Published online Apr 28, 2023. doi: 10.3748/wjg.v29.i16.2495
Peer-review started: February 2, 2023
First decision: March 7, 2023
Revised: March 9, 2023
Accepted: April 7, 2023
Article in press: April 7, 2023
Published online: April 28, 2023
Processing time: 81 Days and 0.1 Hours
To date, endoscopic retrograde cholangiopancreatography has become a well-established treatment for common bile duct (CBD) stones. However, it is not suitable for some special patients, such as pregnant women, children or those who cannot stop taking anti-coagulation/anti-platelet agents because of radiation injury and the risk of postoperative bleeding resulting from endoscopic sphincterotomy. To overcome these two problems, this study introduced cholangioscopy-assisted extraction through a novel papillary support for small-calibre and sediment-like CBD stones.
To assess the feasibility and safety of cholangioscopy-assisted extraction through a novel papillary support (CEPTS) for small-calibre and sediment-like common bile duct (CBD) stones.
This Retrospective study was approved by the Ethics Committee of the Chinese PLA General Hospital. We designed a covered single dumbbell-style papillary support between 2021 and 2022. Between July 2022 and September 2022, 7 consecutive patients with small-calibre (cross diameter ≤ 1.0 cm) or sediment-like CBD stones underwent CETPS procedures in our center. The clinical characteristics and treatment outcomes of these 7 patients were extracted from a pro
A total of 2 patients had yellow sediment-like CBD stones, and aspiration extraction was performed after the insertion of papillary support. Of the 5 patients with clumpy CBD stones (0.4-1.0 cm), 2 underwent basket extraction under direct vision for a single stone (0.5-1.0 cm, black and black grey), 1 underwent balloon plus aspiration extraction under direct vision for 5 stones (0.4-0.6 cm, brown), and 2 underwent aspiration extraction only for a single stone (0.5-0.6 cm, yellow, none). Technical success, namely, no residual stones in the CBD or left and right hepatic ducts, was achieved in all 7 cases (100%). The median operating time was 45.0 minutes (range 13.0–87.0 minutes). Postoperative pancreatitis (PEP) occurred in one case (14.3%). Hyperamylasaemia without abdominal pain was noted in 2 of 7 patients. No residual stones or cholangitis were found during the follow-up.
CETPS appeared to be feasible to treat patients with small-calibre or sediment-like CBD stones. Patients, especially pregnant women and those who cannot stop anticoagulation/anti-platelet agents, could benefit from this technique.
Core Tip: Endoscopic retrograde cholangiopancreatography (ERCP) has become a well-established treatment for common bile duct (CBD) stones. However, the standard ERCP technique always requires endoscopic sphincterotomy (EST), which might lead to the loss of sphincter of Oddi function and some adverse events, including bleeding and perforation. Moreover, radiation injury makes the standard ERCP technique unsuitable for special patients, such as pregnant women and children. To overcome these problems, the present study introduced cholangioscopy-assisted extraction through a novel papillary support for small-calibre and sediment-like CBD stones, reducing radiation injury and avoiding EST.
- Citation: Zhang WG, Chai NL, Zhang B, Li X, Wang JF, Dong H, Feng YJ, Linghu EQ. Cholangioscopy-assisted extraction through novel papillary support for small-calibre and sediment-like common bile duct stones. World J Gastroenterol 2023; 29(16): 2495-2501
- URL: https://www.wjgnet.com/1007-9327/full/v29/i16/2495.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i16.2495
Endoscopic retrograde cholangiopancreatography (ERCP) has become the standard treatment for common bile duct (CBD) stones[1,2]. However, how to reduce radiation injury for special patients, including pregnant women and children, during this technique remains an important issue. Moreover, endoscopic sphincterotomy (EST), which is always necessary during stone extraction procedures, might lead to the loss of sphincter of Oddi (SO) function, some early adverse events, including bleeding and perforation, and some late adverse events, such as cholangitis, malignant degeneration and recurrent CBD stones, owing to free duodenobiliary reflux[3-5]. Importantly, EST was not appropriate for those patients who could not stop taking anti-coagulation/anti-platelet agents.
The emergence of peroral cholangioscopy made it possible to remove CBD stones under direct vison with less radiation injury[6,7]. However, the relatively difficult operation hindered the further development of this technique. In terms of EST, some studies introduce the self-expandable metal stent (SEMS) to avoid EST[8,9]. However, the SEMS was relatively too long and not desirable.
To overcome the problems mentioned above, we optimized the existing metal stent and made a kind of single dumbbell-style papillary support to facilitate cholangioscopy-assisted stone extraction, avoid EST and preserve SO function. In this study, we introduced cholangioscopy-assisted extraction through a novel papillary support (CETPS) for small-calibre and sediment-like CBD stones. This technique combined the advantages of the preservation of SO function and cholangioscopy-assisted stone extraction under direct vision with less radiation injury.
This retrospective study was approved by the Ethics Committee of the Chinese PLA General Hospital. Informed consent was obtained from all participating patients. Of note, some instruments, including the cholangioscope, basket and papillary support, were free for patients in this study.
Endoscopists made the clinical decision to perform CETPS for patients diagnosed with small-calibre (cross diameter ≤ 1.0 cm) or sediment-like CBD stones by magnetic resonance cholangiopancreatography (MRCP) and/or endoscopic ultrasound (EUS). Patients undergoing CETPS between July 2022 and September 2022 were enrolled in this study. Related data were extracted from a prospectively collected database.
The stone size was measured under MRCP on the maximal cross section. The definition of operation time was the course between the endoscope inserting into and withdrawing from the body. Technical success was defined as no residual stones in the CBD and left and right hepatic ducts, which was confirmed under cholangioscopy after stone extraction.
All procedures were performed by one endoscopist who has experience performing more than 2000 ERCP procedures in total.
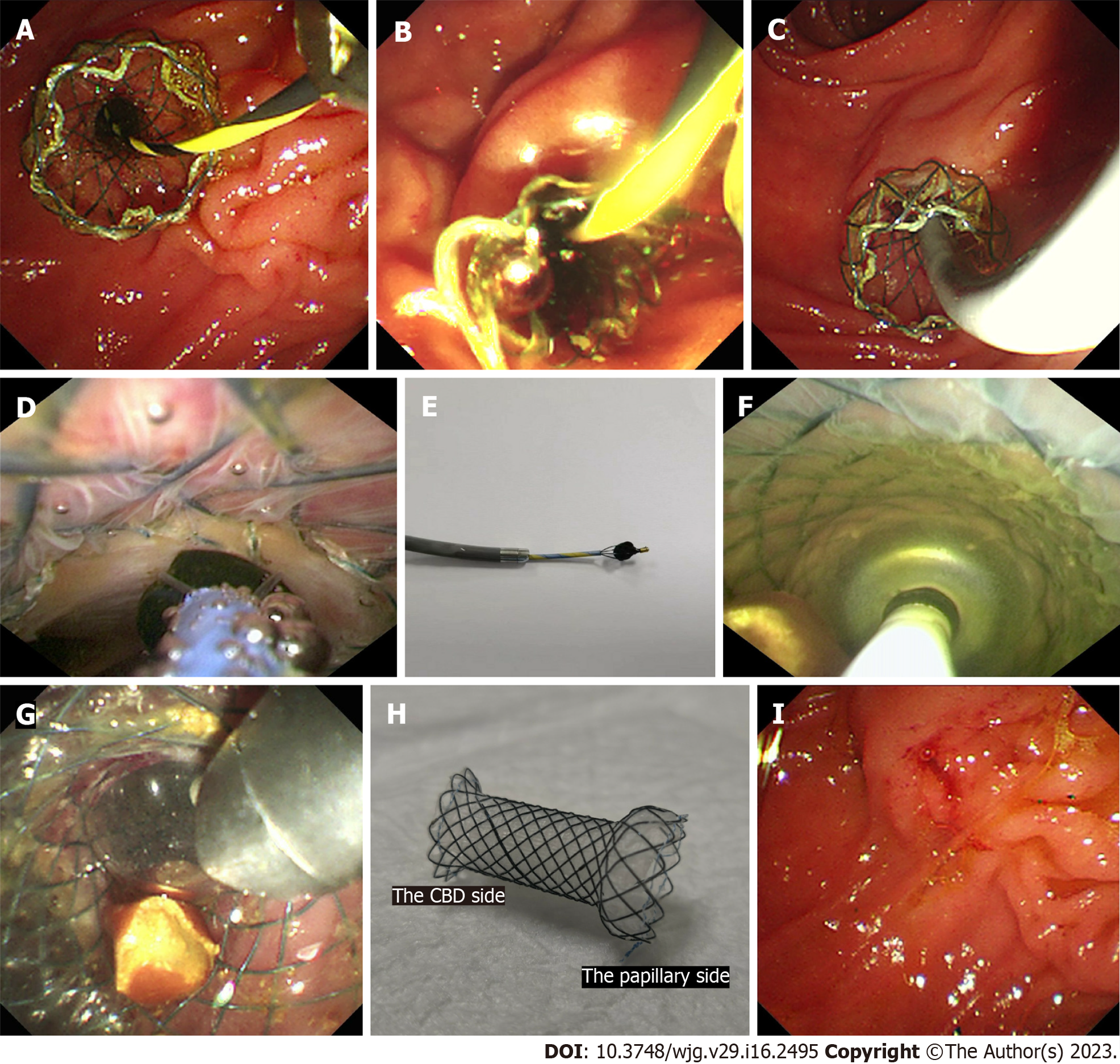
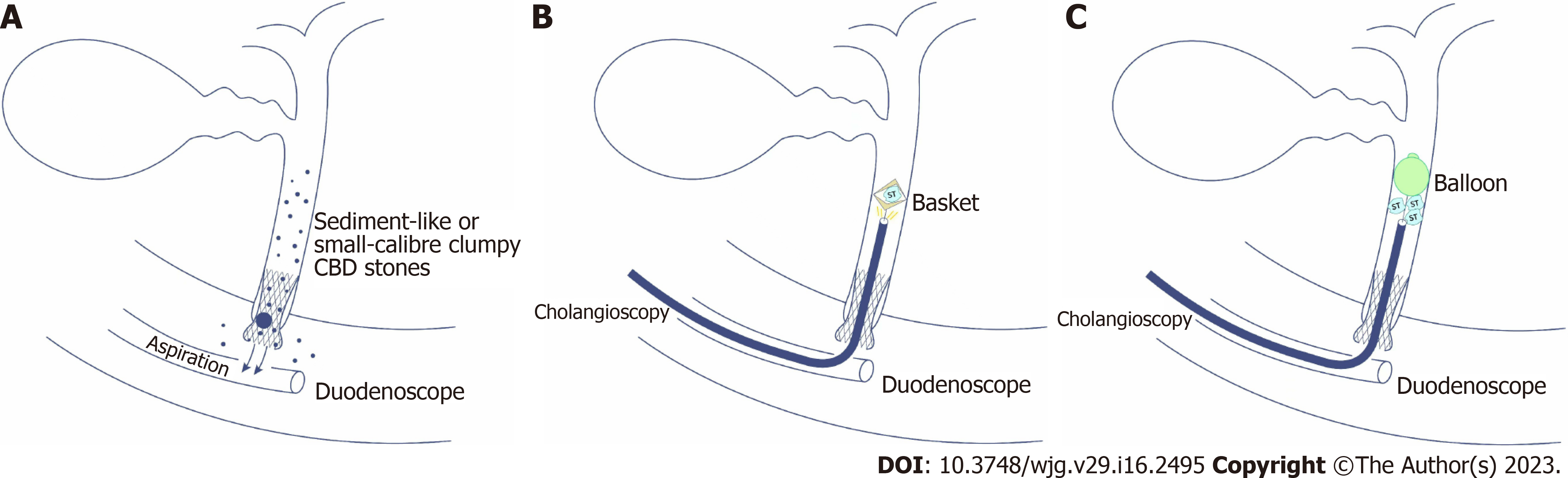
First, biliary intubation was conducted. Second, a covered single dumbbell-style support (12 mm in diameter, 25-30 mm in length) was placed in the distal CBD and papilla (Figure 1A). Third, for sediment-like CBD stones, endoscopic aspiration was performed under negative pressure (Figures 1B and 2A); for single clumpy CBD stones, a cholangioscope (Micro-Tech, eyeMax, 9F) was inserted into the CBD, and basket extraction was performed through the working tunnel of the cholangioscope under direct vision (Figures 1C-E, 2B and Video 1); for multiple clumpy CBD stones, a cholangioscope (Micro-Tech, eyeMax, 11F) was inserted into the CBD, and balloon extraction was performed through the working tunnel of the cholangioscope under direct vision (Figures 1F and G, 2C and Video 1). Fourth, the cholangioscope was inserted into the CBD again to confirm whether there were remnant stones. Finally, the papillary support was removed (Figure 1H and I).
Patients underwent routine blood examination and amylase and lipase tests 24 and 72 h postoperatively. Patients underwent computed tomography (CT) and/or endoscopy if abnormal symptoms or blood test parameters were found postoperatively.
Patients were fasted for 1 day after the procedure, and a liquid diet was followed for an additional 1 day if no adverse events occurred. The diet was gradually restored to normal starting on the third day. Postoperative medications mainly included a double-dose proton pump inhibitor and antibiotics for one day. Somatostatin was used if PEP occurred, and the fasting time was extended accordingly. Of note, of the 7 patients, 3 had gallstones and underwent cholecystectomy within 1 mo after CETPS to avoid the recurrence of CBD stones.
Follow-up with a routine duodenoscope was performed at 2 wk postoperatively to observe the papillary morphology.
In the article, PEP, postoperative bleeding, perforation and cholangitis were regarded as major adverse events. The diagnostic criteria of postoperative bleeding was based on the onset of clinical symptoms, including melena or haematemesis or a decrease > 2 g/dL in haemoglobin level. The present study used the diagnostic and classification criteria of PEP proposed by Cotton et al[10]: (1) New or worsened abdominal pain; (2) Serum amylase at least three times the upper limit of normal, measured more than 24 h after the procedure; and (3) New or prolonged hospitalization for at least 2 days.
Nonparametric data are expressed as medians.
Between July 2022 and September 2022, 7 patients underwent CETPS at the Chinese PLA General Hospital. Clinical characteristics and treatment outcomes for the 7 patients are shown in Table 1.
| Case No. | Age (yr)/sex | Chief complaint | Stone size (cm)1 | Stone colour | Number of stones | Operation time (min) | Balloon dilatation | Extraction method | Postoperative adverse events |
| 1 | 44/female | Abdominal pain | 0.6 | None | 1 | 64 | Yes | Aspiration | Postoperative pancreatitis |
| 2 | 54/female | Abdominal pain | 1.0 | Black grey | 1 | 53 | No | Basket | Hyperamylasaemia |
| 3 | 25/female | Abdominal pain | 0.4-0.6 | Brown | 5 | 45 | No | Balloon and aspiration | None |
| 4 | 68/male | Abdominal pain | 0.5 | Black | 1 | 87 | No | Basket | None |
| 5 | 29/female | Abdominal pain | Sediment-like | Yellow | Sediment-like | 13 | No | Aspiration | None |
| 6 | 83/male | Abdominal pain | Sediment-like | Yellow | Sediment-like | 31 | No | Aspiration | Hyperamylasaemia |
| 7 | 32/female | Abdominal pain | 0.5 cm | Yellow | 1 | 39 | No | Aspiration | None |
A total of 2 patients had yellow sediment-like CBD stones, and aspiration extraction was performed after the insertion of papillary support. Of the 5 patients with clumpy CBD stones (0.4-1.0 cm), 2 underwent basket extraction under direct vision for a single stone (0.5-1.0 cm, black and black grey), 1 underwent balloon plus aspiration extraction under direct vision for 5 stones (0.4-0.6 cm, brown), and 2 underwent aspiration extraction only for a single stone (0.5-0.6 cm, yellow, none).
Technical success, namely, no residual stones in the CBD or left and right hepatic ducts, was achieved in all 7 cases (100%). The median operating time was 45.0 min (range 13.0–87.0 min).
Mild PEP occurred in one case (14.3%). Hyperamylasaemia without abdominal pain was noted in 2 of 7 patients. No residual stones or cholangitis were found during the follow-up.
In one case, the papillary support was dilated by an extraction balloon before the insertion of the cholangioscope, given that the papillary was not dilated enough after the insertion of support.
This study showed that CETPS appears to be a feasible and safe treatment option for small-calibre (cross diameter ≤ 1.0 cm) or sediment-like CBD stones with a 100.0% (7/7) technical success rate and a 14.3% (1/7) PEP rate without other adverse events, such perforation, bleeding and cholangitis.
The major advantage of CETPS over ERCP with EST for CBD stones is that SO function is retained, avoiding relevant adverse events, including bleeding, perforation, malignant degeneration and recurrent CBD stones[11-13]. Jun et al[8] has confirmed that the use of transpapillary SEMSs was effective in the preservation of SO function. Moreover, Cho et al[9] concluded that SEMSs can be used for the extraction of CBD stones in patients on dual antiplatelet agents and do not lead to haemorrhagic or thromboembolic events. Of note, the papillary support introduced in the present study has the following merits compared with the SEMSs used in previous studies[8,9]: (1) The novel papillary support was shorter (25-30 mm) than other SEMSs (40-50 mm); (2) the CBD side of the support had a 70-degree angle; and (3) the papillary side of the support had a single dumbbell-style design. In the case of distal stones, the stones might get stuck in the middle between the relatively long SEMS and CBD wall after stent insertion, so Jun et al[8] recommended that the patient’s position should be tilted to move the stones from the distal CBD to mid-CBD before stent insertion, although it did not always work. Therefore, we designed a support with a shorter length (25-30 mm) and 70-degree angle on the CBD side (Figure 1H), which could lift the stones into the proximal CBD during the process of stent insertion. On the other hand, the single dumbbell-style design (Figure 1H) on the papillary side could protect the support from entering the CBD due to the persistent friction from the cholangioscope. In terms of the PEP, this study presented a reasonable 14.3% (1/7) rate. Theoretically, the use of support could avoid the unintentional PD insertion of the instructions for stone extraction, which might reduce the PEP rate; however, excessive squeezing from the support would induce PEP. Our next method to improve the support is finding the optimal balance between a sufficient support force and a reasonable PEP rate.
Another important advantage of CETPS over traditional ERCP is how the treatment operation is under direct vision. First, radiation injury for patients and surgeons could be minimized, and special patients, including pregnant women and children, could benefit from this technique. Second, the basket and balloon, designed for cholangioscopy, could be opened in the most appropriate position and frap/hold the stones in a timely manner under direct vison. Moreover, operators could find related adverse events, including CBD perforation, bleeding and injury, in a timely manner.
As mentioned above, CETPS combined the advantages of the SEMS technique with the SO function preservation and the cholangioscopy-assisted treatment operation under direct vision. Moreover, the application of novel papillary support established a smooth passageway for the ingress and egress of the cholangioscope and thus facilitated the operation of cholangioscopy-assisted extraction.
The major limitation of our study was the relatively small sample size. However, this paper introduced a novel papillary support that avoids EST during ERCP. Moreover, cholangioscopy-assisted stone extraction using a balloon under direct vision (Table 1, case 3) has not yet been reported.
In conclusion, CETPS seemed to be a new, feasible and safe treatment strategy for small-calibre (cross diameter ≤ 1.0 cm) or sediment-like CBD stones. Patients, especially pregnant women and those who cannot stop taking anti-coagulation/anti-platelet agents, could benefit from this technique because of the visualized operation and absence of EST. However, further prospective studies with larger populations and longer follow-up periods are warranted.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Chinese Society of Digestive Endoscopy, President.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: De Luca L, Italy; Demirli Atici S, Turkey S-Editor: Ma YJ L-Editor: A P-Editor: Zhao S
| 1. | Cotton PB. Fifty years of ERCP: a personal review. Gastrointest Endosc. 2018;88:393-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Arvanitakis M, Devière J. Endoscopic retrograde cholangiopancreatography (ERCP). Endoscopy. 2009;41:890-894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ, Lande JD, Pheley AM. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1716] [Cited by in RCA: 1689] [Article Influence: 58.2] [Reference Citation Analysis (2)] |
| 4. | Frimberger E. Long-term sequelae of endoscopic papillotomy. Endoscopy. 1998;30:A221-A227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Hawes RH, Cotton PB, Vallon AG. Follow-up 6 to 11 years after duodenoscopic sphincterotomy for stones in patients with prior cholecystectomy. Gastroenterology. 1990;98:1008-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 132] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 6. | Han S, Shah RJ. Cholangioscopy-guided basket retrieval of impacted stones. VideoGIE. 2020;5:387-388. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Fejleh MP, Thaker AM, Kim S, Muthusamy VR, Sedarat A. Cholangioscopy-guided retrieval basket and snare for the removal of biliary stones and retained prostheses. VideoGIE. 2019;4:232-234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Jun CH, Park CH, Jeon J, Park IH, Lee HJ, Park SY, Kim HS, Choi SK, Rew JS. Feasibility of self-expandable metal stents for preservation of sphincter of Oddi function in patients with common bile duct stones: a pilot study. Gastrointest Endosc. 2015;82:719-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Cho E, Park CH, Jun CH, Kim HS, Choi SK, Rew JS. Self-expandable metal stents for the extraction of common bile duct stones in patients receiving dual antiplatelet agents: a pilot study. Surg Endosc. 2018;32:1077-1081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1890] [Cited by in RCA: 2036] [Article Influence: 59.9] [Reference Citation Analysis (1)] |
| 11. | Geenen JE, Toouli J, Hogan WJ, Dodds WJ, Stewart ET, Mavrelis P, Riedel D, Venu R. Endoscopic sphincterotomy: follow-up evaluation of effects on the sphincter of Oddi. Gastroenterology. 1984;87:754-758. [PubMed] |
| 12. | Pereira-Lima JC, Jakobs R, Winter UH, Benz C, Martin WR, Adamek HE, Riemann JF. Long-term results (7 to 10 years) of endoscopic papillotomy for choledocholithiasis. Multivariate analysis of prognostic factors for the recurrence of biliary symptoms. Gastrointest Endosc. 1998;48:457-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 140] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 13. | Escourrou J, Cordova JA, Lazorthes F, Frexinos J, Ribet A. Early and late complications after endoscopic sphincterotomy for biliary lithiasis with and without the gall bladder 'in situ'. Gut. 1984;25:598-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 171] [Article Influence: 4.2] [Reference Citation Analysis (0)] |