Published online Nov 28, 2021. doi: 10.3748/wjg.v27.i44.7597
Peer-review started: April 27, 2021
First decision: June 13, 2021
Revised: July 23, 2021
Accepted: November 18, 2021
Article in press: November 18, 2021
Published online: November 28, 2021
Processing time: 211 Days and 14.5 Hours
Endoscopic management for difficult common bile duct (CBD) stones still presents a challenge for several reasons, including anatomic anomalies, patients’ individual conditions and stone features. In recent years, variable methods have emerged that have attributed to higher stone removal success rates, reduced cost and lower adverse events. In this review, we outline a stepwise approach in CBD stone management. As first line therapy, endoscopic sphincterotomy and large balloon dilation are recommended, due to a 30%-50% reduction of the use of mechanical lithotripsy. On the other hand, cholangioscopy-assisted lithotripsy has been increasingly reported as an effective and safe alternative technique to mechanical lithotripsy but remains to be reserved in special settings due to limited large-scale evidence. As discussed, findings suggest that management needs to be tailored to the patient’s characteristics and anatomical conditions. Furthermore, we evaluate the management of CBD stones in various surgical altered anatomy (Billroth II, Roux-en-Y and Roux-en-Y gastric bypass). Moreover, we could conclude that cholangioscopy-assisted lithotripsy needs to be evaluated for primary use, rather than following a failed management option. In addition, we discuss the importance of dissecting other techniques, such as the primary use of interventional endoscopic ultrasound for the management of CBD stones when other techniques have failed. In conclusion, we recognize that endoscopic sphincterotomy and large balloon dilation, mechanical lithotripsy and intraductal lithotripsy substantiate an indication to the management of difficult CBD stones, but emerging techniques are in rapid evolution with encouraging results.
Core Tip: The endoscopic management of difficult common bile (CBD) stones remains a challenge, whilst emerging techniques such as endoscopic sphincterotomy and large balloon dilation, mechanical lithotripsy and intraductal lithotripsy provide a procedural indication that align with the patient’s condition, comorbidities, feature of the CBD stone and the patient’s anatomical features. This review focuses on comprehensively outlining a stepwise approach for the management of difficult CBD stones and comparatively discusses indications depending on surgical altered anatomy and future indications in the management of difficult CBD stones.
- Citation: Tringali A, Costa D, Fugazza A, Colombo M, Khalaf K, Repici A, Anderloni A. Endoscopic management of difficult common bile duct stones: Where are we now? A comprehensive review. World J Gastroenterol 2021; 27(44): 7597-7611
- URL: https://www.wjgnet.com/1007-9327/full/v27/i44/7597.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i44.7597
About 10%-15% of biliary stone extraction procedures are demanding and require additional endoscopic techniques in order to allow stone clearance[1]. Factors that influence the technical difficulty of common bile duct (CBD) endoscopic clearance can be attributed to the patient’s clinical condition, the stone’s characteristics and anatomical factors (Table 1). Furthermore, the concomitant presence of Mirizzi syndrome and/or primary sclerosing cholangitis are also agreed upon by experts to make stone extraction a challenging procedure[2,3].
| Category | Risk factors |
| Patient’s clinical condition | Age > 65 yr; Bleeding tendency; Very poor medical condition |
| Stone characteristics | Stone size > 15 mm; Barrel or square shaped; Multiple stones > 3; Hard stone consistency; Intrahepatic/cystic duct location |
| Anatomical factors | Anatomical CBD factors: Narrowing of the bile duct distal to the stone, sigmoid-shape CBD, distal CBD angulation > 135°, short distal CBD < 36 mm; Periampullary diverticulum; Duodenal stricture; Surgically altered anatomy (Roux-en-Y gastric bypass or Billroth II with long afferent limb) |
In accordance with the European Society of Gastrointestinal Endoscopy (ESGE) guidelines on endoscopic management of common bile duct stones, endoscopic sphincterotomy combined with endoscopic papillary large balloon dilation is considered the first line approach, reserving mechanical lithotripsy in case of failure[4]. Cholangioscopy-assisted lithotripsy has been increasingly reported as an effective and safe alternative technique to treat difficult CBD stones, even though its availability is still limited to referral centers[4,5]. Moreover, endoscopic management of CBD stones in patients with surgically altered anatomy (SAA) is technically demanding with a reduced rate of technical success[6]. Balloon assisted enteroscopy (BAE) has revealed to be effective in this setting, although its rate of failure has been reported to be up to 35%[7]. The use of interventional endoscopic ultrasonography (I-EUS) has been reserved to cases of BAE failure, due to its higher rate of adverse events when compared with BAE in previous reports[8-10]. Nevertheless, recent studies showed that I-EUS is efficacious with a low risk of adverse events, so it should be considered as first line treatment in expert hands and in referral centers[11]. The future of I-EUS requires the development of dedicated devices, making the procedure easier and safer with expanded indications[6,12]. Further studies will help to assess the role of I-EUS as the first approach for the management of CBD stones in patients with SAA. Finally, percutaneous cholangioscopy is also a novel alternative technique that should allow to treat difficult CBD stones in patients with SAA[13].
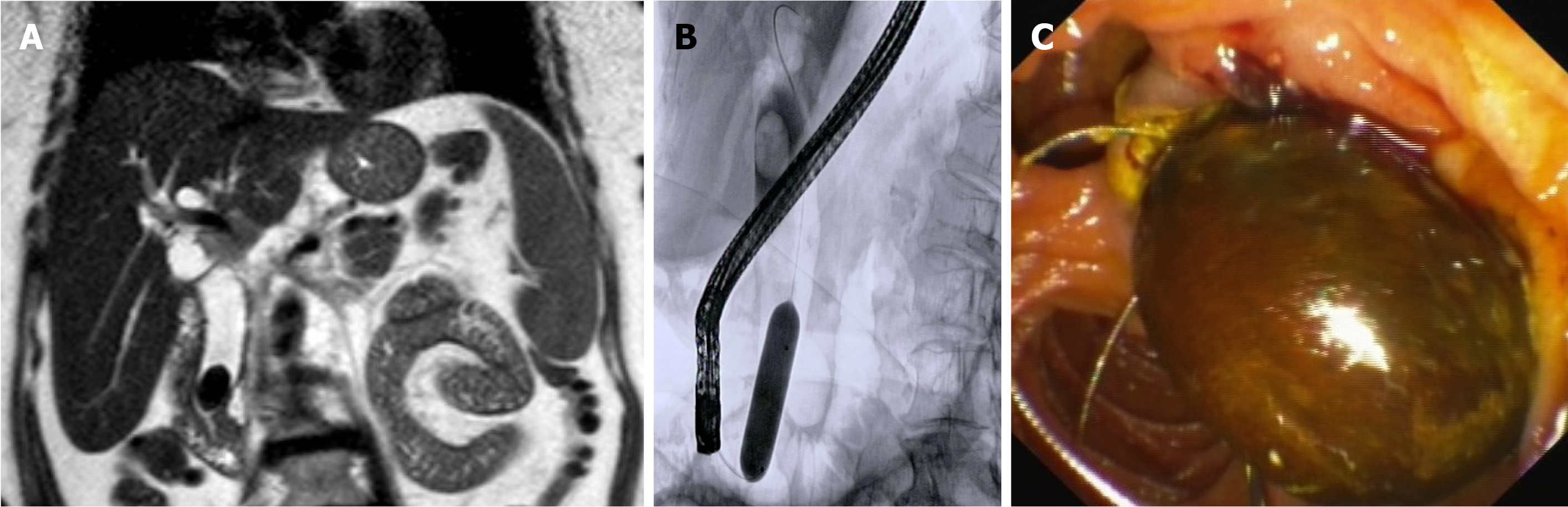
The first step is gaining access to the biliary tree, in order to remove the stone, which can be achieved by three different techniques: Endoscopic sphincterotomy (EST), endoscopic papillary large balloon dilation (EPLBD) and a combination of EST and EPLBD [endoscopic sphincterotomy and large balloon dilation (ESLBD)]. Although the optimal choice remains debatable among endoscopists, the recently published ESGE guidelines[4] recommend ESLBD as the first-line approach to difficult CBD stones (in particular large stones), due to a 30%-50% reduction of the use of mechanical lithotripsy (ML) and a similar rate of technical success when compared to EST alone[14-20] (Figure 1).
However, balloon dilation is contraindicated in cases with distal biliary strictures, due to the increased risk of perforation[21], whereas EST increases the risk of bleeding in patients on antithrombotic agents[22]. A recently published systematic review and metanalysis including 13 randomized controlled trials conducted on 1990 patients[23] focused on the treatment of large CBD stones using the three techniques. Analyzing the surface under the cumulative ranking curve index, Lyu et al[23], concluded that EPLBD had the highest overall and initial success rates and the lowest probability of bleeding. ESLBD also had the lowest probabilities for the need for ML, risk of perforation, morbidity rates and risk of mortality. On the other hand, EST was associated with the lowest rates of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis (PEP) and cholangitis. However, when each outcome was analyzed on pooled network analysis, no significant differences among the three groups emerged. There are many limitations in this study: The definition of the success rate and post-procedure complications varied in the included studies, the details of the different endoscopic procedures, such as the size of the dilation balloon, differed in the studies and the patient’s characteristics changed among studies, such as bleeding predisposing factors and anatomical factors (e.g., the presence of a peripapillary diverticulum and the size of the distal bile duct). To conclude, the technique for removing difficult CBD stones is still debated among endoscopists and needs to be tailored to patient’s characteristics and anatomical conditions[24]. Higher numbers of high-quality trials are required.
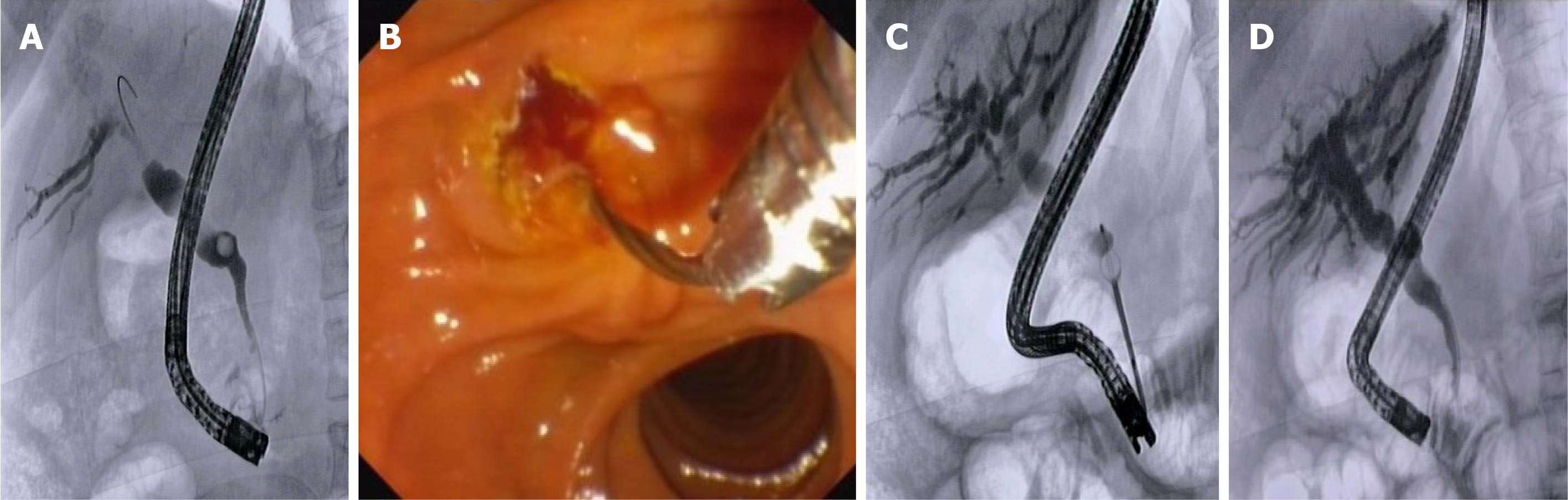
When the size of CBD stones, even after balloon dilation, exceeds the diameter of the distal CBD, ML should be performed (Figure 2). The success of ML has been reported to range between 79% and 96%[25-29], with a low mortality rate and an overall adverse events (AEs) rate of 3.5% in a multicenter study[30], including trapped/broken basket, wire fracture and broken handle perforation/duct injury. Even though previous studies have focused on the importance of stone size as the factor that hampers stone clearance[29], Garg et al[28] demonstrated that the only predictor of unsuccessful ML was the stone impaction into the CBD. This determined the inability to push the basket proximal to the stone or the incapability to open fully the basket to grasp the stone.
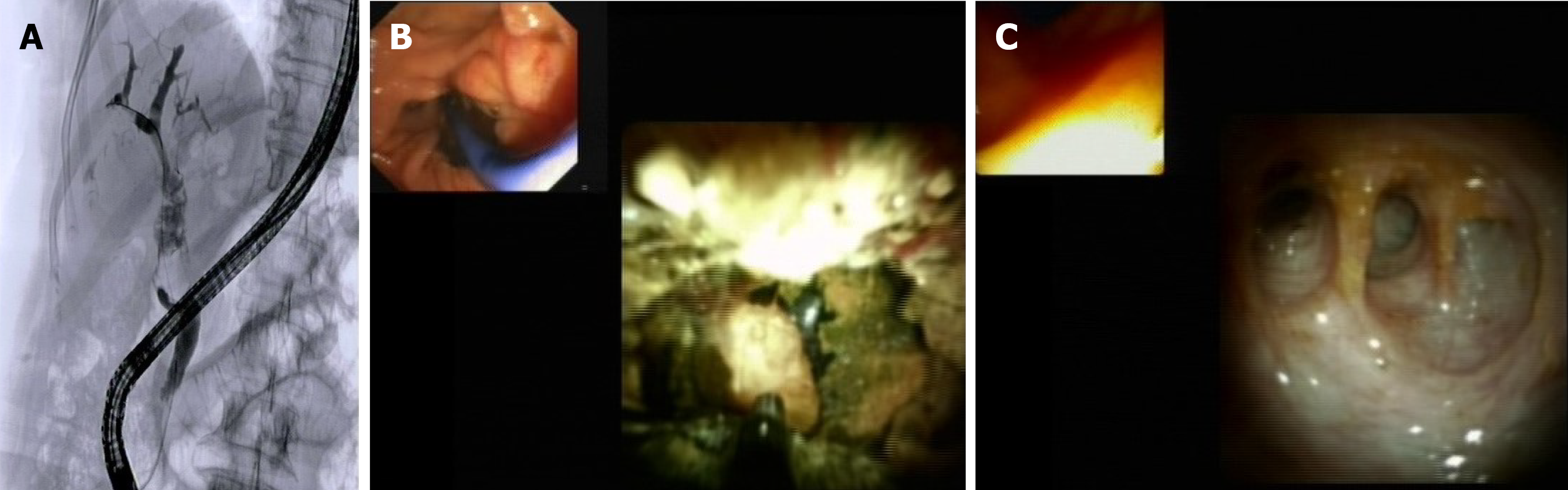
ML can require multiple sessions to achieve stone clearance, undergo AEs and still be ineffective for difficult CBD stones[31]. In such cases, cholangioscopy-assisted intraluminal lithotripsy with electrohydraulic (EHL) or laser lithotripsy (LL) is the technique of choice to fragment large stones under direct visualization. There are three cholangioscopy techniques available: The oldest “dual-operator” mother-baby approach, the “single-operator” mother-baby approach (Spyglass, Boston Scientific, Natick, MA, United States) and the “direct” technique using currently available ultrathin gastroscopes[32].
Each of the three cholangioscopy technique allows EHL or LL under direct visualization (Figure 3). Nevertheless, in regards to which specific type of cholangioscopy and lithotripsy to use, it depends on local expertise and availability, as mentioned in ESGE guidelines[4]. There are currently no studies that compare cholangioscopy techniques. Concerning the type of lithotripsy used, Veld et al[33] recently published a systematic review comparing LL, EHL and extracorporeal shock wave lithotripsy (ESWL) in the treatment of difficult CBD stones after a previously failed ERCP. In their study, LL had a significantly higher complete ductal clearance rate (95.1%) compared with EHL (88.4%) and ESWL (84.5%), while EHL had a higher post-procedural AEs rate (13.8%, including cholangitis, hemobilia and pancreatitis) compared with ESWL (8.4%) or LL (9.6%). In opposition to these results, a more recent meta-analysis[34] reported a superiority of EHL vs LL (mean successful endoscopic clearance rate 91.4% and 88.6%, respectively), explaining a more selective study inclusion than that made by Veld et al[33]. The last published meta-analysis comparing cholangioscopy-guided lithotripsy vs conventional therapy for complex bile duct stones[34] showed no significant difference between ERCP and cholangioscopy in terms of therapeutic success, AEs rate and mean fluoroscopy time, but a shorter mean procedure time for conventional ERCP methods were found. In detail, cholangioscopy-guided lithotripsy showed a successful endoscopic clearance rate of 88.29% [95% confidence interval (CI): 86.9%-90.7%], first session successful endoscopic clearance rate of 72.7% (95%CI: 69.9%-75.3%), mean procedure time of 47.50 ± 6 min for session, number of sessions to clear bile duct of 1.5 ± 0.18 and adverse event rate of 8.7% (95%CI: 7%-10.9%). The majority of patients in the considered studies had a history of failure to remove stones on prior ERCP attempt. Therefore, Galetti et al[34] concluded that cholangioscopy-guided lithotripsy should be reserved to cases where the conventional techniques failed to achieve initially stone clearance. The majority of data published by Galetti et al[34] are in line with an older meta-analysis by Korrapati et al[35]. Regarding AEs, cholangitis is the most frequently reported, while PEP and perforation rarely occur[35].
Cholangioscopy-assisted lithotripsy should be reserved to selected cases and in the setting of tertiary care centers due to its costs, complexity and AEs rate. However, an increasingly number of authors claim that cholangioscopy-assisted lithotripsy may be considered first-line therapy for patients with difficult CBD stones in order to avoid serial procedures[36-38] and decrease costs[39]. Moreover, this procedure must be performed at tertiary centers by expert endoscopists.
When conventional ML fails and intraluminal lithotripsy is not available, the ESGE guidelines suggest to perform ESWL[4]. However, this procedure often requires multiple sessions, the placement of a naso-biliary drainage and subsequent ERCP to extract stone fragments. Ductal clearance rate appeared lower compared with LL (53%-73% vs 83%-97%, respectively)[40,41] but similar to EHL (78.5% vs 74%, respectively)[42]. ESWL-related AEs, including mostly cholangitis and pancreatitis, range from 9%-35.7%[40,42].
When biliary stones remain irretrievable but patients still need biliary drainage due to the risk of cholangitis, the placement of a temporary plastic stent is highly recommended before a second attempt at stone extraction can be made[4]. Horiuchi et al[43] documented that stent placement for 2 mo is associated with large and/or multiple CBD stones becoming smaller and/or disappearing without any complications, with a successful stone removal of 93% on a second ERCP[43]. Likewise, the disintegration of stones depends on the continuous friction between the plastic stent and the stones, which produces stress forces on the stone[43]. In a recent retrospective study, Jang et al[44] compared the use of different stents (7-Fr rather than 10-Fr plastic stents) in this setting, showing that the mean stone size reduction did not differ between the stents (5.7 mm in the 7-Fr stent group and 5.5 mm in the 10-Fr stent group; P = 0.91). However, when performing multivariate analyses, 7-Fr double pigtail stents significantly improved the complete clearance rate. On the other hand, the reduction in stone size was greater in the double-stenting group than in the single-stenting group, but the use of a double stent did not alter the complete stone clearance rate[44]. Covered self-expandable metal stent have been also used as an alternative to plastic stents to drain CBD after unsuccessful difficult stone removal. However, their high cost has not been certainly related to improved benefits[45-48].
Endoscopic management in patients with SAA is still challenging for the endoscopists. Before performing ERCP, it is paramount to understand the anatomy and length of the afferent limb in order to select the appropriate approach, through the revision of the surgical report. The success of interventional endoscopy will depend on the correct choice of the endoscope and devices that should be tailored to the patient’s anatomy[49].
According to the ESGE guideline, a duodenoscope should be the first choice, reserving a forward-viewing endoscope (gastroscope, pediatric colonoscope, device assisted enteroscope) in case of failure[50]. Endoscopic sphincterotomy, where an inverted sphincterotome rather than precut following biliary stent placement in case of dedicated sphincterotome unavailability is used, is the standard of care in this setting. Furthermore, EPLBD could be used as an alternative method to sphincterotomy for CBD stones extraction, especially for stones larger than 10 mm[51,52]. Usually, the length of the afferent limb is short (less than 50 cm), but in cases of antecolic gastrojejunostomy, it could be too long to be reachable by a duodenoscope. In this case, a forward viewing endoscope, allowing better visualization and easier intubation of the afferent limb compared with the lateral viewing endoscope, should be used. However, duodenoscope makes biliary cannulation easier using the elevator, even though it emerged to be associated with a higher perforation rate when compared with the forward viewing endoscope. This is due to limited visualization, difficult control of the scope, and the need to apply more pressure to overcome looping[53,54]. However, according to a recently published review by Krutsri[53], in patients with Billroth II gastrectomy, the duodenoscope has an afferent limb intubation success rate ranging from 62.5%-100%, cannulation success rate 88.2%-100% and complication rate 0%-12.5%. On the other hand, gastroscope with or without cap is reported to have similar results with an afferent loop intubation success rate of 76.8%-100%, cannulation success rate 81.4%-100% and complication rate 0%-10%. A subsequent retrospective study comparing sideviewing duodenoscope and forwardviewing endoscope to perform ERCP in patients with Billroth II gastrectomy reported afferent loop intubation rates of 95.1% for the side-viewing duodenoscope and 100% for the forward-viewing endoscope (P = 0.49). The rates of reaching the papilla were 70.7% and 91.1%, respectively (P = 0.06). Cannulation success rate after reaching the papilla was 100% in the side-viewing duodenoscope group and 90.3% in the forward-viewing endoscope group[55].
In 2015, Bove et al[56] reported a 30-year experience, showing that, in tertiary referral centers, patients with Billroth II (BII) that underwent ERCP had similar rates of morbidity and mortality when compared with patients with normal anatomy. In a recent systematic review and meta-analysis, Park et al[57] compared the efficacy and safety of forward viewing vs lateral viewing endoscopes and demonstrated that there was no statistically significant difference between the two endoscopes.
In referral centers, device-assisted enteroscopies (DAE) could be the first option because of higher technical success rate and lower adverse events, when compared with duodenoscopes and forward viewing endoscopes[53]. The majority of CBD stones in patients with Billroth II anatomy can still be removed by standard techniques such as EST and EPBD.
In a recent retrospective study, Duo et al[58] analyzed the risk factors for technical ERCP failure in Billroth II anatomy, demonstrating that in two or more CBD stones where the largest CBD stone measures to 12 mm or larger in size, stone characteristics for failed stone removal were included. Moreover, after the first ERCP attempt, Braun anastomosis and the use of no cap-assisted gastroscope were risk factors for technical failure of ERCP in this patients’ cluster[58]. The initial stone removal rates of EPLBD have been reported to range from 66.7%-92.5%, while the overall stone clearance rates were from 96%-100%[51,59,60]. EPLBD, with or without EST, showed a high rate of first session stone clearance, reducing the need of endoscopic ML[51]. EPLBD has resulted to be associated with higher risk of post-ERCP pancreatitis in some studies[61-63], unlike most of the recent papers which showed the efficacy of EPLBD without increasing adverse events, including PEP[59,64]. On the other hand, EST is associated with a higher risk of bleeding[65]. However, sometimes lithotripsy is necessary to achieve stone clearance, especially when stones are too large to extract even after EPLBD, or when EPLBD is too risky in cases of distal bile duct narrowing or stricture[66].
There are three treatment options for lithotripsy: Endoscopic ML, cholangioscopic guided lithotripsy (LL or EHL) and ESWL. ML is a first treatment option, although it failed in cases where bile duct stones were larger than 2-3 cm, due to the difficulty to catch with a mechanical lithotriptor. In those cases, intraductal lithotripsy could be used, although cholangioscopy is difficult to carry out in patients with SAA. In these setting of patients, ESWL should be considered as a second option. However, endoscopic naso-biliary drainage is necessary before performing ESWL, which has a lower efficacy compared to LL or EHL[40].
Finally, EUS-guided intraductal lithotripsy or percutaneous transhepatic biliary drainage should be considered if ESWL is ineffective. In the percutaneous transhepatic biliary drainage approach, CBD stones are extracted in the antegrade fashion after balloon dilation of the papilla. In cases with large CBD stones, percutaneous transhepatic cholangioscopy with intraductal lithotripsy or ESWL could be attempted to facilitate stone removal. EUS-guided approach has gained popularity in the management of bile duct stones in patients with BII anatomy. In a retrospective study[9], EUS-guided antegrade (EUS-AG) treatment had a technical success rate of 72%, due to the technical difficulty of the antegrade stone extraction. Moreover, mechanical or intraductal lithotripsy, through an enterobiliary fistula after fistula maturation, could be made[67].
Roux en Y reconstruction can be divided in Roux en Y without gastric bypass (e.g., Roux en Y gastrojejunostomy, Roux en Y hepaticojejunostomy, pancreatico-duodenectomy) and with gastric bypass (RYGB). Roux-en-Y reconstruction, compared to BII surgery, results in a longer and tortuous limb, increasing the difficulty to reach the papilla. In this setting, patients should be managed in referral centers where DAEs are the first option[68], with a reported cannulation rate ranging from 58%-95.6%, and an AEs rate between 7% and 10%, with a perforation rate of 0%-3.2%[69,70].
A systematic review and meta-analysis showed that BAE has a high diagnostic and procedural success rate in patients with Roux-en-Y reconstruction (69.4% and 61.7%, respectively), with an overall AEs rate of 6.5%[71]. Different studies have shown that there is no superiority among different DAE methods [single balloon enteroscopy (SBE), double balloon enteroscopy (DBE) and spiral enteroscopy][72]. Nevertheless, three systematic review and meta-analyses demonstrated better results for DBE compared to SBE (the success rate of reaching the papilla and treatment were 89.7% and 63.5% for DBE and 80.9% and 61.7% for SBE, respectively)[71,73,74].
The success rate of forward viewing endoscopes could be increased by using an underwater cap assisted technique, which combines the use of a cap applied to the tip of a pediatric colonoscope, with the injection of water as an alternative medium to carbon dioxide or air to distend the bowel lumen. It appeared that on one side the underwater technique reduces loop formation and bowel distension, while on the other side, the use of a cap improves the visualization of the papilla and helps in maintaining a stable position[75].
Even after cannulation, extraction of CBD stones can be difficult in patient with Roux-en-Y reconstruction, although different techniques have been described in this cluster of patients. EPLBD has been reported to achieve complete stone removal on a single-session in 66.7%-100%, while overall complete stone removal was obtained in 96.7%-100% of cases[49]. ML can be used, even though it is often technically challenging during enteroscopy-assisted ERCP and may fail.
Therefore, direct peroral cholangioscopy, through direct insertion of an ultra-slim endoscope or an enteroscope into the bile duct, allowing to perform lithotripsy, has been described in some case reports[76-80]. Some authors have also described the placement of an overtube through the scope, which allows the insertion of a cholangioscope (Spyglass, Boston Scientific) and direct lithotripsy[81,82].
EUS-AG stone treatment has also gained popularity. Biliary access is achieved from the stomach or jejunum under EUS-guidance, using a guidewire that is passed through the ampulla into the duodenum. Then the ampulla is dilated using a balloon, and finally, CBD stones are pushed into the duodenum using a stone extraction balloon.
The reason for technical failure is the failed puncture of the intrahepatic bile duct, guidewire passage and difficulty to stone extraction due to large stones size. However, these reasons could be overcome using large balloon dilation. Nevertheless, the maximum balloon size is limited to the size of the distal CBD, therefore intraductal lithotripsy is needed in cases with stones larger than the size of the distal CBD, increasing the risk of bile leak. However, a two-step approach has been proposed to prevent bile leaks and allowing safe usage of ML and cholangioscopy in EUS-AG stone treatment[67].
Mechanical lithotriptor can be introduced over the guidewire and into the bile duct, through the fistula. A fistula dilation up to 10-F using a plastic stent, a fully covered self-expandable metal stent after endoscopic ultrasound-guided hepaticogastrostomy or endoscopic ultrasound-guided hepaticojejunostomy, should be made in order to prevent bile leak and to allow easy access of the cholangioscope into the biliary system[83].
For the management of complex CBD stones, with the use of DAEs in patients with SAA has been studied in larger cohort of patients, EUS-guided therapy in this setting has been increasingly reported in case reports[8-11,84-86]. There are advantages and disadvantages in enteroscope-assisted stone management and EUS-guided interventions in patients with Roux-en-Y anatomy.
Enteroscopy-assisted ERCP uses the physiological biliary access and has a lower risk of bile duct leakage, although scope insertion can be challenging. On the other hand, EUS-guided approach involving the puncture of the left intrahepatic bile duct has a lower risk of bile leak but can be challenging when the intrahepatic bile duct is minimally dilated. Enteroscopy-assisted ERCP should be the first approach, reserving EUS-guided approach in case of failure as a salvage technique. We should keep in mind that enteroscopy-assisted ERCP and EUS-AG stone treatment need expertise as well as dedicated devices, therefore these procedures should be performed by skilled endoscopists in high volume referral centers.
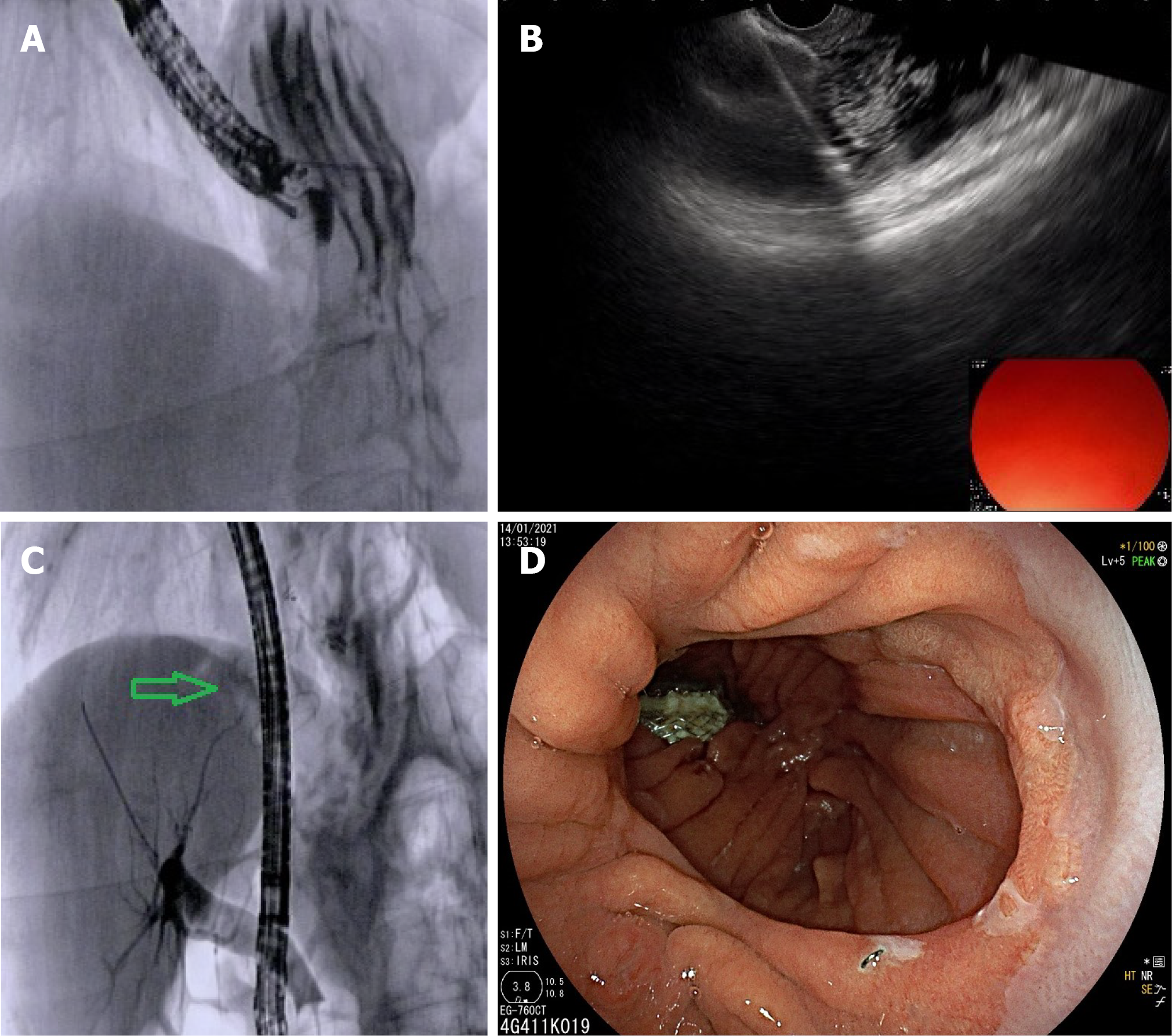
The treatment of CBD stones in patients who underwent weight loss surgery, especially RYGB, is challenging due to difficult access to the CBD. In fact, in Roux en-Y reconstruction, the afferent limb length can be more than 200 cm, with sharp angulation of the jejunojejunal anastomosis, severe adhesion and looping of the scope. Moreover, the incidence of symptomatic gallbladder disease is around 15% after significant weight loss, therefore prophylactic cholecystectomy has been suggested[87]. The percentage of therapeutic success of ERCP using a pediatric colonoscope or with DAEs has been reported around 60%[88]. New techniques to perform ERCP in this setting are EUS-directed transgastric ERCP (EDGE) and laparoscopic-assisted transgastric ERCP (LA-ERCP), which reach a success rates of 80%-100%[89-91]. However, both procedures have some limits. EDGE requires expertise in interventional EUS and ERCP, has higher costs and can be associated with stent migration and subsequent perforation[92,93] and permanent gastro-gastric fistula with weight regain[94]. On the other hand, LA-ERCP needs coordination between surgeon and endoscopist with a gastrostomy tube left in situ, if multiple ERCP procedures are required to obtain stones clearance[95].
EDGE is a two-step procedure; procedures can be performed in the same session or in two separate sessions (Figure 4). Single session EDGE is associated with a higher risk of perforation due to lumen apposing metal stent dislodgement, while dual session has a lower perforation risk, but it requires 10-14 d interval to allow fistula maturation. A shortened interval dual session (2-4 d) has been proposed to overcome this limitation, decreasing the risk of intraprocedural 20 mm lumen apposing metal stent dislodgement and allowing a timely transgastric ERCP[96].
An international, multicenter trial comparing EUS-guided gastro-gastrostomy-assisted ERCP vs enteroscopy-assisted ERCP (e-ERCP) in patients with RYGB has shown that EUS-guided gastro-gastrostomy-assisted ERCP may be superior to e-ERCP in terms of higher technical success and shorter procedural time, with similar safety profile[97]. LA-ERCP provides the opportunity to perform cholecystectomy concomitantly with CBD stones clearance, in case the gallbladder is still in place[98].
CBD stones after liver transplantation have an incidence between 4% and 10% of cases[99]. Biliary strictures are the major predisposing risk factor for biliary CBD stones, occurring in up to 90% of liver transplant patients with biliary stones[100]. Other possible agents for stone formation are cold ischemia, hyperlipidemia, hypercholesterolemia, infections and cyclosporine assumption[100,101]. Biliary stones in post-liver transplantation patients may cause severe complications such as pancreatitis, biliary infections and biliary cirrhosis, which can drastically worsen the graft’s course. The endoscopic management of CBD stones in this setting of patients is successful in over 90% of cases, although the presence of anastomotic strictures results in a challenging and demanding procedure and increases the difficulty of stones removal[99]. In this context the strictures have to be treated simultaneously with stone extraction, using balloon dilation and mechanical lithotripsy and reserving the use of cholangioscopy-assisted lithotripsy in case of failure[102]. CBD stones may be mistaken with biliary casts, which occur in 2.5%-18% of post-liver transplant patients due to hepatic ischemic injury and are associated with poorer graft survival[103]. The differential diagnosis is mainly based on cholangiography features in addition to the endoscopist experience and can be confirmed by cholangioscopy direct visualization. This is fundamental to direct the treatment approach.
The use of cholangioscopy-assisted lithotripsy in patients with difficult CBD stones as a first step rather than after failed traditional treatment, need to be assessed in randomized controlled trials. Many endoscopic techniques have been used in patients with difficult CBD stones and altered anatomy, with variable results. Percutaneous transhepatic cholangioscopy, which has been recently reported as a novel and alternative approach for patients with SAA, allows access to the biliary tree and stones fragmentation under direct visualization[13,104,105]. However, efficacy and safety of its use need to be further investigated.
EUS guided interventions for biliary drainage after failed ERCP are in rapid evolution[106-107], including management of CBD stones in patients with normal anatomy when other techniques have failed[108]. Two retrospective studies and a recent review have compared EUS-rendezvous with precut papillotomy technique, showing that treatment success was significantly higher for EUS-rendezvous than for those with precut papillotomy, without significant differences in terms of complication rate[109-111]. Therefore, in tertiary referral centers, EUS-rendezvous could be used instead of precut papillotomy. The role of EUS-guided biliary treatment in patients with SAA should be investigated as primary technique in well-designed studies comparing safety and efficacy of EUS-guided interventions with enteroscopy-assisted ERCP. Finally, regarding patients with RYGB, more studies are needed in order to assess the role of the three different methods used in this setting (EDGE, LA-ERCP, e-ERCP), allowing endoscopists to tailor the technique to the patient.
The step-up approach involving ESLBD, ML and intraductal lithotripsy for patients with difficult CBD stones has been quite well validated. On the other hand, many different techniques involving the use of EUS in this setting are in rapid evolution with encouraging results. In patients with SAA, the endoscopic management of CBD stones is still challenging and should be managed in referral centers. The role of EDGE compared with LA-ERCP, e-ERCP as well as the efficacy and safety of percutaneous transhepatic cholangioscopy need to be evaluated in further well-designed studies. Finally, the definition of difficult CBD stones includes many different clinical scenarios with distinctive outcomes depending on the treatment choice. The correct pre-operative evaluation of the patient could help in choosing the best treatment strategy, in order to avoid unnecessary, ineffective ERCP session/attempt and can offer the best therapeutical approach to our patients.
Provenance and peer review: Invited article; Externally peer reviewed.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ozkan OF, Pelaez-Luna M S-Editor: Wu YXJ L-Editor: Filipodia P-Editor: Wu YXJ
| 1. | Binmoeller KF, Brückner M, Thonke F, Soehendra N. Treatment of difficult bile duct stones using mechanical, electrohydraulic and extracorporeal shock wave lithotripsy. Endoscopy. 1993;25:201-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 170] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 2. | Kim HJ, Choi HS, Park JH, Park DI, Cho YK, Sohn CI, Jeon WK, Kim BI, Choi SH. Factors influencing the technical difficulty of endoscopic clearance of bile duct stones. Gastrointest Endosc. 2007;66:1154-1160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 89] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 3. | Trikudanathan G, Navaneethan U, Parsi MA. Endoscopic management of difficult common bile duct stones. World J Gastroenterol. 2013;19:165-173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 80] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | Manes G, Paspatis G, Aabakken L, Anderloni A, Arvanitakis M, Ah-Soune P, Barthet M, Domagk D, Dumonceau JM, Gigot JF, Hritz I, Karamanolis G, Laghi A, Mariani A, Paraskeva K, Pohl J, Ponchon T, Swahn F, Ter Steege RWF, Tringali A, Vezakis A, Williams EJ, van Hooft JE. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019;51:472-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 463] [Cited by in RCA: 373] [Article Influence: 62.2] [Reference Citation Analysis (0)] |
| 5. | Doshi B, Yasuda I, Ryozawa S, Lee GH. Current endoscopic strategies for managing large bile duct stones. Dig Endosc. 2018;30 Suppl 1:59-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 6. | Katanuma A, Hayashi T, Kin T, Toyonaga H, Honta S, Chikugo K, Ueki H, Ishii T, Takahashi K. Interventional endoscopic ultrasonography in patients with surgically altered anatomy: Techniques and literature review. Dig Endosc. 2020;32:263-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 7. | Katanuma A, Yane K, Osanai M, Maguchi H. Endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy using balloon-assisted enteroscope. Clin J Gastroenterol. 2014;7:283-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Itoi T, Sofuni A, Tsuchiya T, Ijima M, Iwashita T. Endoscopic ultrasonography-guided transhepatic antegrade stone removal in patients with surgically altered anatomy: case series and technical review (with videos). J Hepatobiliary Pancreat Sci. 2014;21:E86-E93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Iwashita T, Nakai Y, Hara K, Isayama H, Itoi T, Park DH. Endoscopic ultrasound-guided antegrade treatment of bile duct stone in patients with surgically altered anatomy: a multicenter retrospective cohort study. J Hepatobiliary Pancreat Sci. 2016;23:227-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 77] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 10. | Mukai S, Itoi T, Sofuni A, Tsuchiya T, Tanaka R, Tonozuka R, Honjo M, Fujita M, Yamamoto K, Nagakawa Y. EUS-guided antegrade intervention for benign biliary diseases in patients with surgically altered anatomy (with videos). Gastrointest Endosc. 2019;89:399-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 85] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 11. | Hosmer A, Abdelfatah MM, Law R, Baron TH. Endoscopic ultrasound-guided hepaticogastrostomy and antegrade clearance of biliary lithiasis in patients with surgically-altered anatomy. Endosc Int Open. 2018;6:E127-E130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 12. | Mukai S, Tsuchiya T, Itoi T. Interventional endoscopic ultrasonography for benign biliary diseases in patients with surgically altered anatomy. Curr Opin Gastroenterol. 2019;35:408-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 13. | Tripathi N, Mardini H, Koirala N, Raissi D, Emhmed Ali SM, Frandah WM. Assessing the utility, findings, and outcomes of percutaneous transhepatic cholangioscopy with SpyglassTM Direct visualization system: a case series. Transl Gastroenterol Hepatol. 2020;5:12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 14. | Teoh AYB, Cheung FKY, Hu B, Pan YM, Lai LH, Chiu PWY, Wong SKH, Chan FKL, Lau JYW. Randomized trial of endoscopic sphincterotomy with balloon dilation versus endoscopic sphincterotomy alone for removal of bile duct stones. Gastroenterology. 2013;144:341-345.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 94] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 15. | Li G, Pang Q, Zhang X, Dong H, Guo R, Zhai H, Dong Y, Jia X. Dilation-assisted stone extraction: an alternative method for removal of common bile duct stones. Dig Dis Sci. 2014;59:857-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Jun Bo Q, Li Hua X, Tian Min C, Liu Gen G, Yan Mei Y, Hua Sheng L. Small Endoscopic Sphincterotomy plus Large-Balloon Dilation for Removal of Large Common Bile Duct Stones during ERCP. Pak J Med Sci. 2013;29:907-912. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Feng Y, Zhu H, Chen X, Xu S, Cheng W, Ni J, Shi R. Comparison of endoscopic papillary large balloon dilation and endoscopic sphincterotomy for retrieval of choledocholithiasis: a meta-analysis of randomized controlled trials. J Gastroenterol. 2012;47:655-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 84] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 18. | Madhoun MF, Wani S, Hong S, Tierney WM, Maple JT. Endoscopic papillary large balloon dilation reduces the need for mechanical lithotripsy in patients with large bile duct stones: a systematic review and meta-analysis. Diagn Ther Endosc. 2014;2014:309618. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Yang XM, Hu B. Endoscopic sphincterotomy plus large-balloon dilation vs endoscopic sphincterotomy for choledocholithiasis: a meta-analysis. World J Gastroenterol. 2013;19:9453-9460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 36] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 20. | Jin PP, Cheng JF, Liu D, Mei M, Xu ZQ, Sun LM. Endoscopic papillary large balloon dilation vs endoscopic sphincterotomy for retrieval of common bile duct stones: a meta-analysis. World J Gastroenterol. 2014;20:5548-5556. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 40] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 21. | Park SJ, Kim JH, Hwang JC, Kim HG, Lee DH, Jeong S, Cha SW, Cho YD, Kim HJ, Moon JH, Park SH, Itoi T, Isayama H, Kogure H, Lee SJ, Jung KT, Lee HS, Baron TH, Lee DK. Factors predictive of adverse events following endoscopic papillary large balloon dilation: results from a multicenter series. Dig Dis Sci. 2013;58:1100-1109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 82] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 22. | Hakuta R, Kogure H, Nakai Y, Hamada T, Noguchi K, Saito K, Saito T, Takahara N, Mizuno S, Yagioka H, Ito Y, Tada M, Isayama H, Koike K. Endoscopic papillary large balloon dilation without sphincterotomy for users of antithrombotic agents: A multicenter retrospective study. Dig Endosc. 2019;31:316-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Lyu Y, Cheng Y, Wang B, Zhao S, Chen L. Comparison of the Efficacy and Safety of Three Endoscopic Methods to Manage Large Common Bile Duct Stones: A Systematic Review and Network Meta-Analysis. J Laparoendosc Adv Surg Tech A. 2021;31:443-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Anderloni A. Difficult common bile duct stones: still "difficult" or just... "different"? Endoscopy. 2020;52:429-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Chang WH, Chu CH, Wang TE, Chen MJ, Lin CC. Outcome of simple use of mechanical lithotripsy of difficult common bile duct stones. World J Gastroenterol. 2005;11:593-596. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 89] [Cited by in RCA: 78] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 26. | Stefanidis G, Viazis N, Pleskow D, Manolakopoulos S, Theocharis L, Christodoulou C, Kotsikoros N, Giannousis J, Sgouros S, Rodias M, Katsikani A, Chuttani R. Large balloon dilation vs. mechanical lithotripsy for the management of large bile duct stones: a prospective randomized study. Am J Gastroenterol. 2011;106:278-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 111] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 27. | Shaw MJ, Mackie RD, Moore JP, Dorsher PJ, Freeman ML, Meier PB, Potter T, Hutton SW, Vennes JA. Results of a multicenter trial using a mechanical lithotripter for the treatment of large bile duct stones. Am J Gastroenterol. 1993;88:730-733. [PubMed] |
| 28. | Garg PK, Tandon RK, Ahuja V, Makharia GK, Batra Y. Predictors of unsuccessful mechanical lithotripsy and endoscopic clearance of large bile duct stones. Gastrointest Endosc. 2004;59:601-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 93] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 29. | Cipolletta L, Costamagna G, Bianco MA, Rotondano G, Piscopo R, Mutignani M, Marmo R. Endoscopic mechanical lithotripsy of difficult common bile duct stones. Br J Surg. 1997;84:1407-1409. [PubMed] |
| 30. | Thomas M, Howell DA, Carr-Locke D, Mel Wilcox C, Chak A, Raijman I, Watkins JL, Schmalz MJ, Geenen JE, Catalano MF. Mechanical lithotripsy of pancreatic and biliary stones: complications and available treatment options collected from expert centers. Am J Gastroenterol. 2007;102:1896-1902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 74] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 31. | Lee SH, Park JK, Yoon WJ, Lee JK, Ryu JK, Kim YT, Yoon YB. How to predict the outcome of endoscopic mechanical lithotripsy in patients with difficult bile duct stones? Scand J Gastroenterol. 2007;42:1006-1010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 32. | Tringali A, Lemmers A, Meves V, Terheggen G, Pohl J, Manfredi G, Häfner M, Costamagna G, Devière J, Neuhaus H, Caillol F, Giovannini M, Hassan C, Dumonceau JM. Intraductal biliopancreatic imaging: European Society of Gastrointestinal Endoscopy (ESGE) technology review. Endoscopy. 2015;47:739-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 33. | Veld JV, van Huijgevoort NCM, Boermeester MA, Besselink MG, van Delden OM, Fockens P, van Hooft JE. A systematic review of advanced endoscopy-assisted lithotripsy for retained biliary tract stones: laser, electrohydraulic or extracorporeal shock wave. Endoscopy. 2018;50:896-909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 34. | Galetti F, Moura DTH, Ribeiro IB, Funari MP, Coronel M, Sachde AH, Brunaldi VO, Franzini TP, Bernardo WM, Moura EGH. Cholangioscopy-guided lithotripsy vs. conventional therapy for complex bile duct stones: a systematic review and meta-analysis. Arq Bras Cir Dig. 2020;33:e1491. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 35. | Korrapati P, Ciolino J, Wani S, Shah J, Watson R, Muthusamy VR, Klapman J, Komanduri S. The efficacy of peroral cholangioscopy for difficult bile duct stones and indeterminate strictures: a systematic review and meta-analysis. Endosc Int Open. 2016;4:E263-E275. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 81] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 36. | Anderloni A, Auriemma F, Fugazza A, Troncone E, Maia L, Maselli R, Carrara S, D'Amico F, Belletrutti PJ, Repici A. Direct peroral cholangioscopy in the management of difficult biliary stones: a new tool to confirm common bile duct clearance. Results of a preliminary study. J Gastrointestin Liver Dis. 2019;28:89-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 37. | Angsuwatcharakon P, Kulpatcharapong S, Ridtitid W, Boonmee C, Piyachaturawat P, Kongkam P, Pareesri W, Rerknimitr R. Digital cholangioscopy-guided laser versus mechanical lithotripsy for large bile duct stone removal after failed papillary large-balloon dilation: a randomized study. Endoscopy. 2019;51:1066-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 38. | Maydeo AP, Rerknimitr R, Lau JY, Aljebreen A, Niaz SK, Itoi T, Ang TL, Reichenberger J, Seo DW, Ramchandani MK, Devereaux BM, Lee JK, Goenka MK, Sud R, Nguyen NQ, Kochhar R, Peetermans J, Goswamy PG, Rousseau M, Bhandari SP, Angsuwatcharakon P, Tang RSY, Teoh AYB, Almadi M, Lee YN, Moon JH; SpyGlass AMEA Registry Group. Cholangioscopy-guided lithotripsy for difficult bile duct stone clearance in a single session of ERCP: results from a large multinational registry demonstrate high success rates. Endoscopy. 2019;51:922-929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 39. | Deprez PH, Garces Duran R, Moreels T, Furneri G, Demma F, Verbeke L, Van der Merwe SW, Laleman W. The economic impact of using single-operator cholangioscopy for the treatment of difficult bile duct stones and diagnosis of indeterminate bile duct strictures. Endoscopy. 2018;50:109-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 64] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 40. | Neuhaus H, Zillinger C, Born P, Ott R, Allescher H, Rösch T, Classen M. Randomized study of intracorporeal laser lithotripsy versus extracorporeal shock-wave lithotripsy for difficult bile duct stones. Gastrointest Endosc. 1998;47:327-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 95] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 41. | Jakobs R, Adamek HE, Maier M, Krömer M, Benz C, Martin WR, Riemann JF. Fluoroscopically guided laser lithotripsy versus extracorporeal shock wave lithotripsy for retained bile duct stones: a prospective randomised study. Gut. 1997;40:678-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 42] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 42. | Adamek HE, Maier M, Jakobs R, Wessbecher FR, Neuhauser T, Riemann JF. Management of retained bile duct stones: a prospective open trial comparing extracorporeal and intracorporeal lithotripsy. Gastrointest Endosc. 1996;44:40-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 59] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 43. | Horiuchi A, Nakayama Y, Kajiyama M, Kato N, Kamijima T, Graham DY, Tanaka N. Biliary stenting in the management of large or multiple common bile duct stones. Gastrointest Endosc. 2010;71:1200-1203.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 77] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 44. | Jang DK, Lee SH, Ahn DW, Paik WH, Lee JM, Lee JK, Ryu JK, Kim YT. Factors associated with complete clearance of difficult common bile duct stones after temporary biliary stenting followed by a second ERCP: a multicenter, retrospective, cohort study. Endoscopy. 2020;52:462-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 45. | Cerefice M, Sauer B, Javaid M, Smith LA, Gosain S, Argo CK, Kahaleh M. Complex biliary stones: treatment with removable self-expandable metal stents: a new approach (with videos). Gastrointest Endosc. 2011;74:520-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 46. | Minami A, Fujita R. A new technique for removal of bile duct stones with an expandable metallic stent. Gastrointest Endosc. 2003;57:945-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 47. | Hartery K, Lee CS, Doherty GA, Murray FE, Cullen G, Patchett SE, Mulcahy HE. Covered self-expanding metal stents for the management of common bile duct stones. Gastrointest Endosc. 2017;85:181-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 48. | Tringali A, Cintolo M, Mutignani M. Do we really need a fully covered self-expanding metal stent for the treatment of difficult common bile duct stones? Gastrointest Endosc. 2017;86:746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 49. | Nakai Y, Kogure H, Yamada A, Isayama H, Koike K. Endoscopic management of bile duct stones in patients with surgically altered anatomy. Dig Endosc. 2018;30 Suppl 1:67-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 50. | Testoni PA, Mariani A, Aabakken L, Arvanitakis M, Bories E, Costamagna G, Devière J, Dinis-Ribeiro M, Dumonceau JM, Giovannini M, Gyokeres T, Hafner M, Halttunen J, Hassan C, Lopes L, Papanikolaou IS, Tham TC, Tringali A, van Hooft J, Williams EJ. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:657-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 384] [Article Influence: 42.7] [Reference Citation Analysis (1)] |
| 51. | Jang HW, Lee KJ, Jung MJ, Jung JW, Park JY, Park SW, Song SY, Chung JB, Bang S. Endoscopic papillary large balloon dilatation alone is safe and effective for the treatment of difficult choledocholithiasis in cases of Billroth II gastrectomy: a single center experience. Dig Dis Sci. 2013;58:1737-1743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 52. | Cheng CL, Liu NJ, Tang JH, Yu MC, Tsui YN, Hsu FY, Lee CS, Lin CH. Double-balloon enteroscopy for ERCP in patients with Billroth II anatomy: results of a large series of papillary large-balloon dilation for biliary stone removal. Endosc Int Open. 2015;3:E216-E222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 53. | Krutsri C, Kida M, Yamauchi H, Iwai T, Imaizumi H, Koizumi W. Current status of endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy. World J Gastroenterol. 2019;25:3313-3333. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 48] [Cited by in RCA: 62] [Article Influence: 10.3] [Reference Citation Analysis (3)] |
| 54. | Kim MH, Lee SK, Lee MH, Myung SJ, Yoo BM, Seo DW, Min YI. Endoscopic retrograde cholangiopancreatography and needle-knife sphincterotomy in patients with Billroth II gastrectomy: a comparative study of the forward-viewing endoscope and the side-viewing duodenoscope. Endoscopy. 1997;29:82-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 82] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 55. | Coşkun O, Ödemiş B. A comparative study of side-viewing duodenoscope and forward-viewing gastroscope to perform endoscopic retrograde cholangiopancreatography in patients with Billroth II gastrectomy. Surg Endosc. 2021;35:4222-4230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 56. | Bove V, Tringali A, Familiari P, Gigante G, Boškoski I, Perri V, Mutignani M, Costamagna G. ERCP in patients with prior Billroth II gastrectomy: report of 30 years' experience. Endoscopy. 2015;47:611-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 57] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 57. | Park TY, Bang CS, Choi SH, Yang YJ, Shin SP, Suk KT, Baik GH, Kim DJ, Yoon JH. Forward-viewing endoscope for ERCP in patients with Billroth II gastrectomy: a systematic review and meta-analysis. Surg Endosc. 2018;32:4598-4613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (1)] |
| 58. | Li JS, Zou DW, Jin ZD, Shi XG, Chen J, Li ZS, Liu F. Predictive factors for extraction of common bile duct stones during endoscopic retrograde cholangiopancreatography in Billroth II anatomy patients. Surg Endosc. 2020;34:2454-2459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 59. | Choi CW, Choi JS, Kang DH, Kim BG, Kim HW, Park SB, Yoon KT, Cho M. Endoscopic papillary large balloon dilation in Billroth II gastrectomy patients with bile duct stones. J Gastroenterol Hepatol. 2012;27:256-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 60. | Kim KH, Kim TN. Endoscopic papillary large balloon dilation for the retrieval of bile duct stones after prior Billroth II gastrectomy. Saudi J Gastroenterol. 2014;20:128-133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 61. | Fujita N, Maguchi H, Komatsu Y, Yasuda I, Hasebe O, Igarashi Y, Murakami A, Mukai H, Fujii T, Yamao K, Maeshiro K; JESED Study Group. Endoscopic sphincterotomy and endoscopic papillary balloon dilatation for bile duct stones: A prospective randomized controlled multicenter trial. Gastrointest Endosc. 2003;57:151-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 167] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 62. | Yasuda I, Fujita N, Maguchi H, Hasebe O, Igarashi Y, Murakami A, Mukai H, Fujii T, Yamao K, Maeshiro K, Tada T, Tsujino T, Komatsu Y. Long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation for bile duct stones. Gastrointest Endosc. 2010;72:1185-1191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 90] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 63. | Tsujino T, Kawabe T, Komatsu Y, Yoshida H, Isayama H, Sasaki T, Kogure H, Togawa O, Arizumi T, Matsubara S, Ito Y, Nakai Y, Yamamoto N, Sasahira N, Hirano K, Toda N, Tada M, Omata M. Endoscopic papillary balloon dilation for bile duct stone: immediate and long-term outcomes in 1000 patients. Clin Gastroenterol Hepatol. 2007;5:130-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 79] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 64. | Kogure H, Tsujino T, Isayama H, Takahara N, Uchino R, Hamada T, Miyabayashi K, Mizuno S, Mohri D, Yashima Y, Kawakubo K, Sasaki T, Yamamoto N, Nakai Y, Hirano K, Sasahira N, Tada M, Koike K. Short- and long-term outcomes of endoscopic papillary large balloon dilation with or without sphincterotomy for removal of large bile duct stones. Scand J Gastroenterol. 2014;49:121-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 65. | Bergman JJ, van Berkel AM, Bruno MJ, Fockens P, Rauws EA, Tijssen JG, Tytgat GN, Huibregtse K. A randomized trial of endoscopic balloon dilation and endoscopic sphincterotomy for removal of bile duct stones in patients with a prior Billroth II gastrectomy. Gastrointest Endosc. 2001;53:19-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 100] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 66. | Kim TH, Kim JH, Seo DW, Lee DK, Reddy ND, Rerknimitr R, Ratanachu-Ek T, Khor CJ, Itoi T, Yasuda I, Isayama H, Lau JY, Wang HP, Chan HH, Hu B, Kozarek RA, Baron TH. International consensus guidelines for endoscopic papillary large-balloon dilation. Gastrointest Endosc. 2016;83:37-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 62] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 67. | Nakai Y, Isayama H, Koike K. Two-step endoscopic ultrasonography-guided antegrade treatment of a difficult bile duct stone in a surgically altered anatomy patient. Dig Endosc. 2018;30:125-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 68. | Yamauchi H, Kida M, Imaizumi H, Okuwaki K, Miyazawa S, Iwai T, Koizumi W. Innovations and techniques for balloon-enteroscope-assisted endoscopic retrograde cholangiopancreatography in patients with altered gastrointestinal anatomy. World J Gastroenterol. 2015;21:6460-6469. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 69. | Ishii K, Itoi T, Tonozuka R, Itokawa F, Sofuni A, Tsuchiya T, Tsuji S, Ikeuchi N, Kamada K, Umeda J, Tanaka R, Honjo M, Mukai S, Fujita M, Moriyasu F, Baron TH, Gotoda T. Balloon enteroscopy-assisted ERCP in patients with Roux-en-Y gastrectomy and intact papillae (with videos). Gastrointest Endosc. 2016;83:377-86.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 75] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 70. | De Koning M, Moreels TG. Comparison of double-balloon and single-balloon enteroscope for therapeutic endoscopic retrograde cholangiography after Roux-en-Y small bowel surgery. BMC Gastroenterol. 2016;16:98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 71. | Inamdar S, Slattery E, Sejpal DV, Miller LS, Pleskow DK, Berzin TM, Trindade AJ. Systematic review and meta-analysis of single-balloon enteroscopy-assisted ERCP in patients with surgically altered GI anatomy. Gastrointest Endosc. 2015;82:9-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 93] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 72. | Moreels TG. Altered anatomy: enteroscopy and ERCP procedure. Best Pract Res Clin Gastroenterol. 2012;26:347-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 73. | Skinner M, Popa D, Neumann H, Wilcox CM, Mönkemüller K. ERCP with the overtube-assisted enteroscopy technique: a systematic review. Endoscopy. 2014;46:560-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 153] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 74. | Shao XD, Qi XS, Guo XZ. Endoscopic retrograde cholangiopancreatography with double balloon enteroscope in patients with altered gastrointestinal anatomy: A meta-analysis. Saudi J Gastroenterol. 2017;23:150-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 75. | Fugazza A, Anderloni A, Paduano D, Badalamenti M, Maselli R, Carrara S, Gabbiadini R, Colombo M, Spadaccini M, Cappello A, Haber G, Repici A. Underwater cap-assisted endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy: a pilot study. Endoscopy. 2021;53:927-931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 76. | Itoi T, Sofuni A, Itokawa F, Kurihara T, Tsuchiya T, Ishii K, Ikeuchi N, Moriyasu F, Kasuya K, Tsuchida A, Kamisawa T, Baron TH. Diagnostic and therapeutic peroral direct cholangioscopy in patients with altered GI anatomy (with videos). Gastrointest Endosc. 2012;75:441-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 77. | Koshitani T, Matsuda S, Takai K, Motoyoshi T, Nishikata M, Yamashita Y, Kirishima T, Yoshinami N, Shintani H, Yoshikawa T. Direct cholangioscopy combined with double-balloon enteroscope-assisted endoscopic retrograde cholangiopancreatography. World J Gastroenterol. 2012;18:3765-3769. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 78. | Hakuta R, Kogure H, Isayama H, Yamada A, Hamada T, Nakai Y, Koike K. Electrohydraulic lithotripsy of large bile duct stones under direct cholangioscopy with a double-balloon endoscope. Endoscopy. 2015;47 Suppl 1 UCTN:E519-E520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 79. | Sato T, Kogure H, Nakai Y, Isayama H, Koike K. Electrohydraulic lithotripsy under double-balloon endoscope-assisted direct cholangioscopy for treatment of choledocholithiasis in a patient with Roux-en-Y gastrectomy. VideoGIE. 2018;3:113-114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 80. | Kao KT, Batra B. Single-balloon-assisted ERCP with electrohydraulic lithotripsy for the treatment of a bile duct stone in a patient with a hepaticojejunostomy. Gastrointest Endosc. 2014;80:1173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 81. | Hakuta R, Kogure H, Nakai Y, Yamada A, Takahara N, Mizuno S, Koike K. Successful endoscopic lithotripsy using a new digital cholangioscope through an overtube placed by an enteroscope. Endoscopy. 2018;50:E269-E271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 82. | Tonozuka R, Itoi T, Sofuni A, Tsuchiya T, Ishii K, Tanaka R, Honjo M, Mukai S, Yamamoto K, Fujita M, Asai Y, Mastunami Y, Kurosawa T, Kojima H, Kogure H, Nagakawa Y. Novel peroral direct digital cholangioscopy-assisted lithotripsy using a monorail technique through the overtube in patients with surgically altered anatomy (with video). Dig Endosc. 2019;31:203-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 83. | Kamiyama R, Ogura T, Okuda A, Miyano A, Nishioka N, Imanishi M, Takagi W, Higuchi K. Electrohydraulic Lithotripsy for Difficult Bile Duct Stones under Endoscopic Retrograde Cholangiopancreatography and Peroral Transluminal Cholangioscopy Guidance. Gut Liver. 2018;12:457-462. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 84. | Weilert F, Binmoeller KF, Marson F, Bhat Y, Shah JN. Endoscopic ultrasound-guided anterograde treatment of biliary stones following gastric bypass. Endoscopy. 2011;43:1105-1108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 68] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 85. | Iwashita T, Yasuda I, Doi S, Uemura S, Mabuchi M, Okuno M, Mukai T, Itoi T, Moriwaki H. Endoscopic ultrasound-guided antegrade treatments for biliary disorders in patients with surgically altered anatomy. Dig Dis Sci. 2013;58:2417-2422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 86. | James TW, Fan YC, Baron TH. EUS-guided hepaticoenterostomy as a portal to allow definitive antegrade treatment of benign biliary diseases in patients with surgically altered anatomy. Gastrointest Endosc. 2018;88:547-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 87. | Sneineh MA, Harel L, Elnasasra A, Razin H, Rotmensh A, Moscovici S, Kais H, Shirin H. Increased Incidence of Symptomatic Cholelithiasis After Bariatric Roux-En-Y Gastric Bypass and Previous Bariatric Surgery: a Single Center Experience. Obes Surg. 2020;30:846-850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 54] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 88. | Schreiner MA, Chang L, Gluck M, Irani S, Gan SI, Brandabur JJ, Thirlby R, Moonka R, Kozarek RA, Ross AS. Laparoscopy-assisted versus balloon enteroscopy-assisted ERCP in bariatric post-Roux-en-Y gastric bypass patients. Gastrointest Endosc. 2012;75:748-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 168] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 89. | Bowman E, Greenberg J, Garren M, Guda N, Rajca B, Benson M, Pfau P, Soni A, Walker A, Gopal D. Laparoscopic-assisted ERCP and EUS in patients with prior Roux-en-Y gastric bypass surgery: a dual-center case series experience. Surg Endosc. 2016;30:4647-4652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 90. | Habenicht Yancey K, McCormack LK, McNatt SS, Powell MS, Fernandez AZ, Westcott CJ. Laparoscopic-Assisted Transgastric ERCP: A Single-Institution Experience. J Obes. 2018;2018:8275965. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 91. | Kedia P, Tarnasky PR, Nieto J, Steele SL, Siddiqui A, Xu MM, Tyberg A, Gaidhane M, Kahaleh M. EUS-directed Transgastric ERCP (EDGE) Versus Laparoscopy-assisted ERCP (LA-ERCP) for Roux-en-Y Gastric Bypass (RYGB) Anatomy: A Multicenter Early Comparative Experience of Clinical Outcomes. J Clin Gastroenterol. 2019;53:304-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 101] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 92. | Tyberg A, Nieto J, Salgado S, Weaver K, Kedia P, Sharaiha RZ, Gaidhane M, Kahaleh M. Endoscopic Ultrasound (EUS)-Directed Transgastric Endoscopic Retrograde Cholangiopancreatography or EUS: Mid-Term Analysis of an Emerging Procedure. Clin Endosc. 2017;50:185-190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 89] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 93. | Diehl DL, Gabrielsen JD, Strodel WE. The challenges of endoscopic retrograde cholangiopancreatography in gastric bypass patients: the game is not yet over. Gastroenterology. 2015;148:857-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 94. | Abu Dayyeh BK, Thompson CC, Gostout C. Endoscopic Retrograde Cholangiopancreatography After Roux-en-Y Gastric Bypass: Challenges and Cautions. Gastroenterology. 2015;148:858-859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 95. | Yang D, Draganov PV. ERCP in patients with Roux-en-Y gastric bypass: one size does not fit all. Gastrointest Endosc. 2019;89:646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 96. | Krafft MR, Fang W, Nasr JY. Shortened-Interval Dual-Session EDGE Reduces the Risk of LAMS Dislodgement While Facilitating Timely ERCP. Dig Dis Sci. 2021;66:2776-2785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 97. | Bukhari M, Kowalski T, Nieto J, Kunda R, Ahuja NK, Irani S, Shah A, Loren D, Brewer O, Sanaei O, Chen YI, Ngamruengphong S, Kumbhari V, Singh V, Aridi HD, Khashab MA. An international, multicenter, comparative trial of EUS-guided gastrogastrostomy-assisted ERCP versus enteroscopy-assisted ERCP in patients with Roux-en-Y gastric bypass anatomy. Gastrointest Endosc. 2018;88:486-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 112] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 98. | Telfah MM, Noble H, Mahon D, Mason M, Hollyman M, Matull R, Welbourn R. Laparoscopic-Assisted Endoscopic Retrograde Cholangiopancreatography (ERCP) for Bile Duct Stones After Roux-en-Y-Gastric Bypass: Single-Centre Experience. Obes Surg. 2020;30:4953-4957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 99. | Boeva I, Karagyozov PI, Tishkov I. Post-liver transplant biliary complications: Current knowledge and therapeutic advances. World J Hepatol. 2021;13:66-79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 61] [Article Influence: 15.3] [Reference Citation Analysis (5)] |
| 100. | Lee HW, Shah NH, Lee SK. An Update on Endoscopic Management of Post-Liver Transplant Biliary Complications. Clin Endosc. 2017;50:451-463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (1)] |
| 101. | Yu ZY, Zhang M, Qin YS, Zhou XP, Cai MY, Yu SF, Ke QH, Zheng SS. Risk factors of choledocholithiasis formation after liver transplantation. Hepatobiliary Pancreat Dis Int. 2013;12:215-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 102. | Arain MA, Attam R, Freeman ML. Advances in endoscopic management of biliary tract complications after liver transplantation. Liver Transpl. 2013;19:482-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 59] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 103. | Nasr JY, Slivka A. Endoscopic approach to the post liver transplant patient. Gastrointest Endosc Clin N Am. 2013;23:473-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 104. | Chen C, Huang M, Yang J, Yang C, Yeh Y, Wu H, Chou D, Yueh S, Nien C. Reappraisal of percutaneous transhepatic cholangioscopic lithotomy for primary hepatolithiasis. Surg Endosc. 2005;19:505-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 47] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 105. | Franzini T, Cardarelli-Leite L, Figueira ERR, Morita F, Domingos FUG, Carnevale FC, de Moura EGH. SpyGlass percutaneous transhepatic cholangioscopy-guided lithotripsy of a large intrahepatic stone. Endoscopy. 2017;49:E292-E293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 106. | Fugazza A, Colombo M, Repici A, Anderloni A. Endoscopic Ultrasound-Guided Gallbladder Drainage: Current Perspectives. Clin Exp Gastroenterol. 2020;13:193-201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 107. | Anderloni A, Fugazza A, Troncone E, Auriemma F, Carrara S, Semeraro R, Maselli R, Di Leo M, D'Amico F, Sethi A, Repici A. Single-stage EUS-guided choledochoduodenostomy using a lumen-apposing metal stent for malignant distal biliary obstruction. Gastrointest Endosc. 2019;89:69-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 108] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 108. | Nakai Y, Kogure H, Isayama H, Koike K. Endoscopic Ultrasound-Guided Biliary Drainage for Benign Biliary Diseases. Clin Endosc. 2019;52:212-219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 109. | Dhir V, Bhandari S, Bapat M, Maydeo A. Comparison of EUS-guided rendezvous and precut papillotomy techniques for biliary access (with videos). Gastrointest Endosc. 2012;75:354-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 156] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 110. | Lee A, Aditi A, Bhat YM, Binmoeller KF, Hamerski C, Sendino O, Kane S, Cello JP, Day LW, Mohamadnejad M, Muthusamy VR, Watson R, Klapman JB, Komanduri S, Wani S, Shah JN. Endoscopic ultrasound-guided biliary access versus precut papillotomy in patients with failed biliary cannulation: a retrospective study. Endoscopy. 2017;49:146-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 111. | El Chafic AH, Shah JN. Advances in Biliary Access. Curr Gastroenterol Rep. 2020;22:62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |