Published online Jun 14, 2021. doi: 10.3748/wjg.v27.i22.3121
Peer-review started: November 11, 2020
First decision: November 23, 2020
Revised: December 8, 2020
Accepted: May 17, 2021
Article in press: May 17, 2021
Published online: June 14, 2021
Processing time: 208 Days and 21.6 Hours
Slow transit constipation (STC) has traditionally been considered as a functional disorder. However, evidence is accumulating that suggests that most of the motility alterations in STC might be of a neuropathic etiology. If the patient does not meet the diagnosis of pelvic outlet obstruction and poorly response to conservative treatment, surgical intervention with subtotal colectomy may be effective. The most unwanted complication of the procedure is anastomotic leakage, however, preservation of the superior rectal artery (SRA) may reduce its incidence.
To evaluate the preservation of the SRA in laparoscopically assisted subtotal colectomy with ileorectal anastomosis in STC patients.
This was a single-center retrospective observational study. STC was diagnosed after a series of examinations which included a colonic transit test, anal manometry, a balloon expulsion test, and a barium enema. Eligible patients underwent laparoscopically assisted total colectomy with ileorectal anastomosis and were examined between January 2016 and January 2018. The operation time, blood loss, time to first flatus, length of hospital days, and incidence of minor or major complications were recorded.
A total of 32 patients (mean age, 42.6 years) who had received laparoscopic assisted subtotal colectomy with ileorectal artery anastomosis and preservation of the SRA. All patients were diagnosed with STC after a series of examinations. The mean operative time was 151 min and the mean blood loss was 119 mL. The mean day of first time to flatus was 3.0 d, and the mean hospital stay was 10.6 d. There were no any patients conversions to laparotomy. Post-operative minor complications including 1 wound infection and 1 case of ileus. There was no surgical mortality. No anastomosis leakage was noted in any of the patients.
Laparoscopically assisted subtotal colectomy with ileorectal anastomosis and preservation of the SRA can significantly improve bowel function with careful patient selection. Sparing the SRA may protect against anastomosis leakage.
Core Tip: Slow transit constipation (STC) has traditionally been considered as a functional disorder. Surgical intervention with subtotal colectomy may be effective for STC. Laparoscopically assisted subtotal colectomy with ileorectal anastomosis and preservation of the superior rectal artery is tolerated and can have an excellent surgical outcome in reduce anastomosis leakage with significant improvement in bowel function under careful patient enrollment criteria.
- Citation: Wu CW, Pu TW, Kang JC, Hsiao CW, Chen CY, Hu JM, Lin KH, Lin TC. Preservation of superior rectal artery in laparoscopically assisted subtotal colectomy with ileorectal anastomosis for slow transit constipation. World J Gastroenterol 2021; 27(22): 3121-3129
- URL: https://www.wjgnet.com/1007-9327/full/v27/i22/3121.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i22.3121
Constipation means the incapacity to evacuate the bowel. Patients cannot evacuate completely and spontaneously at least three or more times per week although it is commonly one or fewer bowel movements per week. Most patients with constipation have one or more of the following symptoms: Hard infrequent stools, excessive straining, incomplete evacuation, excessive time attempting to evacuate or dissatisfaction with defecation[1-4].
Slow transit constipation (STC) has been traditionally considered and classified as a functional disorder. However, clinical and manometric evidence has been accumulating that suggests most of the motility abnormalities in STC might be neuropathic[5].
Radiopaque markers with a transit colon test showed delayed of the transpiration of the colon is used for making the diagnosis[2,3,6]. If the conservative treatment is failed and pelvic outlet obstruction was ruled out, surgical procedure with a subtotal colectomy may be effective[7]. The most unwanted complication of the procedure is an anastomotic leak (AL). AL is a serious complication of colorectal surgery and can be defined as: ‘the luminal contents leaking from a surgical connection between 2 hollow viscera’[8]. AL is responsible for up to 40% of the postoperative mortality rate, prolonged hospitalization, and an increase in the costs of healthcare due to the treatment of sepsis and the need for re-operation[9]. The main aim of this study is to make known a feasibility and functional outcome of laparoscopically assisted subtotal colectomy with the preservation of the superior rectal artery (SRA) in ileorectal anastomosis for STC.
This investigation is an observational single-center study. The decision on whether to preserve the SRA was left to the discretion of the surgeon. Of the patients who were treated at the Division of Colon and Rectal Surgery at the Taiwan Adventist Hospital between January 2016 and January 2017, patients diagnosed with constipation (compatible with the Rome II criteria)[10] were tested with laboratory studies including a thyroid-function test, serum calcium, serum glucose, and complete blood count. All cases had clinical evaluation, such as a digital rectal examination and a psychological consultation. We excluded secondary causes (colonic obstruction, metabolic disorders, and drug-induced constipation).
The STC diagnostic workup includes a colonic transitional test, pressure measurement of anorectal, a balloon exploration test, and a barium enema. We defined a positive colonic transit test as patients who had greater than 20% of radiopaque marker stasis in the colorectum after 96 h. Anorectal pressure measurement and the balloon exploration test were arranged to assure there was no outlet obstructed defecation and to rule out pelvic floor dysfunction. Patients underwent a barium enema to ensure there were no mechanical obstruction problems, and this investigation showed redundant colon in all cases. Colonoscopy was normal and anal ultrasound showed no disruption of the external anal sphincter in all cases. Suitable patients were those in complete accord with the colonic transition test greater than 96 h, but who had normal results on the barium enema, balloon exploration test, anal pressure measurement, colonoscopy, and anal ultrasound. Informed consent was provided before all examinations. The operations were performed by the same team.
In all, 32 patients were diagnosed with STC and were treated by laparoscopically assisted subtotal colectomy with preservation of the SRA in ileorectal anastomosis between January 2016 and January 2017. Data on age, body mass index, preoperative laxative dependency, preoperative defecation duration, colonic transit time, operative time, estimated volume of blood loss, surgical complications, postoperative bowel movements, length of hospital stay, and functional outcome were recorded.
This study protocol was reviewed and approved by the Institutional Review Board of the Taiwan Adventist Hospital (TAHIRB No. 105-E-10). It was conducted in compliance with the Helsinki Declaration. The patients provided written informed consent before surgery and patient information was anonymized and de-identified before analysis.
Patient characteristics are summarized using total number, percentages, and mean ± SD. All statistical analyses were performed with IBM SPSS statistical software version 22 for Windows (IBM Corp., Armonk, NY, United States).
All the laparoscopic surgical procedures for preservation of SRA in STC patients were performed by two experienced colorectal surgeons who have experience of more than 100 laparoscopic and open colorectal cancer procedures annually. In all cases, the planned procedure was a laparoscopic subtotal colectomy with ileorectal anastomosis. The patients were placed in the modified lithotomy position under general anesthesia. Five trocars were used with the insertion of the primary trocar with a 10 mm port to gain access to the peritoneal cavity and establish the pneumoperitoneum above the umbilicus for the 30° laparoscope. The other four working ports were a 12 mm port in the right iliac fossa, a 10 mm port in the left iliac fossa, and a 5 mm port was placed in each of the right and left upper quadrants of the abdomen. Mobilization of the colonic segments was started at the right side of the colon. Mobilization was performed with the Endoshears (LigaSure device).
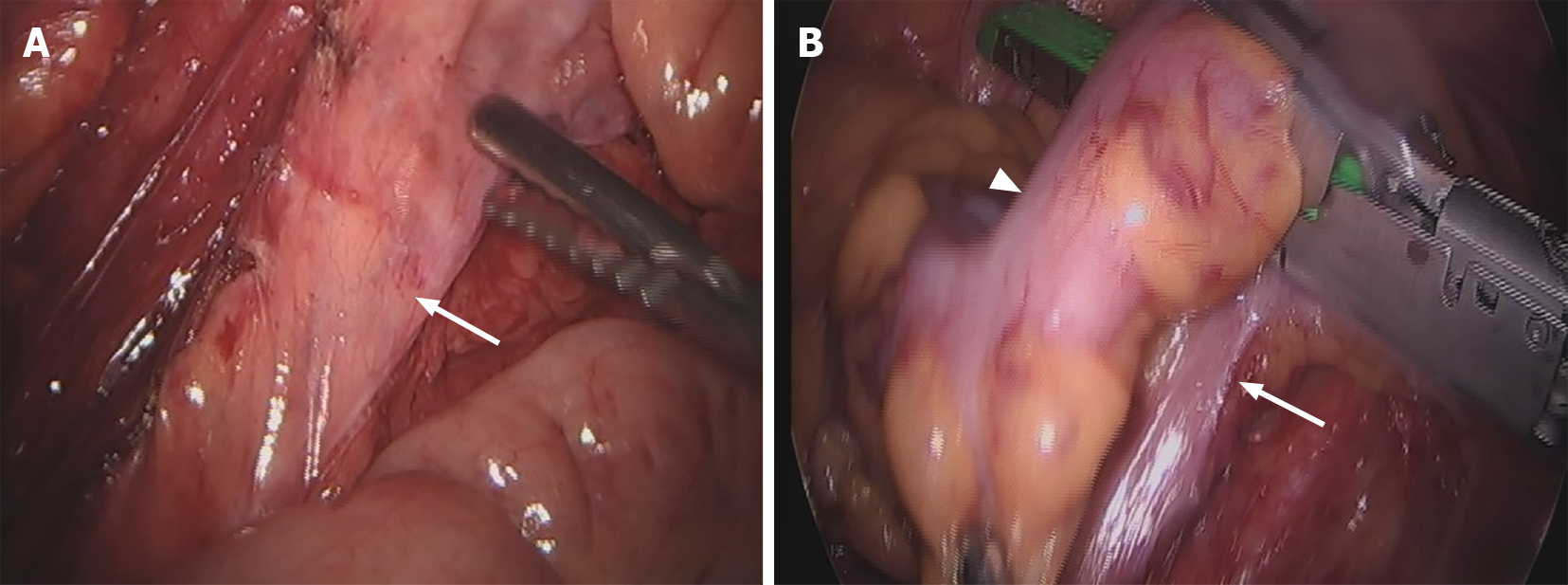
After the colon was fully mobilized, the colon was resected to the level of the junction of the rectosigmoid with a laparoscopic linear stapler. The rectal stump was mobilized to facilitate the transanally inserted circular stapler or Hegar dilator. The SRA was preserved in all patients (Figure 1).
A 4-5 cm Pfannenstiel incision was made, and the mobilized bowel segment was brought out (Figure 2). The terminal ileum was divided a few centimeters proximal to the ileocecal valve with the anvil of a circular stapling device inserted into the lumen of the ileum. The ileum, with the anvil secured, was placed into the abdominal cavity. Finally, we performed the transanal end-to-end anastomosis using the circular stapling device. One Jackson Pratt drain was inserted into the pelvis, and the abdominal wall wounds were closed.
Thirty-two patients diagnosed with STC who had undergone laparoscopically assisted subtotal colectomy with preservation of the SRA in ileorectal anastomosis were included in the study. The preliminary data of these patients are presented in Table 1. Eighteen of them (56.2%) were women. The mean age of our patients was 42.6 ± 10.4 years. The mean body mass index was 26.6 ± 3.1 kg/m2.
| Variables | Mean |
| Age (yr) | 43.0 ± 10.4 |
| Body mass index (kg/m2) | 26.5 ± 2.9 |
| Preoperative laxative dependence (yr) | 13.7 ± 5.0 |
| Preoperative defecation interval (d) | 9.6 ± 3.9 |
| Colonic transit time (h) | 131 ± 13.4 |
| Previous abdominal surgery | 3 (9.4) |
| Preoperative abdominal pain | 31 (96.9) |
All patients had severe constipation, the mean defecation duration was 9.3 d and 3 (9.4%) patients had previous abdominal surgery. All patients complained of intermittent abdominal pain preoperatively. The mean operative time was 151 ± 29.9 min. The mean estimated blood loss was 119.1 ± 40.7 mL (Table 2).
| Variables | mean ± SD |
| Operation time (min) | 151.0 ± 29.9 |
| Estimated blood loss (mL) | 119.1 ± 40.7 |
| Time to first flatus (d) | 3.0 ± 0.8 |
| Time to first stool passing (d) | 2.5 ± 0.5 |
| Time to oral intake (d) | 2.4 ± 0.5 |
| Dose of demerol used (mg) | 87.5 ± 40.15 |
| Duration of hospital stay (d) | 10.6 ± 2.9 |
| Postoperative bowel frequency (per day) | 2.2 ± 1.0 |
The mean time to the first flatus was 3.0 ± 0.8 d, and the average time to the first stool was 2.5 ± 0.5 d. The average time to first oral intake was 2.8 ± 0.8 d. The mean time of discharge from the ward was 10.6 ± 2.9 d. The satisfaction of post-operative patients was excellent in 28 (90%) patients. The satisfaction was poor in 2 (5%) patients due to a wound infection and an incisional hernia.
There were no intraoperative complications. Post-operative complications included 1 wound infection (Pfannenstiel incision wound), prolonged ileus (over 5 d) in 2 patients and three patients developed a urinary tract infection. One patient had an incisional hernia (Table 3). All cases could be fed orally with a clear liquid diet on the 4th postoperative day. There was no major surgical complication and no patient required conversion to an exploratory laparotomy.
| Characteristics | Number of subjects, n (%) |
| Intraoperative complications | |
| None | 32 (100) |
| Postoperative complications | |
| None | 25 (78.1) |
| Urinary tract infection | 3 (9.3) |
| Ileus (over 5 d) | 2 (6.2) |
| Incisional hernia | 1 (3.1) |
| Wound infection | 1 (3.1) |
| Anastomosis leakage | 0 (0) |
| Satisfaction, excellent/good/poor | 28/2/2 (90%/5%/5%) |
Constipation is a common condition. Most patients with constipation are treated with changes in their diet and the use of laxatives. If the condition proves recalcitrant, we should exclude secondary causes which may be underlying metabolic, organic or pharmacological factors. The mechanisms of slow transit include fewer colonic high-amplitude propagated contractions or a reduced colonic contractile response to a meal[1]. The cause for STC is, however, unclear.
STC means a prolonged time in the transit of stools through the colon without an underlying systemic metabolic or pathologic disorder or pelvic floor dysfunction[11]. Delays due to major dysfunction or innervation of colonic smooth muscle[12]. Patients with STC have an incorrect expression of serotonin receptors and incorrect responses to cholinesterase inhibitors[13,14]. The disease induced by a reduction in the interstitial cells of Cajal, which have a role in intestinal innervation and are situated in the submucosal and myenteric plexus of the bowel wall[15].
The enrollment criteria was done by the following steps. First, physiologic examinations for constipated patients are needed and include colonic transit studies with radiopaque markers, balloon tests, check anorectal pressure and defecation test[16]. The radiopaque marker test is very helpful. Physiologic examination should include anorectal manometry to rule out the problem of pelvic floor dysfunction. All of our patients had anorectal manometry which revealed no abnormal anorectal inhibitory reflexes. A colonoscopy or barium enema is a good tool to provide evidence of any pathologic disease or structural lesions[17,18].
The incidence of AL following gastrointestinal surgery varies according to the site of anastomosis (all resections: 4.3%-13%)[19]. Ischemia of the anastomotic region is one of the most significant factors leading to AL. Therefore, the preservation of the anatomical blood supply of the rectum is important. The effect of SRA-sparing on anastomotic healing and perioperative complications is poorly investigated. Sohn et al[20] have demonstrated that preservation of the SRA seems to be associated with a reduction of the leak rate in patients undergoing laparoscopic sigmoid resection for diverticular disease[20]. Beyond AL, an SRA sparing technique leads to preservation of the hypogastric nerves and thereby could potentially improve functional outcomes[20]. However, no studies have focused on the preservation of SRA with subtotal colectomy in STC patients. We observed no AL in our 32 STC patients who underwent an SRA-sparing operation. Although our study had a small sample size, the preservation of the SRA seems to have an excellent surgical outcome.
Laparoscopic techniques have been successfully used in colon surgery, thereby reducing morbidity, mortality and length of hospital stay[21,22]. The length of hospital stay is in the range of 7 to 13 d in STC patients[13,23,24], with postoperative ileus complicating the treatment course in many of them[7]. In our study, the mean hospital stay was 10.6 ± 2.9 d, and the mean number of days to the first flatus was 3.0 ± 0.8 d.
Abdominal distention with pain and vomiting all improved after surgery[25]. In a study by FitzHarris et al[26], although subtotal colectomy for slow-transit constipation increased bowel-movement frequency, the persistence of abdominal pain and diarrhea or postoperative incontinence adversely affected the quality of life following the surgery[26].
Preoperative counseling and an integrated post-operative functional and rehabilitational follow-up is important in patient underwent anterior rectal resection[26]. In a study by Sturiale et al[27], patients with defecation disorders, should receive an adequate re-educational process which often results in relevant clinical improvement for the patient[27]. Biofeedback therapy also shows effective treatment for fecal incontinence patient after anorectal operation[28].
A key limitation of the present study is its retrospective character. Moreover, technical aspects could have influenced the dissection technique. Thus, sparing of the mesosigmoid and the mesorectum can be performed much more easily today than at the beginning of the laparoscopic era, constituting a possible bias. This also explains the late publication of our data. Despite these limitations, and the bias involved through missing randomization, small sample size and surgeon preference of technique, we report the largest patient sample with vascular preservation in STC patients.
In conclusion, laparoscopically assisted subtotal colectomy with ileorectal anastomosis and preservation of the SRA is tolerated and can have better results with significant improvement in bowel function with careful patient enrollment criteria. No anastomosis leakage was noted in any of our patients; preservation of the SRA appears to result in excellent surgical outcomes.
Slow transit constipation (STC) has traditionally been considered as a functional disorder. However, evidence is accumulating that suggests that most of the motility alterations in STC might be of a neuropathic etiology. If the patient’s condition responds poorly to non-surgical treatment, operative intervention with subtotal colectomy may be effective.
However, preservation of the superior rectal artery (SRA) may reduce its incidence.
STC patients underwent laparoscopically assisted total colectomy with ileorectal anastomosis and were examined between January 2016 and January 2017.
This was a single-center retrospective observational study. STC was diagnosed after a series of examinations which included a colonic transit test, anal manometry, a balloon expulsion test, and a barium enema. Eligible patients underwent laparoscopically assisted total colectomy with ileorectal anastomosis and were examined between January 2016 and January 2017. The main outcome include operation time, estimated blood loss, time to first flatulence and incidence of complications.
A total of 32 patients (mean age, 42.6 years) underwent laparoscopically assisted subtotal colectomy with ileorectal anastomosis and preservation of the SRA. All patients were diagnosed with STC after a series of examinations. The mean day of first time to flatus was 3.0 d, and the mean hospital stay was 10.6 d. There were no conversions to laparotomy. Post-operative complications included 1 wound infection and 1 case of ileus. No anastomosis leakage was noted in any of the patients.
Laparoscopically assisted subtotal colectomy with ileorectal anastomosis and preservation of the SRA can significantly improve bowel function with careful patient selection. Sparing the SRA may protect against anastomosis leakage.
Laparoscopically assisted subtotal colectomy with ileorectal anastomosis and preservation of the SRA can have well results with improvement in bowel function with careful patient enrollment criteria. No anastomosis leakage was noted in any of our patients; preservation of the SRA appears to result in excellent surgical outcomes.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Rubbini M S-Editor: Fan JR L-Editor: A P-Editor: Li X
| 1. | Bassotti G, de Roberto G, Castellani D, Sediari L, Morelli A. Normal aspects of colorectal motility and abnormalities in slow transit constipation. World J Gastroenterol. 2005;11:2691-2696. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 74] [Cited by in RCA: 52] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 2. | Lembo A, Camilleri M. Chronic constipation. N Engl J Med. 2003;349:1360-1368. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Pfeifer J, Agachan F, Wexner SD. Surgery for constipation: a review. Dis Colon Rectum. 1996;39:444-460. [RCA] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 70] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Drossman DA. The functional gastrointestinal disorders and the Rome II process. Gut. 1999;45 Suppl 2:II1-II5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 169] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 5. | Bassotti G, Villanacci V. Slow transit constipation: a functional disorder becomes an enteric neuropathy. World J Gastroenterol. 2006;12:4609-4613. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 73] [Cited by in RCA: 71] [Article Influence: 3.7] [Reference Citation Analysis (1)] |
| 6. | Lane WA. Remarks ON THE RESULTS OF THE OPERATIVE TREATMENT OF CHRONIC CONSTIPATION. Br Med J. 1908;1:126-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 7. | Barkley KT. John C. Reeve, M.D., pioneer Dayton physician (1826-1920). Ohio State Med J. 1978;74:187-188, 190. [PubMed] |
| 8. | Veyrie N, Ata T, Muscari F, Couchard AC, Msika S, Hay JM, Fingerhut A, Dziri C; French Associations for Surgical Research. Anastomotic leakage after elective right versus left colectomy for cancer: prevalence and independent risk factors. J Am Coll Surg. 2007;205:785-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 115] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 9. | Boccola MA, Buettner PG, Rozen WM, Siu SK, Stevenson AR, Stitz R, Ho YH. Risk factors and outcomes for anastomotic leakage in colorectal surgery: a single-institution analysis of 1576 patients. World J Surg. 2011;35:186-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 146] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 10. | Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Müller-Lissner SA. Functional bowel disorders and functional abdominal pain. Gut. 1999;45 Suppl 2:II43-II47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 622] [Cited by in RCA: 830] [Article Influence: 31.9] [Reference Citation Analysis (0)] |
| 11. | Preston DM, Lennard-Jones JE. Severe chronic constipation of young women: 'idiopathic slow transit constipation'. Gut. 1986;27:41-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 302] [Cited by in RCA: 284] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 12. | Knowles CH, Martin JE. Slow transit constipation: a model of human gut dysmotility. Review of possible aetiologies. Neurogastroenterol Motil. 2000;12:181-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 94] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 13. | Bassotti G, Chiarioni G, Imbimbo BP, Betti C, Bonfante F, Vantini I, Morelli A, Whitehead WE. Impaired colonic motor response to cholinergic stimulation in patients with severe chronic idiopathic (slow transit type) constipation. Dig Dis Sci. 1993;38:1040-1045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 69] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Zhao RH, Baig MK, Thaler KJ, Mack J, Abramson S, Woodhouse S, Tamir H, Wexner SD. Reduced expression of serotonin receptor(s) in the left colon of patients with colonic inertia. Dis Colon Rectum. 2003;46:81-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Hotta T, Yamaue H. Laparoscopic surgery for rectal cancer: review of published literature 2000-2009. Surg Today. 2011;41:1583-1591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Hsiao KC, Jao SW, Wu CC, Lee TY, Lai HJ, Kang JC. Hand-assisted laparoscopic total colectomy for slow transit constipation. Int J Colorectal Dis. 2008;23:419-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Thompson WG. Constipation: a physiological approach. Can J Gastroenterol. 2000;14 Suppl D:155D-162D. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Lahr SJ, Lahr CJ, Srinivasan A, Clerico ET, Limehouse VM, Serbezov IK. Operative management of severe constipation. Am Surg. 1999;65:1117-21; discussion 1122. [PubMed] |
| 19. | Khan AA, Wheeler JM, Cunningham C, George B, Kettlewell M, Mortensen NJ. The management and outcome of anastomotic leaks in colorectal surgery. Colorectal Dis. 2008;10:587-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 118] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 20. | Sohn M, Schlitt HJ, Hornung M, Zülke C, Hochrein A, Moser C, Agha A. Preservation of the superior rectal artery: influence of surgical technique on anastomotic healing and postoperative morbidity in laparoscopic sigmoidectomy for diverticular disease. Int J Colorectal Dis. 2017;32:955-960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Franklin ME Jr, Rosenthal D, Abrego-Medina D, Dorman JP, Glass JL, Norem R, Diaz A. Prospective comparison of open vs. laparoscopic colon surgery for carcinoma. Five-year results. Dis Colon Rectum. 1996;39:S35-S46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 263] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 22. | Lacy AM, García-Valdecasas JC, Piqué JM, Delgado S, Campo E, Bordas JM, Taurá P, Grande L, Fuster J, Pacheco JL. Short-term outcome analysis of a randomized study comparing laparoscopic vs open colectomy for colon cancer. Surg Endosc. 1995;9:1101-1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 169] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 23. | Piccirillo MF, Reissman P, Wexner SD. Colectomy as treatment for constipation in selected patients. Br J Surg. 1995;82:898-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 62] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 24. | Wexner SD, Daniel N, Jagelman DG. Colectomy for constipation: physiologic investigation is the key to success. Dis Colon Rectum. 1991;34:851-856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 95] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Vergara-Fernandez O, Mejía-Ovalle R, Salgado-Nesme N, Rodríguez-Dennen N, Pérez-Aguirre J, Guerrero-Guerrero VH, Sánchez-Robles JC, Valdovinos-Díaz MA. Functional outcomes and quality of life in patients treated with laparoscopic total colectomy for colonic inertia. Surg Today. 2014;44:34-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 26. | FitzHarris GP, Garcia-Aguilar J, Parker SC, Bullard KM, Madoff RD, Goldberg SM, Lowry A. Quality of life after subtotal colectomy for slow-transit constipation: both quality and quantity count. Dis Colon Rectum. 2003;46:433-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 77] [Article Influence: 3.5] [Reference Citation Analysis (1)] |
| 27. | Sturiale A, Martellucci J, Zurli L, Vaccaro C, Brusciano L, Limongelli P, Docimo L, Valeri A. Long-term functional follow-up after anterior rectal resection for cancer. Int J Colorectal Dis. 2017;32:83-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 99] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 28. | Brusciano L, Gambardella C, Tolone S, Del Genio G, Terracciano G, Gualtieri G, Schiano di Visconte M, Docimo L. An imaginary cuboid: chest, abdomen, vertebral column and perineum, different parts of the same whole in the harmonic functioning of the pelvic floor. Tech Coloproctol. 2019;23:603-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |