Published online Aug 14, 2023. doi: 10.3748/wjg.v29.i30.4671
Peer-review started: March 27, 2023
First decision: April 26, 2023
Revised: May 20, 2023
Accepted: July 11, 2023
Article in press: July 11, 2023
Published online: August 14, 2023
Processing time: 136 Days and 2.6 Hours
Chronic pancreatitis (CP) is a fibroinflammatory syndrome leading to reduced quality of life and shortened life expectancy. Population-based estimates of the incidence, prevalence, and comorbidities of CP in China are scarce.
To characterize the incidence, prevalence, and comorbidities of CP in Sichuan Province, China, with population-based data.
Data on CP from 2015 to 2021 were obtained from the Health Information Center of Sichuan Province. During the study period, a total of 38090 individuals were diagnosed with CP in Sichuan Province. The yearly incidence rate and point prevalence rate (December 31, 2021) of CP were calculated. The prevalence of comorbid conditions in CP patients was estimated. The annual number of CP-related hospitalizations, hospital length of stay, and hospitalization costs for CP were evaluated. Yearly incidence rates were standardized for age by the direct method using the permanent population of Sichuan Province in the 2020 census as the standard population. An analysis of variance test for the linearity of scaled variables and the Cochran-Armitage trend test for categorical data were perfor
The 38090 CP patients comprised 23280 males and 14810 females. The mean age of patients at CP diagnosis was 57.83 years, with male patients (55.87 years) being younger than female patients (60.11 years) (P < 0.001). The mean incidence rate of CP during the study period was 6.81 per 100000 person-years, and the incidence of CP increased each year, from 4.03 per 100000 person-years in 2015 to 8.27 per 100000 person-years in 2021 (P < 0.001). The point prevalence rate of CP in 2021 was 45.52 per 100000 individuals for the total population, with rates of 55.04 per 100000 individuals for men and 35.78 per 100000 individuals for women (P < 0.001). Individuals aged 65 years or older had the highest prevalence of CP (113.38 per 100000 individuals) (P < 0.001). Diabetes (26.32%) was the most common comorbidity in CP patients. The number of CP-related hospitalizations increased from 3739 in 2015 to 11009 in 2021. The total costs for CP-related hospitalizations for CP patients over the study period were 667.96 million yuan, with an average of 17538 yuan per patient.
The yearly incidence of CP is increasing, and the overall CP hospitalization cost has increased by 1.4 times during the last 7 years, indicating that CP remains a heavy health burden.
Core Tip: Chronic pancreatitis (CP) remains a heavy health burden worldwide. However, available epidemiological data on CP in China are scarce. We conducted a population-based study on the incidence, prevalence, comorbidities, and disease burden of CP in Sichuan Province, China, from 2015 to 2021. We analyzed a total of 38090 patients, which represents the largest series of CP patients ever reported in China. We observed an increasing incidence and rising costs for CP-related hospitalization. The point prevalence rate of CP was 45.52 per 100000 individuals in 2021. Metabolic-related diseases and pancreatic tumors were among the most common comorbidities among CP patients.
- Citation: Cai QY, Tan K, Zhang XL, Han X, Pan JP, Huang ZY, Tang CW, Li J. Incidence, prevalence, and comorbidities of chronic pancreatitis: A 7-year population-based study. World J Gastroenterol 2023; 29(30): 4671-4684
- URL: https://www.wjgnet.com/1007-9327/full/v29/i30/4671.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i30.4671
Chronic pancreatitis (CP) is a fibroinflammatory syndrome characterized by chronic upper abdominal pain and exocrine and endocrine pancreatic insufficiency[1]. Although some cases of CP may begin with one or recurrent bouts of pancreatitis, approximately 50% of CP patients have no history of acute pancreatitis[2,3]. Therefore, for a considerable propor
In addition, comorbidities, defined as the cooccurrence of two or more chronic medical conditions in one person[17], usually alter the disease management implications. Multiple comorbidities may reduce QoL and increase the risk of death and the consumption of medical resources[18]. Therefore, comorbidities have become an important part of epidemiological studies for chronic diseases[19]. However, data on the comorbidities of CP are still insufficient[20]. This epidemiological study aimed to characterize the incidence, prevalence, and comorbidities of CP in Sichuan Province in Southwest China from 2015 to 2021 with population-based data.
Data on CP from 2015 to 2021 were obtained from the Health Information Center of Sichuan Province (HIC-SC), which collects electronic hospitalization summary reports (HSRs) from the electronic medical record systems of all hospitals in Sichuan Province. These records contain encrypted patient identification numbers and data on age, sex, admission and discharge dates, International Classification of Diseases, Tenth Revision (ICD-10) codes, and relevant discharge diagnoses. The HIC-SC has provided data for many scientific studies[21-23], verifying the reliability of the database. The data of permanent residents in Sichuan Province over the study years were obtained from the Sichuan Provincial Bureau of Statistics. This study was approved by the biomedical ethics review committee of West China Hospital, Sichuan Univer
In China, the definition of CP as a continuing inflammatory disease of the pancreas, characterized by irreversible morphological changes and pain and/or permanent loss of function, has been widely accepted[7,24]. In clinical practice, computed tomography (CT) or magnetic resonance imaging (MRI) are usually recommended as first-line tests for patients with clinical symptoms of an inflammatory disorder of the pancreas (such as a previous episode of acute pancreatitis, characteristic pain, and/or maldigestion) because they are universally available and reproducible. The major imaging characteristics of CP include pancreatic atrophy, fibrosis, duct distortion and strictures, stones in pancreatic ducts or multiple calcifications distributed throughout the entire pancreas, etc. Endoscopic ultrasound, because of its invasiveness, is used only if the diagnosis is in question after CT or MRI. The diagnosis of CP in some patients is established by histopathological examination after surgery due to unexplained pancreatic masses. Therefore, patients who had a discharge diagnosis of CP in their HSR provided by the HIC-SC with the following ICD-10 codes were included in this study: K86.102 for CP, K86.852 for pancreatic atrophy, K86.811 for pancreatic calcifications, K86.809 for stones in pancreatic ducts, K86.806/807 for duct distortion and strictures, K86.154 for pancreatic fibrosis, K86.201 for pancreatic cysts, K86.804 for pancreatemphraxis, and K86.901/902 for pancreatic masses. Furthermore, this study classified CP according to the following ICD-10 codes: K86.051 for alcoholic CP, K86.153 for autoimmune pancreatitis (AIP), and K86.151 for biliary pancreatitis. Patients with conflicting information, i.e., different birth dates at each admission, were excluded.
The comorbidities of CP in this study were selected by referring to previous studies[4,13,25]. Data on comorbidities were extracted from the electronic database by identifying their corresponding ICD-10 codes (Table 1).
| Comorbidities | ICD-10 codes |
| Diabetes | E10, E11, E12, E13, E14 |
| Type I diabetes | E10 |
| Type II diabetes | E11 |
| Secondary diabetes | E13, E14 |
| Hypertension | I10, I11, I12, I13, I15, O10 |
| Dyslipidemia | E78 |
| Cholelithiasis | K80, O99.603, K56.3 |
| Fatty liver disease | K76.0, K70.0 |
| Alcoholic fatty liver disease | K70.0 |
| Coronary heart disease | I21, I22, I23, I24, I25 |
| Cerebrovascular disease | I60, I61, I62, I63, I64, I65, I66, I67, I69, G45 |
| Ischemic cerebrovascular disease | I63, I64, I65, I66, I67, G45 |
| Hemorrhagic cerebrovascular disease | I60, I61, I62 |
| Pancreatic cyst | K86.2 |
| Pancreatic pseudocyst | K86.3 |
| Acute pancreatitis | K85 |
| Heart failure | I50, I11.0, I13.0, I13.2 |
| Hyperuricemia | M10, E79 |
| Gastrointestinal bleeding | K92.0, K92.1, K92.2 |
| Liver cirrhosis/fibrosis | K70.3, K74 |
| Alcoholic cirrhosis | K70.3 |
| Pancreatic tumor | C24.102, C25, D13.6, D37.752, D37.703, D37.704 |
| Malignant tumor of the pancreas | C25, C24.102 |
| Malnutrition | E12, E40, E41, E42, E43, E44, E45, E46 |
| Ulcer disease | K25, K26, K27, K28 |
| Gastric ulcer | K25 |
| Duodenal ulcer | K26 |
| Osteoporosis | M80, M81 |
| Inflammatory bowel disease | K50, K51 |
| Crohn’s disease | K50 |
| Ulcerative enteritis | K51 |
The major outcomes were the incidence and prevalence of CP. Incident cases were defined as patients with a first-time diagnosis of CP. Patients with a diagnosis of CP before the calculated year were excluded from the incidence estimate calculation. Prevalent cases were defined as patients with a diagnosis at some timepoint before the end of 2021. Crude incidence rates were calculated for each year between 2015 and 2021 as the number of incident CP cases divided by the average permanent population in a year (per 100000 person-years). Yearly incidence rates were standardized for age by the direct method using the permanent population of Sichuan Province in the 2020 census as the standard population. The point prevalence rate (December 31, 2021) was calculated as the number of patients who were diagnosed with CP before the end of 2021 divided by the permanent population of Sichuan Province in 2021. Other outcomes were the number of hospitalizations, the hospital length of stay (LoS), and the hospitalization costs. LoS was defined as the total length of hospital stay of the patient within one year. Costs for hospitalization, including total costs and the mean costs per patient, were calculated. Costs were adjusted by the consumer price index for each year to 2021 costs.
Data management and computations were performed using Oracle version 11.2.0 (https://www.oracle.com) and R version 4.1.3 (R Foundation for Statistical Computing; https://www.R-project.org/). Continuous variables are shown as the means ± SD. Since this was a population-based study including the entire permanent population of Sichuan Province during the observation period, no confidence intervals are provided for the estimates of the incidence or prevalence rates. Statistical analysis, such as the student’s t-test for continuous variables and the chi-squared test for categorical variables, was used for the comparison of statistics between sexes and age groups. To investigate yearly trends, we performed an analysis of variance tests for the linearity of scaled variables and the Cochran-Armitage trend test for categorical data. A two-sided test with P < 0.05 was considered statistically significant.
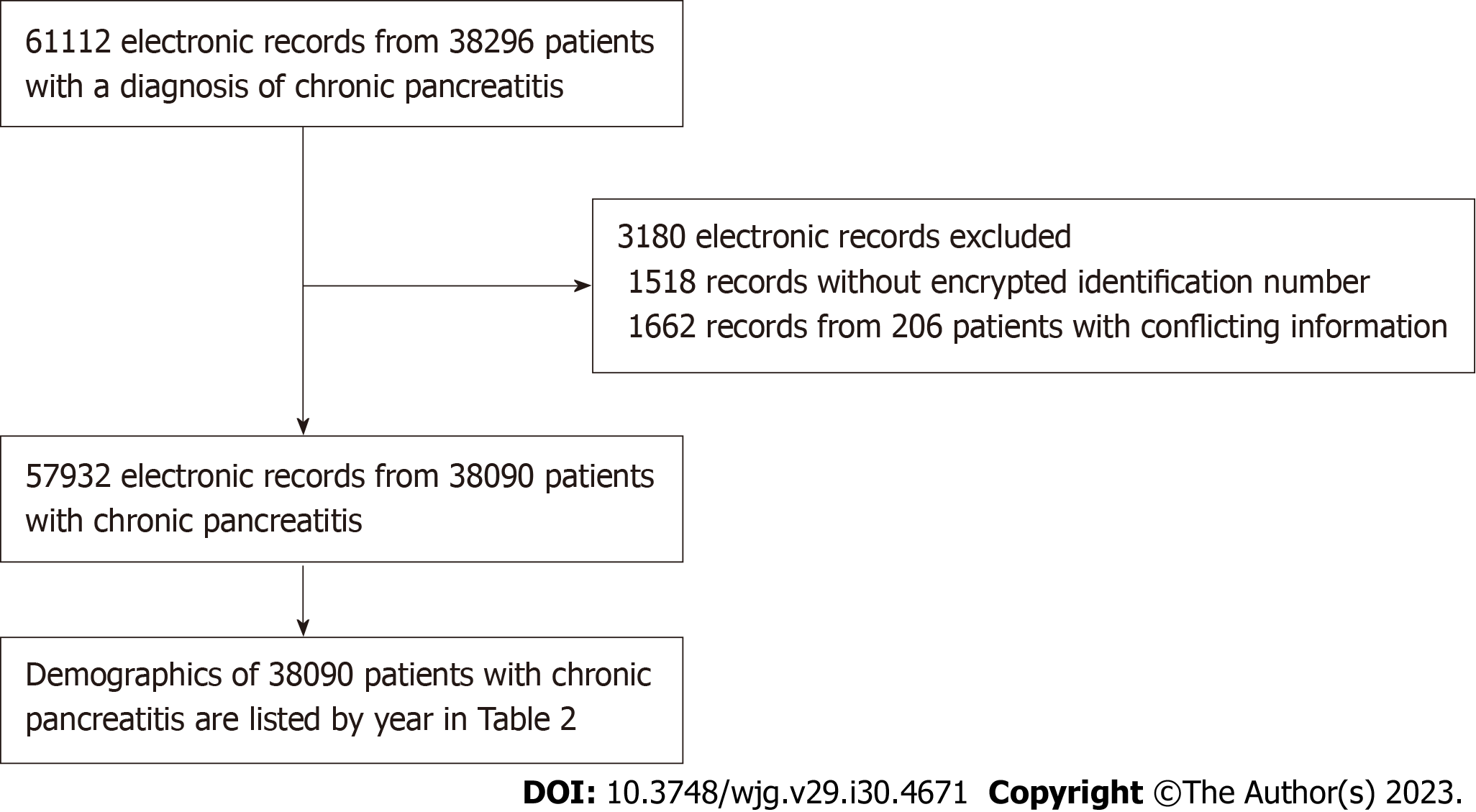
There were a total of 61112 electronic records (38296 individuals) with a diagnosis of CP from 2015 to 2021. Among all the records, 3180 records were excluded due to missing encrypted patient identification numbers (1518 records) and conflicting information (1662 records from 206 individuals). The exclusion of the data resulted in the loss of 5.2% of the original electronic records and a loss of 0.5% from the original patient cohort. Therefore, 57932 electronic records from 38090 unique patients were ultimately analyzed in this study (Figure 1). Data for 30756 CP patients (80.7% of the cohort) were extracted by the ICD-code K86.102. A total of 3641 CP patients (9.6%) were identified by the ICD-10 code K86.809 (pancreatic calculus). The left 9.7% of the CP patients were included by other ICD-10 codes (K86). Only 397 CP patients (1%) were classified as having alcoholic CP. Sichuan Province is one of the most populous provinces in China, with approximately 83.67 million permanent residents in 2020.
The demographics of the CP patients with a first diagnosis are presented in Table 2 by calendar year. The number of new cases increased each year from 2015 to 2021, with a significant upward trend (P < 0.001). There were 1.56-fold more male patients than female patients. The mean age of the patients at CP diagnosis was 57.83 years, with males (55.87 years) being younger than females (60.11 years) (P < 0.001). More than 60% of the patients diagnosed each year were aged 15-64 years, and the proportion of each group remained stable over time (Table 2). Similar to the population ratio, the com
| 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | P value | |
| Electronic records, n | 3739 | 5760 | 7688 | 9488 | 9865 | 10383 | 11009 | < 0.001 |
| New case, n | 3088 | 4334 | 5299 | 5945 | 5987 | 6475 | 6962 | < 0.001 |
| Mean hospitalizations per patient, n | 1.21 | 1.16 | 1.19 | 1.20 | 1.17 | 1.16 | 1.15 | 0.097 |
| Sex, % | ||||||||
| Male | 62.01 | 59.23 | 60.52 | 59.73 | 60.23 | 62.63 | 62.90 | 0.282 |
| Female | 37.99 | 40.77 | 39.48 | 40.27 | 39.77 | 37.37 | 37.10 | |
| Age, yr, mean ± SD | 57.48 ± 15.78 | 58.01 ± 15.31 | 58.28 ± 15.59 | 58.84 ± 15.81 | 58.27 ± 15.77 | 57.52 ± 15.99 | 56.57 ± 16.57 | 0.387 |
| Male | 55.87 ± 15.35 | 56.58 ± 15.19 | 56.85 ± 15.17 | 57.37 ± 15.62 | 56.74 ± 15.38 | 56.10 ± 15.58 | 54.98 ± 16.41 | 0.415 |
| Female | 60.11 ± 16.12 | 60.09 ± 15.25 | 60.48 ± 15.96 | 61.01 ± 15.86 | 60.60 ± 16.06 | 59.88 ± 16.38 | 59.27 ± 16.51 | 0.389 |
| Age group, % | ||||||||
| 0-14 | 0.39 | 0.35 | 0.51 | 0.64 | 0.33 | 0.34 | 0.39 | 0.902 |
| 15-64 | 64.57 | 63.99 | 63.37 | 60.52 | 61.78 | 63.83 | 64.97 | 0.820 |
| ≥ 65 | 35.04 | 35.65 | 36.12 | 38.84 | 37.88 | 35.83 | 34.65 | 0.807 |
| Ethnicity, % | ||||||||
| Han | 94.36 | 94.78 | 95.32 | 95.31 | 94.27 | 94.18 | 95.17 | 0.722 |
| Yi | 1.33 | 1.80 | 1.91 | 1.55 | 2.04 | 2.12 | 2.08 | 0.515 |
| Zang | 1.69 | 2.03 | 1.83 | 2.27 | 2.24 | 2.30 | 1.74 | 0.923 |
| Qiang | 0.36 | 0.39 | 0.47 | 0.37 | 0.45 | 0.83 | 0.43 | 0.646 |
| Other | 2.27 | 0.99 | 0.47 | 0.50 | 1.00 | 0.57 | 0.57 | 0.007 |
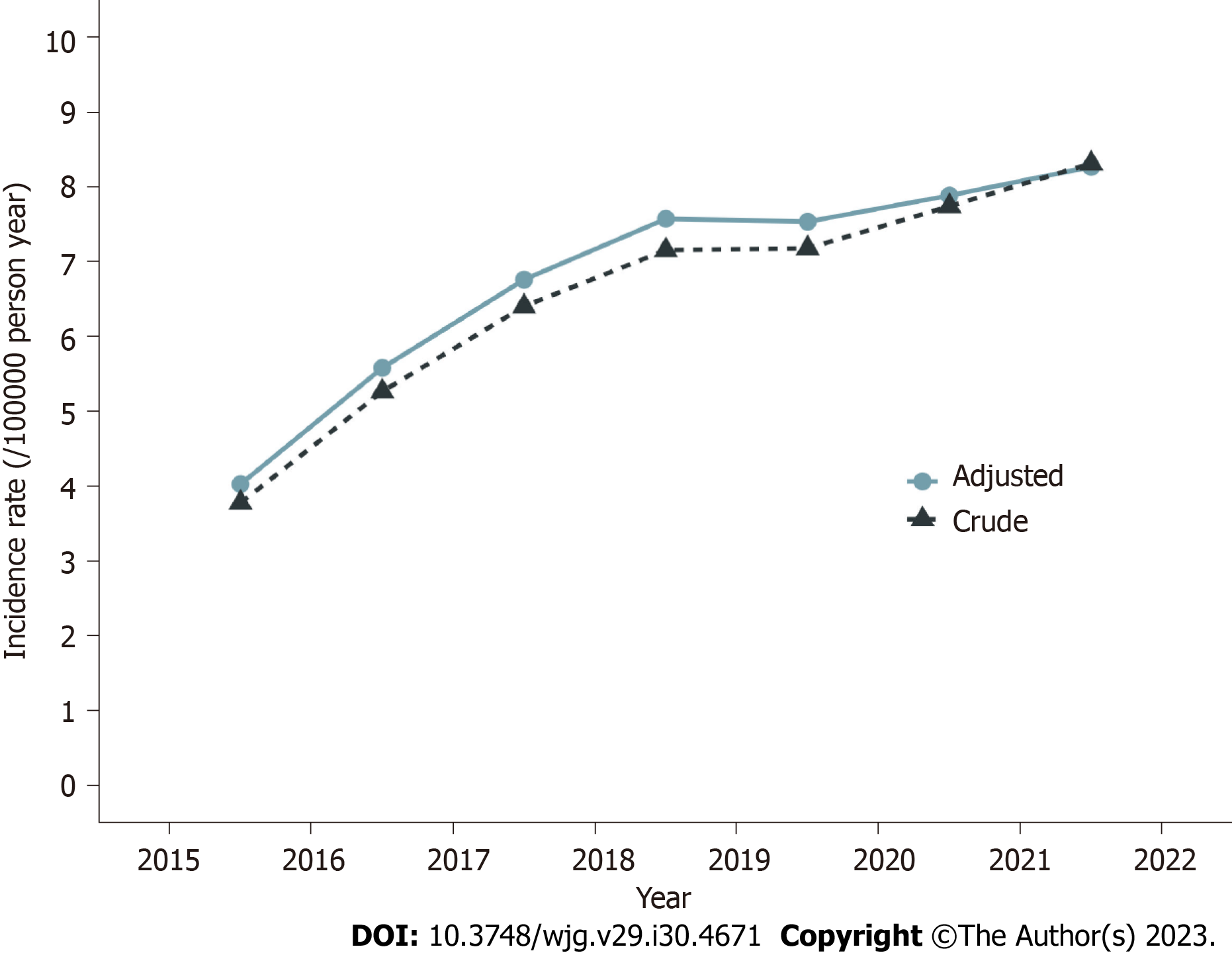
The mean standardized incidence of CP was 6.81 per 100000 person-years, and the incidence of CP increased yearly during the study period (P < 0.001), from 4.03 per 100000 person-years in 2015 to 8.27 per 100000 person-years in 2021 (Figure 2). The mean incidence of CP in males was 7.95 per 100000 person-years, which was significantly higher than that in females (5.13 per 100000 person-years) (P < 0.001). Both sexes presented similar upward trends (P < 0.001) (Figure 3A). For males, the incidence of CP was 4.70 per 100000 person-years in 2015 and 10.36 per 100000 person-years in 2021; for females, the incidence of CP was 2.86 per 100000 person-years in 2015 and 6.24 per 100000 person-years in 2021. The highest CP incidence (16.27 per 100000 person-years) was observed in patients aged ≥ 65 years, with an upward trend from 10.08 per 100000 person-years in 2015 to 16.70 per 100000 person-years in 2021 (P < 0.001) (Figure 3B). Individuals aged 14 years or younger showed the lowest CP incidence (0.17 per 100000 person-years), which remained stable during the 7 years (P = 0.830) (Figure 3B). The seven-year mean incidence for the 15-64-year age group was 6.01 per 100000 person-years, with an increase from 3.45 per 100000 person-years in 2015 to 8.08 per 100000 person-years in 2021 (P < 0.001) (Figure 3B).
A total of 38090 individuals were diagnosed with CP in Sichuan Province during the study period. The age distribution of the CP patients up to 2021 is shown in Figure 4A. Among all the patients, 23280 (61.12%) were men, and 14810 (38.88%) were women (P < 0.001). The point prevalence of CP was 45.52 per 100000 individuals in 2021 for the total population, 55.04 per 100000 individuals for the male population, and 35.78 per 100000 individuals for the female population (P < 0.001). The prevalence of CP was 1.53 times higher [95% confidence interval (CI): 1.51-1.57; P < 0.001) for men than for women. Individuals aged 65 years or older had the highest prevalence of CP (113.38 per 100000 individuals), with a prevalence of 127.58 per 100000 individuals for men and 100.03 per 100000 individuals for women (P < 0.001) (Figure 4B). For individuals aged between 15 and 64 years, the prevalence of CP was 39.11 per 100000 individuals, with a prevalence of 50.86 per 100000 individuals for men and 27.00 per 100000 individuals for women (P < 0.001) (Figure 4B). The prevalence of CP was 2.90 times higher (95%CI: 2.84-2.96; P < 0.001) for individuals aged 65 years or older than for individuals aged between 15 and 64 years. Individuals aged 14 years or younger had the lowest prevalence of CP (0.81 per 100000 individuals), with a prevalence of 0.82 per 100000 individuals for boys and 0.80 per 100000 individuals for girls (P = 1) (Figure 4B).
Diabetes (26.32%) was the most common comorbidity in CP patients, and patients with diabetes were similar in age to the overall cohort (Table 3). Metabolic-related diseases, including hypertension (21.51%), cholelithiasis (16.79%), dyslipidemia (16.70%), and fatty liver diseases (12.39%), were also common comorbidities among CP patients. The incidence of acute exacerbations of CP was 5.08% in all CP patients, with an incidence of 6.35% in males and 3.07% in females. A total of 2.65% of the CP patients were also diagnosed with pancreatic tumors, and 2.36% were diagnosed with malignant tumors of the pancreas.
| Diseases | Total cohort, n = 38090 | Males, n = 23280 | Females, n = 14810 | P value | |||
| n, % | Age, yr, mean ± SD | n, % | Age, yr, mean ± SD | n, % | Age, yr, mean ± SD | ||
| Total | 100.00 | 57.58 ± 15.79 | 100.00 | 56.26 ± 15.25 | 100.00 | 59.99 ± 16.44 | - |
| Diabetes | 26.32 | 56.57 ± 14.60 | 28.94 | 55.43 ± 14.03 | 22.20 | 59.14 ± 15.51 | < 0.001 |
| Type I diabetes | 0.79 | 45.33 ± 15.11 | 0.81 | 47.32 ± 12.81 | 0.76 | 42.23 ± 17.70 | 0.591 |
| Type II diabetes | 21.84 | 58.04 ± 14.26 | 23.73 | 56.78 ± 13.89 | 18.87 | 60.75 ± 14.66 | < 0.001 |
| Secondary diabetes | 2.05 | 50.04 ± 13.24 | 2.71 | 49.35 ± 12.40 | 1.01 | 53.27 ± 16.27 | < 0.001 |
| Hypertension | 21.51 | 66.32 ± 14.41 | 20.23 | 64.27 ± 14.43 | 23.51 | 69.36 ± 13.82 | < 0.001 |
| Cholelithiasis | 16.79 | 62.33 ± 16.14 | 14.95 | 60.23 ± 15.37 | 19.67 | 64.90 ± 16.68 | < 0.001 |
| Dyslipidemia | 16.70 | 51.49 ± 14.28 | 16.76 | 48.57 ± 13.12 | 16.61 | 56.01 ± 14.81 | 0.708 |
| Cerebrovascular disease | 12.76 | 69.75 ± 13.34 | 12.19 | 68.52 ± 13.55 | 13.65 | 71.60 ± 12.79 | < 0.001 |
| Ischemic cerebrovascular disease | 11.75 | 69.55 ± 13.38 | 11.17 | 68.54 ± 13.57 | 12.65 | 71.09 ± 12.92 | < 0.001 |
| Hemorrhagic cerebrovascular disease | 0.34 | 64.05 ± 14.42 | 0.43 | 62.63 ± 14.55 | 0.20 | 69.39 ± 12.79 | < 0.001 |
| Fatty liver disease | 12.39 | 49.53 ± 13.50 | 13.46 | 47.20 ± 12.63 | 10.72 | 54.28 ± 13.96 | < 0.001 |
| Alcoholic fatty liver disease | 0.35 | 54.07 ± 12.45 | 0.53 | 54.32 ± 12.38 | 0.07 | 50.50 ± 13.39 | < 0.001 |
| Coronary heart disease | 10.07 | 72.15 ± 12.77 | 8.37 | 71.13 ± 13.10 | 12.75 | 73.27 ± 12.31 | < 0.001 |
| Heart failure | 5.27 | 74.15 ± 13.38 | 4.72 | 72.62 ± 13.98 | 6.14 | 76.06 ± 12.33 | < 0.001 |
| Acute pancreatitis | 5.08 | 51.38 ± 15.68 | 6.35 | 52.17 ± 14.18 | 3.07 | 48.80 ± 19.57 | < 0.001 |
| Hyperuricemia | 4.93 | 56.86 ± 17.25 | 6.42 | 55.07 ± 16.87 | 2.59 | 64.28 ± 16.85 | < 0.001 |
| Ulcer disease | 4.68 | 60.16 ± 14.54 | 5.28 | 59.30 ± 14.06 | 3.73 | 62.22 ± 15.46 | < 0.001 |
| Gastric ulcer | 2.17 | 60.34 ± 13.91 | 2.40 | 59.36 ± 13.34 | 1.80 | 62.60 ± 14.92 | < 0.001 |
| Duodenal ulcer | 1.30 | 59.15 ± 14.46 | 1.65 | 58.53 ± 14.65 | 0.74 | 61.28 ± 13.62 | < 0.001 |
| Liver cirrhosis/fibrosis | 3.49 | 58.70 ± 13.92 | 4.35 | 57.05 ± 13.12 | 2.13 | 65.09 ± 15.04 | < 0.001 |
| Alcoholic cirrhosis | 0.72 | 53.23 ± 10.21 | 1.15 | 53.31 ± 10.19 | 0.05 | 49.60 ± 10.54 | < 0.001 |
| Pancreatic pseudocyst | 3.45 | 52.55 ± 14.28 | 4.46 | 51.57 ± 12.92 | 1.85 | 56.38 ± 18.17 | < 0.001 |
| Malnutrition | 3.36 | 64.04 ± 16.53 | 3.80 | 62.74 ± 15.52 | 2.67 | 66.86 ± 18.23 | < 0.001 |
| Gastrointestinal bleeding | 2.93 | 61.76 ± 16.38 | 3.46 | 59.78 ± 15.84 | 2.10 | 67.13 ± 16.64 | < 0.001 |
| Pancreatic tumor | 2.65 | 61.43 ± 12.13 | 2.97 | 61.27 ± 11.77 | 2.15 | 61.79 ± 12.89 | < 0.001 |
| Malignant tumor of pancreas | 2.36 | 61.74 ± 11.99 | 2.64 | 61.50 ± 11.67 | 1.91 | 62.27 ± 12.65 | < 0.001 |
| Osteoporosis | 2.03 | 75.28 ± 13.19 | 1.37 | 70.13 ± 13.89 | 3.06 | 78.02 ± 11.94 | < 0.001 |
| Inflammatory bowel disease | 0.14 | 56.13 ± 15.76 | 0.13 | 56.75 ± 14.03 | 0.17 | 55.43 ± 17.76 | 0.388 |
| Crohn’s disease | 0.03 | 56.40 ± 14.07 | 0.03 | 58.67 ± 10.76 | 0.03 | 53.00 ± 19.37 | 1 |
| Ulcerative enteritis | 0.12 | 56.00 ± 16.05 | 0.11 | 56.15 ± 14.56 | 0.14 | 55.83 ± 17.90 | 0.429 |
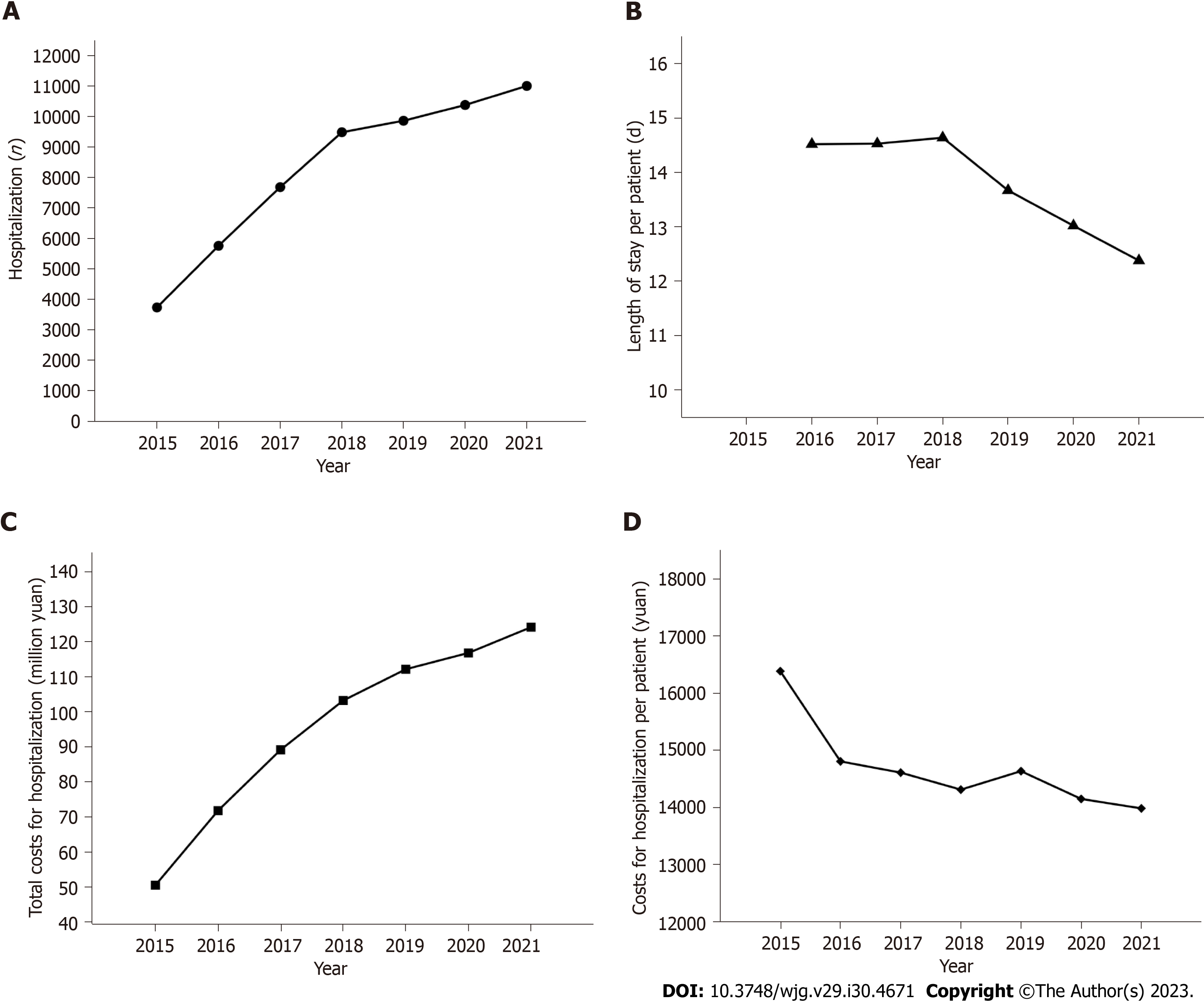
The number of CP-related hospitalizations increased approximately 2-fold, from 3739 in 2015 to 11009 in 2021 (P < 0.001) (Figure 5A). The LoS per CP patient decreased from 14.52 d in 2016 to 12.38 d in 2021 (P = 0.008) (Figure 5B). The total costs for CP-related hospitalizations for CP patients over the study period were 667.96 million yuan, with an average of 17538 yuan per patient. Total costs for CP-related hospitalizations increased from 50.60 million yuan in 2015 to 124.16 million in 2021 (P < 0.001) (Figure 5C), while the costs per patient decreased from 16387 yuan in 2015 to 13986 yuan in 2021 (P = 0.024) (Figure 5D).
We conducted a population-based study on the epidemiology of CP in Sichuan Province, China, from 2015 to 2021. This study showed that the mean incidence of CP was 6.81 per 100000 person-years in the last 7 years, and the point prevalence of CP was 45.52 per 100000 individuals in 2021 for the total population in Sichuan Province. The incidence and prevalence of CP increased with age and were significantly higher in males than in females over the study years. Metabolic-related diseases, including diabetes (26.32%), hypertension (21.51%), cholelithiasis (16.79%), dyslipidemia (16.70%), and fatty liver disease (12.39%), were common comorbidities in CP patients. In addition, 2.65% of the CP patients were diagnosed with pancreatic tumors. During the 7-year period, CP-related hospitalizations increased approximately 2-fold, and the overall hospitalization cost of CP increased by 1.4-fold. However, the LoS and the costs per CP patient decreased over the study years.
It may be valuable to improve epidemiological data of CP in the southwest area of China due to the rapid economic and societal development of the country. The first population-based epidemiological study of CP reported a mean CP incidence of 6.81 per 100000 person-years in Sichuan Province in the last 7 years. In other words, Sichuan Province has an average of 5652 new cases of CP every year. Thus, although hospitalization costs per patient decreased yearly, overall hospitalization costs still increased year by year. The overall hospitalization cost of CP increased by 1.4 times during the 7-year period. Although this study was analyzed with big data, the incidence rate may be underestimated because the data only covered inpatients with CP, and outpatients with CP were not included. A variety of databases have been used for the epidemiological analysis of CP[8,9,14,26], but it is still difficult to accurately describe the epidemic status of CP due to the limitations of various databases. There may be many CP outpatients, but if their condition is not severe enough to require hospitalization, the medical costs and the disease burden would be relatively low, and the epidemiological significance may not be very important. Reportedly, the rates of harmful drinking behaviors and smoking, which may be risk factors for CP, have increased in Chinese individuals in the last 10 years[27,28]. In contrast, the incidences of CP remained stable or even decreased yearly in recent years in the United States and Denmark, indicating that the decline in CP incidence might be due to the decrease in tobacco and alcohol consumption in both countries[8,14,29]. However, it was difficult to evaluate the factors related to the increasing incidence of CP in this study because electronic HSRs did not include risk factors associated with CP. CT and MRI have become universally available in hospitals at all levels in Sichuan Province, China. This greatly enhances the detection rate of CP and may partly contribute to the increasing CP incidence rate.
The point prevalence of CP was 45.52 per 100000 individuals in 2021 for the total population in Sichuan Province. The prevalence of CP was 39.11 and 113.38 per 100000 individuals for the population aged between 15 and 64 years and the population aged 65 years or older, respectively. The current results are consistent with those of studies in Minnesota (41.76/100000 individuals), Japan (52.4/100000 individuals), and Spain (49.3/100000 individuals), which were all based on questionnaire-based surveys[10,11,30]. In contrast, the prevalence of CP was considerably higher in register-based studies covering inpatients as well as outpatients[8,9,14]. Based on insurance claims databases, Machicado et al[9] and Sellers et al[14] reported similar results for the prevalence of CP in adults in America, which was 98.7/100000 individuals (2001-2013) and 91.9/100000 individuals (2007-2014), respectively. Using nationwide health care registries over a long period (1994–2018), Olesen et al[8] estimated the prevalence of CP at 153.9/100000 individuals in Denmark. This discrepancy may be explained by differences in study designs or by true differences in the CP prevalence across regions. Compared to the multicenter study in 2003, our current study adds to the prevalence data on CP over the past decades and verifies the upward trend in the prevalence of CP[15]. The increase in the CP prevalence could be explained by the increasing CP incidence and improved prognosis and life expectancy of CP patients[31-33].
Both the incidence and prevalence of CP in males were significantly higher than those in females over the study years. The prevalence for men was 1.53 times higher than that for women. Of all CP patients, 61.12% were men and 38.88% were women. Both the incidence and prevalence of CP were higher among men than women in all age groups, which was consistent with most previous studies[8,11,15,34,35]. This difference may be due to higher alcohol and tobacco exposure and increased genetic susceptibility to alcoholic CP among men[36,37]. The male hemizygous CLDN2 genotype and the female homozygous CLDN2 genotype are known to confer an amplified risk of pancreatitis together with alcohol use, and the frequency of the male hemizygous CLDN2 genotype (0.26) is much higher than that of the female homozygous CLDN2 genotype (0.07); thus, males have a higher genetic susceptibility to alcoholic CP than females[37]. In addition, the prevalence and incidence of CP were the highest among elderly individuals compared with young and middle-aged people in our study. These results are also similar to those of previous studies, suggesting that the incidence and prevalence of CP increases with aging[8,14]. Although the results might represent the prevalence of CP, it is undeniable that there was bias. In terms of the inpatient database, elderly people had the highest rate of hospitalization, which was accompanied by a higher detection rate of CP. In comparison, the detection rates of CP might be lower in other age groups, leading to an underestimation of the incidence and prevalence of CP.
As comorbidity, diabetes was reported in 26.32% of CP patients in this study. The prevalence of diabetes in CP patients reported in the previous literature was 15.2%-41.5%[4,13,25]. The high comorbidity of CP with diabetes suggests the importance of the identification of post-pancreatitis diabetes mellitus, which might be greatly different from type 2 diabetes mellitus in its manifestation and treatment. In addition, hypertension (21.51%), cholelithiasis (16.79%), and fatty liver disease (12.39%) were also common comorbidities in CP patients. A cohort study of the United Kingdom Biobank reported an even higher prevalence of gallstones (32.4%), hyperlipidemia (34.7%), and pancreatic cancer (4.7%) in CP patients and a strong association between CP and essential hypertension[13]. In the same cohort (United Kingdom Biobank), a case-control study reported that CP was associated with a significantly higher risk of pancreatic cancer in patients within the first 3 years[38]. These comorbidities may be explained by shared etiologies resulting from general exposure to risk factors such as tobacco use and alcohol consumption among CP patients. However, it is also possible that some of these comorbidities are involved in the pathogenesis of CP development, and some comorbidities may be complications caused by CP. Prospective studies, including longitudinal cohort studies and randomized control trials, may provide more definitive evidence on potential associations with multimorbidity. As shown in Table 4, different comorbidities were reported to be associated with CP in European, American, and East Asian countries. This may be related to different regions, times, and types of research. In addition, the pattern of comorbidities of CP is still under exploration, and the comorbidities reported by the abovementioned studies are similar to our findings. Smaller sample sizes and more accurate and complete diagnoses of diseases in cohort studies as well as different study inclusion criteria could explain the discrepancy between cohort and register-based studies.
| Region | Study design | Study period | Total CP patients | Frequent comorbidities compared with controls | Ref. |
| Denmark | Nationwide retrospective cohort study | 1995-2010 | 11972 | Cerebrovascular disease, chronic pulmonary disease, ulcer disease, diabetes, chronic renal disease, and pancreatic cancer | [4] |
| United States and Denmark | Cross-sectional, multicenter prospective study | Not available | 171 | Anxiety and depression | [40] |
| United States | Retrospective cohort study | 2015-2020 | 63230 | Hypertension, diabetes, and myocardial Infarction | [41] |
| United States | Ongoing longitudinal cohort study | 2017-2022 | 488 | Depression, anxiety, sleep disturbance, and physical disability | [42] |
| United States | Cohort study (NAPS2 cohort) | 2000-2014 | 1024 | Gallstones, diabetes, heart disease/heart attack/stroke, liver disease, renal disease, or prior history of cancer | [25] |
| United Kingdom | Cohort Study (the United Kingdom BioBank cohort) | 2000-2020 | 1027 | Gallstones, hyperlipidemia, diabetes, hypertriglyceridemia, hypercalcemia, pancreatic cancer, celiac, and ulcerative colitis | [13] |
| Canada | Retrospective study | 2007-2014 | 75744 | Anxiety and depression | [43] |
| China | Population-based cohort study | 2000-2011 | 15848 | Urolithiasis | [44] |
| China | Population-based cohort study | 2000-2011 | 17810 | Subsequent pyogenic liver abscess | [45] |
| China | Population-based cohort study | 2000-2011 | 16672 | Cerebrovascular disease | [46] |
| China | Population-based cohort study | 2000-2011 | 17778 | Deep vein thrombosis and pulmonary embolism | [20] |
| China | Population-based cohort study | 2000-2011 | 17796 | Inflammatory bowel disease | [47] |
| China | Prospective observational study | 2019-2021 | 720 | Anxiety and depression | [48] |
AIP represents < 5%-10% of pancreatitis cases and has a smaller prevalence of approximately 1-2/100000 individuals[39]. In the design of this study, AIP was classified as a type of CP. However, data on AIP were not extracted from the electronic HSRs because there is no special ICD-10 code for AIP. Moreover, only 1% of CP patients were classified as having alcoholic CP, which might be underestimated because doctors may not have paid enough attention to alcoholic CP when they filled out the electronic HSRs. This study suggests some improvements for the HIC-SC to enhance the quality of electronic HSR completion.
The yearly incidence of CP increased, along with the absolute number of CP patients and associated costs for hospitalization in Sichuan Province over the study period. The current work shows that CP remains a heavy burden on patients and the healthcare system. The implication of the high prevalence of diabetes (26.32%) in CP patients may vary with different people.
Chronic pancreatitis (CP) is a fibroinflammatory syndrome leading to reduced quality of life and shortened life expec
Accurate epidemiological estimates of CP are vital in shaping health resource allocation and medical provider training priorities.
To evaluate the prevalence and time trends of the incidence of CP and describe the comorbidities and disease burden of CP in Sichuan Province, China.
Data on CP from 2015 to 2021 were obtained from the Health Information Center of Sichuan Province. During the study period, a total of 38090 individuals were diagnosed with CP in Sichuan Province. The yearly incidence rate and point prevalence rate (December 31, 2021) of CP were calculated. The prevalence of comorbid conditions in CP patients was estimated. The annual number of CP-related hospitalizations, hospital length of stay, and costs for hospitalization for CP were evaluated. Yearly incidence rates were standardized for age by the direct method using the permanent population of Sichuan Province in the 2020 census as the standard population. An analysis of variance test for the linearity of scaled variables and the Cochran-Armitage trend test for categorical data were performed to investigate the yearly trends, and a two-sided test with P < 0.05 was considered statistically significant.
The 38090 CP patients comprised 23280 males and 14810 females. The mean age of patients at CP diagnosis was 57.83 years, with males (55.87 years) being younger than females (60.11 years) (P < 0.001). The mean incidence rate of CP during the study period was 6.81 per 100000 person-years, and the incidence of CP increased each year, from 4.03 per 100000 person-years in 2015 to 8.27 per 100000 person-years in 2021 (P < 0.001). The point prevalence rate of CP in 2021 was 45.52 per 100000 individuals for the total population, with rates of 55.04 per 100000 individuals for men and 35.78 per 100000 individuals for women (P < 0.001). Individuals aged 65 years or older had the highest prevalence of CP (113.38 per 100000 individuals) (P < 0.001). Diabetes (26.32%) was the most common comorbidity in CP patients. The number of CP-related hospitalizations increased from 3739 in 2015 to 11009 in 2021. The total costs for CP-related hospitalizations for CP patients over the study period were 667.96 million yuan, with an average of 17538 yuan per patient.
The yearly incidence of CP increased in Sichuan Province, along with the absolute number of CP patients and associated costs for hospitalization between 2015 and 2021. The point prevalence rate of CP in 2021 was 45.52/100000 individuals for the total population. Diabetes (26.32%), other metabolic-related diseases, and pancreatic cancer are among the common comorbidities in CP patients. The current work shows that CP continues to place a heavy burden on patients and the healthcare system.
Further studies are needed to identify CP and its comorbidities earlier, triggering potentially preventive mana
The authors are grateful to the staff of the Department of Gastroenterology, West China Hospital, Sichuan University, and the Health Information Center of Sichuan Province for their valuable assistance in this work.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Poddighe D, Kazakhstan; Rathnaswami A, India S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Beyer G, Habtezion A, Werner J, Lerch MM, Mayerle J. Chronic pancreatitis. Lancet. 2020;396:499-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 311] [Article Influence: 62.2] [Reference Citation Analysis (1)] |
| 2. | Hori Y, Vege SS, Chari ST, Gleeson FC, Levy MJ, Pearson RK, Petersen BT, Kendrick ML, Takahashi N, Truty MJ, Smoot RL, Topazian MD. Classic chronic pancreatitis is associated with prior acute pancreatitis in only 50% of patients in a large single-institution study. Pancreatology. 2019;19:224-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 3. | Vege SS, Chari ST. Chronic Pancreatitis. N Engl J Med. 2022;386:869-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 74] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 4. | Bang UC, Benfield T, Hyldstrup L, Bendtsen F, Beck Jensen JE. Mortality, cancer, and comorbidities associated with chronic pancreatitis: a Danish nationwide matched-cohort study. Gastroenterology. 2014;146:989-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 158] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 5. | Cohen SM, Kent TS. Etiology, Diagnosis, and Modern Management of Chronic Pancreatitis: A Systematic Review. JAMA Surg. 2023;158:652-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 6. | Masamune A, Kikuta K, Kume K, Hamada S, Tsuji I, Takeyama Y, Shimosegawa T, Okazaki K; Japan Pancreas Society. Nationwide epidemiological survey of chronic pancreatitis in Japan: introduction and validation of the new Japanese diagnostic criteria 2019. J Gastroenterol. 2020;55:1062-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 7. | Gardner TB, Adler DG, Forsmark CE, Sauer BG, Taylor JR, Whitcomb DC. ACG Clinical Guideline: Chronic Pancreatitis. Am J Gastroenterol. 2020;115:322-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 206] [Article Influence: 41.2] [Reference Citation Analysis (0)] |
| 8. | Olesen SS, Mortensen LH, Zinck E, Becker U, Drewes AM, Nøjgaard C, Novovic S, Yadav D, Tolstrup JS. Time trends in incidence and prevalence of chronic pancreatitis: A 25-year population-based nationwide study. United European Gastroenterol J. 2021;9:82-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 9. | Machicado JD, Dudekula A, Tang G, Xu H, Wu BU, Forsmark CE, Yadav D. Period prevalence of chronic pancreatitis diagnosis from 2001-2013 in the commercially insured population of the United States. Pancreatology. 2019;19:813-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 10. | Domínguez-Muñoz JE, Lucendo A, Carballo LF, Iglesias-García J, Tenías JM. A Spanish multicenter study to estimate the prevalence and incidence of chronic pancreatitis and its complications. Rev Esp Enferm Dig. 2014;106:239-245. [PubMed] |
| 11. | Hirota M, Shimosegawa T, Masamune A, Kikuta K, Kume K, Hamada S, Kanno A, Kimura K, Tsuji I, Kuriyama S; Research Committee of Intractable Pancreatic Diseases. The seventh nationwide epidemiological survey for chronic pancreatitis in Japan: clinical significance of smoking habit in Japanese patients. Pancreatology. 2014;14:490-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 71] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 12. | Capurso G, Archibugi L, Pasquali P, Aceti A, Balducci P, Bianchi P, Buono F, Camerucci S, Cantarini R, Centofanti S, Colantonio P, Cremaschi R, Crescenzi S, Di Mauro C, Di Renzi D, Filabozzi A, Fiorillo A, Giancaspro G, Giovannetti P, Lanna G, Medori C, Merletti E, Nunnari E, Paris F, Pavone M, Piacenti A, Rossi A, Scamuffa MC, Spinelli G, Taborchi M, Valente B, Villanova A, Chiriatti A, Delle Fave G. Prevalence of chronic pancreatitis: Results of a primary care physician-based population study. Dig Liver Dis. 2017;49:535-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Spagnolo DM, Greer PJ, Ohlsen CS, Mance S, Ellison M, Breze C, Busby B, Whitcomb DC, Haupt M. Acute and Chronic Pancreatitis Disease Prevalence, Classification, and Comorbidities: A Cohort Study of the UK BioBank. Clin Transl Gastroenterol. 2022;13:e00455. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 42] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 14. | Sellers ZM, MacIsaac D, Yu H, Dehghan M, Zhang KY, Bensen R, Wong JJ, Kin C, Park KT. Nationwide Trends in Acute and Chronic Pancreatitis Among Privately Insured Children and Non-Elderly Adults in the United States, 2007-2014. Gastroenterology. 2018;155:469-478.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 125] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 15. | Wang LW, Li ZS, Li SD, Jin ZD, Zou DW, Chen F. Prevalence and clinical features of chronic pancreatitis in China: a retrospective multicenter analysis over 10 years. Pancreas. 2009;38:248-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 92] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 16. | Li JN, Lai YM, Qian JM, Guo T, Lü H, Tang XY. Trends in etiologies of chronic pancreatitis within 20 years: analysis of 636 cases. Chin Med J (Engl). 2011;124:3556-3559. [PubMed] |
| 17. | Beard JR, Officer A, de Carvalho IA, Sadana R, Pot AM, Michel JP, Lloyd-Sherlock P, Epping-Jordan JE, Peeters GMEEG, Mahanani WR, Thiyagarajan JA, Chatterji S. The World report on ageing and health: a policy framework for healthy ageing. Lancet. 2016;387:2145-2154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1519] [Cited by in RCA: 1646] [Article Influence: 182.9] [Reference Citation Analysis (0)] |
| 18. | Emerging Risk Factors Collaboration, Di Angelantonio E, Kaptoge S, Wormser D, Willeit P, Butterworth AS, Bansal N, O'Keeffe LM, Gao P, Wood AM, Burgess S, Freitag DF, Pennells L, Peters SA, Hart CL, Håheim LL, Gillum RF, Nordestgaard BG, Psaty BM, Yeap BB, Knuiman MW, Nietert PJ, Kauhanen J, Salonen JT, Kuller LH, Simons LA, van der Schouw YT, Barrett-Connor E, Selmer R, Crespo CJ, Rodriguez B, Verschuren WM, Salomaa V, Svärdsudd K, van der Harst P, Björkelund C, Wilhelmsen L, Wallace RB, Brenner H, Amouyel P, Barr EL, Iso H, Onat A, Trevisan M, D'Agostino RB Sr, Cooper C, Kavousi M, Welin L, Roussel R, Hu FB, Sato S, Davidson KW, Howard BV, Leening MJ, Leening M, Rosengren A, Dörr M, Deeg DJ, Kiechl S, Stehouwer CD, Nissinen A, Giampaoli S, Donfrancesco C, Kromhout D, Price JF, Peters A, Meade TW, Casiglia E, Lawlor DA, Gallacher J, Nagel D, Franco OH, Assmann G, Dagenais GR, Jukema JW, Sundström J, Woodward M, Brunner EJ, Khaw KT, Wareham NJ, Whitsel EA, Njølstad I, Hedblad B, Wassertheil-Smoller S, Engström G, Rosamond WD, Selvin E, Sattar N, Thompson SG, Danesh J. Association of Cardiometabolic Multimorbidity With Mortality. JAMA. 2015;314:52-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 609] [Cited by in RCA: 667] [Article Influence: 66.7] [Reference Citation Analysis (0)] |
| 19. | Jepsen P. Comorbidity in cirrhosis. World J Gastroenterol. 2014;20:7223-7230. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 48] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 20. | Chung WS, Lin CL. Comorbid risks of deep vein thrombosis and pulmonary thromboembolism in patients with chronic pancreatitis: a nationwide cohort study. J Thromb Haemost. 2016;14:98-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Qiu H, Tan K, Long F, Wang L, Yu H, Deng R, Long H, Zhang Y, Pan J. The Burden of COPD Morbidity Attributable to the Interaction between Ambient Air Pollution and Temperature in Chengdu, China. Int J Environ Res Public Health. 2018;15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 68] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 22. | Zhu X, Qiu H, Wang L, Duan Z, Yu H, Deng R, Zhang Y, Zhou L. Risks of hospital admissions from a spectrum of causes associated with particulate matter pollution. Sci Total Environ. 2019;656:90-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 23. | Qiu H, Zhu X, Wang L, Pan J, Pu X, Zeng X, Zhang L, Peng Z, Zhou L. Attributable risk of hospital admissions for overall and specific mental disorders due to particulate matter pollution: A time-series study in Chengdu, China. Environ Res. 2019;170:230-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 80] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 24. | Zou WB, Ru N, Wu H, Hu LH, Ren X, Jin G, Wang Z, Du YQ, Cao YN, Zhang L, Chang XY, Zhang RC, Li XB, Shen Y, Li P, Li ZS, Liao Z; Chronic Pancreatitis Group of Chinese Medical Doctor Association. Guidelines for the diagnosis and treatment of chronic pancreatitis in China (2018 edition). Hepatobiliary Pancreat Dis Int. 2019;18:103-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 25. | Machicado JD, Amann ST, Anderson MA, Abberbock J, Sherman S, Conwell DL, Cote GA, Singh VK, Lewis MD, Alkaade S, Sandhu BS, Guda NM, Muniraj T, Tang G, Baillie J, Brand RE, Gardner TB, Gelrud A, Forsmark CE, Banks PA, Slivka A, Wilcox CM, Whitcomb DC, Yadav D. Quality of Life in Chronic Pancreatitis is Determined by Constant Pain, Disability/Unemployment, Current Smoking, and Associated Co-Morbidities. Am J Gastroenterol. 2017;112:633-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 145] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 26. | Alkhayyat M, Abou Saleh M, Coronado W, Abureesh M, Al-Otoom O, Qapaja T, Mansoor E, Simons-Linares CR, Stevens T, Chahal P. Increasing Prevalence of Anxiety and Depression Disorders After Diagnosis of Chronic Pancreatitis: A 5-Year Population-Based Study. Pancreas. 2021;50:153-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 27. | Im PK, Millwood IY, Guo Y, Du H, Chen Y, Bian Z, Tan Y, Guo Z, Wu S, Hua Y, Li L, Yang L, Chen Z; China Kadoorie Biobank (CKB) collaborative group. Patterns and trends of alcohol consumption in rural and urban areas of China: findings from the China Kadoorie Biobank. BMC Public Health. 2019;19:217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 65] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 28. | Wang M, Luo X, Xu S, Liu W, Ding F, Zhang X, Wang L, Liu J, Hu J, Wang W. Trends in smoking prevalence and implication for chronic diseases in China: serial national cross-sectional surveys from 2003 to 2013. Lancet Respir Med. 2019;7:35-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 240] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 29. | Pernenkil V, Wyatt T, Akinyemiju T. Trends in smoking and obesity among US adults before, during, and after the great recession and Affordable Care Act roll-out. Prev Med. 2017;102:86-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 30. | Yadav D, Timmons L, Benson JT, Dierkhising RA, Chari ST. Incidence, prevalence, and survival of chronic pancreatitis: a population-based study. Am J Gastroenterol. 2011;106:2192-2199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 291] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 31. | Löhr JM, Dominguez-Munoz E, Rosendahl J, Besselink M, Mayerle J, Lerch MM, Haas S, Akisik F, Kartalis N, Iglesias-Garcia J, Keller J, Boermeester M, Werner J, Dumonceau JM, Fockens P, Drewes A, Ceyhan G, Lindkvist B, Drenth J, Ewald N, Hardt P, de Madaria E, Witt H, Schneider A, Manfredi R, Brøndum FJ, Rudolf S, Bollen T, Bruno M; HaPanEU/UEG Working Group. United European Gastroenterology evidence-based guidelines for the diagnosis and therapy of chronic pancreatitis (HaPanEU). United European Gastroenterol J. 2017;5:153-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 521] [Cited by in RCA: 426] [Article Influence: 53.3] [Reference Citation Analysis (0)] |
| 32. | Madzak A, Olesen SS, Wathle GK, Haldorsen IS, Drewes AM, Frøkjær JB. Secretin-Stimulated Magnetic Resonance Imaging Assessment of the Benign Pancreatic Disorders: Systematic Review and Proposal for a Standardized Protocol. Pancreas. 2016;45:1092-1103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 33. | Rosman DA, Duszak R Jr, Wang W, Hughes DR, Rosenkrantz AB. Changing Utilization of Noninvasive Diagnostic Imaging Over 2 Decades: An Examination Family-Focused Analysis of Medicare Claims Using the Neiman Imaging Types of Service Categorization System. AJR Am J Roentgenol. 2018;210:364-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 34. | Xiao AY, Tan ML, Wu LM, Asrani VM, Windsor JA, Yadav D, Petrov MS. Global incidence and mortality of pancreatic diseases: a systematic review, meta-analysis, and meta-regression of population-based cohort studies. Lancet Gastroenterol Hepatol. 2016;1:45-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 549] [Cited by in RCA: 475] [Article Influence: 52.8] [Reference Citation Analysis (0)] |
| 35. | Hirota M, Shimosegawa T, Masamune A, Kikuta K, Kume K, Hamada S, Kihara Y, Satoh A, Kimura K, Tsuji I, Kuriyama S; Research Committee of Intractable Pancreatic Diseases. The sixth nationwide epidemiological survey of chronic pancreatitis in Japan. Pancreatology. 2012;12:79-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 76] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 36. | Petrov MS, Yadav D. Global epidemiology and holistic prevention of pancreatitis. Nat Rev Gastroenterol Hepatol. 2019;16:175-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 265] [Cited by in RCA: 528] [Article Influence: 88.0] [Reference Citation Analysis (0)] |
| 37. | Whitcomb DC, LaRusch J, Krasinskas AM, Klei L, Smith JP, Brand RE, Neoptolemos JP, Lerch MM, Tector M, Sandhu BS, Guda NM, Orlichenko L; Alzheimer's Disease Genetics Consortium, Alkaade S, Amann ST, Anderson MA, Baillie J, Banks PA, Conwell D, Coté GA, Cotton PB, DiSario J, Farrer LA, Forsmark CE, Johnstone M, Gardner TB, Gelrud A, Greenhalf W, Haines JL, Hartman DJ, Hawes RA, Lawrence C, Lewis M, Mayerle J, Mayeux R, Melhem NM, Money ME, Muniraj T, Papachristou GI, Pericak-Vance MA, Romagnuolo J, Schellenberg GD, Sherman S, Simon P, Singh VP, Slivka A, Stolz D, Sutton R, Weiss FU, Wilcox CM, Zarnescu NO, Wisniewski SR, O'Connell MR, Kienholz ML, Roeder K, Barmada MM, Yadav D, Devlin B. Common genetic variants in the CLDN2 and PRSS1-PRSS2 loci alter risk for alcohol-related and sporadic pancreatitis. Nat Genet. 2012;44:1349-1354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 295] [Cited by in RCA: 252] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 38. | Ma DM, Dong XW, Han X, Ling Z, Lu GT, Sun YY, Yin XD. Pancreatitis and Pancreatic Cancer Risk. Technol Cancer Res Treat. 2023;22:15330338231164875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 39. | Poddighe D. Autoimmune pancreatitis and pancreatic cancer: Epidemiological aspects and immunological considerations. World J Gastroenterol. 2021;27:3825-3836. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 19] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 40. | Phillips AE, Faghih M, Drewes AM, Singh VK, Yadav D, Olesen SS; Pancreatic Quantitative Sensory Testing (P-QST) Consortium. Psychiatric Comorbidity in Patients With Chronic Pancreatitis Associates With Pain and Reduced Quality of Life. Am J Gastroenterol. 2020;115:2077-2085. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 41. | Khan D, Abureesh M, Alkhayyat M, Sadiq W, Alshami M, Munir AB, Karam B, Deeb L, Lafferty J. Prevalence of Myocardial Infarction in Patients With Chronic Pancreatitis. Pancreas. 2021;50:99-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 42. | Yadav D, Askew RL, Palermo T, Li L, Andersen DK, Chen M, Fisher WE, Fogel EL, Forsmark CE, Hart PA, Othman MO, Pandol SJ, Park WG, Topazian MD, Van Den Eeden SK, Vege SS, Yang Y, Serrano J, Conwell DL; Consortium for the Study of Chronic Pancreatitis, Diabetes; Pancreatic Cancer (CPDPC). Association of Chronic Pancreatitis Pain Features With Physical, Mental, and Social Health. Clin Gastroenterol Hepatol. 2023;21:1781-1791.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 43. | Makar M, Vodusek Z, Xia W, Greenberg P, Abdelsayed GG. Rising Prevalence of Anxiety and Depression in Chronic Pancreatitis: A Nationwide Analysis. Pancreas. 2022;51:325-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 44. | Chen CH, Lin CL, Jeng LB. Association between chronic pancreatitis and urolithiasis: A population-based cohort study. PLoS One. 2018;13:e0194019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 45. | Tseng CW, Chen YT, Lin CL, Liang JA. Association between chronic pancreatitis and pyogenic liver abscess: a nationwide population study. Curr Med Res Opin. 2017;33:505-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 46. | Wong TS, Liao KF, Lin CM, Lin CL, Chen WC, Lai SW. Chronic Pancreatitis Correlates With Increased Risk of Cerebrovascular Disease: A Retrospective Population-Based Cohort Study in Taiwan. Medicine (Baltimore). 2016;95:e3266. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 47. | Chen YL, Hsu CW, Cheng CC, Yiang GT, Lin CS, Lin CL, Sung FC, Liang JA. Increased subsequent risk of inflammatory bowel disease association in patients with chronic pancreatitis: a nationwide population-based cohort study. Curr Med Res Opin. 2017;33:1077-1082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 48. | Chen C, Zhou Y, Wang D, Li G, Yin K, Tao H, Wang CY, Li ZS, Wei C, Hu LH. Anxiety, depression, and coping styles among patients with chronic pancreatitis in East China. BMC Psychiatry. 2023;23:212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |