Published online May 7, 2022. doi: 10.3748/wjg.v28.i17.1860
Peer-review started: September 17, 2021
First decision: November 16, 2021
Revised: December 4, 2021
Accepted: March 25, 2022
Article in press: March 25, 2022
Published online: May 7, 2022
Processing time: 223 Days and 23.4 Hours
Endoscopic biliary drainage using a self-expandable metallic stent (SEMS) has been widely performed to treat distal malignant biliary obstruction (DMBO). However, the optimal position of the stent remains unclear.
To determine the ideal position for SEMS placement.
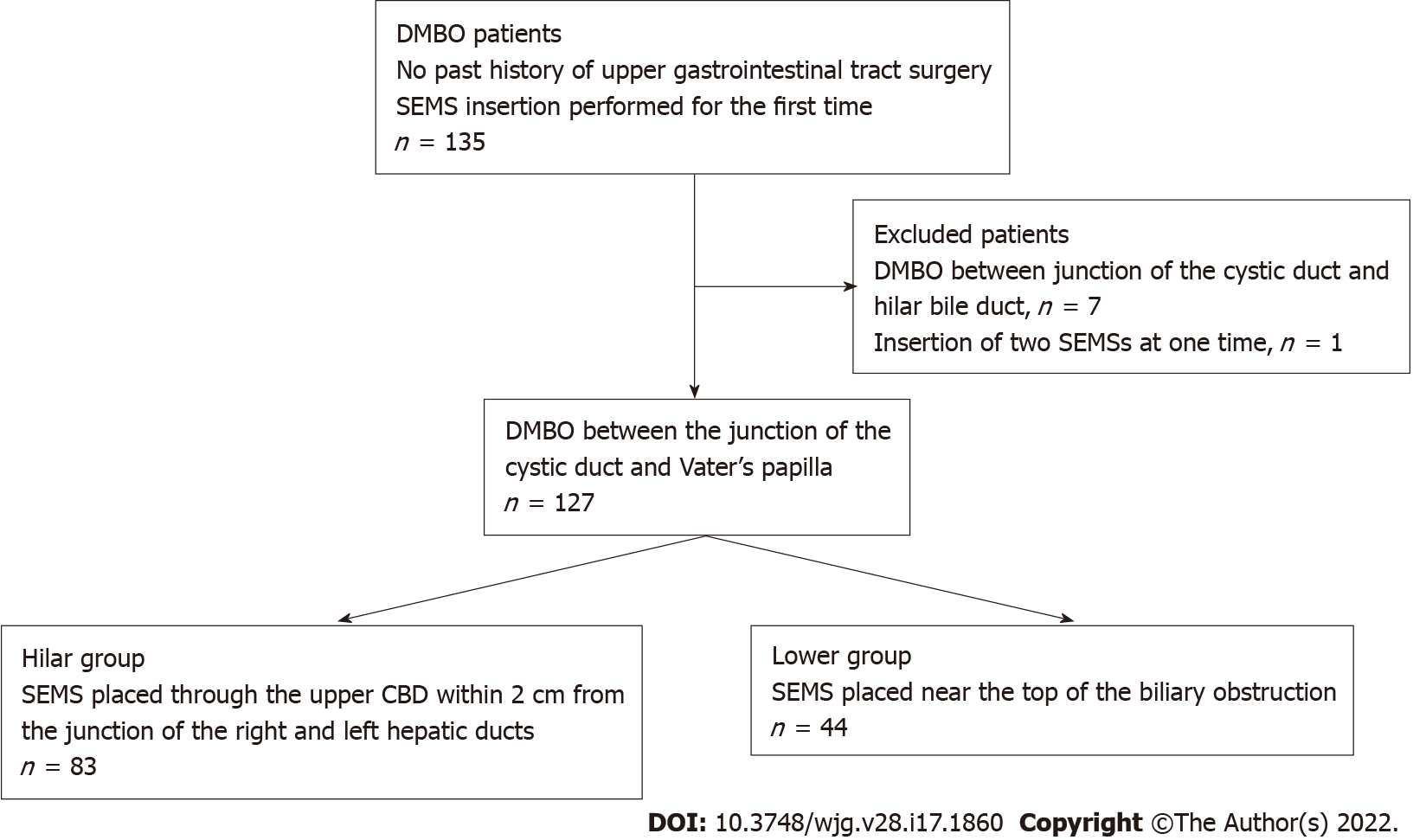
In total, 135 DMBO patients underwent SEMS (uncovered or covered) placement over a ten-year period. A total of 127 patients with biliary obstruction between the junction of the cystic duct and Vater’s papilla were enrolled. An SEMS was placed through the upper common bile duct 2 cm from the biliary hilar duct in 83 patients (Hilar group) or near the top of the biliary obstruction in 44 patients (Lower group). Technical and functional success, adverse events, and risk factors for SEMS dysfunction were evaluated.
The stent patency period was significantly longer in the Hilar group than in the Lower group (P value < 0.01). In multivariate analysis, the only statistically significant risk factor for SEMS dysfunction was being in the Lower group (hazard ratio: 9.94, 95% confidence interval: 2.25–44.0, P < 0.01).
A longer patency period was achieved by positioning the SEMS near the biliary hilar duct.
Core Tip: Endoscopic biliary drainage using a self-expandable metallic stent (SEMS) has been widely performed to treat distal malignant biliary obstruction (DMBO). However, the optimal position of the SEMS remains unclear. This study indicated that the stent patency period was significantly longer when the SEMS was placed near the biliary hilar duct. Furthermore, the placement of a longer SEMS from the biliary hilar duct was thought to overcome several factors of recurrent biliary obstruction in DMBO patients.
- Citation: Sugimoto M, Takagi T, Suzuki R, Konno N, Asama H, Sato Y, Irie H, Okubo Y, Nakamura J, Takasumi M, Hashimoto M, Kato T, Kobashi R, Yanagita T, Hikichi T, Ohira H. Biliary metal stents should be placed near the hilar duct in distal malignant biliary stricture patients. World J Gastroenterol 2022; 28(17): 1860-1870
- URL: https://www.wjgnet.com/1007-9327/full/v28/i17/1860.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i17.1860
Stricture of the common bile duct (CBD) can occur in several severe diseases (for example, bile duct cancer, pancreatic cancer, or metastasis of other cancers). Since transpapillary biliary stent insertion was first reported by Sohendra and Reynders-Frederix[1], it has become the first choice for biliary drainage in patients with malignant biliary obstruction. At present, uncovered self-expandable metallic stents (USEMSs) and covered SEMSs (CSEMSs) have been reported to be more effective at preventing recurrent biliary obstruction (RBO) than plastic stents (PSs) in distal malignant biliary obstruction (DMBO) patients[2,3].
Whether a USEMS or CSEMS should be used remains a topic of debate. Three reports have asserted that the patency period of CSEMSs is superior to that of USEMSs[4-6]. However, others have found that the patency period is similar between CSEMSs and USEMSs[7-9]. Although CSEMS insertion has some disadvantages (such as cholecystitis, pancreatitis, and migration), the stent can be removed[7,10-13].
Based on the above findings, SEMS placement may help drain unresectable DMBOs. Determining which stent (USEMS or CSEMS) should be used has gained increasing attention. However, the optimal position of the inserted SEMS has rarely been discussed and remains unclear. Therefore, we aimed to determine the ideal position for SEMS placement.
This was a retrospective study. The patients were not required to provide informed consent because this study used anonymized clinical data obtained after each patient had provided written consent and agreed to undergo medical procedures. Additional details of this study are published on the home page of Fukushima Medical University (approval number 2453).
A total of 135 DMBO patients underwent SEMS placement between January 2011 and February 2021 (Figure 1). These patients did not undergo previous surgery of the upper gastrointestinal tract and were undergoing SEMS placement for the first time. Seven of these patients whose biliary obstruction was located between the junction of the cystic duct and hilar bile duct were excluded from this study. In addition, one patient who underwent double SEMS placement was excluded. Finally, 127 patients whose biliary obstruction was located between the junction of the cystic duct and Vater’s papilla were enrolled. The SEMS was placed through the upper CBD within 2 cm from the junction of the right and left hepatic ducts in 83 patients (Hilar group) (Figure 2A and B). In the other 44 patients (Lower group), the SEMS was placed near the top of the biliary obstruction (Figure 2C and D).
With the patient in a prone position, a duodenoscope was inserted after the patient was sufficiently sedated with midazolam. When the duodenoscope reached Vater’s papilla, biliary cannulation was initiated. After the range of the DMBO was confirmed by cholangiography, an SEMS was inserted from the upper part of the obstruction to Vater’s papilla. Endoscopic sphincterotomy (EST) was performed for first-time endoscopic biliary drainage with a PS or before SEMS insertion. The position and type of SEMS (USEMS or CSEMS) were randomly determined by each endoscopist. All the procedures were performed by pancreaticobiliary specialists or trainees under the guidance of specialists.
The USEMSs used in this study were as follows: BileRush, 8 mm × 6 cm, 10 mm × 6 or 8 cm (Piolax, Kanagawa, Japan); Bonastent, 10 mm × 8 cm (Standard Sci Tech, Seoul, Korea); HANARO, 10 mm × 7 cm (Boston Scientific, Tokyo, Japan); Niti-S Large cell, 10 mm × 5, 6, 8, or 10 cm (Taewoong Medical, Gyeoenggi-do, Korea); WallFlex, 10 mm × 6, 8, or 10 cm (Boston Scientific); X Suit NIR, 10 mm × 8 cm (Olympus Medical, Tokyo, Japan); and Zilver, 10 mm × 6 cm, and Zilver 635, 10 mm × 6, 8, or 10 cm (Cook Medical Japan, Tokyo, Japan). The CSEMSs used in this study were as follows: Bonastent, 10 mm × 7 cm (Standard Sci Tech); HANARO, 10 mm × 5, 6, or 8 cm (Boston Scientific); Niti-S Comvi, partially covered, 10 mm × 6, 7, or 8 cm (Taewoong Medical); WallFlex, fully covered, 10 mm × 6 cm, and partially covered, 10 mm × 6 or 8 cm (Boston Scientific); and X Suit NIR, 10 mm × 4, 6, or 8 cm (Olympus Medical).
The primary outcome was the stent patency period. The secondary outcomes were the technical success rate, functional success rate, adverse events (pancreatitis, post-EST bleeding), severity of adverse events, and stent dysfunction rate. These outcomes were defined according to partially revised versions of the reported criteria[14]. The stent patency period was determined as the time from first SEMS insertion to SEMS dysfunction. SEMS dysfunction was defined as the recurrence of hepatic dysfunction, jaundice, or dilated bile tract on ultrasonography or computed tomography (CT), which required secondary SEMS placement. Technical success was defined as successful placement of an SEMS that reached from the upper part of the obstruction to Vater’s papilla. Functional success was defined as the return of alanine transaminase (ALT) or total bilirubin (TB) levels to normal values (ALT < 27 U/L, TB < 1.2 mg/dL) or less than half of the pretreatment values. Adverse events and the severity of adverse events were defined according to Cotton’s criteria[15]. Posttreatment pancreatitis was also confirmed by contrast-enhanced CT.
In addition, the patient characteristics (age, sex, serum ALT level, serum TB level, cause of stricture, chemotherapy, duodenal stricture, CBD diameter above the stricture, CBD stricture diameter, CBD stricture length), year of procedure (2011-2015, or 2016-2021), stent diameter, type of SEMS used (USEMS or CSEMS), SEMS shortening, and observational period were compared between the Hilar group and the Lower group. The maximum serum ALT and TB values recorded in the previous week up to endoscopic SEMS insertion were used. The cause of stricture was divided into pancreaticobiliary and metastatic. Duodenal stricture was defined as a stricture that was difficult for the upper gastrointestinal scope to pass through. The diameter and length of the CBD stricture were measured by endoscopic retrograde cholangiography. The year of the procedure was compared between the groups because the techniques and devices have advanced over the approximately ten-year study duration. SEMS shortening was determined as more than 1 cm of shortening evident on X-ray or CT imaging after SEMS placement.
Student’s t test or Welch’s t test was used to compare continuous variables. Fisher’s exact test was used to compare nominal variables. To analyze the SEMS patency period, the log-rank test was used. To analyze the factors that influenced SEMS dysfunction, a Cox proportional hazard model was used. P < 0.05 was considered statistically significant. All statistical analyses were performed using EZR (Saitama Medical Centre, Jichi Medical University, Saitama, Japan).
The patient characteristics are shown in Table 1. There was no significant difference in age, sex, serum ALT level, serum TB level, stricture cause, chemotherapy, duodenal stricture, CBD diameter above the stricture, CBD stricture diameter, or CBD stricture length between the Hilar group and the Lower group.
| Hilar group (n = 83) | Lower group (n = 44) | P value | |
| Age, yr | 68.4 ± 11.8 | 71.2 ± 11.2 | 0.22 |
| Sex | |||
| Female | 33 (39.8) | 16 (36.4) | 0.85 |
| Male | 50 (60.2) | 28 (63.6) | |
| ALT, U/L | 126.0 ± 116.3 | 174.8 ± 177.1 | 0.11 |
| TB, mg/dL | 5.9 ± 7.5 | 6.8 ± 6.8 | 0.47 |
| Cause of stricture | 0.77 | ||
| Pancreaticobiliary tumor | 73 (88.0) | 40 (90.9) | |
| Pancreas | 67 | 31 | |
| Biliary tract | 6 | 9 | |
| Metastasis | 10 (12.0) | 4 (9.1) | |
| Lung | 3 | 1 | |
| Stomach | 3 | ||
| Rhabdomyosarcoma | 1 | ||
| Uterine | 1 | ||
| Ovarian | 1 | ||
| Esophagus | 1 | ||
| Breast | 1 | ||
| Colon | 1 | ||
| Lymph node metastasis from gallbladder cancer | 1 | ||
| Chemotherapy | 35 (42.2) | 23 (52.3) | 0.35 |
| Duodenal stricture | 15 (18.1) | 7 (15.9) | 0.81 |
| CBD diameter above stricture, mm | 11.5 ± 4.3 | 12.2 ± 4.0 | 0.40 |
| CBD stricture diameter, mm | 0.61 ± 0.89 | 0.72 ± 0.8 | 0.50 |
| CBD stricture length, cm | 2.64 ± 1.35 | 2.34 ± 1.11 | 0.21 |
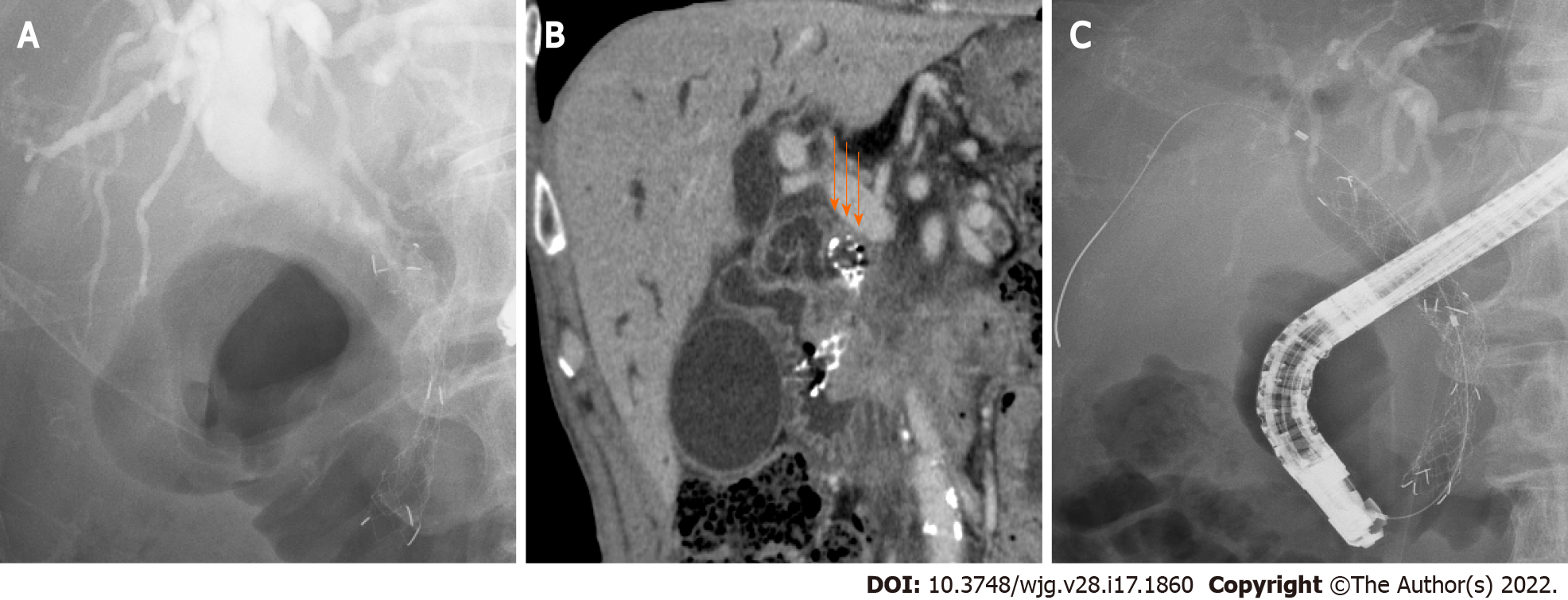
The outcomes of SEMS placement are shown in Table 2. There was no difference in the procedure year, technical success rate, functional success rate, adverse events, or SEMS shortening between the two groups. The rate of CSEMS use and the SEMS diameter were also not significantly different between the two groups. Regarding the type of SEMS used, the covered WallFlex (Boston Scientific) stent was used significantly more frequently in the Hilar group than in the Lower group (28/83 (33.7%) vs 7/44 (15.9%), P value = 0.038), and the X Suit NIR stent was used significantly more frequently in the Lower group than in the Hilar group (6/44 (13.6%) vs 0/83 (0%), P value < 0.01). SEMS dysfunction was observed significantly more often in the Lower group than in the Hilar group [18/44 (41%) vs 2/83 (2.4%), P value < 0.01]. The causes of SEMS dysfunction were as follows: Ingrowth (1) and overgrowth (1) in the Hilar group, and ingrowth (3), overgrowth (2), ingrowth and overgrowth (8), top edge closed by the CBD wall (4), and dislocation (1) in the Lower group. In the cases in which the top edge was closed by the CBD wall, the SEMSs used were the Zilver 635 (Cook Medical), WallFlex (Boston Scientific), Niti-S large cell (Taewoong Medical), and HANARO (Boston Scientific) stents. A representative case in which the top edge of the SEMS was closed by the CBD wall is shown in Figure 3. The observational period was longer in the Lower group than in the Hilar group (9.12 ± 12.07 mo vs 4.16 ± 5.76 mo, P value = 0.012).
| Variable | Hilar group (n = 83) | Lower group (n = 44) | P value |
| Year of procedure | 0.18 | ||
| 2011-2015 | 48 (57.8) | 31 (70.5) | |
| 2016-2021 | 35 (42.2) | 13 (29.5) | |
| Diameter of SEMS | 1.0 | ||
| 8 mm | 1 (1.2) | 0 (0) | |
| 10 mm | 82 (98.8) | 44 (100) | |
| USEMS:CSEMS | 35:48 | 20:24 | 0.85 |
| USEMS used | |||
| BileRush | 2 (2.4) | 1 (2.3) | 1 |
| Bonastent | 1 (1.2) | 0 (0) | 1 |
| HANARO | 1 (1.2) | 0 (0) | 1 |
| Niti-S Large cell | 9 (10.8) | 5 (11.4) | 1 |
| WallFlex | 24 (28.9) | 7 (15.9) | 0.13 |
| X Suit NIR | 0 (0) | 2 (4.5) | 0.12 |
| Zilver | 0 (0) | 1 (2.3) | 0.35 |
| Zilver 635 | 4 (4.8) | 6 (13.6) | 0.09 |
| CSEMS used | |||
| Bonastent | 0 (0) | 1 (2.3) | 0.35 |
| HANARO | 3 (3.6) | 1 (2.3) | 1 |
| Niti-S Comvi | 11 (13.3) | 7 (15.9) | 0.79 |
| WallFlex | 28 (33.7) | 7 (15.9) | 0.038 |
| X Suit NIR | 0 (0) | 6 (13.6) | < 0.01 |
| Technical success | 83 (100) | 44 (100) | |
| Functional success | 81 (97.6) | 41 (93.2) | 0.34 |
| Adverse events | 2 (2.4) | 0 (0) | 0.54 |
| Pancreatitis | 2 | 0 | |
| Mild | 2 | 0 | |
| Post-EST bleeding | 1 | 0 | |
| Severe | 1 | 0 | |
| SEMS shortening1 | 1 (1.3) | 2 (4.7) | 0.28 |
| SEMS dysfunction | 2 (2.4) | 18 (41) | < 0.01 |
| Cause of SEMS dysfunction | |||
| Ingrowth | 1 | 3 | |
| Overgrowth | 1 | 2 | |
| Ingrowth and overgrowth | 8 | ||
| Top edge closed by CBD wall | 4 | ||
| Dislocation | 1 | ||
| Observational period, months | 4.16 ± 5.76 | 9.12 ± 12.07 | 0.012 |
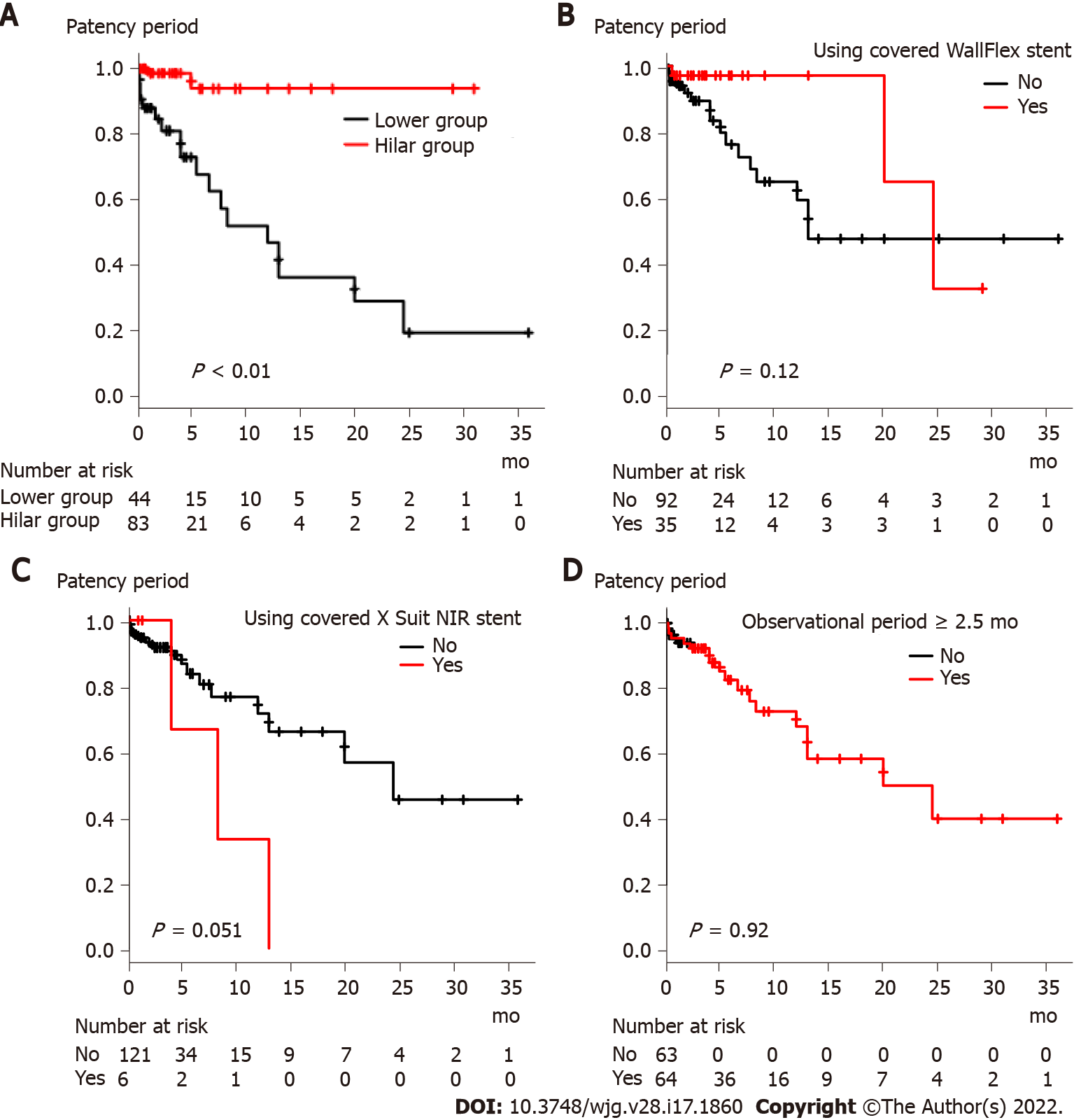
The results of the stent patency comparison are shown in Figure 4 and Supplementary Figure 1. The stent patency period was significantly longer in the Hilar group than in the Lower group (Figure 4A, P value < 0.01). The stent patency period was not significantly different between the groups when the patients were divided according to the use of a covered WallFlex stent, use of a covered X Suit NIR stent, observational period (Figure 4B-D), age, sex, serum ALT level, serum TB level, metastatic or pancreaticobiliary status, presence or absence of chemotherapy, presence or absence of duodenal stricture, CBD diameter above the stricture, CBD stricture diameter, CBD stricture length, year of procedure, USEMS or CSEMS, presence or absence of SEMS shortening (Supplementary Figure 1).
The risk factors for SEMS dysfunction are shown in Table 3. Serum ALT level and lower placement were statistically significant factors in the univariate analysis [ALT: hazard ratio (HR): 1.003, 95% confidence interval (CI): 1.001–1.01, P value < 0.01; Lower group: HR: 11.42, 95%CI: 2.61–49.83, P value < 0.01]. However, the only statistically significant risk factor in the multivariate analysis was lower placement (HR: 9.94, 95%CI: 2.25–44.0, P < 0.01).
| Univariate analysis | Multivariate analysis | |||||
| Hazard ratio | 95%CI | P value | Hazard ratio | 95%CI | P value | |
| Lower group | 11.42 | 2.61–49.83 | < 0.01 | 9.94 | 2.25–44.0 | < 0.01 |
| Age | 1.04 | 0.997–1.09 | 0.07 | |||
| Sex, male | 0.88 | 0.35–2.2 | 0.8 | |||
| ALT | 1.003 | 1.001–1.01 | < 0.01 | 1.002 | 1.0–1.004 | 0.07 |
| TB | 1.05 | 0.99–1.12 | 0.1 | |||
| Cause of stricture, pancreaticobiliary | 0.41 | 0.09–1.9 | 0.26 | |||
| Chemotherapy | 0.89 | 0.34–2.31 | 0.81 | |||
| Duodenal stricture | 1.27 | 0.42–3.83 | 0.67 | |||
| CBD above diameter stricture | 1.06 | 0.94–1.19 | 0.35 | |||
| CBD stricture diameter | 1.004 | 0.56–1.79 | 0.99 | |||
| CBD stricture length | 0.99 | 0.69–1.41 | 0.95 | |||
| Year (2011–2015) | 1.35 | 0.55-3.32 | 0.52 | |||
| Use of CSEMS | 0.67 | 0.28–1.62 | 0.37 | |||
| Use of covered WallFlex stent | 0.4 | 0.12–1.36 | 0.14 | |||
| Use of covered X Suit NIR usage stent | 3.20 | 0.92–11.14 | 0.07 | |||
| SEMS shortening | 1.28 | 0.17–9.73 | 0.81 | |||
| Observational period | 0.98 | 0.92–1.04 | 0.43 | |||
In this study, we investigated the ideal position for SEMS insertion in DMBO patients. The results demonstrated that the SEMS patency period was longer when the stent was placed near the hilar duct.
This finding suggests that this position overcomes several causes of SEMS dysfunction. As shown in Table 2, the main causes of SEMS dysfunction were tumor ingrowth and/or overgrowth and a top edge closed by the CBD wall; notably, overgrowth and a top edge closed by the CBD wall were prevented by using a longer SEMS. Longer SEMSs can delay stent dysfunction due to tumor overgrowth. In the four patients in the Lower group, the top edge of the SEMS was closed by the CBD wall, which may be caused by linearization of the SEMS. The axial force on the stent is thought to be related to the linearization and closing of the top edge by the CBD wall. However, in the four patients with SEMS dysfunction caused by closure of the top edge by the CBD wall, the SEMSs were not necessarily affected by high axial force, except for the WallFlex (Boston Scientific) stent. When a short SEMS is placed near the top edge of the DMBO, the axial force might be enhanced by the biliary stricture. Using longer SEMSs overcomes this problem because the axial force decreases with increasing distance between the top edge of the SEMS and CBD stricture[16]. In fact, a biliary obstruction was relieved by placing a second SEMS near the biliary hilar duct (Figure 3C).
In past reports, time to adequate expansion, degree of CBD stricture[17], duodenal invasion[18], duodenal SEMS[19], and anticancer treatment[18,20] were reported as risk factors for RBO. The factors related to SEMS expansion and CBD stricture were not an issue in this study because functional success was achieved in almost all the patients. Anticancer treatment has been reported to cause RBO as follows. Although anticancer treatment reduces the tumor burden, it can dislocate the CSEMS or induce neutropenia and bacterial overgrowth and, ultimately, cholangitis or sludge formation in the bile duct[20]. However, anticancer treatment was not proposed as a risk factor for RBO in a study that involved patients with a USEMS[21]. This study involved both USEMSs and CSEMSs. Therefore, anticancer treatment may not be a risk factor for SEMS dysfunction. Duodenal invasion from tumors reduces peristalsis and causes food impaction in the biliary duct, and a duodenal SEMS prevents the outflow of bile juice[19]. In this study, any RBO requiring additional SEMS placement was defined as SEMS dysfunction so that SEMS occlusion caused by tumors could be properly evaluated and cases of SEMS occlusion by food impaction could be excluded. Therefore, SEMS placement near the biliary hilar duct was revealed as a new factor related to longer SEMS patency.
There were some limitations to this study. First, this was a retrospective observational study performed at a single institution. In the future, it is hoped that a prospective multicenter study will confirm our findings. Second, the type of SEMS was not unified. The axial force or shortening length varied among the SEMSs. Measurement of the axial force was difficult in this study; instead, different kinds of SEMSs were compared. As a result, the type of SEMS did not influence SEMS dysfunction. The WallFlex stent (Boston Scientific), which has a high axial force and a high shortening rate[22], was used significantly more often in the Hilar group. However, remarkable shortening was rarely observed (the presence or absence of shortening was confirmed in 23 patients 24 h after SEMS placement and in 99 patients more than 48 h after SEMS placement). This was likely due to the placement of an SEMS with a longer than established length because the SEMS could not fully expand in the area of the stricture. As described above, the axial force decreases with increasing SEMS length. Because of these factors, the difference in the type of SEMS did not influence the outcomes. Third, SEMS obstruction of sludge or food debris was not considered SEMS dysfunction. In past reports, sludge formation has been proposed to be a cause of SEMS dysfunction[4,5,21]. This factor is surely important for comparisons of patency periods between USEMS and CSEMS. If SEMS obstruction of sludge or food debris was considered stent dysfunction, the patency period was also significantly longer in the Hilar group than in the Lower group (Supplementary Figure 2). Therefore, the obstruction of sludge or food debris did not influence the results of this study. As described above, the SEMS obstruction of sludge or food debris was excluded from SEMS dysfunction to properly evaluate the relationship between the positions of the SEMS and tumor in this study.
The results of our study revealed that placement of an SEMS near the biliary hilar duct could delay tumor overgrowth and prevent closure of the top edge of the SEMS by the CBD wall. Thus, in DMBO patients, the SEMS should be placed near the biliary hilar duct to achieve a longer patency period.
Endoscopic biliary drainage using a self-expanding metallic stent (SEMS) has a longer patency period than endoscopic biliary drainage using a plastic stent. Therefore, endoscopic SEMS placement is desirable for the treatment of unresectable distant malignant biliary obstruction (DMBO).
The type of SEMS that should be used for DMBO is a point of active discussion. However, the appropriate position for SEMS insertion is unknown.
To clarify the appropriate SEMS insertion point for DMBO.
Among 135 DMBO patients who underwent SEMS placement, 127 patients with biliary obstruction between the junction of the cystic duct and Vater’s papilla were enrolled. In 83 patients (Hilar group), an SEMS was placed through the upper common bile duct within 2 cm from the biliary hilar duct. In the other 44 patients (Lower group), an SEMS was placed near the top of the biliary obstruction. The patency period was compared between the Hilar group and Lower group. The risk factors for SEMS dysfunction were also investigated.
The patency period of SEMS was significantly longer in the Hilar group patients. Multivariate analysis revealed that the Lower group classification was the only significant risk factor for SEMS dysfunction.
SEMS placement near the biliary hilar duct extends the patency period in DMBO patients.
SEMS placement near the biliary hilar duct might prevent obstructive jaundice and cholangitis and contribute to improved prognosis in DMBO patients.
We thank the entire staff at the Department of Gastroenterology of Fukushima Medical University, the Department of Endoscopy of Fukushima Medical University Hospital, and the gastroenterology ward of Fukushima Medical University Hospital.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kim JH, South Korea; Sun SY, China; Zeng YY, China S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Soehendra N, Reynders-Frederix V. Palliative bile duct drainage - a new endoscopic method of introducing a transpapillary drain. Endoscopy. 1980;12:8-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 283] [Cited by in RCA: 245] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 2. | Davids PH, Groen AK, Rauws EA, Tytgat GN, Huibregtse K. Randomised trial of self-expanding metal stents vs polyethylene stents for distal malignant biliary obstruction. Lancet. 1992;340:1488-1492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 753] [Cited by in RCA: 697] [Article Influence: 21.1] [Reference Citation Analysis (1)] |
| 3. | Isayama H, Yasuda I, Ryozawa S, Maguchi H, Igarashi Y, Matsuyama Y, Katanuma A, Hasebe O, Irisawa A, Itoi T, Mukai H, Arisaka Y, Okushima K, Uno K, Kida M, Tamada K. Results of a Japanese multicenter, randomized trial of endoscopic stenting for non-resectable pancreatic head cancer (JM-test): Covered Wallstent vs DoubleLayer stent. Dig Endosc. 2011;23:310-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 97] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 4. | Isayama H, Komatsu Y, Tsujino T, Sasahira N, Hirano K, Toda N, Nakai Y, Yamamoto N, Tada M, Yoshida H, Shiratori Y, Kawabe T, Omata M. A prospective randomised study of "covered" vs "uncovered" diamond stents for the management of distal malignant biliary obstruction. Gut. 2004;53:729-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 460] [Cited by in RCA: 458] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 5. | Krokidis M, Fanelli F, Orgera G, Bezzi M, Passariello R, Hatzidakis A. Percutaneous treatment of malignant jaundice due to extrahepatic cholangiocarcinoma: covered Viabil stent vs uncovered Wallstents. Cardiovasc Intervent Radiol. 2010;33:97-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 79] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 6. | Krokidis M, Fanelli F, Orgera G, Tsetis D, Mouzas I, Bezzi M, Kouroumalis E, Pasariello R, Hatzidakis A. Percutaneous palliation of pancreatic head cancer: randomized comparison of ePTFE/FEP-covered vs uncovered nitinol biliary stents. Cardiovasc Intervent Radiol. 2011;34:352-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 79] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 7. | Almadi MA, Barkun AN, Martel M. No benefit of covered vs uncovered self-expandable metal stents in patients with malignant distal biliary obstruction: a meta-analysis. Clin Gastroenterol Hepatol. 2013;11:27-37.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 145] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 8. | Shamah SP, Chapman CG, Haider H, Liao C, Waxman I, Siddiqui UD. Partially Covered Versus Uncovered Self-Expandable Metal Stents: Coating Nor Diameter Affect Clinical Outcomes. Dig Dis Sci. 2019;64:2631-2637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Elkilany A, Alwarraky M, Geisel D, Maaly MA, Denecke T. Stent performance in palliative transhepatic treatment of malignant biliary obstruction: a randomized study comparing covered vs uncovered stents. Acta Radiol. 2020;61:1591-1599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Gómez-Oliva C, Guarner-Argente C, Concepción M, Jiménez FJ, Rodríguez S, Gonzalez-Huix F, Mugica F, Cabriada JL, Rodríguez C, Aguilar CG; Collaborating Group of the COBIWA Register. Partially covered self-expanding metal stent for unresectable malignant extrahepatic biliary obstruction: results of a large prospective series. Surg Endosc. 2012;26:222-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Shimizu S, Naitoh I, Nakazawa T, Hayashi K, Miyabe K, Kondo H, Yoshida M, Yamashita H, Umemura S, Hori Y, Ohara H, Joh T. Predictive factors for pancreatitis and cholecystitis in endoscopic covered metal stenting for distal malignant biliary obstruction. J Gastroenterol Hepatol. 2013;28:68-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 12. | Nakahara K, Morita R, Michikawa Y, Suetani K, Morita N, Fujita A, Sato J, Igarashi Y, Ikeda H, Matsunaga K, Watanabe T, Kobayashi S, Otsubo T, Itoh F. Endoscopic Transpapillary Gallbladder Drainage for Acute Cholecystitis After Biliary Self-Expandable Metal Stent Placement. Surg Laparosc Endosc Percutan Tech. 2020;30:416-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Takinami M, Murohisa G, Yoshizawa Y, Shimizu E, Nagasawa M. Risk factors for cholecystitis after stent placement in patients with distal malignant biliary obstruction. J Hepatobiliary Pancreat Sci. 2020;27:470-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (1)] |
| 14. | Isayama H, Hamada T, Yasuda I, Itoi T, Ryozawa S, Nakai Y, Kogure H, Koike K. TOKYO criteria 2014 for transpapillary biliary stenting. Dig Endosc. 2015;27:259-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 240] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 15. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1890] [Cited by in RCA: 2032] [Article Influence: 59.8] [Reference Citation Analysis (1)] |
| 16. | Isayama H, Nakai Y, Toyokawa Y, Togawa O, Gon C, Ito Y, Yashima Y, Yagioka H, Kogure H, Sasaki T, Arizumi T, Matsubara S, Yamamoto N, Sasahira N, Hirano K, Tsujino T, Toda N, Tada M, Kawabe T, Omata M. Measurement of radial and axial forces of biliary self-expandable metallic stents. Gastrointest Endosc. 2009;70:37-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 168] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 17. | Kim HS, Lee DK, Kim HG, Park JJ, Park SH, Kim JH, Yoo BM, Roe IH, Moon YS, Myung SJ. Features of malignant biliary obstruction affecting the patency of metallic stents: a multicenter study. Gastrointest Endosc. 2002;55:359-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 64] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 18. | Nakai Y, Isayama H, Kogure H, Hamada T, Togawa O, Ito Y, Matsubara S, Arizumi T, Yagioka H, Mizuno S, Sasaki T, Yamamoto N, Hirano K, Tada M, Koike K. Risk factors for covered metallic stent migration in patients with distal malignant biliary obstruction due to pancreatic cancer. J Gastroenterol Hepatol. 2014;29:1744-1749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 19. | Hamada T, Nakai Y, Isayama H, Sasaki T, Kogure H, Kawakubo K, Sasahira N, Yamamoto N, Togawa O, Mizuno S, Ito Y, Hirano K, Toda N, Tada M, Koike K. Duodenal metal stent placement is a risk factor for biliary metal stent dysfunction: an analysis using a time-dependent covariate. Surg Endosc. 2013;27:1243-1248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Nakai Y, Isayama H, Mukai T, Itoi T, Maetani I, Kawakami H, Yasuda I, Maguchi H, Ryozawa S, Hanada K, Hasebe O, Ito K, Kawamoto H, Mochizuki H, Igarashi Y, Irisawa A, Sasaki T, Togawa O, Hara T, Kamada H, Toda N, Hamada T, Kogure H. Impact of anticancer treatment on recurrent obstruction in covered metallic stents for malignant biliary obstruction. J Gastroenterol. 2013;48:1293-1299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Kitano M, Yamashita Y, Tanaka K, Konishi H, Yazumi S, Nakai Y, Nishiyama O, Uehara H, Mitoro A, Sanuki T, Takaoka M, Koshitani T, Arisaka Y, Shiba M, Hoki N, Sato H, Sasaki Y, Sato M, Hasegawa K, Kawabata H, Okabe Y, Mukai H. Covered self-expandable metal stents with an anti-migration system improve patency duration without increased complications compared with uncovered stents for distal biliary obstruction caused by pancreatic carcinoma: a randomized multicenter trial. Am J Gastroenterol. 2013;108:1713-1722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 170] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 22. | Hori Y, Hayashi K, Yoshida M, Naitoh I, Nakazawa T, Miyabe K, Shimizu S, Kondo H, Nishi Y, Umemura S, Kato A, Ohara H, Joh T. New concept of traction force applied to biliary self-expandable metallic stents. Endoscopy. 2016;48:472-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |