Published online Feb 21, 2023. doi: 10.3748/wjg.v29.i7.1235
Peer-review started: November 8, 2022
First decision: January 3, 2023
Revised: January 19, 2023
Accepted: January 30, 2023
Article in press: January 30, 2023
Published online: February 21, 2023
Processing time: 104 Days and 14.2 Hours
Pancreatic neuroendocrine neoplasms (PNENs) are a rare group of neoplasms originating from the islets of the Langerhans. Portal vein tumor thrombosis has been reported in 33% of patients with PNENs. While the histopathological diagnosis of PNENs is usually based on percutaneous biopsy or endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA), these approaches may be impeded by gastric varices, poor access windows, or anatomically contiguous critical structures. Obtaining a pathological diagnosis using a gastroscope biopsy forceps via percutaneous transhepatic intravascular pathway is an innovative method that has rarely been reported.
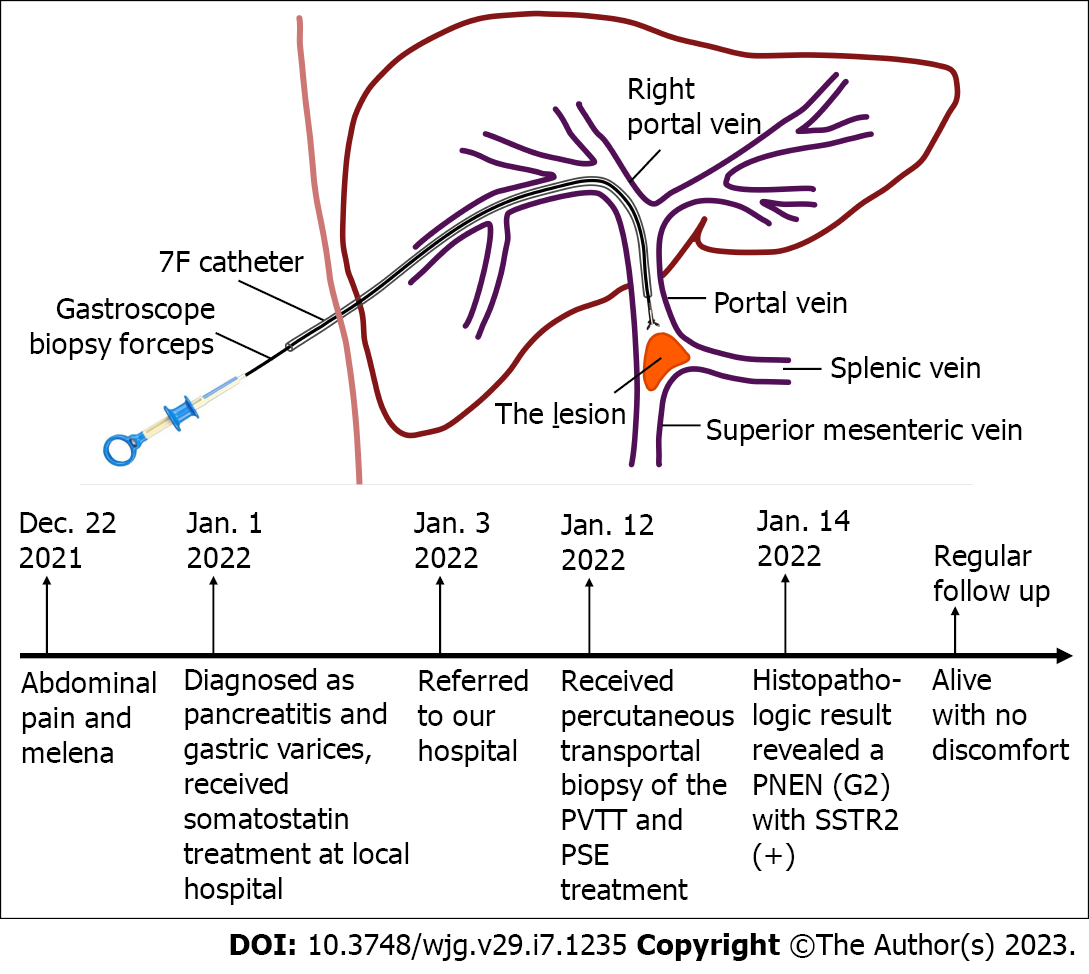
A 72-year-old man was referred to our hospital for abdominal pain and melena. Abdominal contrast-enhanced magnetic resonance imaging revealed a well-enhanced tumor (size: 2.4 cm × 1.2 cm × 1.2 cm) in the pancreatic tail with portal vein invasion. Traditional pathological diagnosis via EUS-FNA was not possible because of diffuse gastric varices. We performed a percutaneous transportal biopsy of the portal vein tumor thrombus using a gastroscope biopsy forceps. Histopathologic examination revealed a pancreatic neuroendocrine neoplasm (G2) with somatostatin receptors 2 (+), allowing systemic treatment.
Intravascular biopsy using gastroscope biopsy forceps appears to be a safe and effective method for obtaining a histopathological diagnosis. Although well-designed clinic trials are required to obtain more definitive evidence, this procedure may help improve the diagnosis of portal vein thrombosis and related diseases.
Core Tip: Endoscopic ultrasound-guided fine-needle aspiration or percutaneous biopsy of pancreatic neuroendocrine neoplasms patients can be impeded by gastric varices and poor access windows. In this patient, we faced the challenge of obtaining biopsy of the pancreatic mass which had invaded the portal vein. We performed a percutaneous transportal biopsy of the portal vein tumor thrombosis using a gastroscope biopsy forceps. Our experience suggests that gastroscope biopsy forceps is a viable alternative to obtain biopsy in the portal vein system. Our work expands the use of diagnostic transhepatic portal catheterization. This method may also help prevent repeated liver puncture, reducing the risk of complications.
- Citation: Wang GC, Huang GJ, Zhang CQ, Ding Q. Percutaneous transhepatic intraportal biopsy using gastroscope biopsy forceps for diagnosis of a pancreatic neuroendocrine neoplasm: A case report. World J Gastroenterol 2023; 29(7): 1235-1242
- URL: https://www.wjgnet.com/1007-9327/full/v29/i7/1235.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i7.1235
Pancreatic neuroendocrine neoplasms (PNENs) are rare tumors accounting for approximately 2% of all pancreatic tumors[1]. Portal vein tumor thrombosis (PVTT) was reported in approximately 33% of patients with non-functioning PNENs (NF-PNENs)[2]. Tumor thrombosis in such cases may cause splenoportomesenteric hypertension, potentially resulting in life-threatening upper gastrointestinal bleeding. Computed tomography (CT) or magnetic resonance imaging (MRI) is useful for diagnosis. Tissue samples are usually obtained via imaging-guided percutaneous fine-needle aspiration biopsy or core needle biopsy, endoscopic retrograde cholangiopancreatography, or endoscopic ultrasound-guided fine-needle aspiration/biopsy (EUS-FNA/B)[3]. This report describes the first diagnostic case of percutaneous transhepatic intravascular biopsy of PVTT caused by PNEN invasion using a gastroscope biopsy forceps in a patient with severe gastric varices in whom diagnosis could not be made through percutaneous or endoscopic approaches.
A 72-year-old man was referred to a local hospital for upper abdominal pain with melena for 10 d.
He was diagnosed with pancreatitis and gastric varices. The abdominal pain was relieved after somatostatin treatment for 2 d. The patient was referred to our hospital for further treatment.
Six months ago, he was diagnosed with gastric varices after undergoing gastroscopy as part of routine medical checkup; however, he did not undergo further evaluation.
He had no family history of malignant tumors, psychological, or genetic disorders.
Physical examination showed pallor.
Laboratory investigations showed three lineage pancytopenia (hemoglobin 66 g/L, WBC count: 2.4 × 109/L, platelet count: 83.0 × 109/L). Serum transaminases, bilirubin, and amylase levels were normal. Urine routine, stool routine and occult blood test were negative. Serum tumor markers (AFP, CEA, CA199, and NSE) were all within the normal reference range.
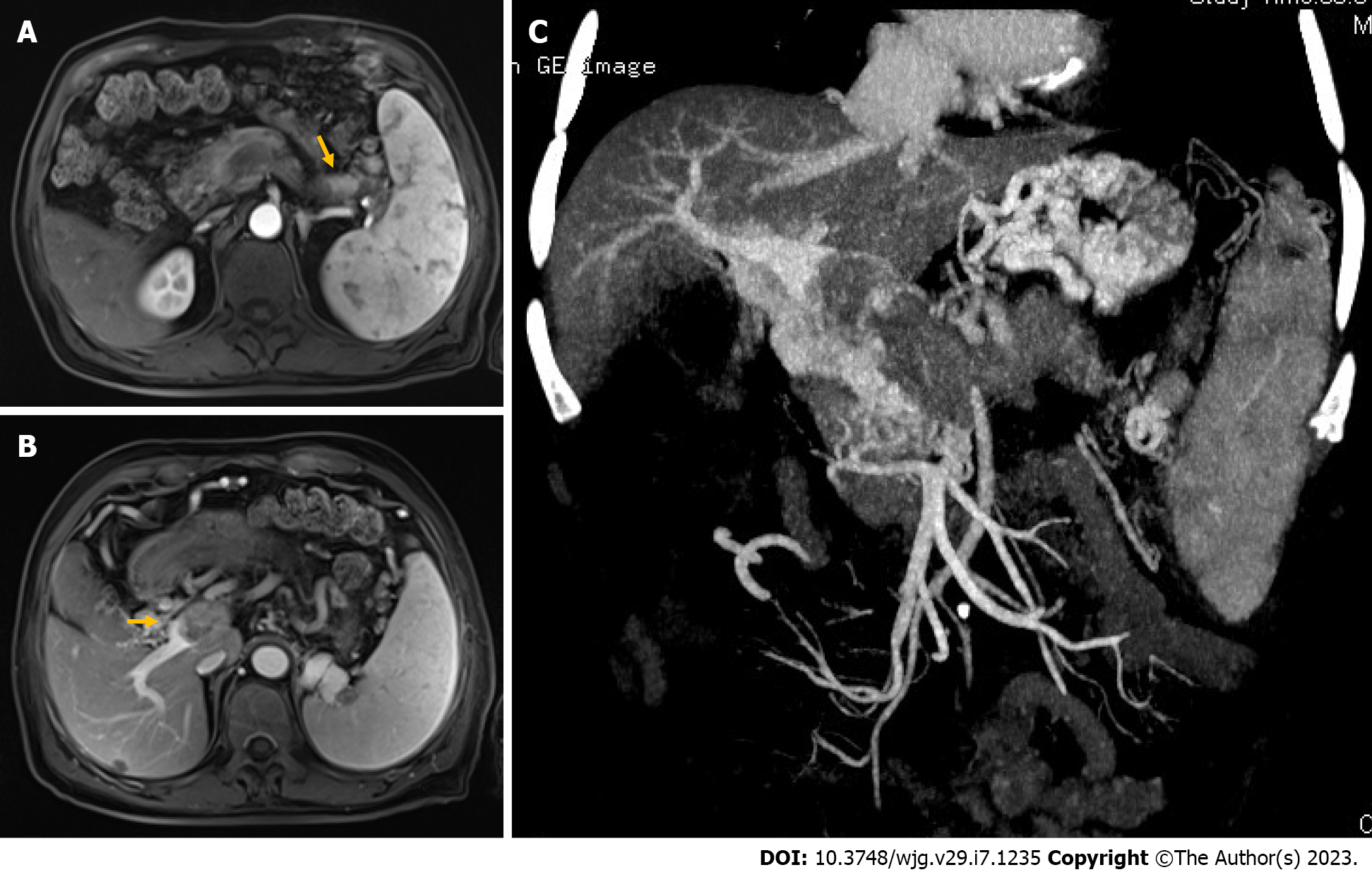
Abdominal contrast-enhanced MRI revealed a well-enhanced tumor (size: 2.4 cm × 1.2 cm × 1.2 cm) in the pancreatic tail (Figure 1A), with portal vein invasion (Figure 1B and C), and the presence of many collateral vessels indicative of portal stenosis (Figure 1C). The mass inside the portal vein was enhanced too, suggesting that it was a tumor rather than a thrombus. Splenomegaly was also observed, which was considered as a secondary change. No metastasis was found in other organs, including the lymph nodes, liver parenchyma, and lungs.
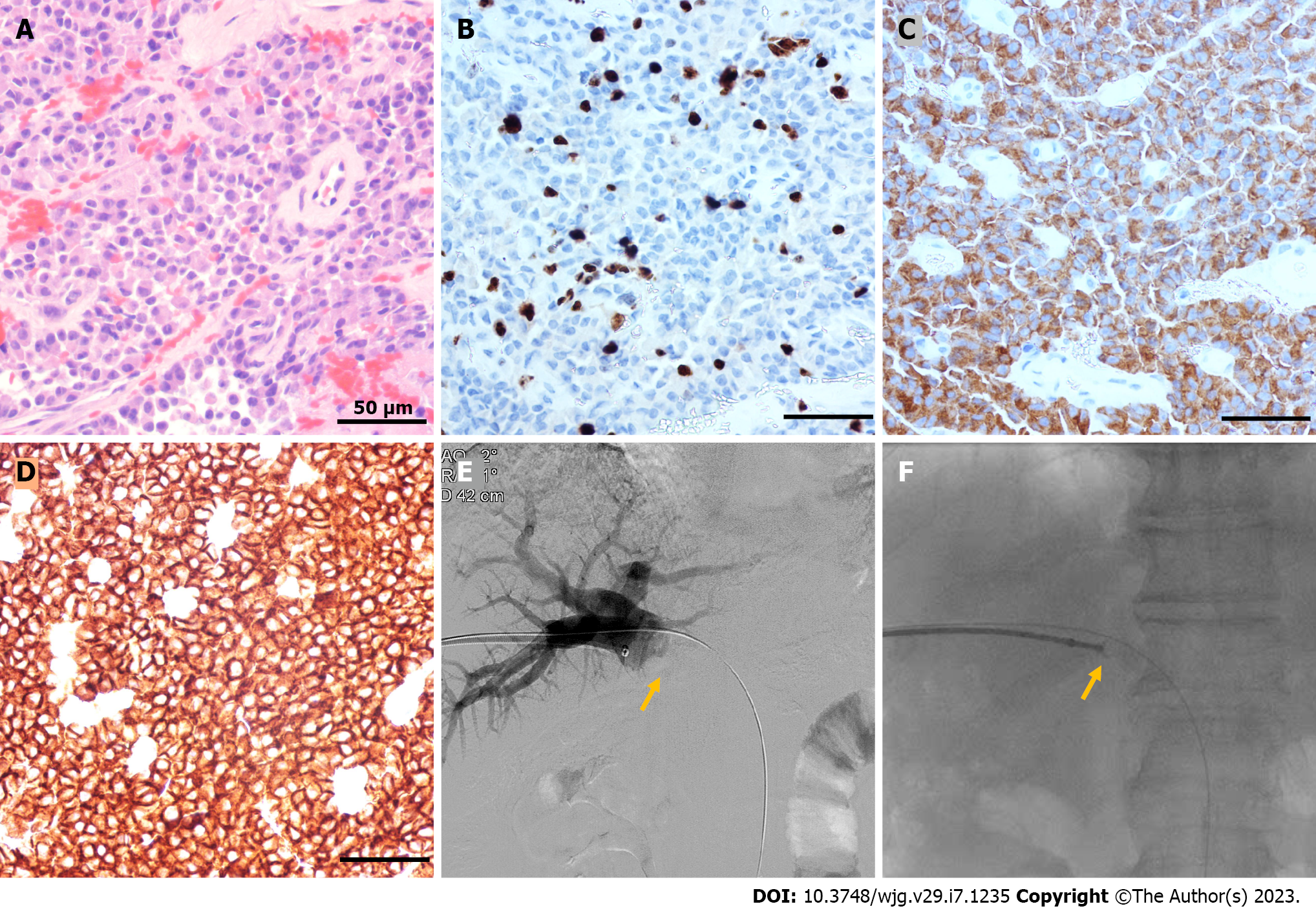
Histopathologic examination revealed a NEN (G2) with somatostatin receptors 2 (SSTR2) (+) (Figure 2A-D).
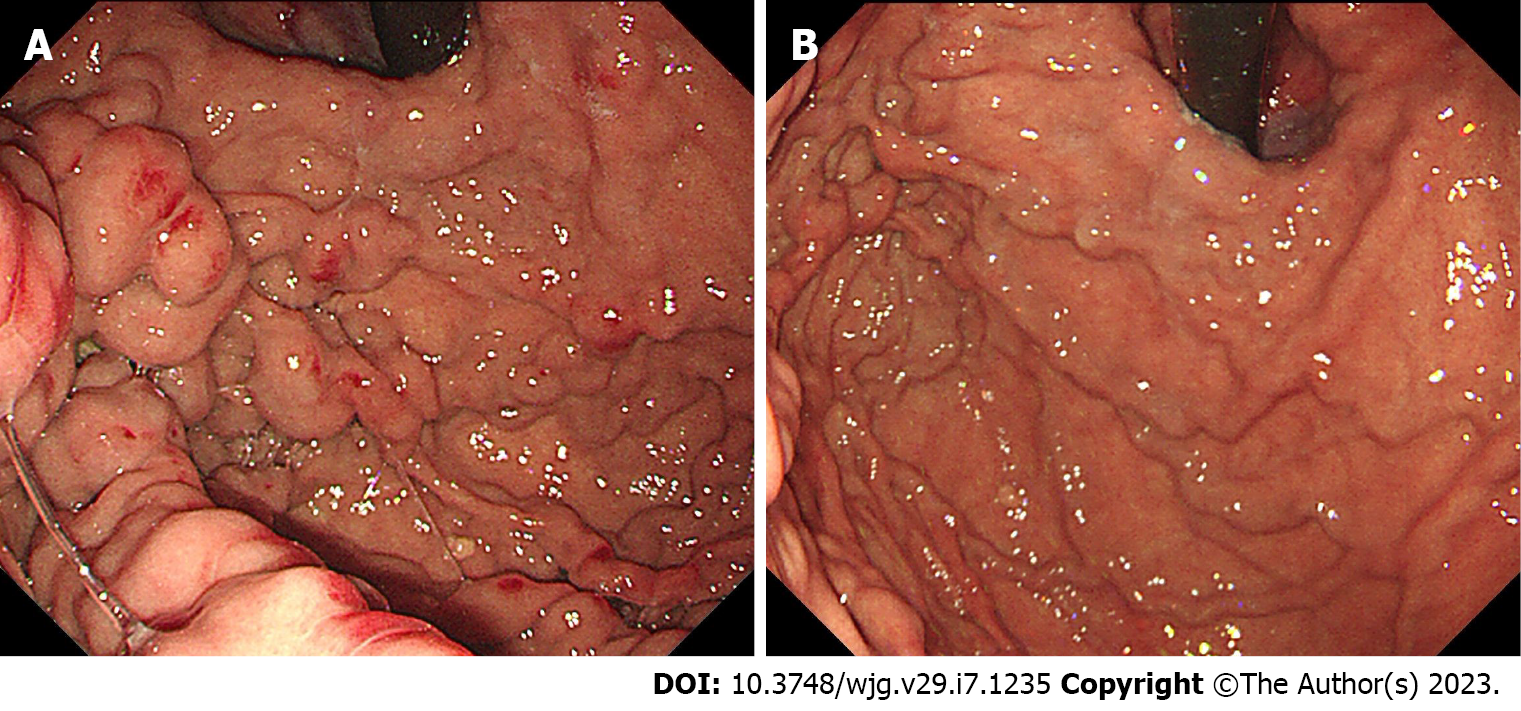
A multidisciplinary team meeting was held to discuss the case. Diagnosis of PNEN with portal vein invasion was highly suspected. Surgical resection was considered risky because of the involvement of adjacent organs and sinistral portal hypertension. Interventional therapy to prevent upper gastrointestinal hemorrhage and chemotherapy were suggested. However, pathological diagnosis via EUS-FNA seemed infeasible because of diffuse gastric varices (Figure 3A). The possibility of percutaneous CT/ultrasound-guided fine-needle aspiration biopsy was also excluded since no adequate access was identified. Finally, we performed percutaneous transportal biopsy of the PVTT using a gastroscope biopsy forceps. After percutaneous transhepatic puncture of the right-portal vein under sonographic guidance, 7F “crossover sheath” catheter was introduced into the right-portal vein and the biopsy forceps was inserted into the catheter. Under X-ray guidance, the biopsy forceps was pushed close to the thrombus and 3 samples were obtained (Figure 2E and F; Figure 4; Supplementary material) and fixed immediately. Subsequently, partial splenic embolization (PSE) was performed for treating the gastric varices. After obtaining the histopathologic results, the patient received octreotide long-acting release (LAR) injection. There were no postoperative complications, and the patient was discharged on postoperative day 8. Owing to the high risk of gastric varices hemorrhage, the patient received repeat PSE treatment.
Follow-up gastroscopy performed after one month showed significant alleviation of gastric varices (Figure 3B). Subsequently, the patient regularly received octreotide LAR injection at a local hospital. He experienced weight loss and fatigue for the following 2-4 mo and recovered gradually. He received no chemotherapy or CT/MRI re-examination for some personal reasons. As of 8-mo follow-up, the patient is alive and showed no discomfort.
Histological diagnosis is essential for the treatment of patients with PNEN and can be carried out using resection samples, while core biopsies can be performed in patients with advanced disease[4]. 68Ga-DOTATOC-PET-CT, with high sensitivity (92%) and specificity (83%), has been recommended as part of tumor staging, preoperative imaging, and restaging[4]. The EUS features (size and irregular lesion margins) associated with malignancy/aggressiveness of iso- and hypervascular solid pancreatic lesions have also been reported[5]. However, a definitive diagnosis cannot be established based on imaging findings alone. Biopsy can be performed by EUS-FNA/B or percutaneous ultrasound/CT-guided biopsy. Currently, EUS-FNA/B represents the gold standard for diagnosis of pancreatic lesions[6]. This technique provides pathological diagnosis as well as mitotic rate and Ki-67 index which defines grading, with an overall accuracy of approximately 92%[5], leading to its fundamental role in PNENs. However, these approaches may be hampered by gastric varices, poor access windows, target mobility, adjacent critical structures, and skin-to-target remoteness.
PNENs originate in the endocrine cells of the pancreas, and some of them can secrete specific hormones. Thus, PNENs can be classified as functional PNENs or non-functioning PNENs (NF-PNENs). Due to the lack of symptoms, NF-PENs tend to remain occult until a late stage of disease. In the study by Balachandran et al[2], venous tumor thrombus was detected by CT in 29 out of 88 (33%) patients with NF-PNEN. Six of these 29 patients showed invasion of portal vein. Portal venous tumor thrombus (PVTT) is a typical complication of hepatocellular carcinoma and is associated with a poor prognosis[7]. Other causes of PVTT include gastrointestinal and abdominal-pelvic malignant tumors[8]. Pancreatic neoplasms, especially neuroendocrine tumors, represent a possible but uncommon etiology of portal venous invasion[9,10].
Due to the PVTT in the present case, a gastroscope biopsy forceps-assisted intravascular biopsy was a safe and effective procedure for obtaining samples for histopathology, allowing the initiation of targeted drugs and chemotherapy. Portal vein catheterization has a certain learning curve, and the biopsy device must be introduced into the lesion by transhepatic approach using a large enough catheter (7 Fr). This would lead to a high risk of bleeding due to hepatic tract puncture. To prevent this complication, the puncture tract was embolized with coils, and the patient recovered well without any complications. Clinical use of percutaneous transhepatic portal catheterization was first described in 1970[11,12]. Since then, this has been proven to be a safe technique with few complications[13,14]. It is widely used to control gastroesophageal variceal bleeding[15-17] and to localize gastrointestinal hormone-producing tumors[18-21]. In hormone-producing tumors, percutaneous transhepatic portal catheterization has usually been performed for blood sampling from the portal vein. Here we expanded the use and value of transhepatic portal catheterization for diagnostic purposes.
The use of endoscopic biopsy forceps in intravenous biopsy has been reported. Guirola et al[22] reported an intravascular biopsy using a bronchoscopy forceps for facilitating the diagnosis of pulmonary artery intimal sarcoma. Chick JFBreported a transbiliary intravascular ultrasound-guided diagnostic biopsy of an inaccessible pancreatic head mass using core biopsy needle[3]. Sherk et al[23] reported a single-center retrospective analysis of 36 patients who underwent transvenous biopsy using cutting biopsy forceps; one of the patients in their study underwent a PVTT biopsy via transhepatic portal vein access, which is similar as our work. Apart from this, the use of biopsy forceps in portal vein biopsy has rarely been reported, let alone gastroscope biopsy forceps. Dodd GD III and Vilana R both performed Doppler-guided percutaneous portal vein thrombi biopsy using aspiration needle[24,25]. The potential side effects of percutaneous portal vein sampling include severe biliary or vascular injury. The potential complications include hepatic arterial or portal venous bleeding, bile duct laceration, and formation of biliary-vascular fistula, arterio-venous fistula, or pseudoaneurysm. EUS-FNA of portal venous thrombi represents an alternative approach which might overcome these limitations. Compared with fine needle aspiration, our method may help avert the need for repeated liver puncture, and reduce the risk of injury.
Currently, dual-tracer (68Ga-DOTATOC and 18F-FDG-)-PET/CT scan is a powerful imaging modality for the diagnosis and evaluation of PNET[26]. We did not perform the PET/CT scan owing to the patient’s financial constraints. Moreover, the final therapeutic choice for the inoperable tumor would not have changed regardless of the tumor stage. The validity of our method was uncertain prior to this case. Lack of malignant cells in the specimen obtained from a malignant thrombus may lead to a false-negative diagnosis. We tried to prevent false-negative result by obtaining samples for 3 times. Our positive result suggests that tumor cells can be obtained from the PVTT. Our work suggests that the gastroscope biopsy forceps of an appropriate size and function is a suitable substitute to obtain biopsy in the portal vein system. There is still a need for well-designed clinic trials, but this procedure may improve the diagnosis of portal vein thrombosis and related diseases.
Percutaneous transhepatic intraportal biopsy is valuable for the diagnosis of portal thrombosis and related diseases. Using gastroscope biopsy forceps through the sheath for tissue sample appears to be safe and effective, and can be performed in the context of other interventional procedures. More clinical trials are required to verify the safety and efficacy of this technique.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sempokuya T, United States; Su YY, Taiwan; Zeng C, United States S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
| 1. | Vega EA, Kutlu OC, Alarcon SV, Salehi O, Kazakova V, Kozyreva O, Chan JA, Conrad C. Clinical Prognosticators of Metastatic Potential in Patients with Small Pancreatic Neuroendocrine Tumors. J Gastrointest Surg. 2021;25:2593-2599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 2. | Balachandran A, Tamm EP, Bhosale PR, Katz MH, Fleming JB, Yao JC, Charnsangavej C. Venous tumor thrombus in nonfunctional pancreatic neuroendocrine tumors. AJR Am J Roentgenol. 2012;199:602-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Chick JFB, Roush BB, Khaja MS, Prohaska D, Cooper KJ, Saad WE, Srinivasa RN. Transbiliary intravascular ultrasound-guided diagnostic biopsy of an inaccessible pancreatic head mass. Radiol Case Rep. 2017;12:323-326. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Pavel M, Öberg K, Falconi M, Krenning EP, Sundin A, Perren A, Berruti A; ESMO Guidelines Committee. Electronic address: clinicalguidelines@esmo.org. Gastroenteropancreatic neuroendocrine neoplasms: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;31:844-860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 465] [Cited by in RCA: 696] [Article Influence: 139.2] [Reference Citation Analysis (0)] |
| 5. | Crinó SF, Brandolese A, Vieceli F, Paiella S, Conti Bellocchi MC, Manfrin E, Bernardoni L, Sina S, D'Onofrio M, Marchegiani G, Larghi A, Frulloni L, Landoni L, Gabbrielli A. Endoscopic Ultrasound Features Associated with Malignancy and Aggressiveness of Nonhypovascular Solid Pancreatic Lesions: Results from a Prospective Observational Study. Ultraschall Med. 2021;42:167-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 6. | Tacelli M, Bina N, Crinò SF, Facciorusso A, Celsa C, Vanni AS, Fantin A, Antonini F, Falconi M, Monica F, Capurso G, Arcidiacono PG, Barresi L; of the Italian Association of Hospital Gastroenterologists and Endoscopists. Reliability of grading preoperative pancreatic neuroendocrine tumors on EUS specimens: a systematic review with meta-analysis of aggregate and individual data. Gastrointest Endosc. 2022;96:898-908.e23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 7. | Giannelli G, Pierri F, Trerotoli P, Marinosci F, Serio G, Schiraldi O, Antonaci S. Occurrence of portal vein tumor thrombus in hepatocellular carcinoma affects prognosis and survival. A retrospective clinical study of 150 cases. Hepatol Res. 2002;24:50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Ishida H, Konno K, Hamashima Y, Naganuma H, Komatsuda T, Sato M, Kimura H, Ishida J, Sakai T, Watanabe S. Portal tumor thrombus due to gastrointestinal cancer. Abdom Imaging. 1999;24:585-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Obuz F, Bora S, Sarioğlu S. Malignant islet cell tumor of the pancreas associated with portal venous thrombus. Eur Radiol. 2001;11:1642-1644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Usatoff V, Wittkop B, Devalia K, Guest P, Buckels J. Solid papillary-cystic carcinoma of the pancreas with portal vein tumour thrombus. ANZ J Surg. 2004;74:291-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Lunderquist A, Vang J. Sclerosing injection of esophageal varices through transhepatic selective catheterization of the gastric coronary vein. A preliminary report. Acta Radiol Diagn (Stockh). 1974;15:546-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Lunderquist A, Vang J. Transhepatic catheterization and obliteration of the coronary vein in patients with portal hypertension and esophageal varices. N Engl J Med. 1974;291:646-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 240] [Cited by in RCA: 201] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 13. | Burcharth F. Percutaneous transhepatic portography. I. Technique and application. AJR Am J Roentgenol. 1979;132:177-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 33] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Viamonte M Jr, LePage J, Lunderquist A, Pereiras R, Russell E, Viamonte M, Camacho M. Selective catheterization of the portal vein and its tributaries. Preliminary report. Radiology. 1975;114:457-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Scott J, Dick R, Long RG, Sherlock S. Percutaneous transhepatic obliteration of gastro-oesophageal varices. Lancet. 1976;2:53-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 51] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Goldman ML, LAND WC, Bradley EL, Anderson RT. Transcatheter therapeutic embolization in the management of massive upper gastrointestinal bleeding. Radiology. 1976;120:513-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 56] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Viamonte M Jr, Pereiras R, Russell E, Le Page J, Hutson D. Transhepatic obliteration of gastroesophageal varices: results in acute and nonacute bleeders. AJR Am J Roentgenol. 1977;129:237-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 47] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Millan VG, Urosa CL, Molitch ME, Miller H, Jackson IM. Localization of occult insulinoma by super-selective pancreatic venous sampling for insulin assay through percutaneous transhepatic catheterization. Diabetes. 1979;28:249-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Reichardt W, Ingemansson S. Selective vein catheterization for hormone assay in endocrine tumours of the pancreas. Technique and results. Acta Radiol Diagn (Stockh). 1980;21:177-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Passaro E Jr. Localization of pancreatic endocrine tumors by selective portal vein catheterization and radioimmunoassay. Gastroenterology. 1979;77:806-807. [PubMed] |
| 21. | Suzuki K, Takahashi S, Aiura K, Hayatsu S, Kitago M, Hoshimoto S, Kitajima M. Evaluation of the usefulness of percutaneous transhepatic portal catheterization for preoperatively diagnosing the localization of insulinomas. Pancreas. 2002;24:96-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Guirola JA, Laborda A, De Gregorio MA. Percutaneous Intravascular Biopsy Using a Bronchoscopy Forceps Diagnosis of a Pulmonary Artery Intimal Sarcoma. Cardiovasc Intervent Radiol. 2017;40:318-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 23. | Sherk WM, Khaja MS, Majdalany BS, Saad WE, Udager AM, Cooper KJ, Williams DM. Transvenous Biopsy in the Diagnosis of Intravascular or Perivascular Neoplasm: A Single-Center Retrospective Analysis of 36 Patients. J Vasc Interv Radiol. 2019;30:54-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Dodd GD 3rd, Carr BI. Percutaneous biopsy of portal vein thrombus: a new staging technique for hepatocellular carcinoma. AJR Am J Roentgenol. 1993;161:229-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 36] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Vilana R, Bru C, Bruix J, Castells A, Sole M, Rodes J. Fine-needle aspiration biopsy of portal vein thrombus: value in detecting malignant thrombosis. AJR Am J Roentgenol. 1993;160:1285-1287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 36] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 26. | Paiella S, Landoni L, Tebaldi S, Zuffante M, Salgarello M, Cingarlini S, D'Onofrio M, Parisi A, Deiro G, Manfrin E, Bianchi B, Montagnini G, Crinò SF, Bassi C, Salvia R. Dual-Tracer (68Ga-DOTATOC and 18F-FDG-)-PET/CT Scan and G1-G2 Nonfunctioning Pancreatic Neuroendocrine Tumors: A Single-Center Retrospective Evaluation of 124 Nonmetastatic Resected Cases. Neuroendocrinology. 2022;112:143-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |