Published online Aug 28, 2022. doi: 10.3748/wjg.v28.i32.4620
Peer-review started: January 10, 2022
First decision: April 16, 2022
Revised: April 26, 2022
Accepted: June 26, 2022
Article in press: June 26, 2022
Published online: August 28, 2022
Processing time: 227 Days and 17.9 Hours
Pancreatic cancer is the most aggressive cancer type. Gemcitabine is the first line chemo-drug used for pancreatic cancer but exerts a broad spectrum of organ toxicities and adverse effects in patients.
To evaluate the anti-tumour activity and toxicological effects of Orthosiphon stamineus extract formulation (ID: C5EOSEW5050ESA trademarked as Nuva-staticTM), and gemcitabine combination on pancreatic xenograft model.
Mice were randomly divided into six groups of 6 mice each (n = 6) and given different treatments for 28 d. The study design consisted of a 2 x 3 factorial treatment structure, with gemcitabine (yes/no) by oral (at 1200 and 400 mg/kg per day). Human pancreatic cancer cells were injected subcutaneously into the flanks of athymic nude mice. C5EOSEW5050ESA (200 or 400 mg/kg per day) was administered orally, while gemcitabine (10 mg/kg per 3 d) was given intraperitoneally either alone or in combination treatment. Histopathological analyses of vital organs, tumour tissues, and incidence of lethality were analysed. Analyses of tumour necrosis and proliferation were determined by haematoxylin-eosin staining and immunohistochemistry for Ki-67, respectively.
No signs of toxicity or damage to vital organs were observed in all treatment groups compared to the untreated group. C5EOSEW5050ESA at 200 mg/kg and gemcitabine combination had no additive antitumor effects compared to a single treatment. Remarkably, a comparably greater response in a reduction in tumour growth, Ki-67 protein expression, and necrosis was demonstrated by 400 mg/kg of C5EOSEW5050ESA and gemcitabine combination than that of the individual agents.
These results highlighted the synergistic activity of C5EOSEW5050ESA with gemcitabine to reduce pancreatic tumour growth in mice compared to a single treatment. Thus, this study provides valuable insights into using C5EOSEW5050ESA as a complementary treatment with gemcitabine for pancreatic cancer.
Core Tip: The combination of C5EOSEW5050ESA at 400 mg/kg and gemcitabine synergistically reduced tumour growth compared to either drug alone by reducing Ki-67 cell proliferation marker and tumour necrosis. In addition, no signs of toxicity or damage to vital organs in single C5EOSEW5050ESA or gemcitabine and chemo-herbal combinations treated animals compared to the untreated group, indicating the safety and efficacy of the combination treatment in a short term study. Findings from this study may provide the basis for product formulation and manufacturing of botanical drugs to be used as complementary medicine for the treatment of cancer.
- Citation: Yehya AHS, Subramaniam AV, Asif M, Kaur G, Abdul Majid AMS, Oon CE. Anti-tumour activity and toxicological studies of combination treatment of Orthosiphon stamineus and gemcitabine on pancreatic xenograft model. World J Gastroenterol 2022; 28(32): 4620-4634
- URL: https://www.wjgnet.com/1007-9327/full/v28/i32/4620.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i32.4620
Pancreatic cancer is one of the deadliest cancers globally and has the most unfavourable survival rate of any cancer[1]. Chemotherapy, radiation, surgery, and molecular targeting agents are common strategies to treat pancreatic cancer. However, the majority of these systemic treatments are associated with severe side effects[1]. Gemcitabine, a nucleoside analogue of cytidine, is the first line of treatment used to treat pancreatic cancer[2]. However, its overall success rates are poor. In addition, combination treatments of gemcitabine with other chemo-drugs, such as capecitabine, irinotecan, oxaliplatin, and cisplatin, may cause multiple adverse reactions and drug resistance, leading to a reduction of drug efficacy[3].
Herbal products have been traditionally used to treat many diseases in Asian countries[4]. Data from pre-clinical and clinical studies have also highlighted that these natural herbs, when combined with conventional radio- or chemotherapies, can sensitise tumour cells to treatments to improve cancer patients' survival and quality of life[5,6]. Nevertheless, this is not always the case, as studies have also shown that herbal medicines, when combined with chemotherapies, may instead enhance the toxicity potential of chemo drugs, leading to increased incidences of severe side effects[7].
Therefore, understanding the interactions of herbal-chemo drugs is necessary for the appropriate use of these combinations to prevent the emergence of toxicity and therapeutic failure in cancer patients. Orthosiphon stamineus (O.s) is a traditional Asian herbal medicine used to treat various diseases, including cancers[8]. The safety profile of O.s has already been established globally by numerous research groups using in vivo and in vitro models[3,9]. Our research group has already established the antitumor efficacy of O.s against colon cancer[9,10]. C5OSEW5050ESA (NuvastaticTM) is a proprietary extract of O.s that completed a phase 2/3 clinical study for cancer fatigue in cancer patients with solid tumours receiving chemotherapy[11]. However, no study has reported the toxicity profile of C5OSEW5050ESA in a pancreatic cancer xenograft model as a stand-alone or in combination with gemcitabine. We have previously reported that the combination treatment of O.s and gemcitabine showed no toxicity in mice, either as a stand-alone or in combination[3]. Furthermore, O.s significantly sensitised Panc-1 towards gemcitabine in vitro[4]. Consequently, the present study was designed to evaluate the toxicological effects of NuvastaticTM and gemcitabine either alone or in combination using the pancreatic cancer nude mice model.
Orthosiphon stamineus extract (C5EOSEW5050ESA) was purchased from NatureCeutical Sdn Bhd, Malaysia. Gemcitabine (Catalogue No. S1149) was obtained from Selleckchem, Houston, TX, United States. C5EOSEW5050ESA was dissolved in sterile distilled water and filtered by a membrane filter unit (0.22 µm). C5EOSEW5050ESA was administered orally to mice, while gemcitabine was given via intraperitoneal injection after being dissolved in phosphate buffer saline (PBS).
Male athymic nude mice (procured from iDNA, Malaysia) were kept in filter-top cages under controlled atmospheric conditions at the EMAN Testing and Research laboratory, School of Pharmaceutical Sciences, USM. Autoclaved food, water, and bedding of cages were changed every 48 h. The animal study was approved and conducted under strict guidelines according to USM Animal Ethics Committee (Reference #: USM/Animal Ethics Approval/2016/(97) (746).
Panc-1, a pancreatic cancer cell line, was purchased from American Type Culture Collection (ATCC). The cells were maintained in Dulbecco’s Modified Eagle Medium (DMEM) (Thermo Scientific, United States) supplemented with 10% fetal bovine serum (Biowest, United States) and 100 units/mL penicillin-streptomycin (Nacalai Tesque, United States). Cells were kept at 37 °C in a humidified incubator with 5% CO2 atmosphere.
In vivo assessment of tumour growth in a nude mouse xenograft model: Panc-1 cells (20 × 106 cells suspended in 200 μL of a mixture of DMEM and matrigel in a 1:1 ratio) were injected subcutaneously on the dorsal side of each mouse. Treatment with gemcitabine and Et. O.s in different combinations or as a stand-alone was initiated when at least three of the tumours in any group reached 100 mm3.
Mice were randomly divided into six groups of 6 mice each (n = 6) and given different treatments for 28 d, as mentioned in Table 1. The body weight of all mice and tumour size was measured every 3rd day. At the end of the study, all the mice were euthanised with a combination of ketamine and xylazine when the tumour volumes from the untreated group reached 1000 mm3. The blood samples were collected for haematological and serum biochemical tests. Organs (liver, kidney, and spleen) were harvested and weighed to observe the changes in the organ weights of treated animals compared to the untreated group. Tumour tissues and organs were collected and fixed with 10% buffered formalin. Paraffin blocks were prepared, and sections of 5 μm were stained with haematoxylin and eosin (HE). Ten microscopic fields per slide were examined at × 20 and × 40 magnification, and photomicrographic images were captured using a digital camera.
| No. | Group | The route of treatment and dose |
| 1 | Group I (untreated group- distilled water) | Oral (1 mg/kg per day) |
| 2 | Group II (chemodrug-gemcitabine) | Intraperitoneal (10 mg/kg per 3 d) |
| 3 | Group III (low dose of O.s) | Oral (200 mg/kg per day) |
| 4 | Group IV (low dose of O.s -gemcitabine combination) | Oral (200 mg/kg per day) + Intraperitoneal (10 mg/kg per 3 d) |
| 5 | Group V (high dose of O.s) | Oral (400 mg/kg per day) |
| 6 | Group VI (high dose of O.s-gemcitabine combination) | Oral (400 mg/kg per day) + Intraperitoneal (10 mg/kg per 3 d) |
Blood samples were used to measure different haematological parameters, including haemoglobin (Hb) levels, total blood count, differential counting of white blood cells, packed cell volume (PCV), mean cell volume (MCV), mean cell haemoglobin (MCH), mean cell haemoglobin concentration (MCHC), red cell distribution width (RDW), creatinine, urea, uric acid, aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), gamma-glutamyl transferase (GGT), total bilirubin, cholesterol (low and high-density cholesterol), triglycerides, total protein, albumin, globulin, albumin/globulin ratio, and minerals (sodium, potassium, and chloride).
Key organs (liver, kidney, and spleen) were harvested and fixed in a 10% buffered formaldehyde solution. An automated tissue processing machine then processed the fixed tissues and embedded them in paraffin wax to prepare sample blocks.
Tissue sections of 5 mm thickness were cut and prepared at 60 °C. The slides were dewaxed in xylene and rehydrated through graded alcohol. Slides were rinsed and incubated with haematoxylin for 4 min. After rinsing, eosin was added to the slides for 1 min. Next, slides were rinsed in tap water and briefly air-dried at room temperature. Slides were then mounted with glycerol (Sigma, United States). Stained slides were examined and scored for the percentage of necrosis within the tumour areas by a pathologist (GK) under a light microscope.
The formalin-fixed-paraffin-embedded (FFPE) tissue sections were prepared at 60 °C, dewaxed in xylene, and rehydrated through graded alcohol. Antigens were retrieved using Dako's antigen retrieval buffer (1 ×, pH 9.0) and then microwaved on high for 15 min. Slides were cooled, washed and then blocked with hydrogen peroxidase and BSA. Then slides were treated with primary antibody Ki67 (Dako, Glostrup, Denmark) and left to incubate at 4 °C overnight at 1:50 dilution. The next day, slides were treated with secondary antibody goat anti-mouse (Dako, Glostrup, Denmark) for 1 h at 1:500 dilution. Later, avidin-biotin complex (Vector Laboratories, United States) was added to tissues for 1 h. After that, Dab stain (Dako, Glostrup, Denmark) and haematoxylin were added to the slides. Finally, slides were air-dried at room temperature and mounted with glycerol (Sigma, United States). Using ImageJ, the Ki-67 score was determined as the percentage of tumour cells that showed brown nuclear staining over the total number of nuclei from five random fields per tumour section.
Graphing software Excel (Microsoft, United States) and Prism (GraphPad, United States) were used for statistical analysis. Data were presented as mean ± SD whereas the parametric data analysis was performed using a one-way analysis of variance (ANOVA). Two-way ANOVA was used to understand if there is an interaction between the two independent variables on the dependent variable. The Tukey’s honest significant difference (HSD) post hoc test was used to assess the significant differences among all groups. Analysis for non-parametric data was performed using Kruskal-Wallis ANOVA. A value of P < 0.05 was considered significant when compared to values in the respective untreated group.
C5EOSEW5050ESA demonstrated no toxicity in mice: The average body weight within the untreated group increased compared to other treatment groups (Table 2). However, there was no notable difference in body weight between untreated groups and other treatment groups (Table 2). In addition, the weight of vital organs, including the kidney, liver, and spleen, remained unchanged post-treatment with either C5EOSEW5050ESA and/or gemcitabine (Table 3).
| No. | Group | Days | P value | ||||||||||
| 0 | 2 | 5 | 8 | 11 | 14 | 17 | 20 | 23 | 26 | 28 | |||
| 1 | Untreated | 24.2 ± 0.8 | 24.5 ± 1.0 | 24.7 ± 0.6 | 24.7 ± 0.9 | 24.6 ± 1.1 | 24.8 ± 0.9 | 25.0 ± 0.3 | 24.8 ± 0.6 | 24.6 ± 0.7 | 24.5 ± 1.1 | 24.5 ± 0.9 | - |
| 2 | Gemcitabine (10 mg/kg per 3 d) | 24.2 ± 0.7 | 24.3 ± 1.5 | 24.1 ± 1.2 | 23.9 ± 1.7 | 24.1 ± 1.3 | 24.0 ± 1.3 | 24.2 ± 0.5 | 24.5 ± 0.9 | 24.6 0 ± .5 | 24.3 ± 0.7 | 24.0 ± 0.9 | NS |
| 3 | O.s (200 mg/kg per day) | 23.6 ± 0.6 | 23.9 ± 0.7 | 24.9 ± 0.9 | 23.9 ± 1.1 | 24.1 ± 1.2 | 23.8 ± 1.1 | 24.0 ± 0.7 | 23.9 ± 9.0 | 23.8 ± 1.2 | 24.0 ± 1.5 | 23.8 ± 0.5 | NS |
| 4 | O.s (200 mg/kg per day) and gemcitabine (10 mg/kg per 3 d) combination | 24.0 ± 0.8 | 24.0 ± 1.2 | 23.9 ± 1.0 | 24.0 ± 1.1 | 23.4 ± 1.3 | 23.9 ± 1.5 | 24.1 ± 0.7 | 24.2 ± 0.7 | 23.9 ± 1.3 | 23.7 ± 1.1 | 23.5 ± 1.1 | NS |
| 5 | O.s (400 mg/kg per day) | 24.2 ± 0.7 | 24.4 ± 0.8 | 24.3 ± 1.0 | 24.5 ± 1.3 | 24.1 ± 1.0 | 24.3 ± 1.0 | 24.2 ± 1.0 | 24.4 ± 1.3 | 24.1 ± 1.4 | 24.0 ± 1.5 | 23.8 ± 1.2 | NS |
| 6 | O.s (400 mg/kg per day) and gemcitabine (10 mg/kg per 3 d) combination | 23.9 ± 0.7 | 24.0 ± 0.2 | 23.4 ± 0.7 | 23.4 ± 0.7 | 23.4 ± 0.5 | 23.4 ± 0.4 | 23.3 ± 0.5 | 23.5 ± 0.5 | 23.3 ± 0.8 | 23.3 ± 0.5 | 23.3 ± 0.3 | NS |
| No. | Group | Organ weight, g | P value | ||
| Liver | Kidney | Spleen | |||
| 1 | Untreated | 1.7 ± 0.22 | 0.47 ± 0.06 | 0.11 ± 0.03 | - |
| 2 | Gemcitabine (10 mg/kg per 3 d) | 1.7 ± 0.23 | 0.46 ± 0.06 | 0.10 ± 0.03 | NS |
| 3 | O.s (200 mg/kg per day) | 1.67 ± 0.23 | 0.47 ± 0.06 | 0.11 ± 0.03 | NS |
| 4 | O.s (200 mg/kg per day) and gemcitabine (10 mg/kg per 3 d) combination | 1.31 ± 0.25 | 0.41 ± 0.08 | 0.07 ± 0.03 | NS |
| 5 | O.s (400 mg/kg per day) | 1.37 ± 0.35 | 0.41 ± 0.09 | 0.24 ± 0.02 | NS |
| 6 | O.s (400 mg/kg per day) and gemcitabine (10 mg/kg per 3 d) combination | 1.43 ± 0.19 | 0.43 ± 0.09 | 0.08 ± 0.02 | NS |
Haematological-biochemical parameters and electrolyte profiles: No significant changes were observed in the Hb level, total blood cells count, or differential counting of WBC, PCV, MCV, MCH, MCHC, and RDW when compared with the corresponding parameters in the untreated group (Table 4). No significant changes were noted in serum parameters, i.e. creatinine, urea, uric acid, AST, ALT, ALP, GGT, total bilirubin, total protein, albumin, globulin, and albumin/globulin ratio, which were observed in animal groups treated with C5EOSEW5050ESA at (200 or 400 mg/kg per day) alone or in combination with gemcitabine (10 mg/kg per 3 d) after 28 d treatment when compared to the untreated group (Table 5). Normal ALT, ALP, and AST levels in the serum indicate that there is no damage in hepatocytes. Similarly, urea and total bilirubin levels were also within the normal range, indicating the lack of toxicity in the kidneys when treated with C5EOSEW5050ESA and gemcitabine either alone or in combination treatment (Table 5). Electrolytes were within the normal ranges in all the groups, with no significant changes observed compared to the untreated group (Table 5).
| No. | Group | Hb,g/L | Total RBC as 1012/L | PCV, L/L | MCV, fL | MCH, pg | MCHC, g/L | RDW, % | Total WBC as 109/L | N, % | L, % | M, % | E, % | B, % | Plts as 109/L |
| 1 | Untreated | 121 ± 1.0 | 7.91 ± 0.9 | 0.36 ± 0.0 | 46 ± 1.5 | 15 ± 0.7 | 332 ± 1.1 | 20.6 ± 1.0 | 5.8 ± 1.3 | 37 ± 1.0 | 55 ± 1.1 | 5 ± 0.8 | 2 ± 0.1 | 1 ± 0.0 | 790 ± 1.2 |
| 2 | Gemcitabine (10 mg/kg per 3 d) | 118 ± 1.4 | 7.60 ± 1.1 | 0.38 ± 0.0 | 50.0 ± 1.8 | 16.0 ± 0.6 | 313 ± 1.8 | 22.1 ± 0.7 | 6.0 ± 1.2 | 33.0 ± 1.2 | 60.0 ± 0.7 | 6.0 ± 1.3 | 1.0 ± 0.1 | 0.0 ± 0.1 | 720 ± 1.4 |
| 3 | O.s (200 mg/kg per day) | 118 ± 1.5 | 8.0 ± 0.8 | 0.38 ± 0.0 | 48.0 ± 2.0 | 15.0 ± 1.1 | 307 ± 0.9 | 22.3 ± 1.6 | 6.10 ± 0.7 | 35.0 ± 0.8 | 53.0 ± 0.6 | 9.0 ± 1.0 | 1.0 ± 0.1 | 2.0 ± 0.0 | 801 ± 0.8 |
| 4 | O.s (200 mg/kg per day) and gemcitabine (10 mg/kg per 3 d) combination | 115 ± 1.7 | 7.1 ± 1.4 | 0.35 ± 0.0 | 50.0 ± 1.6 | 16.0 ± 0.7 | 321 ± 1.5 | 21.5 ± 0.8 | 5.70 ± 1.5 | 32.0 ± 0.9 | 60.0 ± 1.1 | 5.0 ± 0.7 | 2.0 ± 0.1 | 1.0 ± 0.1 | 760 ± 0.9 |
| 5 | O.s (400 mg/kg per day) | 123 ± 1.6 | 7.9 ± 0.7 | 0.36 ± 0.0 | 46.0 ± 1.5 | 16.0 ± 1.6 | 335 ± 2.0 | 21.0 ± 0.9 | 5.70 ± 1.8 | 33.0 ± 1.2 | 61.0 ± 1.2 | 4.0 ± 0.6 | 2.0 ± 0.1 | 0.0 ± 0.0 | 740 ± 1.0 |
| 6 | O.s (400 mg/kg per day) and gemcitabine (10 mg/kg per 3 d) combination | 123 ± 1.1 | 7.70 ± 0.9 | 0.36 ± 0.0 | 47.0 ± 1.2 | 16.0 ± 0.4 | 331 ± 1.2 | 22.6 ± 1.3 | 6.0 ± 1.5 | 30.0 ± 0.9 | 60.0 ± 1.1 | 8.0 ± 1.3 | 1.0 ± 0.1 | 1.0 ± 0.0 | 810 ± 1.3 |
| No. | Group | Creatinine, mmol/L | Urea,mmol/L | Uric acid, mmol/L | AKT, U/L | AST, U/L | ALT, U/L | GGT, U/L | Total protein, g/L | Albumin, g/L | Globulin, g/L | Albumin/ Globulin ratio | Total Bilirubin, µmol/L | Na | K | CL |
| 1 | Untreated | 28.1 ± 1.5 | 8.80 ± 0.9 | 0.20 ± 0.0 | 96.0 ± 0.5 | 195 ± 0.7 | 73.0 ± 0.7 | < 3.0 ± 0.0 | 50.0 ± 0.5 | 30.0 ± 1.1 | 23.0 ± 0.5 | 1.40 ± 0.3 | < 2.0 ± 0.0 | 178 ± 0.3 | 8.00 ± 0.7 | 124 ± 1.1 |
| 2 | Gemcitabine (10 mg/kg per 3 d) | 28.0 ± 1.9 | 9.00 ± 1.1 | 0.16 ± 0.1 | 93.0 ± 1.1 | 190 ± 0.9 | 72.0 ± 0.9 | < 3.0 ± 0.0 | 52.0 ± 1.2 | 32.0 ± 0.7 | 24.0 ± 0.7 | 1.40 ± 0.2 | < 2.0 ± 0.0 | 173 ± 0.5 | 9.30 ± 0.4 | 123 ± 0.2 |
| 3 | O.s (200 mg/kg per day) | 29.0 ± 1.5 | 9.20 ± 1.3 | 0.19 ± 0.0 | 98.0 ± 1.2 | 201 ± 1.1 | 80.0 ± 1.1 | < 3.0 ± 0.0 | 50.5 ± 0.7 | 33.0 ± 0.3 | 23.0 ± 0.7 | 1.30 ± 0.3 | < 2.0 ± 0.0 | 174 ± 0.8 | 9.00 ± 0.8 | 128 ± 0.9 |
| 4 | O.s (200 mg/kg per day) and gemcitabine (10 mg/kg per 3 d) combination | 27.5 ± 1.1 | 9.50 ± 0.9 | 0.21 ± 0.1 | 101 ± 0.9 | 210 ± 0.7 | 77.0 ± 0.7 | < 3.0 ± 0.0 | 51.3 ± 1.1 | 29.9 ± 0.9 | 22.5 ± 0.9 | 1.30 ± 0.2 | < 2.0 ± 0.0 | 186 ± 0.9 | 8.60 ± 0.6 | 130 ± 1.1 |
| 5 | O.s (400 mg/kg per day) | 28.5 ± 0.9 | 8.80 ± 0.7 | 0.22 ± 0.1 | 101 ± 0.7 | 199 ± 0.9 | 66.0 ± 0.5 | < 3.0 ± 0.0 | 51.9 ± 0.5 | 32.4 ± 0.8 | 25.0 ± 0.9 | 1.40 ± 0.2 | < 2.0 ± 0.0 | 190 ± 0.4 | 10.0 ± 0.5 | 133 ± 0.9 |
| 6 | O.s (400 mg/kg per day) and gemcitabine (10 mg/kg per 3 d) combination | 27.0 ± 0.8 | 8.50 ± 1.3 | 0.21 ± 0.0 | 103 ± 0.8 | 190 ± 0.7 | 70.0 ± 0.9 | < 3.0 ± 0.0 | 52.0 ± 0.7 | 30.5 ± 0.6 | 24.0 ± 0.7 | 1.40 ± 0.1 | < 2.0 ± 0.0 | 185 ± 0.6 | 9.80 ± 0.9 | 123 ± 0.5 |
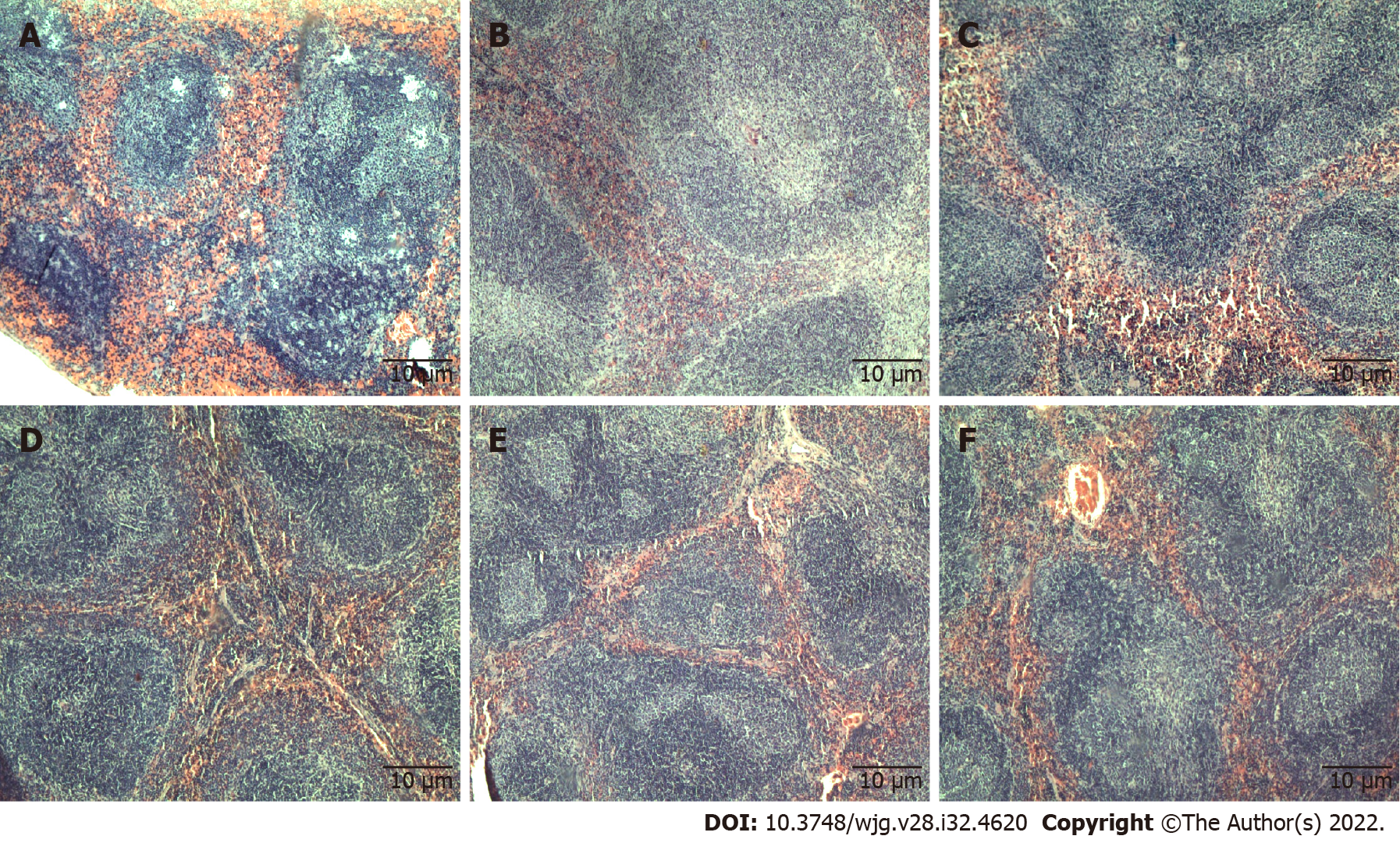
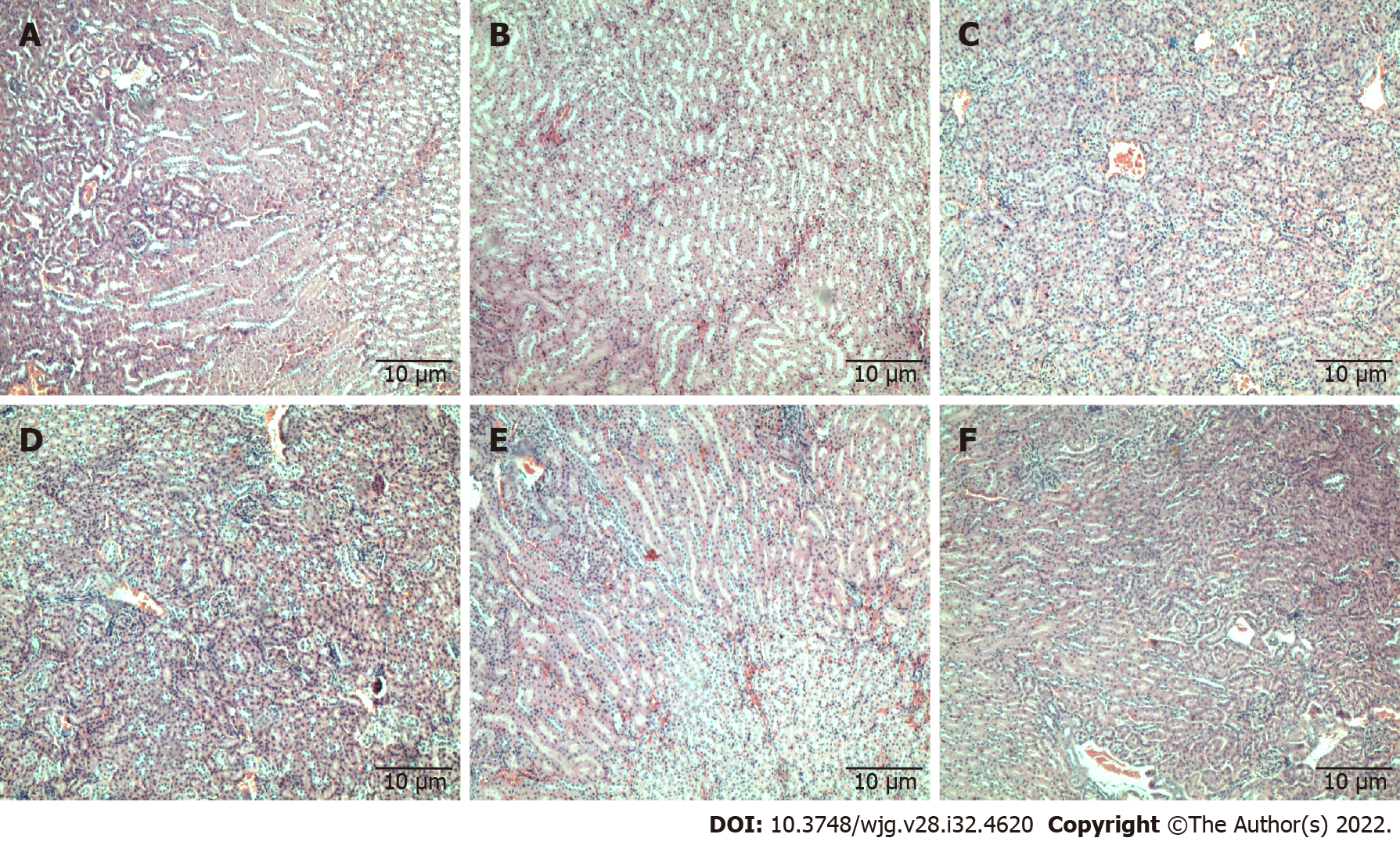
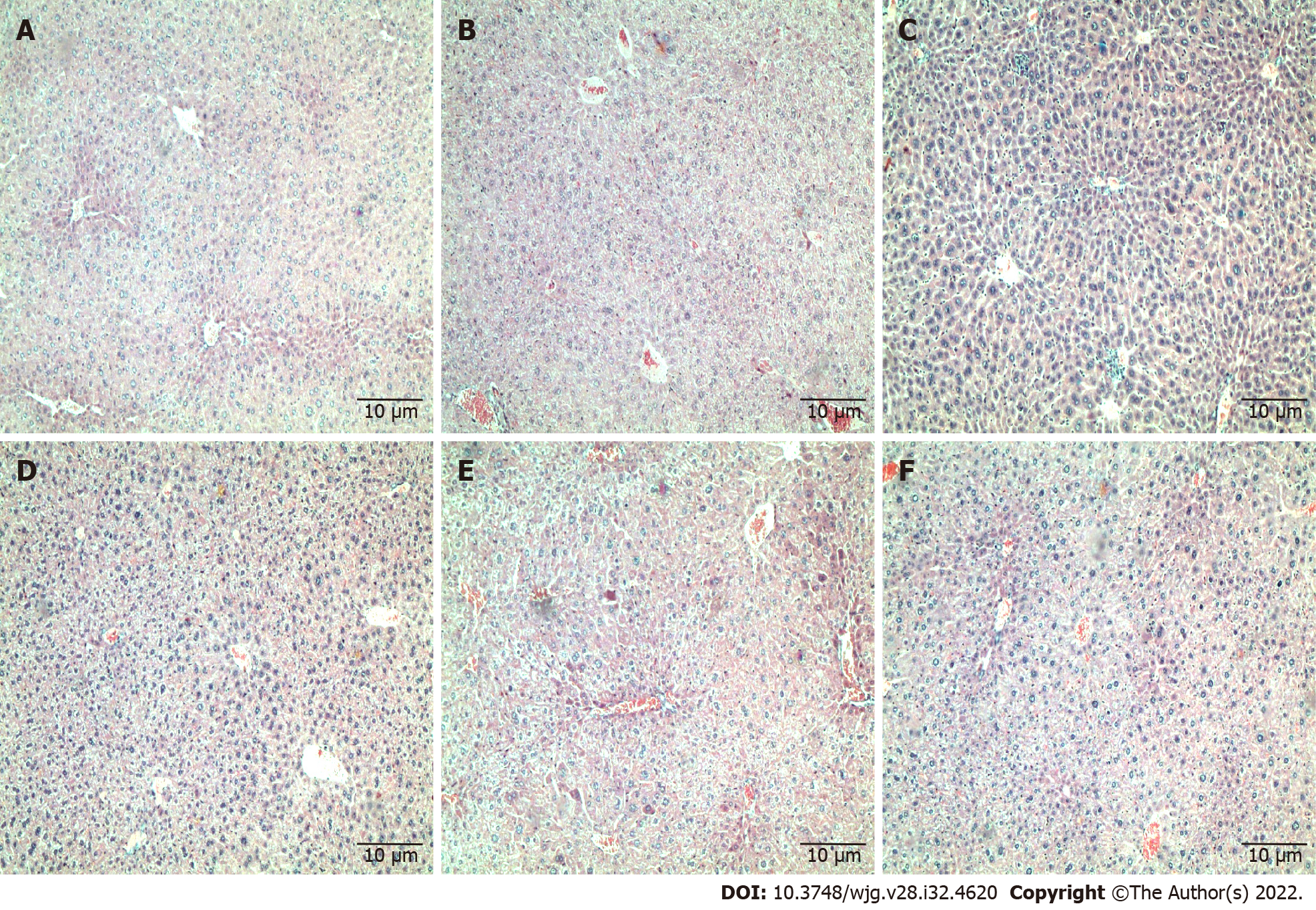
Histopathology analysis: Histopathological examination of formalin-fixed paraffin-embedded tissues of the spleen (Figure 1), kidney (Figure 2), and liver (Figure 3) of all treatment groups, as well as the untreated group, revealed normal histology without pathological evidence of inflammation or necrosis. In addition, the liver did not exhibit an accumulation of neutral fats or triglycerides within the liver cells. However, the liver cells demonstrated mild swelling in all groups except for C5EOSEW5050ESA (200 mg/kg per day) treatment group (Figure 3).
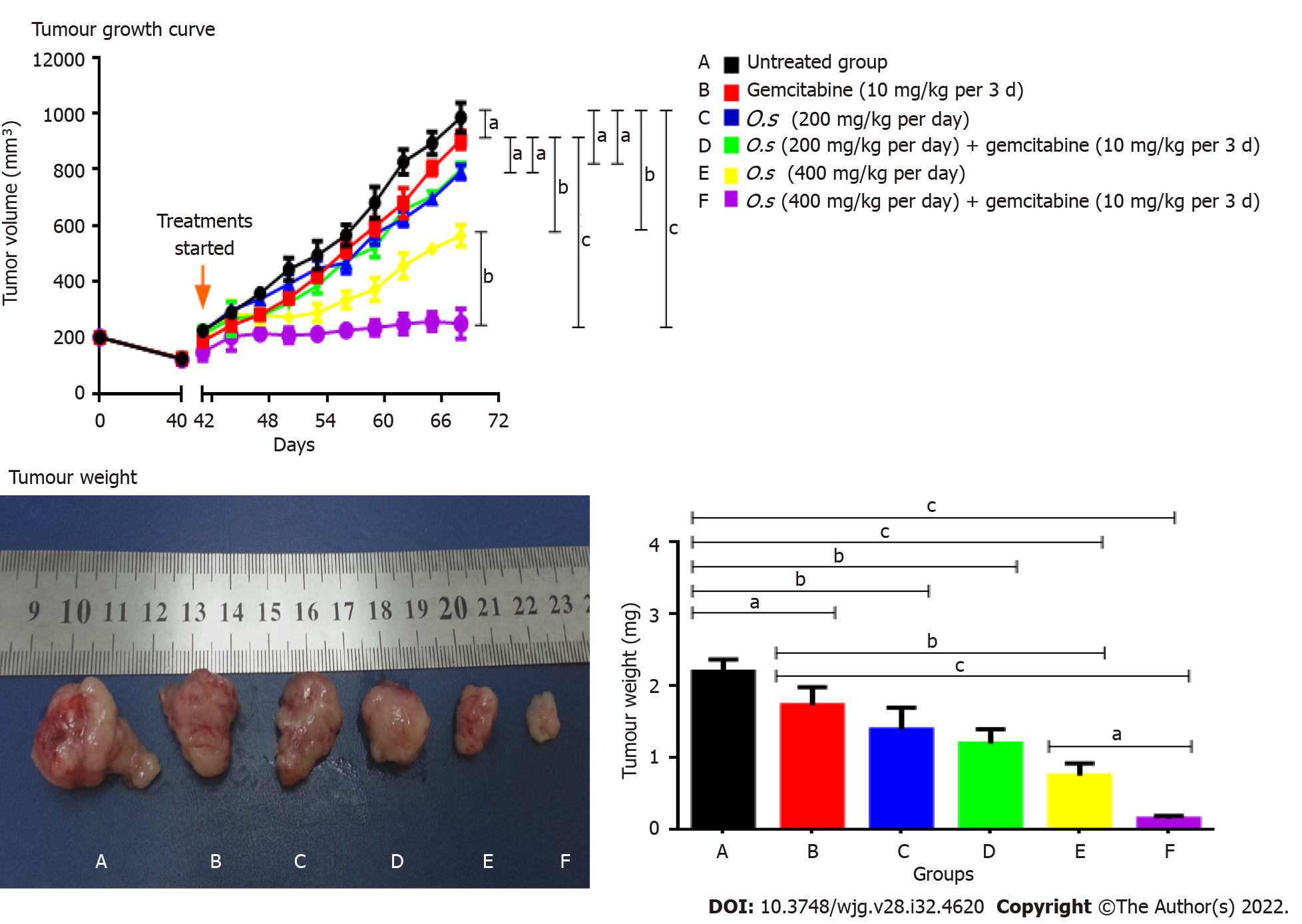
Single treatments with gemcitabine at 10 mg/kg and C5EO-SEW5050ESA at 200 mg/kg or 400 mg/kg inhibited tumour growth and reduced tumour weight compared to the vehicle untreated group (Figures 4A and B). However, compared to a single treatment, no additive effect in inhibiting tumour growth and tumour weight was obtained with 200 mg/kg C5EOSE-W5050ESA combined with gemcitabine (Figure 4A and B). However, C5EOSEW5050ESA at 400 mg/kg combined with gemcitabine significantly reduced tumour growth and tumour weight compared to individual treatment groups (Figures 4A and B).
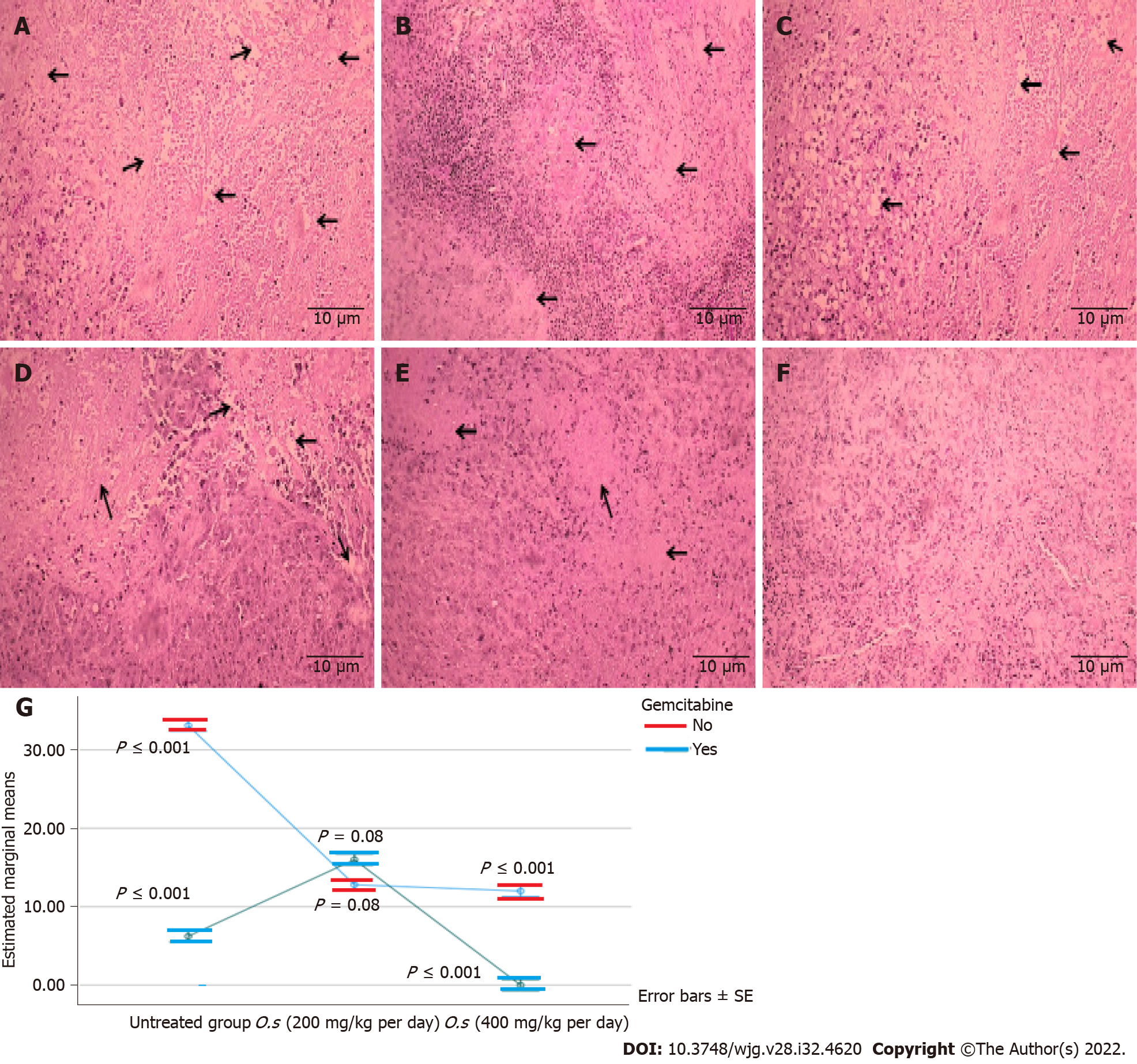
C5EOSEW5050ESA and gemcitabine combination synergistically inhibited pancreatic tumour necrosis in the xenograft model: A single treatment with gemcitabine at 10 mg/kg and C5EO-SEW5050ESA at 200 mg/kg or 400 mg/kg reduced tumour necrosis compared to untreated tumour cells (Figure 5). No additive effect in reducing tumour necrosis was obtained with C5EOSEW5050ESA at 200 mg/kg and gemcitabine combination compared to a single treatment (Figure 5D). However, C5EOSEW5050ESA at 400 mg/kg and gemcitabine combination significantly reduced tumour necrosis compared to single treatment groups of the respective doses (Figure 5).
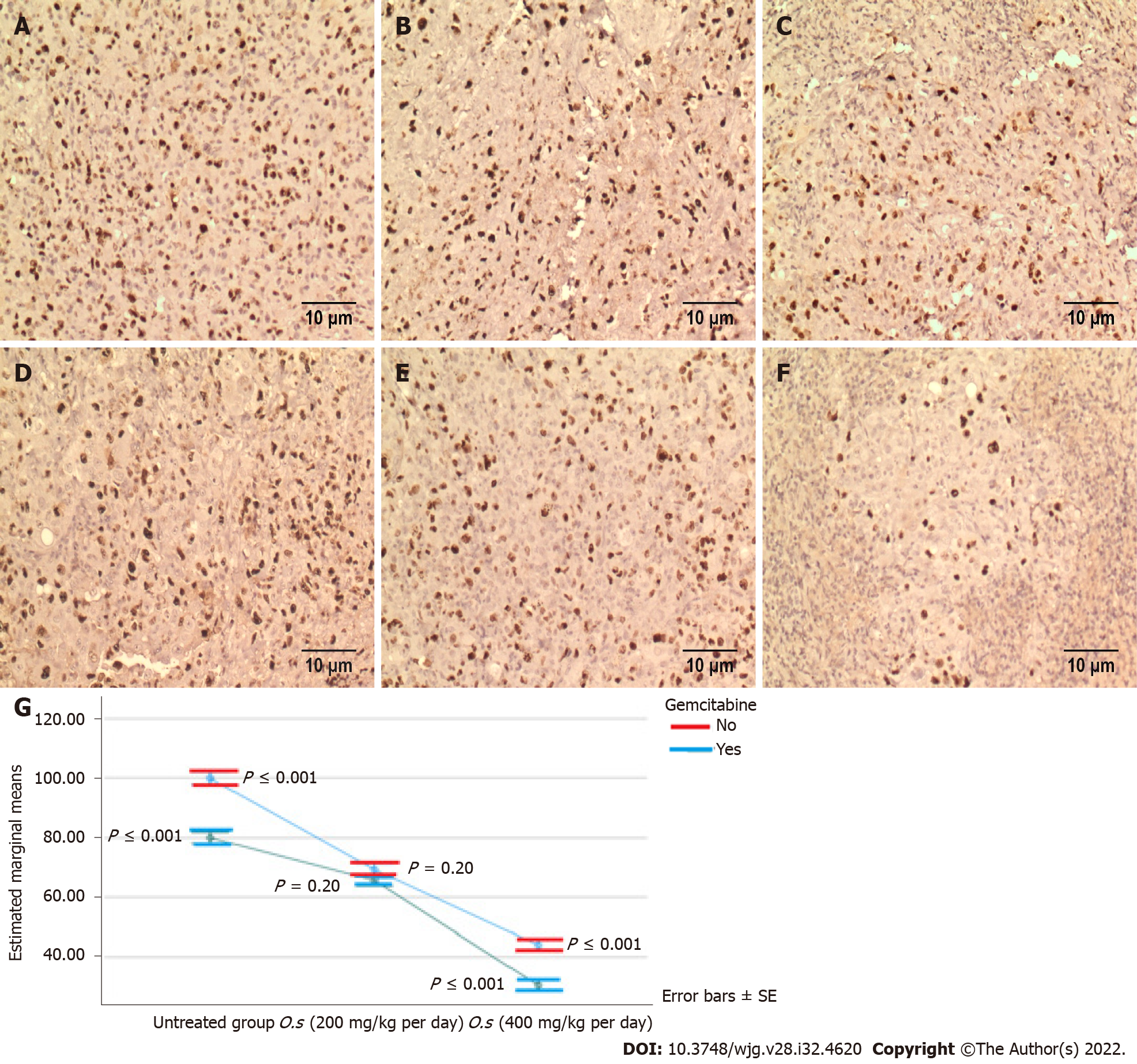
C5EOSEW5050ESA combined with gemcitabine synergistically inhibited Ki67 protein expression in pancreatic tumour tissue: Ki67 proliferative marker protein was highly expressed in the untreated group compared to all treatment groups (Figure 6). Compared to a single treatment, no additive effect in reducing Ki67 protein expression was obtained with 200 mg/kg C5EOSEW5050ESA and gemcitabine combination (Figure 6). However, 400 mg/kg C5EOSEW5050ESA and gemcitabine combination synergistically inhibited the expression of Ki67 protein compared to single treatment and other treatment groups (Figure 6).
Studies have shown that therapeutic combinations containing low-dose marketed drugs and plant extracts/isolated compounds or essential oils may improve the safety profile of marketed drugs and produce synergistic actions[12,13]. The safety profile of C5EOSEW5050ESA has previously been established[14,15], with its LD50 values reported to be greater than 5000 mg/kg[15]. Chemo-herbal combinations are one of the possible therapeutic options which can be employed to improve the efficacy of a drug, reduce adverse drug effects and increase disease-free intervals and overall survival rates in cancer patients. The majority of chemotherapeutic drugs destroy tumours and retard cancer growth but may also damage healthy tissues. Thus, new chemo-herbal combinations are anticipated to play an essential role in developing more effective and safer strategies to inhibit cancer progress with minimal side effects[4].
We have previously shown the synergistic anti-cancer effects of combined C5EOSEW5050ESA and gemcitabine treatment on Panc-1 and MiaPaCa-2 pancreatic cancer cell lines[3]. Moreover, no toxicity was observed in mice in an acute toxicity study[3]. In the current study, the combination treatment in a pancreatic tumour xenograft model revealed no abnormal signs in any of the treatment groups (Figures 1-3). Moreover, no significant difference in organ weight change was noted when compared to the untreated group, supporting the relatively safe nature of selected chemo-herbal combinations (Table 3).
Clinical biochemistry and haematological analyses play a significant role in evaluating the signs of toxicity induced by drugs[16]. No significant alterations in haematological parameters were observed in the animal blood samples treated with C5EOSEW5050ESA and gemcitabine combination, indicating that these combinations did not damage the blood cells (Table 4). Increased serum bilirubin concentration and occurrence of tissue haemolysis are commonly seen when the liver is impaired[17]. The absence of these observations in the current study demonstrated the non-toxic effects of the C5EOSEW5050ESA gemcitabine combination on haemoglobin metabolic pathways (Table 4). A slight drop in white blood count and platelets and mild myelosuppression have been reported with extended treatment duration and high doses of gemcitabine[18]. In 2013, the MPACT phase III trial, which included over 800 patients, showed a significant overall survival benefit with the combination of nanomolecular albumin-bound (nab)-paclitaxel and gemcitabine (nabPGem) over gemcitabine monotherapy, with acceptable toxicity. The overall toxicity of nabPGem is lower than in the triple chemotherapy 5-FU, leucovorin, irinotecan and oxaliplatin, especially haematotoxicity and rates of neutropenic fever[19,20]. However, the current study and our previous toxicity study revealed no reduction in white blood cells and platelets (Table 4)[3]. In fact, C5EOSEW5050ESA and gemcitabine combination at the higher dose enhanced its efficacy at reducing tumour growth without causing any side effects, at least in this short term study.
Kidneys are particularly vulnerable to high doses of drugs as they eradicate many drugs and their metabolites. Therefore, renal function tests measure various substances, including serum urea, serum creatinine, and albumin, to determine the current health of the kidneys[21]. In the present study, there was no nephrotoxicity observed, indicating the safe nature of chemo-herbal combinations. The results showed normal level concentrations of urea, creatinine, and albumin and were supported by the typical renal architecture of kidney sections (Figure 2).
Liver function tests, for such markers as ALT, AST, ALP, and GGT, are used to measure hepatocellular damage during illnesses[22]. There were no significant changes in the serum levels of AST, ALT, ALP, and GGT in all treatment groups (Table 5). In addition, the hepatocellular architecture appeared normal in all treatment groups (Figure 3).
As a single treatment, gemcitabine at 10 mg/kg and C5EOSEW5050ESA at 200 mg/kg or 400 mg/kg inhibited tumour growth compared to untreated mice (Figure 4). Compared to a single treatment, no additive inhibition of tumour growth was obtained with 200 mg/kg C5EOSEW5050ESA and gemcitabine combination (Figure 4). However, C5EOSEW5050ESA at 400 mg/kg and gemcitabine combination significantly reduced tumour growth compared to the single treatment groups of the respective doses (Figure 4). Further studies investigating how combination treatment affects pancreatic cancer cell proliferation and apoptosis or necrosis will shed light on their mode of action. In our previous study, C5EOSEW5050ESA and gemcitabine combination inhibited the survival and proliferation of Panc-1 cells in vitro[23]. Also, the combination of C5EOSEW5050ESA and gemcitabine-induced apoptosis and reduced EMT markers and multidrug-resistant genes (MDR-1, MRP-4, and MRP-5), and the Notch signalling pathway[24]. In the current study, the tumour necrosis percentage was estimated in tissue sections stained by HE. Single treatment of gemcitabine and C5EOSEW5050ESA either at low or high dose reduced the tumour percentage compared to untreated (Figure 5). There were no additional effects in the reduction of tumour necrosis post-treatment with a low dose of C5EOSEW5050ESA and gemcitabine combination compared to a single treatment (Figure 5). However, the high dose of C5EOSEW5050ESA and gemcitabine combination reduced tumour necrosis compared to a single treatment (Figure 5).
The combination treatment of C5EOSEW5050ESA at a high dose and gemcitabine significantly reduced Ki67 protein expression in tumour cells compared to a single treatment (Figure 6), indicating reduced cell proliferation in the former group. The epigallocatechin-3-O-gallate (EGCG) polyphenol is enriched in C5EOSEW5050ESA extract. Others have reported EGCG to inhibit tumour growth and induce apoptosis in mice implanted with head, neck, and lung cancers by decreasing the Ki67 expression in tissues from the xenograft model and downregulating caspase-3, caspase-8, caspase-9, and Bax in mouse vascular smooth muscle cells[25,26]. Another study showed that resveratrol inhibited Ki67 expression in pancreatic cancer cells in vitro and in vivo by sensitising pancreatic cancer cells to gemcitabine treatment[25]. It is postulated that the polyphenols in C5EOSEW5050ESA may act synergistically with gemcitabine in the pancreatic tumour xenograft model. C5EOSEW5050ESA worked in synergy with gemcitabine to reduce pancreatic tumour growth and tumour necrosis in mice compared to a single treatment of either C5EOSEW5050ESA or gemcitabine. Thus, based on current findings, it is proposed that 50% ethanol extract of O.s has the potential to be used in combination with gemcitabine to treat pancreatic cancer.
This study provides preliminary scientific evidence about the safety profile of O.s derived extract C5EOSEW5050ESA present in NuvastaticTM in combination with gemcitabine in an athymic nude mice model. Furthermore, this work demonstrated that C5EOSEW5050ESA extract in combination with gemcitabine is relatively safe in the acute toxicity study. Furthermore, the clinical efficacy and safety of NuvastaticTM in cancer asthenia have been evaluated in phase III clinical trials (ClinicalTrials.gov, Identifier: NCT04546607). Therefore, NuvastaticTM has the potential to be employed as a complementary treatment with gemcitabine to treat pancreatic cancer.
Gemcitabine is the cornerstone for pancreatic cancer but demonstrates adverse effects in patients. Orthosiphon stamineus (O.s) has been traditionally used to treat various diseases. C5OSEW5050ESA (NuvastaticTM) is a proprietary extract of O.s that completed a phase 2/3 clinical study for cancer fatigue in cancer patients with solid tumours receiving chemotherapy.
No study has reported the toxicity profile of C5OSEW5050ESA in a pancreatic tumour animal model either as a stand-alone or in combination with gemcitabine.
To determine the anti-tumour activity and potential toxicity of NuvastaticTM and gemcitabine combination on pancreatic xenograft model.
Human pancreatic cancer cells were injected subcutaneously into athymic nude mice. C5EOSEW5050ESA (200 or 400 mg/kg per day) was administered orally, while gemcitabine (10 mg/kg/ 3 d) was given intraperitoneally either alone or in combination treatment. Histopathological analyses of key organs, tumour tissues, and incidence of lethality were determined.
C5EOSEW5050ESA at 200 mg/kg and gemcitabine combination had no additive antitumor effects compared to a single treatment. A comparably greater response in a reduction in tumour growth via a reduction of Ki-67 protein expression, and a decrease in necrosis was also demonstrated by 400 mg/kg of C5EOSEW5050ESA and gemcitabine combination compared to that of individual agents. No signs of organ toxicities were observed in any treatment group.
The combination of C5EOSEW5050ESA with gemcitabine significantly reduced the pancreatic tumour growth in mice compared to a single treatment. This study provides valuable insights into using C5EOSEW5050ESA as a complementary treatment to gemcitabine for pancreatic cancer.
Findings from this study may provide the basis for product formulation and manufacturing of botanical drugs (NuvastaticTM) to be used as complementary medicine for the treatment of pancreatic cancer patients.
Ashwaq Yehya was supported by TWAS-USM (The Academy of Sciences for the Developing World, Italy-Universiti Sains Malaysia).
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Integrative and complementary medicine
Country/Territory of origin: Malaysia
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Hamaya Y, Japan; Matsumoto T, Japan S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Looi CK, Chung FF, Leong CO, Wong SF, Rosli R, Mai CW. Therapeutic challenges and current immunomodulatory strategies in targeting the immunosuppressive pancreatic tumor microenvironment. J Exp Clin Cancer Res. 2019;38:162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 131] [Cited by in RCA: 132] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 2. | Shukla SK, Purohit V, Mehla K, Gunda V, Chaika NV, Vernucci E, King RJ, Abrego J, Goode GD, Dasgupta A, Illies AL, Gebregiworgis T, Dai B, Augustine JJ, Murthy D, Attri KS, Mashadova O, Grandgenett PM, Powers R, Ly QP, Lazenby AJ, Grem JL, Yu F, Matés JM, Asara JM, Kim JW, Hankins JH, Weekes C, Hollingsworth MA, Serkova NJ, Sasson AR, Fleming JB, Oliveto JM, Lyssiotis CA, Cantley LC, Berim L, Singh PK. MUC1 and HIF-1alpha Signaling Crosstalk Induces Anabolic Glucose Metabolism to Impart Gemcitabine Resistance to Pancreatic Cancer. Cancer Cell. 2017;32:71-87.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 366] [Article Influence: 45.8] [Reference Citation Analysis (0)] |
| 3. | Yehya AHS, Asif M, Kaur G, Hassan LEA, Al-Suede FSR, Abdul Majid AMS, Oon CE. Toxicological studies of Orthosiphon stamineus (Misai Kucing) standardized ethanol extract in combination with gemcitabine in athymic nude mice model. J Adv Res. 2019;15:59-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Yehya AH, Asif M, Tan YJ, Sasidharan S, Majid AMA, Oon CE. Broad spectrum targeting of tumor vasculature by medicinal plants: An updated review. J Herb Med. 2017;169:13. [RCA] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Dhar D. Pancreatic cancer chemoprevention and intervention strategies employing a natural agent-bitter melon juice. University of Colorado at Denver, Anschutz Medical Campus. Strauss Health, 2018. Available from: https://digitalcollections.cuanschutz.edu/work/ns/46f7586e-f98e-459f-ab65-95fdd3a0bad5. |
| 6. | Qi F, Zhao L, Zhou A, Zhang B, Li A, Wang Z, Han J. The advantages of using traditional Chinese medicine as an adjunctive therapy in the whole course of cancer treatment instead of only terminal stage of cancer. Biosci Trends. 2015;9:16-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 323] [Article Influence: 32.3] [Reference Citation Analysis (0)] |
| 7. | Alissa EM. Medicinal herbs and therapeutic drugs interactions. Ther Drug Monit. 2014;36:413-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Tabana YM, Al-Suede FS, Ahamed MB, Dahham SS, Hassan LE, Khalilpour S, Taleb-Agha M, Sandai D, Majid AS, Majid AM. Cat's whiskers (Orthosiphon stamineus) tea modulates arthritis pathogenesis via the angiogenesis and inflammatory cascade. BMC Complement Altern Med. 2016;16:480. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Ahamed MB, Aisha AF, Nassar ZD, Siddiqui JM, Ismail Z, Omari SM, Parish CR, Majid AM. Cat's whiskers tea (Orthosiphon stamineus) extract inhibits growth of colon tumor in nude mice and angiogenesis in endothelial cells via suppressing VEGFR phosphorylation. Nutr Cancer. 2012;64:89-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Yehya AHS, Asif M, Petersen SH, Subramaniam AV, Kono K, Majid AMSA, Oon CE. Angiogenesis: Managing the Culprits behind Tumorigenesis and Metastasis. Medicina (Kaunas). 2018;54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 11. | Xue R, Fang Z, Zhang M, Yi Z, Wen C, Shi T. TCMID: Traditional Chinese Medicine integrative database for herb molecular mechanism analysis. Nucleic Acids Res. 2013;41:D1089-D1095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 300] [Cited by in RCA: 390] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 12. | Mahmood H, Khan IU, Asif M, Khan RU, Asghar S, Khalid I, Khalid SH, Irfan M, Rehman F, Shahzad Y, Yousaf AM, Younus A, Niazi ZR, Asim M. In vitro and in vivo evaluation of gellan gum hydrogel films: Assessing the co impact of therapeutic oils and ofloxacin on wound healing. Int J Biol Macromol. 2021;166:483-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 13. | Tanzeem MU, Asghar S, Khalid SH, Asif M, Ullah MS, Khan IU, Khalid I, Faran SA, Rehman A, Gohar UF, Hussain T. Clove oil based co-surfactant free microemulsion of flurbiprofen: Improved solubility with ameliorated drug-induced gastritis. Pak J Pharm Sci. 2019;32:2787-2793. [PubMed] |
| 14. | Mohamed EA, Lim CP, Ebrika OS, Asmawi MZ, Sadikun A, Yam MF. Toxicity evaluation of a standardised 50% ethanol extract of Orthosiphon stamineus. J Ethnopharmacol. 2011;133:358-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 15. | Shafaei A, Esmailli K, Farsi E, Aisha AF, Abul Majid AM, Ismail Z. Genotoxicity, acute and subchronic toxicity studies of nano liposomes of Orthosiphon stamineus ethanolic extract in Sprague Dawley rats. BMC Complement Altern Med. 2015;15:360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Féres CA, Madalosso RC, Rocha OA, Leite JP, Guimarães TM, Toledo VP, Tagliati CA. Acute and chronic toxicological studies of Dimorphandra mollis in experimental animals. J Ethnopharmacol. 2006;108:450-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Doig K. Introduction to increased destruction of erythrocytes. Rodak's Hematology-E-Book: Clinical Principles and Applications, 2015: 348. |
| 18. | Ou XM, Li WC, Liu DS, Li YP, Wen FQ, Feng YL, Zhang SF, Huang XY, Wang T, Wang K, Wang X, Chen L. VEGFR-2 antagonist SU5416 attenuates bleomycin-induced pulmonary fibrosis in mice. Int Immunopharmacol. 2009;9:70-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 54] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 19. | Von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, Seay T, Tjulandin SA, Ma WW, Saleh MN, Harris M, Reni M, Dowden S, Laheru D, Bahary N, Ramanathan RK, Tabernero J, Hidalgo M, Goldstein D, Van Cutsem E, Wei X, Iglesias J, Renschler MF. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369:1691-1703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4035] [Cited by in RCA: 4853] [Article Influence: 404.4] [Reference Citation Analysis (0)] |
| 20. | Vogl UM, Andalibi H, Klaus A, Vormittag L, Schima W, Heinrich B, Kafka A, Winkler T, Öhler L. Nab-paclitaxel and gemcitabine or FOLFIRINOX as first-line treatment in patients with unresectable adenocarcinoma of the pancreas: does sequence matter? BMC Cancer. 2019;19:28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 21. | Ashley C, Dunleavy A. The renal drug handbook: the ultimate prescribing guide for renal practitioners: CRC Press, 2017. |
| 22. | Ekstedt M, Hagström H, Nasr P, Fredrikson M, Stål P, Kechagias S, Hultcrantz R. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology. 2015;61:1547-1554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1353] [Cited by in RCA: 1693] [Article Influence: 169.3] [Reference Citation Analysis (1)] |
| 23. | Yehya AHS, Asif M, Abdul Majid AMS, Oon CE. Complementary effects of Orthosiphon stamineus standardized ethanolic extract and rosmarinic acid in combination with gemcitabine on pancreatic cancer. Biomed J. 2021;44:694-708. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Hoster E, Rosenwald A, Berger F, Bernd HW, Hartmann S, Loddenkemper C, Barth TF, Brousse N, Pileri S, Rymkiewicz G, Kodet R, Stilgenbauer S, Forstpointner R, Thieblemont C, Hallek M, Coiffier B, Vehling-Kaiser U, Bouabdallah R, Kanz L, Pfreundschuh M, Schmidt C, Ribrag V, Hiddemann W, Unterhalt M, Kluin-Nelemans JC, Hermine O, Dreyling MH, Klapper W. Prognostic Value of Ki-67 Index, Cytology, and Growth Pattern in Mantle-Cell Lymphoma: Results From Randomized Trials of the European Mantle Cell Lymphoma Network. J Clin Oncol. 2016;34:1386-1394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 211] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 25. | Fantini M, Benvenuto M, Masuelli L, Frajese GV, Tresoldi I, Modesti A, Bei R. In vitro and in vivo antitumoral effects of combinations of polyphenols, or polyphenols and anticancer drugs: perspectives on cancer treatment. Int J Mol Sci. 2015;16:9236-9282. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 210] [Cited by in RCA: 226] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 26. | Yan X, Li Y, Yu H, Wang W, Wu C, Yang Y, Hu Y, Shi X, Li J. Epigallocatechin-3-gallate inhibits H2O2-induced apoptosis in Mouse Vascular Smooth Muscle Cells via 67kD Laminin Receptor. Sci Rep. 2017;7:7774. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |