Published online Apr 7, 2023. doi: 10.3748/wjg.v29.i13.1955
Peer-review started: December 1, 2022
First decision: January 14, 2023
Revised: January 22, 2023
Accepted: March 20, 2023
Article in press: March 20, 2023
Published online: April 7, 2023
Processing time: 126 Days and 21.8 Hours
Common bile duct stones are among the most common conditions encountered by endoscopists. Therefore, it is well researched; however, some items, such as indications for endoscopic papillary balloon dilatation (EPBD), safety of EPBD and endoscopic sphincterotomy in patients receiving dual antiplatelet therapy or direct oral anticoagulant, selection strategy for retrieval balloons and baskets, lack adequate evidence. Therefore, the guidelines have been updated with new research, while others remain unchanged due to weak evidence. In this review, we comprehensively summarize the standard methods in guidelines and new findings from recent studies on papillary dilation, stone retrieval devices, difficult-to-treat cases, troubleshooting during the procedure, and complicated cases of cholangitis, cholecystolithiasis, or distal biliary stricture.
Core Tip: In this review, we comprehensively summarized the standard methods for patients with small common bile duct stones in guidelines and new findings from recent studies on papillary dilation, stone retrieval devices, difficult-to-treat cases, troubleshooting during the procedure, and complicated cases of cholangitis, cholecystolithiasis, or distal biliary stricture.
- Citation: Masuda S, Koizumi K, Shionoya K, Jinushi R, Makazu M, Nishino T, Kimura K, Sumida C, Kubota J, Ichita C, Sasaki A, Kobayashi M, Kako M, Haruki U. Comprehensive review on small common bile duct stones. World J Gastroenterol 2023; 29(13): 1955-1968
- URL: https://www.wjgnet.com/1007-9327/full/v29/i13/1955.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i13.1955
Cholangitis is the second or third most common cause of community-acquired bacteremia, with common bile duct (CBD) stones being the most common[1,2]. Recurrence of CBD stones is common, with 111 (11.3%) of 983 patients who underwent endoscopic sphincterotomy (EST) recurred during a median follow-up of 7.5 years, and the cumulative recurrence rates at 5, 10, 15, and 20 years were 8.5%, 12.5%, 19.1%, and 24.2%, respectively[3]. It is frequently encountered by endoscopists, and it is important to improve short-term outcomes and prevent the long-term recurrence of cholelithiasis. This review focuses on small CBD stones. Although the international definition of small CBD stones has not been established, we have followed the standard of approximately 10 mm in some studies[4,5]. We described papillary dilation, stone extraction, difficult cases, troubleshooting during stone extraction in small CBD stones, and complicated cases of cholangitis, cholecystolithiasis, or distal biliary stricture and summarized the European, American, and Japanese guidelines. Moreover, this review addressed the novel literatures on endoscopic papillary balloon dilatation (EPBD) dilation times to prevent post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis (PEP)[6], the duration of direct oral anticoagulants (DOAC) and dual antiplatelet therapy (DAPT) withdrawal to safely perform EST[7,8], EST with balloon dilation (ESBD), and the comparison of the effects of retrieval balloon and basket catheters for small CBD stone extraction[9,10].
Papillary dilation is divided into EST and EPBD, and a nationwide administrative database of 61000 hospitalized patients with CBD stones throughout Japan reported that EST was performed in 89% of patients and EPBD in 11%[11]. Knowledge of the success rate of CBD stone removal and the incidence of short- and long-term complications is important when deciding between EST and EPBD.
A meta-analysis reported that EPBD has a lower incidence of total clearance of CBD stones and more frequent lithotripsy basket use than EST[12]. However, 11 of 14 references in this study included cases of CBD stones larger than 10 mm. Conversely, there were no significant differences in total clearance of CBD stones in another meta-analysis by Liu et al[13].
Yu et al[6] reported that both EST and EPBD have obvious effects in the treatment of bile duct stones with minor diameters (< 10 mm) and small numbers (< 3). The EPBD balloons used in that study were mostly 8 and 10 mm in diameter, especially those with 8 mm in diameter. Because a typical papillary dilation balloon is 8 mm in diameter, the indication for EPBD may be CBD stones up to 10 mm in diameter, considering the flexibility of the papillae. However, even for CBD stones > 10 mm, EPBD combined with endoscopic mechanical lithotripsy may have a success rate of stone retrieval comparable to that of EST[13]. Therefore, EPBD may be useful in cases of coagulopathy in which CBD stones are larger than 10 mm.
There is lack of evidence for the possibility of very small stone extraction without EST or EPBD. It has been reported that if ESWL results in stone fragment size of 3 mm or less, there is a likelihood that the stone will be spontaneously discharged without EST. Therefore, it is possible that stone extraction can be performed without EST or EPBD if the size is less than approximately 3 mm[14], however, there are no studies that have directly examined this issue. Therefore, in principle, EST and EPBD are recommended for stone extraction of CBD stones, as recommended by the European Society of Gastrointestinal Endoscopy (ESGE) and Japan Gastroenterological Endoscopy Society (JGES) guidelines; however, it is at the endoscopist's discretion whether to perform stone extraction without these procedures for very small stones[15,16].
In cases of EPBD compared to EST, post-ERCP pancreatitis increased, bleeding decreased, and there was no significant difference in perforation or post-ERCP cholangitis. PEP and hemorrhage are likely to occur especially in approximately 10% and less than 0.1% of patients in the EPBD group, respectively; and in approximately 3% and 3% of patients in the EST group, respectively[12]. The total data in the meta-analysis has variation in the patient’s background; however, it is consistent with that of a previous report[17].
PEP: PEP may be a short-term complication when selecting EST/EPBD. ESGE describes the following risk factors for PEP:
Patient-related definite risk factors include suspected sphincter of Oddi dysfunction, female sex, previous pancreatitis, and previous PEP. Procedure-related definite risk factors, such as difficult cannulation, pancreatic guidewire passage > 1, and pancreatic injection. Patient-related risk factors include younger age, non-dilated extrahepatic bile duct, normal serum bilirubin, absence of chronic pancreatitis, and end-stage renal disease. Procedure-related risk factors include precut sphincterotomy, pancreatic sphincterotomy, failure to clear bile duct stones, intraductal ultrasound, and biliary balloon sphincter dilation[18]. ESGE especially recommends prophylactic pancreatic stenting in selected patients at high risk for PEP (inadvertent guidewire insertion/opacification of the pancreatic duct and double-guidewire cannulation).
In a multicenter randomized control study, 117 patients with bile duct stones were treated with EPBD; after treatment, the incidence of pancreatitis among those patients reached 15.4%, and two patients died from post-treatment complications[19]. Incomplete dilation of the papilla, intramucosal bleeding, and local edema were considered the main causes of PEP due to EPBD. Conversely, several reports of randomized control trials or network meta-analyses suggested that there is no direct consequence between PEP risk and EPBD[20,21], and PEP usually occurs in the mild or moderate stage[12]. Recently, a network meta-analysis reported that 2 to 5 min of EPBD could decrease the incidence of PEP compared to short-term (< 2 min) EPBD. In addition, it was also reported to reduce PEP without increasing the occurrence of other early complications by extending the duration of balloon dilatation[6]. However, the underlying mechanism for this result remains unclear. A possible reason could be that the dilatation with a small diameter balloon or short duration could result in inadequate papilla expansion; thus, the common discharge channel for bile and pancreatic juice tended to be narrow after the operation[6]. That study did not examine EPBD longer than 5 min; however, another study found that 5-min EPBD increases PEP compared to EPBD of 0.5-3 min[22]. Although this is a study of EPBD combined with small-incision EST, it may be advisable to avoid EPBD for more than 5 min[22]. Therefore, we use a 2-3 min EPBD.
In recent years, diclofenac or diclofenac and sublingual nitrates have been reported to be useful for the prevention of PEP[23,24]. ESGE also recommends routine rectal administration of 100 mg of diclofenac or indomethacin immediately before ERCP in all patients without contraindications to nonsteroidal anti-inflammatory drug administration[18]. These methods were not available in 2004 when EPBD was abandoned by many endoscopists, especially in America, and combining such methods may reduce the incidence of PEP due to EPBD. Furthermore, EPBD may be even safer in Asians, as some race-based studies have shown no increase in PEP in Asian populations[12].
Bleeding: ESGE guidelines suggest that patients should be considered at increased risk of post-EST bleeding if at least one of the following factors is present: anticoagulant intake, platelet count < 50000/mm3, cirrhosis, dialysis of end-stage renal disease, intraprocedural bleeding, and low endoscopist experience[18].
ESGE, JGES, and the American Society of Gastrointestinal Endoscopy (ASGE) guidelines treat antiplatelet medications almost similarly for EST/EPBD. DAPT is permitted in EPBD without drug withdrawal, whereas EST requires DAPT withdrawal. Withdrawal regimens are similar across guidelines, with thienopyridine requiring 5-7 day withdrawal and continuation of aspirin or cilostazol monotherapy[18,25,26]. However, each guideline treats anticoagulants in a slightly complex and different manner. Although it is necessary to evaluate the risk of embolism and procedural bleeding when antithrombotic agents are stopped in EPBD, warfarin can be continued if the PT-INR is within the therapeutic range. In EST, treatment with warfarin can be continued, whereas the PT-INR is within the therapeutic range in Japan and America. However, in Europe and America, it is recommended to discontinue warfarin 5 d before EST and replace it with heparin 2 d before EST, especially in patients at high risk of embolism in aortic or mitral valve replacement, atrial fibrillation, or any thromboembolic risk. Once hemostasis is confirmed, antithrombotic agents must be restarted postoperatively in America, the next day in Japan, and within 2 d in Europe. Warfarin should be resumed after the procedure, and heparin should be used in combination until the PT-INR returns to the therapeutic range[18,25,26]. However, it is difficult to summarize each country's guidelines accurately and concisely; therefore, please refer to each country's guidelines for details. In addition, in DAPT and DOAC, there is a paucity of evidence regarding the ability of guideline-guided withdrawal periods to prevent bleeding[7,8,25,27].
With regards to hemorrhage, Mirjalili and Stringer[28] identified 98 arteries near the major papilla and reported blood vessel distribution on endoscopy. According to their report, blood vessel distribution in the 10 to 11 o'clock region was low at 10%-11%; thus, cutting in this region has a low risk of hemorrhage. The ESGE and Japanese EST guidelines have cited this article[16,18]. No trials have compared hemorrhage and perforation according to cutting direction; however, adding to the reports that bile ducts tend to run in the 11 to 12 o'clock direction in the papillary region, cutting in the 11 to 12 o'clock direction is considered safe, and thus recommended by Japanese EST guidelines[16].
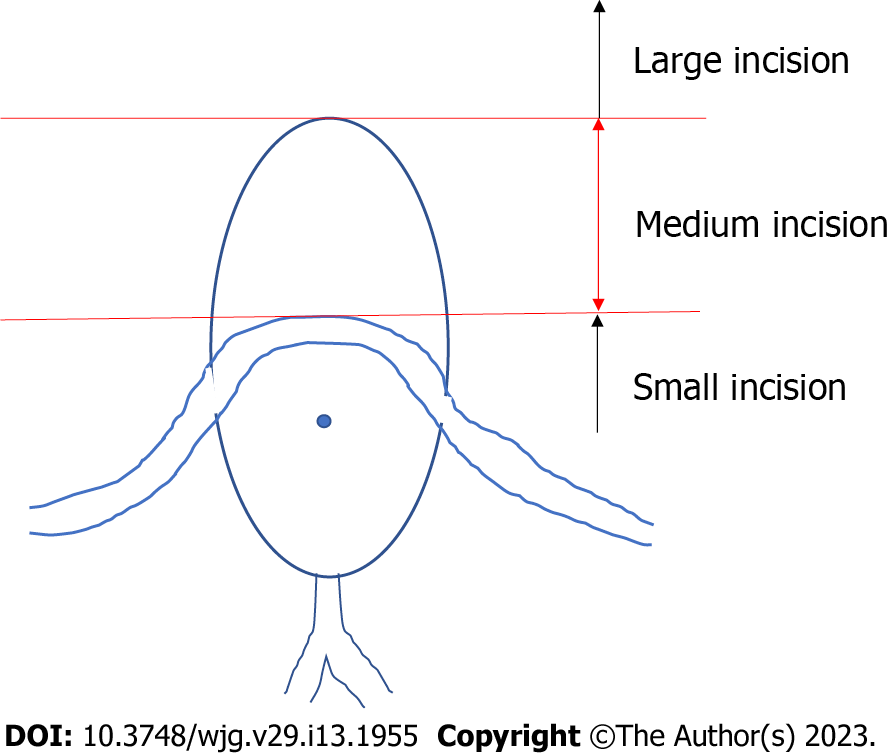
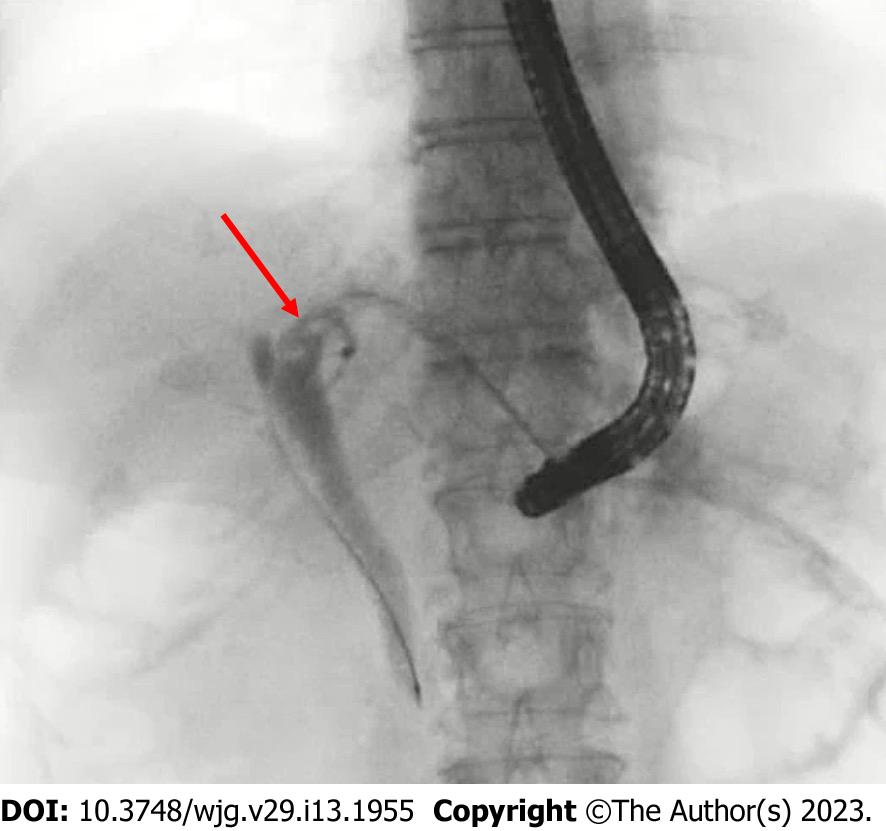
Others: The superior sphincter extends to the bile duct on the lateral wall of the duodenum, and cutting beyond this area increases the risk of perforation. In relation to the papilla, it is believed that the superior margin of the papillary bulge coincides with the middle sphincter, which is considered the upper cutting limit (Figure 1). However, anatomical examinations may not necessarily be consistent with actual living bodies, and depending on the cutting direction, perforation can occur even if the superior margin of the papillary bulge is not reached; thus, due care should be exercised[16]. Moreover, there is no evidence comparing incision size to the incidence of procedural adverse events or therapeutic outcomes following EST[16].
The incidence of short-term cholecystitis after ERCP could be caused by resistance to initial antibiotics on admission[29], and the incidence of long-term cholecystitis and the recurrence of stones in CBD could be decreased by EPBD compared to EST[6,12]. EST causes significant damages to the Oddi sphincter, and post-EST sphincter dysfunction easily occurs[30]. Then, the reflux of intestinal contents such as digestive juices, food residue, and bacteria may increase the risk of biliary tract infection and stone recurrence[31,32].
To summarize the characteristics of EST and EPBD (Table 1), EST is superior in terms of PEP reduction and bile duct large stone retrieval, while EPBD is superior in terms of bleeding reduction, long-term cholecystitis, and bile duct stone recurrence. Based on these findings, we consider EPBD in cases of small bile duct stones, bleeding tendency, young age, and even in surgically altered anatomy in which EST is difficult.
| Short-term complications | Long-term complications | ||||
| Bleeding | PEP | Perforation | Cholecystitis | Recurrence of stones in CBD | |
| Incidence | |||||
| EST | 3% | 3% | Rare | EST > EPBD | EST > EPBD |
| EPBD | Less than 0.1% | 10% | Very rare | ||
| Prophylactic methods | Cessation of anticoagulant and antiplatelet agents referred to each country's guidelines; EST with cutting at approximately 11 o'clock direction | Diclofenac; Pancreatic stenting in selected patients at high risk for PEP; 2-3 min EPBD in patients with EPBD | There is no evidence comparing incision size, the incidence of procedural adverse events, and therapeutic outcomes following EST | We consider EPBD in cases of small bile duct stones, bleeding tendency, young age, and even in surgically altered anatomy in which EST is difficult | We consider EPBD in cases of small bile duct stones, bleeding tendency, young age, and even in surgically altered anatomy in which EST is difficult |
ESBD: Ding et al[4] defined a tunnel from the distal bile duct to the papillary orifice as an extraction tunnel (SET). Based on the anatomical structure, the tunnel was divided into two segments, with the distal bile duct and the intradural portion of the sphincter of Oddi comprising the proximal segment, including the proximal ring, and the intraduodenal portion of the distal segment of the papillae, including the distal ring around the orifice. Conventional EST cuts the distal segment almost completely from the orifice to near the duodenal wall, EPBD extends the entire SET, and EST + EPBD (ESBD) shortens the SET by cutting the distal ring and extends the proximal ring. Therefore, this combination technique is suitable for accessing the wide opening of the SET from an anatomical perspective[4]. In this study, ESBD was reported to reduce the number of treatments for complete stone removal, procedure time, use of mechanical lithotripters, and bleeding rate, and the incidence of PEP was reported to be comparable to that of EST. It has been reported that a small incision did not increase the risk of bleeding compared with non-EST, which might be attributed to a lower chance of injury to the major vessel in the papillary roof[20]. ESBD limits EST to small incisions, which may be the reason for reduced bleeding after ERCP. In a network meta-analysis, ESBD tended to be superior to EST in terms of successful stone removal in the first endoscopic session, the need for mechanical lithotripsy, and the risk of bleeding or perforation. However, none of these variables showed statistical significance[20]. Thus, ESBD may be superior to EST in overall efficacy and short- and long-term complications, and ESBD may be recommended over EST in the future; however, there is insufficient evidence to recommend ESBD over EST. Therefore, to justify updating the current guidelines, researchers will require more evidence that ESBD is superior to EST in terms of overall efficacy[20] and that ESBD may reduce the long-term recurrence rate of bile duct stones[33]. At this time, it is up to each endoscopist to decide whether to perform ESBD or EST.
A recent meta-analysis found that balloon catheters for cholelithiasis were superior to basket catheters for complete stone removal[9]. However, there are some limitations in the studies included in this meta-analysis. Three of the four studies included in the review were on small stones (≤ 10-11 mm), and three of these articles used a four-wire retrieval basket catheter. Four-wire retrieval basket catheters are less suited to retrieve small stones than an eight-wire retrieval basket catheters and retrieval balloon catheters. Therefore, we cannot conclude that the basket catheter is inferior to a balloon catheter in the case of small CBD stones[5,34-36]. One meta-analysis study only included these three studies, but its conclusions were similar to those of a previous meta-analysis[10]. Ozawa et al[5] reported that small stones (maximum diameter, 6 mm) are an independent risk factor for failed stone removal; in their study, the basket failed to grasp a small stone in eight cases, and in four of which, the stones were successfully removed after an exchange with a balloon catheter. Therefore, they suggested that a retrieval balloon catheter may be more appropriate than a basket catheter for removing small stones[5]. However, Ozawa et al[5] also used a four-wire basket.
Once a stone is captured in a basket, reliable extraction is usually ensured. More reliable traction associated with the basket catheter is cited as the main reason for its preferential use in Japan and Europe[5,9]. In the study by Ozawa et al[5], the balloon slipped past the stones and could not provide a sufficient traction force for stone extraction within 10 min in four patients in the balloon group, and the stones were successfully captured and withdrawn after exchange to the basket in all cases. However, a basket with a captured stone may occasionally become impacted at the papilla during extraction if the sphincterotomy is insufficient or if the stone is larger than estimated. According to the ESGE guidelines, the difference between balloon and basket catheters is slightly minimal, so endoscopists can use any of the two; meanwhile, according to the ASGE guidelines, the balloon catheter is highly recommended for safety issues related to basket impaction[18,37].
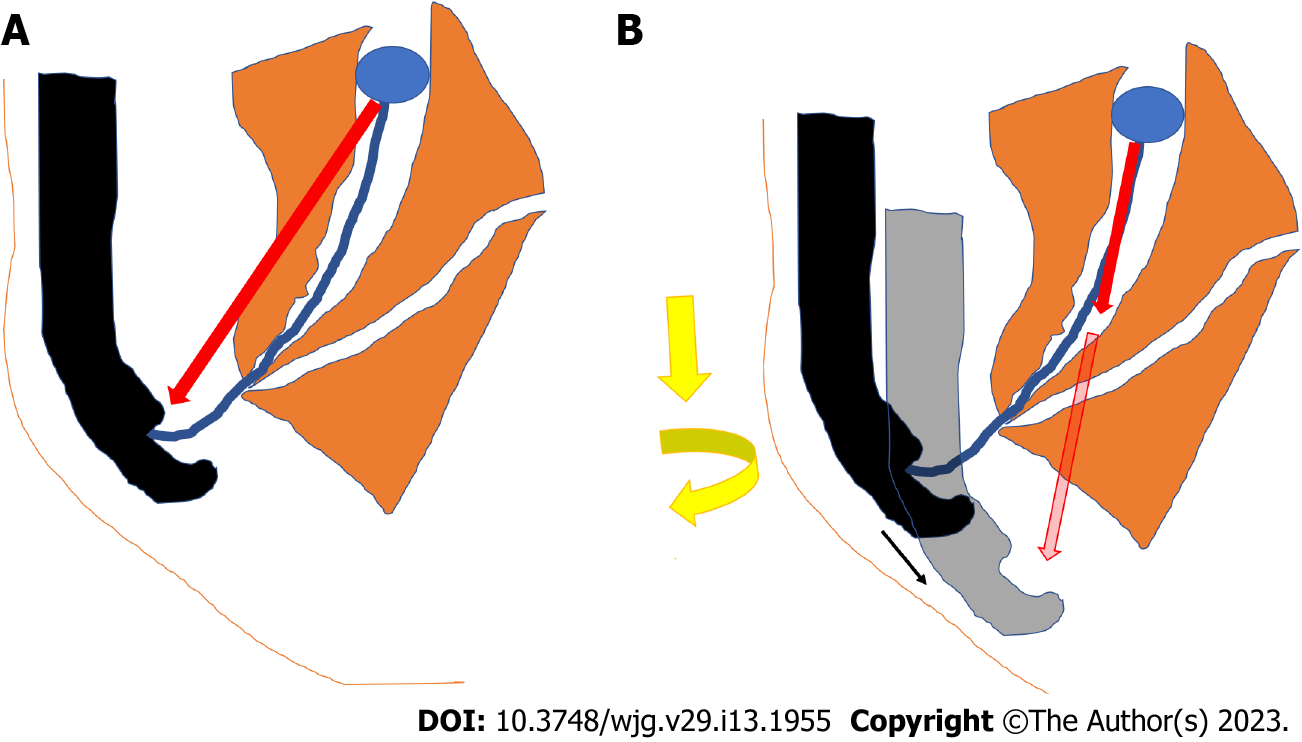
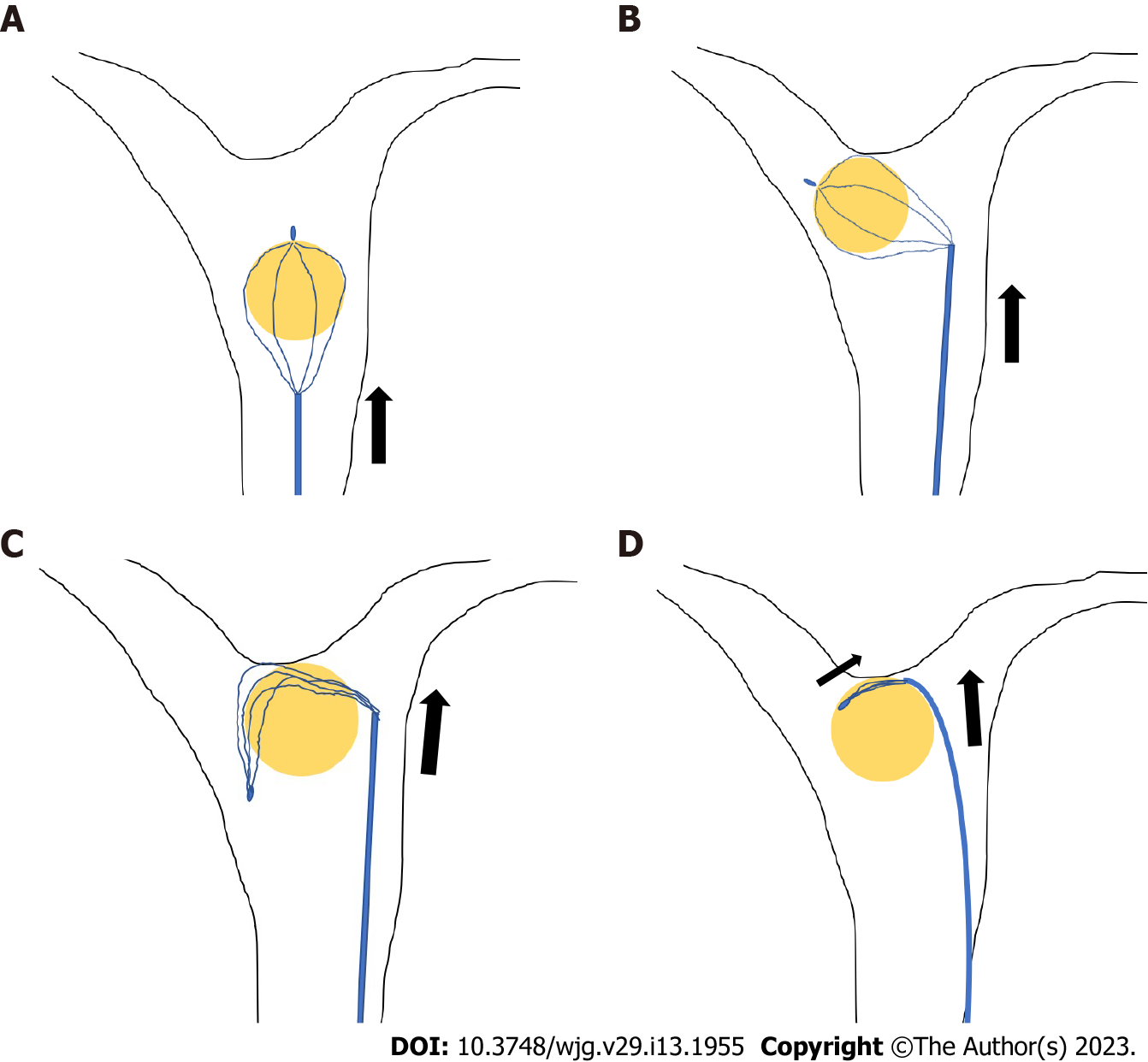
There are two main operations when retrieving CBD stones with a retrieval balloon or basket. First, the catheter was pulled with the right hand. The other is to apply right rotation and push on the endoscope and use the down angle with dial control, if necessary. The difference between the two is the direction of the force on the retrieval balloon or the basket. In the former, the retrieval balloon or basket faces the forceps hole at the endoscope tip, whereas, in the latter, they face the tip of the endoscope that is pushed in (Figure 2). The important basic rule is that the direction of the force applied to the catheter should coincide with the long axis of the bile duct, and one can choose the easier of the two methods to accomplish this.
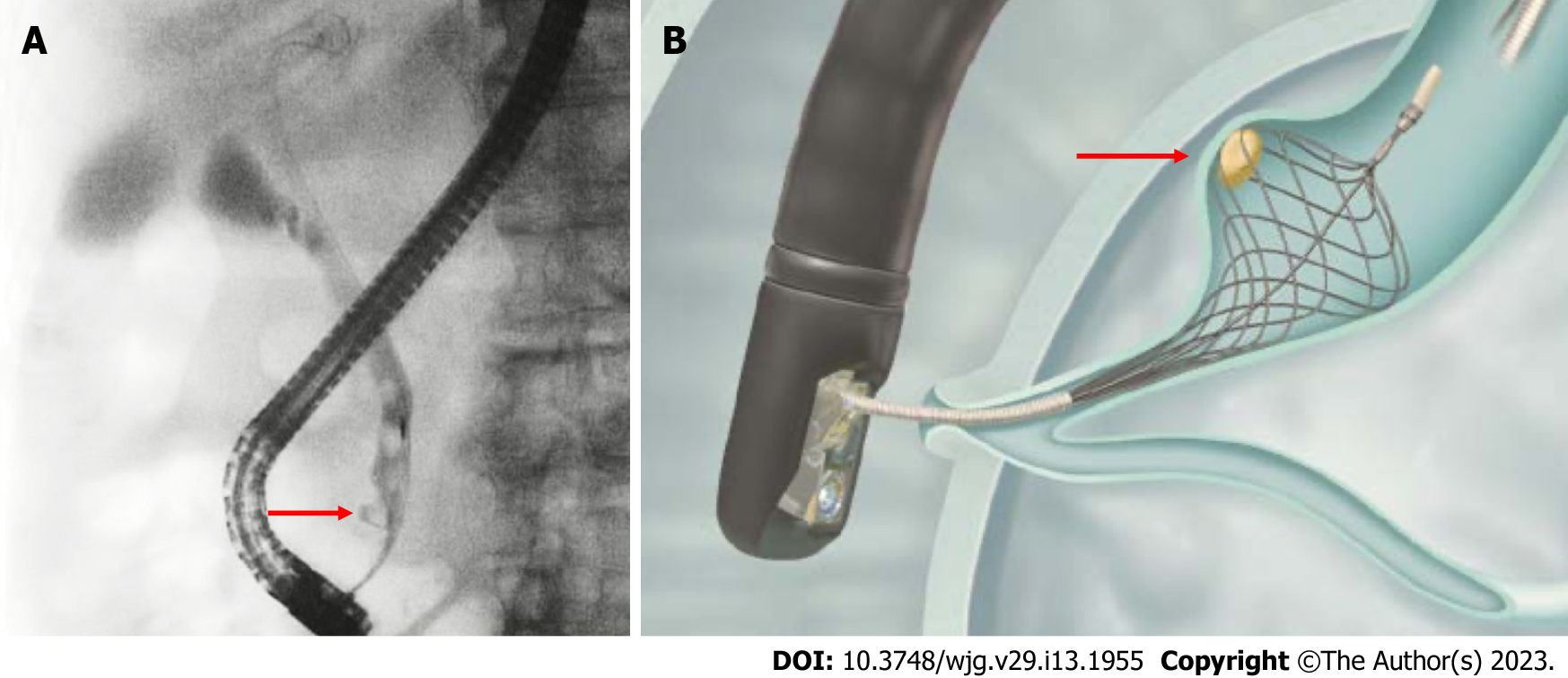
However, in cases with pockets in the lower part of the bile duct, stone extraction is difficult. Once a stone is impacted at the corner pocket, the balloon passes alongside the stone without removing it, and stone removal is often difficult, even after repeated attempts. Such cases can be handled by pushing the stone up to the middle of the bile duct and then grabbing it with a basket or by using a basket shaped to extract the stone out of the pocket, such as a disposable NT retrieval basket (VorticCatch V: Olympus Medical Systems, Japan) (Figure 3).
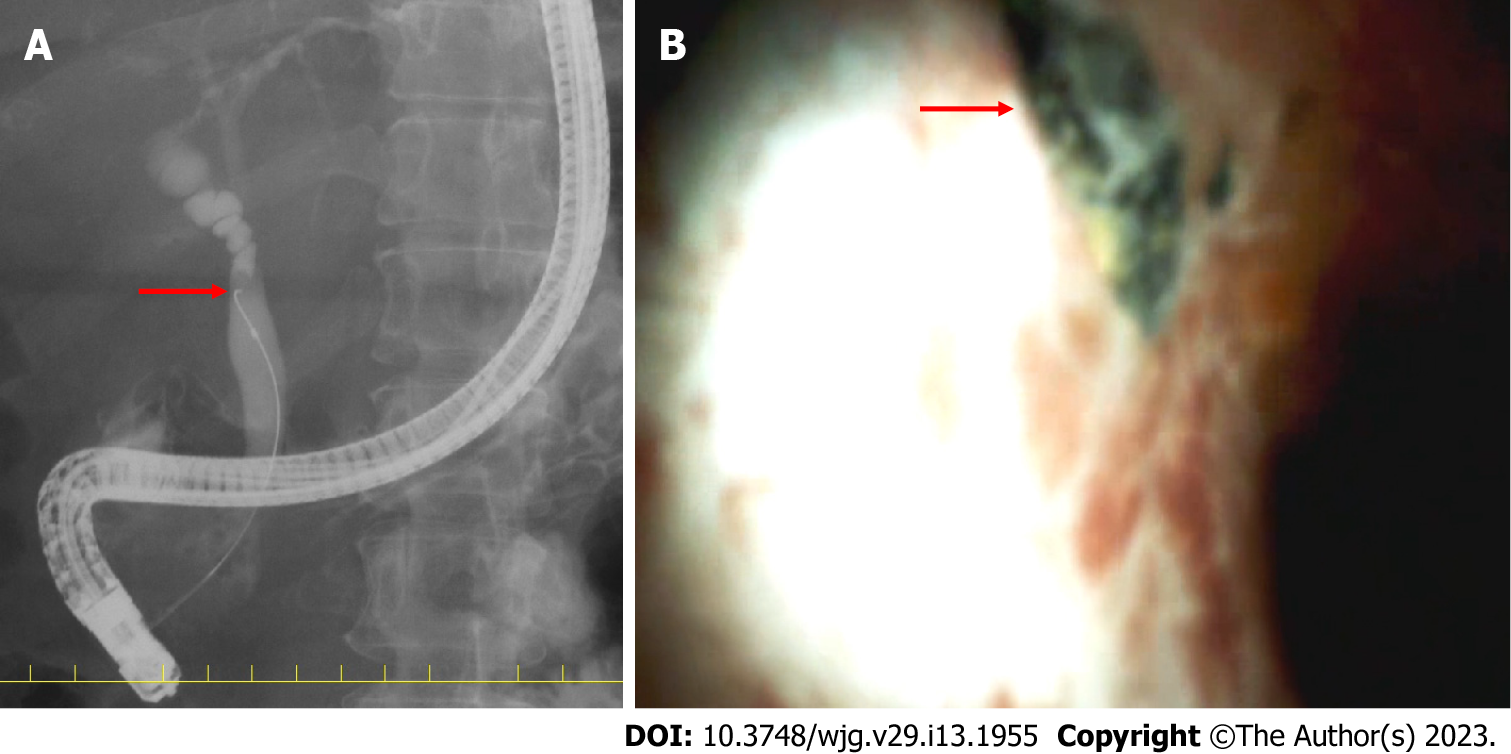
Furthermore, stones near the bifurcation of the gallbladder duct are difficult to grasp using a retrieval balloon or basket (Figure 4). Surgery is considered in these cases; however, they can be addressed with cholangioscopy, such as when in conjunction with electronic hydraulic lithotripsy (EHL)[15]. When it is difficult to grasp a CBD stone, a basket that directly grasps the stone under cholangioscopy is available[38].
Enteroscopy-assisted ERCP (eERCP) is often difficult in cases of surgically altered anatomy (SAA). In cases of SAA, endoscopic ultrasound-guided transmural drainage (EUS-TD) or percutaneous transhepatic biliary drainage (PTBD) may be effective alternatives (Figure 5)[39].
In a multicenter retrospective cohort study involving 98 patients (49 EUS-TD and 49 eERCP groups), technical success was achieved in 98% of patients in the EUS-TD group compared to 65.3% of patients in the eERCP group (OR 12.48, P = 0.001). EUS-TD had a significantly shorter procedural time (55 vs 95 min, P < 0.001). However, more complications of mild/moderate severity occurred in the EUS-TD group (20% vs 4%, P = 0.01). The length of stay was significantly longer in the EUS-TD group (6.6 vs 2.4 d, P < 0.001)[40]. PTBD is also a useful alternative, with a reported success rate of approximately 97%, but this method of stone removal may cause problems, such as drainage tube trouble or an increased number of sessions[41].
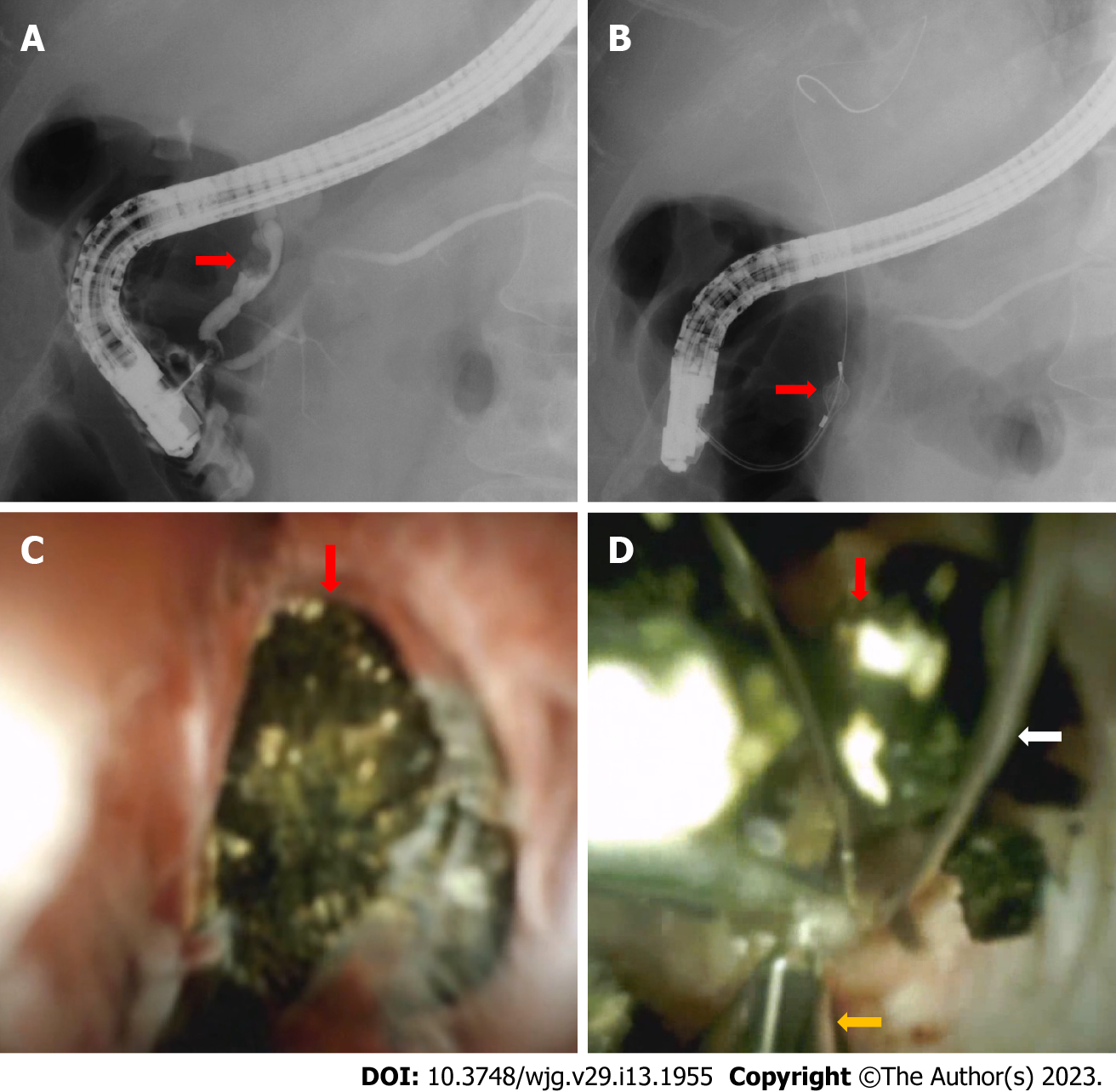
A serious drawback of basket catheters is that during stone extraction, the basket with the captured stone is impacted in the lower bile duct or papilla. When basket impaction occurs, the basket must first be opened and pushed upwards into the hepatic hilum. An attempt was made to curl the basket wires back and disengage the stone (Figure 6). If this technique fails, more complicated techniques, such as mechanical lithotripsy and intra-extracorporeal lithotripsy, are required[5]. To use a lithotripter, such as BML-110A-1 (Olympus Medical Systems, Tokyo) (Figure 7), which can be retrofitted to a basket catheter, the basket catheter is cut outside the body, the endoscope is removed from the body, and the wires of the basket catheter from the mouth are wrapped around the lithotripter. However, if the basket cannot be unmated even with a lithotripter, a cholangioscope can be helpful. The basket and grasped stone were visualized under the cholangioscope and crushed by an EHL or YAG laser (Figure 8).
The Tokyo Guidelines 2018 (TG18) and ASGE suggest that bile duct stone removal following EST in a single session may be considered in patients with mild or moderate acute cholangitis[42,43]. However, given that hemodynamically unstable or coagulopathy patients might not tolerate procedural bleeding or adverse events, decompression alone should be considered in this group[42,43]. PEP does not increase even in cases of complicated cholangitis[43]. TG18 suggested that endoscopic nasobiliary drainage (ENBD) or endoscopic biliary stenting (EBS) may be considered for biliary drainage according to the patient's background and preference. It should be borne in mind that if patients experience discomfort from transnasal tube placement, they are likely to remove the tube themselves, particularly in elderly patients. EBS is an internal drainage technique that does not cause discomfort or loss of electrolytes or fluids. In contrast, ENBD is an external drainage technique that allows monitoring or washing of bile via the transnasal tube, particularly if the bile is purulent[42]. The ESGE did not provide any recommendations for these[15]. We present a table summarizing each guideline, focusing on key points (Table 2).
| JGES/TG18 | ESGE | ASGE | |
| Papillary dilatation | EST is standard | EST is standard | EST is standard |
| EPBD is determined by age, scheduled RFA, antithrombotic medications, parapapillary diverticulum, reconstructed bowel, and stone diameter and number | In anticoagulant users and in cases of SAA, EPBD is an option for stones smaller than 8 mm | In anticoagulant users, in cases of SAA, and in cases of intradiverticular papilla, EPBD is an option | |
| Cases of antithrombotic agents use (EST, high bleeding risk procedures) | ASA or CLZ alone may be continued | ASA or CLZ alone may be continued | ASA or CLZ alone may be continued |
| Thienopyridines discontinued for 5-7 d or replaced with ASA or CLZ | Thienopyridines discontinued for 5-7 d or replaced with ASA or CLZ | Thienopyridines discontinued for 5-7 d or replaced with ASA or CLZ | |
| Warfarin may be continued if in therapeutic range; DOAC is withdrawn on the EST day only | Warfarin stopped 5 d ago and LMWH was started 2 d ago (LMWH also stopped 24 h ago). DOAC stopped 48 h ago | Warfarin users can be treated urgently if INR < 2.5. DOACs should be discontinued prior to treatment, with a discontinuation period of twice the half-life. Heparin replacement is recommended in patients at high risk of thrombosis | |
| Resumed the next day | Warfarin or DOAC resume within 48 h. Warfarin is used with LMWH until the optimal concentration is reached | Resume at the end of the procedure if hemostasis is confirmed. However, evidence for DOACs and APAs are scant | |
| Stone retrieval | No superiority of balloons and baskets is noted | Efficacy of balloons and baskets is almost equal | Recommend using balloons rather than baskets |
| Complicated cases of cholangitis | Patients who are hemodynamically unstable, coagulopathic, or receiving antithrombotic agents; it was believed that decompression alone should be considered.EBS and ENBD are almost equal | Not stated | Given that hemodynamically unstable patients might not tolerate procedural bleeding or adverse events, it was believed that decompression alone should be considered in this group as well as for patients who are coagulopathic and/or are receiving antithrombotic agents and those who would need to have anticoagulation resumed immediately after sphincterotomy (e.g., patients with mechanical heart valves) |
In the general population, CBD stones complicated with cholecystolithiasis commonly occurs. The established gold standard for the treatment of symptomatic cholecystolithiasis is laparoscopic cholecystectomy (LC), but the treatment option for CBD stones is yet to be clarified. CBD stones complicated with cholecystolithiasis can be treated with two-session minimally invasive and one-session feasible strategies. The former requires pre- or post-LC ERCP, whereas the latter requires LC plus intraoperative laparoscopic CBD exploration (LCBDE) or LC with intraoperative ERCP[44]. As per efficacy, morbidity, or mortality endoscopic and surgical techniques for extracting these stones are equally suitable[45]. However, one-session procedures usually result in a shorter hospital stay[15]. Moreover, a recent meta-analysis has demonstrated that the one-session procedure has a higher success rate than the two-session procedure[46].
For one-session procedures, many surgeons prefer the less invasive and less complicated trans
There are no recent reports on laparoscopic surgery for small CBD stones, however, Huang et al[53], in their report on laparoscopic surgery for small CBD with CBD stones, indicated that it is safe and feasible for small CBD patients to perform LCBDE.
Few reports have been published on CBD stones extraction with distal biliary stricture[54,55], however, plastic stent(s)[56,57], covered self-expandable metallic stent(s) (cSEMS)[56-58], balloon dilation[59], and surgery[60] have been used for dilating bile duct stenosis. However, balloon dilation carries the risk of bile duct injury. Therefore, when endoscopic stone extraction is performed for CBD stones with benign biliary stricture, it may be advisable to use multiple plastic stents or cSEMS for several months and perform endoscopic stone extraction after bile duct dilation is achieved[61]. Combining them with mechanical lithotripsy may also be useful[54]. Ogura et al[55] reported that transluminal stone extraction passing through the EUS-TD route, without passing through the distal bile duct might be useful. Reports of CBD stones with malignant biliary stricture are even more scarce, however, the safety of 6-8 mm balloon dilation for malignant biliary stricture has been reported[62]. In malignant biliary stricture with limited prognosis, stenting alone may be sufficient and stone extraction may not be necessary, however, balloon dilation for stone extraction may be considered in cases of short-term stent obstruction.
While EST is the standard treatment for papillary dilatation, EPBD is also a viable option for younger patients who wish to reduce the risk of long-term recurrence and patients with coagulopathy. EPBD is considered to have a lower risk of bleeding and perforation than EST. Several methods have been recently proposed to reduce PEP, the greatest weakness of EPBD. We would also like to focus on ESBD, which should be the subject of future research.
For small stones in the CBD, it is not necessary to strictly distinguish between the retrieval balloon and the basket; however, if one device cannot remove the stone, it is recommended to use the other. In cases of pockets in the lower bile duct, Voltic catch V is also useful. It is also important to gain experience in the use of EUS-TD, lithotripter, and cholangioscopy to deal with troubleshooting such as stones stuck in the basket and difficult cases of stone retrieval.
In cases of complicated cholangitis, stone retrieval can be performed in mild or moderate cases in a single session. In severe cases, decompression alone should be considered, and EBS is generally recommended. Cases of CBD stones complicated with cholecystolithiasis that are scheduled for one-session surgical treatment or CBD stones complicated with distal biliary stricture should be treated in facilities with adequate experience and equipment.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Japan Gastroenterological Endoscopy Society; The Japanese Society of Gastroenterology; Japan Biliary Association; The Japan society of hepatology; Japan Pancreas Society; The Japanese Society of Internal Medicine; Japanese society of interventional radiology.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Huang Y, China; Miao G, China S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Melzer M, Toner R, Lacey S, Bettany E, Rait G. Biliary tract infection and bacteraemia: presentation, structural abnormalities, causative organisms and clinical outcomes. Postgrad Med J. 2007;83:773-776. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 101] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 2. | Kimura Y, Takada T, Strasberg SM, Pitt HA, Gouma DJ, Garden OJ, Büchler MW, Windsor JA, Mayumi T, Yoshida M, Miura F, Higuchi R, Gabata T, Hata J, Gomi H, Dervenis C, Lau WY, Belli G, Kim MH, Hilvano SC, Yamashita Y. TG13 current terminology, etiology, and epidemiology of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2013;20:8-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 124] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 3. | Ando T, Tsuyuguchi T, Okugawa T, Saito M, Ishihara T, Yamaguchi T, Saisho H. Risk factors for recurrent bile duct stones after endoscopic papillotomy. Gut. 2003;52:116-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 124] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 4. | Ding J, Li F, Zhu HY, Zhang XW. Endoscopic treatment of difficult extrahepatic bile duct stones, EPBD or EST: An anatomic view. World J Gastrointest Endosc. 2015;7:274-277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Ozawa N, Yasuda I, Doi S, Iwashita T, Shimizu M, Mukai T, Nakashima M, Ban T, Kojima I, Matsuda K, Matsuda M, Ishida Y, Okabe Y, Ando N, Iwata K. Prospective randomized study of endoscopic biliary stone extraction using either a basket or a balloon catheter: the BasketBall study. J Gastroenterol. 2017;52:623-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | Yu ZY, Liang C, Yang SY, Zhang X, Sun Y. The therapeutic effect of balloon dilatation with different duration for biliary duct calculi: A network meta-analysis. J Minim Access Surg. 2022;18:327-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 7. | Masuda S, Koizumi K, Nishino T, Tazawa T, Kimura K, Tasaki J, Ichita C, Sasaki A, Kako M, Uojima H, Sugitani A. Direct oral anticoagulants increase bleeding risk after endoscopic sphincterotomy: a retrospective study. BMC Gastroenterol. 2021;21:401. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Bhurwal A, Mutneja H, Goel A, Bansal V, Patel A, Brahmbhatt B, Sarkar A. No Significant Difference in Post-ERCP Bleeding Rates Between Dual Antiplatelet Agents and Aspirin Alone: A Systematic Review and Meta-analysis. J Clin Gastroenterol. 2022;56:546-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Elsnhory AB, Mandour OA, Montaser AG, Kereet IM, Rezk HS, Madhoon HW, Rabea RK, Ragab KM, Gbreel MI. A Systematic Review and Meta-analysis of Basket or Balloon Catheter for the Retrieval of Choledocholithiasis. Indian J Surg. 2022;. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Sharma R, Sharma V, Singhal U, Sanaka M. Outcomes of balloon vs basket catheter for clearance of choledocholithiasis: a systematic review and meta-analysis. Endosc Int Open. 2022;10:E1447-E1453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Hamada T, Yasunaga H, Nakai Y, Isayama H, Matsui H, Horiguchi H, Fushimi K, Koike K. Bleeding after endoscopic sphincterotomy or papillary balloon dilation among users of antithrombotic agents. Endoscopy. 2015;47:997-1004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 47] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 12. | Zhao HC, He L, Zhou DC, Geng XP, Pan FM. Meta-analysis comparison of endoscopic papillary balloon dilatation and endoscopic sphincteropapillotomy. World J Gastroenterol. 2013;19:3883-3891. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 50] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (1)] |
| 13. | Liu Y, Su P, Lin S, Xiao K, Chen P, An S, Zhi F, Bai Y. Endoscopic papillary balloon dilatation versus endoscopic sphincterotomy in the treatment for choledocholithiasis: a meta-analysis. J Gastroenterol Hepatol. 2012;27:464-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 14. | Yasuda I, Tomita E. Extracorporeal shockwave lithotripsy of common bile duct stones without preliminary endoscopic sphincterotomy. Scand J Gastroenterol. 1996;31:934-939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Manes G, Paspatis G, Aabakken L, Anderloni A, Arvanitakis M, Ah-Soune P, Barthet M, Domagk D, Dumonceau JM, Gigot JF, Hritz I, Karamanolis G, Laghi A, Mariani A, Paraskeva K, Pohl J, Ponchon T, Swahn F, Ter Steege RWF, Tringali A, Vezakis A, Williams EJ, van Hooft JE. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019;51:472-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 463] [Cited by in RCA: 375] [Article Influence: 62.5] [Reference Citation Analysis (0)] |
| 16. | Ryozawa S, Itoi T, Katanuma A, Okabe Y, Kato H, Horaguchi J, Fujita N, Yasuda K, Tsuyuguchi T, Fujimoto K. Japan Gastroenterological Endoscopy Society guidelines for endoscopic sphincterotomy. Dig Endosc. 2018;30:149-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 57] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 17. | Weinberg BM, Shindy W, Lo S. Endoscopic balloon sphincter dilation (sphincteroplasty) versus sphincterotomy for common bile duct stones. Cochrane Database Syst Rev. 2006;2006:CD004890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 86] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 18. | Dumonceau JM, Kapral C, Aabakken L, Papanikolaou IS, Tringali A, Vanbiervliet G, Beyna T, Dinis-Ribeiro M, Hritz I, Mariani A, Paspatis G, Radaelli F, Lakhtakia S, Veitch AM, van Hooft JE. ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2020;52:127-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 501] [Article Influence: 100.2] [Reference Citation Analysis (1)] |
| 19. | Disario JA, Freeman ML, Bjorkman DJ, Macmathuna P, Petersen BT, Jaffe PE, Morales TG, Hixson LJ, Sherman S, Lehman GA, Jamal MM, Al-Kawas FH, Khandelwal M, Moore JP, Derfus GA, Jamidar PA, Ramirez FC, Ryan ME, Woods KL, Carr-Locke DL, Alder SC. Endoscopic balloon dilation compared with sphincterotomy for extraction of bile duct stones. Gastroenterology. 2004;127:1291-1299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 239] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 20. | Park CH, Jung JH, Nam E, Kim EH, Kim MG, Kim JH, Park SW. Comparative efficacy of various endoscopic techniques for the treatment of common bile duct stones: a network meta-analysis. Gastrointest Endosc. 2018;87:43-57.e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 21. | Bergman JJ, Rauws EA, Fockens P, van Berkel AM, Bossuyt PM, Tijssen JG, Tytgat GN, Huibregtse K. Randomised trial of endoscopic balloon dilation versus endoscopic sphincterotomy for removal of bileduct stones. Lancet. 1997;349:1124-1129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 274] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 22. | Meng W, Leung JW, Zhang K, Zhou W, Wang Z, Zhang L, Sun H, Xue P, Liu W, Wang Q, Zhang J, Wang X, Wang M, Shao Y, Cai K, Hou S, Li Q, Zhu K, Yue P, Wang H, Zhang M, Sun X, Yang Z, Tao J, Wen Z, Chen B, Shao Q, Zhao M, Zhang R, Jiang T, Liu K, Chen K, Zhu X, Zhang H, Miao L, Li J, Yan X, Wang F, Suzuki A, Tanaka K, Nur U, Weiderpass E, Li X. Optimal dilation time for combined small endoscopic sphincterotomy and balloon dilation for common bile duct stones: a multicentre, single-blinded, randomised controlled trial. Lancet Gastroenterol Hepatol. 2019;4:425-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 23. | Tomoda T, Kato H, Ueki T, Akimoto Y, Hata H, Fujii M, Harada R, Ogawa T, Wato M, Takatani M, Matsubara M, Kawai Y, Okada H. Combination of Diclofenac and Sublingual Nitrates Is Superior to Diclofenac Alone in Preventing Pancreatitis After Endoscopic Retrograde Cholangiopancreatography. Gastroenterology. 2019;156:1753-1760.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 24. | Luo H, Zhao L, Leung J, Zhang R, Liu Z, Wang X, Wang B, Nie Z, Lei T, Li X, Zhou W, Zhang L, Wang Q, Li M, Zhou Y, Liu Q, Sun H, Wang Z, Liang S, Guo X, Tao Q, Wu K, Pan Y, Fan D. Routine pre-procedural rectal indometacin versus selective post-procedural rectal indometacin to prevent pancreatitis in patients undergoing endoscopic retrograde cholangiopancreatography: a multicentre, single-blinded, randomised controlled trial. Lancet. 2016;387:2293-2301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 156] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 25. | ASGE Standards of Practice Committee; Acosta RD, Abraham NS, Chandrasekhara V, Chathadi KV, Early DS, Eloubeidi MA, Evans JA, Faulx AL, Fisher DA, Fonkalsrud L, Hwang JH, Khashab MA, Lightdale JR, Muthusamy VR, Pasha SF, Saltzman JR, Shaukat A, Shergill AK, Wang A, Cash BD, DeWitt JM. The management of antithrombotic agents for patients undergoing GI endoscopy. Gastrointest Endosc. 2016;83:3-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 417] [Cited by in RCA: 458] [Article Influence: 50.9] [Reference Citation Analysis (1)] |
| 26. | Fujimoto K, Fujishiro M, Kato M, Higuchi K, Iwakiri R, Sakamoto C, Uchiyama S, Kashiwagi A, Ogawa H, Murakami K, Mine T, Yoshino J, Kinoshita Y, Ichinose M, Matsui T; Japan Gastroenterological Endoscopy Society. Guidelines for gastroenterological endoscopy in patients undergoing antithrombotic treatment. Dig Endosc. 2014;26:1-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 349] [Article Influence: 31.7] [Reference Citation Analysis (0)] |
| 27. | Veitch AM, Vanbiervliet G, Gershlick AH, Boustiere C, Baglin TP, Smith LA, Radaelli F, Knight E, Gralnek IM, Hassan C, Dumonceau JM. Endoscopy in patients on antiplatelet or anticoagulant therapy, including direct oral anticoagulants: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guidelines. Gut. 2016;65:374-389. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 176] [Cited by in RCA: 184] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 28. | Mirjalili SA, Stringer MD. The arterial supply of the major duodenal papilla and its relevance to endoscopic sphincterotomy. Endoscopy. 2011;43:307-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 29. | Masuda S, Koizumi K, Uojima H, Kimura K, Nishino T, Tasaki J, Ichita C, Sasaki A. Effect of Antibiotic Resistance of Pathogens on Initial Antibiotic Therapy for Patients With Cholangitis. Cureus. 2021;13:e18449. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 30. | Goong HJ, Moon JH, Lee YN, Choi HJ, Choi SY, Choi MH, Kim MJ, Lee TH, Park SH, Lee HK. The Role of Endoscopic Biliary Drainage without Sphincterotomy in Gallstone Patients with Cholangitis and Suspected Common Bile Duct Stones Not Detected by Cholangiogram or Intraductal Ultrasonography. Gut Liver. 2017;11:434-439. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 31. | Yasuda I, Fujita N, Maguchi H, Hasebe O, Igarashi Y, Murakami A, Mukai H, Fujii T, Yamao K, Maeshiro K, Tada T, Tsujino T, Komatsu Y. Long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation for bile duct stones. Gastrointest Endosc. 2010;72:1185-1191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 90] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 32. | Cai JS, Qiang S, Bao-Bing Y. Advances of recurrent risk factors and management of choledocholithiasis. Scand J Gastroenterol. 2017;52:34-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 33. | Ji X, Yang Z, Ma SR, Jia W, Zhao Q, Xu L, Kan Y, Cao Y, Wang Y, Fan BJ. New common bile duct morphological subtypes: Risk predictors of common bile duct stone recurrence. World J Gastrointest Surg. 2022;14:236-246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 34. | Takeshita K, Asai S, Fujimoto N, Ichinona T, Akamine E. Comparison of the effects of retrieval balloons and basket catheters for bile duct stone removal on the rate of post-ERCP pancreatitis. Hepatobiliary Pancreat Dis Int. 2021;20:203-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 35. | Ishiwatari H, Kawakami H, Hisai H, Yane K, Onodera M, Eto K, Haba S, Okuda T, Ihara H, Kukitsu T, Matsumoto R, Kitaoka K, Sonoda T, Hayashi T; Hokkaido Interventional EUS/ERCP Study (HONEST) Group. Balloon catheter versus basket catheter for endoscopic bile duct stone extraction: a multicenter randomized trial. Endoscopy. 2016;48:350-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 36. | Ekmektzoglou K, Apostolopoulos P, Dimopoulos K, Tsibouris P, Kalantzis C, Vlachou E, Kalafatis E, Alexandrakis G. Basket versus balloon extraction for choledocholithiasis: a single center prospective single-blind randomized study. Acta Gastroenterol Belg. 2020;83:577-584. [PubMed] |
| 37. | ASGE Standards of Practice Committee; Maple JT, Ikenberry SO, Anderson MA, Appalaneni V, Decker GA, Early D, Evans JA, Fanelli RD, Fisher D, Fisher L, Fukami N, Hwang JH, Jain R, Jue T, Khan K, Krinsky ML, Malpas P, Ben-Menachem T, Sharaf RN, Dominitz JA. The role of endoscopy in the management of choledocholithiasis. Gastrointest Endosc. 2011;74:731-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 128] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 38. | Ogura T, Okuda A, Miyano A, Nishioka N, Higuchi K. Intrahepatic bile duct stone removal through endoscopic ultrasound-guided hepaticogastrostomy using novel basket catheter under digital cholangioscopy guidance. Endoscopy. 2018;50:E301-E303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 39. | van der Merwe SW, van Wanrooij RLJ, Bronswijk M, Everett S, Lakhtakia S, Rimbas M, Hucl T, Kunda R, Badaoui A, Law R, Arcidiacono PG, Larghi A, Giovannini M, Khashab MA, Binmoeller KF, Barthet M, Perez-Miranda M, van Hooft JE. Therapeutic endoscopic ultrasound: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2022;54:185-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 298] [Cited by in RCA: 275] [Article Influence: 91.7] [Reference Citation Analysis (3)] |
| 40. | Khashab MA, El Zein MH, Sharzehi K, Marson FP, Haluszka O, Small AJ, Nakai Y, Park DH, Kunda R, Teoh AY, Peñas I, Perez-Miranda M, Kumbhari V, Van der Merwe S, Artifon EL, Ross AS. EUS-guided biliary drainage or enteroscopy-assisted ERCP in patients with surgical anatomy and biliary obstruction: an international comparative study. Endosc Int Open. 2016;4:E1322-E1327. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 75] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 41. | Iwashita T, Uemura S, Mita N, Iwasa Y, Ichikawa H, Mukai T, Yasuda I, Shimizu M. Endoscopic ultrasound guided-antegrade biliary stenting vs percutaneous transhepatic biliary stenting for unresectable distal malignant biliary obstruction in patients with surgically altered anatomy. J Hepatobiliary Pancreat Sci. 2020;27:968-976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 42. | Mukai S, Itoi T, Baron TH, Takada T, Strasberg SM, Pitt HA, Ukai T, Shikata S, Teoh AYB, Kim MH, Kiriyama S, Mori Y, Miura F, Chen MF, Lau WY, Wada K, Supe AN, Giménez ME, Yoshida M, Mayumi T, Hirata K, Sumiyama Y, Inui K, Yamamoto M. Indications and techniques of biliary drainage for acute cholangitis in updated Tokyo Guidelines 2018. J Hepatobiliary Pancreat Sci. 2017;24:537-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 119] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 43. | Buxbaum JL, Buitrago C, Lee A, Elmunzer BJ, Riaz A, Ceppa EP, Al-Haddad M, Amateau SK, Calderwood AH, Fishman DS, Fujii-Lau LL, Jamil LH, Jue TL, Kwon RS, Law JK, Lee JK, Naveed M, Pawa S, Sawhney MS, Schilperoort H, Storm AC, Thosani NC, Qumseya BJ, Wani S. ASGE guideline on the management of cholangitis. Gastrointest Endosc. 2021;94:207-221.e14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 40] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 44. | Cianci P, Restini E. Management of cholelithiasis with choledocholithiasis: Endoscopic and surgical approaches. World J Gastroenterol. 2021;27:4536-4554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 99] [Cited by in RCA: 81] [Article Influence: 20.3] [Reference Citation Analysis (15)] |
| 45. | Williams EJ, Green J, Beckingham I, Parks R, Martin D, Lombard M; British Society of Gastroenterology. Guidelines on the management of common bile duct stones (CBDS). Gut. 2008;57:1004-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 353] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 46. | Singh AN, Kilambi R. Single-stage laparoscopic common bile duct exploration and cholecystectomy versus two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy for patients with gallbladder stones with common bile duct stones: systematic review and meta-analysis of randomized trials with trial sequential analysis. Surg Endosc. 2018;32:3763-3776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 100] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 47. | Berthou JCh, Dron B, Charbonneau P, Moussalier K, Pellissier L. Evaluation of laparoscopic treatment of common bile duct stones in a prospective series of 505 patients: indications and results. Surg Endosc. 2007;21:1970-1974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 57] [Article Influence: 3.2] [Reference Citation Analysis (1)] |
| 48. | Martin IJ, Bailey IS, Rhodes M, O'Rourke N, Nathanson L, Fielding G. Towards T-tube free laparoscopic bile duct exploration: a methodologic evolution during 300 consecutive procedures. Ann Surg. 1998;228:29-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 125] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 49. | Decker G, Borie F, Millat B, Berthou JC, Deleuze A, Drouard F, Guillon F, Rodier JG, Fingerhut A. One hundred laparoscopic choledochotomies with primary closure of the common bile duct. Surg Endosc. 2003;17:12-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 93] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 50. | Cuschieri A, Croce E, Faggioni A, Jakimowicz J, Lacy A, Lezoche E, Morino M, Ribeiro VM, Toouli J, Visa J, Wayand W. EAES ductal stone study. Preliminary findings of multi-center prospective randomized trial comparing two-stage vs single-stage management. Surg Endosc. 1996;10:1130-1135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 94] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 51. | Tranter SE, Thompson MH. Comparison of endoscopic sphincterotomy and laparoscopic exploration of the common bile duct. Br J Surg. 2002;89:1495-1504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 141] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 52. | Poulose BK, Speroff T, Holzman MD. Optimizing choledocholithiasis management: a cost-effectiveness analysis. Arch Surg. 2007;142:43-8; discussion 49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 53. | Huang XX, Wu JY, Bai YN, Lv JH, Chen WZ, Huang LM, Huang RF, Yan ML. Outcomes of laparoscopic bile duct exploration for choledocholithiasis with small common bile duct. World J Clin Cases. 2021;9:1803-1813. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 54. | Tringali A, Costa D, Fugazza A, Colombo M, Khalaf K, Repici A, Anderloni A. Endoscopic management of difficult common bile duct stones: Where are we now? World J Gastroenterol. 2021;27:7597-7611. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (3)] |
| 55. | Ogura T, Kawai J, Nishiguchi K, Yamamoto Y, Higuchi K. Transluminal intrahepatic bile duct stone removal using a novel spiral basket catheter via the endoscopic ultrasound-guided hepaticogastrostomy route (with video). Dig Endosc. 2022;34:234-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 56. | Siiki A, Helminen M, Sand J, Laukkarinen J. Covered self-expanding metal stents may be preferable to plastic stents in the treatment of chronic pancreatitis-related biliary strictures: a systematic review comparing 2 methods of stent therapy in benign biliary strictures. J Clin Gastroenterol. 2014;48:635-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 57. | Haapamäki C, Kylänpää L, Udd M, Lindström O, Grönroos J, Saarela A, Mustonen H, Halttunen J. Randomized multicenter study of multiple plastic stents vs. covered self-expandable metallic stent in the treatment of biliary stricture in chronic pancreatitis. Endoscopy. 2015;47:605-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 87] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 58. | Devière J, Nageshwar Reddy D, Püspök A, Ponchon T, Bruno MJ, Bourke MJ, Neuhaus H, Roy A, González-Huix Lladó F, Barkun AN, Kortan PP, Navarrete C, Peetermans J, Blero D, Lakhtakia S, Dolak W, Lepilliez V, Poley JW, Tringali A, Costamagna G; Benign Biliary Stenoses Working Group. Successful management of benign biliary strictures with fully covered self-expanding metal stents. Gastroenterology. 2014;147:385-95; quiz e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 170] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 59. | Bonnel DH, Fingerhut AL. Percutaneous transhepatic balloon dilatation of benign bilioenteric strictures: long-term results in 110 patients. Am J Surg. 2012;203:675-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 55] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 60. | Quintero GA, Patiño JF. Surgical management of benign strictures of the biliary tract. World J Surg. 2001;25:1245-1250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 61. | Kitano M, Gress TM, Garg PK, Itoi T, Irisawa A, Isayama H, Kanno A, Takase K, Levy M, Yasuda I, Lévy P, Isaji S, Fernandez-Del Castillo C, Drewes AM, Sheel ARG, Neoptolemos JP, Shimosegawa T, Boermeester M, Wilcox CM, Whitcomb DC. International consensus guidelines on interventional endoscopy in chronic pancreatitis. Recommendations from the working group for the international consensus guidelines for chronic pancreatitis in collaboration with the International Association of Pancreatology, the American Pancreatic Association, the Japan Pancreas Society, and European Pancreatic Club. Pancreatology. 2020;20:1045-1055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 48] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 62. | Shen ZY, Wang JJ, Lu LG, Wan R, Wan XJ, Cai XB. The efficacy and safety of balloon dilation for unresectable malignant biliary obstruction before placement of self-expanding metal stents. J Dig Dis. 2020;21:293-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |