Published online Feb 14, 2022. doi: 10.3748/wjg.v28.i6.675
Peer-review started: October 1, 2021
First decision: November 7, 2021
Revised: November 23, 2021
Accepted: January 19, 2022
Article in press: January 19, 2022
Published online: February 14, 2022
Processing time: 131 Days and 5.1 Hours
Malignant lymphoma is a rare form of gallbladder malignancy. Most of these malignancies are diffuse large B-cell lymphomas or mucosa-associated lymphoid tissue-type lymphomas; however, Burkitt’s lymphoma of the gallbladder is extremely rare, and only two previous reports are available in the literature. Herein, we report a rare case of Burkitt’s lymphoma of the gallbladder mimicking gallbladder adenocarcinoma.
An 83-year-old man with no abdominal complaints was found to have a gallbladder tumor and periportal lymph node enlargement on computed tomography (CT) performed for hypertension screening. His laboratory data revealed slightly elevated serum levels of carcinoembryonic antigen and soluble interleukin 2 receptor. Imaging examinations revealed two irregular and contrast-enhanced masses extending into the gallbladder lumen, but these did not infiltrate the serosa. Moreover, a periportal lymph node had enlarged to 30 mm. Based on these findings, we diagnosed the patient as having gallbladder adenocarcinoma with lymph node metastasis, which was treated using bile duct resection with gallbladder bed resection and periportal lymph node dissection. However, the patient was finally diagnosed as having Burkitt’s lymphoma. Although the surgical margin was pathologically negative, recurrence was noted at the hepatic radical margin and superior pancreaticoduodenal lymph nodes on positron emission tomography/CT soon after discharge. Thus, he was referred to a hematologist and started receiving treatment with reduced-dose cyclophosphamide, doxorubicin, vincristine, and prednisone.
Burkitt’s lymphoma can occur in the gallbladder. Biopsy can be useful in cases with findings suggestive of gallbladder malignant lymphoma.
Core Tip: Malignant lymphoma is a rare form of gallbladder malignancy, and Burkitt’s lymphoma of the gallbladder is especially rare, with only two previous reports available in the literature. We report a case of gallbladder Burkitt’s lymphoma that was preoperatively indistinguishable from gallbladder carcinoma. Unfortunately, the patient had lymphoma recurrence immediately after the surgery because of delayed chemotherapy initiation owing to postoperative complications due to an extended surgery. Although accurate preoperative diagnosis of gallbladder malignant lymphoma is quite difficult, some findings are suggestive of gallbladder malignant lymphoma, and hence, biopsy is recommended in these cases.
- Citation: Hosoda K, Shimizu A, Kubota K, Notake T, Hayashi H, Yasukawa K, Umemura K, Kamachi A, Goto T, Tomida H, Yamazaki S, Narusawa Y, Asano N, Uehara T, Soejima Y. Gallbladder Burkitt’s lymphoma mimicking gallbladder cancer: A case report. World J Gastroenterol 2022; 28(6): 675-682
- URL: https://www.wjgnet.com/1007-9327/full/v28/i6/675.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i6.675
Malignant lymphoma of the gallbladder is extremely rare[1-4]. In almost all cases of this malignancy, patients are diagnosed as having gallbladder adenocarcinoma or cholecystitis at the time of surgery, and preoperative diagnosis is extremely difficult. Although several reports have documented malignant lymphomas of the gallbladder, most of these malignancies are diffuse large B-cell lymphomas and mucosa-associated lymphoid tissue-type lymphomas (MALTomas)[2,4,5], and only two reports have previously documented Burkitt’s lymphoma of the gallbladder[6,7]. Herein, we report the case of a patient with Burkitt’s lymphoma of the gallbladder mimicking gallbladder adenocarcinoma.
An 83-year-old man with no abdominal complaints was found to have a gallbladder tumor along with periportal lymph node enlargement and was admitted to our institution for further investigation.
The tumor was detected during contrast-enhanced computed tomography (CT) performed for a detailed examination of hypertension.
The patient had a history of cerebral artery stenosis and paroxysmal atrial fibrillation.
No personal and family history.
Abdominal examination revealed no palpable mass or tenderness.
Laboratory examinations performed upon admission revealed mild to moderate renal dysfunction (creatinine: 1.21 mg/dL) and slightly elevated levels of serum carcinoembryonic antigen and serum soluble interleukin 2 receptor (6.1 ng/mL and 635 IU/mL, respectively). Other laboratory data were within normal limits.
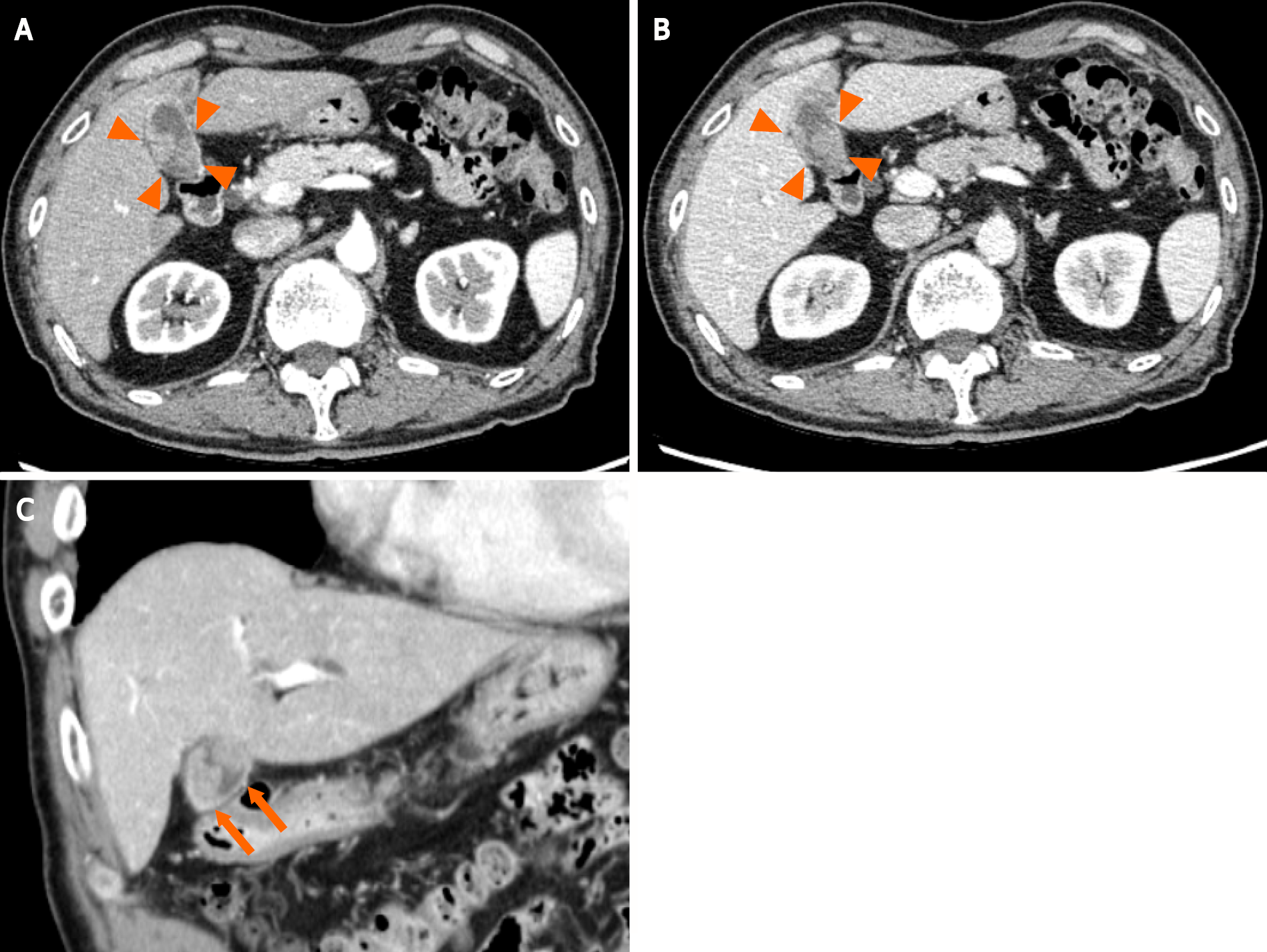
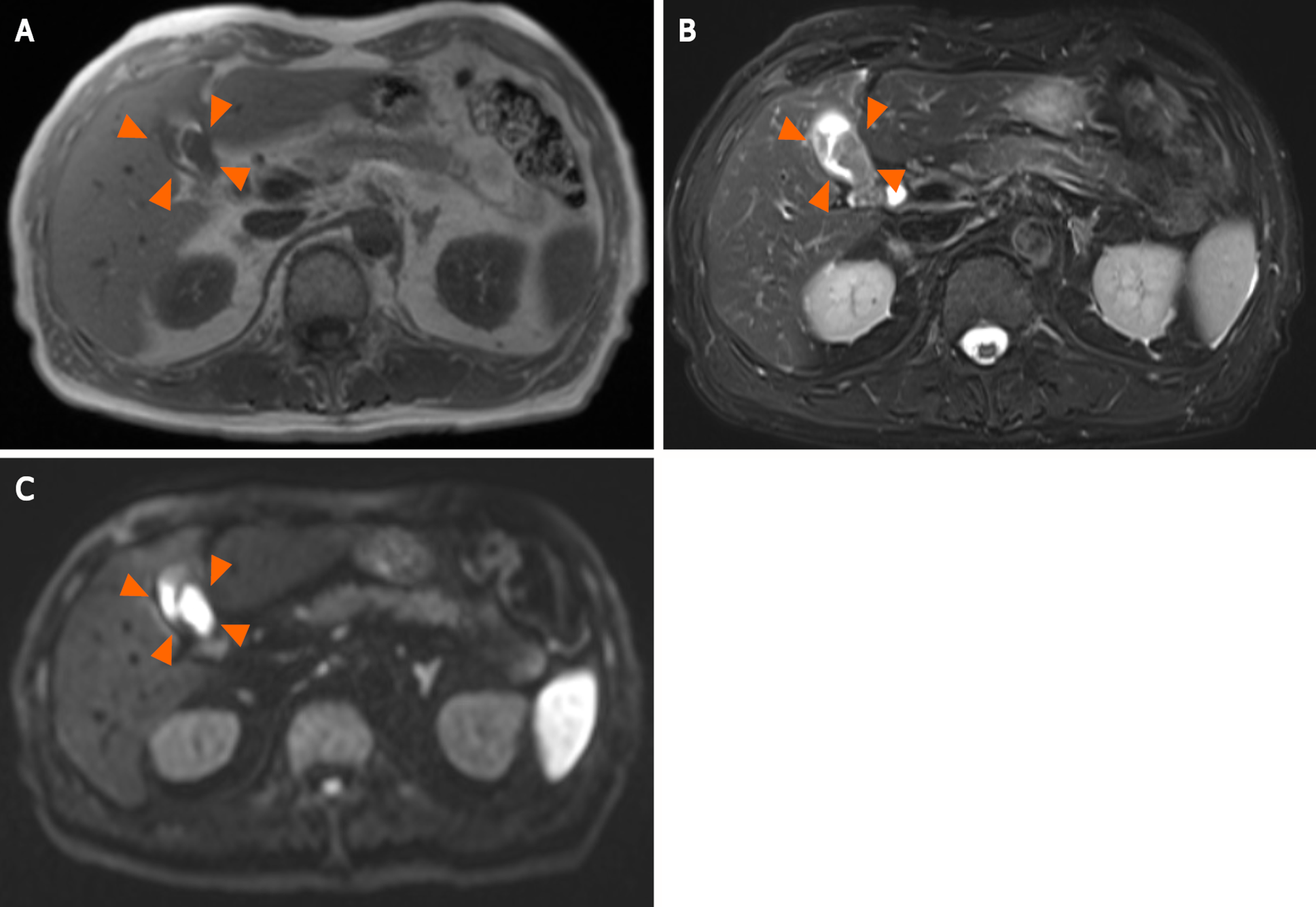
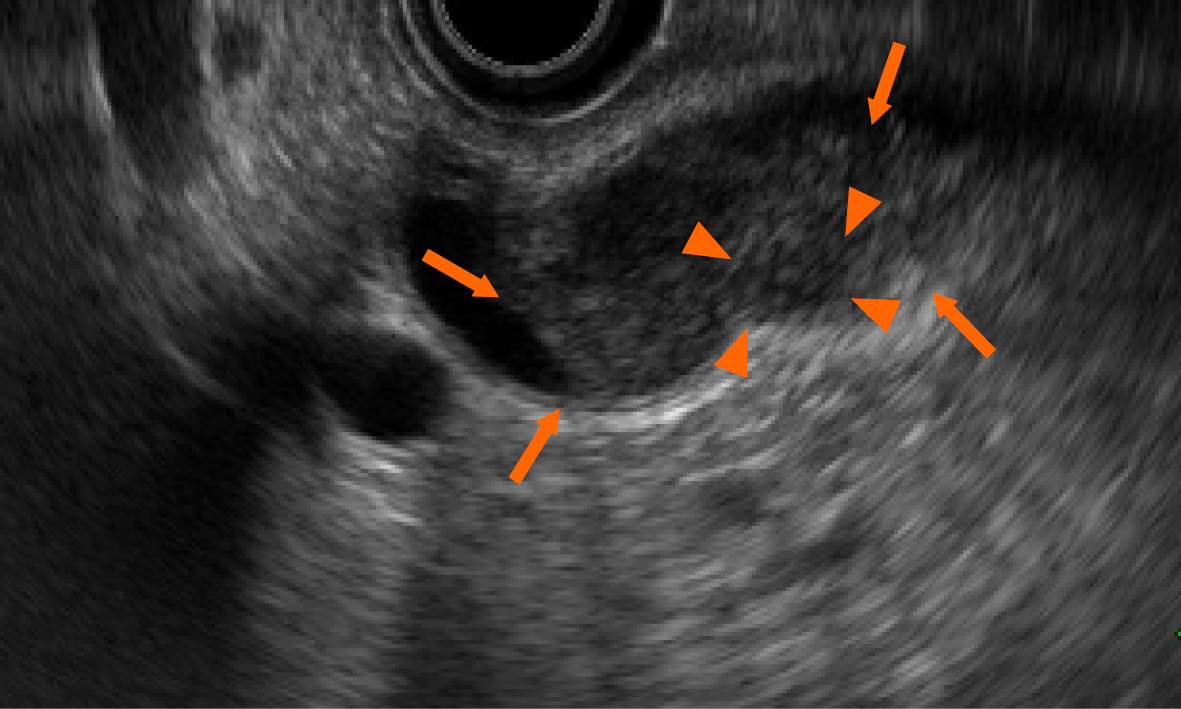
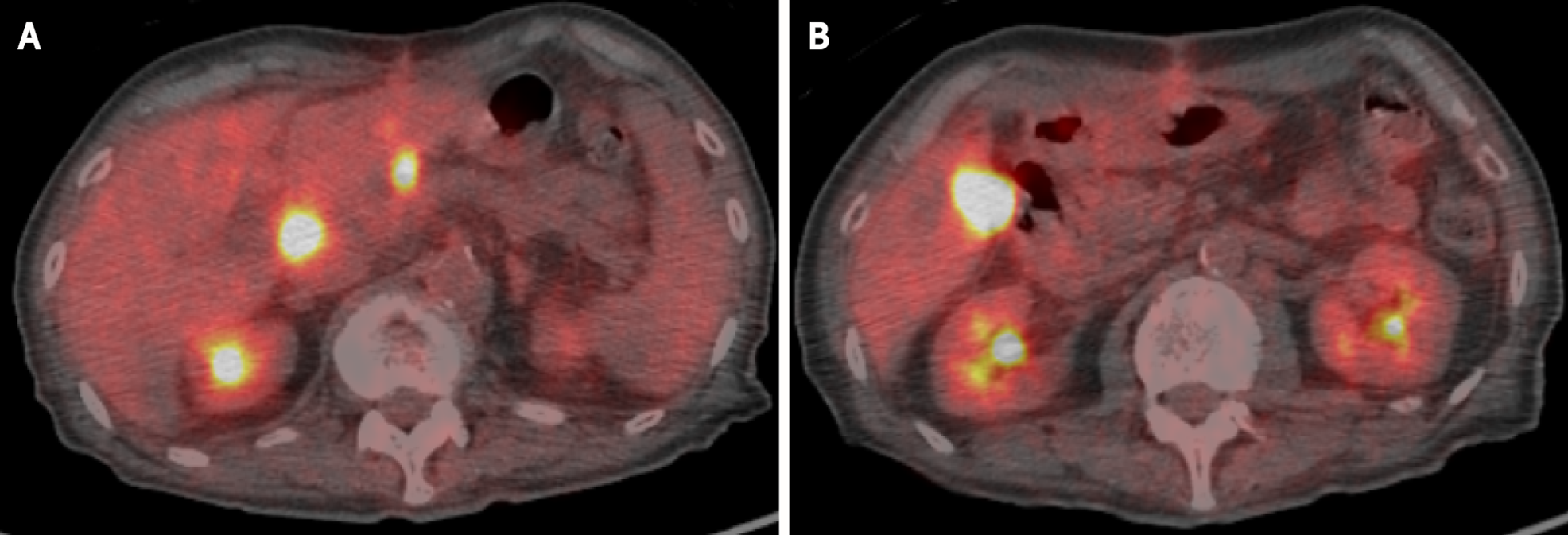
A contrast-enhanced abdominal CT scan revealed two irregular and highly contrast-enhanced masses at the neck and body of the gallbladder as well as periportal lymph node enlargement, measuring 30 mm × 20 mm in diameter and consistent with gallbladder cancer lymph node metastasis (Figure 1). Magnetic resonance imaging revealed that the tumor signal was hypointense on T1-weighted imaging and hyperintense on T2-weighted and diffusion-weighted imaging (Figure 2). Positron emission tomography (PET) revealed increased 18F-fluorodeoxyglucose uptake in the tumor (Figure 3). Endoscopic ultrasonography (EUS) showed a heterogeneous echoic mass extending into the lumen, but it did not infiltrate the serosa (Figure 4).
The final diagnosis was gallbladder adenocarcinoma with lymph node metastasis.
On the basis of these findings, the patient underwent bile duct resection with gallbladder bed resection and periportal lymph node dissection. The surgical findings revealed the gallbladder tumor was relatively softer than ordinary gallbladder cancers. The swollen lymph node was firm but did not invade the portal vein. However, the patient developed severe aspiration pneumonia and bile leakage after the surgery, which were treated conservatively. The patient was discharged 2 mo after the surgery.
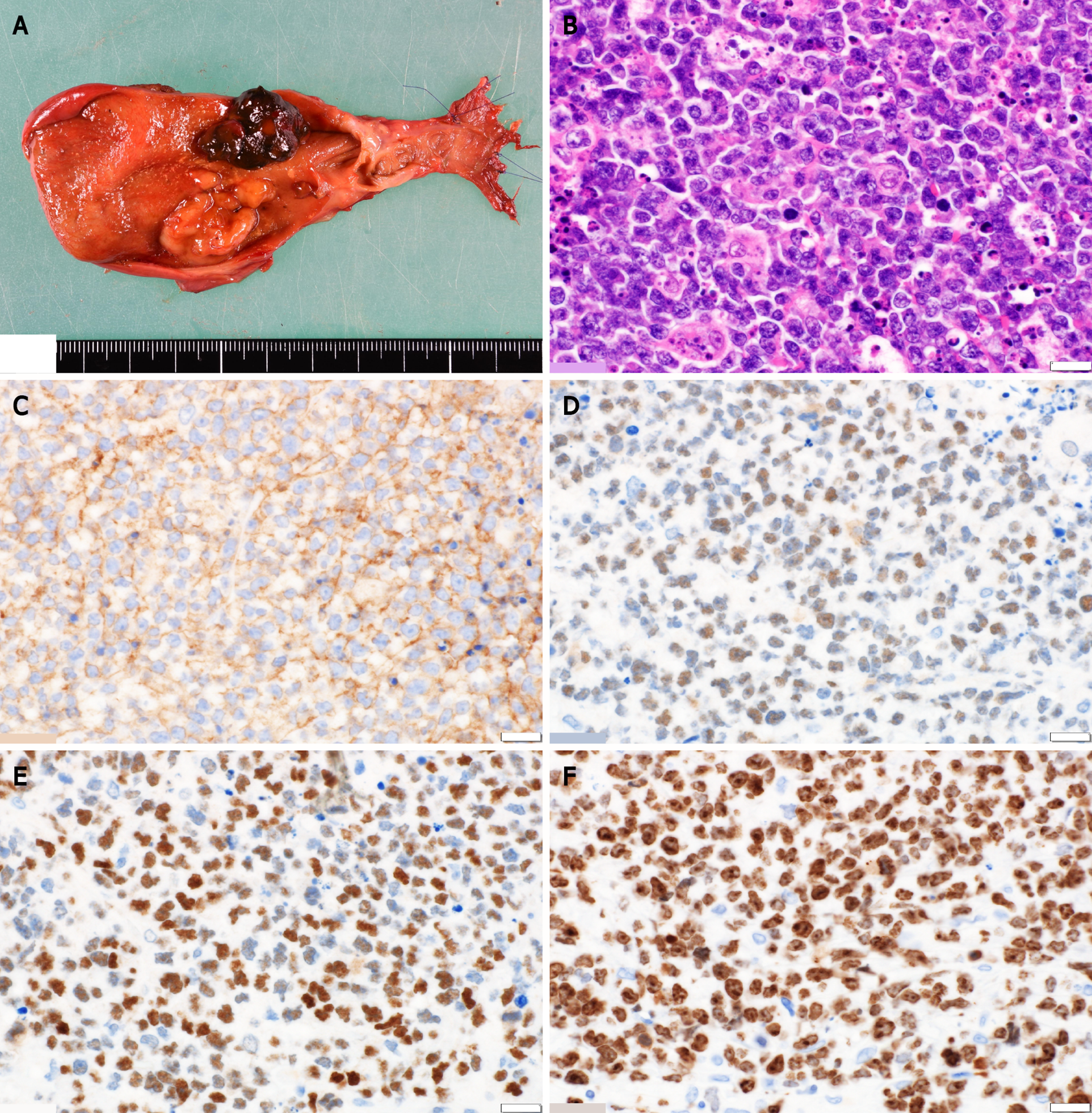
Histologic examination revealed periportal lymphadenopathy and two tumors at the neck and body of the gallbladder, measuring 27 mm × 20 mm and 20 mm × 18 mm in diameter, respectively. Histological findings also showed monotonous lymphoid cells with hemophagocytosis by macrophages. Immunohistochemical staining for markers showed the presence of CD10, BCL6, and c-Myc and the absence of BCL2. The Ki-67 index was > 80% (Figure 5). Therefore, the patient was finally diagnosed as having Burkitt’s lymphoma. Although the surgical margin was pathologically negative, recurrence was noted at the hepatic radical margin and superior pancreaticoduodenal lymph nodes on PET-CT immediately after discharge. Thus, he was referred to a hematologist and started receiving treatment with reduced-dose cyclophosphamide, doxorubicin, vincristine, and prednisone.
Malignant lymphoma of the gallbladder is a rare form of gallbladder malignancy, which accounts for 0.1%-0.2% of all gallbladder cancers[1-3]. In previous reports, most of these malignancies were documented to be diffuse large B-cell lymphomas and MALTomas[2,4], and only two reports had documented Burkitt’s lymphoma of the gallbladder[6,7]. Compared to previous cases, the present case yielded some interesting clinical and imaging findings.
First, this is potentially the first reported case of “primary” gallbladder Burkitt’s lymphoma. According to the diagnostic criteria of primary gastrointestinal lymphoma (Table 1) defined by Dawson et al[8] and Lewin et al[9], the previous two cases were diagnosed as “secondary” gallbladder Burkitt’s lymphoma because they included extra-gallbladder lesions, such as duodenal, hepatic, or central nervous system lesions. In contrast, in the present case, the tumor was localized in the gallbladder and a periportal lymph node. Although no gastrointestinal symptoms were observed because the primary site was the gallbladder, other criteria were fulfilled. Therefore, the patient was diagnosed as having “primary” gallbladder Burkitt’s lymphoma, and the case was considered novel.
| Ref. | Diagnostic criteria |
| Dawson et al[8] | Absence of palpable superficial lymphadenopathy |
| Absence of obvious enlargement of mediastinal lymph nodes | |
| Normal level of total and differential white blood cell counts | |
| The bowel lesion predominating and the only lymph node obviously affected being those in its immediate neighborhood | |
| Absence of tumor in the liver and spleen | |
| Lewin et al[9] | Exhibiting gastroinetstinal symptoms or predominant lesions in the gastrointestinal tract |
Second, gallbladder Burkitt’s lymphoma can present as a localized disease that mimics gallbladder cancer. The imaging features of malignant lymphoma were reported by Ono et al[3], who reported that high-grade malignant lymphomas showed solid and bulky masses or irregular wall thickening. In addition, because Burkitt’s lymphoma is a highly aggressive and rapidly progressive disease, some extranodal sites are generally involved at the time of diagnosis[10] and tumor localization around the primary lesion is rare[11]. In this case, the malignancy was localized in the body of the gallbladder and a periportal lymph node. Since these findings were consistent with the imaging findings of gallbladder adenocarcinoma, we could not confirm a preoperative diagnosis of malignant lymphoma.
Unfortunately, the patient had lymphoma recurrence 2 mo after the surgery because the introduction of chemotherapy had to be delayed owing to postoperative complications. Burkitt’s lymphoma is a highly aggressive disease, but it is highly sensitive to chemotherapy. Therefore, chemotherapy has the highest priority in the treatment of Burkitt’s lymphoma[10], and we should have introduced chemotherapy as soon as possible after the surgery. If we had been aware of the possibility of gallbladder malignant lymphoma, we could have avoided the extended procedure and could have initiated chemotherapy at the appropriate time.
Although the accurate preoperative diagnosis of gallbladder malignant lymphoma is quite difficult[2,12], some previous reports[3,12,13] have suggested the possibility of a precise preoperative diagnosis based on imaging findings. Specifically, Ono et al[3] showed that the signal intensity of the gallbladder wall on T2-weighted imaging is more hypointense in malignant lymphoma than in carcinoma. In addition, Kato et al[12] reported the usefulness of an internal partially low echo in distinguishing malignant lymphoma from carcinoma. On a retrospective review of the present case, although no obvious differences were observed in the intensity of T2-weighted imaging when compared to that of gallbladder cancers, EUS revealed an internal partially low echo of the tumor. Furthermore, in this case, a discrepancy existed in that no serosal invasion was observed despite the size of the tumor and presence of lymphadenopathy. We think this might be a characteristic finding that distinguishes gallbladder malignant lymphoma from carcinoma.
Nevertheless, a biopsy examination seems the best diagnostic technique in the present case, considering the possibility of malignant lymphoma, and hence, biopsy should be planned for patients with the above imaging findings.
Burkitt’s lymphoma can occur in the gallbladder. Therefore, this disease should be considered in the differential diagnosis of a gallbladder tumor, and biopsy can be useful in facilitating the early introduction of chemotherapy in cases with suggestive imaging findings.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gupta P, Zhu CF S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Yasuma T, Yanaka M. Primary sarcoma of the gallbladder--report of three cases. Acta Pathol Jpn. 1971;21:285-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Jelic TM, Barreta TM, Yu M, Frame JN, Estallila OC, Mellen PF, Newman SS, Chang HH. Primary, extranodal, follicular non-Hodgkin lymphoma of the gallbladder: case report and a review of the literature. Leuk Lymphoma. 2004;45:381-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Ono A, Tanoue S, Yamada Y, Takaji Y, Okada F, Matsumoto S, Mori H. Primary malignant lymphoma of the gallbladder: a case report and literature review. Br J Radiol. 2009;82:e15-e19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Ayub A, Rehmani S, Al-Ayoubi AM, Lewis E, Santana-Rodríguez N, Raad W, Bhora F, Kim G. Primary Non-Hodgkin's Lymphoma of the Gallbladder: A Population-based Analysis. Anticancer Res. 2017;37:2581-2586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Mani H, Climent F, Colomo L, Pittaluga S, Raffeld M, Jaffe ES. Gall bladder and extrahepatic bile duct lymphomas: clinicopathological observations and biological implications. Am J Surg Pathol. 2010;34:1277-1286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | Doherty B, Palmer W, Cvinar J, Sadek N. A Rare Case of Systemic Adult Burkitt Lymphoma Presenting as Acute Acalculous Cholecystitis. ACG Case Rep J. 2019;6:e00048. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Repine TB, DeArmond G, López JD. Unusual sites of metastatic malignancy: case 2. Burkitt's lymphoma involving the gallbladder. J Clin Oncol. 2004;22:5014-5015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Dawson IM, Cornes JS, Morson BC. Primary malignant lymphoid tumours of the intestinal tract. Report of 37 cases with a study of factors influencing prognosis. Br J Surg. 1961;49:80-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 525] [Cited by in RCA: 469] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 9. | Lewin KJ, Ranchod M, Dorfman RF. Lymphomas of the gastrointestinal tract: a study of 117 cases presenting with gastrointestinal disease. Cancer. 1978;42:693-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 10. | Crombie J, LaCasce A. The treatment of Burkitt lymphoma in adults. Blood. 2021;137:743-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 61] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 11. | Čubranić A, Golčić M, Fučkar-Čupić D, Brozović B, Gajski D, Brumini I. BURKITT LYMPHOMA IN GASTROINTESTINAL TRACT: A REPORT OF TWO CASES. Acta Clin Croat. 2019;58:386-390. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Kato H, Naganuma T, Iizawa Y, Kitagawa M, Tanaka M, Isaji S. Primary non-Hodgkin's lymphoma of the gallbladder diagnosed by laparoscopic cholecystectomy. J Hepatobiliary Pancreat Surg. 2008;15:659-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Gupta P, Marodia Y, Bansal A, Kalra N, Kumar-M P, Sharma V, Dutta U, Sandhu MS. Imaging-based algorithmic approach to gallbladder wall thickening. World J Gastroenterol. 2020;26:6163-6181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 43] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (3)] |