Published online Feb 7, 2023. doi: 10.3748/wjg.v29.i5.815
Peer-review started: September 17, 2022
First decision: November 15, 2022
Revised: December 25, 2022
Accepted: January 20, 2023
Article in press: January 20, 2023
Published online: February 7, 2023
Processing time: 142 Days and 0.9 Hours
Coronavirus disease 2019 (COVID-19) is primarily a respiratory disease with multi-organ involvement, including impaired liver function. It has been noticed that a significant proportion of COVID-19 patients have liver dysfunction, especially those with a more severe disease course. The coronavirus causes direct damage to the liver using the angiotensin-converting enzyme 2, a cell-surface receptor for cellular entry, that is expressed in the liver. According to previous research, liver enzyme abnormalities were observed in a considerable proportion of COVID-19 patients, and elevated liver transaminases were found in about 20% of these patients, alkaline phosphatase in 6.1%, and gamma-glutamyl transferase in 21.1%. COVID-19 might trigger a deterioration of liver function in patients with pre-existing chronic liver diseases (CLDs) and also in those without previous liver disorders. The majority of COVID-19 patients who develop liver injury are men, the elderly, and those with a higher body mass index. Compared to the general population, COVID-19 is associated with significant morbidity and mortality in patients with liver disease (cirrhosis and liver transplantation recipients). However, some studies indicate that CLDs have a lesser role in determining patient progression towards higher disease severity.
Core Tip: Drastic lifestyle changes during the coronavirus disease 2019 (COVID-19) pandemic have led to an increase in the incidence of liver disease. Liver damage in COVID-19 infection occurs during disease progression in patients with or without previous liver disorders and represents a risk factor for developing severe illness and death. The prognosis of COVID-19 infection depends predominantly on the patients’ characteristics, present comorbidities, severity of clinical symptoms, laboratory parameters, and imaging features. It is important to examine prognostic factors in COVID-19 disease patients with liver disease because it may improve the outcome.
- Citation: Vujčić I. Outcomes of COVID-19 among patients with liver disease. World J Gastroenterol 2023; 29(5): 815-824
- URL: https://www.wjgnet.com/1007-9327/full/v29/i5/815.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i5.815
The coronavirus disease (COVID-19) originated in late 2019 in China and spread with alarming rapidity across the globe[1]. The illness is caused by a novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and during the pandemic, more than 600 million cases and more than 6 million deaths were reported worldwide[2]. COVID-19 clinical manifestations vary, and the disease’s wide clinical spectrum ranges from mild, self-limiting pulmonary tract infection to progressive severe pneumonia with high mortality rates[3]. Drastic lifestyle changes during the COVID-19 pandemic have led to an increase in the incidence of nonalcoholic fatty liver disease (NAFLD), decompensated cirrhosis, acute alcoholic hepatitis, viral hepatitis, and mortality from liver diseases[4]. Liver dysfunction in COVID-19 patients is a risk factor for severe illness and death[5], and significantly higher morbidity and mortality rates were observed among patients with liver disease and COVID-19, compared to the general population[6]. About 2%-11% of COVID-19 patients had already been diagnosed with chronic liver disease (CLD)[7]. However, liver dysfunction includes a variety of etiologies and heterogeneous groups of patients[8]. In addition, COVID-19 can induce liver injury, especially in those patients with severe forms of the disease[7,9].
Globally, two million deaths are attributed to liver diseases, including 1 million due to cirrhosis and 1 million due to viral hepatitis and hepatocellular carcinoma (HCC)[10]. Over the past two decades, the prevalence of CLD has been increasing[11]. CLD includes NAFLD, alcohol-related liver disease (ALD), and chronic viral hepatitis B and C[12], and it can progress to fibrosis, cirrhosis, and HCC[13]. NAFLD, or the recently defined metabolic-associated fatty liver disease (MAFLD), are the most common CLDs, which affect about a quarter of the world’s adult population[14]. The global prevalence of MFALD/ NAFLD has been rapidly increasing in tandem with the rise in diabetes and obesity prevalence, both of which have been associated with increased mortality in COVID-19[15,16]. Hepatitis B and C are still a major cause of liver disease burden globally, especially in low-income countries in Asia and sub-Saharan Africa, despite the availability of effective preventive measures and treatment[10,17].
Although coronavirus can cause the worst damage to the lungs, it can also influence the digestive, cardiac, and endocrine systems[18]. Multifactorial causes of liver damage during COVID-19 infection include direct virus cytopathogenic effect, abnormal immune response associated with the cytokine storm, vascular changes due to coagulopathy, hepatic ischemia/hypoxia reperfusion injury, and drug-induced liver injury[19,20]. The coronavirus causes direct liver injury using the angiotensin converting enzyme 2 receptor for cellular entry, which is expressed mainly in the cholangiocytes and less frequently in the hepatocytes[21]. Certain hepatotoxic medications, such as antibiotics (macrolides, quinolones), antivirals (ribavirin), steroids, and other drugs used to treat patients with COVID-19, are connected with drug-induced liver injury and were found in 10.9% of COVID-19 patients[22-24]. However, in COVID-19 patients, liver damage is primarily secondary to ischemic, hypercoagulable, and hyperinflammatory states, which are independent predictors of death rather than liver injury per se[21]. A cytokine storm and a massive acute-phase response are defined by the acute overproduction and uncontrolled release of the proinflammatory cytokines, tumor necrosis factor (TNF), interleukin 1 (IL-1), and IL-6 paralleled by excessive secretion of C-reactive protein (CRP) and ferritin[25]. Coagulation dysfunction indicates a poor outcome in critically ill COVID-19 patients with hepatic injury, including a significant role of neutrophils and monocytes in amplifying blood clotting[20]. Hepatic apoptosis and elevated liver enzymes are caused by ischemia and reperfusion injury[20].
Advanced age and being male are well-established risk factors for severe COVID-19 outcomes[26]. Various medical underlying conditions, such as cardiovascular disease, lung disease, cancer, diabetes, and obesity have also been associated with increased risk[27-29]. However, the prognostic factors in COVID-19 patients with previous liver diseases are not well-defined[9]. In a multicenter cohort study conducted in the United States, comorbidities such as diabetes, hypertension, chronic obstructive pulmonary disease, current smoking and increasing age in patients with ALD, liver cirrhosis decompensation, and HCC predicted a higher mortality when infected with COVID-19[11]. In another study from the United States conducted among CLD patients, it was reported that older age and pre-existing comorbidities were associated with severe COVID-19[30]. Shen et al[31] found that COVID-19 patients with liver injury had a significantly poorer prognosis than patients without liver dysfunction, and that male sex and elevated CRP were independent prognostic factors in these patients[31]. Preliminary results of a systematic review and meta-analysis involving 88 studies and 6653207 cases of COVID-19 in Europe showed that liver disease was associated with hospital admission and mortality, after adjustment for age and sex[32]. Liver dysfunction during COVID-19 has been associated with increased disease severity, prolonged hospital stays, ventilatory support and mortality[33].
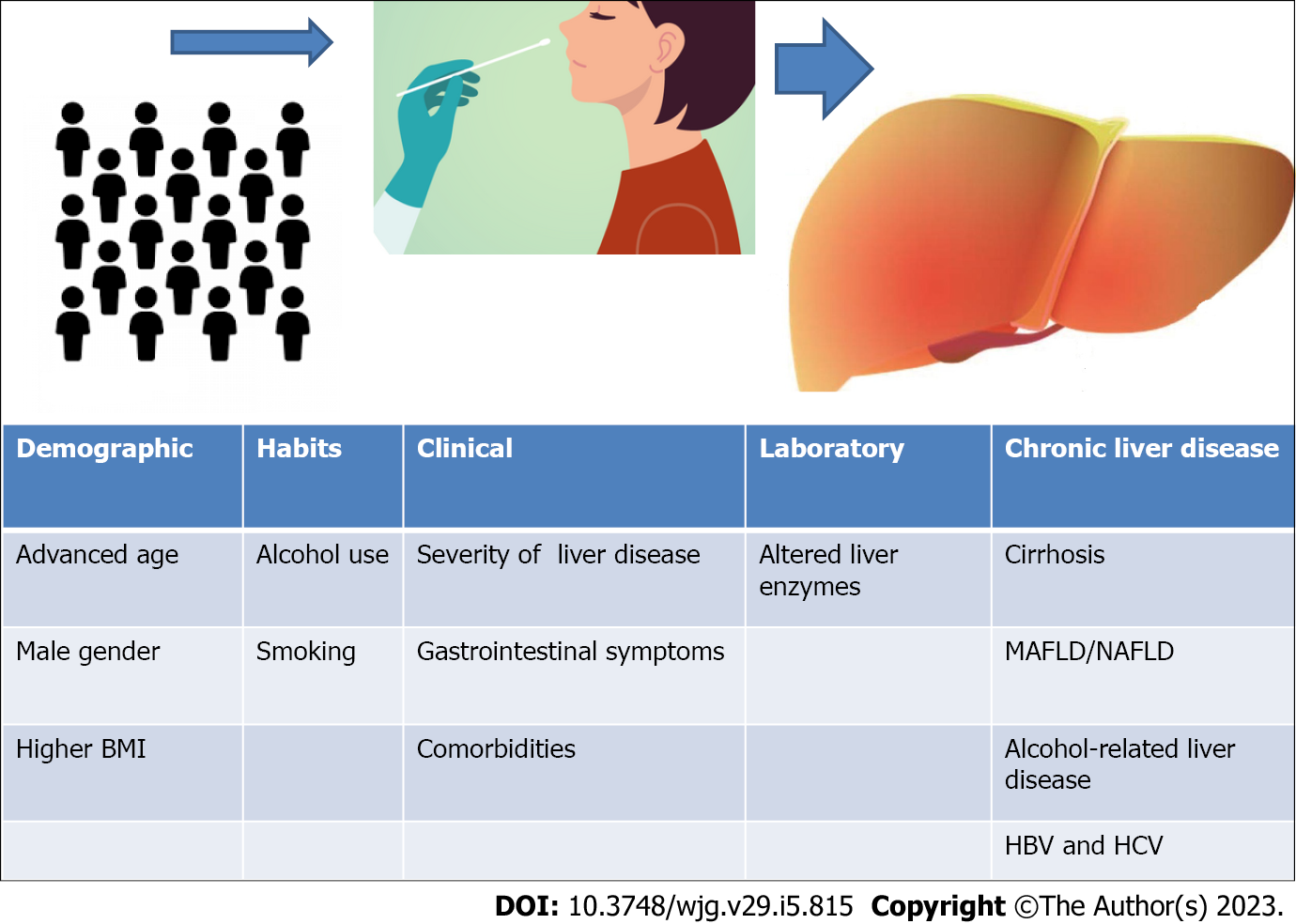
The prognosis of the COVID-19 infection depends primarily on the patients’ characteristics, present comorbidities, severity of clinical symptoms, laboratory parameters, and imaging features[34] (Figure 1). Liver injury occurs in patients with or without pre-existing liver disorders[24]. The incidence of liver injury manifesting as abnormal levels of liver enzymes ranges from 14.8% to 53.0%[18]. The degree of liver injury is generally mild, and those with digestive symptoms were more likely to present hepatocellular injury[3,35,36]. COVID-19 patients who develop liver injury are more likely to be men, older, and have a higher body mass index (BMI)[37]. Liver enzyme abnormalities are frequent in patients with COVID-19 infection, and they are associated with disease severity[18,38]. The most frequently reported mild to moderate elevations were in aspartate aminotransferase (ALT), alanine aminotransferase (AST), and total bilirubin (tBIL) levels[35], but abnormal gamma-glutamyl transferase (GGT), alkaline phosphatase (ALP), and albumin levels have been found in patients with COVID-19 as well[18,22,39]. Liver damage in COVID-19 is usually temporary, and therefore, the enzyme levels of most patients usually return to normal after recovery[18,40]. The systematic review and meta-analysis that included 36 studies and 20724 patients found a 46.9% prevalence of at least one abnormal liver function test, and elevated levels of ALT, AST, and tBIL were independent predictors of COVID-19 severity and in-hospital mortality[41]. A meta-analysis of observational studies revealed that acute liver injury and elevated liver enzymes in COVID-19 patients were significantly associated with disease severity[42]. A study conducted in Hong Kong reported that, ALT/AST elevation at two times the upper normal limit and acute liver injury in patients with COVID-19, were independently associated with poor prognosis, after controlling for diabetes mellitus, hypertension, and albumin level[43]. A systematic review that included 30 articles observed a significantly higher mortality in patients with impaired liver function than in patients with normal function[36]. Wagner et al[44] reported that hypoalbuminemia and abnormalities in liver function tests may be prognostic factors for higher COVID-19 severity. Although, there remains controversy in the scientific literature over whether or not liver enzyme abnormalities are associated with worse clinical outcomes, their alteration probably reflects the systemic involvement of the virus and the potential appearance of severe liver complications[45]. However, patients with severe COVID-19 may show a higher risk of post-COVID cholangiopathy, and liver tests in these patients continue to show abnormal results[46].
A number of studies have investigated the impact of CLD on the outcome of COVID-19[8]. COVID-19 patients with CLD account for less than 1% of the reported cases[47]. CLD includes different etiologies and can manifest from mild asymptomatic disease to severe decompensated cirrhosis, so it could be challenging to generalize results from different studies and countries[11,17]. In China, the main cirrhosis etiology was chronic hepatitis B virus (HBV)[48]. Patients with viral hepatitis, ALD, NFALD, liver cirrhosis, and HCC had a higher risk of developing severe COVID-19 and up to a 10-fold higher mortality rate compared to those without any reported comorbidity[49]. Data collected from 13 Asian countries identified that COVID-19 infection induced significant liver damage in CLD patients, and these patients had a higher risk of getting acute liver injury, hepatic decompensation, or acute-on-chronic liver failure (ACLF)[50]. A Danish prospective, population-based cohort study reported that patients with CLD, particularly those with cirrhosis, were at a major risk of severe COVID-19 outcomes and higher mortality[51]. A Swedish nationwide matched cohort study showed that patients with CLD had a higher risk of hospitalization for COVID-19 compared to the general population[52]. However, there was no evidence that these patients were at a higher risk of developing a severe COVID-19 disease course[52]. A study conducted in China reported that COVID-19 patients with CLD showed a prolonged length of stay, slight liver injuries, and higher mortality rates compared to COVID-19 patients without CLD, and that the neutrophil-to-lymphocyte ratio was an indicator of adverse clinical outcomes in this population[53]. A meta-analysis that included fifty studies revealed that pre-existing liver diseases or acute liver injury associated with severe COVID-19 infection were key factors in the prediction of mortality[54]. According to a study conducted in Massachusetts, United States, CLD in patients with COVID-19 was independently associated with higher rates of intensive care unit (ICU) admission, and a need for mechanical ventilation after controlling for comorbidities[12]. Krishnan et al[30] found that CLD patients with elevated AST and tBIL levels had a significantly higher risk fora more severe COVID-19 disease course and also reported that ALD was the most important factor associated with the need for mechanical ventilation. A systematic review including 40 studies, mainly from China, reported that CLD was significantly associated with COVID-19 severity and mortality[55]. The risk of getting more severe COVID-19 was 2.44 times higher among patients with CLD compared to those without CLD, and the presence of NAFLD was the most strongly associated with higher COVID-19 severity, followed by MAFLD and cirrhosis. In addition, COVID-19 patients with viral hepatitis were not at higher risk of getting a severe form of COVID-19[55]. After COVID-19 infection, approximately 20% of CLD patients develop progressive cholestasis, particularly patients with NAFLD/non-alcoholic steatohepatitis and metabolic risk factors[56].
There is still insufficient evidence for an association between previous hepatitis B and C infection and COVID-19 outcome, and several studies indicated that these patients were not at increased risk for severe COVID-19[57-59]. Most studies that have examined the influence of HBV on COVID-19 prognosis have been conducted in China due to the high prevalence of HBV in the country[60]. Yu et al[61] reported higher in-hospital mortality, more severe disease, and liver function abnormalities in COVID-19 patients infected with HBV compared to COVID-19 patients without HBV. However, the presence of COVID-19 infection or treatment with tocilizumab or corticosteroids could reactivate hepatitis B infection[49,62]. A study conducted in the United States reported that chronic hepatitis C in COVID-19 patients was associated with in-hospital mortality regardless of baseline comorbidities, admission values of laboratory tests, or liver damage induced by COVID-19[63]. The Korean nationwide population-based cohort study reported that after adjusting for age, sex, cirrhosis, and comorbidities, HBV infection itself appears not to influence the prognosis of COVID-19 patients[64].
The prevalence of NAFLD, or the recently renamed MAFLD, in COVID-19 patients is 31%, which is higher than the prevalence in the general population[65]. Patients with NAFLD had a higher risk of COVID-19 progression, a higher likelihood of liver dysfunction, and a longer viral shedding time than the patients without NAFLD[66]. Mahamid et al[16] found an independent association between the COVID-19 severity and NAFLD irrespective of the metabolic syndrome, indicating that NAFLD had a significant impact even in the absence of obesity and/or metabolic syndrome. A systematic review and meta-analysis showed that the proportion of patients with MAFLD and NAFLD ranged from 28% to 50% and from 6% to 38%, respectively, and found that the presence of MAFLD and NAFLD was associated with worse clinical outcomes for COVID-19[67]. Although several studies also showed significant associations between MAFLD and NAFLD and severe COVID-19 outcomes[13,68], there is still no strong evidence that the presence of MAFLD affects its prognosis[65].
The COVID-19 pandemic probably had the biggest effect on patients with ALD due to substantially increased alcohol consumption provoked by adverse economic effects, disruptions in work and education, and social isolation[69]. Patients with alcohol use disorders are more likely to develop acute respiratory distress syndrome and have additional comorbidities such as metabolic syndrome, chronic kidney disease, and smoking, all of which are independent predictors of COVID-19 severity[69]. Several studies have identified that ALD is independently associated with COVID-19 mortality after adjustment for important cofactors such as liver disease severity[11,70].
COVID-19 patients with cirrhosis are at a greater risk of adverse outcomes than the background population[26,71,72]. Cirrhotic patients have significantly higher all-cause mortality in COVID-19 infection than non-cirrhotic patients, and mortality is probably higher in those with more advanced cirrhosis[8]. A significantly higher COVID-19 related morbidity and mortality had been observed in patients with decompensated cirrhosis compared to those with compensated cirrhosis[6]. Studies conducted in the United States and Europe reported that patients with CLD who had acquired COVID-19 had high rates of hospitalization and mortality[71,73,74]. Marjot et al[70] reported that patients with cirrhosis had a higher risk of dying from COVID-19 and that mortality was especially high among patients with more advanced cirrhosis and those with ALD. Hashemi et al[12] demonstrated that the presence of cirrhosis was independently associated with COVID-19-related mortality. Similar results were obtained from the United States study, reporting that the presence of decompensated cirrhosis was an independent predictor of mortality in COVID-19 patients[30]. Jeon et al[75] reported that the COVID-19 infection in patients with cirrhosis was more likely to cause severe complications in comparison with the cirrhotic patients not infected with COVID-19. Satapathy et al[76] found that the development of ACLF was the most important predictor of higher in-hospital mortality in COVID-19 patients with cirrhosis. However, it is still unknown whether the presence of liver disease influences the natural history of COVID-19 infection in cirrhotic patients[21].
The presence of HCC in patients with CLD and COVID-19 infection was associated with a poor prognosis, including a higher risk of all-cause and COVID-19-related mortality[11]. Most HCC patients have concomitant cirrhosis, and that could potentially increase their risk for severe COVID-19[77]. An international, multicenter, retrospective, cross-sectional study, including two hundred fifty patients from 38 centers, reported that 18.4% of patients with HCC died within the first 30 d from the onset of COVID-19 symptoms, and that the mortality rate in that period was 20.25% in patients with HCC history and 12.96% in those with de novo HCC[78]. COVID-19 in HCC patients tends to be more severe and leads to exacerbation of the liver disease[79]. HCC patients infected with COVID-19 are at a higher risk of complications, ICU admission, and death than the patients without cancer[80].
Autoimmune liver disease (AILD) includes primary sclerosing cholangitis, primary biliary cholangitis (PBC), autoimmune hepatitis (AIH), and overlapping syndromes referring to the coexistence of two autoimmune diseases[81]. COVID-19 outcomes in patients with AILD were investigated in international registry studies and retrospective case studies[82]. Combined data from three multinational registries showed that despite the use of immunosuppressive treatment, AIH patients did not seem to have a higher risk of lethal outcomes with COVID-19 compared to patients without liver disease and those with other forms of liver disease[83]. A retrospective study from 34 centers in Europe and the Americas indicated that patients with AIH did not have an increased risk for poor prognosis with COVID-19 than other causes of CLD and that cirrhosis was the most important predictor for high COVID-19 severity in this group of patients[84]. Zecher et al[85] indicated that patients with AILD were not at elevated risk for COVID-19. A Spanish nationwide study reported that cumulative incidences of hospitalization and COVID-19 related mortality were greater in patients with PBC than in the general Spanish population, although the results were not adjusted for other comorbidities[86].
Although the presence of COVID-19 infection in CLD patients is associated with a poor prognosis, including severity and mortality, these results should be interpreted with caution and need to be evaluated in large future studies. Such findings could be explained by overlapping risk factors, therapeutic effort limitations, different etiologies, and the disease spectrum of CLD, which ranges from mild asymptomatic disease to severe decompensated cirrhosis. Cirrhosis severity and older age are the most important predictors of mortality[21]. A French national retrospective cohort study found no increased COVID-19 severity in patients with CLD, alcohol use disorders, cirrhosis, or primary liver cancer, indicating that the COVID-19 outcome in these patients may be more associated with therapeutic effort such as mechanical ventilation and less with liver disease progression or ethanol toxicity[87]. This group of patients was at an elevated risk for mortality from COVID-19 within 30 d after admission but was less likely to need mechanical ventilation[87] in comparison with patients with mild liver diseases, compensated cirrhosis, chronic viral hepatitis, non-viral, non-alcoholic causes of CLD, acquired immunodeficiency syndrome, and liver transplantation, who were not at a higher risk of dying from COVID-19 but were more likely to receive mechanical ventilation[87]. As mentioned earlier, the Swedish nationwide cohort study also did not find an increased risk of getting severe COVID-19 in CLD patients, although they had an increased risk of hospitalization than the background population[52]. The pooled analysis of six studies found that CLD was not related to an elevated risk of a more severe COVID-19 disease course or mortality[88]. Similar results were reported from a nationwide Korean cohort study indicating that LC was not an independent predictor of severe complications, including mortality, in COVID-19 patients and depended on age, hypertension, cancer, chronic obstructive pulmonary disease, and a higher Charlson comorbidity index[75]. After adjustment for age, sex, BMI, cardiac disease, hypertension, diabetes, and respiratory disorders, CLD, and NAFLD were independently associated with ICU admission and the need for mechanical ventilation, but not death[12].
Due to the era of the COVID-19 pandemic and the large number of patients with liver disease, it is very important to study the impact of liver damage on the prognosis of patients with COVID-19 and the predictors that may affect the outcome. Identifying predictors of mortality could allow for risk stratification of patients and help improve healthcare delivery[11]. Therefore, it is necessary to improve the understanding of host genetics, behavior, and pre-existing comorbidities and adequately follow-up liver disease patients[17]. Patients with CLD, especially those with cirrhosis or advanced liver damage, should be prioritized for COVID-19 vaccination[89].
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Serbia
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ariyachet C, Thailand; El-Gendy HA, Egypt; Sitkin S, Russia S-Editor: Chen YL L-Editor: Filipodia P-Editor: Chen YL
| 1. | European Centre for Disease Prevention and Control. COVID-19. [cited 3 December 2022]. Available from: https://www.ecdc.europa.eu/en. |
| 2. | World Health Organization. Coronavirus disease (COVID-19). [cited 3 December 2022]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. |
| 3. | Garrido M, Pereira Guedes T, Alves Silva J, Falcão D, Novo I, Archer S, Rocha M, Maia L, Sarmento-Castro R, Pedroto I. Impact of Liver Test Abnormalities and Chronic Liver Disease on the Clinical Outcomes of Patients Hospitalized with COVID-19. GE Port J Gastroenterol. 2021;158:1-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Mikolasevic I, Bozic D, Pavić T, Ruzic A, Hauser G, Radic M, Radic-Kristo D, Razov-Radas M, Puljiz Z, Milic S. Liver disease in the era of COVID-19: Is the worst yet to come? World J Gastroenterol. 2021;27:6039-6052. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Jaiswal V, Naz S, Ishak A, Batra N, Quinonez J, Mukherjee D, Pokhrel NB. A rare case of pediatric pancreatic pseudocyst. Clin Case Rep. 2022;10:e05879. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 6. | Choudhary NS, Dhampalwar S, Saraf N, Soin AS. Outcomes of COVID-19 in Patients with Cirrhosis or Liver Transplantation. J Clin Exp Hepatol. 2021;11:713-719. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 7. | Jothimani D, Venugopal R, Abedin MF, Kaliamoorthy I, Rela M. COVID-19 and the liver. J Hepatol. 2020;73:1231-1240. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 364] [Cited by in RCA: 358] [Article Influence: 71.6] [Reference Citation Analysis (1)] |
| 8. | Middleton P, Hsu C, Lythgoe MP. Clinical outcomes in COVID-19 and cirrhosis: a systematic review and meta-analysis of observational studies. BMJ Open Gastroenterol. 2021;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 9. | Bahardoust M, Heiat M, Khodabandeh M, Karbasi A, Bagheri-Hosseinabadi Z, Ataee MH, Seidalian N, Babazadeh A, Agah S, Abyazi MA. Predictors for the severe coronavirus disease 2019 (COVID-19) infection in patients with underlying liver disease: a retrospective analytical study in Iran. Sci Rep. 2021;11:3066. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019;70:151-171. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1382] [Cited by in RCA: 2291] [Article Influence: 381.8] [Reference Citation Analysis (0)] |
| 11. | Kim D, Adeniji N, Latt N, Kumar S, Bloom PP, Aby ES, Perumalswami P, Roytman M, Li M, Vogel AS, Catana AM, Wegermann K, Carr RM, Aloman C, Chen VL, Rabiee A, Sadowski B, Nguyen V, Dunn W, Chavin KD, Zhou K, Lizaola-Mayo B, Moghe A, Debes J, Lee TH, Branch AD, Viveiros K, Chan W, Chascsa DM, Kwo P, Dhanasekaran R. Predictors of Outcomes of COVID-19 in Patients With Chronic Liver Disease: US Multi-center Study. Clin Gastroenterol Hepatol. 2021;19:1469-1479.e19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 176] [Cited by in RCA: 184] [Article Influence: 46.0] [Reference Citation Analysis (0)] |
| 12. | Hashemi N, Viveiros K, Redd WD, Zhou JC, McCarty TR, Bazarbashi AN, Hathorn KE, Wong D, Njie C, Shen L, Chan WW. Impact of chronic liver disease on outcomes of hospitalized patients with COVID-19: A multicentre United States experience. Liver Int. 2020;40:2515-2521. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 117] [Article Influence: 23.4] [Reference Citation Analysis (2)] |
| 13. | Hayat U, Ashfaq MZ, Johnson L, Ford R, Wuthnow C, Kadado K, El Jurdi K, Okut H, Kilgore WR, Assi M, Siddiqui AA. The Association of Metabolic-Associated Fatty Liver Disease with Clinical Outcomes of COVID-19: A Systematic Review and Meta-Analysis. Kans J Med. 2022;15:241-246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 14. | Eslam M, Sanyal AJ, George J; International Consensus Panel. MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology. 2020;158:1999-2014.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2367] [Cited by in RCA: 2205] [Article Influence: 441.0] [Reference Citation Analysis (1)] |
| 15. | Testino G. Covid-19 infection, liver injury and prognosis: a suggestion. Eur J Gastroenterol Hepatol. 2021;33:451-452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Mahamid M, Nseir W, Khoury T, Mahamid B, Nubania A, Sub-Laban K, Schifter J, Mari A, Sbeit W, Goldin E. Nonalcoholic fatty liver disease is associated with COVID-19 severity independently of metabolic syndrome: a retrospective case-control study. Eur J Gastroenterol Hepatol. 2021;33:1578-1581. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 68] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 17. | Fierro NA. COVID-19 and the liver: What do we know after six months of the pandemic? Ann Hepatol. 2020;19:590-591. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 18. | Wang X, Lei J, Li Z, Yan L. Potential Effects of Coronaviruses on the Liver: An Update. Front Med (Lausanne). 2021;8:651658. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 19. | Ozkurt Z, Çınar Tanrıverdi E. COVID-19: Gastrointestinal manifestations, liver injury and recommendations. World J Clin Cases. 2022;10:1140-1163. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 29] [Cited by in RCA: 26] [Article Influence: 8.7] [Reference Citation Analysis (7)] |
| 20. | Elghannam MT, Hassanien MH, Ameen YA, ELattar GM, ELRay AA, Turky EA, ELTalkawy MD. COVID-19 and liver diseases. Egypt Liver J. 2022;12:43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 21. | Russo FP, Burra P, Zanetto A. COVID-19 and liver disease: where are we now? Nat Rev Gastroenterol Hepatol. 2022;19:277-278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 22. | Taneva G, Dimitrov D, Velikova T. Liver dysfunction as a cytokine storm manifestation and prognostic factor for severe COVID-19. World J Hepatol. 2021;13:2005-2012. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 23. | Wu J, Song S, Cao HC, Li LJ. Liver diseases in COVID-19: Etiology, treatment and prognosis. World J Gastroenterol. 2020;26:2286-2293. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 105] [Cited by in RCA: 97] [Article Influence: 19.4] [Reference Citation Analysis (1)] |
| 24. | Kanda T, Sasaki-Tanaka R, Ishii T, Abe H, Ogawa M, Enomoto H. Acute Liver Failure and Acute-on-Chronic Liver Failure in COVID-19 Era. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Reference Citation Analysis (0)] |
| 25. | Dufour JF, Marjot T, Becchetti C, Tilg H. COVID-19 and liver disease. Gut. 2022;71:2350-2362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 53] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 26. | Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, Curtis HJ, Mehrkar A, Evans D, Inglesby P, Cockburn J, McDonald HI, MacKenna B, Tomlinson L, Douglas IJ, Rentsch CT, Mathur R, Wong AYS, Grieve R, Harrison D, Forbes H, Schultze A, Croker R, Parry J, Hester F, Harper S, Perera R, Evans SJW, Smeeth L, Goldacre B. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430-436. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4343] [Cited by in RCA: 4205] [Article Influence: 841.0] [Reference Citation Analysis (0)] |
| 27. | Deng G, Yin M, Chen X, Zeng F. Clinical determinants for fatality of 44,672 patients with COVID-19. Crit Care. 2020;24:179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 190] [Cited by in RCA: 413] [Article Influence: 82.6] [Reference Citation Analysis (0)] |
| 28. | Figliozzi S, Masci PG, Ahmadi N, Tondi L, Koutli E, Aimo A, Stamatelopoulos K, Dimopoulos MA, Caforio ALP, Georgiopoulos G. Predictors of adverse prognosis in COVID-19: A systematic review and meta-analysis. Eur J Clin Invest. 2020;50:e13362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 225] [Article Influence: 45.0] [Reference Citation Analysis (0)] |
| 29. | Yang J, Tian C, Chen Y, Zhu C, Chi H, Li J. Obesity aggravates COVID-19: An updated systematic review and meta-analysis. J Med Virol. 2021;93:2662-2674. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 106] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 30. | Krishnan A, Prichett L, Liu Y, Ting PS, Alqahtani SA, Kim AK, Ma M, Hamilton JP, Woreta TA, Chen PH. Risk of Severe Illness and Risk Factors of Outcomes of COVID-19 in Hospitalized Patients with Chronic Liver Disease in a Major U. S. Hospital Network. Can J Gastroenterol Hepatol. 2022;2022:8407990. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 31. | Shen JX, Zhuang ZH, Zhang QX, Huang JF, Chen GP, Fang YY, Cheng AG. Risk Factors and Prognosis in Patients with COVID-19 and Liver Injury: A Retrospective Analysis. J Multidiscip Healthc. 2021;14:629-637. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 32. | Vardavas CI, Mathioudakis AG, Nikitara K, Stamatelopoulos K, Georgiopoulos G, Phalkey R, Leonardi-Bee J, Fernandez E, Carnicer-Pont D, Vestbo J, Semenza JC, Deogan C, Suk JE, Kramarz P, Lamb F, Penttinen P. Prognostic factors for mortality, intensive care unit and hospital admission due to SARS-CoV-2: a systematic review and meta-analysis of cohort studies in Europe. Eur Respir Rev. 2022;31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 63] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 33. | Ortega-Quiroz RJ. COVID-19 and Liver Disease: A panorama that is being clarified. Rev Colomb Gastroenterol. 2022;37:131-135. [DOI] [Full Text] |
| 34. | Besteiro B, Coutinho D, Gomes F, Almeida M. Almeida J. Review of the Prognosis Factors of COVID-19 Infection. Adv Infec Dis. 2021;11:196-215. [DOI] [Full Text] |
| 35. | Kariyawasam JC, Jayarajah U, Abeysuriya V, Riza R, Seneviratne SL. Involvement of the Liver in COVID-19: A Systematic Review. Am J Trop Med Hyg. 2022;106:1026-1041. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 36. | Almeida-Costa T, Cunha-Lima MA, Kniess I, Marques-Vieira L, Delmondes-Freitas LD. Changes in liver function tests caused by COVID-19 and impact on patient outcome: a systematic review. Rev Colomb Gastroenterol. 2021;36:302-312. [DOI] [Full Text] |
| 37. | Cichoż-Lach H, Michalak A. Liver injury in the era of COVID-19. World J Gastroenterol. 2021;27:377-390. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 53] [Cited by in RCA: 51] [Article Influence: 12.8] [Reference Citation Analysis (2)] |
| 38. | Wu Y, Li H, Guo X, Yoshida EM, Mendez-Sanchez N, Levi Sandri GB, Teschke R, Romeiro FG, Shukla A, Qi X. Incidence, risk factors, and prognosis of abnormal liver biochemical tests in COVID-19 patients: a systematic review and meta-analysis. Hepatol Int. 2020;14:621-637. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 81] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 39. | Tokarczyk U, Kaliszewski K, Kopszak A, Nowak Ł, Sutkowska-Stępień K, Sroczyński M, Sępek M, Dudek A, Diakowska D, Trocha M, Gajecki D, Gawryś J, Matys T, Maciejiczek J, Kozub V, Szalast R, Madziarski M, Zubkiewicz-Zarębska A, Letachowicz K, Kiliś-Pstrusińska K, Matera-Witkiewicz A, Pomorski M, Protasiewicz M, Sokołowski J, Adamik B, Kujawa K, Doroszko A, Madziarska K, Jankowska EA. Liver Function Tests in COVID-19: Assessment of the Actual Prognostic Value. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Reference Citation Analysis (1)] |
| 40. | Liao X, Li D, Ma Z, Zhang L, Zheng B, Li Z, Li G, Liu L, Zhang Z. 12-Month Post-Discharge Liver Function Test Abnormalities Among Patients With COVID-19: A Single-Center Prospective Cohort Study. Front Cell Infect Microbiol. 2022;12:864933. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 41. | Del Zompo F, De Siena M, Ianiro G, Gasbarrini A, Pompili M, Ponziani FR. Prevalence of liver injury and correlation with clinical outcomes in patients with COVID-19: systematic review with meta-analysis. Eur Rev Med Pharmacol Sci. 2020;24:13072-13088. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 42. | Sharma A, Jaiswal P, Kerakhan Y, Saravanan L, Murtaza Z, Zergham A, Honganur NS, Akbar A, Deol A, Francis B, Patel S, Mehta D, Jaiswal R, Singh J, Patel U, Malik P. Liver disease and outcomes among COVID-19 hospitalized patients - A systematic review and meta-analysis. Ann Hepatol. 2021;21:100273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 81] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 43. | Yip TC, Lui GC, Wong VW, Chow VC, Ho TH, Li TC, Tse YK, Hui DS, Chan HL, Wong GL. Liver injury is independently associated with adverse clinical outcomes in patients with COVID-19. Gut. 2021;70:733-742. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 119] [Cited by in RCA: 123] [Article Influence: 30.8] [Reference Citation Analysis (0)] |
| 44. | Wagner J, Garcia-Rodriguez V, Yu A, Dutra B, Larson S, Cash B, DuPont A, Farooq A. Elevated transaminases and hypoalbuminemia in Covid-19 are prognostic factors for disease severity. Sci Rep. 2021;11:10308. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 45. | Quintero-Marzola ID, Fontalvo-Mendoza MF, Cárdenas-Gómez JC, Quintana-Pájaro LJ, Ramos-Villegas Y, Manzur-Jattin F, Yepes IJ, Sibaja-Pérez AE. Liver and SARS-CoV-2: Literature key aspects. Rev Colomb Gastroenterol. 2021;36:485-493. [DOI] [Full Text] |
| 46. | Rojas M, Rodríguez Y, Zapata E, Hernández JC, Anaya JM. Cholangiopathy as part of post-COVID syndrome. J Transl Autoimmun. 2021;4:100116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 47. | Elghannam MT, Hassanien MH, Abdelrahman Y, ALattar GM, Turky EA, EL Ray AA, EL Talkawy MD. (2021) COVID-19 and Chronic Viral Liver Diseases. J Biosci Med. 2021;9:138-146. [DOI] [Full Text] |
| 48. | Qi X, Liu Y, Wang J, Fallowfield JA, Li X, Shi J, Pan H, Zou S, Zhang H, Chen Z, Li F, Luo Y, Mei M, Liu H, Wang Z, Li J, Yang H, Xiang H, Liu T, Zheng MH, Liu C, Huang Y, Xu D, Kang N, He Q, Gu Y, Zhang G, Shao C, Liu D, Zhang L, Kawada N, Jiang Z, Wang F, Xiong B, Takehara T, Rockey DC; COVID-Cirrhosis-CHESS Group. Clinical course and risk factors for mortality of COVID-19 patients with pre-existing cirrhosis: a multicentre cohort study. Gut. 2021;70:433-436. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 71] [Article Influence: 17.8] [Reference Citation Analysis (1)] |
| 49. | Taye BW, Valery PC, Clark PJ. Protecting persons at-risk of viral hepatitis and alcohol-related liver disease during the pandemic and beyond: mitigating the impact of coronavirus disease 2019 on liver health. J Glob Health Rep. 2021;5:e2021060. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 50. | Sarin SK, Choudhury A, Lau GK, Zheng MH, Ji D, Abd-Elsalam S, Hwang J, Qi X, Cua IH, Suh JI, Park JG, Putcharoen O, Kaewdech A, Piratvisuth T, Treeprasertsuk S, Park S, Wejnaruemarn S, Payawal DA, Baatarkhuu O, Ahn SH, Yeo CD, Alonzo UR, Chinbayar T, Loho IM, Yokosuka O, Jafri W, Tan S, Soo LI, Tanwandee T, Gani R, Anand L, Esmail ES, Khalaf M, Alam S, Lin CY, Chuang WL, Soin AS, Garg HK, Kalista K, Batsukh B, Purnomo HD, Dara VP, Rathi P, Al Mahtab M, Shukla A, Sharma MK, Omata M; APASL COVID Task Force, APASL COVID Liver Injury Spectrum Study (APCOLIS Study-NCT 04345640). Pre-existing liver disease is associated with poor outcome in patients with SARS CoV2 infection; The APCOLIS Study (APASL COVID-19 Liver Injury Spectrum Study). Hepatol Int. 2020;14:690-700. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 217] [Cited by in RCA: 216] [Article Influence: 43.2] [Reference Citation Analysis (1)] |
| 51. | Dahlin P, Nagras ZG, Attauabi M, Burisch J, Bendtsen F, Kimer N. Outcomes of COVID-19 among Patients with Chronic Liver Disease: A Danish Prospective, Population-Based Cohort Study. GastroHep. 2022;2022. [DOI] [Full Text] |
| 52. | Simon TG, Hagström H, Sharma R, Söderling J, Roelstraete B, Larsson E, Ludvigsson JF. Risk of severe COVID-19 and mortality in patients with established chronic liver disease: a nationwide matched cohort study. BMC Gastroenterol. 2021;21:439. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 53. | Li C, Chen Q, Wang J, Lin H, Lin Y, Lin J, Peng F, Chen J, Yang Z. Clinical characteristics of chronic liver disease with coronavirus disease 2019 (COVID-19): a cohort study in Wuhan, China. Aging (Albany NY). 2020;12:15938-15945. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 54. | Váncsa S, Hegyi PJ, Zádori N, Szakó L, Vörhendi N, Ocskay K, Földi M, Dembrovszky F, Dömötör ZR, Jánosi K, Rakonczay Z Jr, Hartmann P, Horváth T, Erőss B, Kiss S, Szakács Z, Németh D, Hegyi P, Pár G. Pre-existing Liver Diseases and On-Admission Liver-Related Laboratory Tests in COVID-19: A Prognostic Accuracy Meta-Analysis With Systematic Review. Front Med (Lausanne). 2020;7:572115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 55. | Nagarajan R, Krishnamoorthy Y, Rajaa S, Hariharan VS. COVID-19 Severity and Mortality Among Chronic Liver Disease Patients: A Systematic Review and Meta-Analysis. Prev Chronic Dis. 2022;19:E53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 51] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 56. | Hartl L, Haslinger K, Angerer M, Semmler G, Schneeweiss-Gleixner M, Jachs M, Simbrunner B, Bauer DJM, Eigenbauer E, Strassl R, Breuer M, Kimberger O, Laxar D, Lampichler K, Halilbasic E, Stättermayer AF, Ba-Ssalamah A, Mandorfer M, Scheiner B, Reiberger T, Trauner M. Progressive cholestasis and associated sclerosing cholangitis are frequent complications of COVID-19 in patients with chronic liver disease. Hepatology. 2022;76:1563-1575. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 56] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 57. | Mani I, Alexopoulou A. Recent challenges facing patients with preexisting chronic liver disease in the era of the COVID-19 pandemic. Ann Gastroenterol. 2021;34:625-633. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 58. | Zhang B, Huang W, Zhang S. Clinical Features and Outcomes of Coronavirus Disease 2019 (COVID-19) Patients With Chronic Hepatitis B Virus Infection. Clin Gastroenterol Hepatol. 2020;18:2633-2637. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 59. | Liu R, Zhao L, Cheng X, Han H, Li C, Li D, Liu A, Gao G, Zhou F, Liu F, Jiang Y, Zhu C, Xia Y. Clinical characteristics of COVID-19 patients with hepatitis B virus infection - a retrospective study. Liver Int. 2021;41:720-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 60. | Kang SH, Cho DH, Choi J, Baik SK, Gwon JG, Kim MY. Association between chronic hepatitis B infection and COVID-19 outcomes: A Korean nationwide cohort study. PLoS One. 2021;16:e0258229. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 61. | Yu Y, Li X, Wan T. Effects of Hepatitis B Virus Infection on Patients with COVID-19: A Meta-Analysis. Dig Dis Sci. 2022;1-17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 62. | Alqahtani SA, Buti M. COVID-19 and hepatitis B infection. Antivir Ther. 2020;25:389-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 63. | Ronderos D, Omar AMS, Abbas H, Makker J, Baiomi A, Sun H, Mantri N, Choi Y, Fortuzi K, Shin D, Patel H, Chilimuri S. Chronic hepatitis-C infection in COVID-19 patients is associated with in-hospital mortality. World J Clin Cases. 2021;9:8749-8762. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 21] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 64. | Choe JW, Jung YK, Yim HJ, Seo GH. Clinical Effect of Hepatitis B Virus on COVID-19 Infected Patients: A Nationwide Population-Based Study Using the Health Insurance Review & Assessment Service Database. J Korean Med Sci. 2022;37:e29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 65. | Xu Y, Yang X, Bian H, Xia M. Metabolic dysfunction associated fatty liver disease and coronavirus disease 2019: clinical relationship and current management. Lipids Health Dis. 2021;20:126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 66. | Ji D, Qin E, Xu J, Zhang D, Cheng G, Wang Y, Lau G. Non-alcoholic fatty liver diseases in patients with COVID-19: A retrospective study. J Hepatol. 2020;73:451-453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 336] [Cited by in RCA: 408] [Article Influence: 81.6] [Reference Citation Analysis (2)] |
| 67. | Hegyi PJ, Váncsa S, Ocskay K, Dembrovszky F, Kiss S, Farkas N, Erőss B, Szakács Z, Hegyi P, Pár G. Metabolic Associated Fatty Liver Disease Is Associated With an Increased Risk of Severe COVID-19: A Systematic Review With Meta-Analysis. Front Med (Lausanne). 2021;8:626425. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 55] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 68. | Vrsaljko N, Samadan L, Viskovic K, Mehmedović A, Budimir J, Vince A, Papic N. Association of Nonalcoholic Fatty Liver Disease With COVID-19 Severity and Pulmonary Thrombosis: CovidFAT, a Prospective, Observational Cohort Study. Open Forum Infect Dis. 2022;9:ofac073. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 22] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 69. | Moon AM, Curtis B, Mandrekar P, Singal AK, Verna EC, Fix OK. Alcohol-Associated Liver Disease Before and After COVID-19-An Overview and Call for Ongoing Investigation. Hepatol Commun. 2021;5:1616-1621. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 70. | Marjot T, Moon AM, Cook JA, Abd-Elsalam S, Aloman C, Armstrong MJ, Pose E, Brenner EJ, Cargill T, Catana MA, Dhanasekaran R, Eshraghian A, García-Juárez I, Gill US, Jones PD, Kennedy J, Marshall A, Matthews C, Mells G, Mercer C, Perumalswami PV, Avitabile E, Qi X, Su F, Ufere NN, Wong YJ, Zheng MH, Barnes E, Barritt AS 4th, Webb GJ. Outcomes following SARS-CoV-2 infection in patients with chronic liver disease: An international registry study. J Hepatol. 2021;74:567-577. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 399] [Cited by in RCA: 384] [Article Influence: 96.0] [Reference Citation Analysis (0)] |
| 71. | Singh S, Khan A. Clinical Characteristics and Outcomes of Coronavirus Disease 2019 Among Patients With Preexisting Liver Disease in the United States: A Multicenter Research Network Study. Gastroenterology. 2020;159:768-771.e3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 205] [Cited by in RCA: 270] [Article Influence: 54.0] [Reference Citation Analysis (0)] |
| 72. | Nawghare P, Jain S, Chandnani S, Bansal S, Patel S, Debnath P, Rane S, Deshmukh R, Rathi P, Contractor Q. Predictors of Severity and Mortality in Chronic Liver Disease Patients With COVID-19 During the Second Wave of the Pandemic in India. Cureus. 2022;14:e20891. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 73. | Iavarone M, D'Ambrosio R, Soria A, Triolo M, Pugliese N, Del Poggio P, Perricone G, Massironi S, Spinetti A, Buscarini E, Viganò M, Carriero C, Fagiuoli S, Aghemo A, Belli LS, Lucà M, Pedaci M, Rimondi A, Rumi MG, Invernizzi P, Bonfanti P, Lampertico P. High rates of 30-day mortality in patients with cirrhosis and COVID-19. J Hepatol. 2020;73:1063-1071. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 279] [Cited by in RCA: 276] [Article Influence: 55.2] [Reference Citation Analysis (2)] |
| 74. | Moon AM, Webb GJ, Aloman C, Armstrong MJ, Cargill T, Dhanasekaran R, Genescà J, Gill US, James TW, Jones PD, Marshall A, Mells G, Perumalswami PV, Qi X, Su F, Ufere NN, Barnes E, Barritt AS, Marjot T. High mortality rates for SARS-CoV-2 infection in patients with pre-existing chronic liver disease and cirrhosis: Preliminary results from an international registry. J Hepatol. 2020;73:705-708. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 203] [Cited by in RCA: 203] [Article Influence: 40.6] [Reference Citation Analysis (0)] |
| 75. | Jeon D, Son M, Choi J. Impact of liver cirrhosis on the clinical outcomes of patients with COVID-19: a nationwide cohort study of Korea. Korean J Intern Med. 2021;36:1092-1101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 76. | Satapathy SK, Roth NC, Kvasnovsky C, Hirsch JS, Trindade AJ, Molmenti E, Barish M, Hirschwerk D, Da BL, Bernstein D; Northwell Health COVID-19 Research Consortium. Risk factors and outcomes for acute-on-chronic liver failure in COVID-19: a large multi-center observational cohort study. Hepatol Int. 2021;15:766-779. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 77. | Chagas AL, Fonseca LGD, Coelho FF, Saud LRDC, Abdala E, Andraus W, Fiore L, Moreira AM, Menezes MR, Carnevale FC, Tani CM, Alencar RSSM, D'Albuquerque LAC, Herman P, Carrilho FJ. Management of Hepatocellular Carcinoma during the COVID-19 Pandemic - São Paulo Clínicas Liver Cancer Group Multidisciplinary Consensus Statement. Clinics (Sao Paulo). 2020;75:e2192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 78. | Muñoz-Martínez S, Sapena V, Forner A, Bruix J, Sanduzzi-Zamparelli M, Ríos J, Bouattour M, El-Kassas M, Leal CRG, Mocan T, Nault JC, Alves RCP, Reeves HL, da Fonseca L, García-Juárez I, Pinato DJ, Varela M, Alqahtani SA, Alvares-da-Silva MR, Bandi JC, Rimassa L, Lozano M, González Santiago JM, Tacke F, Sala M, Anders M, Lachenmayer A, Piñero F, França A, Guarino M, Elvevi A, Cabibbo G, Peck-Radosavljevic M, Rojas Á, Vergara M, Braconi C, Pascual S, Perelló C, Mello V, Rodríguez-Lope C, Acevedo J, Villani R, Hollande C, Vilgrain V, Tawheed A, Ferguson Theodoro C, Sparchez Z, Blaise L, Viera-Alves DE, Watson R, Carrilho FJ, Moctezuma-Velázquez C, D'Alessio A, Iavarone M, Reig M. Outcome of liver cancer patients with SARS-CoV-2 infection: An International, Multicentre, Cohort Study. Liver Int. 2022;42:1891-1901. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 79. | Pazgan-Simon M, Kucharska M, Górka-Dynysiewicz J, Simon K. Impact of SARS CoV-2 /COVID-19 infection on the course of advanced chronic liver disease and hepatocellular carcinoma. Pharmacol Rep. 2022;74:1306-1314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 80. | Guarino M, Cossiga V, Capasso M, Mazzarelli C, Pelizzaro F, Sacco R, Russo FP, Vitale A, Trevisani F, Cabibbo G; The Associazione Italiana Per Lo Studio Del Fegato AISF HCC Special Interest Group. Impact of SARS-CoV-2 Pandemic on the Management of Patients with Hepatocellular Carcinoma. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 81. | Li P, Liu Y, Cheng Z, Yu X, Li Y. COVID-19-associated liver injury: Clinical characteristics, pathophysiological mechanisms and treatment management. Biomed Pharmacother. 2022;154:113568. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 82. | Floreani A, De Martin S. COVID-19 and Autoimmune Liver Diseases. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 83. | Marjot T, Buescher G, Sebode M, Barnes E, Barritt AS 4th, Armstrong MJ, Baldelli L, Kennedy J, Mercer C, Ozga AK, Casar C, Schramm C; contributing Members and Collaborators of ERN RARE-LIVER/COVID-Hep/SECURE-Cirrhosis, Moon AM, Webb GJ, Lohse AW. SARS-CoV-2 infection in patients with autoimmune hepatitis. J Hepatol. 2021;74:1335-1343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 89] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 84. | Efe C, Dhanasekaran R, Lammert C, Ebik B, Higuera-de la Tijera F, Aloman C, Rıza Calışkan A, Peralta M, Gerussi A, Massoumi H, Catana AM, Torgutalp M, Purnak T, Rigamonti C, Gomez Aldana AJ, Khakoo N, Kacmaz H, Nazal L, Frager S, Demir N, Irak K, Ellik ZM, Balaban Y, Atay K, Eren F, Cristoferi L, Batıbay E, Urzua Á, Snijders R, Kıyıcı M, Akyıldız M, Ekin N, Carr RM, Harputluoğlu M, Hatemi I, Mendizabal M, Silva M, Idilman R, Silveira M, Drenth JPH, Assis DN, Björnsson E, Boyer JL, Invernizzi P, Levy C, Schiano TD, Ridruejo E, Wahlin S. Outcome of COVID-19 in Patients With Autoimmune Hepatitis: An International Multicenter Study. Hepatology. 2021;73:2099-2109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 55] [Article Influence: 13.8] [Reference Citation Analysis (1)] |
| 85. | Zecher BF, Buescher G, Willemse J, Walmsley M, Taylor A, Leburgue A, Schramm C, Lohse AW, Sebode M. Prevalence of COVID-19 in patients with autoimmune liver disease in Europe: A patient-oriented online survey. United European Gastroenterol J. 2021;9:797-808. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 86. | Ampuero J, Lucena A, Hernández-Guerra M, Moreno-Moraleda I, Arenas J, Conde I, Muñoz L, Canillas L, Fernandez E, Quiñones R, Simon MA, Gómez-Dominguez E, Gutierrez ML, Fernandez-Rodriguez C, Domper-Arnal MJ, Jorquera F, Garcia-Buey ML, Garcia-Retortillo M, Morillas R, Berenguer M, Casado M, Morales-Arraez D, Sousa JM, Molina E. Primary biliary cholangitis and SARS-CoV-2 infection: incidence, susceptibility and outcomes. Gut. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 87. | Mallet V, Beeker N, Bouam S, Sogni P, Pol S; Demosthenes research group. Prognosis of French COVID-19 patients with chronic liver disease: A national retrospective cohort study for 2020. J Hepatol. 2021;75:848-855. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 49] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 88. | Lippi G, de Oliveira MHS, Henry BM. Chronic liver disease is not associated with severity or mortality in Coronavirus disease 2019 (COVID-19): a pooled analysis. Eur J Gastroenterol Hepatol. 2021;33:114-115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 89. | Martinez MA, Franco S. Impact of COVID-19 in Liver Disease Progression. Hepatol Commun. 2021;5:1138-1150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |