Published online Feb 7, 2022. doi: 10.3748/wjg.v28.i5.588
Peer-review started: March 4, 2021
First decision: May 1, 2021
Revised: May 3, 2021
Accepted: December 28, 2021
Article in press: December 28, 2021
Published online: February 7, 2022
Processing time: 327 Days and 0.1 Hours
Infected walled-off necrosis is a potentially life-threatening complication of necrotizing pancreatitis. While some patients can be treated by drainage alone, many patients also need evacuation of the infected debris. Central necroses in relation to the pancreatic bed are easily reached via an endoscopic transluminal approach, whereas necroses that involve the paracolic gutters and the pelvis are most efficiently treated via a percutaneous approach. Large and complex necroses may need a combination of the two methods.
Transluminal and percutaneous drainage followed by simultaneous endoscopic and modified video-assisted retroperitoneal debridement was carried out in two patients with very large (32-38 cm), infected walled-off necroses using a laparoscopic access platform. After 34 d and 86 d and a total of 9 and 14 procedures, respectively, complete regression of the walled-off necroses was achieved. The laparoscopic access platform improved both access to the cavities as well as the overview. Simultaneous transluminal and percutaneous necrosectomy are feasible with the laparoscopic access platform serving as a useful adjunctive.
This approach may be necessary to control infection and achieve regression in some patients with complex collections.
Core Tip: Infected walled-off necrosis is a potentially life-threatening complication of necrotizing pancreatitis. In cases with large or complex walled-off necrosis, treatment combining endoscopic, transluminal and percutaneous video-assisted retroperitoneal debridement may be needed. We report on two patients who underwent a combination of endoscopic and percutaneous drainage and necrosectomy for their large, infected walled-off necroses. Furthermore, we introduce a laparoscopic access platform as a useful adjunctive to endoscopic necrosectomy and video-assisted retroperitoneal debridement.
- Citation: Lindgaard L, Lauritsen ML, Novovic S, Hansen EF, Karstensen JG, Schmidt PN. Simultaneous endoscopic and video-assisted retroperitoneal debridement in walled-off pancreatic necrosis using a laparoscopic access platform: Two case reports. World J Gastroenterol 2022; 28(5): 588-593
- URL: https://www.wjgnet.com/1007-9327/full/v28/i5/588.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i5.588
Infected walled-off necrosis (WON) is a potentially life-threatening complication of necrotizing pancreatitis. Traditionally, such patients were treated via open surgery, but during the last decade an endoscopic or surgical step-up approach using minimally invasive techniques has become the treatment of choice[1-5].
Whereas some patients can be treated by drainage alone, many patients also need evacuation of the infected debris. In such cases, it is our experience that central necroses in relation to the pancreatic bed are most easily reached by endoscopic, transluminal drainage followed by endoscopic necrosectomy (EN), whereas necroses that involve the paracolic gutters and the pelvis are more effectively treated with percutaneous drainage and video-assisted retroperitoneal debridement (VARD).
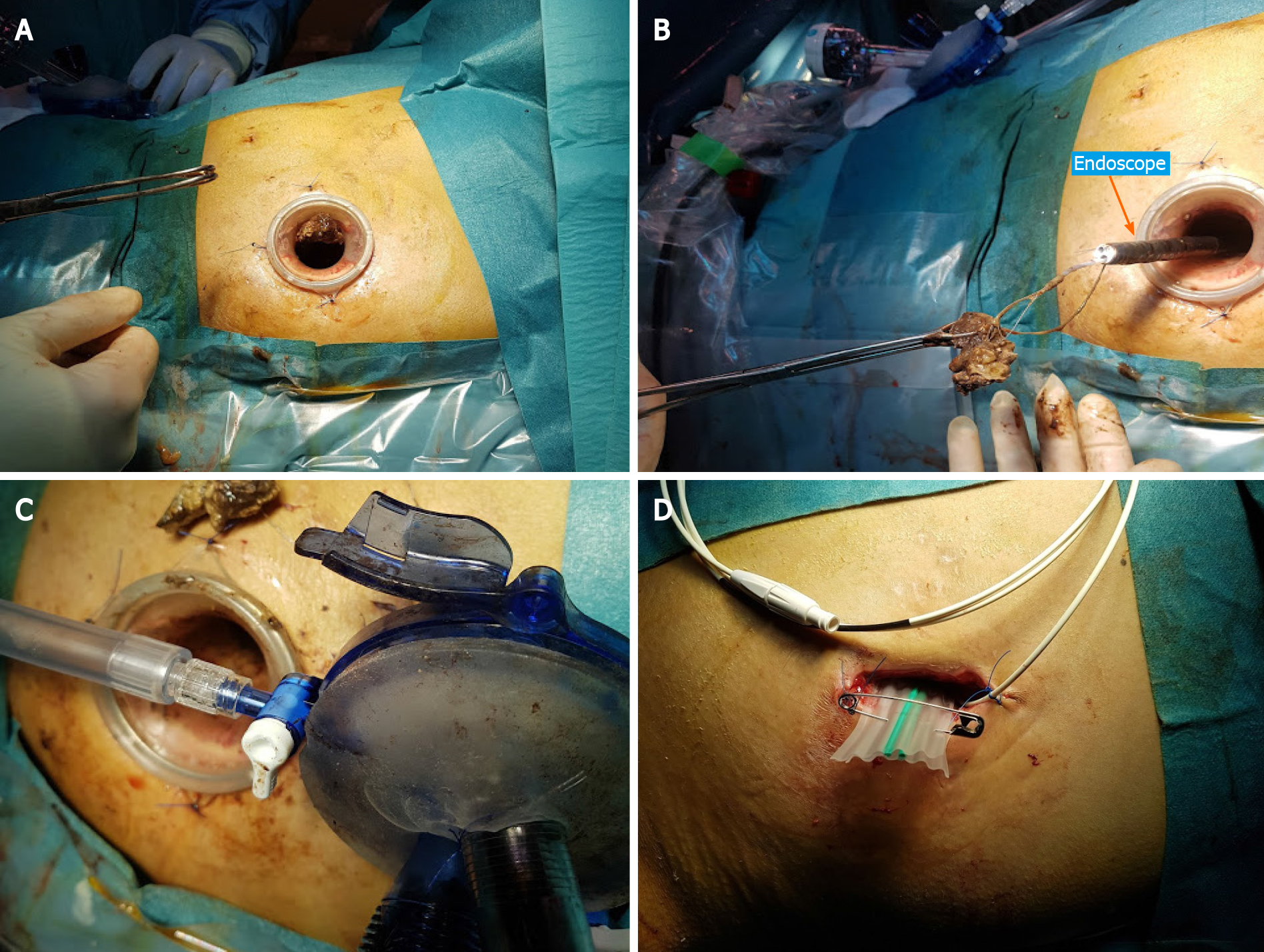
We report on two patients who needed a combination of endoscopic and percutaneous drainage and necrosectomy for their large, infected WONs. Furthermore, we introduce a laparoscopic access platform (Figures 1 and 2) as a useful adjunctive to EN and VARD.
Case 1: A 36-year-old male with a history of proctocolectomy and J-pouch due to ulcerative colitis was admitted to a local hospital because of jaundice.
Case 2: An 18-year-old boy was admitted to another hospital with severe necrotizing pancreatitis of unknown etiology.
Case 1: Magnetic resonance imaging raised suspicion of a cholangiocarcinoma in the liver hilum, a diagnosis that was subsequently confirmed. An endoscopic retrograde cholangiopancreatography revealed multiple intra- and extrahepatic bile duct strictures consistent with primary sclerosing cholangitis but failed to relieve the obstruction. Subsequent percutaneous transhepatic biliary drainage was carried out. After the endoscopic retrograde cholangiopancreatography, the patient developed post-endoscopic retrograde cholangiopancreatography pancreatitis, severe sepsis, and multiple organ failure and was admitted to the intensive care unit (ICU).
Case 2: On day 2, he was referred to the ICU with respiratory and circulatory failure. On day 3, he developed intra-abdominal hypertension and renal failure with the need for dialysis.
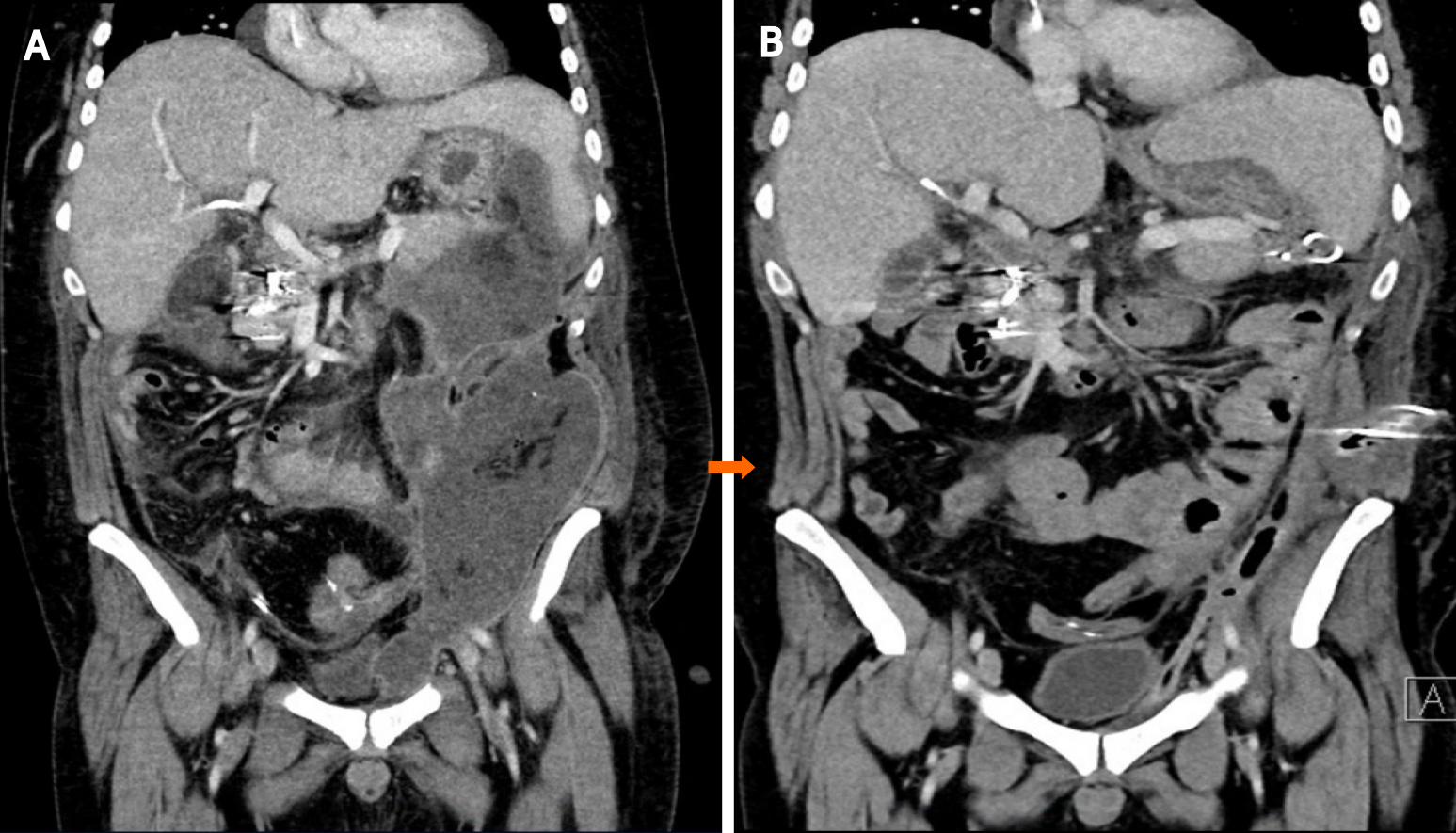
Case 1: After 6 wk, which included severe episodes of gastrointestinal bleeding that needed coiling and laparotomy with creation of an ileostomy, he was referred to our hospital for endoscopic drainage of a large (12 cm × 14 cm × 38 cm), infected, left-sided WON extending from the spleen down through the left paracolic gutter into the left groin (Figure 3A).
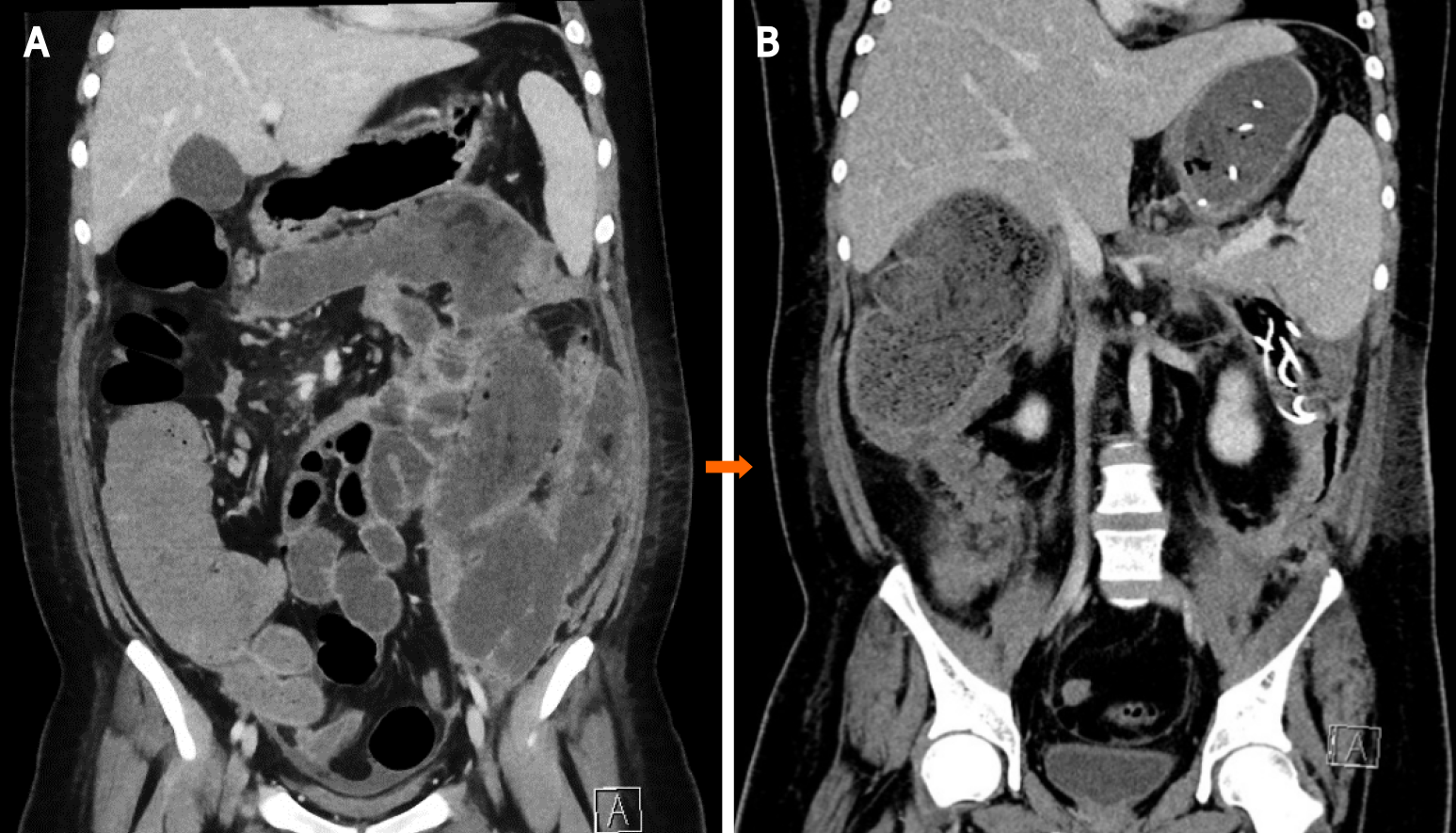
Case 2: On day 43, he was referred to the ICU at our hospital with septicemia and a large (16 cm × 24 cm × 32 cm), infected, left-sided WON extending from the pancreatic bed into the pelvis (Figure 4A).
Case 1: Between days 57 and 143, the patient underwent one endoscopic transluminal drainage, four EN, two VARD, and seven combined EN/VARD procedures.
Case 2: The same day, VARD was performed. Five days later, after only one VARD and one EN session, he was discharged from the ICU. The patient underwent a total of one endoscopic transluminal drainage, four VARD, two EN and two combined VARD/EN procedures, with the last procedure occurring on day 77.
Case 1: There was complete regression of the large WON (Figure 3B).
Case 2: There was complete regression of the large WON (Figure 4B).
In this paper, we describe 2 patients with necrotizing pancreatitis who needed treatment with a combination of EN and VARD. Both patients were referred to our hospital with signs of sepsis due to very large, infected WONs. We chose to combine two minimally invasive techniques to control the infection as quickly as possible in order to accelerate the treatment course.
EN is ideal for treating central WONs, whereas VARD is especially suitable in the case of lateral collections extending into the paracolic gutters and the pelvis. Even though flexible endoscopes can reach remote parts of the retroperitoneum, an isolated endoscopic approach can prove more time-consuming and delay evacuation of large collections as compared to a combined approach. Furthermore, large fluid collections may become compartmentalized over the course of treatment, creating isolated portions of the WON that can no longer be reached via the transluminal route. A successful combination of EN and VARD has been described elsewhere[6,7].
VARD has been thoroughly described in the literature[8,9]. However, use of a laparoscopic platform has not to our knowledge been documented. With the GelSeal cap closed and CO2 insufflation through the platform, the large cavity could be expanded during the procedure, thus making debridement easier. During transgastric necrosectomy, debris was removed through the access channel of the platform by the surgeon or endoscopy assistants, reducing the procedure time. Finally, the platform facilitated debridement via the percutaneous route using the flexible endoscope. The success of the method needs to be investigated in prospective studies evaluating the risk of recurrence and fistula formation as well as matters relating to costs of the technique.
We conclude that simultaneous transluminal and percutaneous necrosectomy is practical and hypothesize that it may accelerate treatment in cases of complex WONs due to acute pancreatitis. Furthermore, a laparoscopic access platform is a useful adjunctive to the procedure.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Denmark
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: De Vincentis F, Liu C S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
| 1. | van Santvoort HC, Besselink MG, Bakker OJ, Hofker HS, Boermeester MA, Dejong CH, van Goor H, Schaapherder AF, van Eijck CH, Bollen TL, van Ramshorst B, Nieuwenhuijs VB, Timmer R, Laméris JS, Kruyt PM, Manusama ER, van der Harst E, van der Schelling GP, Karsten T, Hesselink EJ, van Laarhoven CJ, Rosman C, Bosscha K, de Wit RJ, Houdijk AP, van Leeuwen MS, Buskens E, Gooszen HG; Dutch Pancreatitis Study Group. A step-up approach or open necrosectomy for necrotizing pancreatitis. N Engl J Med. 2010;362:1491-1502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1038] [Cited by in RCA: 1034] [Article Influence: 68.9] [Reference Citation Analysis (0)] |
| 2. | Horvath K, Freeny P, Escallon J, Heagerty P, Comstock B, Glickerman DJ, Bulger E, Sinanan M, Langdale L, Kolokythas O, Andrews RT. Safety and efficacy of video-assisted retroperitoneal debridement for infected pancreatic collections: a multicenter, prospective, single-arm phase 2 study. Arch Surg. 2010;145:817-825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 142] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 3. | Bakker OJ, van Santvoort HC, van Brunschot S, Geskus RB, Besselink MG, Bollen TL, van Eijck CH, Fockens P, Hazebroek EJ, Nijmeijer RM, Poley JW, van Ramshorst B, Vleggaar FP, Boermeester MA, Gooszen HG, Weusten BL, Timmer R; Dutch Pancreatitis Study Group. Endoscopic transgastric vs surgical necrosectomy for infected necrotizing pancreatitis: a randomized trial. JAMA. 2012;307:1053-1061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 506] [Cited by in RCA: 496] [Article Influence: 38.2] [Reference Citation Analysis (0)] |
| 4. | van Brunschot S, van Grinsven J, van Santvoort HC, Bakker OJ, Besselink MG, Boermeester MA, Bollen TL, Bosscha K, Bouwense SA, Bruno MJ, Cappendijk VC, Consten EC, Dejong CH, van Eijck CH, Erkelens WG, van Goor H, van Grevenstein WMU, Haveman JW, Hofker SH, Jansen JM, Laméris JS, van Lienden KP, Meijssen MA, Mulder CJ, Nieuwenhuijs VB, Poley JW, Quispel R, de Ridder RJ, Römkens TE, Scheepers JJ, Schepers NJ, Schwartz MP, Seerden T, Spanier BWM, Straathof JWA, Strijker M, Timmer R, Venneman NG, Vleggaar FP, Voermans RP, Witteman BJ, Gooszen HG, Dijkgraaf MG, Fockens P; Dutch Pancreatitis Study Group. Endoscopic or surgical step-up approach for infected necrotising pancreatitis: a multicentre randomised trial. Lancet. 2018;391:51-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 366] [Cited by in RCA: 473] [Article Influence: 67.6] [Reference Citation Analysis (0)] |
| 5. | Schmidt PN, Novovic S, Roug S, Feldager E. Endoscopic, transmural drainage and necrosectomy for walled-off pancreatic and peripancreatic necrosis is associated with low mortality--a single-center experience. Scand J Gastroenterol. 2015;50:611-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Fagenholz PJ, Thabet A, Mueller PR, Forcione DG. Combined endoscopic trangastric drainage and video assisted retroperitoneal pancreatic debridement - The best of both worlds for extensive pancreatic necrosis with enteric fistulae. Pancreatology. 2016;16:788-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Sorrentino L, Chiara O, Mutignani M, Sammartano F, Brioschi P, Cimbanassi S. Combined totally mini-invasive approach in necrotizing pancreatitis: a case report and systematic literature review. World J Emerg Surg. 2017;12:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Olthof PB, Schnitzbauer AA, Schadde E. The HPB controversy of the decade: 2007-2017 - Ten years of ALPPS. Eur J Surg Oncol. 2018;44:1624-1627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | van Brunschot S, Besselink MG, Bakker OJ, Boermeester MA, Gooszen HG, Horvath KD, van Santvoort HC. Video-Assisted Retroperitoneal Debridement (VARD) of Infected Necrotizing Pancreatitis: An Update. Curr Surg Reports. 2013;1:121. [RCA] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |