Published online Sep 7, 2022. doi: 10.3748/wjg.v28.i33.4920
Peer-review started: March 17, 2022
First decision: April 10, 2022
Revised: April 13, 2022
Accepted: August 16, 2022
Article in press: August 16, 2022
Published online: September 7, 2022
Processing time: 167 Days and 7.7 Hours
Ectopic bronchogenic cysts are a type of congenital cystic tumor that are extremely difficult to diagnose and can be ectopically located in various organs, with the possibility of malignant transformation. Here we report a case of an ectopic bronchogenic cyst in the liver initially misdiagnosed as a gallbladder diverticulum.
The patient was a middle-aged woman whose chief complaint was intermittent pain in the upper abdomen. Imaging examination revealed a cystic space in the left inner lobe of the liver. She was admitted to our hospital for treatment. Based on abdominal examination and imaging findings, the initial diagnosis was gallbladder diverticulum with cholestasis combined with chronic cholecystitis. However, following intraoperative observations and postoperative pathologic assessment, the diagnosis was revised to ectopic bronchogenic cyst of the liver.
Radiologists, hepatobiliary and pancreatic surgeons, gastrointestinal surgeons, urologists, and even neurosurgeons should be aware and consider a possible diagnosis of ectopic bronchogenic cysts, especially when other types of cyst, cystadenoma, and other diseases are excluded. The disease and its complications should be detected and correctly diagnosed and treated as early as possible in order to avoid adverse outcomes.
Core Tip: Ectopic bronchogenic cysts are the rarest type of bronchogenic cyst and can be ectopically located in different organs. When various specialists diagnose cysts, cystadenomas, and other diseases, the possibility of ectopic bronchogenic cyst should not be discounted. We report a case of an ectopic bronchogenic cyst in the liver that was misdiagnosed as gallbladder diverticulum. Early surgical intervention is the most effective strategy to prevent disease transformation.
- Citation: Dong CJ, Yang RM, Wang QL, Wu QY, Yang DJ, Kong DC, Zhang P. Ectopic bronchogenic cyst of liver misdiagnosed as gallbladder diverticulum: A case report. World J Gastroenterol 2022; 28(33): 4920-4925
- URL: https://www.wjgnet.com/1007-9327/full/v28/i33/4920.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i33.4920
A bronchogenic cyst is a rare congenital cystic tumor that can generally be classified as one of three types—namely, intrapulmonary, mediastinal, and heterotopic (the most rare)[1-3]. Bronchogenic cysts often develop ectopically in the neck, retroperitoneum, and stomach wall; very few cases of ectopic cysts in the liver have been reported[4]. Ectopic bronchogenic cysts often have no specific clinical manifestations, imaging characteristics, or changes in laboratory indices, making preoperative diagnosis extremely difficult. The cysts are typically discovered during routine physical examinations or because of complications resulting from the compression of surrounding organs or tissues. Here we report a case of an ectopic bronchogenic cyst in the liver that was preoperatively diagnosed as cholecystic diver
A 40-year-old woman presented with intermittent upper abdominal pain.
Physical examination at the primary hospital revealed a space-occupying lesion above the gallbladder in the left inner lobe of the liver that was complicated by chronic cholecystitis. The patient was transferred to our hospital for further treatment.
The patient was physically fit.
Her family history was noncontributory.
A physical examination of the abdomen showed no muscle tension, tenderness, or rebound pain. No abdominal mass was detected; the liver was not touched under the ribs, and the Murphy sign was positive.
Laboratory examinations including routine blood and blood coagulation, liver function, biochemistry, tumor markers, and infection markers revealed no abnormalities.
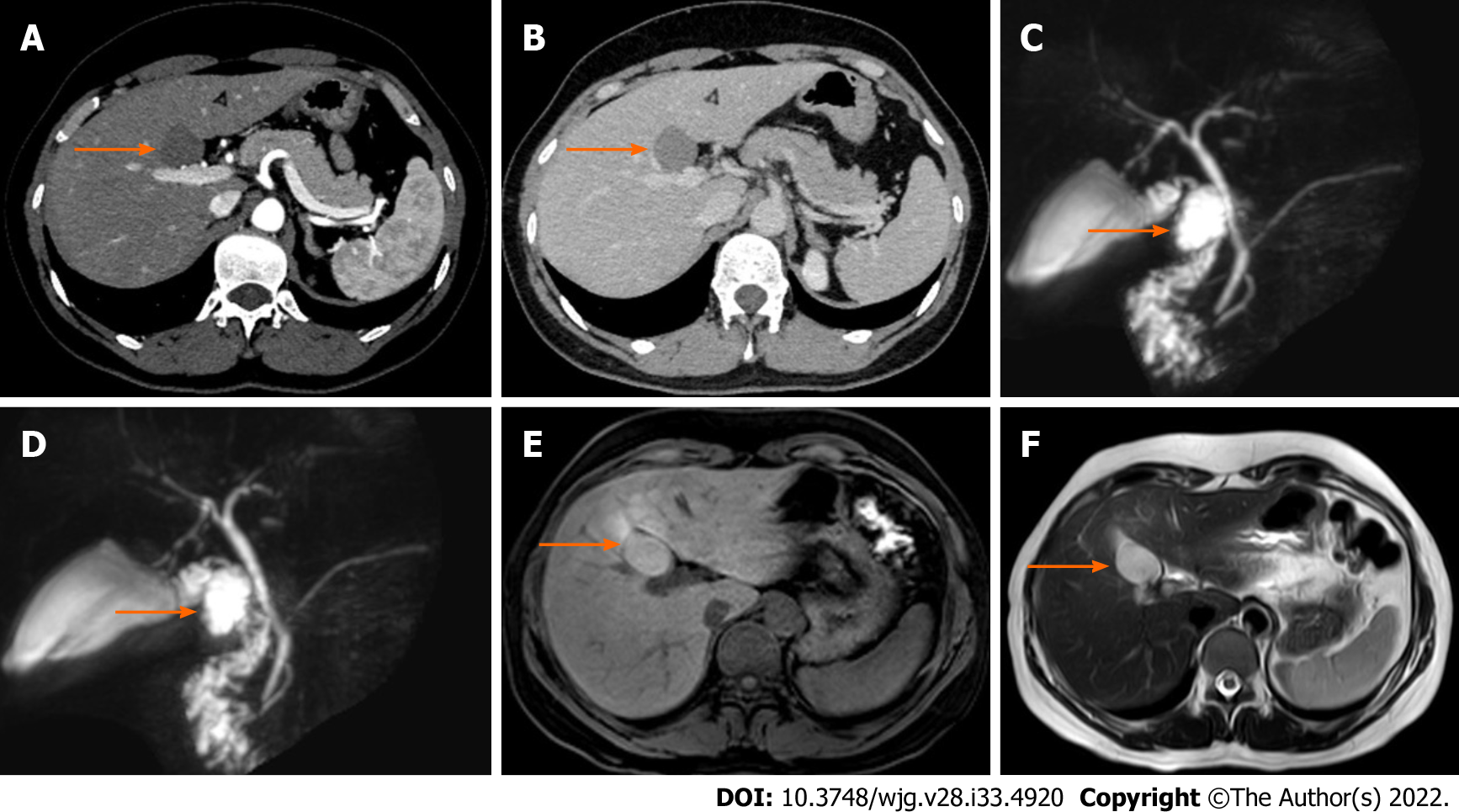
Abdominal color Doppler ultrasound showed a cystic echo beside the gallbladder in the left inner lobe of the liver with a size of 3.2 cm × 1.6 cm. The boundary was clear, the ultrasound transmission was poor, a bile mud echo was observed, there was no blood flow signal, and there appeared to be a connection with the neck of the gallbladder. Gallbladder diverticulum with cholestasis and chronic cholecystitis was suspected. Hepatobiliary, pancreatic, and splenic multi-slice plain computed tomography (CT) scanning and 3-phase enhanced scans showed an elliptical low-density shadow above the gallbladder in the left inner lobe of the liver, with a CT value of about 55 HU. Intrahepatic bile ducts were not dilated. The gallbladder was not enlarged but the wall was slightly thickened, and there was no abnormal density in the cavity. The cystic space-occupying lesion above the gallbladder in the left inner lobe of the liver strongly suggested gallbladder diverticulum with cholestasis. Magnetic resonance cholangiopancreatography (MRCP) was performed to determine the relationship between the lesion and the gallbladder. There was an oval abnormal signal in the gallbladder fossa area about 2.9 cm × 2.0 cm in size. T1-weighted imaging (T1WI) and T2-weighted imaging (T2WI) and diffusion-weighted imaging showed a high-signal shadow and the apparent diffusion coefficient was consistent with a slightly high-signal shadow; the edges of the shadow were thin, smooth, and clear, and there was no enhancement at the lesion center. The lesion appeared to be connected to the cystic duct given the limited fluid signal shadow in the gallbladder fossa area of the intrahepatic lobe (Figure 1).
Based on the patient’s symptoms, abdominal examination, and imaging findings, the initial diagnosis was gallbladder diverticulum with cholestasis combined with chronic cholecystitis. However, based on intraoperative findings and postoperative pathologic results, the diagnosis was later confirmed as ectopic bronchogenic cyst in the liver.
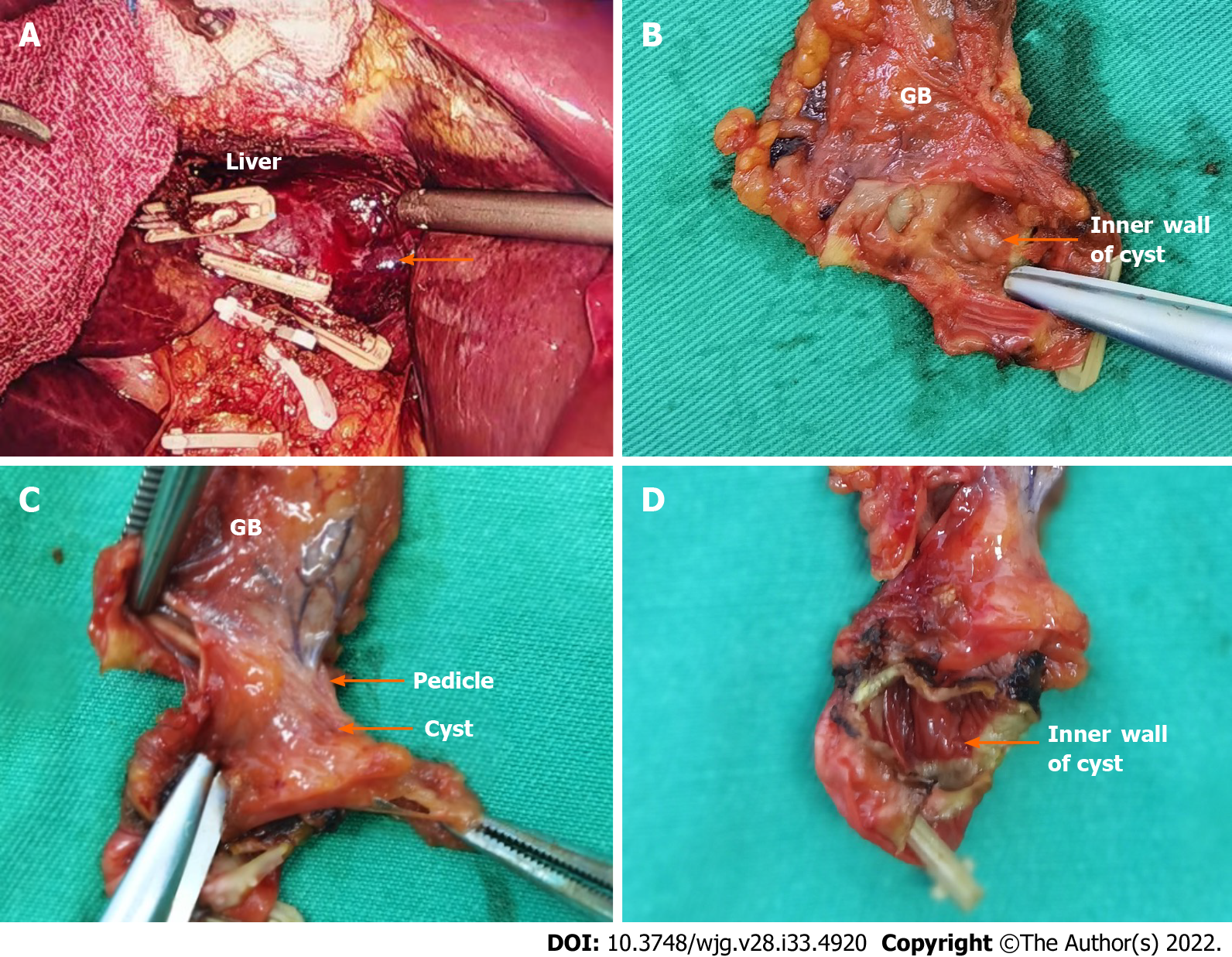
The patient underwent laparoscopic cholecystectomy and cystectomy of the left inner lobe of the liver. During the operation, it was observed that the cyst and gallbladder were connected to a pedicle but not to each other. Dark green bile was drained from the gallbladder, and light yellow turbid fluid was observed inside the cyst (Figure 2).
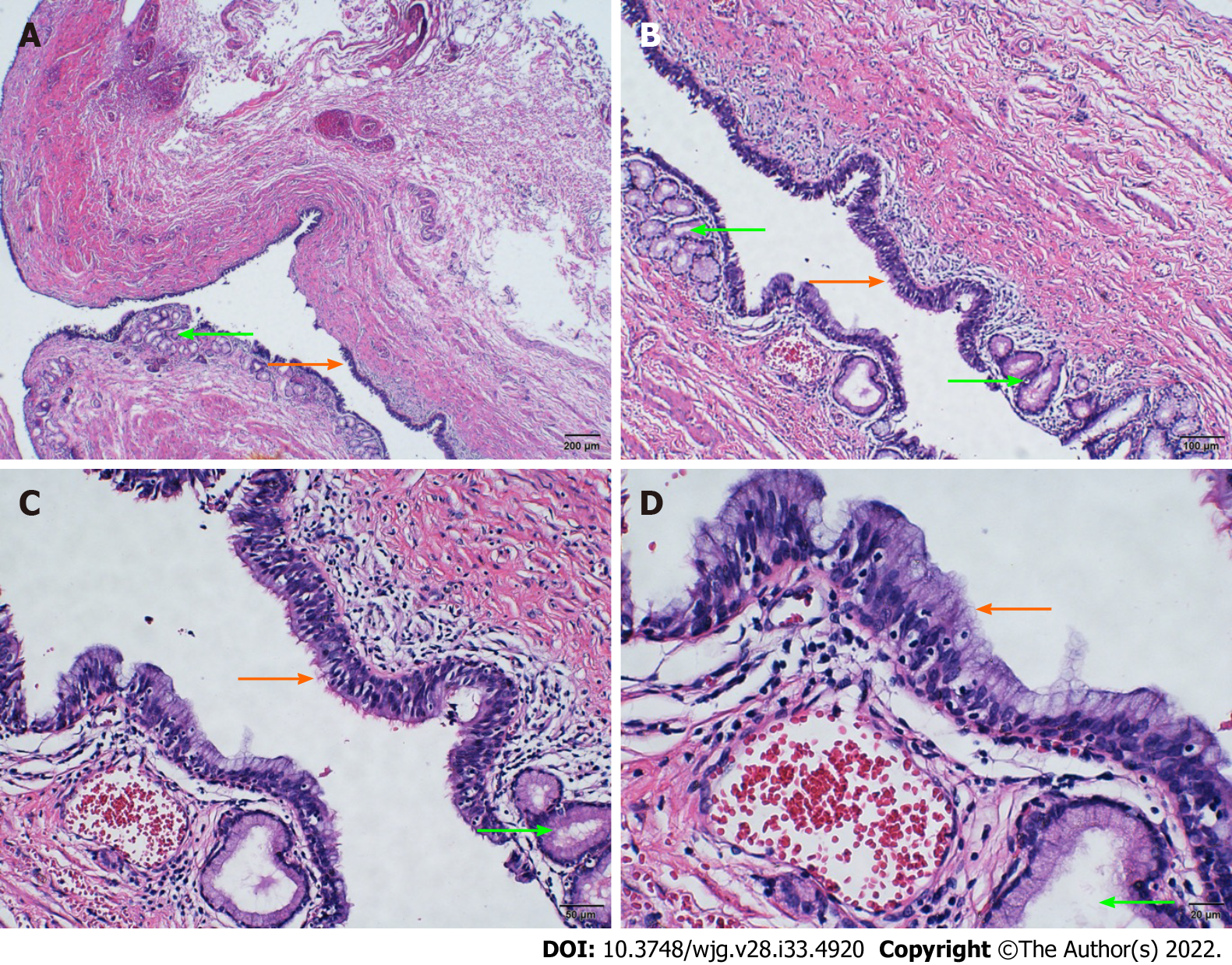
After the operation, we carried out a pathologic examination on the excised specimen. The outer part of the cyst was connected to the gallbladder; the volume was 2 cm × 2 cm × 2 cm, the wall thickness was 0.1-0.2 cm, and the inner wall was smooth and light brown. The cyst wall was fibrous under microscopic examination, with visible muscle tissue. Part of the mucosal epithelium on the inner surface was absent, and the remaining inner surface was partly lined with pseudostratified ciliated columnar epithelium and mucous epithelium. Serous and mucous glands were observed in the lamina propria, consistent with bronchogenic cysts. The intraoperative findings combined with histopathologic examination refuted the preoperative diagnosis of gallbladder diverticulum complicated by cholestasis (Figure 3). No recurrence was found in the color Doppler ultrasonography 6 mo after the operation.
Ectopic bronchogenic cysts can occur at any age, with similar prevalence in men and women. There are few specific manifestations but clinical symptoms can arise when a cyst compresses nearby organs or tissues. For example, a patient developed new abdominal pain and gross hematuria that may have been caused by the aggravation of a lump originating from the left adrenal gland[5]; the pain was intermittent, which may have been related to chronic cholecystitis. Similarly, ectopic bronchogenic cysts have no special imaging findings. Magnetic resonance imaging (MRI) examinations often show isointense shadows on T1WI and high-intensity shadows on T2WI that are not enhanced by the contrast agent. However, in some patients, both T1WI and T2WI show significant enhancement[6]. In our patient, T1WI showed a slightly high-signal shadow and T2WI showed a high-signal shadow; a retrospective analysis of the MRI findings was more suggestive of ectopic bronchogenic cysts, which are associated with elevated levels of the tumor markers carcinoembryonic antigen, carbohydrate antigen (CA)19-9, and CA72-4[7,8].
In countries where bronchogenic cysts are endemic, they are often associated with hydatid disease[9]. The diagnosis and differential diagnosis of ectopic bronchogenic cysts is extremely difficult and they are often confused with other types of cyst and serous or mucinous cystadenoma. The pathogenesis of ectopic bronchogenic cysts in the abdominal cavity is complex and diverse. It has been proposed to originate in the embryonic foregut, which develops from the primordial malformed trachea and bronchial tree in the early embryo; bacteria shed from this structure migrate to the caudal side of the foregut, which forms the abdominal organ or retroperitoneal bronchus cyst. The thoracic and abdominal cavities are thought to be connected in the early embryonic stage. At 6 wk of gestation, the pleura and peritoneum fuse and develop into a mature diaphragm. The body cavity is divided into the mature thoracic cavity and abdominal cavity. The abdominal buds of the tracheobronchial tree are squeezed and migrate into the abdominal cavity at the same time, leading to ectopic bronchogenic cysts in the abdominal cavity[10]. Clarifying the detailed mechanism underlying the development of bronchogenic cysts will facilitate their detection, diagnosis, and treatment.
Most ectopic bronchogenic cysts require surgical removal, and histopathologic examination of surgical specimens must be performed to confirm the diagnosis. Immunopositivity for cytokeratin (CK)7 and thyroid transcription factor 1 and immunonegativity for CK20 and calretinin in the epithelial lining also strongly support a diagnosis of bronchogenic cysts[7,11]. In terms of treatment, as ectopic bronchogenic cysts can be ectopic to different organs, the speed at which they develop and their biological behaviors vary[1,2]. Ectopic bronchogenic cysts are also easily confused with cystic diseases of adjacent organs, patients with bronchogenic cysts or suspected ectopic bronchogenic cysts should be examined by a surgeon, especially when the cyst is small as it may be missed. Thus, immunohistochemistry is useful when bronchial cysts cannot be differentially diagnosed based on histology and microscopic examination alone, and excision by using laparoscopy or robotic surgery and histopathology remain the first choices for treatment and definitive diagnosis[12].
Ectopic bronchogenic cysts are a congenital cystic tumor that are extremely difficult to diagnose and can be ectopically located in various organs, and have a risk of malignant transformation. Radiologists, hepatobiliary and pancreatic surgeons, gastrointestinal surgeons, urologists, and even neurosurgeons should be aware of these cysts. During diagnosis and treatment of a suspected cyst or cystadenoma, the possibility of ectopic bronchogenic cysts should be considered. The disease and its complications should be detected and diagnosed and treated as early as possible to avoid adverse consequences.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Samizadeh B, Iran; Yin F, United States S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Mumtaz A, Dhanani R, Faisal M, Maqbool H, Iqbal Khan A. Bronchogenic Cyst in the Cervical Region: A Rare Entity - A Case Report and Review of the Literature. Cureus. 2021;13:e14413. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Hu L, Fan J, Wang T, Tang G. Ectopic Bronchogenic Cyst in Abdomen- A Rare Special Type. Am J Med Sci. 2021;361:e59-e60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Martinod E, Pons F, Azorin J, Mouroux J, Dahan M, Faillon JM, Dujon A, Lajos PS, Riquet M, Jancovici R. Thoracoscopic excision of mediastinal bronchogenic cysts: results in 20 cases. Ann Thorac Surg. 2000;69:1525-1528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 51] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Kim KH, Kim JI, Ahn CH, Kim JS, Ku YM, Shin OR, Lee EJ, Lim KW. The first case of intraperitoneal bronchogenic cyst in Korea mimicking a gallbladder tumor. J Korean Med Sci. 2004;19:470-473. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Anderson MI, O'Reilly KJ, Costabile RA. Retroperitoneal bronchogenic cyst mimicking a pheochromocytoma. J Urol. 2001;166:1379-1380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Ubukata H, Satani T, Motohashi G, Konishi S, Goto Y, Watanabe Y, Nakada I, Tabuchi T. Intra-abdominal bronchogenic cyst with gastric attachment: report of a case. Surg Today. 2011;41:1095-1100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Yuan K, Shu M, Ma Y, Feng W, Ye J, Yuan Y. Ectopic bronchogenic cyst in the retroperitoneal region: a case report and literature review of adult patients. BMC Surg. 2021;21:347. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | He WT, Deng JY, Liang H, Xiao JY, Cao FL. Bronchogenic cyst of the stomach: A case report. World J Clin Cases. 2020;8:1525-1531. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Limaiem F, Mlika M. Bronchogenic Cyst. 2021 Jul 20. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. [PubMed] |
| 10. | Mirilas P. Embryogenesis of Ectopic Bronchogenic Cysts: Keep It Simple. J Invest Surg. 2020;33:574-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Nishida N, Hata Y, Nomoto K. Intramyocardial bronchogenic cyst: histological appearance and a review of the literature. Cardiovasc Pathol. 2017;28:64-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Taira N, Kawasaki H, Atsumi E, Ichi T, Kawabata T, Saio M, Yoshimi N. Mucoepidermoid Carcinoma of Arising from a Bronchogenic Cyst of the Diaphragm. Ann Thorac Cardiovasc Surg. 2018;24:247-250. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |