Published online Mar 7, 2022. doi: 10.3748/wjg.v28.i9.918
Peer-review started: November 10, 2021
First decision: December 3, 2021
Revised: December 14, 2021
Accepted: January 22, 2022
Article in press: January 22, 2022
Published online: March 7, 2022
Processing time: 112 Days and 21.7 Hours
Intestinal ischemia/reperfusion (I/R) injury is a fatal syndrome that occurs under many clinical scenarios. The apoptosis of intestinal cells caused by ischemia can cause cell damage and provoke systemic dysfunction during reperfusion. However, the mechanism of I/R-induced apoptosis remains unclear. Cystic fibrosis transmembrane conductance regulator (CFTR) is a cAMP-activated chloride channel. Few researchers have paid attention to its role in intestinal I/R injury, or the relationship between CFTR and intestinal apoptosis induced by hypoxia/reoxygenation (H/R).
To investigate the effects of CFTR on I/R-induced intestinal apoptosis and its underlying molecular mechanisms.
An intestinal I/R injury model was established in mice with superior mesenteric artery occlusion, and Caco2 cells were subjected to H/R for the simulation of I/R in vivo.
The results suggested that CFTR overexpression significantly increased the Caco2 cell viability and decreased cell apoptosis induced by the H/R. Interestingly, we found that the translocation of p65, an NF-κB member, from the cytoplasm to the nucleus after H/R treatment can be reversed by the overexpression of CFTR, the NF-κB P65 would return from the nucleus to the cytoplasm as determined by immunostaining. We also discovered that CFTR inhibited cell apoptosis in the H/R-treated cells, and this effect was significantly curbed by the NF-κB activator BA, AKT inhibitor GSK690693 and the PI3K inhibitor LY294002. Moreover, we demonstrated that CFTR overexpression could reverse the decreased PI3K/AKT expression induced by the I/R treatment in vivo or H/R treatment in vitro.
The results of the present study indicate that the overexpression of CFTR protects Caco2 cells from H/R-induced apoptosis; furthermore, it also inhibits H/R-induced apoptosis through the PI3K/AKT/NF-κB signaling pathway in H/R-treated Caco2 cells and intestinal tissues.
Core Tip: Intestinal ischemia/reperfusion (I/R) injury is a fatal syndrome that occurs under many clinical scenarios. The apoptosis of intestinal cells caused by ischemia can cause cell damage and provoke systemic dysfunction during reperfusion. However, the mechanism of I/R-induced apoptosis remains unclear. In our paper, our data demonstrate that cystic fibrosis transmembrane conductance regulator (CFTR) is downregulated in hypoxia/reoxygenation (H/R)-treated Caco2 cells, and overexpression of CFTR protects Caco2 cells from H/R-induced apoptosis. Additionally, CFTR is involved in inhibiting H/R-induced apoptosis, and it inhibits apoptosis through PI3K/AKT/NF-κB signaling pathway. In all, this work suggests that overexpression of CFTR attenuates H/R-induced apoptosis through PI3K/AKT/NF-κB signaling pathway in H/R-treated Caco2 cells.
- Citation: Dong ZW, Liu H, Su FF, Fan XZ, Zhang Y, Liu P. Cystic fibrosis transmembrane conductance regulator prevents ischemia/reperfusion induced intestinal apoptosis via inhibiting PI3K/AKT/NF-κB pathway. World J Gastroenterol 2022; 28(9): 918-932
- URL: https://www.wjgnet.com/1007-9327/full/v28/i9/918.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i9.918
Intestinal ischemia/reperfusion (I/R) injury is a fatal syndrome that occurs in different critical clinical scenarios, including acute mesenteric ischemia, burn injury, sepsis, and hemorrhagic shock, and is characterized by high incidence and mortality rates[1]. Intestinal I/R causes local injuries in the intestine and multiple organ dysfunction syndromes or even multiple organ failure (MOF) in distant organs with a mortality rate ranging from 30%–90%[2]. The underlying mechanisms are very complex, including damage by oxygen radicals, the release of large numbers of inflammatory factors, bacterial translocation, and cell apoptosis. Protecting intestinal apoptosis is one of the critical targets in treating patients with intestinal I/R injury.
The innate and adaptive apoptosis resulting from intracellular damage and translocation of gut pathogens play a critical role in the pathological process of intestinal I/R[3]. The apoptosis of intestinal cells induced by ischemia can cause cell damage and activate epithelial barrier dysfunction during reperfusion, leading to system dysfunction[4]. However, the mechanism of apoptosis induced by H/R remains unclear.
Cystic fibrosis transmembrane conductance regulator (CFTR), a cAMP-activated chloride channel, mutations of which cause the most common lethal genetic disease[5]. Mutation in CFTR causes cystic fibrosis (CF) and induces severe damage to body organs, especially the lungs and digestive system. Extensive research on the role of CFTR has focused on epithelial cell function, while its role in other types of cells, such as endothelial cells, is largely unclear[6]. Many studies have indicated that patients with CF had endothelial perturbation and microvascular dysfunction, suggesting that CFTR deficiency contributes to endothelial dysfunction[7]. Furthermore, CFTR protects against endothelial apoptosis from oxidative stress and inflammation[8]. However, the relationship between CFTR and I/R-induced apoptosis in enterocytes has not been reported.
It was reported that the activation of the NF-κB signaling pathway is involved in apoptosis, autophagy, and inflammatory gene transcription[1,9]. Moreover, NF-κB can be the target for disease treatment. Inhibition of NF-κB activation could attenuate LPS-induced apoptosis[1]. H/R stress was reported to trigger apoptosis by impairing NF-ĸB survival signaling in malignant B cells[10]. Additionally, the PI3K/AKT pathway is considered an essential regulatory factor in NF-κB activation. Conditional CFTR knockout mice showed increased inflammatory cell infiltration and activation of the NF-ĸB signaling pathway[4]. In endothelial cells, CFTR modulates inflammation by regulating the NF-ĸB signaling[11]. But how CFTR modulates PI3K/AKT/NF-ĸB signaling in apoptosis induced by H/R has not been fully elucidated.
It was hypothesized that CFTR could affect I/R-induced intestinal apoptosis through the NF-ĸB signaling pathway. In this study, a CFTR activator and CFTR overexpression vector were used to investigate the effects of CFTR on I/R-induced intestinal apoptosis and its underlying molecular mechanisms.
Caco2 cells purchased from American Type Culture Collection were maintained in a high-glucose DMEM medium (Gibco, Rockville, MD, United States) supplemented with 10% fetal bovine serum (Gibco, Rockville, MD, United States), 100-U/mL penicillin, 100-mg/mL streptomycin (Sigma, St. Louis, MO, United States), and 5% CO2 at 37 °C in a humidified atmosphere for 48 h. To mimic hypoxic conditions, the cells were incubated in a microaerophilic system (Thermo Fisher Scientific, Waltham, MA, United States) with 5% CO2 and 1% O2 balanced with 94% N2 for 12 h. Then, the cells were cultured under normal conditions for 0, 12, 24, and 48 h to achieve reoxygenation.
For inhibitor treatment, the cells were incubated with NF-κB inhibitor BAY11 (40 μmol/L) (Beyotime, Nantong, China), AKT activator IGF-1 (20 μmol/L) (Beyotime, Nantong, China), PI3K activator (740 Y-P, 10 μmol/L) (Beyotime, Nantong, China), NF-κB activator Betulinic acid (BA) (20 μmol/L) (Beyotime, Nantong, China), AKT inhibitor GSK690693 (20 μmol/L) (Beyotime, Nantong, China), and PI3K inhibitor LY294002 (10 μmol/L) (Beyotime, Nantong, China) for 1–8 h and then subjected to H/R. The cells were used for various experiments at different times after the H/R treatment.
To overexpress CFTR, Caco2 cells were transfected with the expression vector Human CFTR lentivirus (LV-CFTR), which was bought from Genechem Company (Shanghai Genechem Co., Ltd., Shanghai, China). The lentivirus was transfected into the Caco2 cells (80% confluence) at the multiplicity of infection (MOI) 20 before the experiment. After 6 h, the cell culture medium was replaced with a fresh medium, and the cells were used for the experiments 2 d later.
Cell counting kit-8 (CCK8; Dojindo Laboratories, Kumamoto, Japan) assay was employed to investigate cell survival following the manufacturer’s instructions. In brief, Caco2 cells after various treatments were plated in 96-well plates at a density of 2.5 × 103 cells/well. On the other day, 15-μL CCK-8 was added to each well and incubated at 37 °C for 4 h. Absorbance was measured at 450 nm using a microplate spectrophotometer (Molecualr Devices LLC, Sunnyvale, CA, United States).
According to instruction, one-step TUNEL apoptosis assay kit (Beyotime, Nantong, China) was used to conduct TUNEL staining. The images of the FITC-labeled TUNEL-positive cells were captured using a fluorescence microscope (Nikon Corporation, Tokyo, Japan). The nick-ends labeled in red indicated apoptotic cells. The cell nucleus was labeled in blue using DAPI (Invitrogen, Carlsbad, CA, United States).
Western blotting was conducted as previously described[11]. Briefly, total proteins were obtained from cultured Caco2 cells using RIPA (Beyotime, Nantong, China), and the concentrations were tested using the bicinchoninic acid (BCA) Protein Assay Kit (Pierce, Rockford, IL, United States). The intestinal tissues were taken and washed thrice with PBS, then stored at -80 °C. A 100-μg intestinal tissue was removed for the Western blotting using the same protocol used for the isolation of the cell protein; further, 50-μg protein was separated in 10% SDS-PAGE and transferred to PVDF membranes. The membranes were blocked in 5% nonfat dry milk and then probed with mouse monoclonal anti-p-NF-κB p65 and anti-NF-κB p65 (1:2000 dilution, Cell Signaling Technology, Danvers, MA, United States), and rabbit anti-GAPDH (1:1000 dilution; Santa Cruz Biotechnology, Dallas, TX, United States) overnight at 4 °C. On the other day, membranes were then incubated with the HRP-conjugated anti-rabbit or goat anti-mouse secondary antibody (1:3000; Santa Cruz Biotechnology, Dallas, TX, United States) for 1 h at room temperature. The protein bands were visualized using Amersham Hyperfilm™ ECL (Thermo Fisher Scientific; former, MA, United States). ImageJ 1.41o software (National Institutes of Health (Bethesda, MD, United States) was used to quantify protein expression.
C57BL/6J mice aged 8–12 wk old were supplied by the Experimental Animal Center at the southwest hospital. All experimental procedures conformed to the institutional guidelines and protocols approved by the Animal Care and Use Committee of Air Force Medical Center. All animal studies complied with the principle for replacement, refinement, or reduction. The mice were randomly separated into five groups (n = 8): Sham and I/R groups (45 min of ischemia and reperfusion for 30, 90, 720, and 1440 min). All animals were group-housed with 2–3 mice per cage on a 12 h light/dark cycle in a temperature-controlled (25 °C ± 2 °C) room with free access to water and food. Before the experiment, all mice were fasted for 24 h, but the water was supplied. The animals were anesthetized with intraperitoneal injection, 1.0–1.25 g/kg 10% urethane in 0.9% saline (w/v) (Sigma-Aldrich, St. Louis, MO, United States), and all mice were kept under anesthesia during the surgery period[12]. In the Sham group, the wound was closed after finding the superior mesenteric artery using laparotomy. In I/R groups, the abdominal cavity was opened, the superior mesenteric artery and its adjacent tissues were cautiously isolated and clamped using a microvascular clip for 45 min to induce ischemia, and then the clip was gently removed to allow reperfusion for 30, 90, 720, and 1440 min. After the procedure, the surgical incision was sutured with sutures. The mice were placed on a warming plate and sacrificed after the injury during the process. Then, the whole intestines were obtained and stored at -80 °C, which was used for the test[13]. FSK, an adenylate cyclase activator, was administered to activate the CFTR chloride channel for Con + FSK and I/R + FSK groups through intraperitoneal injection (2 mg/kg, Sigma-Aldrich, United States)[14].
The GraphPad Prism 7.0 statistical software (GraphPad Software, Inc., La Jolla, San Diego, CA, United States) was used for statistical analysis. Data are presented as mean ± SD. Multiple comparisons between more than two groups were analysed by one-way ANOVA test or Kruskal–Wallis test (non-parametric). P < 0.05 was considered statistically significant.
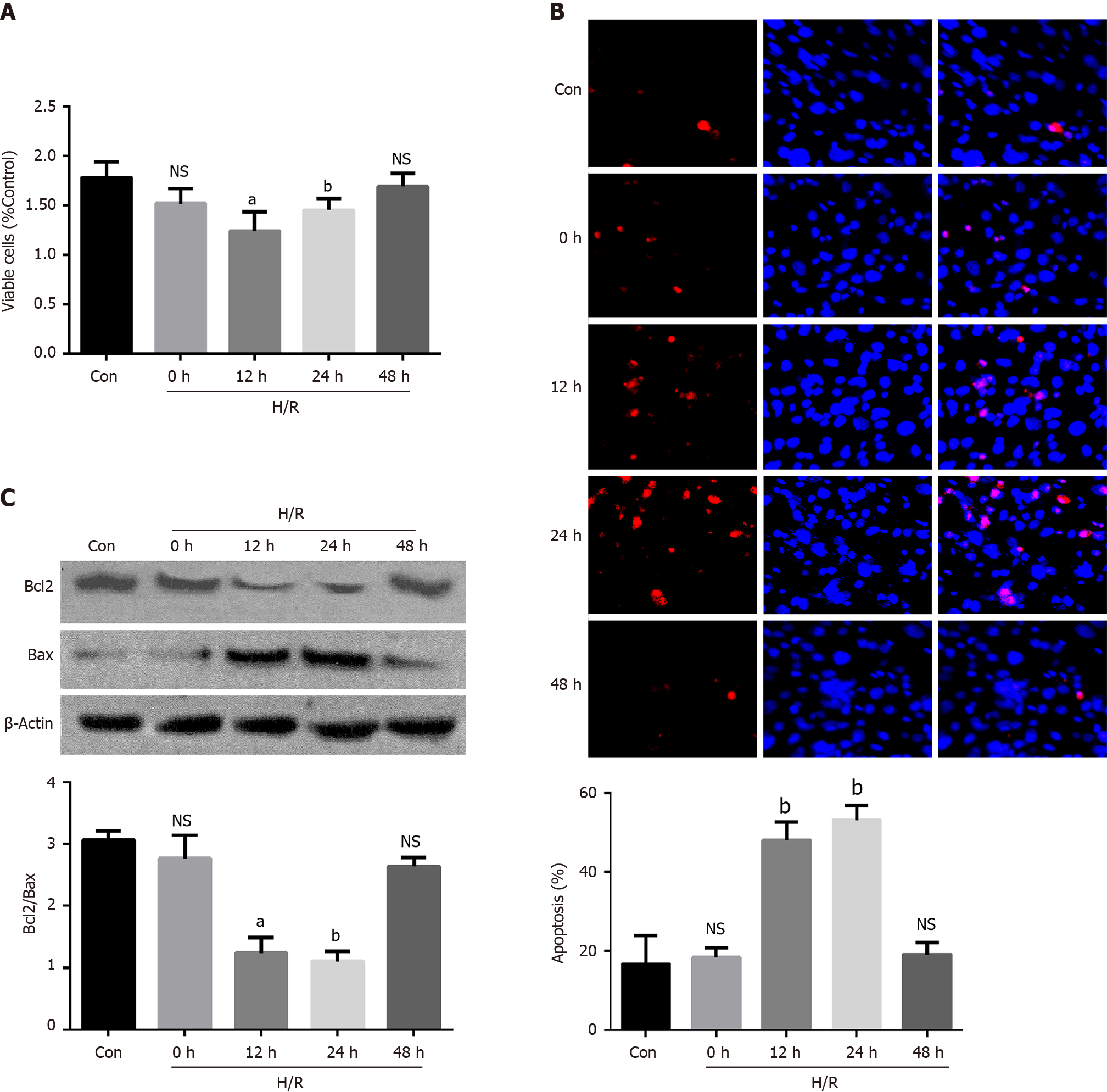
To investigate the effect of H/R injury on cell injuries, cell viability was examined in vitro. As shown in Figure 1A, after a reoxygenation period of 12 h and 24 h, cell viability decreased significantly compared with the control group, and returned to normal 48 h after reoxygenation. Meanwhile, as shown in Figure 1B, after the reoxygenation period, the percentage of apoptosis was elevated compared with the control group, and it also returned to normal 48 h after reoxygenation. The western blotting was used to test the cell apoptosis after H/R treatment. The results showed that the ratio of Bcl-2/Bax was significantly decreased at 12 h and 24 h, indicating that apoptosis was remarkably elevated by the H/R treatment (Figure 1C).
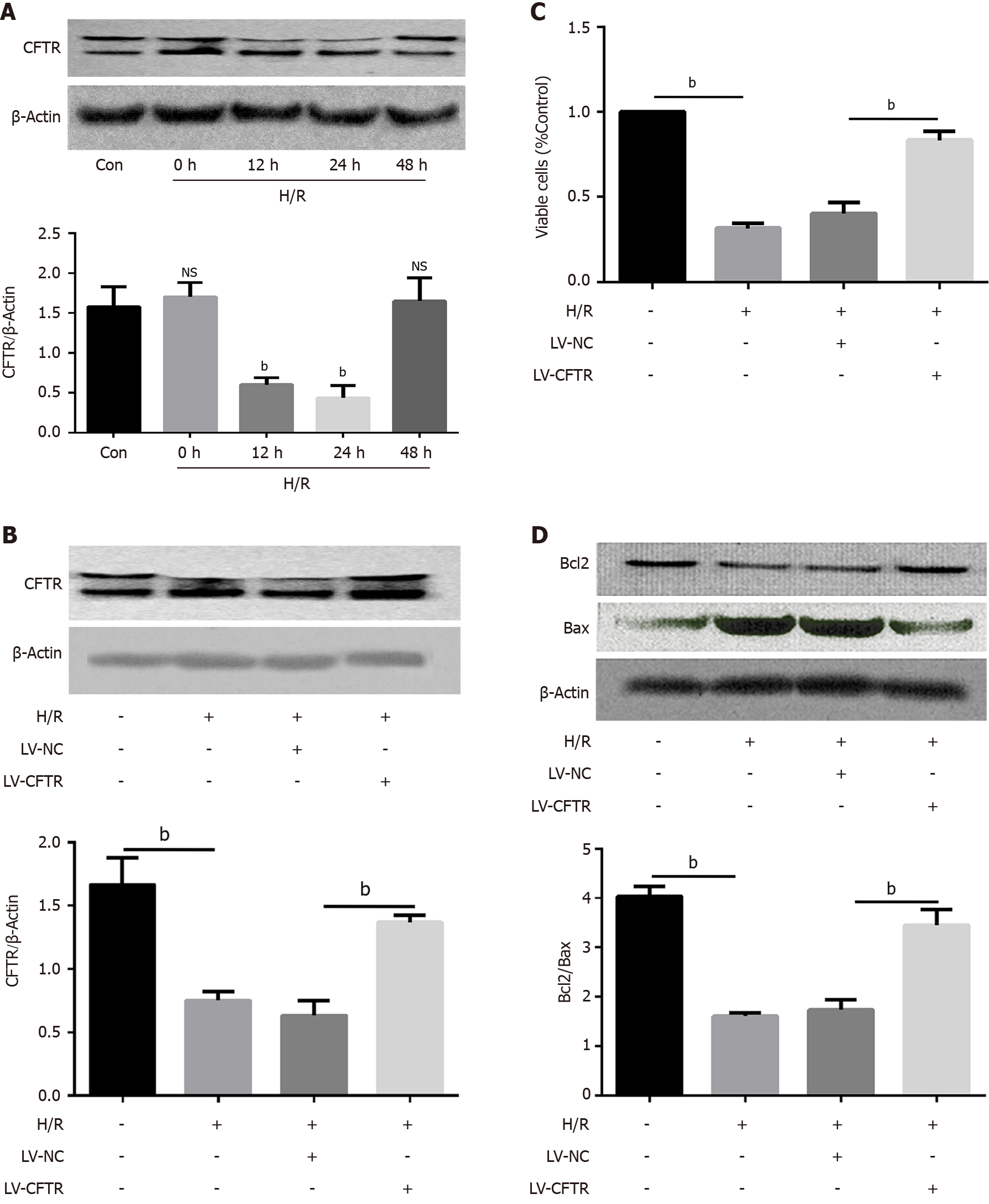
To explore the effect of CFTR on H/R-induced apoptosis, the expression of the CFTR protein before and after H/R was assessed using western blotting analysis of protein lysate from the H/R treatment Caco2 cells. The results indicated that CFTR proteins were detectable at high levels in the control group, while its level was remarkably downregulated 12 h and 24 h after reoxygenation (Figure 2A). To assess whether CFTR was responsible for altering the levels of apoptosis markers, the endogenous CFTR in Caco2 cells was increased by approximately 80% using the LV-CFTR. Infection of Caco2 cells with LV-CFTR 2 d before the experiment modestly increased CFTR levels compared with Caco2 cells infected with LV-NC (lentivirus expressed with empty vector). In addition, LV-CFTR also increased CFTR levels in Caco2 cells treated with H/R treatment (Figure 2B). Considering that the apoptosis reached its maximum at 12 h (Figure 1B and C), this time point was used to test the effect of CFTR on cell apoptosis. It was discovered that the CFTR overexpression significantly increased the viability of Caco2 cells induced by H/R treatments (Figure 2C), and Caco2 cells with high LV-CFTR expression had increased levels of Bcl-2/Bax (P < 0.001) compared to the control infected with LV-NC (Figure 2D). These results indicate that CFTR can protect the Caco2 cells from apoptosis induced by the H/R treatment.
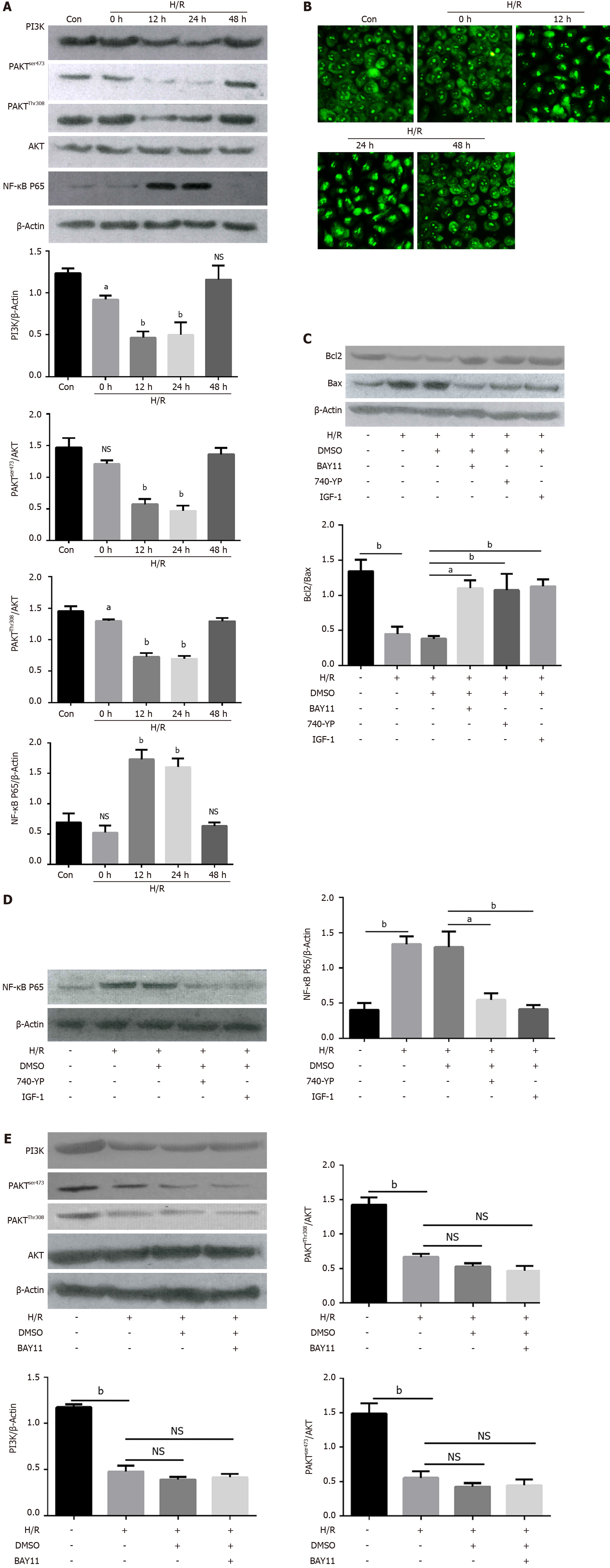
It has been reported that PI3K/AKT/NF-κB mediates the H/R injury in many physiological and pathological means, including apoptosis, inflammation, autophagy, etc. The effect of H/R on the PI3K/AKT/NF-κB pathway was quantified in the Caco2 cells. As shown in Figure 3A, the protein expressions of PI3K, phosphorylated AKTser473 (p-AKTser473), phosphorylated AKTThr308 (p-AKTThr308) were decreased 12 h and 24 h after the H/R treatment, and returned to normal at 48 h; on the contrary, the activation of the NF-κB P65 was upregulated 12 h and 24 h after the H/R treatment. More importantly, H/R treatment provoked the translocation of p65, an NF-κB member, from the cytoplasm to the nucleus at 12 h and 24 h, as observed through immunofluorescence staining, and then returned to the cytoplasm at 48 h (Figure 3B). Furthermore, the cells were treated with NF-κB inhibitor BAY11 (40 μmol/L), AKT activator IGF-1(20 μmol/L), and PI3K activator (740 Y-P, 10 μmol/L) 6 h before the H/R experiment, apoptotic activity was checked 12 h after the H/R treatment. Interestingly, we discovered that NF-κB inhibitor, AKT activator, and PI3K activator could reverse the H/R-induced cell apoptosis (Figure 3C). Furthermore, the PI3K and AKT activator significantly decreased the NF-κB elevations induced by the H/R (Figure 3D), whereas the NF-κB inhibitor could not impend the decline of PI3K and AKT in H/R-treated cells (Figure 3E), indicating that NF-κB was downstream of PI3K and AKT in the H/R-treated cells. All of these results suggested that PI3K/AKT/NF-κB pathway is involved in H/R-induced apoptosis.
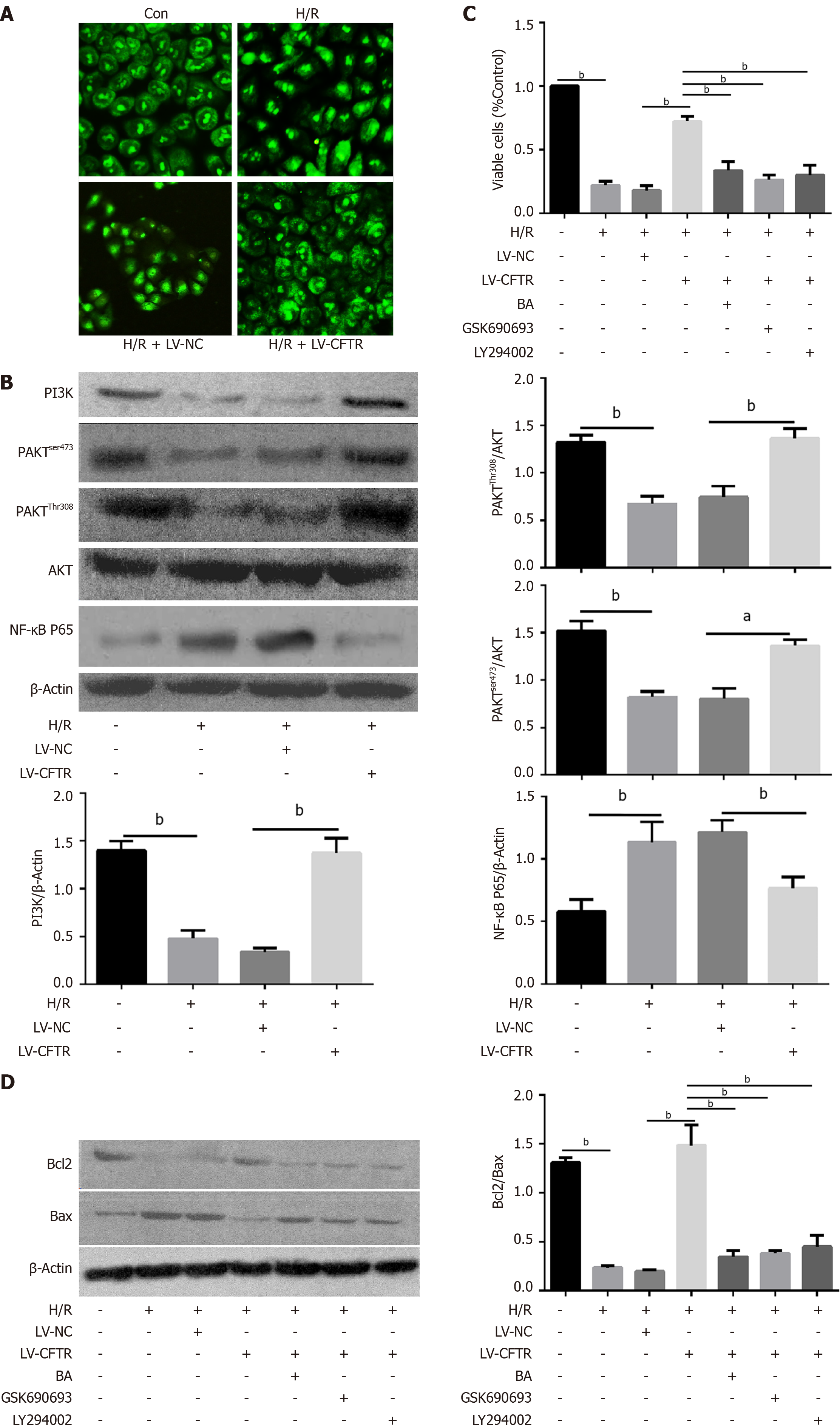
Previous research has established that CFTR can regulate PI3K/AKT/NF-κB pathway in tumor cell migration and cell permeability. To assess the relationship between CFTR and PI3K/AKT/NF-κB in H/R-induced apoptosis, CFTR was overexpressed and the H/R condition stimulated. Interestingly, compared with the H/R treatment groups, the overexpression of CFTR can inhibit the NF-κB P65 activation and instigate the return of NF-κB P65 from nuclei to the cytoplasm (Figure 4A). The results showed that overexpression of CFTR significantly limited the activation of the NF-κB p65 induced by the H/R treatment, and can also increase the PI3K/AKT expression (Figure 4B). Furthermore, cells were treated with NF-κB activator betulinic acid (BA) (20 μmol/L), AKT inhibitor GSK690693 (20 μmol/L), and PI3K inhibitor LY294002 (10 μmol/L) 6 h before the H/R treatment experiment. Our results implied that CFTR increased cell viability and inhibited cell apoptosis in the H/R-treated cells, and this effect was significantly inhibited by BA, GSK690693, and LY294002 (Figure 4C). Furthermore, results from western blotting showed that CFTR could not increase Bcl-2/Bax ration after BA, GSK690693, and LY294002 treatment (Figure 4D). Together, these results indicate that the inhibition of PI3K/AKT or the activation of NF-κB both impeded the protective effect of CFTR on H/R-induced apoptosis, and also demonstrate that CFTR protects the Caco2 cells from H/R-induced apoptosis by inhibiting the PI3K/AKT/NF-κB pathway.
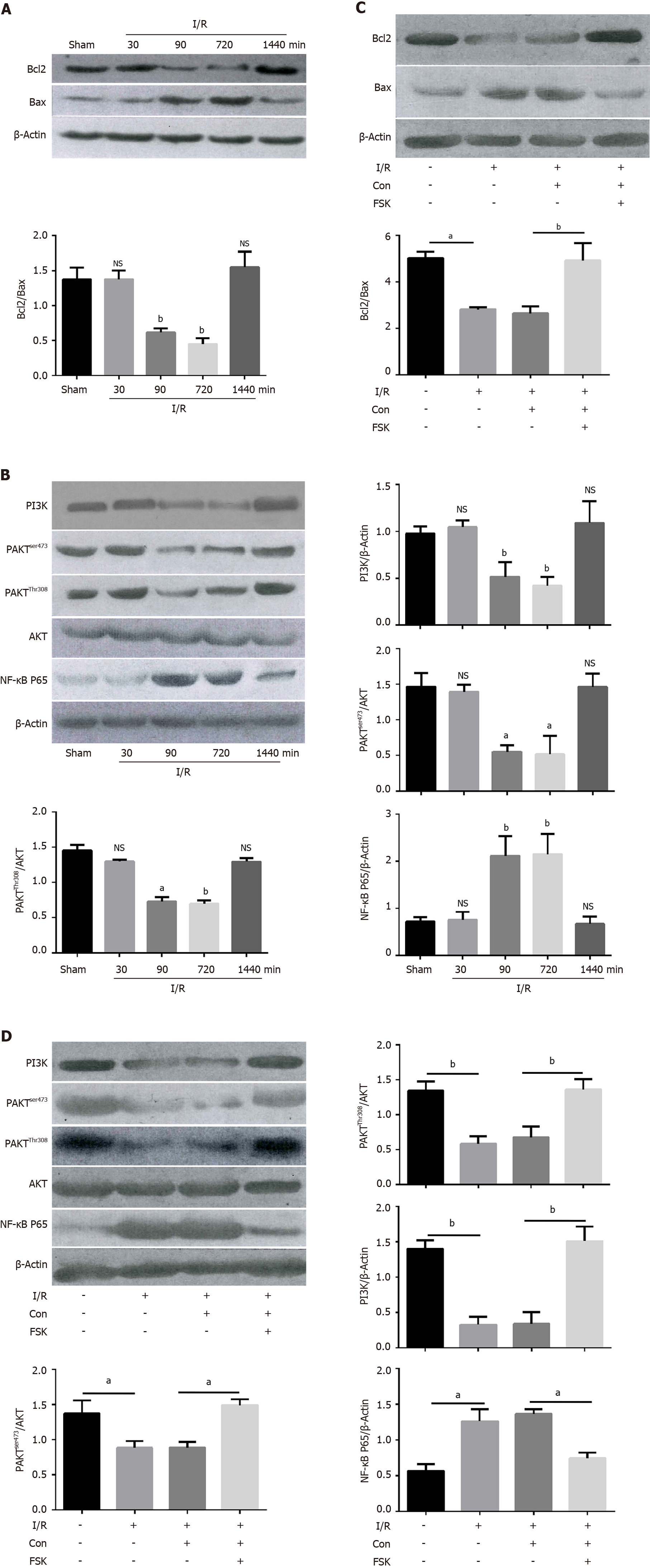
To assess whether the findings of CFTR in Caco2 cell lines were relevant to animal models in vivo, we performed the I/R-induced intestinal injury in animal models. Results from the western blotting demonstrated that the ratio of Bcl-2/Bax was significantly decreased at 90 min and 720 min, indicating that I/R treatment could significantly instigate apoptosis in vivo (Figure 5A), and the expressions of PI3K, p-AKTser473 and p-AKTThr308 were all decreased at 90 and 720 min, but they all returned to the normal level at 1440 min (Figure 5B). Similarly, the activation of the NF-κB P65 was increased at 90 and 720 min after the I/R treatment (Figure 5B). Furthermore, we treated the animals with the FSK, an activator of adenylate cyclase, and checked the apoptosis after I/R treatment. As shown in Figure 5C, the apoptosis of the intestines after FSK administration was significantly lower than those who received control treatment. The NF-κB was also activated in the I/R treatment and downregulated by the FSK administration. FSK administration could also increase the expression of PI3K and AKT, which was downregulated by I/R treatment (Figure 5D). To sum up, results indicate that CFTR can attenuate intestinal apoptosis in the I/R treatment model relating to the PI3K/AKT/NF-κB pathway.
To the best of our knowledge, this study is the first to investigate the possible involvement of CFTR, as an essential therapeutic target, in I/R injury. Additionally, it has been demonstrated that CFTR/PI3K/AKT/NF-κB pathway is the underlying signaling mechanism in the I/R-induced intestinal cell apoptosis.
I/R can cause intestinal mucosal injury, ultimately leading to bacterial translocation, sepsis, MOF, and eventually death[15,16]. I/R injury is caused by complex pathological damage with different factors involved. Early tissue ischemia could induce intestinal mucosal barrier dysfunction, while subsequent reperfusion could cause oxidative stress, cell apoptosis, and immune activation[1,5]. Many studies have shown that H/R can induce apoptosis and necrosis in various cell lines, including lymphocytes, blood cells, and cancer cells[12]. However, the sensitivity of different cell lines differ widely according to the H/R exposure[17]. In our study, the focus was on the effect of H/R on intestinal cells. After hypoxia, cell viability significantly reduced compared with the control group in the time point of 12 h and 24 h after reo
The effect of H/R stimulation on cells is multifaceted and holistic, including all intracellular biochemical reactions and intracellular structures. In the process of H/R, several physiological changes were induced after H/R treatment in the cell, such as the cytoskeleton, intracellular calcium concentration, HSP and mitochondrial, etc.[18]. Thus, it is necessary to investigate the primary mechanism of H/R-induced apoptosis in Caco2 cells, and it is vital to identify new targets for the therapy of intestinal injury. Activation of NF-κB controls multiple cellular processes and several molecules involved in apoptosis[19]. CFTR maintains NF-κB activation by inhibiting the degradation of kappa B kinase γ (IKKγ) inhibitor[20]. It was also reported that the phosphorylation of NF-κB p65 was reduced in CFTR knockdown mice[21]. A recent study on intestinal Caco2 cells also found that knockdown of CFTR significantly increased IκB phosphorylation compared to control cells under IL-1β stimulation[7]. Despite the well-demonstrated inverse relationship between CFTR and NF-κB activation in various experimental settings[22,23], the solid evidence linking CFTR mutation to aberrant NF-κB activation remains mysteriously missing. Moreover, most studies focus on the relationship between CFTR/NF-κB and apoptosis in lung epithelial injury[7,24]. And the role of CFTR and NF-κB in intestinal apoptosis caused by H/R remains unclear. In our study, the activation of NF-κB P65 was upregulated at 12 h and 24 h after the H/R treatment. And H/R treatment provoked the translocation of p65 from the cytoplasm to the nucleus at 12 h and 24 h, as observed through immunofluorescence staining, and then returned to the cytoplasm at 48 h. Additionally, NF-κB inhibitor BAY11 could reduce the apoptotic activity induced by the H/R treatment. And CFTR overexpression could inhibit the NF-κB P65 activation and make the NF-κB p65 come back from the nucleus to the cytoplasm. These results indicated that overexpression of CFTR significantly limited the activation of the NF-κB p65, which was caused by the H/R treatment.
PI3K/AKT plays a role in inducing inflammation, oxidative stress, and apoptosis in tissue injuries[15,25]. The key signaling molecule of PI3K is Akt[26]. Previous studies have observed the correlation of CFTR with PI3K/AKT pathway in both physiological and pathological conditions. Aberrant activity of AKT has been observed in CF cells and mice. For instance, the macrophages obtained from CF mice shed a significant decrease in AKT phosphorylation at serine 473 compared with those obtained from wild-type mice after LPS challenge, which might contribute to the extravagant inflammatory response manifested by CF mice. Accordingly, insulin-induced activation of Akt1 and Akt2 signaling was diminished in human airway epithelia expressing F508del-CFTR compared with wild-type CFTR cells. In this study, the protein expressions of PI3K, p-AKTser473, and p-AKTThr308 were reduced at 12 h and 24 h after the H/R treatment and returned to normal at 48 h. Interestingly, it was discovered that the AKT activator and PI3K activator could reverse the H/R-induced cell apoptosis. The results indicated that overexpression of CFTR can significantly enhance the PI3K/AKT expression in the H/R-induced apoptosis. Our results implied that CFTR increased cell viability and inhibited cell apoptosis in the H/R-treated cells, and BA, GSK690693, and LY294002 significantly inhibited this effect. Altogether, based on our findings and previous studies, these results indicate that the inhibition of PI3K/AKT or the activation of NF-κB both impedes the protective effect of CFTR on H/R-induced apoptosis and showed that CFTR protects the Caco2 cells from H/R-induced apoptosis through the PI3K/AKT and NF-κB pathway.
Since the above experiments seemed to indicate that PI3K/AKT and NF-κB are involved in the same signaling pathway, we proceeded to test the relationship between PI3K/AKT and NF-κB activation. Recent studies have confirmed that the PI3K/AKT pathway reduces nuclear translocation of p65[27,28]. But some studies have shown that AKT overexpression increases NF-κB-dependent gene expression[2,29]. In our study, it was found that PI3K/AKT is upstream of NF-κB in H/R-induced response since PI3K inhibitor can abrogate the elevation of NF-κB P65 induced by H/R, whereas NF-κB inhibitor does not affect the activation of PI3K/AKT. And it was also found that activation of PI3K/AKT is sooner than that of NF-κB after H/R treatment was detected using Western blotting, supporting the notion that PI3K/AKT is the upstream of NF-κB. Additionally, the H/R-induced apoptosis can be reversed through PI3K/AKT or NF-κB inhibitor alone, with no additive effect if treated in combination, suggesting that PI3K/AKT and NF-κB are on the same pathway.
Although this study has achieved certain results, there are some limitations. First, we use an immortal human intestinal epithelial cell instead of primary cells, which limits the research’s authenticity and reliability to a certain extent. Second, the simulated hypoxic environment in vitro may be different from the real intestinal ischemia-reperfusion. However, the mechanism of ischemia-reperfusion affecting intestinal barrier permeability is complex, including the activity of inflammatory cytokines, endotoxemia of mitochondria or endoplasmic reticulum, and congenital immune dysfunction, which may become the mutual network of cellular pathways. Thus, further research is needed to clarify this mechanism.
In conclusion, our data demonstrate that CFTR is downregulated in H/R-treated Caco2 cells, and overexpression of CFTR protects Caco2 cells from H/R-induced apoptosis. Additionally, CFTR is involved in inhibiting H/R-induced apoptosis, and it inhibits apoptosis through PI3K/AKT/NF-κB signaling pathway. In all, this work suggests that overexpression of CFTR attenuates H/R-induced apoptosis through PI3K/AKT/NF-κB signaling pathway in H/R-treated Caco2 cells.
Intestinal ischemia/reperfusion (I/R) causes local injuries in the intestine and multiple organ dysfunction syndromes or even multiple organ failure in distant organs with a mortality rate ranging from 30%–90%. The underlying mechanisms are very complex. preventing intestinal apoptosis is one of the critical targets in treating patients with intestinal I/R injury.
Exploring the mechanism of apoptosis in intestinal I/R injury and preventing intestinal apoptosis is one of the critical targets in treating patients with intestinal I/R injury.
To apoptosis and its mechanism.
An intestinal I/R injury model was established in mice with superior mesenteric artery occlusion, and Caco2 cells were subjected to hypoxia/reoxygenation (H/R) for the simulation of I/R in vivo.
Cystic fibrosis transmembrane conductance regulator (CFTR) overexpression significantly increased the Caco2 cell viability and decreased cell apoptosis induced by the H/R. And CFTR overexpression could reverse the decreased PI3K/AKT expression induced by the I/R treatment in vivo or H/R treatment in vitro.
Overexpression of CFTR attenuates H/R-induced apoptosis through PI3K/AKT/NF-κB signaling pathway in H/R-treated Caco2 cells.
CFTR/PI3K/AKT/NF-κB signaling pathway is potential mechanism to protect intestinal cell from apoptosis in intestinal I/R injury and critical targets in treating patients with intestinal I/R injury.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: McDowell HR, Nardone G, Valery PC S-Editor: Fan JR L-Editor: A P-Editor: Li X
| 1. | Wu MB, Ma B, Zhang TX, Zhao K, Cui SM, He SC. Propofol improves intestinal ischemia-reperfusion injury in rats through NF-κB pathway. Eur Rev Med Pharmacol Sci. 2020;24:6463-6469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 2. | Wang Z, Sun R, Wang G, Chen Z, Li Y, Zhao Y, Liu D, Zhao H, Zhang F, Yao J, Tian X. SIRT3-mediated deacetylation of PRDX3 alleviates mitochondrial oxidative damage and apoptosis induced by intestinal ischemia/reperfusion injury. Redox Biol. 2020;28:101343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 159] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 3. | Gonzalez LM, Moeser AJ, Blikslager AT. Animal models of ischemia-reperfusion-induced intestinal injury: progress and promise for translational research. Am J Physiol Gastrointest Liver Physiol. 2015;308:G63-G75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 182] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 4. | Zhang S, Shrestha CL, Wisniewski BL, Pham H, Hou X, Li W, Dong Y, Kopp BT. Consequences of CRISPR-Cas9-Mediated CFTR Knockout in Human Macrophages. Front Immunol. 2020;11:1871. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 5. | Wu Z, Li J, Zhang Y, Hu L, Peng X. CFTR Regulates the Proliferation, Migration and Invasion of Cervical Cancer Cells by Inhibiting the NF-κB Signalling Pathway. Cancer Manag Res. 2020;12:4685-4697. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Zhao M, Zhang J, Huang W, Dong J, Guo J, U KP, Weng Z, Liu S, Chan HC, Feng H, Jiang X. CFTR promotes malignant glioma development via up-regulation of Akt/Bcl2-mediated anti-apoptosis pathway. J Cell Mol Med. 2020;24:7301-7312. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Xu X, Huang H, Yin X, Fang H, Shen X. Effect of lentivirus-mediated CFTR overexpression on oxidative stress injury and inflammatory response in the lung tissue of COPD mouse model. Biosci Rep. 2020;40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Liu J, Ou C, Zhu X, Tan C, Xiang X, He Y. Potential role of CFTR in bisphenol A-induced malignant transformation of prostate cells via mitochondrial apoptosis. Toxicol Ind Health. 2020;36:531-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Zhao P, Li F, Gao W, Wang J, Fu L, Chen Y, Huang M. Angiotensin1-7 protects cardiomyocytes from hypoxia/reoxygenation-induced oxidative stress by preventing ROS-associated mitochondrial dysfunction and activating the Akt signaling pathway. Acta Histochem. 2015;117:803-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Liu M, Liao H, Chen Y, Lin Z, Liu Y, Zhang X, Chan HC, Sun H. Treatment of human T-cell acute lymphoblastic leukemia cells with CFTR inhibitor CFTRinh-172. Leuk Res. 2019;86:106225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Li J, Liu S. LncRNA GAS5 suppresses inflammatory responses and apoptosis of alveolar epithelial cells by targeting miR-429/DUSP1. Exp Mol Pathol. 2020;113:104357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 12. | Dai Y, Mao Z, Han X, Xu Y, Xu L, Yin L, Qi Y, Peng J. MicroRNA-29b-3p reduces intestinal ischaemia/reperfusion injury via targeting of TNF receptor-associated factor 3. Br J Pharmacol. 2019;176:3264-3278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | Hu Y, Tao X, Han X, Xu L, Yin L, Sun H, Qi Y, Xu Y, Peng J. MicroRNA-351-5p aggravates intestinal ischaemia/reperfusion injury through the targeting of MAPK13 and Sirtuin-6. Br J Pharmacol. 2018;175:3594-3609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 14. | Zhang YP, Zhang Y, Xiao ZB, Zhang YB, Zhang J, Li ZQ, Zhu YB. CFTR prevents neuronal apoptosis following cerebral ischemia reperfusion via regulating mitochondrial oxidative stress. J Mol Med (Berl). 2018;96:611-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 15. | Zheng L, Han X, Hu Y, Zhao X, Yin L, Xu L, Qi Y, Xu Y, Liu K, Peng J. Dioscin ameliorates intestinal ischemia/reperfusion injury via adjusting miR-351-5p/MAPK13-mediated inflammation and apoptosis. Pharmacol Res. 2019;139:431-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 16. | Du J, Fan X, Yang B, Chen Y, Liu KX, Zhou J. Irisin pretreatment ameliorates intestinal ischemia/reperfusion injury in mice through activation of the Nrf2 pathway. Int Immunopharmacol. 2019;73:225-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 17. | Lin ZL, Yu WK, Tan SJ, Duan KP, Dong Y, Bai XW, Xu L, Li N. Protective effects of terminal ileostomy against bacterial translocation in a rat model of intestinal ischemia/reperfusion injury. World J Gastroenterol. 2014;20:17905-17913. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Schofield ZV, Wu MCL, Hansbro PM, Cooper MA, Woodruff TM. Acetate protects against intestinal ischemia-reperfusion injury independent of its cognate free fatty acid 2 receptor. FASEB J. 2020;34:10418-10430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Piao X, Liu B, Sui X, Li S, Niu W, Zhang Q, Shi X, Cai S, Fan Y. Picroside II Improves Severe Acute Pancreatitis-Induced Intestinal Barrier Injury by Inactivating Oxidative and Inflammatory TLR4-Dependent PI3K/AKT/NF-κB Signaling and Improving Gut Microbiota. Oxid Med Cell Longev. 2020;2020:3589497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 20. | Dong ZW, Chen J, Ruan YC, Zhou T, Chen Y, Tsang LL, Chan HC, Peng YZ. CFTR-regulated MAPK/NF-κB signaling in pulmonary inflammation in thermal inhalation injury. Sci Rep. 2015;5:15946. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 21. | Crites KS, Morin G, Orlando V, Patey N, Cantin C, Martel J, Brochiero E, Mailhot G. CFTR Knockdown induces proinflammatory changes in intestinal epithelial cells. J Inflamm (Lond). 2015;12:62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Liu K, Zhang X, Zhang JT, Tsang LL, Jiang X, Chan HC. Defective CFTR- β-catenin interaction promotes NF-κB nuclear translocation and intestinal inflammation in cystic fibrosis. Oncotarget. 2016;7:64030-64042. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 23. | Chen J, Chen Y, Yang Z, You B, Ruan YC, Peng Y. Epidermal CFTR Suppresses MAPK/NF-κB to Promote Cutaneous Wound Healing. Cell Physiol Biochem. 2016;39:2262-2274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 24. | Bodas M, Min T, Vij N. Critical role of CFTR-dependent lipid rafts in cigarette smoke-induced lung epithelial injury. Am J Physiol Lung Cell Mol Physiol. 2011;300:L811-L820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 78] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 25. | Liu B, Piao X, Niu W, Zhang Q, Ma C, Wu T, Gu Q, Cui T, Li S. Kuijieyuan Decoction Improved Intestinal Barrier Injury of Ulcerative Colitis by Affecting TLR4-Dependent PI3K/AKT/NF-κB Oxidative and Inflammatory Signaling and Gut Microbiota. Front Pharmacol. 2020;11:1036. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 122] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 26. | Xu H, Wang Y, Jurutka PW, Wu S, Chen Y, Cao C, Chen G, Tian B, Wang S, Cheng S. 16α-Hydroxytrametenolic Acid from Poria cocos Improves Intestinal Barrier Function Through the Glucocorticoid Receptor-Mediated PI3K/Akt/NF-κB Pathway. J Agric Food Chem. 2019;67:10871-10879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 27. | Radwan RR, Karam HM. Resveratrol attenuates intestinal injury in irradiated rats via PI3K/Akt/mTOR signaling pathway. Environ Toxicol. 2020;35:223-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 28. | Khedr RM, Ahmed AAE, Kamel R, Raafat EM. Sitagliptin attenuates intestinal ischemia/reperfusion injury via cAMP/PKA, PI3K/Akt pathway in a glucagon-like peptide 1 receptor-dependent manner. Life Sci. 2018;211:31-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 29. | Losa D, Köhler T, Bellec J, Dudez T, Crespin S, Bacchetta M, Boulanger P, Hong SS, Morel S, Nguyen TH, van Delden C, Chanson M. Pseudomonas aeruginosa-induced apoptosis in airway epithelial cells is mediated by gap junctional communication in a JNK-dependent manner. J Immunol. 2014;192:4804-4812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |