Published online May 21, 2022. doi: 10.3748/wjg.v28.i19.2148
Peer-review started: December 16, 2021
First decision: January 27, 2022
Revised: February 1, 2022
Accepted: April 9, 2022
Article in press: April 9, 2022
Published online: May 21, 2022
Processing time: 151 Days and 22.2 Hours
The association between type 2 diabetes mellitus (DM) and colorectal cancer (CRC) has been thoroughly investigated and reports have demonstrated that the risk of CRC is increased in DM patients. The association between DM and the survival of patients with CRC is controversial. Evidence suggests that metformin with its anti-inflammatory effects is a protective factor against the development of CRC among DM patients and that metformin therapy is associated with a better prognosis in patients with DM. In our cohort, we did not find any associations between the presence of DM or metformin and cancer specific survival or any relation to plasma levels of a panel of 40 inflammatory factors and irisin. On the other hand, we identified that the insulin-like growth factor binding protein 7 single nucleotide polymorphism rs2041437 was associated with DM in CRC patients. The dominance of the T bearing genotypes in patients with DM was statistically significant (P = 0.038), with an odds ratio of 1.66 (95% confidence interval: 1.03-2.69).
Core Tip: Type 2 diabetes mellitus (DM) or metformin treatment does not influence mortality in colorectal cancer (CRC). Type 2 DM or metformin does not influence the levels of inflammatory factors in plasma in patients with CRC. Single nucleotide polymorphisms of insulin-like growth factor binding protein 7 are associated with type 2 DM in patients with CRC.
- Citation: Dimberg J, Shamoun L, Landerholm K, Wågsäter D. Effects of diabetes type 2 and metformin treatment in Swedish patients with colorectal cancer. World J Gastroenterol 2022; 28(19): 2148-2151
- URL: https://www.wjgnet.com/1007-9327/full/v28/i19/2148.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i19.2148
Having read the article “How far along are we in revealing the connection between metformin and colorectal cancer?” by Cigrovski Berkovic et al[1] in World Journal of Gastroenterology 2021, we want to contribute with some aspects and data on this matter.
Colorectal cancer (CRC) is one of the most common cancer types worldwide and several genetic pathways affecting CRC initiation and progression have been described[2]. The association between type 2 diabetes mellitus (DM) and CRC has been thoroughly investigated and reports have demonstrated that the risk of CRC is higher in DM patients[3]. However, the association between DM and the survival of patients with CRC is controversial[4,5].
Metformin is an oral glucose-lowering agent used to treat DM. It has also been reported to possess properties that inhibit the proliferation and growth of certain types of cancer[6]. Moreover, recent studies show that metformin has anti-inflammatory effects, a property that can be beneficial in conditions other than DM, such as cardiovascular disease and cancer[7].
Overall, evidence suggests that metformin could protect against the development of CRC among DM patients and that metformin therapy is associated with a better prognosis in patients with DM[1,6,8]. However, this protective role of metformin in CRC remains controversial[1,8]. In light of the above and with special reference to a report by Cigrovski Berkovic et al[1], we here add our observations of CRC patients (n = 408) without DM (n = 310) or with DM (n = 98), treated with metformin (n = 63) or not (n = 35), and any associations of these factors with cancer-specific survival, inflammatory factors, or single nucleotide polymorphisms (SNPs).
Blood samples were obtained from all consecutive CRC patients who underwent surgical resection for primary colorectal adenocarcinomas between 2006 and 2019 at the Department of Surgery, Ryhov County Hospital, Jönköping, Sweden. Follow-up for the estimation of cancer-specific survival ended on the date of death or on February 23, 2021. The patient data have been prospectively recorded in a database, comprising 236 males and 172 females with a mean age of 71 years. The study included 172 patients with rectal cancer and 236 patients with colon cancer, based on the primary tumor site. The tumors were classified as stage I in 63 patients, stage II in 148, stage III in 148, and stage IV in 49. The study was approved by the Regional Ethical Review Board in Linköping, Sweden, and informed consent was obtained from each participant.
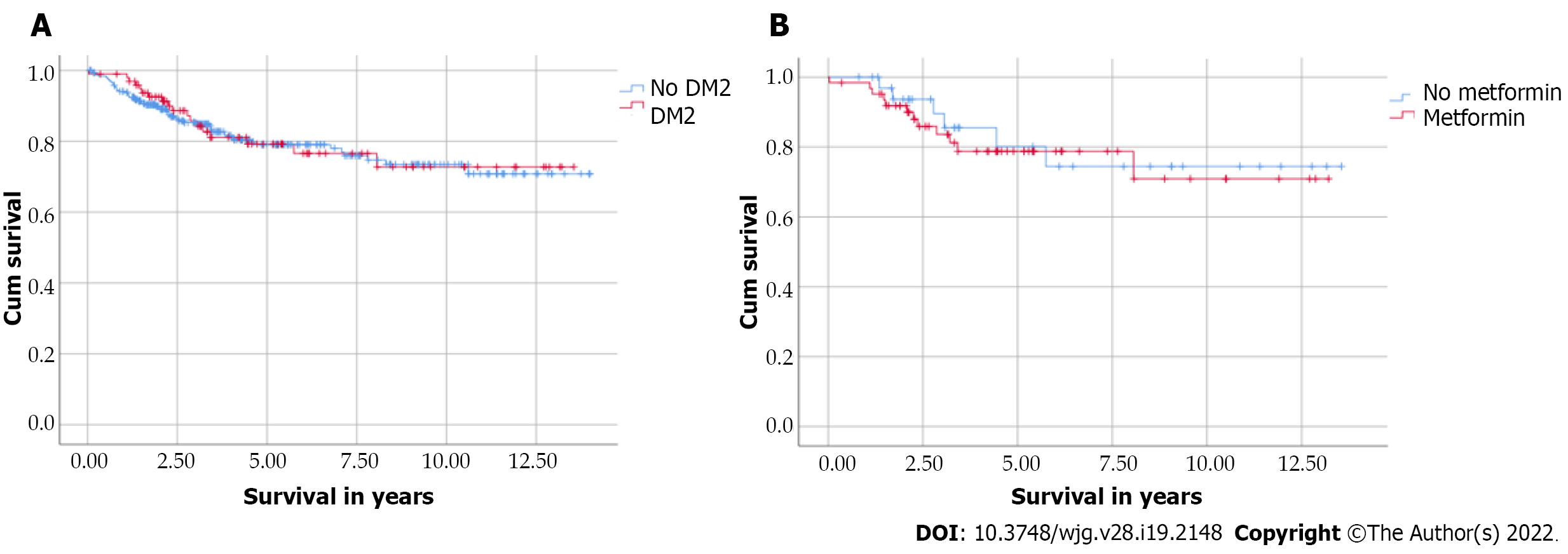
We did not find any relationships between the presence of DM or metformin and cancer-specific survival in patients with CRC in our cohort, as demonstrated by Kaplan-Maier curves (Figure 1). Receiver operating characteristic curve analysis confirmed this result (data not shown).
Against the background that inflammation has a driving force in carcinogenesis of CRC[2] and that metformin has anti-inflammatory effects, we have applied data that we have previously published in World J Gastroenterology[9] regarding a panel of 40 circulating inflammatory factors in a cohort of 174 CRC patients, of whom 44 had DM and 17 were treated with metformin. We found that plasma levels of these factors did not differ between CRC patients with or without DM, whether treated with metformin or not (data not shown). This was also the case when similar analyses were performed regarding carcinoembryonic antigen (CEA) levels, which were available for 332 of the patients.
Irisin is a relatively recently discovered hormone (myokine) that is involved in the regulation of metabolic processes such as stimulation of glycogenesis and inhibition of glycogenolysis and has been suggested to play an important role in DM[10]. However, studies have reported both decreased and increased irisin levels in DM patients[10]. In a clinical study, Zhu et al[11] showed reduced serum levels of irisin in CRC patients and suggested that irisin might be used as a serum diagnostic marker. In our analysis, we found no general difference in cancer-specific survival depending on the levels of irisin. Nor were differences in cancer-specific survival observed in those with or without DM and with or without metformin treatment.
Insulin-like growth factor-binding protein 7 (IGFBP 7) binds strongly to insulin and has been found, by us[12] and others[13], to be increased in CRC tissue. Moreover, we have investigated the IGFBP 7 SNP rs2041437 (C > T) in relation to CRC development[12]. When adding further CRC patients (n = 340) to the earlier study, we found that the rate of the CC genotype was 45.4% and that of CT/TT was 54.6% among patients without DM, while they were 33.3% and 66.7%, respectively, in patients with DM. The dominance of the T-bearing genotypes in patients with DM was statistically significant (P = 0.038), with an odds ratio of 1.66 (95% confidence interval: 1.03-2.69).
In summary, our data do not support the hypothesis that DM increases mortality in CRC or that metformin prevents death from CRC, at least in patients in Swedish healthcare. We could not see any association between circulatory inflammatory factors, irisin, or CEA levels and DM or metformin among CRC patients. On the other hand, we identified that the IGFBP 7 SNP rs2041437 was associated with DM in CRC patients. It should be pointed out that patients with metformin treatment were relatively few, rendering interpretation of data regarding this group uncertain.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Sweden
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Liu J, China; Wang QY, China; Wu QN, China S-Editor: Chen YL L-Editor: Wang TQ P-Editor: Chen YL
| 1. | Berkovic MC, Mikulic D, Bilic-Curcic I, Mrzljak A. How far along are we in revealing the connection between metformin and colorectal cancer? World J Gastroenterol. 2021;27:1362-1368. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Ahmad R, Singh JK, Wunnava A, Al-Obeed O, Abdulla M, Srivastava SK. Emerging trends in colorectal cancer: Dysregulated signaling pathways (Review). Int J Mol Med. 2021;47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 107] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 3. | Larsson SC, Orsini N, Wolk A. Diabetes mellitus and risk of colorectal cancer: a meta-analysis. J Natl Cancer Inst. 2005;97:1679-1687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 719] [Cited by in RCA: 752] [Article Influence: 37.6] [Reference Citation Analysis (0)] |
| 4. | Noh GY, Hwang DY, Choi YH, Lee YY. Effect of diabetes mellitus on outcomes of colorectal cancer. J Korean Soc Coloproctol. 2010;26:424-428. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Mills KT, Bellows CF, Hoffman AE, Kelly TN, Gagliardi G. Diabetes mellitus and colorectal cancer prognosis: a meta-analysis. Dis Colon Rectum. 2013;56:1304-1319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 151] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 6. | Yu H, Zhong X, Gao P, Shi J, Wu Z, Guo Z, Wang Z, Song Y. The Potential Effect of Metformin on Cancer: An Umbrella Review. Front Endocrinol (Lausanne). 2019;10:617. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 89] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 7. | Bai B, Chen H. Metformin: A Novel Weapon Against Inflammation. Front Pharmacol. 2021;12:622262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 83] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 8. | Wang Q, Shi M. Effect of metformin use on the risk and prognosis of colorectal cancer in diabetes mellitus: a meta-analysis. Anticancer Drugs. 2022;33:191-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Olsen RS, Nijm J, Andersson RE, Dimberg J, Wågsäter D. Circulating inflammatory factors associated with worse long-term prognosis in colorectal cancer. World J Gastroenterol. 2017;23:6212-6219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 32] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 10. | Mahgoub MO, D'Souza C, Al Darmaki RSMH, Baniyas MMYH, Adeghate E. An update on the role of irisin in the regulation of endocrine and metabolic functions. Peptides. 2018;104:15-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 71] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 11. | Zhu H, Liu M, Zhang N, Pan H, Lin G, Li N, Wang L, Yang H, Yan K, Gong F. Serum and Adipose Tissue mRNA Levels of ATF3 and FNDC5/Irisin in Colorectal Cancer Patients With or Without Obesity. Front Physiol. 2018;9:1125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 12. | Mälarstig A, Wågsäter D, Löfgren S, Hugander A, Zar N, Dimberg J. Tumour-derived adhesion factor in colorectal cancer. Mol Med Rep. 2009;2:971-976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Jin L, Shen F, Weinfeld M, Sergi C. Insulin Growth Factor Binding Protein 7 (IGFBP7)-Related Cancer and IGFBP3 and IGFBP7 Crosstalk. Front Oncol. 2020;10:727. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 69] [Article Influence: 13.8] [Reference Citation Analysis (0)] |