Published online Apr 21, 2023. doi: 10.3748/wjg.v29.i15.2349
Peer-review started: January 15, 2023
First decision: February 7, 2023
Revised: February 20, 2023
Accepted: March 29, 2023
Article in press: March 29, 2023
Published online: April 21, 2023
Processing time: 88 Days and 21.5 Hours
For recurrent achalasia after initial peroral endoscopic myotomy (POEM) failure, repeat POEM (Re-POEM) has been reported as a treatment option. However, severe esophageal interlayer adhesions caused by previous procedures impede the successful establishment of a submucosal tunnel and lead to aborted Re-POEM procedures. Our team previously described POEM with simultaneous submucosal and muscle dissection (POEM-SSMD) as a feasible solution for achalasia with severe interlayer adhesions.
To investigate the effectiveness and safety of Re-POEM with simultaneous submucosal and muscle dissection (Re-POEM-SSMD).
A total of 1049 patients with achalasia who underwent successful endoscopic myotomy at the Digestive Endoscopic Center of Chinese PLA General Hospital from December 2014 to May 2022 were reviewed. Patients with recurrent achalasia who experienced initial POEM clinical failure were retrospectively included in this study. The primary endpoint was retreatment clinical success, defined as an Eckardt score ≤ 3 during the postretreatment follow-up and no need for additional treatment. Procedure-related adverse events, changes in mano
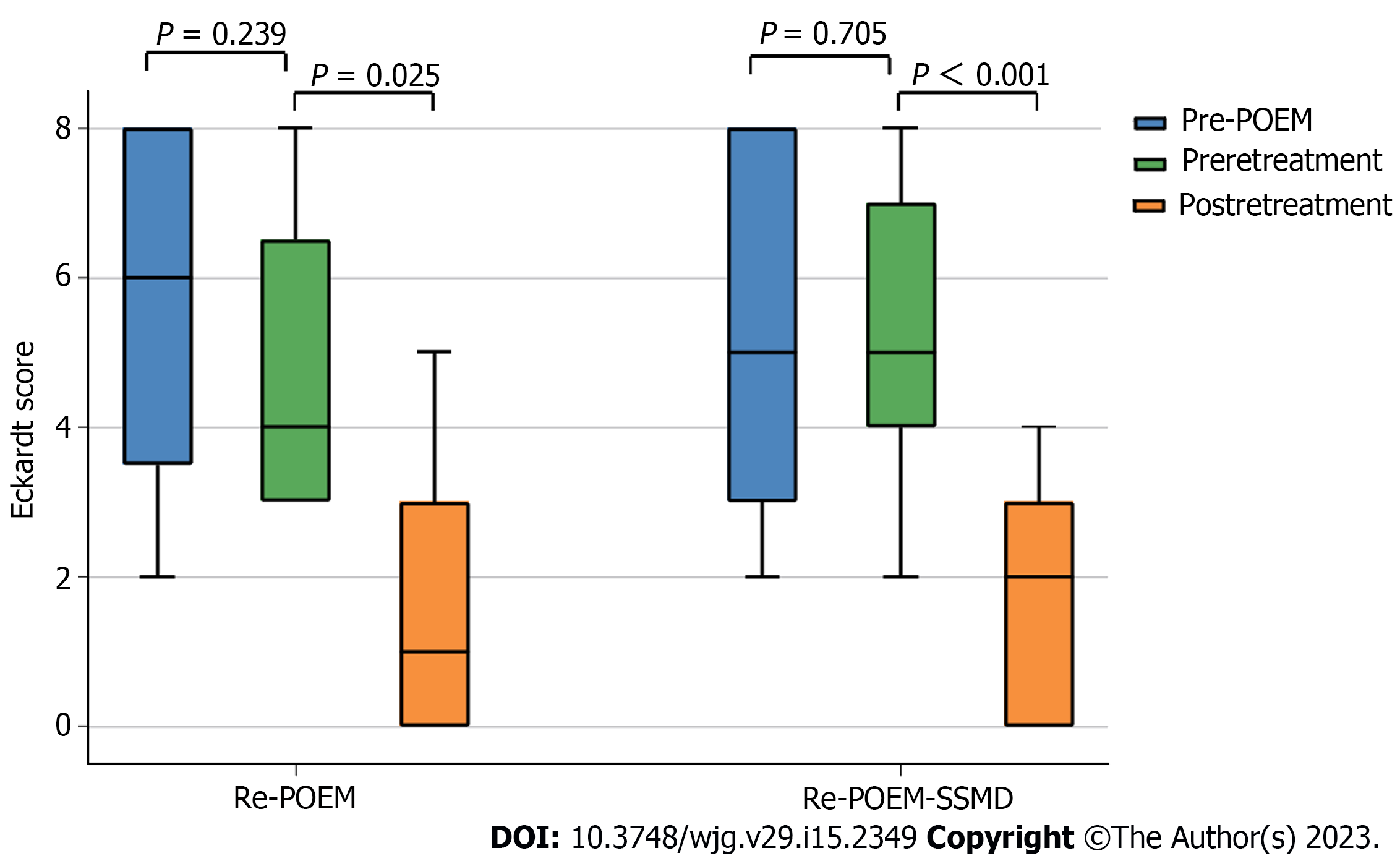
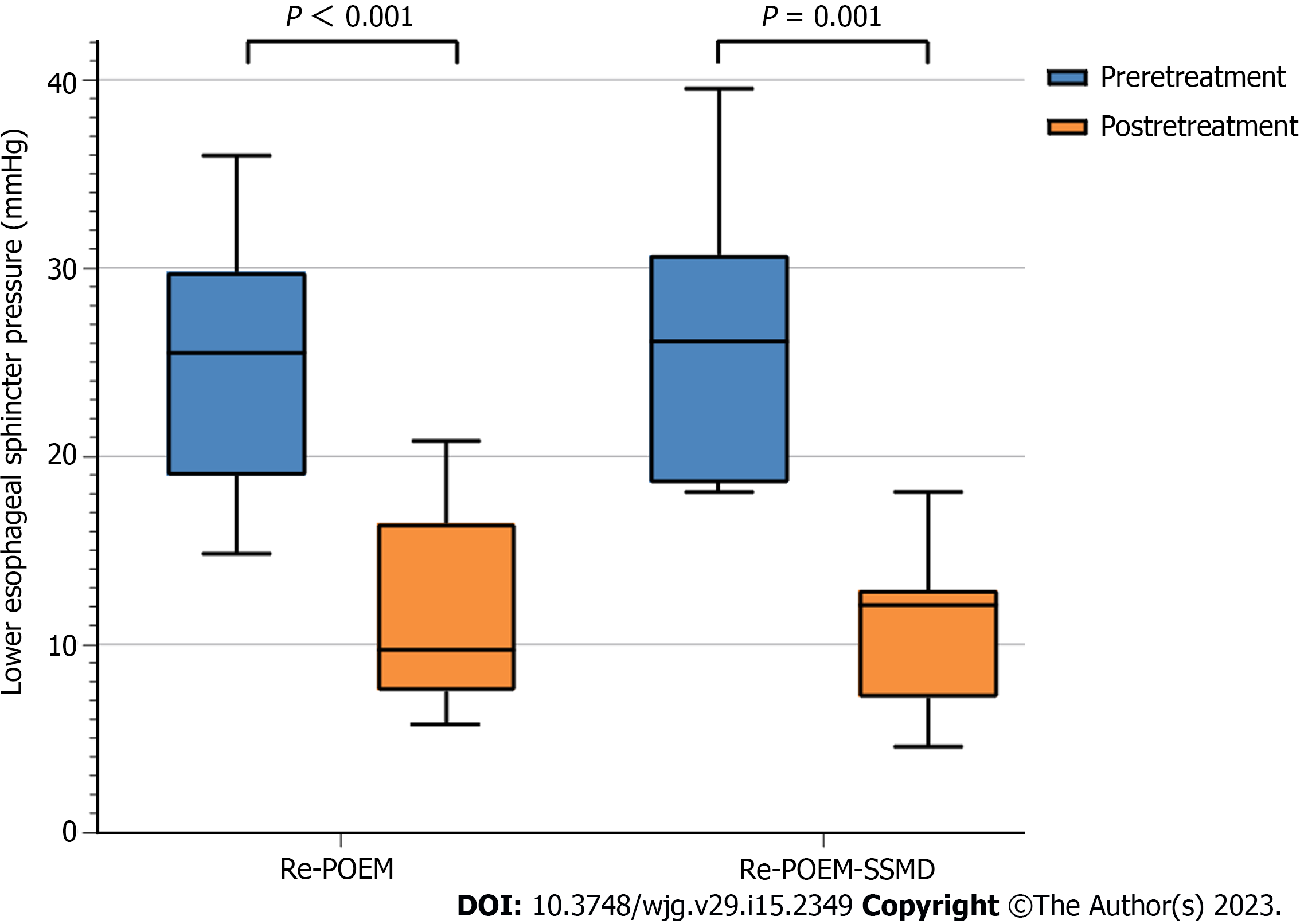
Sixteen patients underwent Re-POEM (9 patients) or Re-POEM-SSMD (7 patients) successfully at a median of 45.5 mo (range, 4-95 mo) after initial POEM. During a median follow-up period of 31 mo (range, 7-96 mo), clinical success (Eckardt score ≤ 3) was achieved in 8 (88.9%) and 6 (85.7%) patients after Re-POEM and Re-POEM-SSMD, respectively (P = 0.849). The median Eckardt score dropped from 4 (range, 3-8) at preretreatment to 1 (range, 0-5) at postretreatment in the Re-POEM group (P = 0.025) and from 5 (range, 2-8) to 2 (range, 0-4) in the Re-POEM-SSMD group (P < 0.001). The mean manometric LES pressure decreased from 23.78 ± 9.04 mmHg to 11.45 ± 5.37 mmHg after Re-POEM (P < 0.001) and from 26.80 ± 7.48 mmHg to 11.05 ± 4.38 mmHg after Re-POEM-SSMD (P < 0.001). No serious adverse events were recorded in both groups.
In conclusion, Re-POEM-SSMD appears to be a safe and effective salvage therapy for recurrent achalasia with severe interlayer adhesions.
Core Tip: For recurrent achalasia after initial peroral endoscopic myotomy (POEM) failure, repeat POEM (Re-POEM) has been reported as a potential treatment option. However, severe interlayer adhesions caused by previous procedures impede the successful establishment of a submucosal tunnel. In this study, we retrospectively analyzed the data of patients who had persistent or recurrent symptoms after initial POEM and underwent Re-POEM or Re-POEM with simultaneous submucosal and muscle dissection (Re-POEM-SSMD). The results show that Re-POEM-SSMD could serve as an effective and safe salvage option for patients with recurrent achalasia when conventional POEM procedures are impeded by severe interlayer adhesions.
- Citation: Lin YJ, Liu SZ, Li LS, Han K, Shao BZ, Linghu EQ, Chai NL. Repeat peroral endoscopic myotomy with simultaneous submucosal and muscle dissection as a salvage option for recurrent achalasia. World J Gastroenterol 2023; 29(15): 2349-2358
- URL: https://www.wjgnet.com/1007-9327/full/v29/i15/2349.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i15.2349
Achalasia is an uncommon esophageal motor disorder estimated to affect 2 to 3 people per 100000 people in the general population and is caused by failure of adequate relaxation of the lower esophageal sphincter (LES) and impaired esophageal peristalsis[1]. Treatment options mainly include endoscopic botulinum toxin injection, laparoscopic Heller’s myotomy (LHM), pneumatic dilation (PD) and peroral endoscopic myotomy (POEM) and aim to relax or cause a mechanical disruption of the LES in order to achieve symptom relief and restore quality of life[2].
POEM is a super minimally invasive surgery (SMIS) with transesophageal tunnelling endoscopic myotomy and has been used to treat achalasia since 2010[3]. Because of digestive endoscopic tunnel techniques (DETTs), diseases such as achalasia that were previously treated surgically can now be treated endoscopically by creating a submucosal tunnel as a surgical space[4]. Based on results from a multitude of retrospective studies, the clinical success rate of POEM for achalasia treatment exceeds 90%, with only approximately 5%-10% of patients remaining symptomatic postoperatively[5-7].
Recently, repeat POEM (Re-POEM) has been reported as an endoscopic therapeutic option for patients with persistent or recurrent symptoms of achalasia after POEM[8,9]. However, severe interlayer adhesions in the submucosa caused by previous POEM could hinder the establishment of a submucosal tunnel and therefore increase the procedural difficulty of RE-POEM. Coincidentally, we previously reported POEM with simultaneous submucosal and muscle dissection (POEM-SSMD) as a treatment option for patients with achalasia and severe interlayer adhesions[10]. Herein, we retrospectively compared Re-POEM and Re-POEM with simultaneous submucosal and muscle dissection (Re-POEM-SSMD) as a salvage therapy for patients with prior failed POEM procedures in terms of clinical efficacy and safety.
We reviewed 1049 patients with achalasia who underwent successful endoscopic myotomy (POEM, Re-POEM and Re-POEM-SSMD) at the Digestive Endoscopic Center of Chinese PLA General Hospital from December 2014 to May 2022. Patients with recurrent acha
The standard endoscopic procedures were performed by two senior endoscopists with sufficient experience in therapeutic endoscopy as previously described[12]. Patients were kept in the supine position with the right shoulder elevated. Re-POEM or Re-POEM-SSMD was performed using a single-channel high-definition gastroscope and carbon dioxide (CO2) gas for insufflation during the procedure.
During the Re-POEM procedure, the scarred area was avoided in the opposite orientation of the initial POEM site to allow the establishment of a new submucosal tunnel. When severe interlayer adhesions impeded the establishment of new submucosal tunnel, Re-POEM-SSMD was performed to dissect the submucosa and muscle synchronously as we described previously[13].
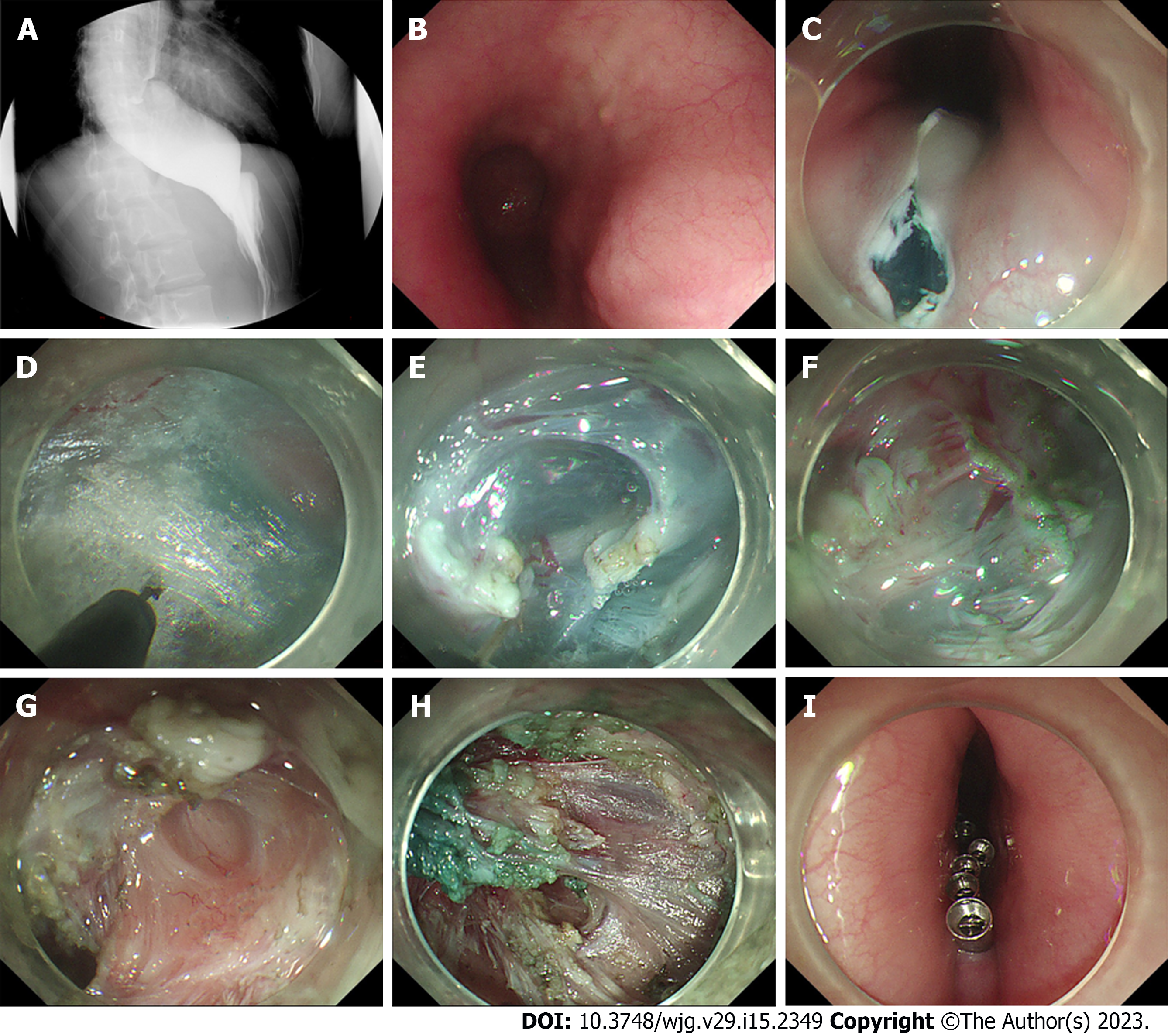
The sequential steps were generally performed as follows: (1) The submucosal space was created by injecting methylene blue saline solution to create a liquid mat, and then an inverse T incision was made for tunnel entry; (2) the extended submucosal tunnel was terminated at the lesser curvature of the cardia (Re-POEM) or as far as possible due to the interlayer adhesions (RE-POEM-SSMD); (3) a circumferential layer myotomy was performed at the proximal esophagus and a full-thickness myotomy was performed extended to 2-3 cm below the cardia (Re-POEM), or the submucosa and muscle were incised simultaneously and a full-thickness myotomy was performed 2-3 cm below the cardia without impairing the mucosa (RE-POEM-SSMD); and (4) then the mucosal incision site was sealed using endoscopic metal clips after hemostasis was achieved.
All patients were observed for gas-related adverse events such as subcutaneous emphysema, pneumothorax or pneumoperitoneum to confirm the absence of gas leakage. After the procedure, dietary restrictions were enforced, and proton pump inhibitors (PPIs) and antibiotics were routinely administered intravenously. Upon discharge, patients were instructed to continue taking oral PPIs and adhere to a soft diet for at least four weeks.
The primary endpoint was retreatment clinical success, which was defined as an Eckardt score of ≤ 3 during the postprocedure follow-up and no need for additional treatment. Secondary outcome measures were procedure-related adverse events, changes in manometric LES pressure and Eckardt score, reflux complications after retreatment, and procedure-related parameters such as operative time, tunnel length, myotomy length and length of hospital stay.
LES pressures before and after retreatment were recorded by using a high-resolution manometry (HRM) system at 1-cm intervals with high-fidelity circumferential sensors (ManoScan; Sierra Scientific Instruments Inc, Los Angeles, CA, United States) as we previously described[12]. HRM was performed with patients in a supine position after a minimum of 6 hours of fasting. Pressure data of 10 wet swallows were recorded and analyzed with Mano-View software. Ling classification of achalasia, which is used to describe the endoscopic morphology of the esophageal lumen, was recorded as we previously described[14].
Upper gastrointestinal endoscopic evaluation including monitoring of wound healing and examination of objective signs of reflux esophagitis and HRM were scheduled at 3, 6 and 12 mo post retreatment. Patient-reported outcomes such as Eckardt scores and symptomatic reflux were recorded in the outpatient clinic or by telephone at 3, 6 and 12 mo and then annually thereafter.
The results were expressed as the mean with a standard deviation (SD) or median with a range for quantitative data and numbers with percentages for categorical data. Student’s t test and the Mann–Whitney U test were used to compare baseline characteristics (other than sex), operation parameters, Eckardt score and LES pressure between the Re-POEM and Re-POEM-SSMD groups. Fisher’s exact test was used to compare sex, clinical success and reflux complications between the Re-POEM and Re-POEM-SSMD groups. The Friedman Test was used to compare the baseline, preretreatment and postretreatment Eckardt score and Paired Student’s t test was used to compare preretreatment and postretreatment LES pressure. All reported P values were two-tailed, with statistical significance set at P < 0.05. Statistical analyses were performed using SPSS software (version 26.0; SPSS, Chicago, IL, United States).
Sixteen patients (9 male, 7 female; mean age 43.4 ± 16.3 years) who experienced initial POEM clinical failure were diagnosed with recurrent achalasia. The median duration of dysphagia was 86.5 mo (range, 16-420 mo). Symptoms of achalasia recurred a median time of 15.5 mo (range, 0-92 mo) after initial POEM. Retreatment procedures were conducted after a mean of 45.5 mo (range, 4-95 mo) following the initial POEM. According to the Ling classification, 2 patients (12.5%), 5 patients (31.3%), 1 patient (6.3%), 5 patients (31.3%) and 3 patients (18.8%) had Ling I, Ling IIa, Ling IIb, Ling IIc and Ling IIIr types, respectively (Table 1).
| Total (n = 16) | Re-POEM (n = 9) | Re-POEM-SSMD (n = 7) | P value | |
| Age, mean ± SD, yr | 43.4 ± 16.3 | 43.0 ± 15.4 | 43.86 ± 18.7 | 0.916 |
| Male, n (%) | 9 (56.3) | 4 (44.4) | 5 (71.4) | 0.008 |
| Duration of dysphagia, median (range), mo | 86.5 (16-420) | 92 (16-147) | 24 (16-420) | 0.751 |
| Time symptoms recurred after initial POEM, median (range), mo | 15.5 (0-92) | 12 (0-92) | 7.5 (0-50) | 0.414 |
| Interval between initial POEM and Re-POEM, median (range), mo | 45.5 (4-95) | 64 (14-95) | 9 (4-60) | 0.013 |
| Achalasia endoscopy type, n (%) | ||||
| Ling I | 2 (12.5) | 2 (22.2) | 0 (0) | |
| Ling IIa | 5 (31.3) | 3 (33.3) | 2 (28.6) | |
| Ling IIb | 1 (6.3) | 0 (0) | 1 (14.3) | |
| Ling IIc | 5 (31.3) | 3 (33.3) | 2 (28.6) | |
| Ling IIIr | 3 (18.8) | 1 (11.1) | 2 (28.6) |
Re-POEM (9 patients) and Re-POEM-SSMD (7 patients) procedures were conducted successfully in all patients. A representative case of Re-POEM-SSMD is described in Figure 1. The mean operative time was 39.22 ± 15.19 min in the Re-POEM group and 47.86 ± 9.71 min in the Re-POEM-SSMD group (P = 0.414). The median lengths of the submucosal tunnel and myotomy were 9 cm (range, 7-13 cm) and 6 cm (range, 4.5-11 cm) in the Re-POEM group and 5 cm (range, 4-12 cm) (P = 0.012) and 6 cm (range, 4-11 cm) (P = 1.000) in the Re-POEM-SSMD group, respectively. Prophylactic antibiotics were administered for 3 to 6 d after the procedures. The average length of hospital stay was 6.0 ± 1.7 d and 7.1 ± 1.3 d after Re-POEM and Re-POEM-SSMD, respectively (P = 0.454). Regarding procedure-related adverse events, computed tomography showed pneumoperitoneum in two patients in the Re-POEM group but no apparent clinical consequence occurred during later follow-up. One patient in the Re-POEM-SSMD group sustained mucosal perforation during submucosal tunnel construction and was treated by endoscopic metal clips, no additional clinical complications were observed (Table 2).
| Re-POEM (n = 9) | Re-POEM-SSMD (n = 7) | P value | |
| Operation parameters | |||
| Operative time, mean ± SD, min | 39.22 ± 15.19 | 47.86 ± 9.71 | 0.414 |
| Submucosal tunnel length, median (range), cm | 9 (7-13) | 5 (4-12) | 0.012 |
| Myotomy length, median (range), cm | 6 (4.5-11) | 6 (4-11) | 1.000 |
| Postoperative hospital stay, mean ± SD, d | 6.0 ± 1.7 | 7.1 ± 1.3 | 0.454 |
| Adverse events, n | |||
| Mucosal injury | 0 | 1 | |
| Subcutaneous emphysema | 0 | 0 | |
| Pneumothorax | 0 | 0 | |
| Pneumoperitoneum | 2 | 0 | |
| Tunnel infection | 0 | 0 | |
| Clinical success during follow-up, n (%) | 8 (88.9) | 6 (85.7) | 0.849 |
| Eckardt score, median (range) | |||
| Pre-POEM | 6 (2-8) | 5 (2-8) | 0.892 |
| Preretreatment | 4 (3–8) | 5 (2-8) | 0.425 |
| Postretreatment | 1 (0-5) | 2 (0-4) | 0.416 |
| Lower esophageal sphincter pressure, mean ± SD, mmHg | |||
| Preretreatment | 23.78 ± 9.04 | 26.80 ± 7.48 | 0.489 |
| Postretreatment | 11.45 ± 5.37 | 11.05 ± 4.38 | 0.872 |
| Reflux complications | |||
| Symptomatic reflux, n (%) | 6 (66.7) | 0 (0) | 0.001 |
| R, n (%) | 6 (66.7) | 3 (42.9) | 0.100 |
During a median follow-up period of 31 mo (range, 7-96 mo), clinical success (Eckardt score ≤ 3) was achieved in 8 (88.9%) and 6 (85.7%) patients after Re-POEM and Re-POEM-SSMD, respectively (P = 0.849). None of the patients underwent balloon dilation, temporary esophageal stent placement, or botulinum toxin injections after POEM or retreatment. One patient in the Re-POEM group had recurrent symptoms of achalasia and chose a follow-up strategy. Reintervention was performed in 1 patient in the Re-POEM-SSMD group for recurrent symptoms (Table 2).
The median Eckardt score dropped from 4 (range, 3-8) at preretreatment to 1 (range, 0-5) at postretreatment in the Re-POEM group (P = 0.025) and from 5 (range, 2-8) to 2 (range, 0-4) in the Re-POEM-SSMD group (P < 0.001) (Figure 2). The mean manometric LES pressure decreased from 23.78 ± 9.04 mmHg to 11.45 ± 5.37 mmHg after Re-POEM (P < 0.001) and from 26.80 ± 7.48 mmHg to 11.05 ± 4.38 mmHg after Re-POEM-SSMD (P < 0.001) (Figure 3).
At the follow-up EGD, no severe complications, such as delayed bleeding or mucosal barrier failure, were detected. The overall rate of clinical reflux complications following retreatment was 56.3% (9/16). Six patients developed symptomatic gastroesophageal reflux such as heartburn and reflux after Re-POEM and were treated by intermittent administration of standard-dose PPI. Reflux esophagitis was detected in six patients (Los Angeles classification A, 2; B, 1; C, 3) in the Re-POEM and three (Los Angeles classification B, 1; C, 2) in the Re-POEM-SSMD group (P = 0.100).
Although POEM is highly effective as a first-line treatment for achalasia, a small percentage of patients remain symptomatic or experience relapse after POEM[15,16]. Inadequate myotomy below the EGJ, premature fusion healing and early myotomy site scarring may be the main causes of recurrent dysphagia in POEM patients. Prior botulinum toxin injections and balloon dilations may also lead to substantial fibrosis, making myotomy more difficult. Consensus on the optimal management strategy for patients with recurrent achalasia after initial POEM failure has not yet been reached.
Re-POEM after failed surgical Heller myotomy has been reported to have good short-term results[17,18]. Recently, Re-POEM has also been described as an effective endoscopic therapy for the treatment of achalasia after failed initial POEM procedures with clinical success rates ranging from 63%-100%[8,19]. Moreover, Ichkhanian et al[9] reported that when compared with pneumatic dilation and LHM, Re-POEM had a higher clinical success rate in the management of patients with failed initial POEM. As a SMIS, Re-POEM is less invasive compared to Heller myotomy and requires fewer attempts compared to balloon dilation. In this retrospective study, we found that Re-POEM had a clinical success rate of 88.9% for recurrent achalasia after initial POEM failure, which is similar to that reported in previous studies.
In POEM procedures, submucosal tunnel dissection and endoscopic myotomy must extend deep beyond the gastroesophageal junction (at least 2 cm) to guarantee the success of POEM[16]. Re-POEM is technically challenging due to the presence of post-POEM interlayer adhesions and fibrosis and is usually performed using a new submucosal tunnel in a relatively unobstructed area to avoid contact with the previous procedure site. The presence of severe esophageal interlayer adhesions impede the establishment of a new submucosal tunnel. In 2014, our team introduced a novel, modified procedure, entitled POEM-SSMD, to address severe interlayer adhesions[10]. As a result of the procedure, the long-term symptom relief rate was 83% with controllable adverse events for patients with achalasia and severe interlayer adhesions[13]. Interlayer adhesions are more common in patients with recurrent achalasia who underwent initial POEM than in patients with untreated achalasia. Re-POEM-SSMD can be performed in the scar area of an earlier myotomy site without considering the adhesions or fibrosis from the previous operation, which makes it easier for the endoscopist to select the preferred direction of the myotomy. Based on our data, Re-POEM-SSMD had a comparable clinical success rate of 85.7% and could serve as an effective salvage option when conventional endoscopic procedures are impeded by severe interlayer adhesions caused by previous POEM procedures.
The orientation selection of Re-POEM and whether to use SSMD operation depends on the preference of the endoscopists and their own technical levels. Before retreatment, mucosal inflammation and submucosal fibrosis of the esophagus are classified to determine the degree of adhesion[20]. If the initial operative region has obvious adhesions and the rest of esophagus has no or mild adhesions, another tunnel can be created at the contralateral esophagus to improve the success rate of Re-POEM. If the esophagus has severe and extensive adhesions and performing SSMD is necessary, the endoscopist can choose to create a tunnel at the original procedure site, which usually means a relatively comfortable operative orientation and may help to improve the technical success rate.
In the Re-POEM-SSMD group, due to the presence of post-POEM adhesions and fibrosis, the submucosa and muscle layer are cut simultaneously from the adhesion site with aborted intended termination point of the submucosal tunnel, leading to a shorter submucosal tunnel than that created in conventional RE-POEM procedures.
The incidence of major adverse events such as vital-sign instability and intensive care unit stay ranged between 2% and 4% in the published literature[21-23]. No major adverse events were recorded in both groups of our study. A rupture in the mucosa may compromise its integrity and lead to esophageal leakage and secondary infection, which should be managed appropriately once identified. One mucosal injury in the Re-POEM-SSMD group was successfully managed with secure closure and sufficient drainage without the need for surgical repair. The incision made at the tunnel entry site in the mucosa should be tightly clipped after myotomy. CO2 should be used as the insufflation gas and a lower flow should be used sparingly once the creation of the submucosal tunnel or SSMD is started. In our study, two cases of pneumoperitoneum in the Re-POEM group were recorded but no apparent clinical consequence occurred during later follow-up. It should be noted that Re-POEM-SSMD should be performed by endoscopists with sufficient experience in therapeutic endoscopy and after preparation for all contingencies.
Gastroesophageal reflux and Barrett’s esophagus are usually considered long-term major concerns after POEM with no antireflux procedure[15]. Our study showed that fewer cases of symptomatic reflux occurred in the Re-POEM-SSMD group than in the Re-POEM group. Re-POEM-SSMD was more likely to be performed in the earlier myotomy site, while Re-POEM was usually performed in the opposite direction with a new myotomy site. Therefore, in Re-POEM-SSMD, less damage to the muscular layer may be responsible for less symptomatic reflux. Nevertheless, follow-up EGD showed no difference in postretreatment LES pressure or incidence of esophagitis between the two groups. Therefore, the results should be interpreted with caution and effectiveness of Re-POEM-SSMD in reducing reflux must be verified in prospective studies with large samples.
There are several limitations to the current study. For instance, a small sample of patients were classified into two groups, so a subgroup analysis of the Ling classification could not be performed. Moreover, the retrospective nature of the study and variable duration of follow-up were also limitations. There was also a potential for patient selection bias.
In conclusion, Re-POEM-SSMD appears to be a safe and effective salvage option for recurrent achalasia with adhesions or fibrosis caused by previous POEM procedures, thereby broadening the applicability of Re-POEM to patients after failed POEM. We are awaiting the results of the RCT and long-term follow-up.
For recurrent achalasia after initial peroral endoscopic myotomy (POEM) failure, repeat POEM (Re-POEM) has been reported as a treatment option.
Interlayer adhesions caused by previous POEM procedures are common, which could impede the establishment of a submucosal tunnel and even lead to aborted Re-POEM procedures.
This study aimed to evaluate the efficacy and safety of Re-POEM with simultaneous submucosal and muscle dissection (Re-POEM-SSMD) as a salvage therapy for recurrent achalasia with severe esophageal interlayer adhesions after prior failed POEM procedures.
Patients diagnosed with recurrent achalasia who underwent Re-POEM or Re-POEM-SSMD in our center were retrospectively analyzed in terms of clinical efficacy, incidence of procedure-related adverse events and reflux complications.
Clinical success (Eckardt score ≤ 3) was achieved in 8 (88.9%) patients after Re-POEM and 6 (85.7%) patients after Re-POEM-SSMD (P = 0.849). No severe adverse events were recorded in both groups.
Re-POEM-SSMD could serve as a safe and effective salvage therapy for recurrent achalasia with severe interlayer adhesions.
Further studies in large-scale patient population and prospective studies are required to verify the efficacy and safety of Re-POEM-SSMD in the management of patients after failed POEM. Further evaluation of the validity of Re-POEM-SSMD in reducing reflux is also awaited.
We thank our peer reviewers for the insightful and thorough suggestions on this manuscript.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hakimi T, Afghanistan; Herbella FAM, Brazil; Vyshka G, Albania S-Editor: Yan JP L-Editor: A P-Editor: Cai YX
| 1. | Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet. 2014;383:83-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 390] [Cited by in RCA: 428] [Article Influence: 38.9] [Reference Citation Analysis (0)] |
| 2. | Eckardt AJ, Eckardt VF. Treatment and surveillance strategies in achalasia: an update. Nat Rev Gastroenterol Hepatol. 2011;8:311-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 115] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 3. | Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1168] [Cited by in RCA: 1234] [Article Influence: 82.3] [Reference Citation Analysis (1)] |
| 4. | Chai NL, Li HK, Linghu EQ, Li ZS, Zhang ST, Bao Y, Chen WG, Chiu PW, Dang T, Gong W, Han ST, Hao JY, He SX, Hu B, Huang XJ, Huang YH, Jin ZD, Khashab MA, Lau J, Li P, Li R, Liu DL, Liu HF, Liu J, Liu XG, Liu ZG, Ma YC, Peng GY, Rong L, Sha WH, Sharma P, Sheng JQ, Shi SS, Seo DW, Sun SY, Wang GQ, Wang W, Wu Q, Xu H, Xu MD, Yang AM, Yao F, Yu HG, Zhou PH, Zhang B, Zhang XF, Zhai YQ. Consensus on the digestive endoscopic tunnel technique. World J Gastroenterol. 2019;25:744-776. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 41] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 5. | Khashab MA, El Zein M, Kumbhari V, Besharati S, Ngamruengphong S, Messallam A, Abdelgalil A, Saxena P, Tieu AH, Raja S, Stein E, Dhalla S, Garcia P, Singh VK, Pasricha PJ, Kalloo AN, Clarke JO. Comprehensive analysis of efficacy and safety of peroral endoscopic myotomy performed by a gastroenterologist in the endoscopy unit: a single-center experience. Gastrointest Endosc. 2016;83:117-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 61] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 6. | Rodríguez de Santiago E, Shimamura Y, Pioche M, Eleftheriadis N, Albéniz E, Bechara R, Yan Chiu PW, Guarner-Argente C, Herreros de Tejada A, Uchima H, Fujiyoshi Y, Ponchon T, González-Gete G, Hew S, Murzi-Pulgar M, Matallana V, Parejo-Carbonell S, Estremera-Arévalo F, Moll F, Onimaru M, Inoue H. Safety and effectiveness of peroral endoscopic myotomy in patients on antiplatelet or anticoagulant therapy: an international multicenter case-control study. Gastrointest Endosc. 2021;93:839-849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Von Renteln D, Fuchs KH, Fockens P, Bauerfeind P, Vassiliou MC, Werner YB, Fried G, Breithaupt W, Heinrich H, Bredenoord AJ, Kersten JF, Verlaan T, Trevisonno M, Rösch T. Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study. Gastroenterology. 2013;145:309-11.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 265] [Cited by in RCA: 249] [Article Influence: 20.8] [Reference Citation Analysis (1)] |
| 8. | Li QL, Yao LQ, Xu XY, Zhu JY, Xu MD, Zhang YQ, Chen WF, Zhou PH. Repeat peroral endoscopic myotomy: a salvage option for persistent/recurrent symptoms. Endoscopy. 2016;48:134-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Ichkhanian Y, Assis D, Familiari P, Ujiki M, Su B, Khan SR, Pioche M, Draganov PV, Cho JY, Eleftheriadis N, Barret M, Haji A, Velanovich V, Tantau M, Marks JM, Bapaye A, Sedarat A, Albeniz E, Bechara R, Kumta NA, Costamagna G, Perbtani YB, Patel M, Sippey M, Korrapati SK, Jain R, Estremera F, El Zein MH, Brewer Gutierrez OI, Khashab MA. Management of patients after failed peroral endoscopic myotomy: a multicenter study. Endoscopy. 2021;53:1003-1010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Li Y, LingHu E, Ding H, Zhang X, Li M, Xiong Y, Wang X. Peroral endoscopic myotomy with simultaneous submucosal and muscle dissection for achalasia with severe interlayer adhesions. Gastrointest Endosc. 2016;83:651-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Eckardt VF, Aignherr C, Bernhard G. Predictors of outcome in patients with achalasia treated by pneumatic dilation. Gastroenterology. 1992;103:1732-1738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 483] [Cited by in RCA: 523] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 12. | Zhang WG, Linghu EQ, Chai NL, Li HK. Ling classification describes endoscopic progressive process of achalasia and successful peroral endoscopy myotomy prevents endoscopic progression of achalasia. World J Gastroenterol. 2017;23:3309-3314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Feng J, Chai N, Zhang W, Li L, Tang X, Zou J, Ye L, Linghu E. Long-term outcomes of peroral endoscopic myotomy with simultaneous submucosal and muscle dissection (POEM-SSMD) for achalasia with severe interlayer adhesions. Chin Med J (Engl). 2022;135:724-726. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 14. | Li HK, Linghu EQ. New endoscopic classification of achalasia for selection of candidates for peroral endoscopic myotomy. World J Gastroenterol. 2013;19:556-560. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Werner YB, Hakanson B, Martinek J, Repici A, von Rahden BHA, Bredenoord AJ, Bisschops R, Messmann H, Vollberg MC, Noder T, Kersten JF, Mann O, Izbicki J, Pazdro A, Fumagalli U, Rosati R, Germer CT, Schijven MP, Emmermann A, von Renteln D, Fockens P, Boeckxstaens G, Rösch T. Endoscopic or Surgical Myotomy in Patients with Idiopathic Achalasia. N Engl J Med. 2019;381:2219-2229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 398] [Cited by in RCA: 338] [Article Influence: 56.3] [Reference Citation Analysis (1)] |
| 16. | NOSCAR POEM White Paper Committee; Stavropoulos SN, Desilets DJ, Fuchs KH, Gostout CJ, Haber G, Inoue H, Kochman ML, Modayil R, Savides T, Scott DJ, Swanstrom LL, Vassiliou MC. Per-oral endoscopic myotomy white paper summary. Gastrointest Endosc. 2014;80:1-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 121] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 17. | Tyberg A, Sharaiha RZ, Familiari P, Costamagna G, Casas F, Kumta NA, Barret M, Desai AP, Schnoll-Sussman F, Saxena P, Martínez G, Zamarripa F, Gaidhane M, Bertani H, Draganov PV, Balassone V, Sharata A, Reavis K, Swanstrom L, Invernizzi M, Seewald S, Minami H, Inoue H, Kahaleh M. Peroral endoscopic myotomy as salvation technique post-Heller: International experience. Dig Endosc. 2018;30:52-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 18. | Onimaru M, Inoue H, Ikeda H, Yoshida A, Santi EG, Sato H, Ito H, Maselli R, Kudo SE. Peroral endoscopic myotomy is a viable option for failed surgical esophagocardiomyotomy instead of redo surgical Heller myotomy: a single center prospective study. J Am Coll Surg. 2013;217:598-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 124] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 19. | Tyberg A, Seewald S, Sharaiha RZ, Martinez G, Desai AP, Kumta NA, Lambroza A, Sethi A, Reavis KM, DeRoche K, Gaidhane M, Talbot M, Saxena P, Zamarripa F, Barret M, Eleftheriadis N, Balassone V, Inoue H, Kahaleh M. A multicenter international registry of redo per-oral endoscopic myotomy (POEM) after failed POEM. Gastrointest Endosc. 2017;85:1208-1211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 58] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 20. | Feng X, Linghu E, Chai N, Ding H. New endoscopic classification of esophageal mucosa in achalasia: A predictor for submucosal fibrosis. Saudi J Gastroenterol. 2018;24:122-128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Mittal C, Wagh MS. Technical Advances in Per-Oral Endoscopic Myotomy (POEM). Am J Gastroenterol. 2017;112:1627-1631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Liu X, Yao L, Cheng J, Xu M, Chen S, Zhong Y, He M, Chen W, Zhang Y, Qin W, Hu J, Cai M, Zhou P, Li Q. Landscape of Adverse Events Related to Peroral Endoscopic Myotomy in 3135 Patients and a Risk-Scoring System to Predict Major Adverse Events. Clin Gastroenterol Hepatol. 2021;19:1959-1966.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 23. | Gupta S, Sidhu M, Banh X, Bradbear J, Byth K, Hourigan LF, Raftopoulos S, Bourke MJ. A prospective multicentre study of per-oral endoscopic myotomy (POEM) for achalasia in Australia. Med J Aust. 2021;214:173-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |