Published online Aug 7, 2023. doi: 10.3748/wjg.v29.i29.4571
Peer-review started: June 19, 2023
First decision: July 6, 2023
Revised: July 10, 2023
Accepted: July 17, 2023
Article in press: July 17, 2023
Published online: August 7, 2023
Processing time: 44 Days and 8.2 Hours
Prophylactic enterostomy surgery is a common surgical approach used to reduce the risk of anastomotic leakage in patients who have undergone partial intestinal resection due to trauma or tumors. However, the traditional interrupted suturing technique used in enterostomy closure surgery has several issues, including lon
To compare the effectiveness of improved gunsight suture technique with traditional interrupted suture in closing intestinal stomas.
In this study, a retrospective, single-center case analysis was conducted on 270 patients who underwent prophylactic ileostomy closure surgery at the Department of Colorectal Surgery of Qilu Hospital from April 2017 to December 2021. The patients were divided into two groups: 135 patients received sutures using the improved gunsight method, while the remaining 135 patients were sutured with the traditional interrupted suture method. We collected data on a variety of parameters, such as operation time, postoperative pain score, body temperature, length of hospital stays, laboratory indicators, incidence of incisional complications, number of wound dressing changes, and hospitalization costs. Non-parametric tests and chi-square tests were utilized for data analysis.
There were no statistically significant differences in general patient information between the two groups, including the interval between the first surgery and the stoma closure [132 (105, 184) d vs 134 (109, 181) d, P = 0.63], gender ratio (0.64 vs 0.69, P = 0.44), age [62 (52, 68) years vs 60 (52, 68) years, P = 0.33], preoperative body mass index (BMI) [23.83 (21.60, 25.95) kg/m² vs 23.12 (20.94, 25.06) kg/m², P = 0.17]. The incidence of incision infection in the improved gunsight suture group tended to be lower than that in the traditional interrupted suture group [ (n = 2/135, 1.4%) vs (n = 10/135, 7.4%), P < 0.05], and the postoperative hospital stay in the improved gunsight suture group was significantly shorter than that in the traditional interrupted suture group [5 (4, 7) d vs 7 (6, 8) d, P < 0.05]. Additionally, the surgical cost in the modified gunsight suture group was slightly lower than that in the traditional suture group [4840 (4330, 5138) yuan vs 4980 (4726, 5221) yuan, P > 0.05], but there was no significant difference in the total hospitalization cost between the two groups.
In stoma closure surgery, the improved gunsight technique can reduce the incision infection rate, shorten the postoperative hospital stay, reduce wound tension, and provide better wound cosmetic effects compared to traditional interrupted suture.
Core Tip: Based on the gunsight technique, we proposed an improved gunsight closure method for enterostomy surgery in this study. This closure method can reduce the incision tension, lower the risk of incision infection, decrease the length of hospital stay, and reduce hospitalization costs. Additionally, it requires less postoperative wound care and provides a better cosmetic outcome.
- Citation: Chen C, Zhang X, Cheng ZQ, Zhang BB, Li X, Wang KX, Dai Y, Wang YL. Comparison of modified gunsight suture technique and traditional interrupted suture in enterostomy closure. World J Gastroenterol 2023; 29(29): 4571-4579
- URL: https://www.wjgnet.com/1007-9327/full/v29/i29/4571.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i29.4571
Patients with colon cancer, inflammatory bowel disease, or intestinal trauma may require partial bowel resection. However, a simple one-stage surgery may result in complications such as anastomotic leakage, significantly affecting patient health and increasing the economic burden. To reduce this risk, a prophylactic intestinal stoma is often performed in patients at high risk for anastomotic leakage during routine surgery[1,2]. After 2-3 mo, the patient’s condition was evaluated and a second-stage anastomosis was performed to restore gastrointestinal continuity[3]. Although prophylactic intestinal stoma can reduce complications such as anastomotic leakage[4], second-stage anastomotic surgery also has its own risks, including incision infection, intestinal obstruction, and incisional hernia[5-8]. Unlike Class II incisions in other gastrointestinal surgeries, the skin around the colostomy site is continuously exposed to feces, classifying it as a Class III incision. Incision infections are particularly common, with an incidence of up to 41% reported[9]. Due to factors, such as contamination of the intestinal contents, preventing incision infections may be challenging.
According to guidelines published by different countries, surgical site infection increases hospital stay and the risk of death by 2-11 times[10-13]. To address this issue, researchers have proposed improved surgical methods, such as placing drainage tubes at the incision site, selecting special suture materials, and modifying the suture technique[14-19]. Some special antimicrobial suture materials and techniques are highly regarded; however, there is currently no recognized surgical procedure to reduce the incidence of incision infections. Studies have shown that compared with traditional interrupted sutures, the purse-string suture technique can effectively drain subcutaneous fluid and significantly reduce the incidence of incision infections. However, owing to the high tension at the center of the incision[20-22], the healing process of the abdominal incision after closure may take up to 3 wk.
In 2010, Lim et al[23] proposed a suture technique called “gunsight suture” that can reduce tension at the incision site and leave a smaller drainage gap at the center of the incision. This technique can effectively drain subcutaneous blood and fluid, reduce infection rate, and provide good cosmetic results with minimal scarring[20,24,25]. However, it is difficult to drain all the subcutaneous blood and fluid by placing a drainage tube or strip at an angle in the central gap. In addition, the vertical placement of the drainage tube significantly affects the postoperative activity range, and frequent dressing changes are required owing to leakage at the center of the incision, which can cause serious psychological and economic burdens on patients. Moreover, fixing the drainage tube in the central gap of the gunsight suture incision is challenging; therefore, drainage strips are often used, resulting in a shorter drainage time and a slightly inferior drainage effect.
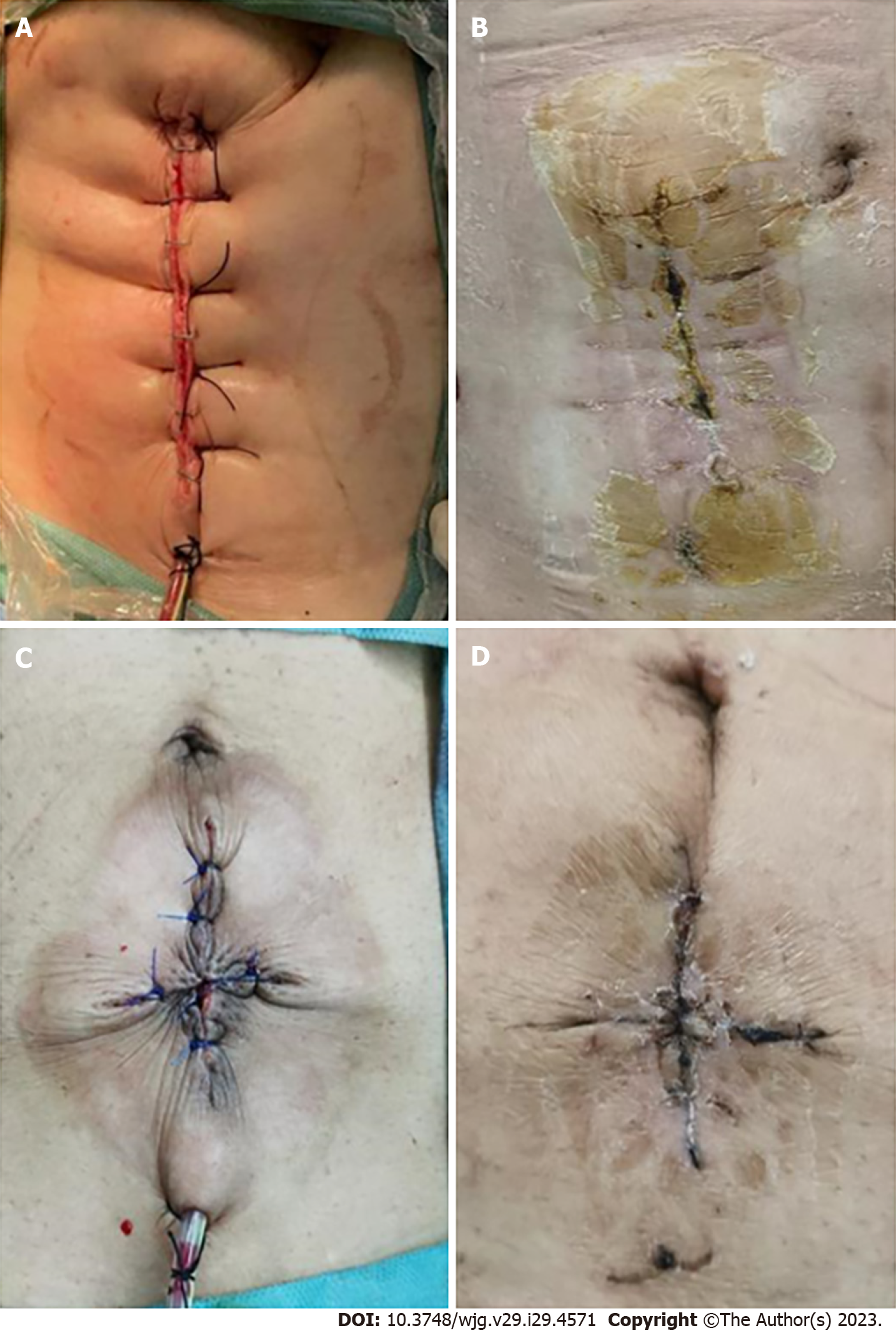
Therefore, in our hospital, we reserve a smaller gap (approximately 0.2 cm) at the center and place a drainage tube through the entire subcutaneous gap in a small incision next to the incision. The catheter was left in place for approximately 14 d and removed after the incision healed (Figure 1). This design effectively drained the subcutaneous fluid and reduced the local tension at the incision site (Figure 1C). Theoretically, it can reduce the incidence of incision infection, shorten the postoperative hospital stay, provide better cosmetic results, and reduce hospitalization costs. To verify the significance of the improved gunsight suture method in clinical practice, data were collected from 270 patients who underwent ileostomy closure surgery between April 2017 and December 2022. Our findings are reported below.
This retrospective case-control study was conducted between April 2017 and December 2022 to evaluate the effectiveness of a modified surgical technique for ileostomy closure and lateral ileal anastomosis. This study was approved by the Ethics Committee of Qilu Hospital, Shandong University (Approval No: KYLL-2020-120).
A total of 270 patients who underwent ileostomy closure and ileo-ileal lateral anastomosis surgery at the Department of Colorectal Surgery at Qilu Hospital were included in this study.
Inclusion criteria: Age > 18 years, patients who underwent ileostomy closure and ileo-ileal lateral anastomosis surgery, no stenosis of the intestinal lumen near the stoma on preoperative colonoscopy, and no concomitant colitis.
Exclusion criteria: Patients who required hernia repair due to concomitant incisional hernia, patients with mental dysfunction, and patients with other tumors, serious illnesses, or severe abdominal adhesions.
The day before surgery, the patient underwent mechanical bowel preparation with polyethylene glycol and rectal cleansing enema. This procedure improved the patient’s general condition, eliminated distant obstruction, and controlled the inflammation around the stoma. Prophylactic antibiotics were administered 30 min before surgery to prevent infection.
After the patients were fully anesthetized, they were placed in the supine position. First, a 2-0 silk suture was used to close the ileostomy and prevent intestinal contents from spilling out during the reduction process. After re-disinfecting, an appropriate stoma incision was made using the suturing method. The tissues surrounding the stoma were separated layer by layer to avoid damage to the intestinal wall. The freed intestine was then separated in all directions, and the direction with less adhesion was chosen to cut open the peritoneum and enter the abdominal cavity where the adhesions were loosened. The two ends of the freed intestinal tube were pulled out of the abdominal wall by > 5 cm, and a linear cutting closure device was used to perform a side-to-side anastomosis of the proximal and distal ends of the ileum to restore intestinal continuity. The 4-0 absorbable suture (Vycrl, Ethicon) was used to intermittently suture and reinforce the ileal muscularis layers. The bowel is returned to the abdominal cavity without placement of an abdominal drainage tube. Subsequently, a continuous suture is performed using 2-0 absorbable antibacterial sutures (VCP-603) to close the peritoneum and rectal sheath, leaving a subcutaneous drainage tube in place. The appropriate skin closure method is chosen based on the group.
Simple interrupted suture group (A, B): No or only minimal trimming is required at the site of repositioning. A 2-0 suture is used for full-thickness vertical mattress suturing, with a needle margin of 1 cm, a stitch spacing of 2 cm, and avoiding residual ineffective cavities. Reinforcement sutures can be placed between every two stitches, with a needle margin of 0.5 cm. This approach can better support skin closure and reduce tension on the surgical incision. After disinfection, sterile auxiliary materials are used for compression and bandaging.
Modified gunsight suture group (C, D): The incision was marked at the 3, 6, 9, and 12 o’clock positions, and the skin tissue between the marked points was triangularly excised to form a gunsight incision. A 2-0 silk suture was used to suture the subcutaneous tissue at the four marked points, and the skin was tightened and knotted after closure. The central part of the incision was brought together as closely as possible without leaving or leaving a gap of approximately 0.2 cm. Finally, a 2-0 silk suture was used to suture the midpoints of the four edges of the gunsight incision to complete the reinforcement. After disinfection, sterile auxiliary materials were applied for compression and bandaging.
The patients’ baseline data included age, sex, surgery time, postoperative pain score, postoperative temperature changes, hospitalization time, postoperative laboratory indicators, incision infection rate, and hospitalization costs. The temperature was recorded for 3 d after surgery. The Numeric Rating Scale (NRS) was used to assess the pain scores.
Data analysis was performed using the SPSS 26 statistical software. Normally distributed metric data were expressed as mean ± SD and intergroup comparisons were performed using independent sample t-tests. Non-normally distributed quantitative data were expressed as median (interquartile range) [M (IQR)], and intergroup comparisons were performed using the Mann-Whitney U test. Categorical variables were expressed as frequencies, and intergroup comparisons were performed using Chi-squared test or Fisher’s exact test. Statistical significance was set at P < 0.05.
The study included 270 patients who underwent stoma closure surgery at Qilu Hospital. All the patients completed the procedure without anastomotic leakage. Among them, 135 patients received modified Gunsight sutures, and 135 received traditional simple interrupted sutures. Statistical comparisons showed no significant differences in sex ratio, age, preoperative BMI, or the proportion of patients with diabetes between the two groups (Table 1).
| Group | Gunsight suture | Traditional suture | Statistical quantity | P value |
| Case number | 135 | 135 | - | - |
| Male (%) | 86 (63.7) | 92 (68.1) | χ2 = 0.59 | 0.440 |
| Age in yr (IQR) | 62 (52, 68) | 60 (52, 68) | Z = -0.97 | 0.332 |
| BMI (IQR) | 23.83 (21.60, 25.95) | 23.12 (20.94, 25.06) | Z = -1.377 | 0.169 |
| DM (%) | 17 (12.6) | 23 (17.0) | χ2 = 1.06 | 0.300 |
| Length of time between two surgeries, d (IQR) | 132 (105, 184) | 134 (109, 181) | Z = -0.489 | 0.625 |
Laboratory indicators included the systemic immune inflammation index (SII), red blood cell count, and hemoglobin levels. The SII was calculated as the platelet count multiplied by the ratio of neutrophils to lymphocytes and was used as a simple and effective evaluation index to assess the immune and inflammatory status and prognosis of patients before and after colorectal surgery. Previous studies have shown that the SII is an independent risk factor for the prognosis of colorectal cancer patients. There were no statistically significant differences in the laboratory indicators between the two groups[26-28].
According to the comparison of the main observation indicators (Table 2), the incidence of surgical site infection (SSI) in the modified gunsight suture group was lower than that in the traditional simple interrupted suture group [ (n = 2/135, 1.4%) vs (n = 10/135, 7.4%), P < 0.05], and the length of hospital stay and the number of dressing changes were also significantly better than those in the traditional simple interrupted suture group. However, there were no significant differences in the postoperative body temperature, pain score, or postoperative first bowel gas passage time between the two groups (P > 0.05). In addition, we compared the surgical and hospitalization costs between the two groups and found that the surgical cost in the modified Gunsight suture group was slightly lower than that in the traditional suture group [4840 (4330, 5138) yuan vs 4980 (4726, 5221) yuan, P > 0.05], but there was no significant difference in the total hospitalization cost between the two groups. Furthermore, scar formation after incision healing was significantly lower in the modified Gunsight suture group than in the control group (Figure 1B and D).
| Group | Gunsight suture (IQR) | Traditional suture (IQR) | Statistical quantity | P value | |
| SII (postoperative/preoperative) | 3.24 (2.16, 4.78) | 3.14 (2.10, 5.47) | Z = -0.592 | 0.554 | |
| Red blood cell (postoperative/preoperative) | 0.90 (0.84, 0.95) | 0.91 (0.87, 9.96) | Z = -1.445 | 0.148 | |
| Haemoglobin (postoperative/postoperative) | 0.91 (0.85, 0.97) | 0.92 (0.88, 0.96) | Z = -1.231 | 0.218 | |
| SSI (%) | 2 (1.4) | 10 (7.4) | χ2 = -5.580 | 0.018 | |
| Postoperative intestinal exhaust time (d) | 3 (2, 3) | 3 (2, 3) | Z = -1.171 | 0.242 | |
| Total cost of hospitalization (Yuan) | 33569 (30545, 36757) | 32782 (29134, 36199) | Z = -1.199 | 0.230 | |
| Cost of surgery (Yuan) | 4840 (4330, 5138) | 4980 (4726, 5221) | Z = -2.745 | 0.006 | |
| Number of dressing changes for surgical incision | 2 (1, 3) | 4 (3, 6) | Z = -2.460 | < 0.001 | |
| Operation time | 80 (70, 90) | 80 (70, 85) | Z = -1.210 | 0.220 | |
| Early postoperative pain score (NRS) | DAY1 | 3 (3, 3) | 3 (3, 3) | Z = -1.145 | 0.252 |
| DAY2 | 2 (2, 2) | 2 (2, 2) | Z = -0.044 | 0.965 | |
| DAY3 | 2.0 (1.5, 2.0) | 1.5 (1.5, 2.0) | Z = -0.603 | 0.547 | |
| Early postoperative body temperature (°C) | DAY1 | 36.7 (36.4, 36.9) | 36.7 (36.4, 36.9) | Z = -0.476 | 0.634 |
| DAY2 | 37.4 (37.1, 37.9) | 37.6 (37.1, 38.1) | Z = -1.769 | 0.077 | |
| DAY3 | 37.1 (36.9, 37.4) | 37.20 (36.85, 37.50) | Z = -1.385 | 0.166 | |
| DAY4 | 36.9 (36.7, 37.1) | 36.9 (36.7, 37.3) | Z = -1.315 | 0.189 | |
| Postoperative hospital stay (d) | 5 (4, 7) | 7 (6, 8) | Z = -5.181 | < 0.001 | |
During stoma closure surgery in patients who undergo preventive ostomy, there is a high incidence of incisional infections due to environmental contamination, subcutaneous fluid accumulation, and other reasons, with reported rates ranging from 3% to 41%[29]. This delay in wound healing can severely affect patients’ quality of life. To reduce the risk of postoperative incisional infections, many clinicians have proposed improvements in the suture method of the incision[20], among which the modified Gunsight suture technique has shown promise.
Reid et al[30] conducted a randomized controlled clinical trial involving 61 patients to compare postoperative complications of the purse-string suture technique with those of the traditional simple interrupted suture technique. They found that purse-string sutures had fewer surgical site infections than conventional sutures, with two out of 30 patients experiencing infections compared to 12 out of 31 patients in the conventional suture group[30]. In a multicenter prospective study by Han et al[20], the effectiveness of the gunsight and purse-string suture techniques in closing skin incisions was compared. This study found that the gunsight suture technique has a lower incision infection rate, similar to that of the purse-string suture technique. Additionally, patients in the Gunsight suture group had shorter incision healing times and higher patient satisfaction[20]. In a case-review study of 233 patients, Li et al[31] compared the clinical characteristics between patients with traditional simple interrupted sutures and those with gunsight sutures. The incidence of surgical site infections was significantly lower in the Gunsight suture group than in the traditional simple interrupted suture group. Gunsight sutures were identified as an independent protective risk factor for surgical site infections, with a dominance ratio of 0.212 and a P value of 0.048.
This study showed that our modified Gunsight suture technique is associated with a lower incidence of surgical site infection when compared with the traditional simple interrupted suture technique. Specifically, 10 patients in the traditional simple interrupted suture group experienced postoperative incisional infections, with three of these patients requiring a second surgical intervention and wound resuturing after failed conservative treatment. In contrast, only two patients in the modified gunsight suture group developed postoperative incisional infections, which resolved after conservative treatment. These findings provide evidence supporting the effectiveness of the modified Gunsight suture technique in reducing the risk of incisional infection.
In addition to the reduced incidence of SSI, patients in the modified Gunsight suture group also experienced shorter postoperative hospitalization days than those in the simple interrupted suture group. This difference in hospitalization time may be due to an increased risk of incision infection and the need for more frequent and longer wound care, such as wet alcohol dressing, in the simple interrupted suture group.
Furthermore, the surgical costs for patients in the gunsight suture group were slightly lower than those in the traditional suture group, and there was no significant difference in total hospitalization costs between the two groups. Furthermore, there were no significant differences between the two groups in terms of postoperative pain scores, exhaust time, and related laboratory indicators. Postoperative pain scores were evaluated using the NRS, with most patients scoring between 1 and 3 indicating mild pain. This may explain the lack of significant differences between the two groups. Additionally, the postoperative exhaust time and laboratory test results were not significantly associated with wound closure.
The modified Gunsight suture technique is an effective method for reducing the risk of surgical site infection and shortening postoperative hospitalization. Although this technique may require additional surgical steps, the reduced incidence of SSI and lower surgical costs make it a viable option for wound closure. Further research is needed to investigate the potential benefits of this technique in larger patient populations and evaluate its long-term effectiveness.
In the traditional intestinal stoma closure surgery, the interrupted suturing technique used has some issues, such as longer incisions and higher tension on the incision, which may increase the risk of postoperative complications. To address these concerns, scholars have proposed the use of the “gunsight suture” technique. This method involves using a gun-shaped incision instead of the conventional linear incision, leaving a gap in the center for drainage of blood and fluids to reduce the risk of infection. Building on this, we have proposed an improved gunsight suture technique.
Motivated by the need to enhance patient outcomes, this study focuses on developing an improved prophylactic stoma reversal abdominal closure suturing technique. Our goal is to reduce incision infection rates and alleviate patient burden, improving a key issue in stoma closure methods. We strive to contribute to the advancement of surgical research and help shape safer and more effective surgical practices in the future.
To compare the outcomes of the improved gunsight suture technique with traditional interrupted suture techniques in enterostomy closure. The objective is to minimize complications and related burdens following prophylactic ileostomy closure.
This study analyzed 270 patients who underwent prophylactic ileostomy closure surgery at Qilu Hospital from April 2017 to December 2021. The patients were divided into two groups, one group received sutures using the improved gunsight method while the other group was sutured with the traditional interrupted suture method, and data on various parameters such as operation time, postoperative pain score, and hospitalization costs were collected. Non-parametric tests and chi-square tests were used for data analysis.
This retrospective study compared two suture methods for prophylactic ileostomy closure surgery in 270 patients. The modified gunsight suture group had better outcomes, including lower incidence of surgical site infections, shorter hospital stays, and fewer dressing changes than the traditional simple interrupted suture group. Laboratory parameters, postoperative temperature, pain scores, and time to first bowel gas passage did not differ significantly. The modified gunsight suture group had slightly lower surgical costs and significantly lower scar formation after incision healing.
The modified Gunsight suture technique reduces the risk of surgical site infection and shortens postoperative hospitalization. Despite requiring additional surgical steps, the technique lowers surgical costs and is a viable option for wound closure.
Despite the study’s retrospective design and challenges in obtaining accurate data on bowel obstruction incidence and long-term complications like incisional hernias, it provides valuable insights. However, the single-center data source may introduce bias during data collection and analysis. Further research on larger patient populations is needed to evaluate the technique’s long-term effectiveness and potential benefits.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Maher CA, United States; Tie J, Australia; Zingg U, Switzerland S-Editor: Chen YL L-Editor: A P-Editor: Yu HG
| 1. | Hüser N, Michalski CW, Erkan M, Schuster T, Rosenberg R, Kleeff J, Friess H. Systematic review and meta-analysis of the role of defunctioning stoma in low rectal cancer surgery. Ann Surg. 2008;248:52-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 418] [Cited by in RCA: 427] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 2. | Gastinger I, Marusch F, Steinert R, Wolff S, Koeckerling F, Lippert H; Working Group ‘Colon/Rectum Carcinoma’. Protective defunctioning stoma in low anterior resection for rectal carcinoma. Br J Surg. 2005;92:1137-1142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 266] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 3. | Chow A, Tilney HS, Paraskeva P, Jeyarajah S, Zacharakis E, Purkayastha S. The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6,107 cases. Int J Colorectal Dis. 2009;24:711-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 293] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 4. | Mrak K, Uranitsch S, Pedross F, Heuberger A, Klingler A, Jagoditsch M, Weihs D, Eberl T, Tschmelitsch J. Diverting ileostomy vs no diversion after low anterior resection for rectal cancer: A prospective, randomized, multicenter trial. Surgery. 2016;159:1129-1139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 100] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 5. | Krebs B, Ivanecz A, Potrc S, Horvat M. Factors affecting the morbidity and mortality of diverting stoma closure: retrospective cohort analysis of twelve-year period. Radiol Oncol. 2019;53:331-336. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Åkesson O, Syk I, Lindmark G, Buchwald P. Morbidity related to defunctioning loop ileostomy in low anterior resection. Int J Colorectal Dis. 2012;27:1619-1623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 67] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 7. | Sajid MS, Craciunas L, Baig MK, Sains P. Systematic review and meta-analysis of published, randomized, controlled trials comparing suture anastomosis to stapled anastomosis for ileostomy closure. Tech Coloproctol. 2013;17:631-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Faunø L, Rasmussen C, Sloth KK, Sloth AM, Tøttrup A. Low complication rate after stoma closure. Consultants attended 90% of the operations. Colorectal Dis. 2012;14:e499-e505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Milanchi S, Nasseri Y, Kidner T, Fleshner P. Wound infection after ileostomy closure can be eliminated by circumferential subcuticular wound approximation. Dis Colon Rectum. 2009;52:469-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 10. | Anderson DJ, Podgorny K, Berríos-Torres SI, Bratzler DW, Dellinger EP, Greene L, Nyquist AC, Saiman L, Yokoe DS, Maragakis LL, Kaye KS. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35:605-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 584] [Cited by in RCA: 592] [Article Influence: 53.8] [Reference Citation Analysis (0)] |
| 11. | Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, Fish DN, Napolitano LM, Sawyer RG, Slain D, Steinberg JP, Weinstein RA; American Society of Health-System Pharmacists; Infectious Disease Society of America; Surgical Infection Society; Society for Healthcare Epidemiology of America. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013;70:195-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1238] [Cited by in RCA: 1364] [Article Influence: 113.7] [Reference Citation Analysis (0)] |
| 12. | Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999;20:250-78; quiz 279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2944] [Cited by in RCA: 2797] [Article Influence: 107.6] [Reference Citation Analysis (0)] |
| 13. | Magill SS, Edwards JR, Bamberg W, Beldavs ZG, Dumyati G, Kainer MA, Lynfield R, Maloney M, McAllister-Hollod L, Nadle J, Ray SM, Thompson DL, Wilson LE, Fridkin SK; Emerging Infections Program Healthcare-Associated Infections and Antimicrobial Use Prevalence Survey Team. Multistate point-prevalence survey of health care-associated infections. N Engl J Med. 2014;370:1198-1208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2799] [Cited by in RCA: 2789] [Article Influence: 253.5] [Reference Citation Analysis (0)] |
| 14. | Banerjee A. Pursestring skin closure after stoma reversal. Dis Colon Rectum. 1997;40:993-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 67] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Pan HD, Wang L, Peng YF, Li M, Yao YF, Zhao J, Zhan TC, Du CZ, Gu J. Subcutaneous vacuum drains reduce surgical site infection after primary closure of defunctioning ileostomy. Int J Colorectal Dis. 2015;30:977-982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Cantero R, Rubio-Perez I, Leon M, Alvarez M, Diaz B, Herrera A, Diaz-Dominguez J, Rodriguez-Montes JA. Negative-Pressure Therapy to Reduce the Risk of Wound Infection Following Diverting Loop Ileostomy Reversal: An Initial Study. Adv Skin Wound Care. 2016;29:114-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 17. | Blinov AV, Kachanov MD, Gvozdenko AA, Nagdalian AA, Blinova AA, Rekhman ZA, Golik AB, Vakalov DS, Maglakelidze DG, Nagapetova AG, Pokhilko AD, Burkina IV. Synthesis and Characterization of Zinc Oxide Nanoparticles Stabilized with Biopolymers for Application in Wound-Healing Mixed Gels. Gels. 2023;9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 18. | Blinov AV, Nagdalian AA, Povetkin SN, Gvozdenko AA, Verevkina MN, Rzhepakovsky IV, Lopteva MS, Maglakelidze DG, Kataeva TS, Blinova AA, Golik AB, Osipchuk GV, Shariati MA. Surface-Oxidized Polymer-Stabilized Silver Nanoparticles as a Covering Component of Suture Materials. Micromachines (Basel). 2022;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Dragovic M, Pejovic M, Stepic J, Colic S, Dozic B, Dragovic S, Lazarevic M, Nikolic N, Milasin J, Milicic B. Comparison of four different suture materials in respect to oral wound healing, microbial colonization, tissue reaction and clinical features-randomized clinical study. Clin Oral Investig. 2020;24:1527-1541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 20. | Han JG, Yao HW, Zhou JP, Zhang H, Wang GY, Shen ZL, Gong JF, Wang ZJ; Colorectal Surgery Group of Chinese Academic Society of Young Surgeons. Gunsight Procedure Versus the Purse-String Procedure for Closing Wounds After Stoma Reversal: A Multicenter Prospective Randomized Trial. Dis Colon Rectum. 2020;63:1411-1418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Amano K, Ishida H, Kumamoto K, Okada N, Hatano S, Chika N, Tajima Y, Ohsawa T, Yokoyama M, Ishibashi K, Mochiki E. Purse-string approximation vs primary closure with a drain for stoma reversal surgery: results of a randomized clinical trial. Surg Today. 2019;49:231-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Hajibandeh S, Hajibandeh S, Kennedy-Dalby A, Rehman S, Zadeh RA. Purse-string skin closure vs linear skin closure techniques in stoma closure: a comprehensive meta-analysis with trial sequential analysis of randomised trials. Int J Colorectal Dis. 2018;33:1319-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 23. | Lim JT, Shedda SM, Hayes IP. "Gunsight" skin incision and closure technique for stoma reversal. Dis Colon Rectum. 2010;53:1569-1575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Lee JR, Kim YW, Sung JJ, Song OP, Kim HC, Lim CW, Cho GS, Jung JC, Shin EJ. Conventional Linear vs Purse-string Skin Closure after Loop Ileostomy Reversal: Comparison of Wound Infection Rates and Operative Outcomes. J Korean Soc Coloproctol. 2011;27:58-63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 25. | Moreton A, Shankar S, Jones S. Randomized clinical trial of short-term outcomes following purse-string vs conventional closure of ileostomy wounds (Br J Surg 2010; 97: 1511-1517). Br J Surg. 2011;98:458; author reply 458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 26. | Xie QK, Chen P, Hu WM, Sun P, He WZ, Jiang C, Kong PF, Liu SS, Chen HT, Yang YZ, Wang D, Yang L, Xia LP. The systemic immune-inflammation index is an independent predictor of survival for metastatic colorectal cancer and its association with the lymphocytic response to the tumor. J Transl Med. 2018;16:273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 87] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 27. | Mangalesh S, Dudani S, Malik A. The systemic immune-inflammation index in predicting sepsis mortality. Postgrad Med. 2023;135:345-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 29] [Reference Citation Analysis (0)] |
| 28. | Dong M, Shi Y, Yang J, Zhou Q, Lian Y, Wang D, Ma T, Zhang Y, Mi Y, Gu X, Fan R. Prognostic and clinicopathological significance of systemic immune-inflammation index in colorectal cancer: a meta-analysis. Ther Adv Med Oncol. 2020;12:1758835920937425. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 55] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 29. | Dusch N, Goranova D, Herrle F, Niedergethmann M, Kienle P. Randomized controlled trial: comparison of two surgical techniques for closing the wound following ileostomy closure: purse string vs direct suture. Colorectal Dis. 2013;15:1033-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 30. | Reid K, Pockney P, Pollitt T, Draganic B, Smith SR. Randomized clinical trial of short-term outcomes following purse-string versus conventional closure of ileostomy wounds. Br J Surg. 2010;97:1511-1517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 31. | Li CK, Liang WW, Wang HM, Guo WT, Qin XS, Zhao J, Zhou WB, Li Y, Wang H, Huang RK. Gunsight sutures significantly reduce surgical-site infection after ileostomy reversal compared with linear sutures. Gastroenterol Rep (Oxf). 2021;9:357-362. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |