Published online Jul 28, 2022. doi: 10.3748/wjg.v28.i28.3739
Peer-review started: October 30, 2021
First decision: April 16, 2022
Revised: May 4, 2022
Accepted: July 11, 2022
Article in press: July 11, 2022
Published online: July 28, 2022
Processing time: 269 Days and 12.1 Hours
Pneumatosis intestinalis (PI) is defined as the presence of gas within the submucosal or subserosal layer of the gastrointestinal tract. It is a radiologic sign suspicious for bowel ischemia, hence non-viable bowel must be ruled out in patients with PI. However, up to 15% of cases with PI are not associated with bowel ischemia or acute abdomen. We described an asymptomatic patient with prednisolone-induced PI and modified the Naranjo score to aid in a surgeon’s decision-making for emergency laparotomy vs non-operative management with serial assessment in patients who are immunocompromised due to long-term steroid use.
Core Tip: We described an asymptomatic patient with prednisolone-induced pneumatosis intestinalis and modified the Naranjo score to aid in a surgeon’s decision-making for emergency laparotomy vs non-operative management with serial assessment in patients who are immunocompromised due to long-term steroid use.
- Citation: Goh SSN, Shelat V. Prednisolone induced pneumatosis coli and pneumoperitoneum. World J Gastroenterol 2022; 28(28): 3739-3742
- URL: https://www.wjgnet.com/1007-9327/full/v28/i28/3739.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i28.3739
We read with interest the report by Azzaroli et al[1], who conservatively managed two patients with benign pneumatosis intestinalis (PI). We would like to share a similar clinical case with prednisolone-induced pneumatosis coli and propose a modified Naranjo score for prednisolone-induced pneumatosis.
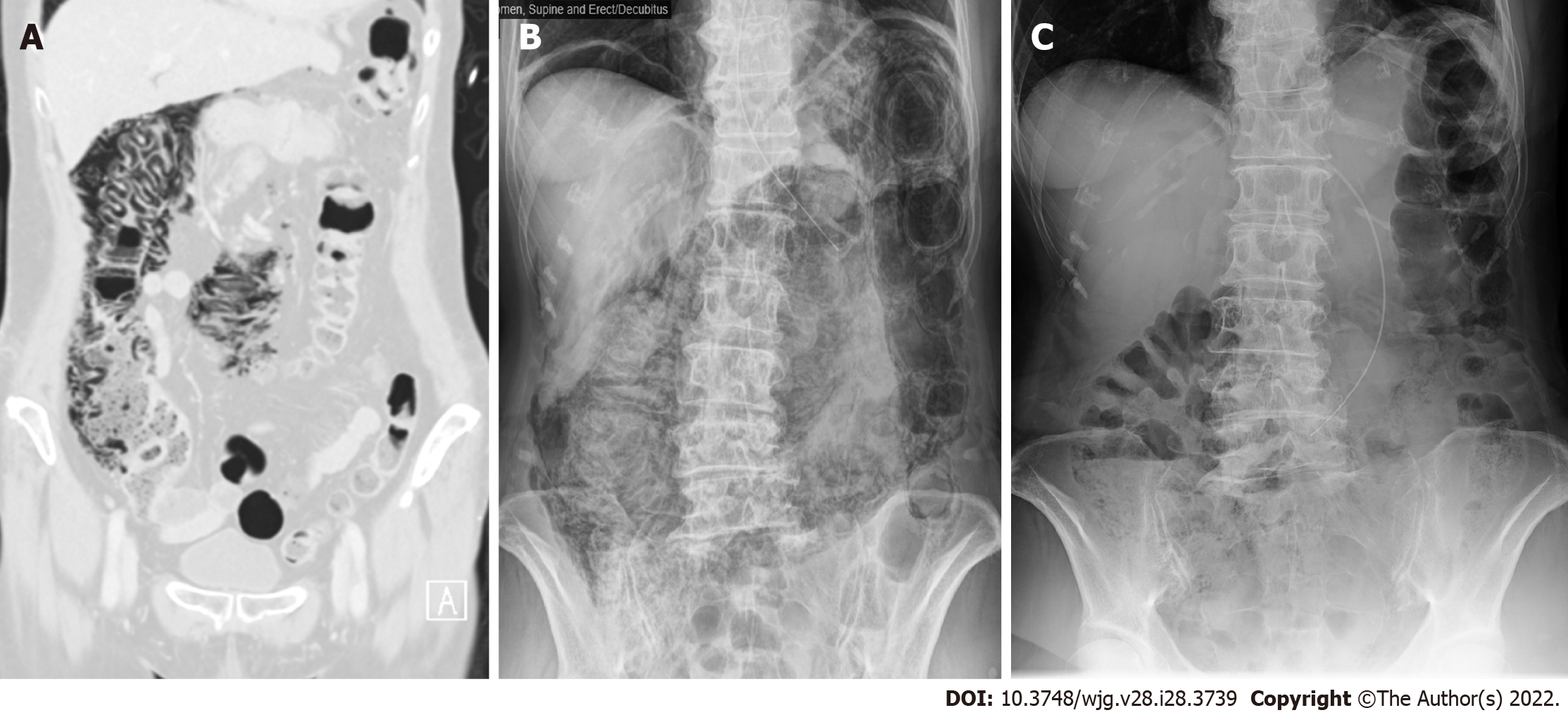
A 71-year-old lady with dysphagia and diplopia symptoms was diagnosed with Neuromyelitis Optica (NMO). Treatment with prednisolone 20 mg once daily improved her diplopia. Nasogastric tube (NGT) feeding was commenced due to malnourishment from dysphagia. The chest radiograph for NGT placement showed pneumoperitoneum, and she was referred urgently to the surgical unit. She was asymptomatic, afebrile with normal hemodynamics. Abdomen was soft and non-tender. Leukocyte count, procalcitonin, lactate, and arterial blood gas were normal. A computed tomography of abdomen and pelvis (CTAP) with intravenous and NGT contrast confirmed pneumoperitoneum and pneumatosis coli from cecum to splenic flexure (Figure 1). There was no contrast extravasation, portal venous gas, inflammatory pathology, or mesenteric ischemia. Non-operative management with nil enteral feeding, serial abdominal examination, serum tests, and abdominal radiographs (AXR) was done. The patient remained asymptomatic with normal serum tests. A repeat CTAP showed minimal improvement of pneumoperitoneum. A follow-up AXR two weeks later showed worsening of pneumatosis coli. Hyperbaric oxygen therapy (HBOT) was arranged. Five HBOT sessions were performed at 2.2 atmospheric pressure for 90 min. Her abdominal girth reduced from 79 to 73 cm with minimal AXR improvement. Prednisolone was weaned over next five days and she was discharged well on oral diet. At two-weeks outpatient follow-up, AXR showed improvement (Figure 1).
Corticosteroid therapy remains the cornerstone for the treatment of autoimmune diseases. The true incidence of benign PI as an ADR secondary to corticosteroids is unknown[2,3]. The hypothesis is due to atrophy of lymphoid follicles in the bowel wall. Although PI occurred after prednisolone's commencement in our patient, we did not initially stop prednisolone in balancing risk vs benefits for NMO therapy. When PI worsened, HBOT was offered due to concerns for secondary bowel ischemia from PI. The HBOT regimen was similar to that described by Feuerstein et al[4], who suggested at least three sessions. As our patient's PI improved but did not resolve fully after 5 HBOT sessions, we reduced prednisolone dose. After two weeks of cessation, PI resolved, similar to a report described by Choi et al[5].
According to the Naranjo score (adverse drug reaction probability scale) of 6, PI was probably caused by prednisolone in our patient. Naranjo score recommends isolation of drug in toxic concentrations in body fluid, response to placebo administration, and drug rechallenge to evaluate for the occurrence of symptoms. These three criteria are not routinely done due to practical and safety reasons[6]. We propose a modified Naranjo score (Tables 1 and 2) for prednisolone-induced pneumatosis which replaces these three criteria with the following: (1) No symptoms or signs of abdominal pathology; (2) Serum investigations for inflammatory markers (e.g., C-reactive protein and procalcitonin) must be normal; and (3) Imaging studies should rule out hollow viscus perforation or inflammatory abdominal pathology as a cause for PI. With the modified Naranjo score, the causal link of PI due to prednisolone becomes definite. We propose validation of modified Naranjo score.
| Question | Yes/No/Do not know | Score |
| Are there previous conclusive reports on this reaction? | Yes | 1 |
| Did the adverse event appear after the suspected drug was administered? | Yes | 2 |
| Did the adverse reaction improve when the drug was discontinued, or a specific antagonist was administered? | Yes | 1 |
| Are there alternative causes (other than the drug) that could on their own have caused the reaction? | No | 0 |
| Was the reaction more severe when the dose was increased or less severe when the dose was decreased? | Yes | 1 |
| Did the patient have a similar reaction to the same or similar drugs in any previous exposure? | No | 0 |
| Did any objective evidence confirm the adverse event? | Yes | 1 |
| Were there any symptoms or signs of abdominal pathology? (instead of isolation of drug in toxic concentrations in body fluid) | No | 1 |
| Were the serum inflammatory markers normal? (instead of drug rechallenge to evaluate for reoccurrence of symptoms) | Yes | 1 |
| Did imaging studies rule out hollow viscus perforation or inflammatory abdominal organ pathology? (instead of response to placebo administration) | Yes | 1 |
| Total score | 9 (definite) | |
| Total score | Interpretation of scores |
| ≥ 9 | Definite |
| 5 to 8 | Probable |
| 1 to 4 | Possible |
| ≤ 0 | Doubtful |
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Singapore
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Lassandro F, Italy S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Azzaroli F, Turco L, Ceroni L, Galloni SS, Buonfiglioli F, Calvanese C, Mazzella G. Pneumatosis cystoides intestinalis. World J Gastroenterol. 2011;17:4932-4936. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 45] [Cited by in RCA: 49] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Berritto D, Crincoli R, Iacobellis F, Iasiello F, Pizza NL, Lassandro F, Musto L, Grassi R. Primary pneumatosis intestinalis of small bowel: a case of a rare disease. Case Rep Surg. 2014;2014:350312. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Paradkar S. Reported Adverse Drug Reactions During the Use of Corticosteroids in a Tertiary Care Hospital. Ther Innov Regul Sci. 2019;53:128-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Feuerstein JD, White N, Berzin TM. Pneumatosis intestinalis with a focus on hyperbaric oxygen therapy. Mayo Clin Proc. 2014;89:697-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 5. | Choi JY, Cho SB, Kim HH, Lee IH, Lee HY, Kang HS, Lee SY. Pneumatosis intestinalis complicated by pneumoperitoneum in a patient with asthma. Tuberc Respir Dis (Seoul). 2014;77:219-222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Shelat VG. Sulfasalazine induced acute pancreatitis in a patient with prior cholecystectomy. Postgrad Med J. 2021;97:738-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |