Published online Dec 21, 2021. doi: 10.3748/wjg.v27.i47.8058
Peer-review started: June 29, 2021
First decision: August 8, 2021
Revised: August 22, 2021
Accepted: December 7, 2021
Article in press: December 7, 2021
Published online: December 21, 2021
Processing time: 170 Days and 21.5 Hours
Single port surgery (SPS) was introduced as an attractive, minimally invasive surgical technique that ensures esthetic results for many types of visceral surgery. Initially, surgeons immediately set about performing SPS without preliminary knowledge or training, which resulted in higher complication rates. Today, current studies conclusively show that SPS is scientifically rehabilitated and indicated for simple and complex laparoscopic procedures. We here describe the astonishing analogies between Greek mythology and modern surgery.
Core Tip: Single port surgery (SPS) was introduced as an attractive, minimally invasive surgical technique that ensures esthetic results for many types of visceral surgery. Initially, surgeons immediately set about performing SPS without preliminary knowledge or training, which resulted in higher complication rates. Today, current studies conclusively show that SPS is scientifically rehabilitated and indicated for simple and complex laparoscopic procedures. We here describe the astonishing analogies between Greek mythology and modern surgery.
- Citation: Mittermair C, Weiss HG. Analogies between medusa and single port surgery in gastroenterology and hepatology: A review. World J Gastroenterol 2021; 27(47): 8058-8068
- URL: https://www.wjgnet.com/1007-9327/full/v27/i47/8058.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i47.8058
One of the most striking analogies between single port surgery (SPS) and the mythological creature Medusa is of course her hair, reminiscent as it is of the four or more prominent, flexible trocars of SP systems. However, a closer look at the mythological story and the development of SPS brings to light many more surprising similarities.
The following brief resumé is by no means historically all-embracing, but necessary for a better understanding of relationships in Greek mythology: The Greek gods had absolute power over mortals and tended to be jealous, quick-tempered and cunning. Many of them had numerous amours, sexual liaisons and scandals. The children resulting from these dalliances were demigods with impressive skills and an adventurous spirit. The skills or assets were commonly applied by these heroes or the gods themselves to their own advantage. Against this background, the following lines serve to outline Medusa’s place in Greek mythology and to bring it into line with developments in SPS.
The modern concept of doing something "under someone’s aegis" means doing something under the protection of a knowledgeable and benevolent power. In Greek mythology the aegis, as described by Homer in 735 BCE, was a device carried by Athena and Zeus. It was interpreted as a shield featuring the hideous head of Medusa with live venomous snakes in place of hair[1].
The Roman poet Ovid portrayed Medusa, the only mortal of the three Gorgon sisters, Medusa, Stheno, and Euryale, as an originally beautiful maiden ravished by Poseidon in Athena’s temple. As one of the first ideological accounts of rape-victim blaming, Athena punished Medusa by transforming her magnificent hair into horrifying snakes[2].
Anyone who gazed into Medusa’s eyes was horror-stricken and turned into stone. Medusa’s head was cut off by the Greek hero Perseus, who then used it for its ability to turn someone to stone. Finally, he gifted the head to Athena to be mounted on her royal shield. In Ancient Greece the image of Medusa’s head appeared on the Gorgoneion, an amulet worn to avert evil[3]. Although modern interpretations of this myth already range widely from psychoanalysis as an oedipal, libidinous symptom[4] to feminism, which depicts Medusa as a guardian of female power[5], we in all humility would now like to emphasize several parallels between SPS and the mythological story of Medusa.
SPS was developed to minimize the surgically traumatic approach to the peritoneal cavity for a variety of indications. The concept of SPS is a modified laparoscopy based on a solitary short skin incision allowing all necessary surgical instruments to be delivered in parallel or crossed at the level of the abdominal wall.
Hans Christian Jacobaeus, a Swedish gastroenterologist, is regarded as the first person to have performed SPS in humans in 1910[6].
After Power and Barnes published their findings with laparoscopic tubal ligation in 1941[7], gynecologists were the first to adopt SPS for routine interval tubal ligations from the 1960s on[8]. Although more demanding SPS procedures such as hysterectomies were introduced by gynecologists in 1991[9], the SPS technique still did not win over the surgical community as transumbilically assisted laparoscopic appendectomies or single-port laparoscopic cholecystectomies using several percutaneous suspension sutures were viewed as not yet fully developed[10,11].
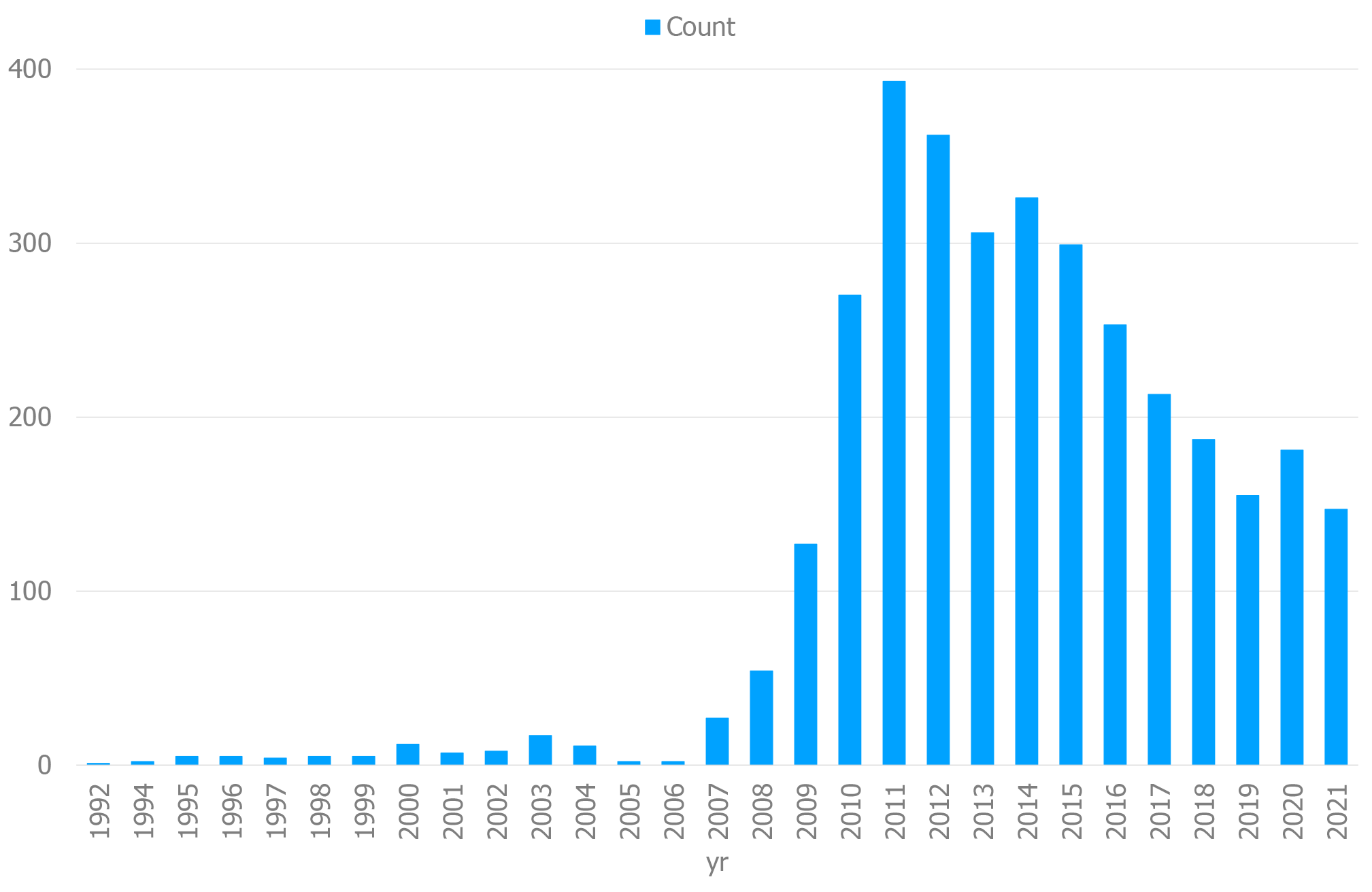
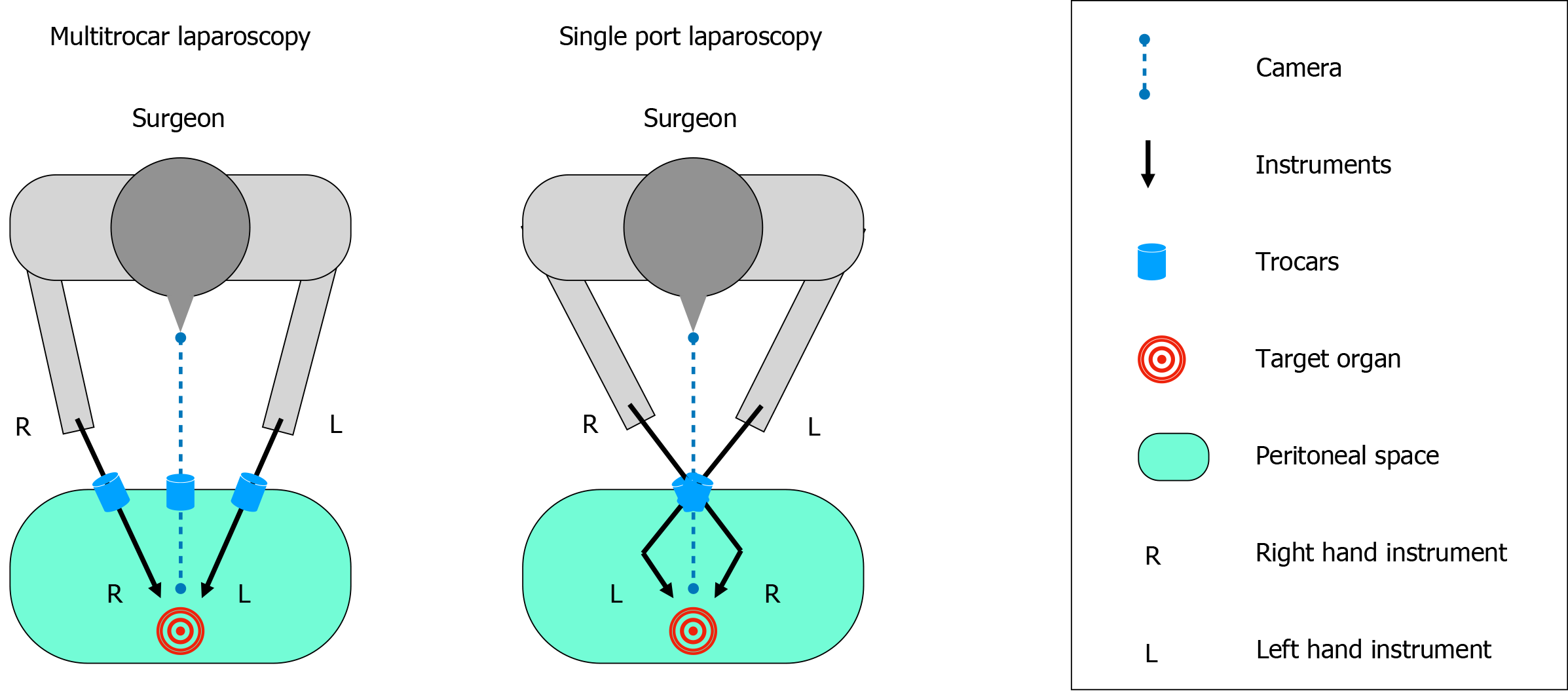
It took another decade of technical development to more appreciably comprehend the beauty of the minimized abdominal wall trauma afforded by SPS. The allure of improved cosmesis roused the surgical community to commence feasibility studies for routine procedures, such as appendectomy[12], cholecystectomy[13], fundoplication[14] or benign colon resection[15]. The publication of scientific reports took off during the next years and peaked in 2012 and 2013 (Figure 1). Compared to conventional multiport laparoscopy, SPS is founded on three fundamental preliminaries: first, a special trocar system; second, a lengthening of the optic and some of the instruments; and third, a modified manipulation of the camera and the non-dominant hand of the surgeon. With regard to the abdominal approach, SPS development began with three to four small trocars used side-by-side after being delivered together through one skin incision[15]. The main disadvantage of this technique was permanent leakage of the pneumoperitoneum, thus impeding safe exposure of the surgical field[16]. In addition, separate fascial defects or specimen retrieval without wound protection significantly increased wound complication rates[16]. The switch from single incision to SPS allowed the pneumoperitoneum to be stabilized. A remarkable variety of single-port devices were introduced, some of them reusable, some of them single-use products. The portfolio ranged from simple home-made ports employing a surgical glove and a wound protector for delivery of all instruments to sophisticated port systems equipped with ambient intraabdominal light, powerful smoke evacuation and routable smart tubing (Figure 2). Delivering all instruments via a fulcrum at the incisional site resulted in a clash of trocar valves or a collision of hands during manipulation. This unpleasant side-effect was at least partially averted by arranging the bulky tubing valves at different distances and by elongating the instruments to enable additional degrees of freedom for the surgeon’s hands. Last but not least, triangulation between the eyes and hands or the target and instruments is fundamental for spatial orientation and dissection. Delivering instruments and the camera together in one line would make triangulation impossible. For this reason, a 30° to 45° optical view is mandatory in SPS. On the other hand, the use of two instruments close to a target requires at least one of the two instruments to be bent and held preferably in the non-dominant hand in order to enable triangulation (Figure 3). The degrees of freedom are comparable to those for conventional multitrocar surgery. Nevertheless, SPS has been seen to involve an increase in wrist rotating movements[17].
While ensuring all these conditions it was possible for the first time to perform standard surgical procedures solely via one nearly invisible incision in the groove of the navel. At first glance, this improved cosmesis would seem to be insignificant in light of the bulk of unsolved problems bothering surgical science. However, esthetic aspects undoubtedly exert an important impact on quality of life[18] and are underestimated by surgeons who focus solely on overall and disease-free survival.
SPS was developed at the same time as two novel surgical approaches, namely tele-manipulating technologies generally summarized under robotic surgery and intraabdominal or intrathoracic procedures performed via a natural orifice, abbreviated as NOTES (natural orifice translumenal endoscopic surgery). In contrast to SPS, which is viewed as an evolutionary development employing standard laparoscopic strategies, the other two concepts revolutionized strategic standards by implementing unconventional instruments and increasing procedural costs. Industrial marketing whipped up a hype particularly for tele-manipulating techniques and NOTES and as a result the tabloid press reported visionary promises long before SPS, robotic and NOTES achieved evidence-based status. Over the last decades all three techniques have gained scientific justification for various surgical indications[19], but are still far from routine daily use because skills remain underdeveloped without additional training and because of the financial burden and prolonged procedural times.
The SPS technique spread to all surgical subdivisions and new applications were created. From 2008, delighted by the first scientific reports[11,20,21], many surgeons immediately felt qualified to perform SPS without in-depth knowledge or training. The resulting disaster saw many procedures fail. Suddenly, SPS was criticized and faulted for providing the negligible benefit of better cosmesis accompanied by an increased hernia rate, prolonged procedural time and possibly increased complication rates in general.
This misunderstanding was prompted by the fallacy that SPS requires a skin incision that is longer than for conventional laparoscopy[20]. A simple comparative calculation of the incision needed to pass a 10 mm trocar (outer diameter 11mm) vs the incision for introduction of three instruments with an external diameter of 5 mm each refutes this assumption: Notwithstanding the elasticity of the fascial sheaths and the skin, a minimum incision length of more or less 17 mm is needed for a "10 mm" trocar and three SPS instruments. The bias against a greater inherent risk for poor wound healing with SPS was fed by numerous publications that reported early learning curve data resulting in meta-analysis similar to that in[23]. A minimized incision is particularly beneficial in those types of surgery where small meshes have to be applied in the abdominal cavity for hernia reconstruction or where no or very small specimens have to be removed. A low rate of less than 1% incisional hernias was achieved in our patient cohort by using a multichannel port or a home-made port and closing the sole fascial incision with running sutures made with non-absorbable monofilament (data submitted for publication).
Insufficient exposure of the surgical field was argued to cause an increased rate of intraoperative complications and prolonged procedural times. This is why an inquiry directed at 600 surgeons from all over the world found that they preferred a standard four-port cholecystectomy rather than SPS if they themselves were undergoing the procedure. However, the prime factors in the decision-making process are the surgeon’s inexperience with this technique and the procedure’s safety[24]. Similar to other types of visceral surgery, the best approach for each patient is chosen by the surgeon at his own discretion. Our own experience is slightly different as all our surgeons have the freedom to perform SPS, dual- or multiport laparoscopic cholecystectomy, and we have not observed these techniques to have any differences with regard to procedural times or complication rates. However, as these procedures demand good triangulation and adequate exposure, we do not wait long before implementing suspension sutures and additional trocars in patients or pathologies that are challenging. Obviously, part of the hard-core resistance to SPS may be ascribed to many disconcerting examples of surgical bravado and the onerous need to devote time and energy to on-going skills training with a view to learning efficient execution of the SPS technique.
SPS has shown equipotent feasibility and safety in many surgical indications as compared to multiport laparoscopy. In particular, some of the following visceral surgery procedures are viewed as standard in our department based on current scientific evaluation.
For appendectomy, recent meta-analyses have demonstrated that patients stay in-hospital less long, return to their jobs sooner and enjoy better cosmesis in the SPS group vis-à-vis briefer operating time and smaller numbers of conversions in the customary three-port groups[25,26]. We incorporated the technique into our clinical routine in 2009 and have meanwhile successfully performed 903 procedures (Table 1) with no significant technical changes.
| SPS Procedures | Procedural numbers | Specific surgical methods |
| Cholecystectomies | 2216 | Including intraoperative ERCPs/Cholangiographies |
| Inguinal hernia repairs | 1850 | TAPP/TEP |
| Appendectomies | 903 | |
| Colorectal resections | 798 | TME/APR/ ta TME |
| Liver resections | 106 | Minor/Major hepatectomies |
| Small bowel resections | 90 | |
| Gastric resections | 49 | Oncologic surgery: Gastrectomy with D1 Lymphadenectomy, Partial gastric resections, Transgastric resections, Metabolic surgery: Sleeve gastrectomies, RY-gastric bypass, Omega-loop bypass |
| Pancreas resections | 29 | Distal pancreas resections, Enucleations |
| Adrenalectomies | 25 | Trans-/retroperitoneoscopic approach |
| Fundoplications | 21 | Nissen/Toupet reconstructions |
| Other procedures | 256 | Abdominal wall reconstructions, Adhesiolysis, Nephrectomies, Lymphadenectomies, Splenectomies, Intraabdominal foreign body removals, Adnexectomies, Hysterectomies, Cyst unroovings, Diagnostic laparoscopies, Ligamentum arcuatum resections, Abscess evacuation, Necrosectomies, Neurectomy |
| Total | 6343 |
Cholecystectomy is undoubtedly the most discussed of all SPS procedures. Despite the many prophets of doom and some terrible outcomes produced by so-called early adopters, the results of more recent trials including some randomised controlled trials and a multicenter trial from Korea are more encouraging. Better cosmesis, less postoperative pain, shorter recovery time and a comparably low rate of adverse events[27,28] are proven benefits of the method. This is consistent with our personal experience with more than 2200 performed cases. In this context it should be noted that a low threshold for the implementation of intracorporeal retractors, suspending sutures or additional trocars for optimal exposure or safe dissection is mandatory to prevent adverse events in complex cases.
Colorectal resections are some of the most appropriate procedures for SPS for the following reasons: All parts of the colorectal frame are ideally reachable from the umbilicus, but also even bulky specimens can be removed via this incision without destroying the natural shape of the umbilicus. Again, improved cosmesis, less postoperative pain and earlier return to normal life are scientifically proven[29,30] and, more importantly, oncological safety has been demonstrated[31]. Additionally, recent data suggest an even smaller number of postoperative complications[32]. These findings completely match our own experience, but we would like to add that there are key success factors that, amazingly enough, are underestimated. Meticulous handling of the umbilical incision by means of wound protectors and additional retrieval bags (Figure 4), prudent preparation techniques with reduced shear forces and thorough closing of the fascial and skin defect are mandatory for successful implementation of SPS in colorectal surgery.
Procedures involving the upper gastro-intestinal tract are meanwhile routinely performed, but exclude esophageal resections because intrathoracic dissection is awkward from the umbilicus in general. Gastric or intragastric resections, bariatric procedures and fundoplications are frequently performed with the SP technique and provide good cosmetic results and less postoperative pain at an acceptable level of postoperative complications[33,34,35]. However, the role of SPS in complex oncologic gastric resections with D2 Lymphadenectomy must be scrutinized, as the current evidence in no way allows a final conclusion to be drawn on minimally invasive surgery in these cases.
In contrast to the aforementioned indications and procedures with a high level of evidence and a comparably large number of surgeons performing these operations, other procedures have met with less acceptance and distribution among the surgical community.
Despite the probable benefit of reduced trauma to the abdominal wall in patients undergoing inguinal hernia repair, the SP technique did not prevail. While experts demonstrated the safety and feasibility of the technique[36], the complexity of the method, on the one hand, and the very high standard of modern three-port hernia surgery, on the other hand, may have impeded further attempts to implement it in clinical routine. In contrast, we have successfully performed 1850 cases of SP inguinal hernia repair to date. Although the aforementioned high complexity of the procedure is admittedly undisputed and only strong personal convictions allow someone to make a strategic switch to SPS, the pathology of groin or umbilical hernia is closely linked to a disarrangement of micro-tubular tissue assembly. Therefore, minimizing incisional length, which is done better in SPS than in any other type of laparoscopic or open hernia repair, would strongly advocate SP transperitoneal or total extraperitoneal mesh repair.
Larger incisions required for specimen retrieval would speak in favor of SPS. However, the high complexity of minimally invasive liver resection has delayed its implementation. SPS was seen to be superior to multiport surgery in left lateral sectionectomies with regard to operative time[37]. Additionally, our group has demonstrated the feasibility of SP minor liver resection in combination with radiofrequency pre-coagulation[38]. The feasibility of SP major resections has been demonstrated by experienced minimally invasive liver surgeons[39]. These results were confirmed by a series from our department. Nevertheless, we observed an increased risk of substantial blood loss when bleeding occurs in these complex resections[40].
Pancreatic resections generally rank among the most demanding procedures in minimally invasive surgery. This explains the very small number of procedures as well as the small number of published reports, not counting case reports or small case series. Generally, only pathologies at the tail of the pancreas have been treated by means of SPS and even these resections are hampered by reduced degrees of freedom. As a consequence, dual incision laparoscopy was introduced and promoted by some groups to overcome the hurdles of impeded suturing and stapling[41,42].
In addition, some procedures favor SPS for its conceptual features although basically all types of laparoscopy with specimen retrieval are good candidates for exemplary performance via a single port.
Intraperitoneal laparoscopic redo surgery is one of the ideal applications for SPS as a single incision permits not only an immediate view, but also delivery of dissection instruments for preexisting adhesions. This efficiency is appreciated to free peritoneal adhesion cords in small bowel obstruction or assist in abdominal wall repair for incisional hernia.
As every incision entails the risk for acute or chronic complications, the SPS concept should support all types of possible repetitive intraperitoneal procedures such as hepatic or lymphonodular metastasectomies in oncologic surgery and preserve the fitness of patients undergoing exhausting polychemotherapies, where staging laparoscopies are required. Indeed, after one century of modern surgery the latter indication has proven a valuable reminder of the early days of SPS. On the other side of the street from oncologic diseases, palliative decompression procedures, such as gastro-enterostomies in gastric outlet obstruction for cancer, can ideally be performed by means of SPS with minimal trauma to patients having limited length and quality of life.
Furthermore, SPS brings momentum to an alternative situation: metabolic surgery for morbid obesity is undoubtedly one of the most important medical interventions available in the fight against the pandemic of obesity and diabetes in the common world. Sadly, society unjustly denounces morbidly obese patients for their psychological weakness. Fear of outing oneself for needing surgical help to cope with obesity as well as fear of invasive surgery itself rob many of these patients of the opportunity to obtain proper treatment. SPS provides a tool for safe metabolic surgery with minimal trauma so as to prevent telltale surgical scars. In this way, patients are protected from the psychological wrath of society for being overweight and for lacking mental or behavioral fortitude.
At the same time, it is mandatory that the limitations of the SPS concept be made known.
First, different targets that are spaced far apart and that can hardly be reached from one incision (e.g., left colonic flexure mobilization in deep rectal resection operated via incision of the protective ileostomy or the intrathoracic esophageal dissection required in fundoplication for gastro-esophageal reflux disease) are obvious limitations.
Second, it is recommended that surgical procedures requiring wound drainage not be performed via the umbilicus because of the risk of wound complications in the longer term. Therefore, for dual-port laparoscopy in distal pancreas resections an additional port away from the umbilicus is recommended for the drain, as described above[41,42].
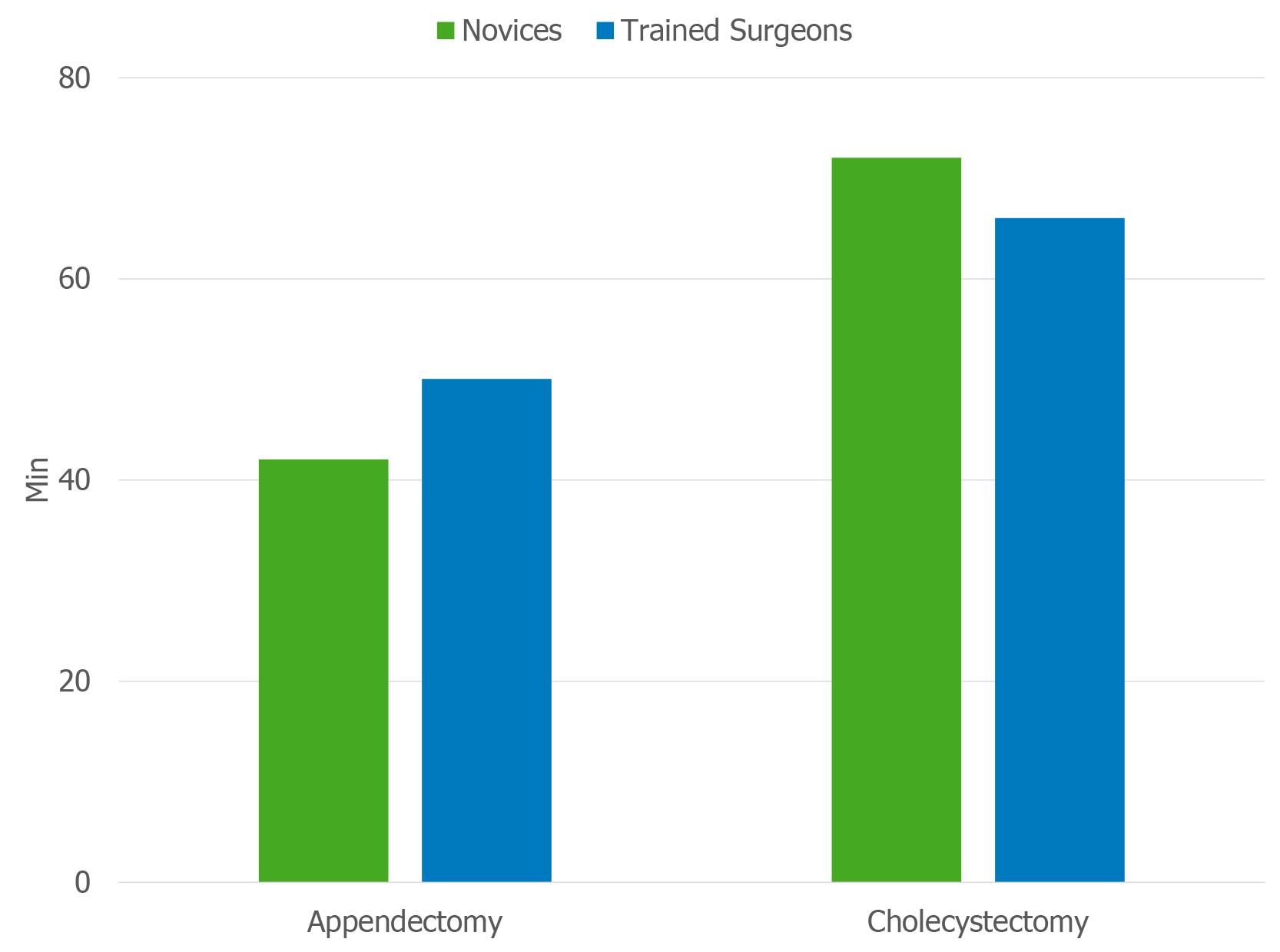
The knowledgeable and benevolent skills that are acquired when performing SPS are described in many reports made by expert surgeons[43]. Better skills for both conventional laparoscopy and SPS are acquired by experienced laparoscopic surgeons, who pass the learning curve for this uncommon minimally invasive technique. On the other hand, SPS training is even less arduous for surgical novices as they are not hampered by the consolidated motion patterns typical of multiport laparoscopy. We have demonstrated that standard SPS procedures can be performed at the same level of expertise by residents and senior surgeons alike (Figure 5).
Furthermore, SPS also generates skills that are useful for other indications. For example, transanal rectal resections, such as transanal total mesorectal rectal excision (taTME) would never have become reality if SPS had not laid the groundwork. Moreover, current techniques of abdominal wall reconstruction (e.g., SPS-enhanced view total extraperitoneal patch hernia repair; eTEP) benefit from small incisions enabled by SPS. Transgastric SPS for oncologic resections of gastrointestinal stroma tumors in rendez-vous technique with flexible endoscopy, on the one hand, and transumbilical resection of hepatic segments 2,3 or 7,8 using inline precoagulation or single-port retroperitoneoscopic adrenalectomy, on the other hand, are the bright and shining pieces of the novel surgical mosaic made possible by SPS skills.
Although marketing experts tout telemanipulation as an unrivalled technique, multiport robotic surgery itself has to date hardly accomplished the aims of improved patient outcome in visceral surgery. Single-port telemanipulation with SP robotics, the newest innovation in this field, is already undergoing clinical evaluation and should soon realize the vision of wide-use reduced port surgery. Advantages over conventional laparoscopy for both patients and surgeons who wish to reduce abdominal wall trauma would be the strongest argument for its large-scale implementation.
SPS is an attractive minimally invasive surgical technique that ensures esthetic results for many types of simple and complex visceral surgery. Having traversed the valley of tears when SPS was disdained as inappropriate for use (blame the victim) and criticized by jealous, quick-tempered and big-headed surgical opinion leaders as a rubbish technique, SPS is scientifically rehabilitated when it is performed by surgeons who are willing to tackle the learning curve. Under the aegis of SPS, surgeons have the opportunity to become more accomplished in their professional routine and to finally add the SPS gem to their armamentarium for special indications. Gianni Versace, founder of the Italian luxury fashion label, chose Medusa as his logo because he knew that once people looked his products in the eye, they would be spellbound by their beauty and perfection.
We gratefully acknowledge the valuable discussions with Univ.-Prof. Dr. Frass M and Wiedergut J for the better understanding of Greek mythology.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Austria
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lu C, Palacios Huatuco RM, Zhou S S-Editor: Wang LL L-Editor: A P-Editor: Wang LL
| 1. | Homer. The Iliad. 1st published 735 B.C., Penguin Classics translated by Martin Hammond, 1987: 446-449. [DOI] [Full Text] |
| 2. | Ovid. Metamorphoses 4.798: "the Sovereign of the Sea attained her love in chaste Minerva`s temple (Brookes More translation)" or "in Minerva`s temple Neptune, lord of the Ocean, ravished her" (Frank Justus Miller translation, as revised by G. P. Goold). [DOI] [Full Text] |
| 3. | Potts, Albert A. The World`s Eye. Lexington, KY: The University Press of Kentucky, 1982. |
| 4. | Freud S. "Medusa`s Head". The Standard Edition of the Complete Psychological Works of Sigmund Freud. The Hogarth Press, 2017: 273. |
| 5. | Wilk S. Medusa: Solving the Mystery of the Gorgon. New York: Oxford University Press, 2000: 219. [DOI] [Full Text] |
| 6. | Jacobaeus HC. Über die Möglichkeit die Zystoskopie bei Untersuchungen seröser Höhlen anzuwenden. Munch Med Wochenschr. 1910;57:2090. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Powers FH, Barnes AC. Sterilization by means of peritonoscopic tubal fulguration: Preliminary report. Am J Obstet Gynecol. 1941;41:1038. [RCA] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 30] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Siegler AM. An instrument to aid tubal sterilization by laparoscopy. Fertil Steril. 1972;23:367-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Pelosi MA, Pelosi MA 3rd. Laparoscopic hysterectomy with bilateral salpingo-oophorectomy using a single umbilical puncture. N J Med. 1991;88:721-726. [PubMed] |
| 10. | Inoue H, Takeshita K, Endo M. Single-port laparoscopy assisted appendectomy under local pneumoperitoneum condition. Surg Endosc. 1994;8:714-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 52] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. Br J Surg. 1997;84:695. [PubMed] |
| 12. | Martínez AP, Bermejo MA, Cortś JC, Orayen CG, Chacón JP, Bravo LB. Appendectomy with a single trocar through the umbilicus: results of our series and a cost approximation. Cir Pediatr. 2007;20:10-14. [PubMed] |
| 13. | Romanelli JR, Mark L, Omotosho PA. Single port laparoscopic cholecystectomy with the TriPort system: a case report. Surg Innov. 2008;15:223-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 104] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 14. | Fahrner R, Neuhaus V, Schöb O. Modified single incision laparoscopic fundoplication is feasible: a technical description. Am Surg. 2010;76:E100-E101. [PubMed] |
| 15. | Brunner W, Schirnhofer J, Waldstein-Wartenberg N, Frass R, Weiss H. Single incision laparoscopic sigmoid colon resections without visible scar: a novel technique. Colorectal Dis. 2010;12:66-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 64] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 16. | Weiss HG, Brunner W, Biebl MO, Schirnhofer J, Pimpl K, Mittermair C, Obrist C, Brunner E, Hell T. Wound complications in 1145 consecutive transumbilical single-incision laparoscopic procedures. Ann Surg. 2014;259:89-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 60] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 17. | McCrory B, Lowndes BR, Wirth LM, de Laveaga AE, LaGrange CA, Hallbeck MS. Ergonomic evaluation of laparoendoscopic single-site surgery ports in a validated laparoscopic training model. Work. 2012;41 Suppl 1:1884-1890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Piarulli A, Chiariello GA, Bruno P, Cammertoni F, Rabini A, Pavone N, Pasquini A, Ferraro F, Mazza A, Nesta M, Iafrancesco M, Colizzi C, Massetti M. Psychological Effects of Skin Incision Size in Minimally Invasive Valve Surgery Patients. Innovations (Phila). 2020;15:532-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Arezzo A. The past, the present, and the future of minimally invasive therapy in laparoscopic surgery: a review and speculative outlook. Minim Invasive Ther Allied Technol. 2014;23:253-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Rao PP, Bhagwat SM, Rane A, Rao PP. The feasibility of single port laparoscopic cholecystectomy: a pilot study of 20 cases. HPB (Oxford). 2008;10:336-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 107] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 21. | Remzi FH, Kirat HT, Kaouk JH, Geisler DP. Single-port laparoscopy in colorectal surgery. Colorectal Dis. 2008;10:823-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 425] [Cited by in RCA: 405] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 22. | Blinman T, Ponsky T. Pediatric minimally invasive surgery: laparoscopy and thoracoscopy in infants and children. Pediatrics. 2012;130:539-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 65] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 23. | Jensen SAS, Fonnes S, Gram-Hanssen A, Andresen K, Rosenberg J. Low long-term incidence of incisional hernia after cholecystectomy: A systematic review with meta-analysis. Surgery. 2021;169:1268-1277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Lima DL, Lima RNCL, Dos Santos DC, Shadduck PP, Carvalho GL, Malcher F. Which Cholecystectomy Technique Would Surgeons Prefer on Themselves? Surg Laparosc Endosc Percutan Tech. 2020;30:495-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 25. | Deng L, Xiong J, Xia Q. Single-incision vs conventional three-incision laparoscopic appendectomy: A meta-analysis of randomized controlled trials. J Evid Based Med. 2017;10:196-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 26. | Aly OE, Black DH, Rehman H, Ahmed I. Single incision laparoscopic appendicectomy vs conventional three-port laparoscopic appendicectomy: A systematic review and meta-analysis. Int J Surg. 2016;35:120-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 47] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 27. | Pan MX, Jiang ZS, Cheng Y, Xu XP, Zhang Z, Qin JS, He GL, Xu TC, Zhou CJ, Liu HY, Gao Y. Single-incision vs three-port laparoscopic cholecystectomy: prospective randomized study. World J Gastroenterol. 2013;19:394-398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 38] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 28. | Lee W, Roh YH, Kang SH, Kim CY, Choi Y, Han HS, Han HJ, Song TJ, Kang CM, Lee WJ, Choi SH, Jeong SY, Hong TH, You YK, Lee JH, Moon JI, Choi IS. The chronological change of indications and outcomes for single-incision laparoscopic cholecystectomy: a Korean multicenter study. Surg Endosc. 2021;35:3025-3032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Poon JT, Cheung CW, Fan JK, Lo OS, Law WL. Single-incision vs conventional laparoscopic colectomy for colonic neoplasm: a randomized, controlled trial. Surg Endosc. 2012;26:2729-2734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 153] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 30. | Hoyuela C, Juvany M, Carvajal F. Single-incision laparoscopy vs standard laparoscopy for colorectal surgery: A systematic review and meta-analysis. Am J Surg. 2017;214:127-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 31. | Hebbar M, Riaz W, Sains P, Baig MK, Sajid MS. Meta-analysis of randomized controlled trials only exploring the role of single incision laparoscopic surgery vs conventional multiport laparoscopic surgery for colorectal resections. Transl Gastroenterol Hepatol. 2018;3:30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | Lee YS, Kim JH, Kim HJ, Lee SC, Kang BM, Kim CW, Lim SW, Lee SH, Kim JG. Short-term Outcomes of Single-port Versus Multiport Laparoscopic Surgery for Colon Cancer: The SIMPLE Multicenter Randomized Clinical Trial. Ann Surg. 2021;273:217-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 33. | Ross S, Roddenbery A, Luberice K, Paul H, Farrior T, Vice M, Patel K, Rosemurgy A. Laparoendoscopic single site (LESS) vs. conventional laparoscopic fundoplication for GERD: is there a difference? Surg Endosc. 2013;27:538-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 34. | Moreno-Sanz C, Morandeira-Rivas A, Sedano-Vizcaino C, Tenías-Burillo JM, Román-Ortíz C, de la Espada JB. Single-incision laparoscopic bariatric surgery: a systematic review. Surg Obes Relat Dis. 2015;11:248-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 35. | Jing K, Shuo-Dong W, Ying F, Yu W. Feasibility and safety of single-incision laparoscopic surgery in gastric benign and malignant diseases. Gastroenterol Res Pract. 2014;2014:782035. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 36. | Sajid MS, Khawaja AH, Sayegh M, Baig MK. A systematic review comparing single-incision vs multi-incision laparoscopic surgery for inguinal hernia repair with mesh. Int J Surg. 2016;29:25-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 37. | Struecker B, Haber P, Öllinger R, Bahra M, Pascher A, Pratschke J, Schmelzle M. Comparison of Single-Port Versus Standard Multiport Left Lateral Liver Sectionectomy. Surg Innov. 2018;25:136-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 38. | Weiss M, Mittermair C, Brunner E, Schirnhofer J, Obrist C, Pimpl K, Hell T, Weiss H. Inline radiofrequency pre-coagulation simplifies single-incision laparoscopic minor liver resection. J Hepatobiliary Pancreat Sci. 2015;22:831-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 39. | Saad MR, Choi Y, Han HS, Yoon YS, Cho JY, Lee JS, Lee BR. Solo single-incision laparoscopic liver resection: a cohort series. ANZ J Surg. 2020;90:1108-1111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 40. | Mittermair C, Weiss M, Schirnhofer J, Brunner E, Fischer K, Obrist C, de Cillia M, Kemmetinger V, Gollegger E, Hell T, Weiss H. The Shift from Multiport to Single Port Increases the Amount of Bleeding in Laparoscopic Major Hepatectomy. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 41. | Kim EY, You YK, Kim DG, Lee SH, Han JH, Park SK, Na GH, Hong TH. Dual-incision laparoscopic spleen-preserving distal pancreatectomy. Ann Surg Treat Res. 2015;88:174-177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 42. | Mittermair C, Weiss M, Schirnhofer J, Brunner E, Obrist C, Biebl M, Hell T, Weiss H. Dual trocar laparoscopy improves reduced-port surgery of the distal pancreas. Minim Invasive Ther Allied Technol. 2021;1-7. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 43. | Morales-Conde S, Peeters A, Meyer YM, Antoniou SA, Del Agua IA, Arezzo A, Arolfo S, Yehuda AB, Boni L, Cassinotti E, Dapri G, Yang T, Fransen S, Forgione A, Hajibandeh S, Mazzola M, Migliore M, Mittermair C, Mittermair D, Morandeira-Rivas A, Moreno-Sanz C, Morlacchi A, Nizri E, Nuijts M, Raakow J, Sánchez-Margallo FM, Sánchez-Margallo JA, Szold A, Weiss H, Weiss M, Zorron R, Bouvy ND. European association for endoscopic surgery (EAES) consensus statement on single-incision endoscopic surgery. Surg Endosc. 2019;33:996-1019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |