Published online Feb 14, 2023. doi: 10.3748/wjg.v29.i6.1054
Peer-review started: September 29, 2022
First decision: December 12, 2022
Revised: December 23, 2022
Accepted: January 20, 2023
Article in press: January 20, 2023
Published online: February 14, 2023
Processing time: 133 Days and 16.9 Hours
Hepatocellular carcinoma (HCC) is one of the world’s deadliest and fastest-growing tumors, with a poor prognosis. HCC develops in the context of chronic liver disease. Curative resection, surgery (liver transplantation), trans-arterial chemoembolization, radioembolization, radiofrequency ablation and chemo
Core Tip: Hepatocellular carcinoma (HCC) is a multifaceted illness with multiple faces. It avoids early discovery, which provides the best chance of cure by resection/transplant, and systemic treatments are only of marginal efficacy at best, despite recent therapeutic advances. Current advances in immunotherapy and its combinations have altered the HCC treatment landscape, and clinical studies are continuing to pave the path forward. Immunotherapy increases survival rates and provides long-term cancer control in subsets of HCC patients while also minimizing side effects. Further research into immunotherapy in combination with current treatments for HCC in the early and intermediate stages may assist a greater spectrum of patients. Continued research into programmed cell death-1/ programmed cell death ligand 1, TMB, ctDNA, microsatellite stability, DNA mismatch repair, neutrophil/lymphocyte ratio, cytokines, and cellular peripheral immune response will hopefully identify the most reliable marker for selecting and sequencing systemic treatments to achieve the best outcome in HCC patients. Despite such significant treatment advances in HCC, numerous hurdles remain. The scientific community must figure out how to appropriately sequence these medicines for the best potential response, how to control toxicities, and how to develop indicators to monitor for response and relapse.
- Citation: Mandlik DS, Mandlik SK, Choudhary HB. Immunotherapy for hepatocellular carcinoma: Current status and future perspectives. World J Gastroenterol 2023; 29(6): 1054-1075
- URL: https://www.wjgnet.com/1007-9327/full/v29/i6/1054.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i6.1054
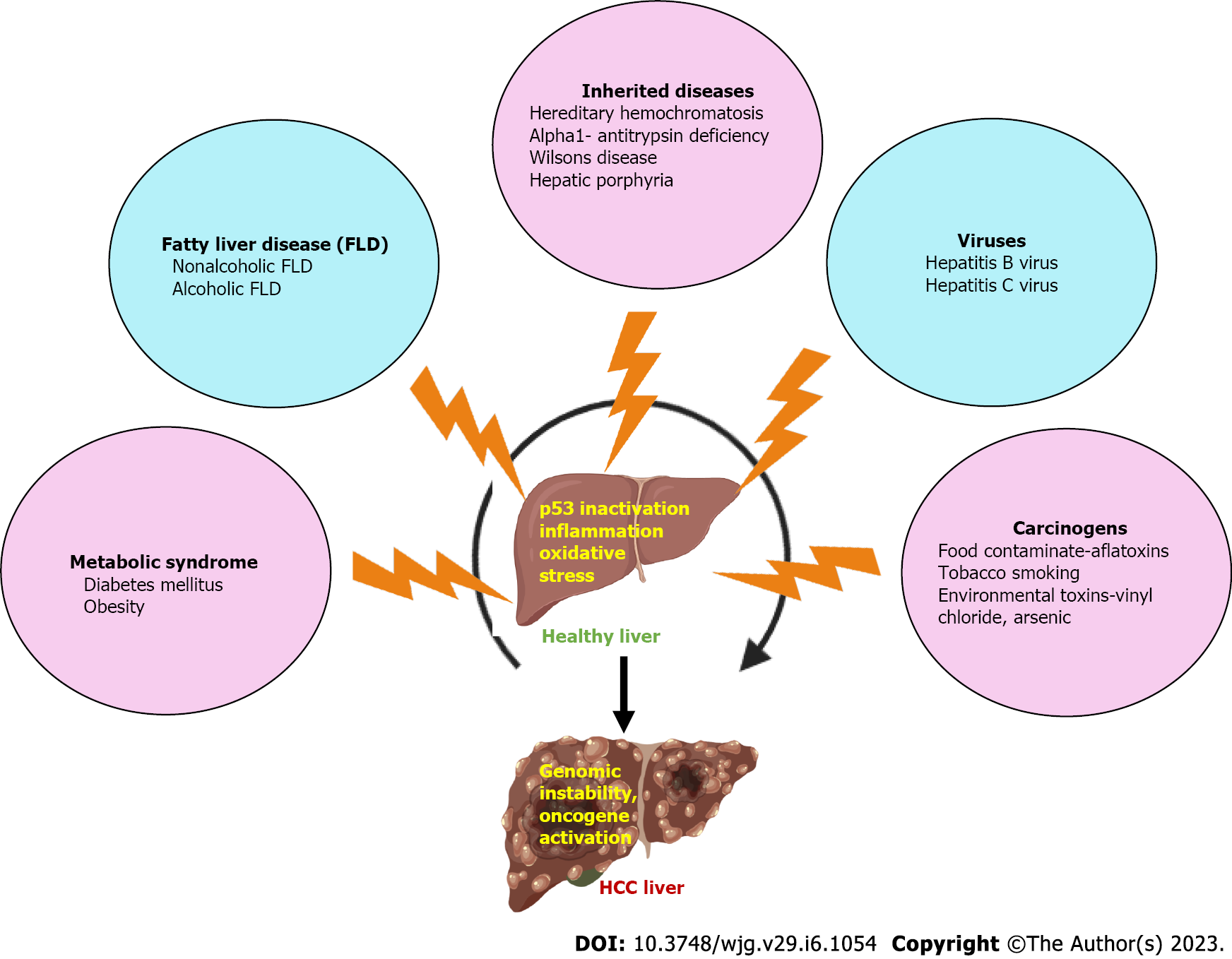
Hepatocellular carcinoma (HCC) is the world’s fifth most frequent malignancy and the third main cause of cancer death[1]. Men are slightly more likely than women to get HCC (3:1 male-to-female ratio). Globally, primary liver cancer caused an estimated 906000 new cases and 830000 fatalities in 2020; the majority of these cases (75%-85%) were HCC[2]. Underlying liver conditions including cirrhosis or chronic hepatitis frequently led to HCC. Hepatitis C virus (HCV), hepatitis B virus (HBV), fatty liver disease like non-alcoholic steatohepatitis, and alcohol consumption are the most prominent risk factors (Figure 1)[3]. The 5-year age-standardized rate of relative survival for HCC is only 18.1%, even though surgical intervention is currently the best therapy for HCC. Tumor reappearance is common after tumor removal[4]. In adult males, HCC is the second most common cancer-related killer after lung cancer because of the challenge of earlier detection, which results in the vast bulk of HCC patients receiving a higher stage diagnosis at their first visit and being ineligible for treatments like radiofrequency ablation (RFA) or hepatectomy[5]. Sorafenib and lenvatinib, the two clinically authorized targeted therapy medicines, could barely extend survival time by 2 to 3 mo[6,7]. As a result, novel HCC therapy techniques are urgently required.
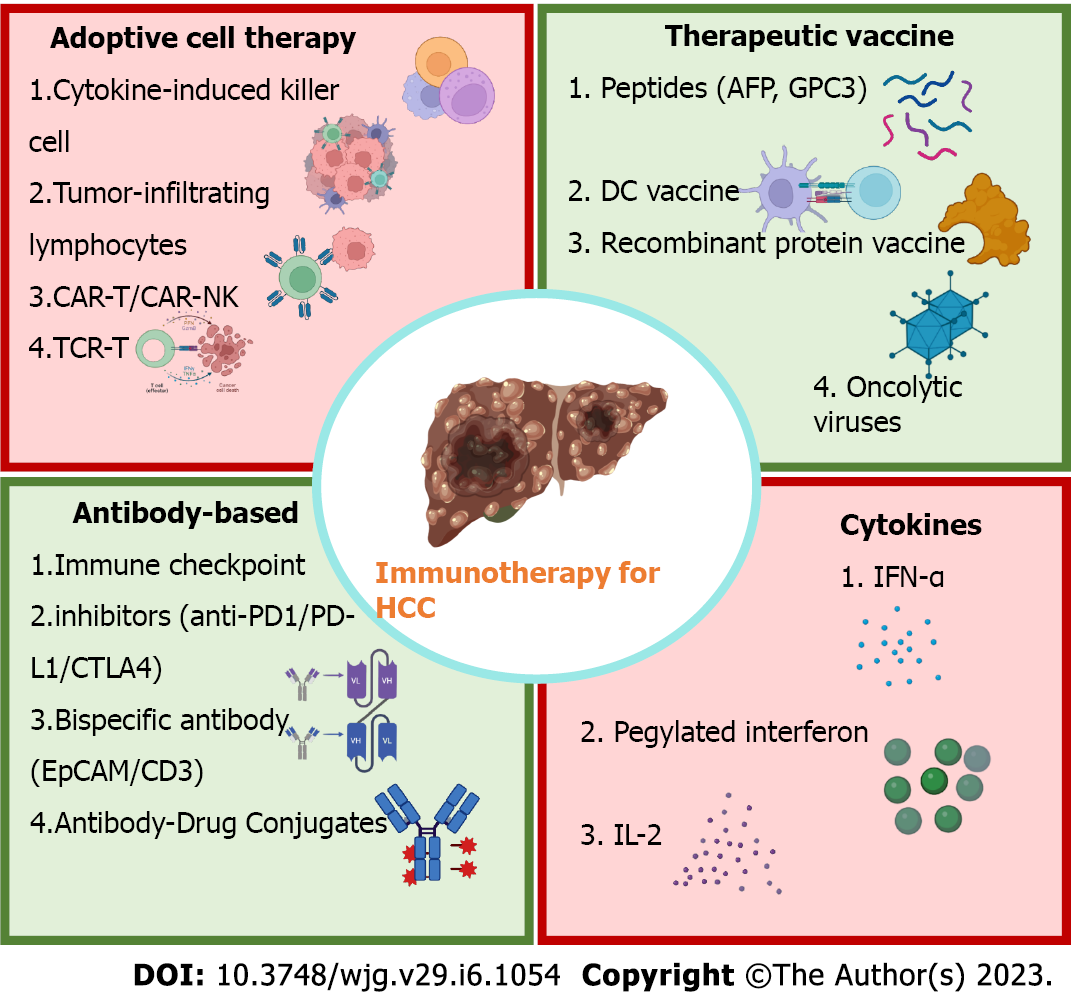
Immunotherapy is successful and safe in the treatment of solid tumors, resulting in long-term survival and manageable toxicity[8,9]. The liver is a remarkable immunologically tolerant organ that is exceptional in its capacity to accept liver transplants and diminish responsiveness to antigens in bacterial and food products through the portal vein[10]. This tolerogenic trait of the liver and the immunosuppressive tumor microenvironment of HCC may jointly inhibit the formation of anti-tumor immunity against HCC. Cancer immunotherapy may be a compelling therapeutic approach for HCC, which has a metachronous, multicentric incidence due to its capacity to trigger systemic and long-lasting anti-tumor actions. For numerous forms of malignancies, along with HCC, the FDA has so far approved seven immune checkpoint inhibitors (ICIs) that target the programmed cell death protein-1 (PD-1), proteins cytotoxic T lymphocyte antigen 4 (CTLA-4), or its ligand programmed cell death-ligand 1 (PD-L1)[11,12]. Other immunotherapeutic approaches, like immune cells modified with chimeric antigen receptors, adoptive cell treatment, tailored cytokines, and cancer vaccines, are almost ready and provide HCC patients new hope[13-15]. In this review, we first provide an overview of the current state of immunotherapy for HCC (Figure 2), after which we analyze the challenges, opportunities, and potential directions of this field of study.
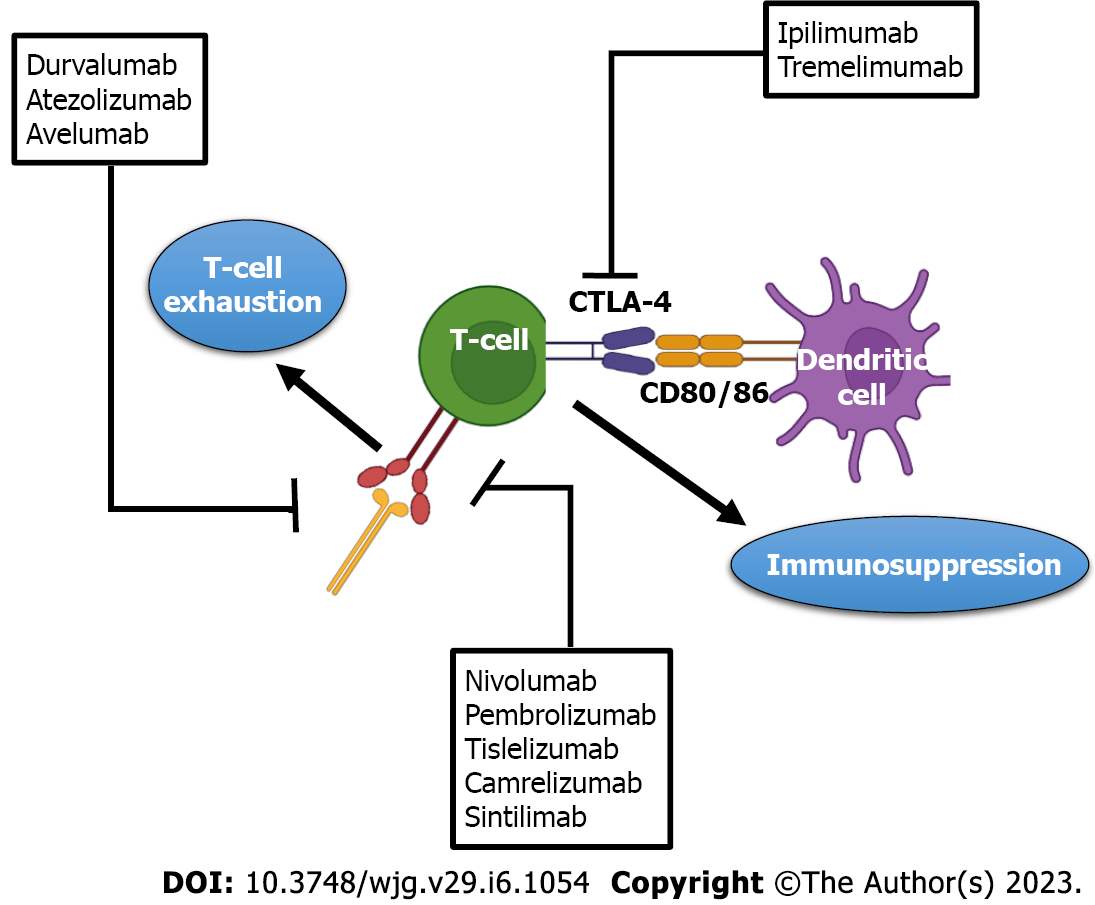
Effector immune cells express inhibitory immunoreceptors called immunological checkpoints that keep the immune system from overreacting. The T cell immunoreceptor with Ig and ITIM domains (TIGIT), lymphocyte-activation gene 3 (LAG3), B and T lymphocyte attenuator, and T cell immunoglobulin and mucin domain containing-3 (TIM3) are only a few of the inhibitory receptors in this group[16]. This physiological process is employed by HCC and other solid tumors to thwart anti-tumor immune reactions[17]. Monoclonal antibodies known as ICIs have the potential to prevent immunological checkpoint proteins from interacting with their ligands. This could improve the immune response against tumors by preventing T cell inactivation and reactivating immune attack and immune recognition. At the moment, ICIs’ primary targets are CTLA-4, PD-1, and PD-L1[13]. Most immune cells, myeloid-derived suppressor cells, primarily activated T cells, regulatory T cells (Tregs), natural killer (NK) cells, dendritic cells (DCs), and monocytes express PD-1 and are members of the CD28 family. When PD-1 binds to its ligands, i.e. PD-L1 and PD-L2, that are stimulated in a variety of cancers, including HCC, it can send T cells inhibitory signals and cause tumor cells to bypass the immune system[18].
Nivolumab, a PD1 inhibitor, was given expedited approval in the United States in 2017 for this second-line treatment of patients with severe HCC following sorafenib therapy. ICIs have been used to treat HCC in several exploratory trials that have been completed so far. PD-1 and PD-L1 inhibitors pembrolizumab and atezolizumab, which target these receptors, respectively, have been steadily proposed as a clinical therapy strategy for HCC and added to the treatment recommendations of numerous nations. Nivolumab and pembrolizumab cause objective remissions of 15%-20%, which includes complete remissions of 1%-5%, and these remissions are long-lasting and linked with improved survival. Nivolumab had a median response duration of 17 mo in the dose-escalation cohort in 48 patients of the CheckMate 040 investigation, and responders had a survival rate of about 2 years of more than 80%[19]. Statistically longer survival was seen in the 413 patients who took part in phase III clinical trial KEYNOTE-240, which compared pembrolizumab after sorafenib medication to placebo. Pembrolizumab was found to have long-term advantages for some people, as seen by the overall survival curves and progression-free survival. Around 20% of patients who got pembrolizumab stayed in progression-free status for longer than a year, as opposed to merely 7% of the control group[20]. In the phase III CheckMate 459 trial, 743 patients who had never received systemic medications were compared between nivolumab and sorafenib. Patients who received nivolumab had a longer median survival time than those who received sorafenib[21]. The CheckMate 459 study’s lengthier follow-up period confirmed nivolumab’s better ability to sorafenib to raise the long-term rate of survival[22].
Recent studies presented at the ESMO 2021 Annual Meeting revealed that tislelizumab, a humanized monoclonal antibody (mAb) with substantial adhesion for PD-1, evidenced durable response and was well tolerated in individuals who had previously systemically treated unresectable HCC. In a global, randomized phase 3 trial, the first-line therapies for adult patients having unresectable HCC are tislelizumab and sorafenib (NCT03412773)[23]. The majority of activated T cells and DCs express CTLA-4, a member of the CD28 family. After binding to B7 molecules, it participates in the downregulation of the immune response[24]. The FDA approved ipilimumab, the first ICI, in 2011 for the therapy of patients with severe skin cancer. Tremelimumab is another CTLA-4 inhibitor[25].
Tremelimumab, an IgG2 mAb, has different antibody-dependent cell-mediated cytotoxicity and complement-dependent cytotoxicity activities than Ipilimumab, an IgG1 mAb[26]. Tremelimumab demonstrated a potent anti-HCC impact in a clinical trial conducted in 2013, with a 17.6% of partial response (PR) rate and 76.4% of disease control rate[27]. With the in-depth analysis of CTLA-4 inhibitors’ mechanism, some researchers hypothesize that it involves the targeted eradication of Tregs from tumors rather than the immune checkpoint[28]. In human HCC, the presence of TIM3 on tumor-associated macrophages and tumor-infiltrating lymphocytes (TILs) impairs T cells’ ability to operate as effector cells, while increasing the activation of Tregs’ suppressor genes[29]. Less differentiated HCC is linked to the highly expressed TIM3[30]. LAG3 appearance is much greater on tumor-specific CD4+ and CD8+ TILs in patients with HCC compared to other immune compartments. Hepatocytes produce fibrinogen-like protein 1, another useful soluble ligand for LAG3[31]. The most recent studies published demonstrate that Siglec-15 inhibits CD44’s lysosomal degradation, which encourages the migration of liver cancer cells[31,32]. T-cell immunoreceptor with immunoglobulin and ITIM domains also plays a role in TIGIT[33]. The TIGIT/CD155 pathway increases interleukin (IL)-10 synthesis and decreases IL-12 by DCs to prevent T cell activation[34]. The exploration of Siglec-15, TIM3, TIGIT, and LAG3 inhibitors in HCC in conjunction with PD1 and PDL1 inhibition is supported by the preclinical evidence presented here. According to the findings of current clinical studies, patients medicated with ICIs alone, have a lower rate of response; as a result, future therapies will combine ICIs and other therapies.
The results of the worldwide, randomized phase 3 IMbrave150 trial in 2020 showed that atezolizumab plus bevacizumab an anti-angiogenic drug considerably lowered the probability of mortality in patients with severe unresectable HCC and enhanced the rate of patient survival[35]. Lenvatinib, a tyrosine kinase inhibitor (TKI), was combined with pembrolizumab to provide an overall response rate of 46%. Patients with unresectable HCC who were enrolled in the study saw complete responses (CRs) and PR in proportions of 11% and 35%, respectively[36]. Similar to this, newer preclinical and clinical investigations have demonstrated that the administration of ICIs in combination with radiation, RFA, and transcatheter arterial chemoembolization (TACE) can enhance the effectiveness of anti-tumor immunotherapy[37,38]. In a phase, Ib/II clinical trial, camrelizumab and the chemotherapy FOLFOX4 are being used to treat advanced HCC[39].
The HIMALAYA phase 3 trial, which evaluated a single, high dose of tremelimumab, an anti-CTLA-4 antibody, added to durvalumab, an anti-PD-L1 antibody, or durvalumab alone in comparison to sorafenib as first-line treatment in 1171 patients with advanced HCC, has provided additional evidence that single-agent PD1/PD-L1 inhibition has antitumor activity (NCT03298451). Durvalumab monotherapy achieved the goal of overall survival without being inferior to sorafenib while being less toxic[40]. Regarding anti-CTLA-4 monotherapy, the research 22 revealed that tremelimumab monotherapy in patients previously treated with sorafenib after unacceptable toxicity or rejection of sorafenib had a manageable safety profile. However, the benefit-risk ratio was often better when tremelimumab and durvalumab were used together[41].
Figure 3 depicts several ICIs in HCC. Table 1 presents a summary of the clinical trials including ICIs treatment for HCC conducted during the previous 3 years.
| Treatment | Patients, n | ORR% | OS in mo | Ref. |
| Atezolizumab | 59 | 17 (5) | NA | [44] |
| Nivolumab | 371 | 15(4) | 16.4 | [21] |
| Camrelizumab | 217 | 15 (0) | 13.8 | [165] |
| Pembrolizumab | 278 | 18 (2) | 13.9 | [36] |
| Durvalumab | 104 | 11 (0) | 13.6 | [46] |
| Tremelimumab | 69 | 7 (0) | 15.1 | [46] |
| Durvalumab and tremelimumab | 159 | 9.5-24.0 (1-2) | 11.3-18.7 | [46] |
| Pembrolizumab and levantinib | 100 | 36 (1) | 22 | [20] |
| Nivolumab and ipilimumab | 148 | 31-32 (0-8) | 12.5-22.8 | [42] |
| Atezolizumab and bevacizumab | 336 | 27 (6) | NE | [20] |
| Nivolumab and cabozantinib | 36 | 14 (3) | 21.5 | [42] |
| Nivolumab, ipilimumab and cabozantinib | 35 | 31 (6) | NE | [42] |
Combining PD-1 and CTLA-4 inhibitors: The concept of combining inhibitors of several immune checkpoints, including as PD-1 and CTLA-4, is now being investigated in advanced HCC. Dual treatments combining PD-1 and CTLA-4 inhibitors have been studied in other cancer types, such as melanoma. The CheckMate 040 trial, which evaluated nivolumab and ipilimumab, an anti-CTLA-4 antibody, in 148 patients with advanced HCC who had progressed on sorafenib, provided the first clinical data[42]. Nivolumab and ipilimumab were administered to patients in three separate arms (Arm A, Arm B, and Arm C) at various doses and frequencies. The trial reported a 49% disease control rate, a 31% overall response rate, and a 17-mo median duration of response. The longest overall survival was 23 mo for patients in arm A. The patient side-effect profile was deemed acceptable. To treat side effects, more than 50% of patients required systemic steroids. Overall, the trial’s findings were positive, and the FDA eventually approved the use of nivolumab and ipilimumab together. Additionally, the combination is presently being evaluated in the CheckMate 9DW phase 3 study as a first-line treatment for advanced HCC in comparison to sorafenib or lenvatinib (NCT04039607). Similar to this, durvalumab and tremelimumab together exhibited strong action in unresectable HCC, with a response rate overall of 17.5%[43].
ICIs with anti-vascular endothelial growth factor antibodies: The combination of a PD1/PD-L1 inhibitor with a vascular endothelial growth factor (VEGF) inhibitor has been established as a novel paradigm for the treatment of advanced HCC in light of the encouraging results of the IMbrave150 phase 3 trial[20]. Atezolizumab plus bevacizumab had initially shown good safety and promising anticancer activity in patients with untreated advanced HCC in a phase 1b study[44]. The next phase of the IMbrave150 trial compared sorafenib and atezolizumab in patients with advanced HCC who had never received systemic therapy and were randomly assigned (2:1) to either study arm[20]. Compared to sorafenib, the combination of atezolizumab plus bevacizumab therapy lowered the death risk by 42%. The IMbrave150 trial, which is significant, excluded patients with problems related to portal hypertension, such as severe ascites and esophageal or gastric varices at a high risk of bleeding. This atezolizumab and bevacizumab combination, which is the current standard therapy that has replaced the TKIs sorafenib and lenvatinib, were approved as a first-line treatment for unresectable HCC in the United States and Europe as a result of the IMbrave150 trial. Inhibiting PD-L1, which activates the immune system (especially T-effector cells), and inhibiting VEGF, which lessens VEGF-mediated immunosuppression and encourages T-cell infiltration in the tumor microenvironment, are probable synergistic anticancer agents that account for its effectiveness[45].
Dual therapies combining immune checkpoint with multi-kinase inhibitors: An alternative to antibody-mediated VEGF suppression may be achieved by combining ICIs with TKIs instead of anti-VEGF antibodies. The multicohort COSMIC-021 phase 1b trial is evaluating the combination of cabozantinib and atezolizumab in advanced solid tumors, including HCC (NCT03170960). Additionally, it is being evaluated in the COSMIC-312 phase 3 trial (NCT03755791) as a first-line treatment for patients with advanced HCC in comparison to sorafenib[46]. As a secondary outcome metric, cabozantinib/monotherapy is also contrasted with sorafenib in this study. A predetermined interim analysis for overall survival, however, failed to achieve statistical significance. Early 2022 is when its final analysis should produce results[47]. In 104 patients with unresectable HCC who had not previously undergone systemic treatment, the combination of lenvatinib and pembrolizumab showed reasonable results in a phase 1b trial[36]. This combination is currently being compared to lenvatinib monotherapy in the LEAP002 phase 3 trial (NCT03713593)[48]. Finally, the combination of apatinib and camrelizumab, an anti-PD-1 antibody is under clinical development. An overall response rate of 50% was found in a phase 1 study of individuals with advanced HCC[49]. Additionally, a phase 3 trial is currently comparing the combination to sorafenib in the first-line setting for patients with advanced HCC (NCT03764293).
Bispecific antibody (BsAbs), in contrast to monoclonal antibodies, are made primarily using recombinant DNA technology and may concurrently and precisely bind two antigens or epitopes[50]. BsAb can target immunological checkpoints and tumor-associated antigens (TAAs) to alter immunosuppression in the tumor environment. It can also directly increase the action of immune cells against tumors. As a result, they outperform monoclonal antibodies in aspects of synergistic effects and can mediate a wide range of particular biological effects. Most of the time, BsAbs bridge the gap between immune cells and tumor cells to attract and activate them to attack tumor cells[51]. An EpCAM/CD3 bispecific antibody called Solitomab (AMG110, MT110) is humanized. Bispecific T-cell Engager (BITE), which can lyse HCC cell lines almost completely in vitro when it binds to gd T cells, is created by joining the anti-EpCAM single-chain variable fragment (scFv) to the anti-CD3 scFv via a Gly4Ser linker[52]. To remove glypican-3 (GPC3) + HCC cells, a different BsAb called GPC3/CD3 BITE is expected to entice CTL. In one work, an IgG-shaped TriFab, that can be employed to activate two antigens sequentially or for targeted delivery of tiny and large payloads, was created by joining two anti-GPC3 Fab fragments to one asymmetric third Fab-sized binding module using flexible linker peptides[53].
Adoptive cell transfer (ACT), an immunotherapy that harnesses the patient’s immune cells or those of a healthier donor to combat cancer, has currently emerged as a crucial component of cancer treatment[54]. ACT could be stimulated and replicated in vivo and has a long-lasting anti-tumor impact, in contrast to antibodies or other targeted medications. As a result, the ACT is also known as a “living” therapeutic strategy[55]. Since the majority of ACT’s effector cells come from the patient, it is regarded as a highly personalized cancer therapy. ACT is more targeted than chemotherapy because enlarged or genetically altered effector cells can identify and target tumor antigens[56]. Adoptive cell transfer, as opposed to checkpoint inhibition therapy, which passively administers autologous lymphocytes after ex vivo cultivation, aims to improve the outcomes for patients with HCC[57]. Table 2 lists the ACT clinical studies for the HCC treatment that were published at clinicaltrials.gov in the previous 3 years.
| Vaccine type | Advantages | Disadvantages |
| Peptides | Easy to prepare; known target Ag | Adjuvants are needed; restricted Ag repertoire; restriction to human leukocyte Ag |
| Dendritic cells | Adjuvants are not needed | Individualized production |
| Peptide pulsed | Known target Ag | Restriction to human leukocyte Ag; restricted Ag repertoire |
| Protein pulsed | No restriction to human leukocyte Ag; known target Ag | Protein synthesis is more interesting; restricted Ag repertoire |
| Tumor lysate pulsed | Not human leukocyte Ag restricted full Ag repertoire; available | Tumor samples not always available; the predominance of self-Ags that may eclipse tumor Ags |
| Cell line pulsed | Not human leukocyte Ag restricted; unlimited Ag source | Responses against cell line-specific Ag |
Cytokine-induced killer cell: IL-2, interferon-alpha (IFN)-α, and anti-CD3 monoclonal antibodies are used to create cytokine-induced killer cell (CIK) cells, a heterogeneous population of immune cells, from human peripheral blood mononuclear cells (PBMC) in a laboratory setting[58]. NK cells, NKT cells, and CTLs make up the majority of CIK cells (CTLs). Through adhesion molecules, CIK can lyse tumor cells and recognize them without the assistance of the major histocompatibility complex (MHC). Shi et al[59] showed that autologous CIK cells can effectively enhance the immunological condition of HCC patients by using them to treat primary HCC in a phase I clinical study and finding that the signs and features of HCC patients were diminished without notable adverse effects. Clinical studies have also demonstrated that CIK cell treatment could be utilized to cure individuals having primary HCC that is inoperable as well as HCC patients who have had their tumors removed. Takayama et al[60] published the results of a 150-patient clinical trial of CIK therapy for postoperative HCC. They discovered no significant treatment adverse effects and an 18% lesser recurrence rate in the treatment group than in the control group, indicating that CIK cells treatment can lower reappearance rates and lengthen recurrence-free survival in patients with postoperative HCC[61]. Additionally, conventional therapies and CIK cell therapy have frequently been combined by researchers. As opposed to TACE alone, TACE combined with CIK cells may increase progression-free survival in HCC patients. T and NKT cells dramatically increased with the addition of CIK cells to local radio frequency hyperthermia, whereas alpha-fetoprotein (AFP) levels decreased, according to research by Wang et al[61]. Although 17% of patients reported experiencing pyrexia, chills, myalgia, and fatigue, these symptoms were not severe enough to require therapy to be stopped[62]. These results suggest that the combination of CIK cells having TACE or RF hyperthermia is a harmless and efficient therapy for HCC patients.
Tumor-infiltrating lymphocytes: TIL is a part of the host immune response against tumors, which also consists of Tregs, T cells, NK cells, and B cells[63]. TIL is 50-100 times more effective as compared to lymphokine-activated killer cells at curing mice with severe metastatic cancer, according to experiments[64]. A phase I clinical trial in individuals with primary HCC established the viability of TIL treatment[65]. Because TILs are derived from surgical tumor tissues and can detect several antigens, they have a stronger tumor-inhibitory effect than medications that target certain antigens or mutations. TILs in HCC are uncommon, however, prior research has shown that despite this, they can significantly affect tumor recurrence and patient prognosis[66]. Clinical research with 150 HCC patients demonstrated that adoptive TIL treatment improved recurrence-free survival following liver resection[60]. Patients who received surgical resection of their HCC and had considerable lymphocyte infiltration had a lower recurrence rate and a greater survival rate than those who did not have significant lymphocyte infiltration[67]. However, isolating TILs from HCC tumor tissues and expanding them in vitro is difficult. Additionally, only a small number of HCC patients could survive lymphocyte deletion, which is necessary before TIL infusion[68].
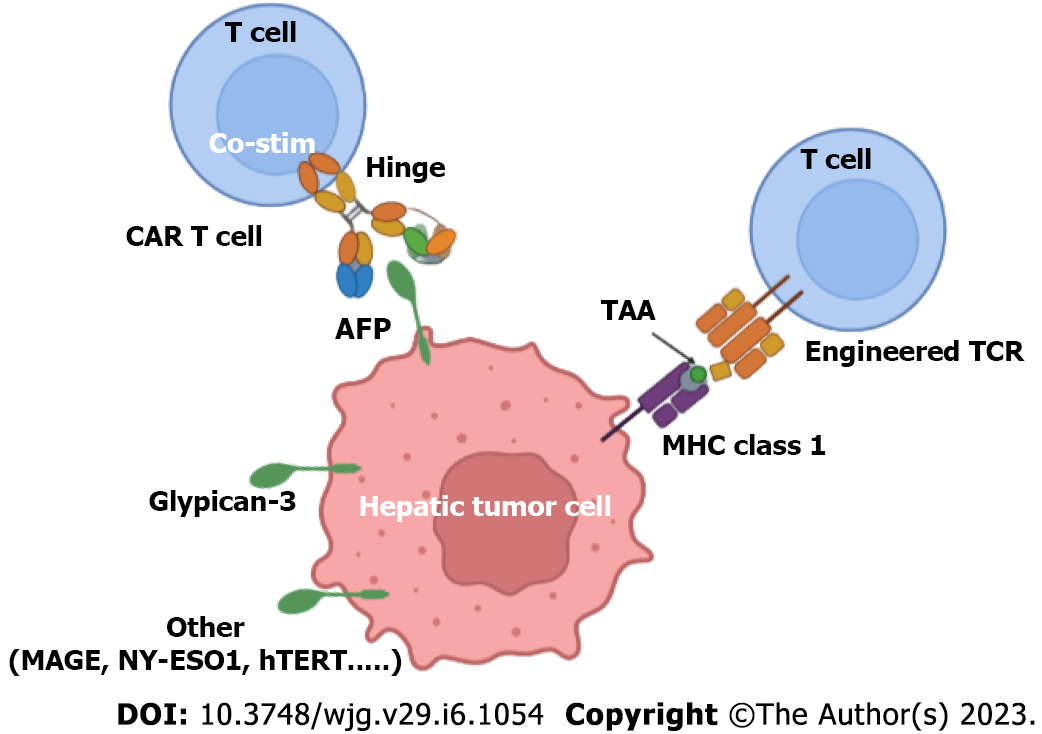
Chimeric antigen receptor T Cell: ACT research is now focused on Chimeric antigen receptor T Cell (CAR-T) treatment, novel immunotherapy for cancer wherein T cells are genetically altered to recognize particular TAA[69]. Hematological cancers can be successfully treated with CAR-T cell therapy. The FDA has approved CAR-T cells that target CD19 and B-cell maturation antigen (BCMA) for the management of acute B-cell lymphocytic leukemia, several lymphomas, and multiple myeloma[70]. CAR-T therapy for liver malignancy is currently being developed because of the variety of solid tumors, the absence of specific targets, and the liability to the tumor microenvironment[71]. Conventional T cells have a T cell receptor (TCR) structure that is reliant on MHC antigen presentation. The CAR structure is independent of MHC antigen presentation, evades MHC molecule restriction, and resolves the issue of tumor immune escape caused by MHC downregulation[72] (Figure 4). To date, an increasing series of clinical trials have been carried out to show the effectiveness of CAR-T cell treatment in solid tumors. GPC3, a 580 amino acid long heparan sulphate proteoglycan, is overexpressed in HCC yet not at all in healthy tissues[73,74]. Gao et al[75] created CAR-T cells targeting GPC3 for the first time and showed that GPC3 CAR-T cells can successfully eradicate the proliferation of HCC cells both in vitro and in vivo. In a recent study, researchers found that by dividing the CAR design into two parts, HCC tumors may be removed with a lower level of proinflammatory cytokines (split GPC-3 CAR-T cells)[76]. A different study used patient-derived xenograft (PDX) HCC models and showed that GPC3 CAR-T cells reduced tumor development, however to differing degrees because of variations in PDL1 expression on cancer cells[77]. This demonstrates that combining CAR-T treatment and ICIs is a workable way to increase the efficiency of curing PD-L1- +ve HCC. The secreted glycoprotein known as AFP is extensively expressed in fetuses but only modestly so in adults. However, AFP is once again expressed when HCC manifests in adults[78]. Traditional CAR-T cells are only able to identify tumor surface antigens; they are unable to identify intracellular antigens. Liu et al[79] developed some distinctive CAR-T cells that could bind to the AFP158-166 peptide-MHC complex and then damage HLA-A*02:01+/AFP+ tumor cells because all intracellular antigens are delivered by MHC class I molecules. A phase I clinical trial (NCT03349255) assessing the security and performance of CAR-T cells in patients with AFP-expressing HCC was successfully finished in the interim. As a result, using CAR-T cells to target intracellular antigens is an effective way to treat HCC. The c-Met tyrosine kinase receptor could promote hepatocyte survival, regeneration, and proliferation[80].
HCC development and progression can be aided by c-Met overexpression. As a result, c-Met is being evaluated as a possible target for the therapy of HCC. Jiang et al[81] developed CAR-T cells that simultaneously targeted c-Met and PD-L1, and they discovered that these cells significantly cytotoxic attacked c-Met+ PD-L1+ HCC cells. NKG2DL ligands (NK group 2 member D ligands) are present in a variety of primary malignancies, along with HCC, yet not found in healthy tissues[82]. Therefore, NKG2DL might be a good candidate for HCC immunotherapy. Innovative NKG2D-CAR-T cells that specifically target NKG2DL expressed on HCC cells were developed by Sun et al[83]. They also discovered that NKG2D-CART cells only targeted ruptured HCC cells with elevated NKG2DL expression and had no effect on the NKG2DL negative cell line. The xenograft model further demonstrated that NKG2D-CAR-T cells may prominently limit in vivo tumor growth. Type I transmembrane glycoprotein CD147 was discovered in high levels in HCC and various solid tumors[84]. When Tet-On inducible CD147-CART cells were administered Dox, Zhang et al[85] found that Tet-On inducible CD147-CART cells can successfully rupture numerous HCC cell lines in vitro and reduce the development of cancer cells in the HCC xenograft model. The safety of hepatic artery infusions (HAI) of CD147-CART cells for severe HCC was recently evaluated in a phase I trial (NCT03993743). Mucin 1[86], EpCAM[87], and CD133 are further potential targets antigens for HCC CAR-T treatment[88,89]. The majority of the above-stated targets, though, are TAAs, which are expressed at low levels in both cancerous and healthy cells, leading to both on- and off-target toxicities in normal tissue. The most significant objective for future researchers will be to identify new targeted antigens and improve the effectiveness and safety of CAR-T treatment for HCC.
Chimeric antigen receptor NK cells: The distribution of NK cells in the liver is substantially greater as compared to the peripheral blood and spleen. As a result, NK cells are thought to be important in the prevention of HCC and are assumed to be a promising source for cell therapy in the treatment of HCC[90]. The technique utilized to produce CAR-T cells could likewise be employed to generate CAR-NK cells from NK cells. Furthermore, because CAR-NK cells have a shorter lifespan as compared to CAR-T cells, they can lower the danger of autoimmune response and tumor transformation[91]. CAR-NK cells could also be generated from various resources, such as the peripheral blood mononuclear cells (PBMC), NK92 cell line, umbilical cord blood (UCB), and induced pluripotent stem cells (IPSC). Since CAR-NK cells could be delivered “off-the-shelf”, abolishing the requirement for customized and patient-specific products, so is the case with CAR-T therapies currently, the danger of syngeneic xenograft responses and graft-versus-host (GVHD) sickness is reduced[92]. The therapeutic potential of GPC3-specific CAR-NK cells for HCC was investigated by Yu et al[93] in 2018. In vitro co-culture experiments with GPC3+ HCC cells revealed considerable cytotoxicity and cytokine generation by GPC3-specific CAR-NK cells. Additionally, cytotoxicity was unaffected by soluble GPC3 and TGF-b, and hypoxic (1%) conditions did not significantly alter anti-tumor efficacy. In a different study, Tseng et al[94] developed CD147-specific CAR-T and CAR-NK cells to treat HCC using CD147 as the target antigen. The results indicated that numerous malignant HCC cell lines in vitro, as well as HCC tumors in xenograft and PDX animal models, could be successfully eliminated by CD147-specific CAR-NK cells. In a human CD147 transgenic mouse model, GPC3-synNotch-inducible CD147-specific CAR-NK cells preferentially destroy GPC3+CD147+ however not GPC3-CD147+ HCC cells and don’t induce substantial on-target/off-tumor damage. The lack of effective gene transfer techniques in primary NK cells is one of the fundamental obstacles to CAR-NK immunotherapy. Numerous current investigations have shown that retroviral vectors may successfully transduce larger NK cells with efficiency ranging around 27% to 52% after just one round of transduction[95]. The insertional mutations linked to retroviral transduction and the detrimental actions on primary NK cell survival, however, are the most significant drawbacks of this strategy in a clinical setting.
TCR-engineered T Cell: TCR-Engineered T Cell (TCR-T) cells are created by altering T cells with the exogenous TCRs gene to precisely identify tumor antigen peptides-MHC complexes[96]. All tumor-derived proteins could indeed be broken down via proteasomes and displayed by MHC, allowing TCR-T cells to target both tumor surface and intracellular antigens. TCR-T therapy should therefore be more widely applicable compared to CAR-T therapy. HCV infection affects 130-150 million people worldwide and could result in conditions like HCC[97]. Spear et al[98] engineered T cells with a high affinity, HLA-A2-restricted, HCV NS3:1406-1415-reactive TCR to create HCV-specific TCR-T cells. The findings demonstrated that HCV-specific TCR-T cells may cause a relapse of established HCV+ HCC in vivo, indicating that HCV-specific TCR-T therapy might be an efficient technique for curing HCV-associated HCC. A lesser proportion of HCC tissues produced from HBV infection detain HBV gene expression, which may become TCR-T targets. In 2011, Gehring et al[99] identified TCR-T cells specific for the HBV surface antigen in PBMC of patients with chronic HBV and HBV-related HCC. These HBV-specific TCR-T cells may recognize HCC tumor cells and have a variety of uses.
Additionally, a phase I clinical experiment was carried out to assess the safety and efficiency of
Despite being produced in humans, the melanoma-associated antigen (MAGE)-A3/HLA-A1TCR induced severe cardiac damage via targeting the cardiac muscle protein titin[106]. However, while NY-ESO-1 TCRT has demonstrated clinical anti-tumor efficacy, the majority of similar TCRTs haven’t been confirmed to be useful for patients. Various aspects could be addressed to increase the anti-tumor efficacy of TCR-T therapy, such as extending TCR-T in vivo survival, enhancing tumor infiltration, and preventing T cell depletion.
Key elements of the immune system, cytokines are crucial in the immunological response to cancer. Recently, there has been a lot of interest in using cytokines to treat cancer as the immune system is competent in identifying and eliminating cancer cells[107]. In 1986, the United States FDA approved the use of IFN-α as the first cytokine for the treatment of hairy cell leukemia (HCL)[108]. In 1992, the use of high-dose IL-2 as a therapy for metastatic renal cell carcinoma (mRCC) and metastatic melanoma was approved (MM). Besides its original approval, IFN-α has been used to treat a variety of cancers, including mRCC, melanoma, follicular lymphoma when combined with bevacizumab, and Kaposi’s sarcoma linked to the AIDS virus. Numerous factors can be used to categorize advanced diseases in HCC. The major liver disease societies approve the BCLC staging, which has been well verified[109]. In the BCLC staging system, level C is the advanced stage, and stage D is the final stage[110]. Multiple cytokines and stimulatory substances have been linked to the likelihood of progressive disease in HCC patients.
Interleukin-10: IL-10 is a highly effective anti-inflammatory cytokine[111]. The majority of activated immune cells, along with macrophages and monocytes, secrete IL-10, which reduces the secretion of inflammatory mediators, prevents the formation of antigens, and controls several other immunological properties[112]. While its significance in viral infections is widely known, its function in HCC is less clear. Interpreting IL-10 data for HCC is complicated by the finding that HCC patients have greater levels of IL-10 than cirrhotic patients and healthy controls, although not in viral hepatitis patients[113]. In one investigation, it was discovered that patients with IL-10 levels of more than 12 pg/mL had inferior post-operative results. It has also been investigated how IL-10 affects HCC which is incurable. IL-10 levels in serum were revealed to be a poor prognostic predictor in a prospective analysis of 74 patients with unresectable HCC, with a considerably poorer median survival (3 mo vs 12 mo; P = 0.02)[114]. Patients with elevated IL-10 levels in serum performed markedly worse than patients with decreased IL-10 levels in a larger trial of 222 patients with unresectable HCC (mainly related to HBV) [hazard ratio (HR) 2.2][114]. Elevated IL-10 levels dramatically decreased overall survival in patients with advanced disease (BCLC stage C) from 10.2 mo to 3.5 mo, compared to those with low IL-10 levels, who exhibited average mortality of 10.2 mo[115].
Interleukin-37β: The wideset of the 5 distinct isoforms of IL-37β (named IL-37a-e) is IL-37β[116]. This cytokine, which is generated by epithelial cells, macrophages, and monocytes inhibits the production of pro-inflammatory cytokines as well as EMT by activating the STAT3/IL-6 pathway[117]. Additionally, recombinant IL-37β studies in vivo on mice showed that the tumor volume was lowered compared to the untreated controls[118]. IL-37 β serum levels were found to be negatively correlated with the survival of advanced HCC in a study of HBV-related HCC patients. Higher levels of IL-37β in the subjects’ bodies led to prolonged overall survival and disease-free survival[119]. Similarly, in a cohort with a high percentage of HBV-HCC, higher IL-37β expression in HCC tissues was linked with better DFS and survival[118]. These HCC findings, along with decreased IL-37β expression and production in metastatic tumors, suggest that IL-37β is implicated in signaling pathways that control metastasis and may have an impact on histopathologic prognosis[119].
CC Chemokine Ligand 20: CC Chemokine Ligand 20 (CCL20) (also known as macrophage inflammatory protein-3 alpha) links with CC chemokine receptor 6 (CCR6), causing immune cells to be chemoattracted to the zone of inflammation. CCL20 have been demonstrated to play several functions in rheumatoid arthritis, general inflammation, and various cancers[120]. In vitro and in vivo studies have revealed a function for the CCL20-CCR6 axis in HCC generation, development, and invasion[121]. Furthermore, in an investigation of 33 specimens from 22 patients, CCL20 overexpression was detected in tumors, indicating a function in hepatocarcinogenesis[122]. A role in tumor invasion, angiogenesis, and the development of hepatic malignancies has been suggested by several studies that have detected significant amounts of CCL20 and its receptor CCR6 in HCC and colorectal cancer liver metastases. The relationship between CCL20 expression and tumor grading, however, was only identified in one small study including 11 HCC patients (TNM stage 3 vs 2)[123]. Tumor-infiltrating regulatory T cells may be preferentially attracted to the tumor via the CCR6-CCL20 axis, according to an investigation of 293 HCC patients. This study found a favorable correlation between the number of regulatory T cells infiltrating the tumor and CCL20 expression in the tumor. Significantly, patients with HCC who had larger levels of tumor-infiltrating regulatory T cells had a worse prognosis[124].
IL-6: The predictive importance of pre-treatment blood IL-6 levels in the condition of advanced HCC was examined in research on 128 sorafenib-treated HCC patients divided into a finding and validating cohort. In both groups, a high level of serum IL-6 before therapy was a reliable indicator of poor overall survival. The time to progression and progression-free survival were comparable independent of pretreatment IL-6 levels, hence there was no association with sorafenib efficacy. Furthermore, pretreatment IL-6 levels were not associated with macrovascular invasion or extrahepatic dissemination[125]. Although promising, further research which is presently being undertaken, is required to establish the function of IL-6 in HCC therapeutic response. Interestingly, recent research in cellular models has shown that blocking IL-6-related pathways reduces sorafenib resistance[126].
Angiopoietin-2: A major regulator of vascular development, angiopoietin-2 (ANG-2) is nearly entirely generated by epithelial cells and supports the actions of other endothelial-acting cytokines[127]. Superior pretreatment in the SHARP research, the first randomized placebo-controlled experiment to assess the effect of sorafenib in advanced HCC as well as the prognostic significance of multiple cytokines, ANG-2 levels were associated with shorter overall survival in the overall cohort as well as in the sorafenib arm. However, no link was discovered between sorafenib-associated survival and therapy interaction analyses. Nonetheless, those with higher plasma ANG-2 levels at week 12 had a smaller total survival and time to progression than those who did not have an increase in plasma levels[128]. A year after, the Okayama Liver Group (Japan) then performed a longitudinal analysis and retrospective investigation of serum cytokines in 2 independent sorafenib-treated advanced HCC cohorts. Increased pretreatment ANG-2 levels, as in the SHARP research, were linked to a worse overall survival rate[129]. Furthermore, when the researchers assessed ANG-2 in a prospective cohort, the difference was not statistically significant, most likely because there were fewer patients, even though patients with progressive disease had higher ANG-2 levels at the beginning of treatment than those having the non-progressive disease. ANG-2 levels, on the other hand, increased only in patients with worsening disease over time[129].
Hepatocyte growth factor: In vitro and animal models have revealed that hepatocyte growth factor (HGF) could either promote or prevent the development of HCC[130]. In both the sorafenib arm and the overall cohort of the SHARP trial, increased pretreatment plasma HGF levels were a significant independent predictor of worse overall survival. Surprisingly, sorafenib was linked with a greater benefit in terms of total survival and time to progression in patients with reduced HGF amount at the start of therapy. Additionally, in the therapy arm, a reduction in median HGF plasma levels at 12 wk was not associated with overall survival but was associated with a lengthier duration of progression[128]. In a prospective cohort, the Okayama Liver Group discovered pretreatment serum HGF levels to be a potential independent marker of overall survival, albeit significance was lost following multivariate analysis. Additionally, only in the retrospective cohort, HGF pretreatment levels were higher in patients with the progressive disease compared to non-progressive disease[131].
VEGF: Multityrosine kinase inhibitors, such as Sorafenib, target VEGF signaling as a major cytokine causing angiogenesis. The SHARP study looked at VEGF as a predictive marker in addition to ANG-2 and HGF. Similar to ANG-2, higher pretreatment VEGF amounts were linked to reducing survival. Nevertheless, the Sorafenib arm did not convert its predictive value. Interesting, the Sorafenib group’s average plasma VEGF levels were significantly greater than those of the placebo group[128]. Furthermore, VEGF levels were shown to be higher in individuals than those later experienced disease advancement compared to non-disease progression in a retrospective study on HCC patients administered with sorafenib by the Okayama Liver group. Furthermore, higher baseline VEGF levels were linked to shorter overall survival and progression-free survival, which is consistent with the results of the SHARP trial. Nevertheless, the multivariate analysis failed to identify VEGF as a predictor of total survival[131]. Later, the same study team verified this finding in a prospective cohort of HCC patients receiving sorafenib therapy[129]. A decrease in plasma VEGF levels at 8 wk from baseline was shown by Tsuchiya et al[132] to be an independent predictive factor linked with 1-year survival following Sorafenib therapy in a small cohort of HCC patients.
Tumor vaccines are substances that boost particular immune reactions to tumor antigens. For patients whose tumors don’t have a lymphocytic infiltration that can be treated with ICI, immune-enhancing techniques may be helpful. One of the earliest immunotherapeutic methods applied in HCC among these methods is vaccination. In comparison to studies looking at adoptive cellular therapies and checkpoint inhibitors, clinical trials for such tumor vaccines in HCC are presently being conducted far less frequently. This is partly due to earlier disappointing trial results as well as the relative ineffectiveness of other tumor vaccines. This could be because it was formerly challenging to identify the proper tumor antigens, but that is now possible because of recent technology advancements permitting huge parallel DNA sequencing. Therefore, inducing an immune response remains a promising treatment strategy for HCC, either by itself or more likely in combination including an immune modulator. To date, several agents have been looked at in this area.
The high recurrence rate cannot be avoided by current treatments for advanced-stage HCC due to their insufficient efficacy. Vaccines have already been suggested as potential solutions to this problem, able to enhance clinical results when used in conjunction with existing recognized systemic treatments. Though they are harmless and have immunologic effects, the few trials that have been undertaken so far have only shown disappointing/poor clinical results/efficacy[133]. The majority of them are quite old, and they are all phase I or II trials (Table 1). Peptide-based or DC-based vaccines are two categories of HCC vaccination methods now in use (Table 1). Additionally, this could be further divided into peptide-loaded and tumor lysate-pulsed DCs. Epitopes from the oncofetal antigens AFP[134,135], glypican 3 (GPC-3)[136], and the hTERT peptide GV1001 are the principal antigens used for peptide-based vaccinations in HCC[137]. Additionally, peptides from AFP and AFP coupled with MAGE-1 and GPC3 have been tested in clinical trials utilizing DCs loaded with peptides[138]. HepG2 (a hepatoma cell line) and autologous tumor lysates have both been employed in clinical trials[138,139]. All of these vaccination methods are risk-free, and even though clinical outcomes were subpar, the majority of them produced antigen-specific immune reactions without inducing toxic or autoimmune reactions. The various characteristics of HCC tumors and the vaccine’s design, or even the combination of the two, may be to blame for this poor performance.
TAA-based vaccines are prone to tolerance mechanisms because they are not entirely tumor specific, which is reflected in the dearth of highly reactive clones against them[140]. As a result, responses are typically insufficient to stop tumor development. Additionally, as previously mentioned, the immun
| Vaccine | Patient inclusion criteria | Patients, n | Immune response, % | Observations | Ref. |
| AFP HLA-A*02 restricted peptides + IFA | AFP + tumors from (stage IV patients) | 6 | 66 | Increased CTL response | [134] |
| DCs pulsed with autologous tumor lysate | Unresectable HCC | 8 | 62 | Immune response generation | [152] |
| DCs pulsed with autologous tumor lysate | Advanced HCC | 31 | 0 | Improved survival | [138] |
| DCs pulsed with AFP HLA-A*02 restricted peptides | Stage IV patients with surgery chemotherapy | 10 | 60 | No clinical responses | [135] |
| DCs pulsed with hepatoma cell-line (HEP-G2) lysate | No other therapeutic option | 35 | 11.4 | Evidence of antitumor efficacy | [139] |
| Gv1001 peptide + GM-CSF + cyclophosphamide | Advanced-stage HCC with no previous antitumor treatment | 37 | 0 | The immunological response is not detected | [137] |
| GPC3 HLA-A*24:02 and HLA-A*02-restricted peptides + IFA | Metastatic HCC or advanced HCC | 33 | 91 | Antitumor efficacy | [148] |
| DCs pulsed with fused recombinant proteins (AFP, MAGE-1 and GPC-3) | Surgical resection and locoregional therapy | 12 | 92 | Improved survival | [65] |
| GPC3 HLA-A*24:02 and HLA-A*02-restricted peptides + IFA | Vaccines as adjuvant therapy | 41 | 85 | Improved recurrence rate | [136] |
| AFP HLA-A*24:02 restricted peptides + IFA | Stage B/C tumors | 15 | 33 | Increased CTL response | [154] |
DCs are expert antigen-presenting cells with a wide range of responsibilities, including the processing, presentation, and absorption of TAAs. Allogeneic DCs make up a significant portion of vaccines because they provide the antigen as well as the secondary co-stimulation required to effectively elicit a T cell activation. DCs from peripheral blood are isolated, grown ex vivo, and activated with cytokines like granulocyte-macrophage colony-stimulating factor (GM-CSF) to produce primed DCs for reinfusion. Another appealing, targeted strategy involves injecting such cells to cause the activation of effector cells, trigger a cascade of tumor rupture, and cause more TAA secretion[146]. To boost the effectiveness of the vaccine and optimize this TAA priming, a variety of approaches may be used. DCs might be cultured with tumor lysate or the fusion of DCs and tumor cells, or they may be transduced with DNA or RNA encoding recognized TAAs[141]. Ilixadencel (pro-inflammatory allogeneic DCs activated by GM-CSF and IL-4) was injected intratumorally in a newly published phase I trial, where 17 patients received it either alone or in conjunction with sorafenib. Tolerability evaluation was the main goal. There was just one grade 3 adverse event noted. Enhanced tumor-specific CD8+ T cells were seen in the peripheral blood of 73% of the 15 evaluable patients, indicating at least a successful immune-provoked response[147].
An alternate choice for eliciting a powerful immune response is peptide vaccinations. However, despite immunological surrogates, like the generation of GPC-3 reactive cytotoxic T cells in one phase I trial, being successful, this has not led to clinical results[148]. GPC-3 and MRP3 have shown any efficacy in inducing a T cell response rate over 70%, while other TAAs such as SSX-2, NY-ESO-1, hTERT, and MAGE-A all induce considerably lower rates. This is despite a plethora of TAAs being found in HCC trials using AFP[149].
A more recent development in the arena of tumor vaccines is the use of oncolytic viruses. These therapeutically useful viruses are targeted to preferentially replicate in cancer cells. To date, they have been predominantly introduced by intra-tumoral injection. The modified poxvirus JX-594 remains the lead oncolytic virus of interest in clinical trials about HCC. As an immunotherapeutic agent, it piqued considerable interest when it conferred a dose-related survival benefit (median of 14.1 mo compared to 6.7 mo) in a phase II dose-finding trial of 30 patients[150,151]. The global, randomized, open-label, phase III study of Pexa-Vec (JX-594; an oncolytic vaccinia virus which selectively targets cancer cells) is currently recruiting patients with advanced HCC to two arms of vaccination with sorafenib vs sorafenib alone[152]. We excitedly await the results of this, particularly as a combination therapy.
Immune-related adverse events: Immune checkpoint molecules serve an important function in immune homeostasis. Inhibitory immune checkpoint molecules, like PD-1 and CTL-4, are particularly important for balancing activation of T-cell and self-tolerance[153-155]. ICIs targeting PD-1 or CTL-4 may thereby produce a range of immune-related adverse events (IrAEs) by increasing self-immunity. IrAEs can affect every organ system and can range from a minor rash to life-threatening consequences. IrAEs caused by PD-1/PD-L1 inhibition are dose-independent[156]. Unlike anti-PD-1/PD-L1 agents, the risk of antiCTL-4-related adverse events is dose-dependent[157]. The gastrointestinal tract and skin were the most often affected organ systems by both anti-CTLA-4 and PD-1/PD-L1 inhibitors, whereas the endocrine systems and liver were less frequently affected[156,157]. In meta-analysis of phase 2/3 trials patients treated with ICIs, found that a rash was the most prevalent all-grade IrAE, with colitis and an increase in aspartate aminotransferase level being the most common high-grade IrAEs. Ipilimumab was related with a significantly greater incidence of rash and colitis when compared to anti-PD-1/PD-L1 drugs[158].
Management of IrAEs: Because IrAEs are linked with a wide range of aggravating factors in the context of HCC, hepatologists face significant hurdles in detecting and managing them. First, liver cirrhosis causes progressive immunological dysfunction, including immune deficiency as well as systemic inflammation[159]. Thus, in these patients, the liver-related immune homeostasis is already significantly disrupted. Second, cirrhosis-related hepatic and extrahepatic problems may overlap with or intensify symptoms caused by IrAEs, hampered early and rapid detection, which is compulsory concerning the consequence of potentially life-threatening episodes. Thus, before starting ICI therapy, individuals with HCC should be carefully selected and evaluated. In general, IrAE management is built on three pillars. First, close monitoring is required, including weekly clinical controls and, depending on the severity of the incidents, hospitalization. Importantly, individuals with severe IrAEs should be referred to a specialized center as soon as possible. This is especially important in patients with liver cirrhosis because distinguishing between cirrhosis-associated complications and IrAEs can be difficult, and premature discontinuation of an effective antitumor therapy or starting of steroid therapy in cirrhotic patients can have serious consequences[160]. Second, depending on the type and severity of IrAEs, ICI therapy may need to be either interrupted or permanently discontinued. Apart from PD-1/PD-L1-driven rash, adrenal insufficiency, nephritis and hypothyroidism, which recover after 1 mo of cessation, permanent termination of ICI therapy should be considered for higher grade IrAEs[160]. Re-exposure to ICI therapy after withdrawal, on the other hand, is associated with a significant risk of IrAE recurrence[161]. Third, for IrAEs of greater than grade 2, glucocorticoids (0.5 to 2 mg/kg/d prednisone oral or intravenous depending on the type and severity of IrAEs) may be needed. Cutaneous IrAEs are treated with topical, oral, or intravenous glucocorticoids and topical or oral antihistamines, depending on the severity of clinical presentation. Cutaneous IrAEs range from commonly observed rash or pruritus to very less common but more severe disorders such as Stevens-Johnson syndrome[160]. Steroids should be continued for at least 3 d and then tapered over a period of 1 wk to 4 wk[162,163].
Differential diagnosis is required for gastrointestinal IrAEs, notably colitis and/or diarrhea, in order to rule out infectious disorders and pharmacological side effects[160]. In the event of glucocorticoid failure, immunosuppressive medication (such as vedolizumab or infliximab) should be started as soon as possible[164]. The diagnosis and management of immune-related hepatitis in HCC patients receiving ICI therapy is particularly difficult[160]. As a result, seeking the advice of an experienced hepatologist as soon as possible is strongly advised. Intrahepatic tumor growth, hepatitis B virus and/or hepatitis C virus or newly acquired viral hepatitis, cytomegalovirus reactivation, hepatotoxic medication side effects, cholestasis, and ascites should all be ruled out before diagnosing immune-related hepatitis[160]. A liver biopsy should also be considered prior to steroid therapy. For severe cases of immune-related hepatitis, oral or intravenous steroids may be used[160]. After the toxicity has subsided, tapering should be done over a period of 4-6 wk[162,163].
Pneumonitis is a potentially life-threatening IrAE. As a result, the pneumonitis should be followed by a prompt and thorough differential diagnosis, including the elimination of viral etiologies, hepatopulmonary syndrome and porto-pulmonary hypertension[160]. Steroids should be started, and tapering should take 4-6 wk[163]. Following glucocorticoid failure, infliximab or mycophenolate mofetil may be administered[160]. Thyroid-related IrAEs include hypothyroidism and hyperthyroidism caused by thyroiditis. A progressive reduction in thyroid-stimulating hormone in conjunction with normal or decreasing thyroxine levels should trigger repeated cortisol assessments to rule out immune-related hypopituitarism. In the case of hypothyroidism, thyroxine substitution is only recommended in symptomatic patients[162]. Thyroid antibodies and uptake should be assessed in symptomatic hyperthyroid patients, and beta-blockers and/or carbimazole should be investigated. Asymptomatic patients do not require any special treatment, and ICI therapy should be continued. Patients on ICI therapy should have regular thyroid stimulating hormone and free thyroxine tests. If central hypothyroidism is suspected, each pituitary hormone axis should be examined[160]. Cortisol, corticotropin-releasing hormone, adrenocorticotropic hormone, luteinizing hormone, thyroid stimulating hormone, free thyroxine, follicle-stimulating hormone, estradiol (premenopausal women), testosterone (men), insulin-like growth factor 1, and electrolytes are examples of these hormones[162,163].
Finally, HCC is a multifaceted illness with multiple faces. It avoids early discovery, which provides the best chance of cure by resection/transplant, and systemic treatments are only of marginal efficacy at best, despite recent therapeutic advances. Current advances in immunotherapy and its combinations have altered the HCC treatment landscape and clinical studies are continuing to pave the path forward. Immunotherapy increases survival rates and provides long-term cancer control in subsets of HCC patients while also minimizing side effects. Further research into immunotherapy in combination with current treatments for HCC in the early and intermediate stages may assist a greater spectrum of patients. Continued research into PD-1/PD-L1, TMB, ctDNA, microsatellite stability, DNA mismatch repair, neutrophil/lymphocyte ratio, cytokines, and cellular peripheral immune response will hopefully identify the most reliable marker for selecting and sequencing systemic treatments to achieve the best outcome in HCC patients. Despite such significant treatment advances in HCC, numerous hurdles remain. The scientific community must figure out how to appropriately sequence these medicines for the best potential response, how to control toxicities, and how to develop indicators to monitor for response and relapse.
We want to thank you, Dr. A. P. Pawar, Principal, Poona College of Pharmacy, Bharati Vidyapeeth (Deemed to be University), for providing the necessary facilities to carry out this research work.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author’s Membership in Professional Societies: Association of Pharmaceutical Teachers in India, No. MA/LM-851.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Leng C, China; Luo Y, China S-Editor: Chen YL L-Editor: Filipodia A P-Editor: Chen YL
| 1. | Heimbach JK, Kulik LM, Finn RS, Sirlin CB, Abecassis MM, Roberts LR, Zhu AX, Murad MH, Marrero JA. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2107] [Cited by in RCA: 3023] [Article Influence: 431.9] [Reference Citation Analysis (3)] |
| 2. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 64542] [Article Influence: 16135.5] [Reference Citation Analysis (176)] |
| 3. | Mittal S, El-Serag HB. Epidemiology of hepatocellular carcinoma: consider the population. J Clin Gastroenterol. 2013;47 Suppl:S2-S6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 770] [Cited by in RCA: 879] [Article Influence: 73.3] [Reference Citation Analysis (0)] |
| 4. | Hassanipour S, Vali M, Gaffari-Fam S, Nikbakht HA, Abdzadeh E, Joukar F, Pourshams A, Shafaghi A, Malakoutikhah M, Arab-Zozani M, Salehiniya H, Mansour-Ghanaei F. The survival rate of hepatocellular carcinoma in Asian countries: a systematic review and meta-analysis. EXCLI J. 2020;19:108-130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 32] [Reference Citation Analysis (0)] |
| 5. | Ferlay J, Colombet M, Soerjomataram I, Parkin DM, Piñeros M, Znaor A, Bray F. Cancer statistics for the year 2020: An overview. Int J Cancer. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2411] [Cited by in RCA: 2956] [Article Influence: 739.0] [Reference Citation Analysis (7)] |
| 6. | Terashima T, Yamashita T, Takata N, Toyama T, Shimakami T, Takatori H, Arai K, Kawaguchi K, Kitamura K, Sakai Y, Mizukoshi E, Honda M, Kaneko S. Comparative analysis of liver functional reserve during lenvatinib and sorafenib for advanced hepatocellular carcinoma. Hepatol Res. 2020;50:871-884. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 7. | Casadei-Gardini A, Scartozzi M, Tada T, Yoo C, Shimose S, Masi G, Lonardi S, Frassineti LG, Nicola S, Piscaglia F, Kumada T, Kim HD, Koga H, Vivaldi C, Soldà C, Hiraoka A, Bang Y, Atsukawa M, Torimura T, Tsuj K, Itobayashi E, Toyoda H, Fukunishi S, Rimassa L, Rimini M, Cascinu S, Cucchetti A. Lenvatinib versus sorafenib in first-line treatment of unresectable hepatocellular carcinoma: An inverse probability of treatment weighting analysis. Liver Int. 2021;41:1389-1397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 8. | Schizas D, Charalampakis N, Kole C, Economopoulou P, Koustas E, Gkotsis E, Ziogas D, Psyrri A, Karamouzis MV. Immunotherapy for pancreatic cancer: A 2020 update. Cancer Treat Rev. 2020;86:102016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 295] [Article Influence: 59.0] [Reference Citation Analysis (0)] |
| 9. | Keilson JM, Knochelmann HM, Paulos CM, Kudchadkar RR, Lowe MC. The evolving landscape of immunotherapy in solid tumors. J Surg Oncol. 2021;123:798-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 10. | Zheng M, Tian Z. Liver-Mediated Adaptive Immune Tolerance. Front Immunol. 2019;10:2525. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 143] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 11. | Cheng AL, Hsu C, Chan SL, Choo SP, Kudo M. Challenges of combination therapy with immune checkpoint inhibitors for hepatocellular carcinoma. J Hepatol. 2020;72:307-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 372] [Article Influence: 74.4] [Reference Citation Analysis (1)] |
| 12. | Federico P, Petrillo A, Giordano P, Bosso D, Fabbrocini A, Ottaviano M, Rosanova M, Silvestri A, Tufo A, Cozzolino A, Daniele B. Immune Checkpoint Inhibitors in Hepatocellular Carcinoma: Current Status and Novel Perspectives. Cancers (Basel). 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 66] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 13. | Zongyi Y, Xiaowu L. Immunotherapy for hepatocellular carcinoma. Cancer Lett. 2020;470:8-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 178] [Article Influence: 35.6] [Reference Citation Analysis (0)] |
| 14. | Kole C, Charalampakis N, Tsakatikas S, Vailas M, Moris D, Gkotsis E, Kykalos S, Karamouzis MV, Schizas D. Immunotherapy for Hepatocellular Carcinoma: A 2021 Update. Cancers (Basel). 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 97] [Cited by in RCA: 95] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 15. | Sangro B, Sarobe P, Hervás-Stubbs S, Melero I. Advances in immunotherapy for hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol. 2021;18:525-543. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 264] [Cited by in RCA: 852] [Article Influence: 213.0] [Reference Citation Analysis (0)] |
| 16. | He X, Xu C. Immune checkpoint signaling and cancer immunotherapy. Cell Res. 2020;30:660-669. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 231] [Cited by in RCA: 848] [Article Influence: 169.6] [Reference Citation Analysis (0)] |
| 17. | Zhang Y, Zhang Z. The history and advances in cancer immunotherapy: understanding the characteristics of tumor-infiltrating immune cells and their therapeutic implications. Cell Mol Immunol. 2020;17:807-821. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1361] [Cited by in RCA: 1778] [Article Influence: 355.6] [Reference Citation Analysis (0)] |
| 18. | Okazaki T, Honjo T. PD-1 and PD-1 ligands: from discovery to clinical application. Int Immunol. 2007;19:813-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 808] [Cited by in RCA: 980] [Article Influence: 54.4] [Reference Citation Analysis (0)] |
| 19. | El-Khoueiry AB, Sangro B, Yau T, Crocenzi TS, Kudo M, Hsu C, Kim TY, Choo SP, Trojan J, Welling TH Rd, Meyer T, Kang YK, Yeo W, Chopra A, Anderson J, Dela Cruz C, Lang L, Neely J, Tang H, Dastani HB, Melero I. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet. 2017;389:2492-2502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3278] [Cited by in RCA: 3305] [Article Influence: 413.1] [Reference Citation Analysis (1)] |
| 20. | Finn RS, Ikeda M, Zhu AX, Sung MW, Baron AD, Kudo M, Okusaka T, Kobayashi M, Kumada H, Kaneko S, Pracht M, Mamontov K, Meyer T, Kubota T, Dutcus CE, Saito K, Siegel AB, Dubrovsky L, Mody K, Llovet JM. Phase Ib Study of Lenvatinib Plus Pembrolizumab in Patients With Unresectable Hepatocellular Carcinoma. J Clin Oncol. 2020;38:2960-2970. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 661] [Cited by in RCA: 874] [Article Influence: 174.8] [Reference Citation Analysis (0)] |
| 21. | Yau T, Park JW, Finn RS, Cheng AL, Mathurin P, Edeline J, Kudo M, Han KH, Harding JJ, Merle P, Rosmorduc O. CheckMate 459: A randomized, multi-center phase III study of nivolumab (NIVO) vs sorafenib (SOR) as first-line (1L) treatment in patients (pts) with advanced hepatocellular carcinoma (aHCC). Ann Oncol. 2019;30:v874-v875. [RCA] [DOI] [Full Text] [Cited by in Crossref: 426] [Cited by in RCA: 433] [Article Influence: 72.2] [Reference Citation Analysis (0)] |
| 22. | Sangro B, Chan SL, Meyer T, Reig M, El-Khoueiry A, Galle PR. Diagnosis and management of toxicities of immune checkpoint inhibitors in hepatocellular carcinoma. J Hepatol. 2020;72:320-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 192] [Article Influence: 38.4] [Reference Citation Analysis (0)] |
| 23. | Ducreux M, Abou-Alfa G, Ren Z, Edeline J, Li Z, Assenat E, Rimassa L, Blanc J, Ross P, Fang W, Hu S. O-1 Results from a global phase 2 study of tislelizumab, an investigational PD-1 antibody, in patients with unresectable hepatocellular carcinoma. Ann Oncol. 2021;32:S217. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (1)] |
| 24. | Liu Y, Zheng P. Preserving the CTLA-4 Checkpoint for Safer and More Effective Cancer Immunotherapy. Trends Pharmacol Sci. 2020;41:4-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 114] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 25. | Graziani G, Tentori L, Navarra P. Ipilimumab: a novel immunostimulatory monoclonal antibody for the treatment of cancer. Pharmacol Res. 2012;65:9-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 116] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 26. | Furness AJ, Vargas FA, Peggs KS, Quezada SA. Impact of tumour microenvironment and Fc receptors on the activity of immunomodulatory antibodies. Trends Immunol. 2014;35:290-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 88] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 27. | Sangro B, Gomez-Martin C, de la Mata M, Iñarrairaegui M, Garralda E, Barrera P, Riezu-Boj JI, Larrea E, Alfaro C, Sarobe P, Lasarte JJ, Pérez-Gracia JL, Melero I, Prieto J. A clinical trial of CTLA-4 blockade with tremelimumab in patients with hepatocellular carcinoma and chronic hepatitis C. J Hepatol. 2013;59:81-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 634] [Cited by in RCA: 750] [Article Influence: 62.5] [Reference Citation Analysis (0)] |
| 28. | Du X, Tang F, Liu M, Su J, Zhang Y, Wu W, Devenport M, Lazarski CA, Zhang P, Wang X, Ye P, Wang C, Hwang E, Zhu T, Xu T, Zheng P, Liu Y. A reappraisal of CTLA-4 checkpoint blockade in cancer immunotherapy. Cell Res. 2018;28:416-432. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 186] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 29. | Gautron AS, Dominguez-Villar M, de Marcken M, Hafler DA. Enhanced suppressor function of TIM-3+ FoxP3+ regulatory T cells. Eur J Immunol. 2014;44:2703-2711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 187] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 30. | Wolf Y, Anderson AC, Kuchroo VK. TIM3 comes of age as an inhibitory receptor. Nat Rev Immunol. 2020;20:173-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 666] [Article Influence: 111.0] [Reference Citation Analysis (0)] |
| 31. | Wang J, Sun J, Liu LN, Flies DB, Nie X, Toki M, Zhang J, Song C, Zarr M, Zhou X, Han X, Archer KA, O'Neill T, Herbst RS, Boto AN, Sanmamed MF, Langermann S, Rimm DL, Chen L. Siglec-15 as an immune suppressor and potential target for normalization cancer immunotherapy. Nat Med. 2019;25:656-666. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 270] [Cited by in RCA: 488] [Article Influence: 81.3] [Reference Citation Analysis (0)] |
| 32. | Liu W, Ji Z, Wu B, Huang S, Chen Q, Chen X, Wei Y, Jiang J. Siglec-15 promotes the migration of liver cancer cells by repressing lysosomal degradation of CD44. FEBS Lett. 2021;595:2290-2302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 33. | Zheng Q, Xu J, Gu X, Wu F, Deng J, Cai X, Wang G, Li G, Chen Z. Immune checkpoint targeting TIGIT in hepatocellular carcinoma. Am J Transl Res. 2020;12:3212-3224. [PubMed] |
| 34. | Yu X, Harden K, Gonzalez LC, Francesco M, Chiang E, Irving B, Tom I, Ivelja S, Refino CJ, Clark H, Eaton D, Grogan JL. The surface protein TIGIT suppresses T cell activation by promoting the generation of mature immunoregulatory dendritic cells. Nat Immunol. 2009;10:48-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 760] [Cited by in RCA: 1077] [Article Influence: 63.4] [Reference Citation Analysis (0)] |
| 35. | Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim TY, Kudo M, Breder V, Merle P, Kaseb AO, Li D, Verret W, Xu DZ, Hernandez S, Liu J, Huang C, Mulla S, Wang Y, Lim HY, Zhu AX, Cheng AL; IMbrave150 Investigators. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N Engl J Med. 2020;382:1894-1905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2542] [Cited by in RCA: 4682] [Article Influence: 936.4] [Reference Citation Analysis (2)] |
| 36. | Finn RS, Ryoo BY, Merle P, Kudo M, Bouattour M, Lim HY, Breder V, Edeline J, Chao Y, Ogasawara S, Yau T, Garrido M, Chan SL, Knox J, Daniele B, Ebbinghaus SW, Chen E, Siegel AB, Zhu AX, Cheng AL; KEYNOTE-240 investigators. Pembrolizumab As Second-Line Therapy in Patients With Advanced Hepatocellular Carcinoma in KEYNOTE-240: A Randomized, Double-Blind, Phase III Trial. J Clin Oncol. 2020;38:193-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1365] [Cited by in RCA: 1339] [Article Influence: 267.8] [Reference Citation Analysis (0)] |
| 37. | Cui J, Wang N, Zhao H, Jin H, Wang G, Niu C, Terunuma H, He H, Li W. Combination of radiofrequency ablation and sequential cellular immunotherapy improves progression-free survival for patients with hepatocellular carcinoma. Int J Cancer. 2014;134:342-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 98] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 38. | Duffy AG, Ulahannan SV, Makorova-Rusher O, Rahma O, Wedemeyer H, Pratt D, Davis JL, Hughes MS, Heller T, ElGindi M, Uppala A, Korangy F, Kleiner DE, Figg WD, Venzon D, Steinberg SM, Venkatesan AM, Krishnasamy V, Abi-Jaoudeh N, Levy E, Wood BJ, Greten TF. Tremelimumab in combination with ablation in patients with advanced hepatocellular carcinoma. J Hepatol. 2017;66:545-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 454] [Cited by in RCA: 639] [Article Influence: 79.9] [Reference Citation Analysis (0)] |
| 39. | Li H, Qin S, Liu Y, Chen Z, Ren Z, Xiong J, Meng Z, Zhang X, Wang L, Zou J. Camrelizumab Combined with FOLFOX4 Regimen as First-Line Therapy for Advanced Hepatocellular Carcinomas: A Sub-Cohort of a Multicenter Phase Ib/II Study. Drug Des Devel Ther. 2021;15:1873-1882. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 40. | Abou-Alfa GK, Chan SL, Kudo M, Lau G, Kelley RK, Furuse J, Sukeepaisarnjaroen W, Kang YK, Dao TV, De Toni EN, Rimassa L. Phase 3 randomized, open-label, multicenter study of tremelimumab (T) and durvalumab (D) as first-line therapy in patients (pts) with unresectable hepatocellular carcinoma (uHCC): HIMALAYA. J Clin Oncol. 2022;40:379. [RCA] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 100] [Article Influence: 33.3] [Reference Citation Analysis (0)] |
| 41. | Kelley RK, Sangro B, Harris W, Ikeda M, Okusaka T, Kang YK, Qin S, Tai DW, Lim HY, Yau T, Yong WP, Cheng AL, Gasbarrini A, Damian S, Bruix J, Borad M, Bendell J, Kim TY, Standifer N, He P, Makowsky M, Negro A, Kudo M, Abou-Alfa GK. Safety, Efficacy, and Pharmacodynamics of Tremelimumab Plus Durvalumab for Patients With Unresectable Hepatocellular Carcinoma: Randomized Expansion of a Phase I/II Study. J Clin Oncol. 2021;39:2991-3001. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 79] [Cited by in RCA: 328] [Article Influence: 82.0] [Reference Citation Analysis (0)] |
| 42. | Yau T, Kang YK, Kim TY, El-Khoueiry AB, Santoro A, Sangro B, Melero I, Kudo M, Hou MM, Matilla A, Tovoli F, Knox JJ, Ruth He A, El-Rayes BF, Acosta-Rivera M, Lim HY, Neely J, Shen Y, Wisniewski T, Anderson J, Hsu C. Efficacy and Safety of Nivolumab Plus Ipilimumab in Patients With Advanced Hepatocellular Carcinoma Previously Treated With Sorafenib: The CheckMate 040 Randomized Clinical Trial. JAMA Oncol. 2020;6:e204564. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 908] [Cited by in RCA: 967] [Article Influence: 193.4] [Reference Citation Analysis (0)] |
| 43. | Martinez-Cannon BA, Castro-Sanchez A, Barragan-Carrillo R, de la Rosa Pacheco S, Platas A, Fonseca A, Vega Y, Bojorquez-Velazquez K, Bargallo-Rocha JE, Mohar A, Villarreal-Garza C. Adherence to Adjuvant Tamoxifen in Mexican Young Women with Breast Cancer. Patient Prefer Adherence. 2021;15:1039-1049. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 44. | Lee M, Ryoo BY, Hsu CH, Numata K, Stein S, Verret W, Hack S, Spahn J, Liu B, Abdullah H, He R. Randomised efficacy and safety results for atezolizumab (Atezo)+ bevacizumab (Bev) in patients (pts) with previously untreated, unresectable hepatocellular carcinoma (HCC). Annals Oncol. 2019;30:v875. [RCA] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 45. | Hegde PS, Wallin JJ, Mancao C. Predictive markers of anti-VEGF and emerging role of angiogenesis inhibitors as immunotherapeutics. Semin Cancer Biol. 2018;52:117-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 334] [Article Influence: 41.8] [Reference Citation Analysis (0)] |
| 46. | Kelley RK, Sangro B, Harris WP, Ikeda M, Okusaka T, Kang YK, Qin S, Tai WM, Lim HY, Yau T, Yong WP. Efficacy, tolerability, and biologic activity of a novel regimen of tremelimumab (T) in combination with durvalumab (D) for patients (pts) with advanced hepatocellular carcinoma (aHCC). J Clin Oncol. 2020;38:4508. [RCA] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 74] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 47. | Exelixis. Exelixis and Ipsen announce cabozantinib in combination with an immune checkpoint inhibitor significantly improved progression-free survival in phase 3 COSMIC-312 pivotal trial in patients with previously untreated advanced liver cancer. September 12, 2021. [cited 3 September 2022]. Available from: https://ir.exelixis.com/news-releases/news-release-details/exelixis-and-ipsen-announce-cabozantinib-combination-immune. |
| 48. | Llovet JM, Kudo M, Cheng AL, Finn RS, Galle PR, Kaneko S, Meyer T, Qin S, Dutcus CE, Chen E, Dubrovsky L. Lenvatinib (len) plus pembrolizumab (pembro) for the first-line treatment of patients (pts) with advanced hepatocellular carcinoma (HCC): phase 3 LEAP-002 study. J Clin Oncol. 2019;37:TPS4152. [RCA] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 77] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 49. | Xu J, Zhang Y, Jia R, Yue C, Chang L, Liu R, Zhang G, Zhao C, Chen C, Wang Y, Yi X, Hu Z, Zou J, Wang Q. Anti-PD-1 Antibody SHR-1210 Combined with Apatinib for Advanced Hepatocellular Carcinoma, Gastric, or Esophagogastric Junction Cancer: An Open-label, Dose Escalation and Expansion Study. Clin Cancer Res. 2019;25:515-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 359] [Article Influence: 51.3] [Reference Citation Analysis (0)] |
| 50. | Hosseini SS, Khalili S, Baradaran B, Bidar N, Shahbazi MA, Mosafer J, Hashemzaei M, Mokhtarzadeh A, Hamblin MR. Bispecific monoclonal antibodies for targeted immunotherapy of solid tumors: Recent advances and clinical trials. Int J Biol Macromol. 2021;167:1030-1047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 52] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 51. | Hoseini SS, Cheung NV. Immunotherapy of hepatocellular carcinoma using chimeric antigen receptors and bispecific antibodies. Cancer Lett. 2017;399:44-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 39] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 52. | Hoh A, Dewerth A, Vogt F, Wenz J, Baeuerle PA, Warmann SW, Fuchs J, Armeanu-Ebinger S. The activity of γδ T cells against paediatric liver tumour cells and spheroids in cell culture. Liver Int. 2013;33:127-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 53. | Mayer K, Baumann AL, Grote M, Seeber S, Kettenberger H, Breuer S, Killian T, Schäfer W, Brinkmann U. TriFabs--Trivalent IgG-Shaped Bispecific Antibody Derivatives: Design, Generation, Characterization and Application for Targeted Payload Delivery. Int J Mol Sci. 2015;16:27497-27507. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 54. | Laskowski T, Rezvani K. Adoptive cell therapy: Living drugs against cancer. J Exp Med. 2020;217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 55. | Rosenberg SA, Restifo NP. Adoptive cell transfer as personalized immunotherapy for human cancer. Science. 2015;348:62-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1877] [Cited by in RCA: 1842] [Article Influence: 184.2] [Reference Citation Analysis (0)] |
| 56. | Hendrickson PG, Olson M, Luetkens T, Weston S, Han T, Atanackovic D, Fine GC. The promise of adoptive cellular immunotherapies in hepatocellular carcinoma. Oncoimmunology. 2020;9:1673129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 57. | Baruch EN, Berg AL, Besser MJ, Schachter J, Markel G. Adoptive T cell therapy: An overview of obstacles and opportunities. Cancer. 2017;123:2154-2162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 68] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 58. | Gao X, Mi Y, Guo N, Xu H, Xu L, Gou X, Jin W. Cytokine-Induced Killer Cells As Pharmacological Tools for Cancer Immunotherapy. Front Immunol. 2017;8:774. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 117] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 59. | Shi M, Zhang B, Tang ZR, Lei ZY, Wang HF, Feng YY, Fan ZP, Xu DP, Wang FS. Autologous cytokine-induced killer cell therapy in clinical trial phase I is safe in patients with primary hepatocellular carcinoma. World J Gastroenterol. 2004;10:1146-1151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 92] [Cited by in RCA: 101] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 60. | Takayama T, Sekine T, Makuuchi M, Yamasaki S, Kosuge T, Yamamoto J, Shimada K, Sakamoto M, Hirohashi S, Ohashi Y, Kakizoe T. Adoptive immunotherapy to lower postsurgical recurrence rates of hepatocellular carcinoma: a randomised trial. Lancet. 2000;356:802-807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 630] [Cited by in RCA: 653] [Article Influence: 26.1] [Reference Citation Analysis (0)] |
| 61. | Wang XP, Xu M, Gao HF, Zhao JF, Xu KC. Intraperitoneal perfusion of cytokine-induced killer cells with local hyperthermia for advanced hepatocellular carcinoma. World J Gastroenterol. 2013;19:2956-2962. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 62. | Wang H, Liu A, Bo W, Feng X, Hu Y, Tian L, Zhang H, Tang X. Adjuvant immunotherapy with autologous cytokine-induced killer cells for hepatocellular carcinoma patients after curative resection, a systematic review and meta-analysis. Dig Liver Dis. 2016;48:1275-1282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 63. | Paijens ST, Vledder A, de Bruyn M, Nijman HW. Tumor-infiltrating lymphocytes in the immunotherapy era. Cell Mol Immunol. 2021;18:842-859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 491] [Cited by in RCA: 567] [Article Influence: 141.8] [Reference Citation Analysis (0)] |
| 64. | Topalian SL, Muul LM, Solomon D, Rosenberg SA. Expansion of human tumor infiltrating lymphocytes for use in immunotherapy trials. J Immunol Methods. 1987;102:127-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 263] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 65. | Lee JH, Lee JH, Lim YS, Yeon JE, Song TJ, Yu SJ, Gwak GY, Kim KM, Kim YJ, Lee JW, Yoon JH. Adjuvant immunotherapy with autologous cytokine-induced killer cells for hepatocellular carcinoma. Gastroenterology. 2015;148:1383-91.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 283] [Cited by in RCA: 388] [Article Influence: 38.8] [Reference Citation Analysis (0)] |
| 66. | Jochems C, Schlom J. Tumor-infiltrating immune cells and prognosis: the potential link between conventional cancer therapy and immunity. Exp Biol Med (Maywood). 2011;236:567-579. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 293] [Cited by in RCA: 265] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 67. | Wada Y, Nakashima O, Kutami R, Yamamoto O, Kojiro M. Clinicopathological study on hepatocellular carcinoma with lymphocytic infiltration. Hepatology. 1998;27:407-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 301] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 68. | Ma W, Chen X, Yuan Y. T-cell-associated immunotherapy: a promising strategy for the treatment of hepatocellular carcinoma. Immunotherapy. 2017;9:523-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 69. | Jiang SS, Tang Y, Zhang YJ, Weng DS, Zhou ZG, Pan K, Pan QZ, Wang QJ, Liu Q, He J, Zhao JJ, Li J, Chen MS, Chang AE, Li Q, Xia JC. A phase I clinical trial utilizing autologous tumor-infiltrating lymphocytes in patients with primary hepatocellular carcinoma. Oncotarget. 2015;6:41339-41349. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 84] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 70. | Fucà G, Reppel L, Landoni E, Savoldo B, Dotti G. Enhancing Chimeric Antigen Receptor T-Cell Efficacy in Solid Tumors. Clin Cancer Res. 2020;26:2444-2451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 105] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 71. | June CH, Sadelain M. Chimeric Antigen Receptor Therapy. N Engl J Med. 2018;379:64-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1140] [Cited by in RCA: 1601] [Article Influence: 228.7] [Reference Citation Analysis (0)] |
| 72. | June CH, O’Connor RS, Kawalekar OU, Ghassemi S, Milone MC. CAR T Cell Immunotherapy for Human Cancer. Sci. 2018;359:1361-1365. |
| 73. | Yong CSM, Dardalhon V, Devaud C, Taylor N, Darcy PK, Kershaw MH. CAR T-cell therapy of solid tumors. Immunol Cell Biol. 2017;95:356-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 147] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 74. | Zhou F, Shang W, Yu X, Tian J. Glypican-3: A promising biomarker for hepatocellular carcinoma diagnosis and treatment. Med Res Rev. 2018;38:741-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 257] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 75. | Gao H, Li K, Tu H, Pan X, Jiang H, Shi B, Kong J, Wang H, Yang S, Gu J, Li Z. Development of T cells redirected to glypican-3 for the treatment of hepatocellular carcinoma. Clin Cancer Res. 2014;20:6418-6428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 231] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 76. | Liu X, Wen J, Yi H, Hou X, Yin Y, Ye G, Wu X, Jiang X. Split chimeric antigen receptor-modified T cells targeting glypican-3 suppress hepatocellular carcinoma growth with reduced cytokine release. Ther Adv Med Oncol. 2020;12:1758835920910347. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 77. | Jiang Z, Jiang X, Chen S, Lai Y, Wei X, Li B, Lin S, Wang S, Wu Q, Liang Q, Liu Q, Peng M, Yu F, Weng J, Du X, Pei D, Liu P, Yao Y, Xue P, Li P. Anti-GPC3-CAR T Cells Suppress the Growth of Tumor Cells in Patient-Derived Xenografts of Hepatocellular Carcinoma. Front Immunol. 2016;7:690. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 139] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 78. | Schieving JH, de Vries M, van Vugt JM, Weemaes C, van Deuren M, Nicolai J, Wevers RA, Willemsen MA. Alpha-fetoprotein, a fascinating protein and biomarker in neurology. Eur J Paediatr Neurol. 2014;18:243-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 79. | Liu H, Xu Y, Xiang J, Long L, Green S, Yang Z, Zimdahl B, Lu J, Cheng N, Horan LH, Liu B, Yan S, Wang P, Diaz J, Jin L, Nakano Y, Morales JF, Zhang P, Liu LX, Staley BK, Priceman SJ, Brown CE, Forman SJ, Chan VW, Liu C. Targeting Alpha-Fetoprotein (AFP)-MHC Complex with CAR T-Cell Therapy for Liver Cancer. Clin Cancer Res. 2017;23:478-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 171] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 80. | Huh CG, Factor VM, Sánchez A, Uchida K, Conner EA, Thorgeirsson SS. Hepatocyte growth factor/c-met signaling pathway is required for efficient liver regeneration and repair. Proc Natl Acad Sci U S A. 2004;101:4477-4482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 559] [Cited by in RCA: 616] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 81. | Jiang W, Li T, Guo J, Wang J, Jia L, Shi X, Yang T, Jiao R, Wei X, Feng Z, Tang Q, Ji G. Bispecific c-Met/PD-L1 CAR-T Cells Have Enhanced Therapeutic Effects on Hepatocellular Carcinoma. Front Oncol. 2021;11:546586. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 82. | Guerra N, Lanier LL. Editorial: Emerging Concepts on the NKG2D Receptor-Ligand Axis in Health and Diseases. Front Immunol. 2020;11:562. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 83. | Sun B, Yang D, Dai H, Liu X, Jia R, Cui X, Li W, Cai C, Xu J, Zhao X. Eradication of Hepatocellular Carcinoma by NKG2D-Based CAR-T Cells. Cancer Immunol Res. 2019;7:1813-1823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 105] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 84. | Wang SJ, Chao D, Wei W, Nan G, Li JY, Liu FL, Li L, Jiang JL, Cui HY, Chen ZN. CD147 promotes collective invasion through cathepsin B in hepatocellular carcinoma. J Exp Clin Cancer Res. 2020;39:145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 85. | Zhang RY, Wei D, Liu ZK, Yong YL, Wei W, Zhang ZY, Lv JJ, Zhang Z, Chen ZN, Bian H. Doxycycline Inducible Chimeric Antigen Receptor T Cells Targeting CD147 for Hepatocellular Carcinoma Therapy. Front Cell Dev Biol. 2019;7:233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 64] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 86. | Ma YD, Wang Z, Gong RZ, Li LF, Wu HP, Jin HJ, Qian QJ. Specific Cytotoxicity of MUC1 Chimeric Antigen Receptor-Engineered Jurkat T Cells Against Hepatocellular Carcinoma. Acad J Second Military Med Univ. 2014;35:1177-1182. [RCA] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 87. | Vasanthakumar S, Sasikala P, Padma M, Balachandar V, Venkatesh B, Ganesan S. EpCAM as a novel therapeutic target for hepatocellular carcinoma. J Oncolog Sci. 2017;3:71-76. [RCA] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 88. | Dai H, Tong C, Shi D, Chen M, Guo Y, Chen D, Han X, Wang H, Wang Y, Shen P. Efficacy and biomarker analysis of CD133-directed CAR T cells in advanced hepatocellular carcinoma: a single-arm, open-label, phase II trial. Oncoimmunology. 2020;9:1846926. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 111] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 89. | Liu F, Qian Y. The role of CD133 in hepatocellular carcinoma. Cancer Biol Ther. 2021;22:291-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 90. | Sun H, Sun C, Tian Z, Xiao W. NK cells in immunotolerant organs. Cell Mol Immunol. 2013;10:202-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 91. | Kalathil SG, Thanavala Y. Natural Killer Cells and T Cells in Hepatocellular Carcinoma and Viral Hepatitis: Current Status and Perspectives for Future Immunotherapeutic Approaches. Cells. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 92. | King C. CAR NK Cell Therapy for T Follicular Helper Cells. Cell Rep Med. 2020;1:100009. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 93. | Yu M, Luo H, Fan M, Wu X, Shi B, Di S, Liu Y, Pan Z, Jiang H, Li Z. Development of GPC3-Specific Chimeric Antigen Receptor-Engineered Natural Killer Cells for the Treatment of Hepatocellular Carcinoma. Mol Ther. 2018;26:366-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 139] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 94. | Tseng HC, Xiong W, Badeti S, Yang Y, Ma M, Liu T, Ramos CA, Dotti G, Fritzky L, Jiang JG, Yi Q, Guarrera J, Zong WX, Liu C, Liu D. Efficacy of anti-CD147 chimeric antigen receptors targeting hepatocellular carcinoma. Nat Commun. 2020;11:4810. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 121] [Cited by in RCA: 130] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 95. | Streltsova MA, Barsov E, Erokhina SA, Kovalenko EI. Retroviral gene transfer into primary human NK cells activated by IL-2 and K562 feeder cells expressing membrane-bound IL-21. J Immunol Methods. 2017;450:90-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 96. | Watanabe K, Nishikawa H. Engineering strategies for broad application of TCR-T- and CAR-T-cell therapies. Int Immunol. 2021;33:551-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 97. | Rosen HR. Clinical practice. Chronic hepatitis C infection. N Engl J Med. 2011;364:2429-2438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 333] [Cited by in RCA: 316] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 98. | Spear TT, Callender GG, Roszkowski JJ, Moxley KM, Simms PE, Foley KC, Murray DC, Scurti GM, Li M, Thomas JT, Langerman A, Garrett-Mayer E, Zhang Y, Nishimura MI. TCR gene-modified T cells can efficiently treat established hepatitis C-associated hepatocellular carcinoma tumors. Cancer Immunol Immunother. 2016;65:293-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 99. | Gehring AJ, Xue SA, Ho ZZ, Teoh D, Ruedl C, Chia A, Koh S, Lim SG, Maini MK, Stauss H, Bertoletti A. Engineering virus-specific T cells that target HBV infected hepatocytes and hepatocellular carcinoma cell lines. J Hepatol. 2011;55:103-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 177] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 100. | Qasim W, Brunetto M, Gehring AJ, Xue SA, Schurich A, Khakpoor A, Zhan H, Ciccorossi P, Gilmour K, Cavallone D, Moriconi F, Farzhenah F, Mazzoni A, Chan L, Morris E, Thrasher A, Maini MK, Bonino F, Stauss H, Bertoletti A. Immunotherapy of HCC metastases with autologous T cell receptor redirected T cells, targeting HBsAg in a liver transplant patient. J Hepatol. 2015;62:486-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 154] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 101. | Docta RY, Ferronha T, Sanderson JP, Weissensteiner T, Pope GR, Bennett AD, Pumphrey NJ, Ferjentsik Z, Quinn LL, Wiedermann GE, Anderson VE, Saini M, Maroto M, Norry E, Gerry AB. Tuning T-Cell Receptor Affinity to Optimize Clinical Risk-Benefit When Targeting Alpha-Fetoprotein-Positive Liver Cancer. Hepatology. 2019;69:2061-2075. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (1)] |
| 102. | Zhu W, Peng Y, Wang L, Hong Y, Jiang X, Li Q, Liu H, Huang L, Wu J, Celis E, Merchen T, Kruse E, He Y. Identification of α-fetoprotein-specific T-cell receptors for hepatocellular carcinoma immunotherapy. Hepatology. 2018;68:574-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 82] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 103. | Dargel C, Bassani-Sternberg M, Hasreiter J, Zani F, Bockmann JH, Thiele F, Bohne F, Wisskirchen K, Wilde S, Sprinzl MF, Schendel DJ, Krackhardt AM, Uckert W, Wohlleber D, Schiemann M, Stemmer K, Heikenwälder M, Busch DH, Richter G, Mann M, Protzer U. T Cells Engineered to Express a T-Cell Receptor Specific for Glypican-3 to Recognize and Kill Hepatoma Cells In Vitro and in Mice. Gastroenterology. 2015;149:1042-1052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 77] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 104. | Thomas R, Al-Khadairi G, Roelands J, Hendrickx W, Dermime S, Bedognetti D, Decock J. NY-ESO-1 Based Immunotherapy of Cancer: Current Perspectives. Front Immunol. 2018;9:947. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 174] [Cited by in RCA: 288] [Article Influence: 41.1] [Reference Citation Analysis (0)] |
| 105. | Mizukoshi E, Nakamoto Y, Marukawa Y, Arai K, Yamashita T, Tsuji H, Kuzushima K, Takiguchi M, Kaneko S. Cytotoxic T cell responses to human telomerase reverse transcriptase in patients with hepatocellular carcinoma. Hepatology. 2006;43:1284-1294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 92] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 106. | Cameron BJ, Gerry AB, Dukes J, Harper JV, Kannan V, Bianchi FC, Grand F, Brewer JE, Gupta M, Plesa G, Bossi G, Vuidepot A, Powlesland AS, Legg A, Adams KJ, Bennett AD, Pumphrey NJ, Williams DD, Binder-Scholl G, Kulikovskaya I, Levine BL, Riley JL, Varela-Rohena A, Stadtmauer EA, Rapoport AP, Linette GP, June CH, Hassan NJ, Kalos M, Jakobsen BK. Identification of a Titin-derived HLA-A1-presented peptide as a cross-reactive target for engineered MAGE A3-directed T cells. Sci Transl Med. 2013;5:197ra103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 443] [Cited by in RCA: 542] [Article Influence: 49.3] [Reference Citation Analysis (0)] |
| 107. | Waldmann TA. Cytokines in Cancer Immunotherapy. Cold Spring Harb Perspect Biol. 2018;10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 340] [Article Influence: 48.6] [Reference Citation Analysis (0)] |
| 108. | Rai KR, Davey F, Peterson B, Schiffer C, Silver RT, Ozer H, Golomb H, Bloomfield CD. Recombinant alpha-2b-interferon in therapy of previously untreated hairy cell leukemia: long-term follow-up results of study by Cancer and Leukemia Group B. Leukemia. 1995;9:1116-1120. [PubMed] |
| 109. | European Association For The Study Of The Liver; Clinical Practice Guidelines Panel; Chair; EASL Governing Board Representative; Panel Members. Corrigendum to 'EASL recommendations on treatment of hepatitis C: Final update of the series(') [J Hepatol 73 (2020) 1170-1218]. J Hepatol. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 110. | Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS, Abecassis MM, Roberts LR, Heimbach JK. Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018;68:723-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2121] [Cited by in RCA: 3237] [Article Influence: 462.4] [Reference Citation Analysis (1)] |
| 111. | Iyer SS, Cheng G. Role of interleukin 10 transcriptional regulation in inflammation and autoimmune disease. Crit Rev Immunol. 2012;32:23-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 622] [Cited by in RCA: 1056] [Article Influence: 81.2] [Reference Citation Analysis (0)] |
| 112. | Ouyang W, O'Garra A. IL-10 Family Cytokines IL-10 and IL-22: from Basic Science to Clinical Translation. Immunity. 2019;50:871-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 536] [Cited by in RCA: 722] [Article Influence: 120.3] [Reference Citation Analysis (0)] |
| 113. | Shakiba E, Ramezani M, Sadeghi M. Evaluation of serum interleukin-6 levels in hepatocellular carcinoma patients: a systematic review and meta-analysis. Clin Exp Hepatol. 2018;4:182-190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 114. | Hattori E, Okumoto K, Adachi T, Takeda T, Ito J, Sugahara K, Watanabe H, Saito K, Saito T, Togashi H, Kawata S. Possible contribution of circulating interleukin-10 (IL-10) to anti-tumor immunity and prognosis in patients with unresectable hepatocellular carcinoma. Hepatol Res. 2003;27:309-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 41] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 115. | Chan SL, Mo FK, Wong CS, Chan CM, Leung LK, Hui EP, Ma BB, Chan AT, Mok TS, Yeo W. A study of circulating interleukin 10 in prognostication of unresectable hepatocellular carcinoma. Cancer. 2012;118:3984-3992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 55] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 116. | Zhao M, Li Y, Guo C, Wang L, Chu H, Zhu F, Wang X, Wang Q, Zhao W, Shi Y, Chen W, Zhang L. IL-37 isoform D downregulates pro-inflammatory cytokines expression in a Smad3-dependent manner. Cell Death Dis. 2018;9:582. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 117. | Pu XY, Zheng DF, Shen A, Gu HT, Wei XF, Mou T, Zhang JB, Liu R. IL-37b suppresses epithelial mesenchymal transition in hepatocellular carcinoma by inhibiting IL-6/STAT3 signaling. Hepatobiliary Pancreat Dis Int. 2018;17:408-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 118. | Liu R, Tang C, Shen A, Luo H, Wei X, Zheng D, Sun C, Li Z, Zhu D, Li T, Wu Z. IL-37 suppresses hepatocellular carcinoma growth by converting pSmad3 signaling from JNK/pSmad3L/c-Myc oncogenic signaling to pSmad3C/P21 tumor-suppressive signaling. Oncotarget. 2016;7:85079-85096. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 119. | Luo C, Shu Y, Luo J, Liu D, Huang DS, Han Y, Chen C, Li YC, Zou JM, Qin J, Wang Y, Li D, Wang SS, Zhang GM, Chen J, Feng ZH. Intracellular IL-37b interacts with Smad3 to suppress multiple signaling pathways and the metastatic phenotype of tumor cells. Oncogene. 2017;36:2889-2899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 120. | Kadomoto S, Izumi K, Mizokami A. The CCL20-CCR6 Axis in Cancer Progression. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 168] [Article Influence: 33.6] [Reference Citation Analysis (0)] |
| 121. | Guo W, Li H, Liu H, Ma X, Yang S, Wang Z. DEPDC1 drives hepatocellular carcinoma cell proliferation, invasion and angiogenesis by regulating the CCL20/CCR6 signaling pathway. Oncol Rep. 2019;42:1075-1089. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 122. | Rubie C, Frick VO, Wagner M, Rau B, Weber C, Kruse B, Kempf K, Tilton B, König J, Schilling M. Enhanced expression and clinical significance of CC-chemokine MIP-3 alpha in hepatocellular carcinoma. Scand J Immunol. 2006;63:468-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 123. | Rubie C, Frick VO, Wagner M, Weber C, Kruse B, Kempf K, König J, Rau B, Schilling M. Chemokine expression in hepatocellular carcinoma versus colorectal liver metastases. World J Gastroenterol. 2006;12:6627-6633. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 33] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 124. | Chen KJ, Lin SZ, Zhou L, Xie HY, Zhou WH, Taki-Eldin A, Zheng SS. Selective recruitment of regulatory T cell through CCR6-CCL20 in hepatocellular carcinoma fosters tumor progression and predicts poor prognosis. PLoS One. 2011;6:e24671. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 147] [Cited by in RCA: 188] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 125. | Shao YY, Lin H, Li YS, Lee YH, Chen HM, Cheng AL, Hsu CH. High plasma interleukin-6 levels associated with poor prognosis of patients with advanced hepatocellular carcinoma. Jpn J Clin Oncol. 2017;47:949-953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 126. | Li Y, Chen G, Han Z, Cheng H, Qiao L, Li Y. IL-6/STAT3 Signaling Contributes to Sorafenib Resistance in Hepatocellular Carcinoma Through Targeting Cancer Stem Cells. Onco Targets Ther. 2020;13:9721-9730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 127. | Augustin HG, Koh GY, Thurston G, Alitalo K. Control of vascular morphogenesis and homeostasis through the angiopoietin-Tie system. Nat Rev Mol Cell Biol. 2009;10:165-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 995] [Cited by in RCA: 1069] [Article Influence: 66.8] [Reference Citation Analysis (0)] |
| 128. | Llovet JM, Peña CE, Lathia CD, Shan M, Meinhardt G, Bruix J; SHARP Investigators Study Group. Plasma biomarkers as predictors of outcome in patients with advanced hepatocellular carcinoma. Clin Cancer Res. 2012;18:2290-2300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 464] [Cited by in RCA: 455] [Article Influence: 35.0] [Reference Citation Analysis (2)] |
| 129. | Adachi T, Nouso K, Miyahara K, Oyama A, Wada N, Dohi C, Takeuchi Y, Yasunaka T, Onishi H, Ikeda F, Nakamura S, Shiraha H, Takaki A, Takabatake H, Fujioka SI, Kobashi H, Takuma Y, Iwadou S, Uematsu S, Takaguchi K, Hagihara H, Okada H; Okayama Liver Cancer Group. Monitoring serum proangiogenic cytokines from hepatocellular carcinoma patients treated with sorafenib. J Gastroenterol Hepatol. 2019;34:1081-1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 130. | Giordano S, Columbano A. Met as a therapeutic target in HCC: facts and hopes. J Hepatol. 2014;60:442-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 141] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 131. | Miyahara K, Nouso K, Morimoto Y, Takeuchi Y, Hagihara H, Kuwaki K, Onishi H, Ikeda F, Miyake Y, Nakamura S, Shiraha H, Takaki A, Honda M, Kaneko S, Sato T, Sato S, Obi S, Iwadou S, Kobayashi Y, Takaguchi K, Kariyama K, Takuma Y, Takabatake H, Yamamoto K; Okayama Liver Cancer Group. Pro-angiogenic cytokines for prediction of outcomes in patients with advanced hepatocellular carcinoma. Br J Cancer. 2013;109:2072-2078. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 132. | Tsuchiya K, Asahina Y, Matsuda S, Muraoka M, Nakata T, Suzuki Y, Tamaki N, Yasui Y, Suzuki S, Hosokawa T, Nishimura T, Ueda K, Kuzuya T, Nakanishi H, Itakura J, Takahashi Y, Kurosaki M, Enomoto N, Izumi N. Changes in plasma vascular endothelial growth factor at 8 weeks after sorafenib administration as predictors of survival for advanced hepatocellular carcinoma. Cancer. 2014;120:229-237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 133. | Buonaguro L; HEPAVAC Consortium. New vaccination strategies in liver cancer. Cytokine Growth Factor Rev. 2017;36:125-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 134. | Butterfield LH, Ribas A, Meng WS, Dissette VB, Amarnani S, Vu HT, Seja E, Todd K, Glaspy JA, McBride WH, Economou JS. T-cell responses to HLA-A*0201 immunodominant peptides derived from alpha-fetoprotein in patients with hepatocellular cancer. Clin Cancer Res. 2003;9:5902-5908. [PubMed] |
| 135. | Butterfield LH, Ribas A, Dissette VB, Lee Y, Yang JQ, De la Rocha P, Duran SD, Hernandez J, Seja E, Potter DM, McBride WH, Finn R, Glaspy JA, Economou JS. A phase I/II trial testing immunization of hepatocellular carcinoma patients with dendritic cells pulsed with four alpha-fetoprotein peptides. Clin Cancer Res. 2006;12:2817-2825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 197] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 136. | Sawada Y, Yoshikawa T, Ofuji K, Yoshimura M, Tsuchiya N, Takahashi M, Nobuoka D, Gotohda N, Takahashi S, Kato Y, Konishi M, Kinoshita T, Ikeda M, Nakachi K, Yamazaki N, Mizuno S, Takayama T, Yamao K, Uesaka K, Furuse J, Endo I, Nakatsura T. Phase II study of the GPC3-derived peptide vaccine as an adjuvant therapy for hepatocellular carcinoma patients. Oncoimmunology. 2016;5:e1129483. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 97] [Cited by in RCA: 136] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 137. | Greten TF, Forner A, Korangy F, N'Kontchou G, Barget N, Ayuso C, Ormandy LA, Manns MP, Beaugrand M, Bruix J. A phase II open label trial evaluating safety and efficacy of a telomerase peptide vaccination in patients with advanced hepatocellular carcinoma. BMC Cancer. 2010;10:209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 162] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 138. | Lee WC, Wang HC, Hung CF, Huang PF, Lia CR, Chen MF. Vaccination of advanced hepatocellular carcinoma patients with tumor lysate-pulsed dendritic cells: a clinical trial. J Immunother. 2005;28:496-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 141] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 139. | Palmer DH, Midgley RS, Mirza N, Torr EE, Ahmed F, Steele JC, Steven NM, Kerr DJ, Young LS, Adams DH. A phase II study of adoptive immunotherapy using dendritic cells pulsed with tumor lysate in patients with hepatocellular carcinoma. Hepatology. 2009;49:124-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 215] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 140. | Campillo-Davo D, Flumens D, Lion E. The Quest for the Best: How TCR Affinity, Avidity, and Functional Avidity Affect TCR-Engineered T-Cell Antitumor Responses. Cells. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 52] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 141. | Shang N, Figini M, Shangguan J, Wang B, Sun C, Pan L, Ma Q, Zhang Z. Dendritic cells based immunotherapy. Am J Cancer Res. 2017;7:2091-2102. [PubMed] |
| 142. | Silva L, Egea J, Villanueva L, Ruiz M, Llopiz D, Repáraz D, Aparicio B, Lasarte-Cia A, Lasarte JJ, Ruiz de Galarreta M, Lujambio A, Sangro B, Sarobe P. Cold-Inducible RNA Binding Protein as a Vaccination Platform to Enhance Immunotherapeutic Responses Against Hepatocellular Carcinoma. Cancers (Basel). 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 143. | Chen Y, Huang A, Gao M, Yan Y, Zhang W. Potential therapeutic value of dendritic cells loaded with NYESO1 protein for the immunotherapy of advanced hepatocellular carcinoma. Int J Mol Med. 2013;32:1366-1372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 144. | Charneau J, Suzuki T, Shimomura M, Fujinami N, Nakatsura T. Peptide-Based Vaccines for Hepatocellular Carcinoma: A Review of Recent Advances. J Hepatocell Carcinoma. 2021;8:1035-1054. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 145. | Schumacher TN, Scheper W, Kvistborg P. Cancer Neoantigens. Annu Rev Immunol. 2019;37:173-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 404] [Article Influence: 57.7] [Reference Citation Analysis (0)] |
| 146. | Gustafsson K, Ingelsten M, Bergqvist L, Nyström J, Andersson B, Karlsson-Parra A. Recruitment and activation of natural killer cells in vitro by a human dendritic cell vaccine. Cancer Res. 2008;68:5965-5971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 62] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 147. | Rizell M, Sternby Eilard M, Andersson M, Andersson B, Karlsson-Parra A, Suenaert P. Phase 1 Trial With the Cell-Based Immune Primer Ilixadencel, Alone, and Combined With Sorafenib, in Advanced Hepatocellular Carcinoma. Front Oncol. 2019;9:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 148. | Sawada Y, Yoshikawa T, Nobuoka D, Shirakawa H, Kuronuma T, Motomura Y, Mizuno S, Ishii H, Nakachi K, Konishi M, Nakagohri T, Takahashi S, Gotohda N, Takayama T, Yamao K, Uesaka K, Furuse J, Kinoshita T, Nakatsura T. Phase I trial of a glypican-3-derived peptide vaccine for advanced hepatocellular carcinoma: immunologic evidence and potential for improving overall survival. Clin Cancer Res. 2012;18:3686-3696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 233] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 149. | Sun Z, Zhu Y, Xia J, Sawakami T, Kokudo N, Zhang N. Status of and prospects for cancer vaccines against hepatocellular carcinoma in clinical trials. Biosci Trends. 2016;10:85-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 150. | Heo J, Reid T, Ruo L, Breitbach CJ, Rose S, Bloomston M, Cho M, Lim HY, Chung HC, Kim CW, Burke J, Lencioni R, Hickman T, Moon A, Lee YS, Kim MK, Daneshmand M, Dubois K, Longpre L, Ngo M, Rooney C, Bell JC, Rhee BG, Patt R, Hwang TH, Kirn DH. Randomized dose-finding clinical trial of oncolytic immunotherapeutic vaccinia JX-594 in liver cancer. Nat Med. 2013;19:329-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 490] [Cited by in RCA: 613] [Article Influence: 51.1] [Reference Citation Analysis (0)] |
| 151. | Abou-Alfa GK, Galle PR, Chao Y, Brown KT, Heo J, Borad MJ, Luca A, Pelusio A, Agathon D, Lusky M, Breitbach C, Burke J, Qin S. PHOCUS: A phase 3 randomized, open-label study comparing the oncolytic immunotherapy Pexa-Vec followed by sorafenib (SOR) vs SOR in patients with advanced hepatocellular carcinoma (HCC) without prior systemic therapy. J Clin Oncol. 2016;34:TPS4146-TPS4146. [RCA] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 152. | Iwashita Y, Tahara K, Goto S, Sasaki A, Kai S, Seike M, Chen CL, Kawano K, Kitano S. A phase I study of autologous dendritic cell-based immunotherapy for patients with unresectable primary liver cancer. Cancer Immunol Immunother. 2003;52:155-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 93] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 153. | Lee JH, Lee Y, Lee M, Heo MK, Song JS, Kim KH, Lee H, Yi NJ, Lee KW, Suh KS, Bae YS, Kim YJ. A phase I/IIa study of adjuvant immunotherapy with tumour antigen-pulsed dendritic cells in patients with hepatocellular carcinoma. Br J Cancer. 2015;113:1666-1676. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 73] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 154. | Nakagawa H, Mizukoshi E, Kobayashi E, Tamai T, Hamana H, Ozawa T, Kishi H, Kitahara M, Yamashita T, Arai K, Terashima T, Iida N, Fushimi K, Muraguchi A, Kaneko S. Association Between High-Avidity T-Cell Receptors, Induced by α-Fetoprotein-Derived Peptides, and Anti-Tumor Effects in Patients With Hepatocellular Carcinoma. Gastroenterology. 2017;152:1395-1406.e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 67] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 155. | Rowshanravan B, Halliday N, Sansom DM. CTLA-4: a moving target in immunotherapy. Blood. 2018;131:58-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 586] [Cited by in RCA: 834] [Article Influence: 119.1] [Reference Citation Analysis (0)] |
| 156. | Wang PF, Chen Y, Song SY, Wang TJ, Ji WJ, Li SW, Liu N, Yan CX. Immune-Related Adverse Events Associated with Anti-PD-1/PD-L1 Treatment for Malignancies: A Meta-Analysis. Front Pharmacol. 2017;8:730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 231] [Cited by in RCA: 347] [Article Influence: 43.4] [Reference Citation Analysis (0)] |
| 157. | Bertrand A, Kostine M, Barnetche T, Truchetet ME, Schaeverbeke T. Immune related adverse events associated with anti-CTLA-4 antibodies: systematic review and meta-analysis. BMC Med. 2015;13:211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 511] [Cited by in RCA: 520] [Article Influence: 52.0] [Reference Citation Analysis (0)] |
| 158. | De Velasco G, Je Y, Bossé D, Awad MM, Ott PA, Moreira RB, Schutz F, Bellmunt J, Sonpavde GP, Hodi FS, Choueiri TK. Comprehensive Meta-analysis of Key Immune-Related Adverse Events from CTLA-4 and PD-1/PD-L1 Inhibitors in Cancer Patients. Cancer Immunol Res. 2017;5:312-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 358] [Article Influence: 44.8] [Reference Citation Analysis (0)] |
| 159. | Albillos A, Lario M, Álvarez-Mon M. Cirrhosis-associated immune dysfunction: distinctive features and clinical relevance. J Hepatol. 2014;61:1385-1396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 691] [Cited by in RCA: 847] [Article Influence: 77.0] [Reference Citation Analysis (1)] |
| 160. | Sangro B, Park J, Finn R, Cheng A, Mathurin P, Edeline J, Kudo M, Han K, Harding J, Merle P, Rosmorduc O. LBA-3 CheckMate 459: long-term (minimum follow-up 33.6 mo) survival outcomes with nivolumab vs sorafenib as first-line treatment in patients with advanced hepatocellular carcinoma. Ann Oncol. 2020;31:S241-S242. [RCA] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 161. | Simonaggio A, Michot JM, Voisin AL, Le Pavec J, Collins M, Lallart A, Cengizalp G, Vozy A, Laparra A, Varga A, Hollebecque A, Champiat S, Marabelle A, Massard C, Lambotte O. Evaluation of Readministration of Immune Checkpoint Inhibitors After Immune-Related Adverse Events in Patients With Cancer. JAMA Oncol. 2019;5:1310-1317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 275] [Article Influence: 45.8] [Reference Citation Analysis (0)] |
| 162. | Haanen JBAG, Carbonnel F, Robert C, Kerr KM, Peters S, Larkin J, Jordan K; ESMO Guidelines Committee. Management of toxicities from immunotherapy: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28:iv119-iv142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1607] [Cited by in RCA: 1501] [Article Influence: 187.6] [Reference Citation Analysis (1)] |
| 163. | Brahmer JR, Lacchetti C, Schneider BJ, Atkins MB, Brassil KJ, Caterino JM, Chau I, Ernstoff MS, Gardner JM, Ginex P, Hallmeyer S, Holter Chakrabarty J, Leighl NB, Mammen JS, McDermott DF, Naing A, Nastoupil LJ, Phillips T, Porter LD, Puzanov I, Reichner CA, Santomasso BD, Seigel C, Spira A, Suarez-Almazor ME, Wang Y, Weber JS, Wolchok JD, Thompson JA; National Comprehensive Cancer Network. Management of Immune-Related Adverse Events in Patients Treated With Immune Checkpoint Inhibitor Therapy: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2018;36:1714-1768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2245] [Cited by in RCA: 2583] [Article Influence: 369.0] [Reference Citation Analysis (0)] |
| 164. | Abu-Sbeih H, Ali FS, Wang X, Mallepally N, Chen E, Altan M, Bresalier RS, Charabaty A, Dadu R, Jazaeri A, Lashner B, Wang Y. Early introduction of selective immunosuppressive therapy associated with favorable clinical outcomes in patients with immune checkpoint inhibitor-induced colitis. J Immunother Cancer. 2019;7:93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 144] [Article Influence: 24.0] [Reference Citation Analysis (1)] |
| 165. | Qin S, Ren Z, Meng Z, Chen Z, Chai X, Xiong J, Bai Y, Yang L, Zhu H, Fang W, Lin X, Chen X, Li E, Wang L, Chen C, Zou J. Camrelizumab in patients with previously treated advanced hepatocellular carcinoma: a multicentre, open-label, parallel-group, randomised, phase 2 trial. Lancet Oncol. 2020;21:571-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 453] [Cited by in RCA: 425] [Article Influence: 85.0] [Reference Citation Analysis (0)] |