Published online Aug 21, 2022. doi: 10.3748/wjg.v28.i31.4456
Peer-review started: May 16, 2022
First decision: June 6, 2022
Revised: June 10, 2022
Accepted: July 25, 2022
Article in press: July 25, 2022
Published online: August 21, 2022
Processing time: 92 Days and 2.6 Hours
Low-grade myofibroblastic sarcoma (LGMS) is a rare malignant tumor. It has no specific clinical manifestations and commonly occurs in the head and neck, extremities and other body parts, with the liver not as its predisposing site.
We report a case report of a 58-year-old man with right upper abdominal pain for 11 d. Contrast-enhanced computed tomography (CECT), CE magnetic resonance imaging and CE ultrasound (US) all showed a cystic-solid mass in the right liver. As the initial clinical diagnosis was hepatic cystadenoma, surgical resection was performed, and the postoperative pathology indicated hepatic LGMS. The 3-mo follow-up showed favorable recovery of the patient. However, at 7-mo follow-up, two-dimensional US and CECT showed a suspected metastatic lesion in the right-middle abdomen.
Hepatic MS is particularly rare and easily misdiagnosed, more cases will contribute to the understanding and the diagnosis accuracy.
Core Tip: Myofibroblastic sarcoma (MS) is a rare malignant spindle-shaped cell tumor derived from mesenchymal tissue, and it is particularly rare in the liver. Pathological examination is the gold standard for the diagnosis of hepatic MS. There are different biological characteristics of different lesions and protocols for surgical treatment; therefore, we should pay attention to more information conducive to differential diagnosis in order to improve the preoperative diagnosis, and to choose an appropriate surgical approach.
- Citation: Li J, Huang XY, Zhang B. Low-grade myofibroblastic sarcoma of the liver misdiagnosed as cystadenoma: A case report. World J Gastroenterol 2022; 28(31): 4456-4462
- URL: https://www.wjgnet.com/1007-9327/full/v28/i31/4456.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i31.4456
Myofibroblastic sarcoma (MS) is a rare mesenchymal spindle-shaped cell tumor, first discovered by Mentzel et al[1] in 1998. According to the differential degree of myofibroblasts, it can be divided into low, intermediate and high grade. The first two are collectively called low-grade MS (LGMS)[2]. MS is common in the head and neck, limbs and trunk, but it is extremely rare in the liver. So far, there are only four English language reports available. Here, we present a case of LGMS of the liver.
Right upper abdominal pain for 11 d.
A 58-year-old Chinese man presented with right upper abdominal pain without obvious predisposing factors 11 d prior to the visit. The symptom was not associated with eating and body position. He experienced no nausea or vomiting, no chills or fever, and no significant weight loss.
Right inguinal hernia surgery had been performed at another hospital 3 years prior to the present visit.
No history of hepatitis and family or genetic history was claimed.
Physical examination showed a flat and soft abdomen without tenderness and rebound pain, and no palpable mass was found. The rest of the physical examination showed no abnormalities.
Cholesterol (5.3 mmol/L) and low density lipoprotein (3.78 mmol/L) were elevated. Routine blood, liver function, renal function and prothrombin tests were normal. Complete quantitative detection of hepatitis B was negative. Alpha-fetoprotein (AFP), carcinoembryonic antigen (CEA) and carbohydrate antigen 19-9 (CA19-9) were normal.
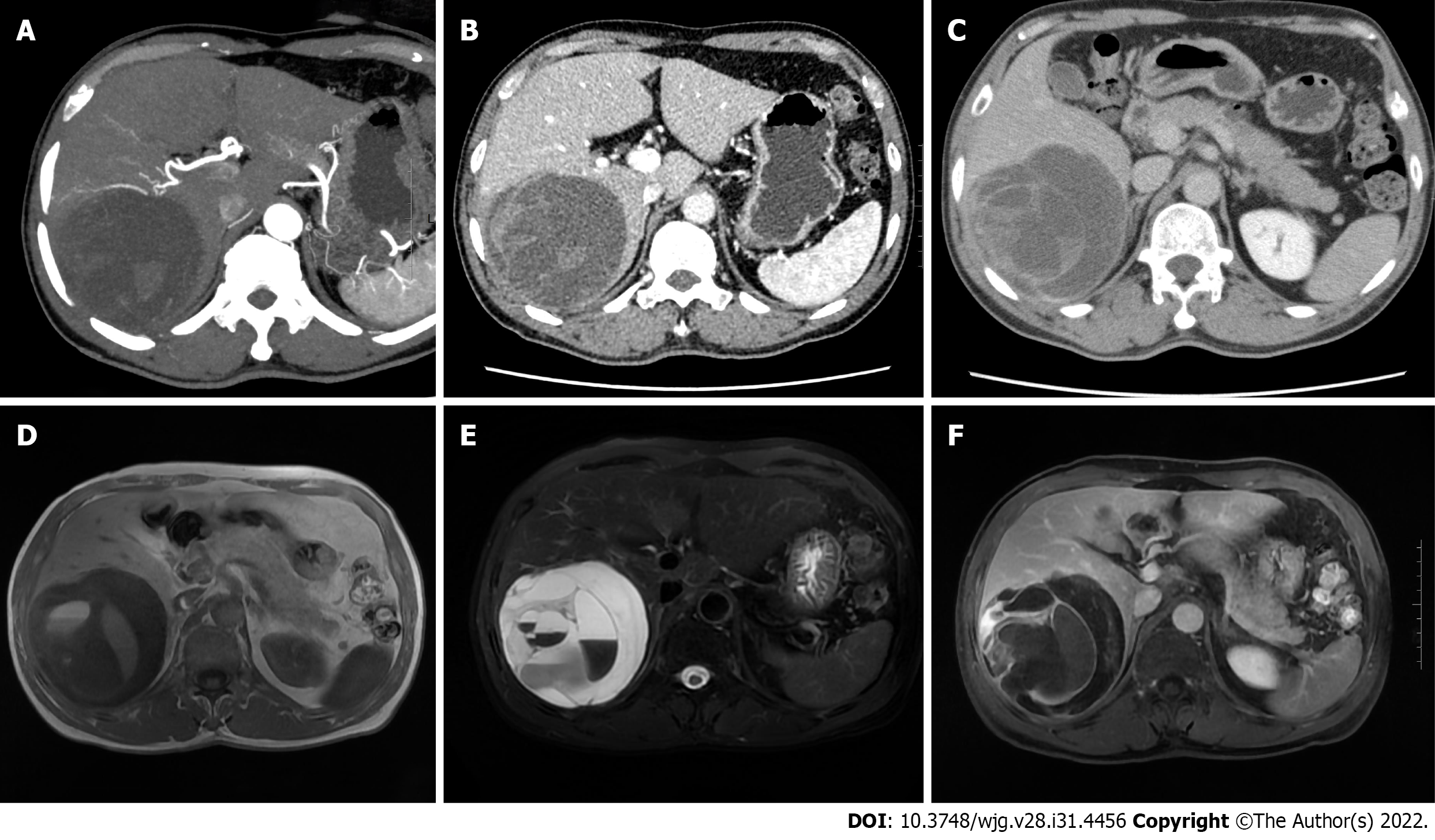
Abdominal contrast-enhanced computed tomography (CECT) and hepatic vascular imaging showed that there was a cystic-solid hypodense mass with a size of approximate 99 mm × 92 mm in the right liver. Septa, which were slightly enhanced along with the solid parenchyma, were visible in the mass. The right hepatic vein was displaced due to the compression of the mass supplied by the right hepatic artery (Figure 1A-C). Abdominal CE-magnetic resonance imaging and diffusion-weighted imaging (DWI) showed: (1) A cystic-solid mass with low signal on T1-weighted imaging and high signal on T2-weighted imaging in the right liver, about 101 mm × 98 mm in size; (2) multiple uneven septa and fluid-fluid levels in the lesion; (3) DWI and apparent diffusion coefficient showed high signal and high B value, respectively; and (4) after enhancement, solid components and internal septa of the tumor were significantly enhanced accompanied by unenhanced cystic components (Figure 1D-F).
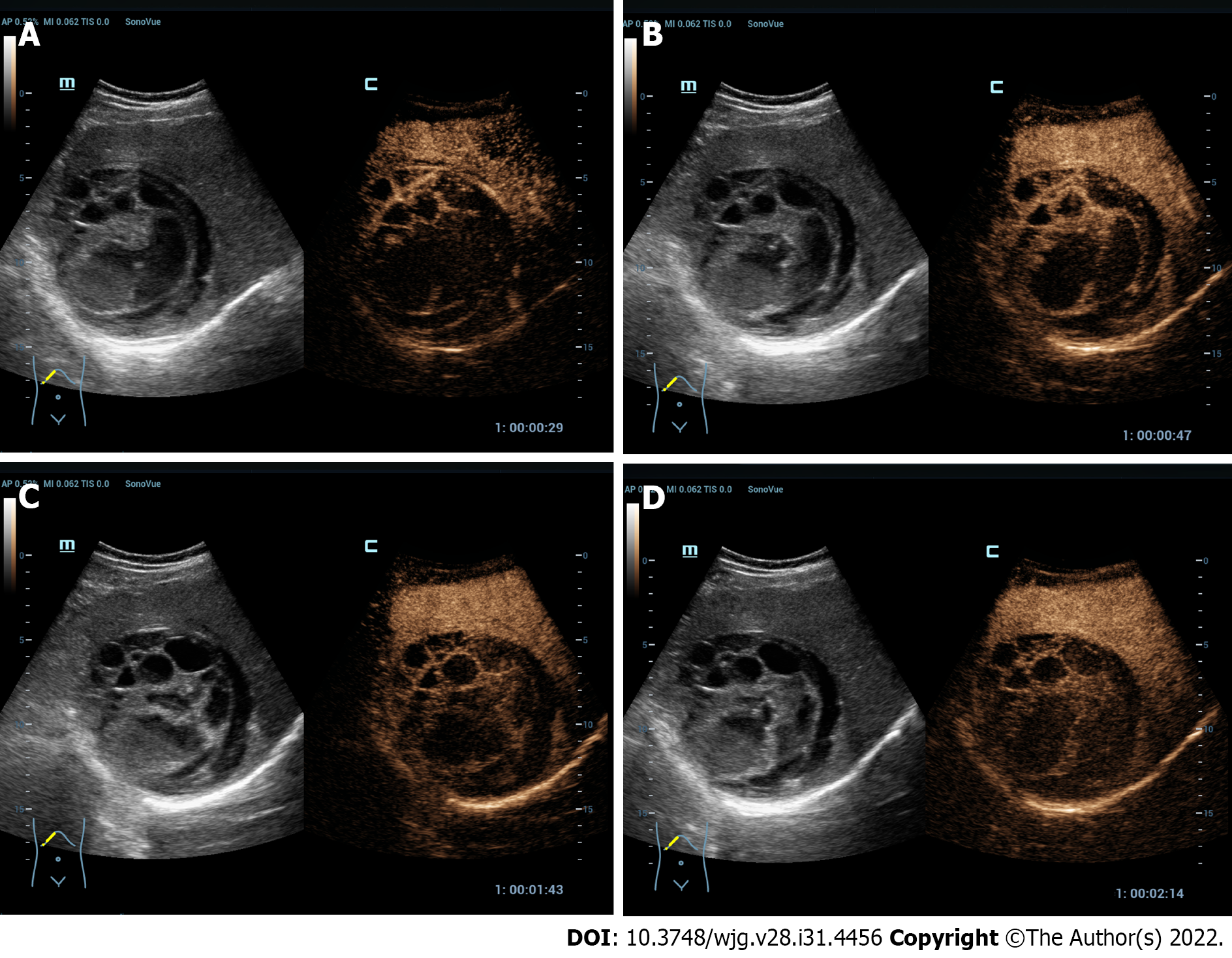
Ultrasound (US) examination showed a 123 mm × 98 mm mixed-echo mass with regular shape and clear boundary in the right liver. The anechoic dark area was the main portion of the mass. The parenchymatous septa with uneven thickness were visible in the mass in which no obvious parasitic body sonogram was found. Color Doppler flow imaging showed punctate blood flow signals in the mass. CEUS showed that the peripheral and internal septa of the tumor were hyper-enhanced in the arterial phase, iso-enhanced in the portal and delayed phases, and unenhanced in the anechoic area in these three phases (Figure 2). Based on the above-mentioned examination, the mass was preliminarily identified as hepatic cystadenoma.
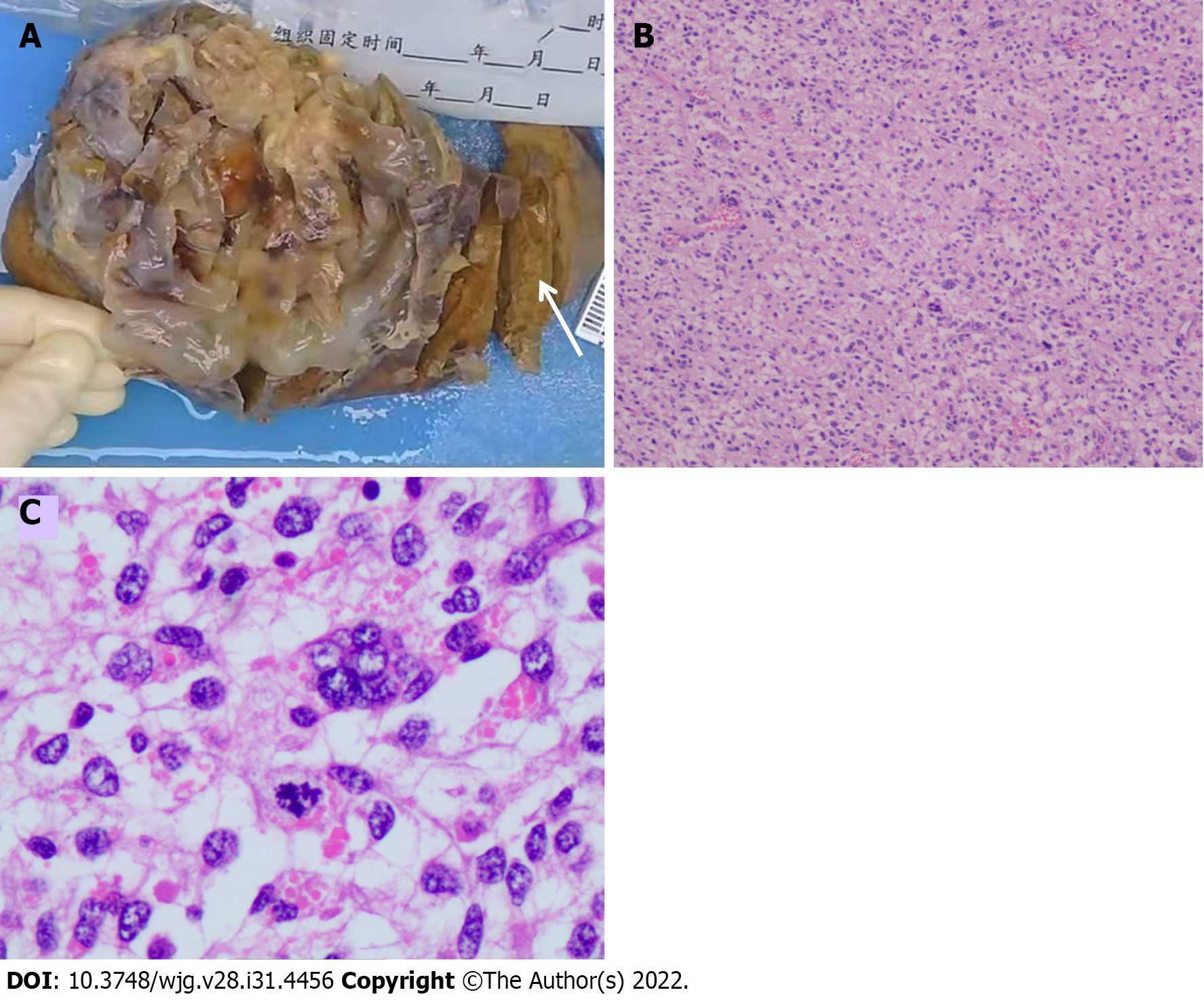
The postoperative pathology diagnosis of the presented case is LGMS of right liver (Figure 3).
The patient underwent laparoscopic right hepatectomy under general anesthesia after preoperative investigations were completed.
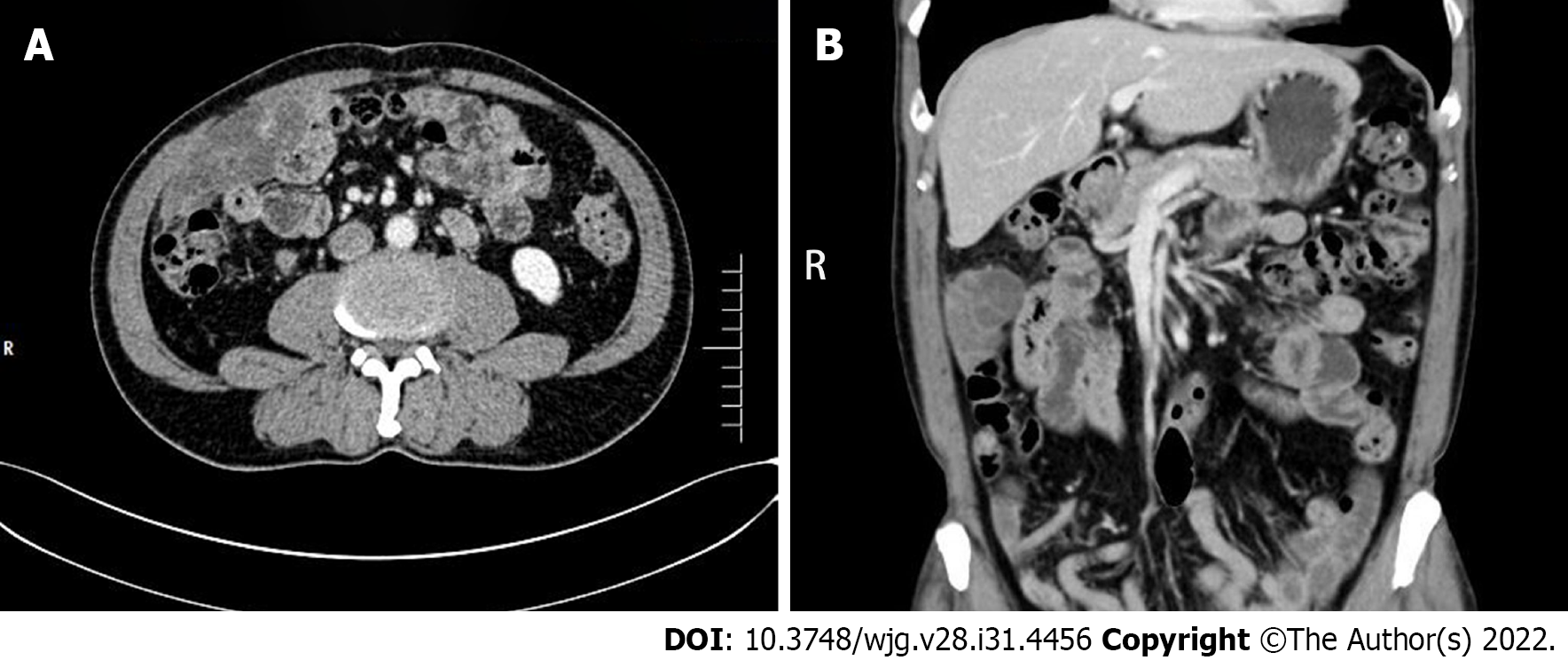
The patient recovered well after the operation with the surgical incision healed uneventfully. No apparent event was observed at the postoperative 3-mo follow-up. However, at the 7-mo follow-up, two-dimensional ultrasound and CECT showed a 100 mm × 40 mm cystic-solid lesion occurring in the right middle abdomen, which showed similar properties to a liver lesion. The mass wall was enhanced after enhancement (Figure 4). The patient refused further surgery although the clinician initially believed that metastasis had probably occurred.
MS is a rare histological type of hepatic sarcoma. Given its rarity, the etiology is not clear, and most of the relevant reports are case reports or case series. Only seven relevant case reports[3-9] were obtained after a comprehensive literature search was conducted by us in CNKI, PubMed and Web of Science databases, involving seven patients (four men, three women; aged 25–38 years, n = 5; > 60 years, n = 2). As described in the WHO classification, males are slightly more predisposed for this disease than females; thus, not surprisingly, the present case was male. Most of the MSs were identified due to the swelling lesion detected or during physical examination. In the literature reports, five of the seven patients presented with abdominal distension and pain, and another two were asymptomatic. As for the present patient, the complaint was right upper abdominal pain. He had no history of hepatitis, although two of the seven patients reported previously had a history of hepatitis B. Serological examination, such as routine blood, liver function, renal function, and AFP and other tumor markers such as CEA, CA19-9 (all of which were in the normal range), was available for six of the seven patients reported previously and for the patient reported here. The remaining patient reported previously had impaired liver function. The lesions reported were mostly located in the right liver, and cystic-solid tumor was found in five cases, but no relevant data were available for the other two cases. For the present case, a cystic-solid tumor located in the right liver was also observed. Among the seven cases reported previously, five were misdiagnosed as liver cancer or hydatid disease as their preliminary clinical diagnosis, while the present case was misdiagnosed as hepatic cystadenoma. Surgical resection was performed in six of the seven patients, and liver lesions were found and biopsy was performed at 3 mo after surgery for the remaining patient initially diagnosed with retroperitoneal inflammatory myofibroblastic tumor. The pathological diagnosis for the current patient was LGMS infiltrated in the liver. Currently, surgical resection of MS is the preferred treatment, although primary treatment, prognosis and follow-up treatment are not clear. More data are needed to obtain reliable conclusions about the role of follow-up treatment such as radiotherapy and chemotherapy.
No specific clinical signs and symptoms were established currently due to the low incidence of hepatic MS, which was generally manifested as abdominal distension or discomfort and/or abnormal liver function, sometimes accompanied by sweating and weight loss. Although there was no clear report on tumor recurrence and metastasis, most hepatic MSs were observed as cystic-solid masses, showing infiltrative and destructive growth.
At present, hepatic MS is mainly diagnosed by histopathology and immunohistochemistry. Under light microscopy, the tumor tissue of the present case was mainly composed of spindle-shaped cells with a diffuse infiltrative distribution. The cytoplasm was eosinophilic and the nucleus was polymorphic. Abnormal mitotic figures were present. The histopathological findings of this case are consistent with those previously reported. In the immunohistochemical study of the cases reported previously, expression of vimentin, smooth muscle actin (SMA) and desmin was commonly observed, along with partially positive actin. No hepatocyte markers, epithelial markers, S100, CD117, CD34, myogenin, pan-cytokeratin (CK-Pan) and h-caldesmon were not found in the tissue[10]. In the of the case reported here, immunohistochemical study was positive for vimentin, SMA and desmin, and negative for HePar-1, Glypican-3, CK-Pan, myogenin, Ard-1, MYOD1, SOX10 and CD31, with an approximately 10% Ki-67 index. As can be seen, the present case is mostly similar to those reported previously for this profile.
To date, due to lack of specific manifestations in imaging examinations, hepatic MS is easily misdiagnosed as liver cancer, hepatic hydatid disease, cystadenoma and other space-occupying lesions, and it is difficult to make a diagnosis in clinical practice as well. The hepatic MS reported here was mainly observed as a cystic-solid mass with well-defined borders and regular morphology. The cystic components within the mass were separated by septa of varying thickness, with a partially visible fluid-fluid levels. After enhancement, the solid portion and septa of the mass were enhanced to different degrees, with inconspicuous regression for the degree and velocity.
CEUS of this case showed that the peripheral and internal septa of the tumor were hyper-enhanced in the arterial phase, isoenhanced in the portal and delayed phases, while in two of the seven cases reported in the literature, the portal and delayed phases were hypo-enhanced. Hence, the CEUS features of hepatic MS require more case data.
Hepatic MS needs to be differentiated from liver cancer (particularly with liquefaction and necrosis), hepatic hydatid disease, and cystadenoma. When liver cancer is accompanied by liquefaction and necrosis, three-phase non-enhanced areas in the lesions may also be found, but most of them are patchy or irregular. Moreover, the substantial portion of the mass shows high enhancement in the arterial phase, and low enhancement in the portal and delayed phases. The process behaves in a fast-in and fast-out mode. In contrast, the non-enhancing area of hepatic MS lesions was separated by the internal septa of the mass, and the parenchyma and internal septa of the mass were not significantly regressed after enhancement. Patients with liver hydatid disease generally have a history of living in pastoral areas or exposure to pathogens. The typical imaging manifestations are mainly cystic masses, showing the mother and daughter sporocysts, with varying degrees of eggshell-like cyst wall calcification, intracystic streamer sign, lily sign, and cyst-within-cyst. Liver cystadenomas are cystic-solid masses with predominantly cystic components, along with mural nodules (papillary-solid components protruding into the cystic cavity on the cyst wall) as specific signs. Mural nodules show nodular enhancement in the portal phase and can continue to enhance in the delayed phase. Imaging examination can clearly show the size, location, border, number, blood supply, and internal and surrounding adjacent tissues of the tumor. However, there is currently no characteristic diagnostic basis for the imaging manifestations of hepatic MS.
The presented case was misdiagnosed for several reasons. First, the patient had no specific clinical history, presentation and abnormal laboratory indexes. Second, the preoperative imaging images were similar to those of cystadenoma. The internal separation of the mass was uniform, the blood flow of the mass was not abundant, and there was no washout after enhancement. Therefore, imaging diagnosis was limited to benign lesions, and malignant behavior was not considered.
In summary, MS of the liver has no characteristic manifestations in clinical performance, serological indicators and imaging findings. Therefore, there is a need to accumulate a large number of cases with complete data to provide meaningful research data for the diagnosis and treatment strategies of MS of the liver.
Due to the rarity of hepatic MS, more clinical data and in-depth research are needed to further analyze its pathological mechanism, biomarkers, and imaging manifestations. Improving the understanding of the imaging manifestations of hepatic MS will help improve the preoperative diagnosis rate and assist clinicians in performing precise surgical resection and follow-up treatment.
We are very grateful to Dr. Jiang Jia-Rui (Department of Pathology, Xiangya Hospital, Central South University) for providing professional guidance to the pathological analysis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: El-Gendy HA, Egypt; Samizadeh B, Iran S-Editor: Chen YL L-Editor: Kerr C P-Editor: Chen YL
| 1. | Mentzel T, Dry S, Katenkamp D, Fletcher CD. Low-grade myofibroblastic sarcoma: analysis of 18 cases in the spectrum of myofibroblastic tumors. Am J Surg Pathol. 1998;22:1228-1238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 192] [Article Influence: 7.1] [Reference Citation Analysis (1)] |
| 2. | Montgomery E, Fisher C. Myofibroblastic differentiation in malignant fibrous histiocytoma (pleomorphic myofibrosarcoma): a clinicopathological study. Histopathology. 2001;38:499-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 50] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Fang Y, Yan T, Bi X, Zhang H, Zhou J, Huang Z, Xie Y, Zhang L, Zhao P, Cai J. Clinicopathological and immunohistochemical study of low-grade myofibroblastic sarcoma of the liver-One case report. Zhongliu Yanjiu Yu Linchuang. 2011;8:250-253. [DOI] [Full Text] |
| 4. | Pan Y, Wu X, Liu J, Muheremu A. Abnormal liver function induced by myofibroblastic sarcoma infiltrating the liver: A case report. Oncol Lett. 2015;9:798-800. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Yi X, Xiao D, Long X. Myofibroblastic sarcoma in liver: a case report. Int J Clin Exp Pathol. 2015;8:1073-1076. [PubMed] |
| 6. | Wen J, Zhao W, Li C, Shen JY, Wen TF. High-grade myofibroblastic sarcoma in the liver: A case report. World J Gastroenterol. 2017;23:7054-7058. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Yan T, Bi X Y, Zhang H T, Zhao J J, Zhang L, Huang Z, Zhou H T, Li C, Cai J Q. A case of malignant myofibroblastic sarcoma of the liver. Zhongguo Zhongliu Zazhi. 2011;33:477-478. [DOI] [Full Text] |
| 8. | Zhang J Y, Luo Y. Contrast-enhanced ultrasonographic manifestations of hepatic myofibroblastic sarcoma: a case report. Linchuang Chaosheng Yixue Zazhi. 2021;23:80. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Chen L G, Li J. A case of spontaneous rupture of liver myofibroblastic sarcoma. Zhongguo Gandan Waike Zazhi. 2021;27:218-219. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Jo VY, Fletcher CD. WHO classification of soft tissue tumours: an update based on the 2013 (4th) edition. Pathology. 2014;46:95-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 505] [Cited by in RCA: 671] [Article Influence: 61.0] [Reference Citation Analysis (0)] |