a consequence of dietary habits and could harbour a risk for the development of CRC. Besides diet, the use of antibiotics may also affect the microbiota composition and it has been showed that the use of antibiotics, especially when used repeatedly[55] or for long periods during early to middle adulthood[56], is associated with an increased risk of developing CRC. From this point on, further research is needed before a microbiota modifying approach is considered. Current data shows conflicting results on prebiotic and probiotic therapy in CRC patients[57,58]. Based on the already mentioned birth-cohort effect, it seems that modifiable risk factors may play an important role in EO-CRC pathogenesis. The majority of the already known modifiable factors for CRC in general are believed to also apply to EO-CRC[41]. However, conflicting and limited evidence demands more studies.
The most consensual risk factor for CRC is a positive family history[17]: First-degree relatives (FDR) have an increased risk of developing CRC, especially when the proband was diagnosed at a younger age. In fact, having a FDR diagnosed under the age of 50 increases the risk of developing CRC by more than three-fold[59]. This risk is also increased for people with more than one affected relative[59], and for family history among distant relatives[60]. Additionally, a history of advanced adenomas or even a family history of any kind of adenomas also increases CRC risk[61,62].
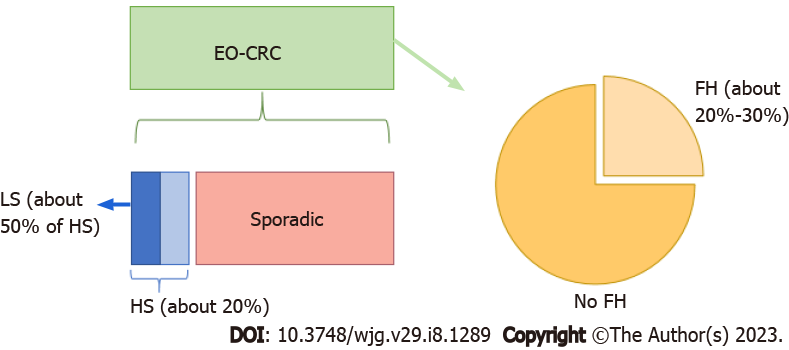
Other known conditions that increase the risk for EO-CRC are Lynch syndrome (LS) and familial adenomatous polyposis, among other hereditary CRC syndromes, with a larger proportion of EO-CRC being hereditary compared with older CRC patients[12,63] (Figure 1). Additional risk of EO-CRC has also been described for patients treated with pelvic radiation at young age[17,64].
Finally, patients with inflammatory bowel disease (IBD) are also known to be at increased risk for CRC[54], due to long-term inflammation. The highest risk is associated with extensive long duration colitis and/or a concomitant primary sclerosing cholangitis diagnosis. The association with EO-CRC, especially for ulcerative colitis, has been clearly demonstrated[15].
Conflicting data has been published about the correlation between breast cancer and CRC. Several studies have suggested an increased risk of CRC for patients with breast cancer at younger ages, and this relationship has also been suggested for EO-CRC[15].
Evidence from different studies found some differences between EO-CRC and older patients CRC, concerning clinical presentation, location and histological characteristics, suggesting it might be a distinct entity. Most studies have agreed on the clinical features of EO-CRC, namely on the most common presentation symptoms, with abdominal pain, rectal bleeding, weight loss, anaemia, decreased appetite and change in bowel habits[12,52,65], as well as on the more frequent presentation with bowel obstruction[66]. These common clinical symptoms are in accordance with the most common location of EO-CRC in the left colon, more precisely the rectum and the sigmoid colon, as described in the United States[12,23,67-69]. However, global data regarding location are conflicting.
A delay in the diagnosis of EO-CRC has been consistently described, with one series showing an average delay of 4[70] to 6 mo[71] and even with case-reports of a 2 years delay[72]. This represents a 1.4-fold increase in time when compared to older patients[70]. Various reasons can justify this, both doctor and patient related. There is probably both a lower suspicion by the clinicians, hence assuming that the symptomatology is associated to other benign and more common pathology (such as irritable bowel syndrome or haemorrhoids) and consequently not investigating further, and a younger patients’ delay in seeking medical attention, out of fear, denial, absence of information about alert symptoms, difficult access to health care or financial reasons[17,72,73].
Several studies consistently demonstrated that younger patients present more often with stage III or IV disease[10,66,74]. In fact, one multicentre retrospective study found that 61.2% of EO-CRC compared to 44.5% of older patients presented metastatic disease at diagnosis[12,13,75]. A plausible explanation for this relates to the absence of screening programs for younger patients but it may also be due to aggressive histopathological characteristics of EO-CRC and to its potential genetic basis, that may predispose to accelerated carcinogenesis in young patients. The diagnostic delay in younger patients may also contribute to more advanced disease at EO-CRC diagnosis[76], although this is not completely explained by the longer time to diagnosis[70].
Furthermore, synchronous or metachronous tumours more frequently arise in EO-CRC[76] but precursor adenomatous lesion are less frequently identified in the EO-CRC groups compared with older ones[13,52] - this also favours the accelerated carcinogenesis hypothesis. Histological predictors of bad prognosis have also been often found in EO-CRC. Young patients’ tumours more frequently display adverse histologic features compared with older CRC patients, such as mucinous or signet cell differentiation and poorly differentiated tumours[13,66,68,77]; lymphovascular, venous, and perineural invasion have also been described to be more common[13,66].
Since the classical sequence adenoma-carcinoma implicated in the carcinogenesis of CRC has been proposed, our understanding of its biology has evolved and currently CRC and particularly EO-CRC is believed to be an heterogenous disease, including cases with a strong hereditary component as well as sporadic disease[78]. For every CRC patient, a genetic aetiology should be considered, and this is particularly important for EO-CRC patients. In the EO-CRC group, even if we exclude LS (the most common hereditary CRC syndrome) patients, there is still a clear familial component, stronger than for older patients[78].
It is estimated that 20%-30% of CRC are associated with a family history of colorectal polyps or cancer, and that up to 3%-5% of CRC are attributed to an identifiable inherited CRC syndrome, such as LS, familial adenomatous polyposis, MUTYH-associated polyposis, juvenile polyposis syndrome, Peutz-Jeghers syndrome or others[79]. Recent studies concluded that 1 in 5 of EO-CRC cases is attributed to hereditary cancer syndromes[63], and half of those particularly to LS[80] (Figure 1).
Observing mutational profiles of left-sided CRCs, EO-CRC patients were found to have higher rates of mutations in genes related to cancer-predisposing syndromes, such as MSH2 and MSH6 (LS), neurofibromatosis type 1, PTEN hamartoma tumours syndrome or Cowden’s syndrome, tuberous sclerosis complex (TSC)1 and TSC2, and BRCA2 (hereditary breast and ovarian cancer syndrome)[81].
Due to the fact that a larger proportion of EO-CRC seems to be hereditary compared with older patients CRCs, the diagnosis of EO-CRC is currently an indication for referral for genetic evaluation[82]. Additionally, the variability in clinical presentations and potential for phenotypic overlap in CRC justifies the recommendation for genetic testing using a multigene panel for all individuals with an age below 50 years old[83]. This next-generation genetic tests identify pathogenic germline variants in 16%-20% of EO-CRC cases, including genes with moderate to high penetrance in cancer syndromes[63,80].
The diagnosis of a hereditary cancer syndrome frequently influences therapeutical options. In fact, it determines the surgical approach (e.g., subtotal colectomy instead of segmental resection), the chemotherapy regimen choice, colonoscopy surveillance intervals, and management of potential extracolonic cancers[84]. Furthermore, genetic testing is also important to identify relatives that may benefit from anticipation of colonoscopy screening[85].
Although germline genetic alterations can be implicated in 20% of individuals with EO-CRC, hereditary syndromes continue to account for only a minority of cases and the majority of EO-CRC are sporadic, in patients with no family history of CRC[86,87]. CRC represents a heterogenous group of cancers, although its majority can be divided in a few molecular subtypes, that influence treatment options such as chemotherapy regimens and correlate with cancer survival. Interestingly, current evidence suggests a different proportion of molecular tumour subtypes between older and EO-CRCs[68,78,88,89].
CRC usually follows one of the three main molecular subtypes: Chromosomal instability (CIN) or suppressor pathway subtype (80%-85%), CpG island methylator phenotype (CIMP) or serrated pathway (40%) or microsatellite instability (MSI) or mutator pathway subtype (10%-15%). The later is characterized by MSI due to loss of DNA mismatch repair (MMR), occurring both in a sporadic manner or in association with germline alterations in MMR genes (LS), as reviewed in Currais et al[84]. These subtypes are not mutually exclusive and can frequently overlap, with a minority of CRCs exhibiting both microsatellite and chromosome stability (MACS)[78,89].
The currently available studies addressing the molecular profile in EO-CRC have reached conflicting results. Some authors present evidence that EO-CRC tumours present more frequently with MSI (MSI-H)[81,90]. MSI tumours in these patients are mostly related to LS[91] and rarely to inactivation of MLH1 (which commonly occurs in older patients) but are more frequently associated with MSH2 inactivation[92]. They are associated with a better prognosis than microsatellite stable (MSS) tumours[93]. Other reports describe that the majority of EO-CRC are rather MSS, lacking DNA repair mechanism abnormalities[94,95]. EO-CRC MSS tumours are typically localized in the left colon, rarely associate with other primary neoplasms and have a strong familial component, features that distinguish them from MSS CRC in older patients[94].
MMR status has potential therapeutical implications. For example, CRCs exhibiting MMR deficiency typically have poor response to fluorouracil-based adjuvant chemotherapy[93]. Interestingly, however, patients with MMR-deficient tumours tend to exhibit better OS, attributed to the more immunogenic nature of these tumours[89]. Additionally, metastatic tumours with MMR deficiency are candidates for immune checkpoint inhibitors[88].
The CpG island methylator phenotype, seems to play a modest role in EO-CRC. EO-CRC are frequently CIMP-low except for EO-CRC LS patients, for whom a higher proportion will be CIMP-high, compared to those who develop LS-related CRC later in life[94]. A more recently described subset of CRC, defined by MACS, because of their diploid DNA content and lack of MMR deficiency, may account for 30% of all sporadic CRCs. These affect younger patients more commonly and have been identified frequently in the left distal colon and rectum. Moreover, this molecular subtype has been associated with poor differentiation, early occurrence of metastasis, disease recurrence and lower survival than patients with MSI or CIN. This can be related to its lack of immune response, opposite to the immunogenic favourable properties of MSI-H CRC[89]. There is still an incomplete understanding of the molecular profile of MACS. Silla et al[78] reviewed its main features: MACS tumours are usually CIMP-low, are rarely associated with BRAF mutations, lack MLH1 expression, and present a different pattern of hypomethylation than MSI and CIN CRC. Some published studies suggest that MACS may be related to familial CRC syndromes, based on observed increased frequency in young patients[96].
LINE-1 hypomethylation is another feature implied in EO-CRC and is considered to be a surrogate marker for genome-wide hypomethylation. It is associated with increased CIN[97]. Evidence shows that the degree of LINE-1 hypomethylation is an independent factor for increased cancer related mortality and overall mortality in CRC[98]. Antelo et al[91] compared this marker in EO-CRC and older CRC and concluded that the first group presented lower levels of LINE-1 methylation, which suggests a distinct molecular subtype of these tumours. Additional studies are needed in order to confirm this association and properly assess the prognostic value of LINE-1 in young-onset CRC.
As for the consensus molecular subtypes classification, EO-CRC tumours are more likely to have subtypes CMS1 or CMS2 tumours compared with CMS3 or CMS4 tumours[68]. From a mutational perspective, despite some conflicting data, the most consensual results show that EO-CRC has lower prevalence of BRAF V600, NRAS, KRAS and APC mutations in comparison with late-onset CRC[13,68].
In order to rigorously determine if the described characteristics are sufficient to consider EO-CRC as a distinct molecular profile, more and larger trials are needed. In fact, although lifestyle factors and exposure are believed to contribute to the EO-CRC incidence increase, germline and molecular data also provide clues to a different CRC pathogenesis.
EO-CRC does not have specific evidence-based treatment protocols. The subset of EO-CRC patients that present an inherited CRC syndrome, such as LS and polyposis syndromes, should follow their respective guidelines. This is important as the surgical approach is generally more radical and there is a need to manage the risk for other syndrome related malignancies by appropriate screening[3,99].
For the majority of the patients, although there are no age specific recommendations, current studies show that different therapeutic strategies are being implemented according to the patient’s age. Surgery is the main curative treatment for CRC, but for high-risk stage II and stage III there is a role for adjuvant chemotherapy[100]. When comparing EO-CRC with an older cohort (65-75 years old), various studies have found that more patients with early-stage EO-CRC are treated with adjuvant therapy for stage II and III disease. In fact, stage II low-risk EO-CRC patients receive adjuvant therapy 50% of the time, compared with 19.1% in the older cohort[101,102]. Curiously, these regimens were not associated with increased survival in stage I or stage II cancers and offered only marginal benefit in stage III and stage IV diseases[102].
Additionally, EO-CRC patients have better chances of receiving surgical treatment either for early-stage or for metastatic disease[66,103], of receiving radiotherapy at all disease stages and also of being offered more aggressive adjuvant treatment, including multi-agent chemotherapy[102]. Another study found that EO-CRC patients with stage I or II were more likely to receive adjuvant or neoadjuvant therapy, compared to older patients[66].
These studies may reflect the fewer comorbidities of EO-CRC patients, a better performance status and fewer adverse reactions to systemic treatment leading to a better tolerance to multiagent regimens than the older patients[66]. However, they may also show a bias towards offering more treatment to younger patients and there is a question of whether they are being victims of overtreatment with no proven benefit. According to current knowledge, equal treatment should be offered to EO-CRC (without a hereditary syndrome). More studies on the putative molecular differences between EO-CRC and older age CRC may in the future bring new molecular treatment targets, allowing specific treatment[11].
Some authors, supported by population-based studies, suggest that EO-CRC presents a better survival at every stage[77,103] and even that 5 years after curative treatment, EO-CRC survivors present the same main causes of death than the general population[104]. Other studies demonstrated that, after adjusting for stage, the prognosis is not influenced by CRC age[13,66], with no difference in stage-specific 5-year disease free survival and OS rates[66].
On the contrary, there also reports from single institution studies that showed poor clinical outcomes for EO-CRC and some authors suggest that the worse survival described for EO-CRC is caused by adverse histopathological features[105,106]. O’Connell et al[12]’s review found the average overall 5-year survival for young patients to be 33.4%, consistent with other reports[107,108]. When comparing stage-for-stage survival for younger vs older patients with CRC, it seems that young patients with earlier stages have better survival than older patients with the same stage disease. On the contrary, EO-CRC patients with advanced stages do the same or worse than older patients with the same advanced stage. This may justify the described overall lower 5-year survival for EO-CRC because these patients frequently present advanced disease, possibly as a consequence of the delayed diagnosis and/or the more aggressive underlying nature of the disease[12].
Regarding advanced and metastatic disease, studies found that EO-CRC patients have a lower progression-free survival although this does not impact the relative risk of death or OS compared with older CRC patients[109]. As for the mortality rate, although CRC mortality is declining overall and, from 2000 to 2014, CRC death rates decreased by 34% in individuals older than 50 years old, it increased by 13% in EO-CRC patients[110]. One limitation of the studies is that survival outcomes for EO-CRC are often confounded by the inclusion of hereditary colorectal carcinomas, such as LS related CRCs, that are believed to present a better survival compared with non-syndromic colorectal carcinomas[111,112].
CRC incidence and mortality for people older than 50 years old have been declining and the main proposed reason for that is the successful implementation of CRC screening, with a possible contribution of a change in lifestyle. Screening programmes have mostly emerged over the past few decades and generically apply to adults starting from 50 to 60 years old[113]. A recent study shows that from 36 countries from 5 continents, only 4 (Costa Rica, Cyprus, India and Philippines) lack any form of screening programmes[10]. Additionally, only 4 from the 36 mentioned countries have an earlier age cut-off for screening: Italy, beginning at 44 years; China, Japan and Austria, where it begins at 40 years old[113].
On the contrary, prevalence of EO-CRC is increasing. Although one reason for this increase could be over detection through screening, that seems unlikely since screening before age 50 is rare in the general population in most countries[113]. This was the reality until the most recent publication of the American Cancer Society (ACS) guidelines that, for the first time, recommend starting CRC screening at 45 years old for the standard-risk population. The previous CRC screening recommendations have been based on randomized controlled trials and prospective cohort studies. Since there is a lack of data on screening below 50 years old, this recommendation was a result of simulation modelling analyses of screening outcomes, that showed a favourable balance between benefits of screening from 45 years old with its potential life-years gained and the related burdens[114].
Although the absolute risk for EO-CRC is still low, it is expected to increase and the disease burden for younger patients is already substantial and potentially long-term. Additionally, current data show that 40-45 years old adults have the same prevalence of adenomas - CRC precursor lesions[115] - than adults 50-54.5 years old and people aged 40-49 years old account for 75% of the EO-CRC patients[116]. This questions the current age threshold and supports the ACS recommendation.
The debate about lowering the screening age is ongoing, as reviewed in Anderson and Samadder[117]. Those who are favourable to this approach prioritize the need to control the increase in EO-CRC. A study on screening worldwide, showed that two (Austria and Italy) of the only three countries where EO-CRC has declined have screening programs that begin below 50 years old (Italy at 44 and Austria at 40)[113]. Curiously, in Austria, the decreasing incidence of EO-CRC has only occurred in the 40 to 49 years age group[10]. Although another study showed that the same happened in Italy, other described an incidence decrease among the 20-39 years old patients[24].
Reasons for opposing the new 45 years old age threshold are diverse. One argument is that studies have shown that the biggest increase rate in EO-CRC was observed for people aged 20 to 39 years old, an age sector still not included in the suggested screening program. Another argument is that, although increasing, the absolute numbers of EO-CRC are still low, not relevant enough for a screening strategy change. Other concerns are related to the risk of augmenting health inequities related to access to health care services as well as for excessive financial health care costs, especially considering most European countries are still struggling to finance the current screening programs or are still in the process of implementing them[24].
Other authors suggest waiting for adequate randomized screening studies to test the ACS recent recommendation before adopting it and even question if the screening strategy should be applied to a malignancy whose biological and molecular substrate is not fully understood[95], which could mean that standard screening methods and prevention may not even be appropriate for it.
Another small study, based on the evidence that EO-CRC affects predominantly the left side of the colon, suggests a screening strategy with flexible sigmoidoscopy to be applied to people from 40 to 49 years old, as their study group observed that 80% to 83% of those tumours were theoretically within the reach of a flexible sigmoidoscopy[67]. From a different angle, another important factor when reflecting on EO-CRC diagnosis is that only half of the EO-CRC patients with germline pathogenic mutations reported a CRC diagnosis in a FDR and, consequently, were not eligible for high-risk CRC screening[63]. This contributes to the recommendation of performing genetic testing in all EO-CRC. Moreover, tumour testing for MSI or immunohistochemistry for MLH1, MSH2, MSH6, and PMS2 is recommended for all EO-CRC patients, even in countries where universal CRC MSI screening is still not implemented[3].
Another important aspect is the need to alert the medical community for the increasing incidence of EO-CRC and the consequent need for a rigorous assessment of CRC family risk trough detailed and complete family history in medical records, namely reviewing the familiar history of cancer including first- and second-degree relatives as well as personal and familiar history of advanced polyps[82]. Such systematic evaluation may be difficult to reliably execute in real world clinical practice, but it allows an appropriate determination of the patient risk for CRC and the identification of high-risk patients who should be offered earlier screening. Additionally, existing genetic risk models can also be employed and help identifying patients that benefit from genetic testing[118].
Another debatable option is to offer EO-CRC patients next-generation sequencing technology for genetic germline testing. Multigene panel testing has increased detection of germline mutations[79] in a feasible and more cost-effective way than single gene testing[82]. Recently, the National Comprehensive Cancer Network guidelines proposed offering multigene panel testing to all EO-CRC, aiming to increase opportunities for primary and secondary cancer prevention[83].
The disadvantage of this approach is that by testing more genes there is a higher risk of finding genetic variants of unknown significance or without a clear management evidence-based guideline[3]. As so, a multidisciplinary discussion with the active participation of a genetics specialist is recom-mended to appropriately offer and interpret genetic results, hence providing an appropriate counselling to EO-CRC patients and their families[3].
When dealing with younger patients with a malignancy, there are some extra needs that should be remembered and appropriately managed. EO-CRC patients, as older ones, may need to deal with adverse effects of the different treatment modalities. They face a higher rate of sexual dysfunction than the general population and report to be less sexually active after surgery[119]. Although surgery for CRC does not generally affect fertility[3], chemotherapy, particularly fluorouracil, may reduce sperm count or cause amenorrhea and radiotherapy may also reduce fertility in both men and women[120].
Fertility may play a central concern in the management of EO-CRC patients since they may still be in the reproductive age and have incomplete reproductive plans. As so, patients should be referred to reproductive specialists because options for fertility preservation such as banking of cryopreservation of sperm/oocytes/embryos is recommended prior to gonadotoxic chemotherapy and should be discussed, ahead of starting treatment[121].
Other aspect to consider in EO-CRC patients is the possibility of the diagnosis and/or treatment to be coincidental with a pregnancy, especially with the common delay in childbearing age in the developed world. In that scenario, a multidisciplinary approach, weighting the risks and benefits for both the mother and the foetus should be employed. Although studies in pregnant women are missing, it is consensually agreed that the first trimester is the most vital period to avoid, if possible, systemic agents[122]. Besides fertility, another concern for EO-CRC is to cope with the eventual need for transient or permanent ostomy. The present or past history of an ostomy can contribute to worse sexual function and body image[123].
Additionally, EO-CRC patients, especially the ones submitted to multimodality therapy, will live the rest of their lives under the threat or burden of long-term sequelae. Long-term survivors have reported sustained functional deficits and symptoms, such as sexual disfunction, anxiety, worse body image, embarrassment with bowel movements and faecal incontinence[124], with an impact on their quality of life. Concerning the psychosocial dimension, higher depression and anxiety diagnosis have been described for CRC survivors[125]. Concordantly, the American Society of Clinical Oncology recom-mends that all cancer survivors should be periodically evaluated for symptoms of depression and anxiety using validated measures and adequately managed, if necessary with the referral for psychological or psychiatric consultation[126]. All of these afore-mentioned factors contribute to the EO-CRC burden of disease, diminish patients’ quality of life and should be appropriately addressed throughout patients’ life.
By 2030, previsions are that more than 1 in 10 colon cancers and 1 in 4 rectal cancers will be diagnosed in patients younger than 50 years old[5]. These numbers are alarming and, consequently, as EO-CRC incidence increases, many studies have tried to shed light on this entity, especially comparing it to the traditional older patient CRC. Evidence suggests that EO-CRC differs from older-onset CRC in its clinical characteristics, pathological features, aggressive behaviour, and molecular profiles. These may be responsible for different responses to treatment and survival, although further studies are needed.
Although a higher proportion of cases, comparing to older patients, is genetic or familial, the majority of EO-CRC cases is still probably related to somatic genetic mutations or epigenetic alterations induced by modifiable risk factors. This is consistent with the birth-cohort effect observed. The contribution of lifestyle risk factors stands as an opportunity for implementing primary prevention measures for CRC, such as the practice of physical activity, having a healthy diet, quitting smoking and limiting alcohol consumption, also preventing obesity and diabetes. A study showed that risk factor modification could diminish CRC-related mortality in about 12% over 20-years[2].
This paper also aims at raising awareness of all the clinicians for the need to lower the suspicion threshold for young patients presenting with alarming gastrointestinal symptoms. We also stress the need to obtain complete clinical information, such as history of polyps, familial history (first- and second-degree relatives) and personal diseases history, namely previous radiation therapy or IBD. Only with this information can the genetic risk of EO-CRC be properly evaluated and subsequent genetic consultation be asked for, when indicated.
EO-CRC patients have some peculiarities and clinicians should be conscious of them. Financial burden and treatment sequelae such as sexual dysfunction, incontinence, anxiety and depression must be considered and managed. Patient’s reproductive plans should also be discussed. To conclude, although currently we already have some important data about EO-CRC, larger studies with longer follow-up of these patients are needed in order to reach consensus about the nature and pathogenesis of this disease.
Namely, ongoing studies and clinical trials, by our group and several others across the world, on the impact on survival of increasing clinician awareness on EO-CRC, on the definition of potentially specific phenotypes of EO-CRC, or on their specific responses to radio-, chemo- or immunotherapy will shed light on the subject. Hopefully, by improving young patients’ diagnosis, diminishing its observed delay, tailoring its treatment and follow-up and implementing modifications in lifestyle risk factors, in the future EO-CRC incidence will follow CRC incidence pattern and both entities’ burden will decrease.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author’s Membership in Professional Societies: American Gastroenterological Association, 1248915.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Portugal
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Oprea VD, Romania; Mao Y, China S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Xi Y, Xu P. Global colorectal cancer burden in 2020 and projections to 2040. Transl Oncol. 2021;14:101174. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 687] [Cited by in RCA: 1354] [Article Influence: 338.5] [Reference Citation Analysis (5)] |
| 2. | Vogelaar I, van Ballegooijen M, Schrag D, Boer R, Winawer SJ, Habbema JD, Zauber AG. How much can current interventions reduce colorectal cancer mortality in the U.S.? Cancer. 2006;107:1624-1633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 152] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 3. | Boardman LA, Vilar E, You YN, Samadder J. AGA Clinical Practice Update on Young Adult-Onset Colorectal Cancer Diagnosis and Management: Expert Review. Clin Gastroenterol Hepatol. 2020;18:2415-2424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 4. | Bacon HE, Sealy WB. Malignancy of the anus, rectum and sigmoid colon in the young: With report of a case at four and a half years. Am J Surg. 1939;45:339-347. [RCA] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Bailey CE, Hu CY, You YN, Bednarski BK, Rodriguez-Bigas MA, Skibber JM, Cantor SB, Chang GJ. Increasing disparities in the age-related incidences of colon and rectal cancers in the United States, 1975-2010. JAMA Surg. 2015;150:17-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 513] [Cited by in RCA: 777] [Article Influence: 77.7] [Reference Citation Analysis (0)] |
| 6. | Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H, Forman D, Bray F. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013;49:1374-1403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3526] [Cited by in RCA: 3658] [Article Influence: 304.8] [Reference Citation Analysis (2)] |
| 7. | Pignone M, Rich M, Teutsch SM, Berg AO, Lohr KN. Screening for colorectal cancer in adults at average risk: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;137:132-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 500] [Cited by in RCA: 486] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 8. | Murphy CC, Sandler RS, Sanoff HK, Yang YC, Lund JL, Baron JA. Decrease in Incidence of Colorectal Cancer Among Individuals 50 Years or Older After Recommendations for Population-based Screening. Clin Gastroenterol Hepatol. 2017;15:903-909.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 106] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 9. | Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66:683-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3058] [Cited by in RCA: 3306] [Article Influence: 413.3] [Reference Citation Analysis (3)] |
| 10. | Siegel RL, Torre LA, Soerjomataram I, Hayes RB, Bray F, Weber TK, Jemal A. Global patterns and trends in colorectal cancer incidence in young adults. Gut. 2019;68:2179-2185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 417] [Cited by in RCA: 540] [Article Influence: 90.0] [Reference Citation Analysis (1)] |
| 11. | Galloway DJ, Burns HJ, Bear H, Jarrett F, Boyle P, George WD. Colorectal cancer in young adults. Clin Oncol. 1984;10:205-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 12. | O'Connell JB, Maggard MA, Livingston EH, Yo CK. Colorectal cancer in the young. Am J Surg. 2004;187:343-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 253] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 13. | Chang DT, Pai RK, Rybicki LA, Dimaio MA, Limaye M, Jayachandran P, Koong AC, Kunz PA, Fisher GA, Ford JM, Welton M, Shelton A, Ma L, Arber DA. Clinicopathologic and molecular features of sporadic early-onset colorectal adenocarcinoma: an adenocarcinoma with frequent signet ring cell differentiation, rectal and sigmoid involvement, and adverse morphologic features. Mod Pathol. 2012;25:1128-1139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 260] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 14. | Done JZ, Fang SH. Young-onset colorectal cancer: A review. World J Gastrointest Oncol. 2021;13:856-866. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 28] [Cited by in RCA: 54] [Article Influence: 13.5] [Reference Citation Analysis (6)] |
| 15. | Danial D, Youssef ED, Maryam BM, Mohammad A, Moein BM, Liliane D. Risk Factors of Young-Onset Colorectal Cancer: Analysis of a Large Population-Based Registry. Can J Gastroenterol Hepatol. 2022;2022:3582443. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 16. | Stjepanovic N, Moreira L, Carneiro F, Balaguer F, Cervantes A, Balmaña J, Martinelli E; ESMO Guidelines Committee. Electronic address: clinicalguidelines@esmo.org. Hereditary gastrointestinal cancers: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up†. Ann Oncol. 2019;30:1558-1571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 141] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 17. | Siegel RL, Jakubowski CD, Fedewa SA, Davis A, Azad NS. Colorectal Cancer in the Young: Epidemiology, Prevention, Management. Am Soc Clin Oncol Educ Book. 2020;40:1-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 98] [Article Influence: 19.6] [Reference Citation Analysis (1)] |
| 18. | Griffin PM, Liff JM, Greenberg RS, Clark WS. Adenocarcinomas of the colon and rectum in persons under 40 years old. A population-based study. Gastroenterology. 1991;100:1033-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 89] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Holowatyj AN, Ruterbusch JJ, Rozek LS, Cote ML, Stoffel EM. Racial/Ethnic Disparities in Survival Among Patients With Young-Onset Colorectal Cancer. J Clin Oncol. 2016;34:2148-2156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 119] [Article Influence: 13.2] [Reference Citation Analysis (1)] |
| 20. | Meester RG, Doubeni CA, Lansdorp-Vogelaar I, Goede SL, Levin TR, Quinn VP, Ballegooijen Mv, Corley DA, Zauber AG. Colorectal cancer deaths attributable to nonuse of screening in the United States. Ann Epidemiol. 2015;25:208-213.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 106] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 21. | Neufeld D, Shpitz B, Bugaev N, Grankin M, Bernheim J, Klein E, Ziv Y. Young-age onset of colorectal cancer in Israel. Tech Coloproctol. 2009;13:201-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Murphy CC, Lund JL, Sandler RS. Young-Onset Colorectal Cancer: Earlier Diagnoses or Increasing Disease Burden? Gastroenterology. 2017;152:1809-1812.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 66] [Article Influence: 8.3] [Reference Citation Analysis (1)] |
| 23. | Siegel RL, Fedewa SA, Anderson WF, Miller KD, Ma J, Rosenberg PS, Jemal A. Colorectal Cancer Incidence Patterns in the United States, 1974-2013. J Natl Cancer Inst. 2017;109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 568] [Cited by in RCA: 836] [Article Influence: 104.5] [Reference Citation Analysis (0)] |
| 24. | Vuik FE, Nieuwenburg SA, Bardou M, Lansdorp-Vogelaar I, Dinis-Ribeiro M, Bento MJ, Zadnik V, Pellisé M, Esteban L, Kaminski MF, Suchanek S, Ngo O, Májek O, Leja M, Kuipers EJ, Spaander MC. Increasing incidence of colorectal cancer in young adults in Europe over the last 25 years. Gut. 2019;68:1820-1826. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 476] [Cited by in RCA: 533] [Article Influence: 88.8] [Reference Citation Analysis (1)] |
| 25. | Park HK. Nutrition policy in South Korea. Asia Pac J Clin Nutr. 2008;17 Suppl 1:343-345. [PubMed] |
| 26. | Sung H, Siegel RL, Torre LA, Pearson-Stuttard J, Islami F, Fedewa SA, Goding Sauer A, Shuval K, Gapstur SM, Jacobs EJ, Giovannucci EL, Jemal A. Global patterns in excess body weight and the associated cancer burden. CA Cancer J Clin. 2019;69:88-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 277] [Article Influence: 46.2] [Reference Citation Analysis (0)] |
| 27. | Mármol I, Sánchez-de-Diego C, Pradilla Dieste A, Cerrada E, Rodriguez Yoldi MJ. Colorectal Carcinoma: A General Overview and Future Perspectives in Colorectal Cancer. Int J Mol Sci. 2017;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 520] [Cited by in RCA: 907] [Article Influence: 113.4] [Reference Citation Analysis (2)] |
| 28. | Nimptsch K, Wu K. Is Timing Important? Curr Colorectal Cancer Rep. 2018;14:1-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 29. | Karahalios A, English DR, Simpson JA. Weight change and risk of colorectal cancer: a systematic review and meta-analysis. Am J Epidemiol. 2015;181:832-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 92] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 30. | Wang Y, Beydoun MA, Min J, Xue H, Kaminsky LA, Cheskin LJ. Has the prevalence of overweight, obesity and central obesity levelled off in the United States? Int J Epidemiol. 2020;49:810-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 387] [Article Influence: 96.8] [Reference Citation Analysis (0)] |
| 31. | Patel P, De P. Trends in colorectal cancer incidence and related lifestyle risk factors in 15-49-year-olds in Canada, 1969-2010. Cancer Epidemiol. 2016;42:90-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 100] [Article Influence: 11.1] [Reference Citation Analysis (1)] |
| 32. | Liu PH, Wu K, Ng K, Zauber AG, Nguyen LH, Song M, He X, Fuchs CS, Ogino S, Willett WC, Chan AT, Giovannucci EL, Cao Y. Association of Obesity With Risk of Early-Onset Colorectal Cancer Among Women. JAMA Oncol. 2019;5:37-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 352] [Article Influence: 58.7] [Reference Citation Analysis (2)] |
| 33. | Hidayat K, Yang CM, Shi BM. Body fatness at an early age and risk of colorectal cancer. Int J Cancer. 2018;142:729-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 49] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 34. | van Kruijsdijk RC, van der Wall E, Visseren FL. Obesity and cancer: the role of dysfunctional adipose tissue. Cancer Epidemiol Biomarkers Prev. 2009;18:2569-2578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 483] [Cited by in RCA: 518] [Article Influence: 32.4] [Reference Citation Analysis (0)] |
| 35. | Larsson SC, Orsini N, Wolk A. Diabetes mellitus and risk of colorectal cancer: a meta-analysis. J Natl Cancer Inst. 2005;97:1679-1687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 719] [Cited by in RCA: 754] [Article Influence: 37.7] [Reference Citation Analysis (0)] |
| 36. | Ali Khan U, Fallah M, Sundquist K, Sundquist J, Brenner H, Kharazmi E. Risk of colorectal cancer in patients with diabetes mellitus: A Swedish nationwide cohort study. PLoS Med. 2020;17:e1003431. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 48] [Article Influence: 9.6] [Reference Citation Analysis (1)] |
| 37. | Li Z, Chen H, Fritz CDL, Zheng X, Zong X, Nickel KB, Tipping A, Nguyen LH, Chan AT, Giovannucci EL, Colditz GA, Olsen MA, Campbell PT, Davidson NO, Fields RC, Cao Y. Type 2 Diabetes and Risk of Early-Onset Colorectal Cancer. Gastro Hep Advances. 2022;1:186-193. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 38. | McNabb S, Harrison TA, Albanes D, Berndt SI, Brenner H, Caan BJ, Campbell PT, Cao Y, Chang-Claude J, Chan A, Chen Z, English DR, Giles GG, Giovannucci EL, Goodman PJ, Hayes RB, Hoffmeister M, Jacobs EJ, Joshi AD, Larsson SC, Le Marchand L, Li L, Lin Y, Männistö S, Milne RL, Nan H, Newton CC, Ogino S, Parfrey PS, Petersen PS, Potter JD, Schoen RE, Slattery ML, Su YR, Tangen CM, Tucker TC, Weinstein SJ, White E, Wolk A, Woods MO, Phipps AI, Peters U. Meta-analysis of 16 studies of the association of alcohol with colorectal cancer. Int J Cancer. 2020;146:861-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 103] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 39. | Botteri E, Iodice S, Bagnardi V, Raimondi S, Lowenfels AB, Maisonneuve P. Smoking and colorectal cancer: a meta-analysis. JAMA. 2008;300:2765-2778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 510] [Cited by in RCA: 577] [Article Influence: 33.9] [Reference Citation Analysis (0)] |
| 40. | Zisman AL, Nickolov A, Brand RE, Gorchow A, Roy HK. Associations between the age at diagnosis and location of colorectal cancer and the use of alcohol and tobacco: implications for screening. Arch Intern Med. 2006;166:629-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 84] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 41. | Rosato V, Bosetti C, Levi F, Polesel J, Zucchetto A, Negri E, La Vecchia C. Risk factors for young-onset colorectal cancer. Cancer Causes Control. 2013;24:335-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 128] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 42. | Wolin KY, Yan Y, Colditz GA, Lee IM. Physical activity and colon cancer prevention: a meta-analysis. Br J Cancer. 2009;100:611-616. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 398] [Cited by in RCA: 384] [Article Influence: 24.0] [Reference Citation Analysis (3)] |
| 43. | Kreger BE, Anderson KM, Schatzkin A, Splansky GL. Serum cholesterol level, body mass index, and the risk of colon cancer. The Framingham Study. Cancer. 1992;70:1038-1043. [PubMed] [DOI] [Full Text] |
| 44. | Yao X, Tian Z. Dyslipidemia and colorectal cancer risk: a meta-analysis of prospective studies. Cancer Causes Control. 2015;26:257-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 93] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 45. | Vieira AR, Abar L, Chan DSM, Vingeliene S, Polemiti E, Stevens C, Greenwood D, Norat T. Foods and beverages and colorectal cancer risk: a systematic review and meta-analysis of cohort studies, an update of the evidence of the WCRF-AICR Continuous Update Project. Ann Oncol. 2017;28:1788-1802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 288] [Article Influence: 41.1] [Reference Citation Analysis (0)] |
| 46. | Parr CL, Hjartåker A, Lund E, Veierød MB. Meat intake, cooking methods and risk of proximal colon, distal colon and rectal cancer: the Norwegian Women and Cancer (NOWAC) cohort study. Int J Cancer. 2013;133:1153-1163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 47. | Chao A, Thun MJ, Connell CJ, McCullough ML, Jacobs EJ, Flanders WD, Rodriguez C, Sinha R, Calle EE. Meat consumption and risk of colorectal cancer. JAMA. 2005;293:172-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 371] [Cited by in RCA: 339] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 48. | Fuchs MA, Sato K, Niedzwiecki D, Ye X, Saltz LB, Mayer RJ, Mowat RB, Whittom R, Hantel A, Benson A, Atienza D, Messino M, Kindler H, Venook A, Ogino S, Wu K, Willett WC, Giovannucci EL, Meyerhardt JA. Sugar-sweetened beverage intake and cancer recurrence and survival in CALGB 89803 (Alliance). PLoS One. 2014;9:e99816. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 49. | O'Keefe SJ. Diet, microorganisms and their metabolites, and colon cancer. Nat Rev Gastroenterol Hepatol. 2016;13:691-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 521] [Cited by in RCA: 779] [Article Influence: 86.6] [Reference Citation Analysis (0)] |
| 50. | Ma Y, Zhang P, Wang F, Yang J, Liu Z, Qin H. Association between vitamin D and risk of colorectal cancer: a systematic review of prospective studies. J Clin Oncol. 2011;29:3775-3782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 306] [Cited by in RCA: 287] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 51. | Rostom A, Dubé C, Lewin G, Tsertsvadze A, Barrowman N, Code C, Sampson M, Moher D; U. S. Preventive Services Task Force. Nonsteroidal anti-inflammatory drugs and cyclooxygenase-2 inhibitors for primary prevention of colorectal cancer: a systematic review prepared for the U.S. Preventive Services Task Force. Ann Intern Med. 2007;146:376-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 240] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 52. | Glover M, Mansoor E, Panhwar M, Parasa S, Cooper GS. Epidemiology of Colorectal Cancer in Average Risk Adults 20-39 Years of Age: A Population-Based National Study. Dig Dis Sci. 2019;64:3602-3609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 62] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 53. | Wu N, Yang X, Zhang R, Li J, Xiao X, Hu Y, Chen Y, Yang F, Lu N, Wang Z, Luan C, Liu Y, Wang B, Xiang C, Wang Y, Zhao F, Gao GF, Wang S, Li L, Zhang H, Zhu B. Dysbiosis signature of fecal microbiota in colorectal cancer patients. Microb Ecol. 2013;66:462-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 317] [Cited by in RCA: 343] [Article Influence: 28.6] [Reference Citation Analysis (1)] |
| 54. | Annese V, Beaugerie L, Egan L, Biancone L, Bolling C, Brandts C, Dierickx D, Dummer R, Fiorino G, Gornet JM, Higgins P, Katsanos KH, Nissen L, Pellino G, Rogler G, Scaldaferri F, Szymanska E, Eliakim R; ECCO. European Evidence-based Consensus: Inflammatory Bowel Disease and Malignancies. J Crohns Colitis. 2015;9:945-965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 332] [Cited by in RCA: 323] [Article Influence: 32.3] [Reference Citation Analysis (0)] |
| 55. | Dik VK, van Oijen MG, Smeets HM, Siersema PD. Frequent Use of Antibiotics Is Associated with Colorectal Cancer Risk: Results of a Nested Case-Control Study. Dig Dis Sci. 2016;61:255-264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 92] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 56. | Cao Y, Wu K, Mehta R, Drew DA, Song M, Lochhead P, Nguyen LH, Izard J, Fuchs CS, Garrett WS, Huttenhower C, Ogino S, Giovannucci EL, Chan AT. Long-term use of antibiotics and risk of colorectal adenoma. Gut. 2018;67:672-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 99] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 57. | Roller M, Clune Y, Collins K, Rechkemmer G, Watzl B. Consumption of prebiotic inulin enriched with oligofructose in combination with the probiotics Lactobacillus rhamnosus and Bifidobacterium lactis has minor effects on selected immune parameters in polypectomised and colon cancer patients. Br J Nutr. 2007;97:676-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 72] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 58. | Rafter J, Bennett M, Caderni G, Clune Y, Hughes R, Karlsson PC, Klinder A, O'Riordan M, O'Sullivan GC, Pool-Zobel B, Rechkemmer G, Roller M, Rowland I, Salvadori M, Thijs H, Van Loo J, Watzl B, Collins JK. Dietary synbiotics reduce cancer risk factors in polypectomized and colon cancer patients. Am J Clin Nutr. 2007;85:488-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 356] [Cited by in RCA: 327] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 59. | Lowery JT, Ahnen DJ, Schroy PC 3rd, Hampel H, Baxter N, Boland CR, Burt RW, Butterly L, Doerr M, Doroshenk M, Feero WG, Henrikson N, Ladabaum U, Lieberman D, McFarland EG, Peterson SK, Raymond M, Samadder NJ, Syngal S, Weber TK, Zauber AG, Smith R. Understanding the contribution of family history to colorectal cancer risk and its clinical implications: A state-of-the-science review. Cancer. 2016;122:2633-2645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 138] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 60. | Samadder NJ, Curtin K, Tuohy TM, Rowe KG, Mineau GP, Smith KR, Pimentel R, Wong J, Boucher K, Burt RW. Increased risk of colorectal neoplasia among family members of patients with colorectal cancer: a population-based study in Utah. Gastroenterology. 2014;147:814-821.e5; quiz e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 66] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 61. | Tuohy TM, Rowe KG, Mineau GP, Pimentel R, Burt RW, Samadder NJ. Risk of colorectal cancer and adenomas in the families of patients with adenomas: a population-based study in Utah. Cancer. 2014;120:35-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 59] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 62. | Ng SC, Lau JY, Chan FK, Suen BY, Tse YK, Hui AJ, Leung-Ki EL, Ching JY, Chan AW, Wong MC, Ng SS, To KF, Wu JC, Sung JJ. Risk of Advanced Adenomas in Siblings of Individuals With Advanced Adenomas: A Cross-Sectional Study. Gastroenterology. 2016;150:608-16; quiz e16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 63. | Stoffel EM, Koeppe E, Everett J, Ulintz P, Kiel M, Osborne J, Williams L, Hanson K, Gruber SB, Rozek LS. Germline Genetic Features of Young Individuals With Colorectal Cancer. Gastroenterology. 2018;154:897-905.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 246] [Article Influence: 35.1] [Reference Citation Analysis (0)] |
| 64. | Rombouts AJM, Hugen N, Elferink MAG, Poortmans PMP, Nagtegaal ID, de Wilt JHW. Increased risk for second primary rectal cancer after pelvic radiation therapy. Eur J Cancer. 2020;124:142-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 65. | Riaz R, Masood N, Benish A. Red flag symptoms: detailed account of clinicopathological features in young-onset colorectal cancer. Intest Res. 2017;15:203-207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 66. | Goldvaser H, Purim O, Kundel Y, Shepshelovich D, Shochat T, Shemesh-Bar L, Sulkes A, Brenner B. Colorectal cancer in young patients: is it a distinct clinical entity? Int J Clin Oncol. 2016;21:684-695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 67. | Segev L, Kalady MF, Church JM. Left-Sided Dominance of Early-Onset Colorectal Cancers: A Rationale for Screening Flexible Sigmoidoscopy in the Young. Dis Colon Rectum. 2018;61:897-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 54] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 68. | Willauer AN, Liu Y, Pereira AAL, Lam M, Morris JS, Raghav KPS, Morris VK, Menter D, Broaddus R, Meric-Bernstam F, Hayes-Jordan A, Huh W, Overman MJ, Kopetz S, Loree JM. Clinical and molecular characterization of early-onset colorectal cancer. Cancer. 2019;125:2002-2010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 242] [Article Influence: 40.3] [Reference Citation Analysis (0)] |
| 69. | Petrelli F, Tomasello G, Borgonovo K, Ghidini M, Turati L, Dallera P, Passalacqua R, Sgroi G, Barni S. Prognostic Survival Associated With Left-Sided vs Right-Sided Colon Cancer: A Systematic Review and Meta-analysis. JAMA Oncol. 2017;3:211-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 538] [Article Influence: 67.3] [Reference Citation Analysis (0)] |
| 70. | Chen FW, Sundaram V, Chew TA, Ladabaum U. Advanced-Stage Colorectal Cancer in Persons Younger Than 50 Years Not Associated With Longer Duration of Symptoms or Time to Diagnosis. Clin Gastroenterol Hepatol. 2017;15:728-737.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 203] [Article Influence: 25.4] [Reference Citation Analysis (0)] |
| 71. | Marble K, Banerjee S, Greenwald L. Colorectal carcinoma in young patients. J Surg Oncol. 1992;51:179-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 71] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 72. | Myers EA, Feingold DL, Forde KA, Arnell T, Jang JH, Whelan RL. Colorectal cancer in patients under 50 years of age: a retrospective analysis of two institutions' experience. World J Gastroenterol. 2013;19:5651-5657. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 104] [Cited by in RCA: 128] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 73. | Mitchell E, Macdonald S, Campbell NC, Weller D, Macleod U. Influences on pre-hospital delay in the diagnosis of colorectal cancer: a systematic review. Br J Cancer. 2008;98:60-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 158] [Cited by in RCA: 166] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 74. | Fu J, Yang J, Tan Y, Jiang M, Wen F, Huang Y, Chen H, Yi C, Zheng S, Yuan Y. Young patients (≤ 35 years old) with colorectal cancer have worse outcomes due to more advanced disease: a 30-year retrospective review. Medicine (Baltimore). 2014;93:e135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 75. | Rho YS, Gilabert M, Polom K, Aladashvili A, Kopeckova K, Megdanova V, Coleman N, Greally M, Marrelli D, Roviello F, McDermott R, Petrova V, Mihaylova Z, Bortlicek Z, Prausova J, Batist G, Azoulay L, Kavan P. Comparing Clinical Characteristics and Outcomes of Young-onset and Late-onset Colorectal Cancer: An International Collaborative Study. Clin Colorectal Cancer. 2017;16:334-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 57] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 76. | Kim TJ, Kim ER, Hong SN, Chang DK, Kim YH. Long-Term Outcome and Prognostic Factors of Sporadic Colorectal Cancer in Young Patients: A Large Institutional-Based Retrospective Study. Medicine (Baltimore). 2016;95:e3641. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 77. | Wang R, Wang MJ, Ping J. Clinicopathological Features and Survival Outcomes of Colorectal Cancer in Young Versus Elderly: A Population-Based Cohort Study of SEER 9 Registries Data (1988-2011). Medicine (Baltimore). 2015;94:e1402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 71] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 78. | Silla IO, Rueda D, Rodríguez Y, García JL, de la Cruz Vigo F, Perea J. Early-onset colorectal cancer: a separate subset of colorectal cancer. World J Gastroenterol. 2014;20:17288-17296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 93] [Cited by in RCA: 94] [Article Influence: 8.5] [Reference Citation Analysis (2)] |
| 79. | Yurgelun MB, Kulke MH, Fuchs CS, Allen BA, Uno H, Hornick JL, Ukaegbu CI, Brais LK, McNamara PG, Mayer RJ, Schrag D, Meyerhardt JA, Ng K, Kidd J, Singh N, Hartman AR, Wenstrup RJ, Syngal S. Cancer Susceptibility Gene Mutations in Individuals With Colorectal Cancer. J Clin Oncol. 2017;35:1086-1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 371] [Article Influence: 46.4] [Reference Citation Analysis (0)] |
| 80. | Pearlman R, Frankel WL, Swanson B, Zhao W, Yilmaz A, Miller K, Bacher J, Bigley C, Nelsen L, Goodfellow PJ, Goldberg RM, Paskett E, Shields PG, Freudenheim JL, Stanich PP, Lattimer I, Arnold M, Liyanarachchi S, Kalady M, Heald B, Greenwood C, Paquette I, Prues M, Draper DJ, Lindeman C, Kuebler JP, Reynolds K, Brell JM, Shaper AA, Mahesh S, Buie N, Weeman K, Shine K, Haut M, Edwards J, Bastola S, Wickham K, Khanduja KS, Zacks R, Pritchard CC, Shirts BH, Jacobson A, Allen B, de la Chapelle A, Hampel H; Ohio Colorectal Cancer Prevention Initiative Study Group. Prevalence and Spectrum of Germline Cancer Susceptibility Gene Mutations Among Patients With Early-Onset Colorectal Cancer. JAMA Oncol. 2017;3:464-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 369] [Cited by in RCA: 516] [Article Influence: 64.5] [Reference Citation Analysis (0)] |
| 81. | Puccini A, Lenz HJ, Marshall JL, Arguello D, Raghavan D, Korn WM, Weinberg BA, Poorman K, Heeke AL, Philip PA, Shields AF, Goldberg RM, Salem ME. Impact of Patient Age on Molecular Alterations of Left-Sided Colorectal Tumors. Oncologist. 2019;24:319-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 82. | Gupta S, Provenzale D, Llor X, Halverson AL, Grady W, Chung DC, Haraldsdottir S, Markowitz AJ, Slavin TP Jr, Hampel H; CGC, Ness RM, Weiss JM, Ahnen DJ, Chen LM, Cooper G, Early DS, Giardiello FM, Hall MJ, Hamilton SR, Kanth P, Klapman JB, Lazenby AJ, Lynch PM, Mayer RJ, Mikkelson J; CGC, Peter S, Regenbogen SE, Dwyer MA; CGC, Ogba N. NCCN Guidelines Insights: Genetic/Familial High-Risk Assessment: Colorectal, Version 2.2019. J Natl Compr Canc Netw. 2019;17:1032-1041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 180] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 83. | Weiss JM, Gupta S, Burke CA, Axell L, Chen LM, Chung DC, Clayback KM, Dallas S, Felder S, Gbolahan O, Giardiello FM, Grady W, Hall MJ, Hampel H, Hodan R, Idos G, Kanth P, Katona B, Lamps L, Llor X, Lynch PM, Markowitz AJ, Pirzadeh-Miller S, Samadder NJ, Shibata D, Swanson BJ, Szymaniak BM, Wiesner GL, Wolf A, Yurgelun MB, Zakhour M, Darlow SD, Dwyer MA, Campbell M. NCCN Guidelines® Insights: Genetic/Familial High-Risk Assessment: Colorectal, Version 1.2021. J Natl Compr Canc Netw. 2021;19:1122-1132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 46] [Reference Citation Analysis (0)] |
| 84. | Currais P, Rosa I, Claro I. Colorectal cancer carcinogenesis: From bench to bedside. World J Gastrointest Oncol. 2022;14:654-663. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 85. | Syngal S, Brand RE, Church JM, Giardiello FM, Hampel HL, Burt RW; American College of Gastroenterology. ACG clinical guideline: Genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015;110:223-62; quiz 263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 957] [Cited by in RCA: 1090] [Article Influence: 109.0] [Reference Citation Analysis (0)] |
| 86. | Stoffel EM, Murphy CC. Epidemiology and Mechanisms of the Increasing Incidence of Colon and Rectal Cancers in Young Adults. Gastroenterology. 2020;158:341-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 381] [Article Influence: 76.2] [Reference Citation Analysis (1)] |
| 87. | Chen FW, Sundaram V, Chew TA, Ladabaum U. Low Prevalence of Criteria for Early Screening in Young-Onset Colorectal Cancer. Am J Prev Med. 2017;53:933-934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 88. | André T, Cohen R, Salem ME. Immune Checkpoint Blockade Therapy in Patients With Colorectal Cancer Harboring Microsatellite Instability/Mismatch Repair Deficiency in 2022. Am Soc Clin Oncol Educ Book. 2022;42:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 89. | Banerjea A, Hands RE, Powar MP, Bustin SA, Dorudi S. Microsatellite and chromosomal stable colorectal cancers demonstrate poor immunogenicity and early disease recurrence. Colorectal Dis. 2009;11:601-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 43] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 90. | Khan SA, Morris M, Idrees K, Gimbel MI, Rosenberg S, Zeng Z, Li F, Gan G, Shia J, LaQuaglia MP, Paty PB. Colorectal cancer in the very young: a comparative study of tumor markers, pathology and survival in early onset and adult onset patients. J Pediatr Surg. 2016;51:1812-1817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 76] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 91. | Antelo M, Balaguer F, Shia J, Shen Y, Hur K, Moreira L, Cuatrecasas M, Bujanda L, Giraldez MD, Takahashi M, Cabanne A, Barugel ME, Arnold M, Roca EL, Andreu M, Castellvi-Bel S, Llor X, Jover R, Castells A, Boland CR, Goel A. A high degree of LINE-1 hypomethylation is a unique feature of early-onset colorectal cancer. PLoS One. 2012;7:e45357. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 180] [Cited by in RCA: 166] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 92. | Yiu R, Qiu H, Lee SH, García-Aguilar J. Mechanisms of microsatellite instability in colorectal cancer patients in different age groups. Dis Colon Rectum. 2005;48:2061-2069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 93. | Popat S, Hubner R, Houlston RS. Systematic review of microsatellite instability and colorectal cancer prognosis. J Clin Oncol. 2005;23:609-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1267] [Cited by in RCA: 1347] [Article Influence: 67.4] [Reference Citation Analysis (1)] |
| 94. | Perea J, Rueda D, Canal A, Rodríguez Y, Álvaro E, Osorio I, Alegre C, Rivera B, Martínez J, Benítez J, Urioste M. Age at onset should be a major criterion for subclassification of colorectal cancer. J Mol Diagn. 2014;16:116-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 67] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 95. | Ballester V, Rashtak S, Boardman L. Clinical and molecular features of young-onset colorectal cancer. World J Gastroenterol. 2016;22:1736-1744. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 107] [Cited by in RCA: 124] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 96. | Chan TL, Curtis LC, Leung SY, Farrington SM, Ho JW, Chan AS, Lam PW, Tse CW, Dunlop MG, Wyllie AH, Yuen ST. Early-onset colorectal cancer with stable microsatellite DNA and near-diploid chromosomes. Oncogene. 2001;20:4871-4876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 58] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 97. | Jones PA, Baylin SB. The epigenomics of cancer. Cell. 2007;128:683-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3299] [Cited by in RCA: 3405] [Article Influence: 189.2] [Reference Citation Analysis (0)] |
| 98. | Ogino S, Nosho K, Kirkner GJ, Kawasaki T, Chan AT, Schernhammer ES, Giovannucci EL, Fuchs CS. A cohort study of tumoral LINE-1 hypomethylation and prognosis in colon cancer. J Natl Cancer Inst. 2008;100:1734-1738. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 312] [Cited by in RCA: 302] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 99. | Herzig D, Hardiman K, Weiser M, You N, Paquette I, Feingold DL, Steele SR. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Management of Inherited Polyposis Syndromes. Dis Colon Rectum. 2017;60:881-894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 100. | Argilés G, Tabernero J, Labianca R, Hochhauser D, Salazar R, Iveson T, Laurent-Puig P, Quirke P, Yoshino T, Taieb J, Martinelli E, Arnold D; ESMO Guidelines Committee. Electronic address: clinicalguidelines@esmo.org. Localised colon cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;31:1291-1305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 491] [Cited by in RCA: 806] [Article Influence: 161.2] [Reference Citation Analysis (0)] |
| 101. | Quah HM, Joseph R, Schrag D, Shia J, Guillem JG, Paty PB, Temple LK, Wong WD, Weiser MR. Young age influences treatment but not outcome of colon cancer. Ann Surg Oncol. 2007;14:2759-2765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 110] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 102. | Kneuertz PJ, Chang GJ, Hu CY, Rodriguez-Bigas MA, Eng C, Vilar E, Skibber JM, Feig BW, Cormier JN, You YN. Overtreatment of young adults with colon cancer: more intense treatments with unmatched survival gains. JAMA Surg. 2015;150:402-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 204] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 103. | Abdelsattar ZM, Wong SL, Regenbogen SE, Jomaa DM, Hardiman KM, Hendren S. Colorectal cancer outcomes and treatment patterns in patients too young for average-risk screening. Cancer. 2016;122:929-934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 181] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 104. | van Erning FN, van Steenbergen LN, Lemmens VEPP, Rutten HJT, Martijn H, van Spronsen DJ, Janssen-Heijnen MLG. Conditional survival for long-term colorectal cancer survivors in the Netherlands: who do best? Eur J Cancer. 2014;50:1731-1739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 105. | D'Onofrio GM, Tan EG. Is colorectal carcinoma in the young a more deadly disease? Aust N Z J Surg. 1985;55:537-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 106. | Chung YF, Eu KW, Machin D, Ho JM, Nyam DC, Leong AF, Ho YH, Seow-Choen F. Young age is not a poor prognostic marker in colorectal cancer. Br J Surg. 1998;85:1255-1259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 82] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 107. | Varma JR, Sample L. Colorectal cancer in patients aged less than 40 years. J Am Board Fam Pract. 1990;3:54-59. [PubMed] |
| 108. | Bülow S. Colorectal cancer in patients less than 40 years of age in Denmark, 1943-1967. Dis Colon Rectum. 1980;23:327-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 75] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 109. | Blanke CD, Bot BM, Thomas DM, Bleyer A, Kohne CH, Seymour MT, de Gramont A, Goldberg RM, Sargent DJ. Impact of young age on treatment efficacy and safety in advanced colorectal cancer: a pooled analysis of patients from nine first-line phase III chemotherapy trials. J Clin Oncol. 2011;29:2781-2786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 57] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 110. | Siegel RL, Miller KD, Fedewa SA, Ahnen DJ, Meester RGS, Barzi A, Jemal A. Colorectal cancer statistics, 2017. CA Cancer J Clin. 2017;67:177-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2526] [Cited by in RCA: 2912] [Article Influence: 364.0] [Reference Citation Analysis (3)] |
| 111. | Sankila R, Aaltonen LA, Järvinen HJ, Mecklin JP. Better survival rates in patients with MLH1-associated hereditary colorectal cancer. Gastroenterology. 1996;110:682-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 233] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 112. | Watson P, Lin KM, Rodriguez-Bigas MA, Smyrk T, Lemon S, Shashidharan M, Franklin B, Karr B, Thorson A, Lynch HT. Colorectal carcinoma survival among hereditary nonpolyposis colorectal carcinoma family members. Cancer. 1998;83:259-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 113. | Schreuders EH, Ruco A, Rabeneck L, Schoen RE, Sung JJ, Young GP, Kuipers EJ. Colorectal cancer screening: a global overview of existing programmes. Gut. 2015;64:1637-1649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 674] [Cited by in RCA: 916] [Article Influence: 91.6] [Reference Citation Analysis (0)] |
| 114. | Wolf AMD, Fontham ETH, Church TR, Flowers CR, Guerra CE, LaMonte SJ, Etzioni R, McKenna MT, Oeffinger KC, Shih YT, Walter LC, Andrews KS, Brawley OW, Brooks D, Fedewa SA, Manassaram-Baptiste D, Siegel RL, Wender RC, Smith RA. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin. 2018;68:250-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 945] [Cited by in RCA: 1313] [Article Influence: 187.6] [Reference Citation Analysis (0)] |
| 115. | Rundle AG, Lebwohl B, Vogel R, Levine S, Neugut AI. Colonoscopic screening in average-risk individuals ages 40 to 49 vs 50 to 59 years. Gastroenterology. 2008;134:1311-1315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 97] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 116. | You YN, Xing Y, Feig BW, Chang GJ, Cormier JN. Young-onset colorectal cancer: is it time to pay attention? Arch Intern Med. 2012;172:287-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 215] [Article Influence: 15.4] [Reference Citation Analysis (1)] |
| 117. | Anderson JC, Samadder JN. To Screen or Not to Screen Adults 45-49 Years of Age: That is the Question. Am J Gastroenterol. 2018;113:1750-1753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 118. | Kastrinos F, Steyerberg EW, Mercado R, Balmaña J, Holter S, Gallinger S, Siegmund KD, Church JM, Jenkins MA, Lindor NM, Thibodeau SN, Burbidge LA, Wenstrup RJ, Syngal S. The PREMM(1,2,6) model predicts risk of MLH1, MSH2, and MSH6 germline mutations based on cancer history. Gastroenterology. 2011;140:73-81. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 134] [Cited by in RCA: 145] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 119. | Hendren SK, O'Connor BI, Liu M, Asano T, Cohen Z, Swallow CJ, Macrae HM, Gryfe R, McLeod RS. Prevalence of male and female sexual dysfunction is high following surgery for rectal cancer. Ann Surg. 2005;242:212-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 408] [Cited by in RCA: 430] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 120. | Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K, Beck LN, Brennan LV, Oktay K; American Society of Clinical Oncology. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006;24:2917-2931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1448] [Cited by in RCA: 1350] [Article Influence: 71.1] [Reference Citation Analysis (0)] |
| 121. | Oktay K, Harvey BE, Loren AW. Fertility Preservation in Patients With Cancer: ASCO Clinical Practice Guideline Update Summary. J Oncol Pract. 2018;14:381-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 103] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 122. | Rogers JE, Dasari A, Eng C. The Treatment of Colorectal Cancer During Pregnancy: Cytotoxic Chemotherapy and Targeted Therapy Challenges. Oncologist. 2016;21:563-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 123. | Reese JB, Finan PH, Haythornthwaite JA, Kadan M, Regan KR, Herman JM, Efron J, Diaz LA Jr, Azad NS. Gastrointestinal ostomies and sexual outcomes: a comparison of colorectal cancer patients by ostomy status. Support Care Cancer. 2014;22:461-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 124. | Bailey CE, Tran Cao HS, Hu CY, Chang GJ, Feig BW, Rodriguez-Bigas MA, Nguyen ST, Skibber JM, You YN. Functional deficits and symptoms of long-term survivors of colorectal cancer treated by multimodality therapy differ by age at diagnosis. J Gastrointest Surg. 2015;19:180-8; discussio 188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 125. | Mols F, Schoormans D, de Hingh I, Oerlemans S, Husson O. Symptoms of anxiety and depression among colorectal cancer survivors from the population-based, longitudinal PROFILES Registry: Prevalence, predictors, and impact on quality of life. Cancer. 2018;124:2621-2628. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 127] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 126. | Andersen BL, DeRubeis RJ, Berman BS, Gruman J, Champion VL, Massie MJ, Holland JC, Partridge AH, Bak K, Somerfield MR, Rowland JH; American Society of Clinical Oncology. Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer: an American Society of Clinical Oncology guideline adaptation. J Clin Oncol. 2014;32:1605-1619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 500] [Cited by in RCA: 502] [Article Influence: 45.6] [Reference Citation Analysis (0)] |