Published online Jan 14, 2021. doi: 10.3748/wjg.v27.i2.143
Peer-review started: October 25, 2020
First decision: November 13, 2020
Revised: November 13, 2020
Accepted: November 29, 2020
Article in press: November 29, 2020
Published online: January 14, 2021
Processing time: 77 Days and 17 Hours
Roma people make up a significant ethnic minority in many European countries, with the vast majority living in Central and Eastern Europe. Roma are a vulnerable population group in social, economic, and political terms. Frequent migrations, life in segregated communities, substandard housing, poverty, and limited access to quality health care, including low immunization coverage, affect their health status and predispose them to various diseases, including viral hepatitis. Hepatitis A, B, and E are highly prevalent among Roma and mainly associated with low socioeconomic status. In contrast, hepatitis C does not seem to be more frequent in the Roma population. Enhanced efforts should be directed towards the implementation of screening programs, preventive measures, and treatment of viral hepatitis in Roma communities throughout Europe.
Core Tip: Roma people constitute the most important transnational minority in Europe. They are a vulnerable population group in social, economic, and political terms. Low socioeconomic conditions and lack of quality health care predispose them to viral hepatitis, especially hepatitis A, B, and E. In the global attempt to eliminate viral hepatitis, Roma should be considered a high priority group for screening and treatment based on the epidemiological and social context.
- Citation: Mrzljak A, Bajkovec L, Vilibic-Cavlek T. Hepatotropic viruses: Is Roma population at risk? World J Gastroenterol 2021; 27(2): 143-151
- URL: https://www.wjgnet.com/1007-9327/full/v27/i2/143.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i2.143
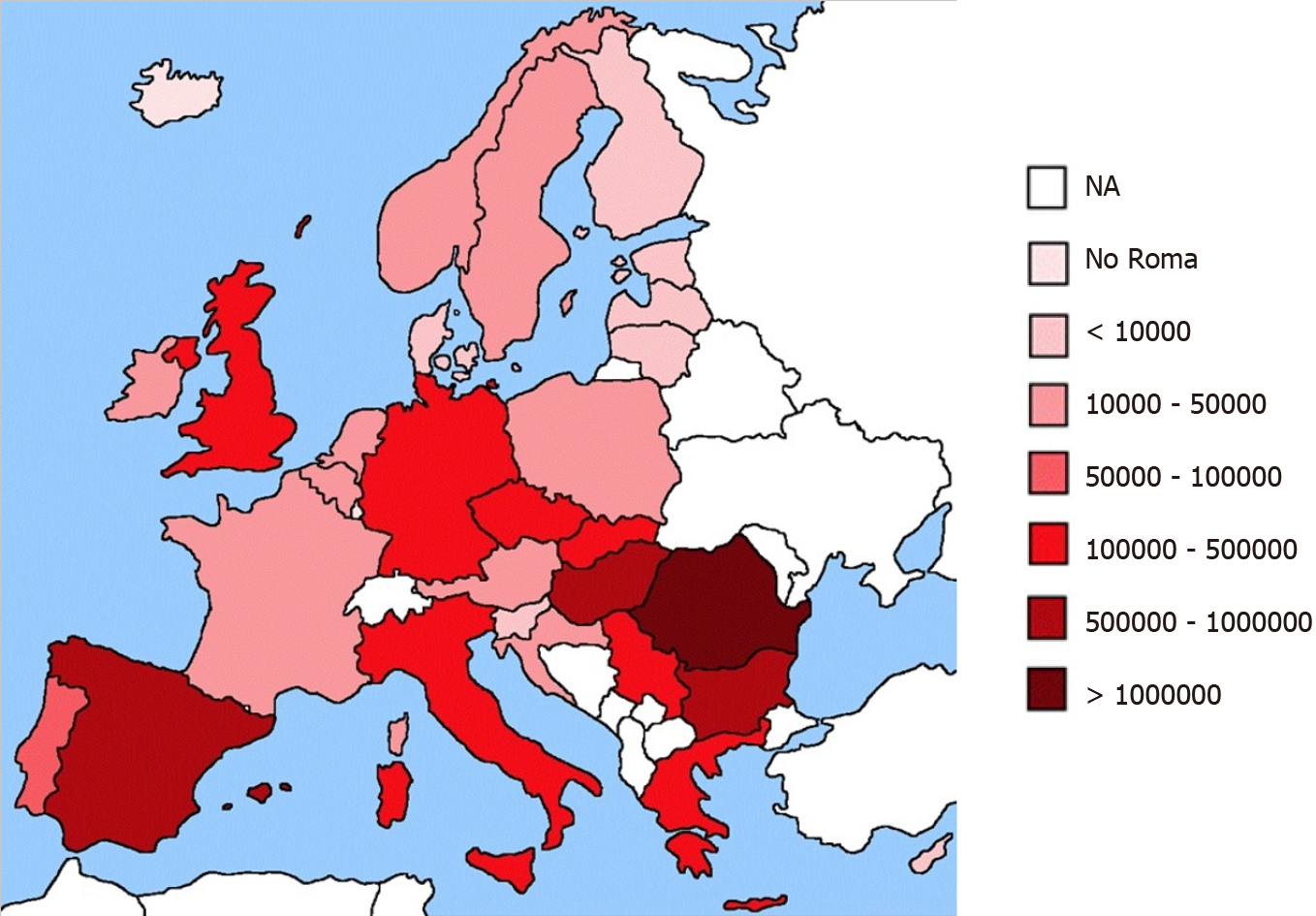
Roma people are a distinct ethnic minority dispersed worldwide, with an estimated population of around 12 million. In Europe, they are the largest minority group (5.2 million), with the vast majority living in Central and Eastern Europe (Figure 1)[1-3]. However, the exact number is uncertain due to their nomadic life and historical lack of birth and death records[4]. Roma are a vulnerable population group in social, economic, and political terms. This vulnerability is manifested in widespread poverty, unemployment, illiteracy, lack of formal education, segregation in the educational system, and substandard housing[5,6]. Roma people have worse health status, higher infant mortality rates, shorter (10-15 years) life expectancy, and a higher prevalence of chronic diseases than the non-Roma[2,7,8]. Unhealthy habits, smoking, and lack of physical activity are common in Roma population[9,10]. Moreover, Roma experience difficulties accessing healthcare due to fear, lack of trust, and previous bad experiences with health providers[11]. Poor socioeconomic factors predispose Roma to a number of various infectious diseases, including viral hepatitis[6,12,13]. Moreover, many Roma believe in folk medicine and prefer home-made remedies, resulting in low immunization coverage and outbreaks of infectious diseases[4].
In the attempt of global elimination of viral hepatitis[14], preventive measures, linkage to care, and treatment process may be challenging in vulnerable populations. In this opinion review, we aim to summarize available data and address practical issues related to viral hepatitis in the European Roma population.
According to the European Centre for Disease Prevention and Control[15], there were 11296 hepatitis A cases in 2019 in the European Union. The incidence of hepatitis A globally decreases, but it is still high in developing countries and among minorities living in low socioeconomic conditions in developed countries[16]. In low-income countries, almost 100% of older children and adults are seropositive[17]. As hepatitis A virus (HAV) is transmitted by person-to-person contact or through contaminated water and food[16], access to clean water and hygiene facilities contributes to the reduction of HAV prevalence[18]. Socioeconomic factors are the most important predictors of HAV infection. Better living standards, including higher incomes and higher education degrees, as well as better housing conditions, significantly decrease the risk of HAV infection[17]. Hepatitis A can be prevented with a vaccine that provides long-term immunity[16].
Roma people are recognized as a high-risk group for HAV infection, in addition to migrants, travelers to endemic countries, and men who have sex with other men[19,20]. In Slovakia and Greece, the countries with a significant number of Roma residents, several hepatitis A outbreaks were reported over the last 15 years[16,19,21]. In the period between 2009 and 2018, 1193 cases of HAV infection were reported in Greece. Roma people accounted for approximately 20% of all infections, with 80.7% of cases affecting Roma children under 15 years old, whereas in the non-Roma population, the percentage of children was significantly lower (5.3%)[19]. Even though the HAV vaccine is mandatory for all children in Greece since 2008, the study from 2013 showed that only 22.6% of Roma children were vaccinated against HAV[22]. In the Roma population, both genders were equally affected, whereas in the non-Roma population, infection predominantly occurred in males. Almost half of HAV clusters (2009-2018) were reported in the Roma population, which accounts for the minority of the Greek population[19]. The study on the HAV outbreak in south-eastern Greece (2007) demonstrated that Roma are susceptible to HAV infection, which appears at an earlier age than in non-Roma[16,20]. In Portugal, an outbreak of HAV was reported in 2005, which involved Roma children[23]. In 2008, there were 9 HAV outbreaks in Slovakia, and four of them took place in the districts predominantly inhabited by the Roma population. The biggest outbreak was registered in Lomnička village (298 cases), where 99% of the residents are Roma. Living conditions in the village, inadequate clean water supplies, and sewage systems predisposed the outbreak[21]. The only data on hepatitis A in Roma from the Czech Republic derives from the European Commission Roma Health Report (2014), stating two epidemics; one in 2009 and the other in 2010 when 30%-50% of Roma from all reported cases developed symptoms[1]. In the Czech Republic, the vaccination against HAV is easily accessible but not obligatory and not free. The HAV vaccination rates among Roma are estimated as low[1]. In the Plovdiv region in Bulgaria, 3911 cases of HAV were documented between 2005 and 2008, most of them associated with Roma. Notification rate in groups of respondents living in worse socioeconomic conditions, mostly Roma, was remarkably higher than in those living in good sanitary conditions[24]. In France, the hepatitis A outbreak involved a total of 492 cases over the 2008-2009 period, including eight clusters of cases among communities living in sites with poor sanitation[1]. A seroepidemiological study conducted in 1995 in San Sebastian, Spain, showed that 82.2% of Roma children were HAV seropositive compared to 9.3% of non-Roma children[25].
HAV infection in Roma differs from the non-Roma population in terms of the lower age of infection and equal distribution among genders[16,19]. The high prevalence is mainly due to poor socioeconomic factors, inadequate sanitary conditions, and sewage systems, contributing to easier transmission of the disease. Additionally, the vaccination coverage in Roma children is low[22,26,27]. In the attempt to lower the HAV incidence, better vaccination coverage and improvement of living conditions in Roma communities should be continuously and decisively implemented.
Hepatitis B virus (HBV) infection has a chronic course and leads to fibrosis, cirrhosis, and hepatocellular carcinoma. The pattern of HBV transmission is vertical and horizontal by infected blood or sexual contact[28]. The HBV vaccine prevents HBV infection and has significantly decreased HBV-related mortality[29]. As HBV infection is associated with poor socioeconomic conditions[28,30], Roma living in communities with poor hygiene are predisposed to have a higher incidence of HBV infection[31,32].
Several studies addressed the prevalence of HBV in Slovakia, where the Roma minority is very numerous. It is estimated that approximately 400000 Roma people live in Slovakia, which accounts for 7.5% of the Slovak population[8]. Their socioeconomic (lower education, unemployment, social benefits) and living conditions (lack of standard household facilities such as sewage system, water supply, flush toilet, bathroom or shower, electricity) are significantly worse compared with the majority[14]. In 2008-2009, a study was conducted in 9 districts of Eastern Slovakia, comparing districts with higher (> 5%) and lower (< 5%) Roma population. There was no significant difference in the overall prevalence of HBsAg (1.95% vs 1.62%). However, pregnant women showed a higher prevalence of HBV infection in districts with a higher Roma population (2.72% vs 0.98%)[33]. In addition, a cross-sectional epidemiological study on hepatitis B was conducted in 2011 among randomly sampled Roma and non-Roma populations. Roma population had a significantly higher prevalence of HBsAg (12.4% vs 2.8%) and anti-HBc (52.8% vs 15.9%) than the non-Roma population. Furthermore, HBsAg positive Roma population was more commonly HBV DNA positive compared to HBsAg positive non-Roma population (94.3% vs 70.0%). Tattooing, economic factors (unemployment, elementary education, poverty), and male sex were found to be risk factors for HBV positivity[34]. Furthermore, targeted testing in primary care demonstrated a high prevalence of HBV infection within the Slovak-Roma population in Sheffield, United Kingdom. The HBsAg positivity was found to be 9.4%, while 28% had evidence of cleared past HBV infection (anti-HBc positive)[35].
One Greek study (2002) analyzed the prevalence and risk factors of hepatitis B in Roma and non-Roma children who lived in a deprived suburb of Athens. Among Roma children, 22.0% were identified with evidence of past HBV infection (anti-HBc positive), of whom 4.2% were chronic carriers (HBsAg positive), whereas no past infection was detected among the non-Roma. The evidence of HBV vaccination (anti-HBs positive) was detected in only 13.6% Roma, but in 95.9% non-Roma children. Among possible risk factors, unfavorable living conditions, frequent residency change, lack of child insurance and primary healthcare delivery were significantly associated with HBV seroprevalence among Roma[36]. Although overall vaccination coverage in Roma children is low[22], it varies in different European countries. For instance, in Slovakia, 59.2% of Roma children are vaccinated against HBV[23]. In the Doctors of the World report (2011) the HBV vaccination coverage in Roma children under two years of age was 43.5%[37]. On the other hand, in the Czech Republic, 95% of Roma children are vaccinated for obligatory diseases, including HBV[1].
Tattooing, blood transfusions, drug use, and imprisonment carry a high risk for HBV and are more common in Roma people[38]. However, it is considered that sexual intercourse is more significant for horizontal transmission of HBV among Roma, since a minority of them use preventive methods against sexually transmitted diseases[34,38]. Vaccination against HBV is less common in Roma; it is not completed because of lack of compliance[38]. Lastly, the efficacy of HBV treatment in Roma is concerning, mainly due to non-compliance and poor availability of healthcare[34].
Hepatitis C virus (HCV) is a widespread cause of acute and chronic hepatitis and a significant risk factor for liver cirrhosis and hepatocellular carcinoma. Around 71 million people worldwide are suffering from chronic hepatitis C infection[39]. It is a blood-borne virus, most commonly transmitted by contaminated needles (intravenous drug users), through blood transfusions or sexual intercourse[40,41]. Vertical transmission is also possible[39].
Some of the risky behaviors appear to be common among Roma. For instance, studies reported an increase in Roma women participating in sex work and a higher prevalence of injection drug use among Roma[3,42,43].
In 2010, a seroprevalence study on HCV was conducted among Roma youth aged 15–24 years in two cities in Serbia-Belgrade (the nation's capital and largest city with 1.2% of residents estimated to be Roma) and Kragujevac (the fourth largest city in Serbia with up to 14% Roma by estimates). Although some of the risk factors were highly prevalent (intravenous drug use, 0.5%-3%; experience with sex workers, 5%-10%; tattooing in non-sterile conditions, 2%-14%; the use of a condom with a constant partner, 1%-25%), only four of 240 (1.7%) participants tested positive for HCV antibodies. Two reported intravenous drug use and three reported having a tattoo[44].
Similar results were found in Slovakia among 441 Roma with HCV seropositivity of 0.7% (1.5% in the general population). Predisposing factors for HCV were tattooing, blood transfusions, and having more sexual partners[32]. In a study conducted among students of two elementary schools in Greece (2002), none of the 118 Roma children involved were positive for HCV antibodies[36]. According to these studies, HCV infection is not as frequent as other hepatitis viruses among Roma.
Hepatitis E virus (HEV) is an emerging viral disease, with 20 million infection cases and 55000 deaths worldwide. Its prevalence is higher in developing countries; however, lately, it has been recognized as a significant cause of hepatitis in resource-rich countries[45]. HEV can be transmitted through contaminated water; however, food-borne, blood transfusion-related transmission by gained significant attention in recent decades[45,46].
The data about HEV among Roma in Europe are scarce and conducted only in Slovakia. The Roma population's HEV prevalence ranged from 21.5% to 45.5%, and the only significant risk factor appeared to be the consumption of raw meat[47,48].
In 2016, the World Health Organization adopted the first Global Health Sector Strategy on Viral Hepatitis, calling for its elimination as a public health threat. The strategy presented a target for 2030–of reducing new hepatitis B and C infections by 90% and mortality by 65%[14]. Roma constitute the most important transnational minority in Europe and a highly vulnerable population affected by viral hepatitis. Based on their epidemiological and social context, living conditions, lack of access to clean water, safe food, and medical services to maintain effective infection control measures, Roma should be considered a high priority group in managing viral hepatitis.
Screening is of particular importance as data on viral hepatitis prevalence in European Roma are scarce and limited to specific regions (Table 1). In Roma, hepatitis B prevalence is high, and mother-to-child transmission is likely a major mode of transmission and early childhood infection based on low vaccination. In addition, the fecal-oral and/or food-borne hepatitis (HAV and HEV) are more common in Roma than in the non-Roma population. In contrast, HCV infection does not seem to be more frequent in Roma.
| Region | Year | Population, N | (Sero) Prevalence | Acute cases/outbreaks | Ref. |
| Northeastern Greece | 2007 | 124 inhabitants of Xanthi, Rodopi and Evros, mostly Roma | 54% males, 46% females, age 2–17 yr | Vantarakis et al[16], 2010 | |
| Greece | 2004–2013 | 295 Roma/995 confirmed cases | Median age 5.9 yr; 2007 outbreak: 139 cases, 82% Roma | Mellou et al[20], 2015 | |
| Greece | 2009-2018 | 240 Roma/1193 confirmed cases | 51.2% males, 80.4% < 15 years old, median age 7 yr; 20 clusters recorded among Roma; 2013: Greatest outbreak, 112 cases among Roma | Mellou et al[19], 2020 | |
| Athens, Greece | 1999-2013 | 467 children hospitalized with hepatitis A, age 0-14 yr | HAV hospitalization rates per 1000 admissions, among Roma: 233.1 (1999-2008), 54.3 (2009-2013) | Papaevangelou et al[27], 2016 | |
| Western Athens, Greece | 2002 | 216 children from two elementary schools, 118 Roma | Anti-HAV IgG: Roma children 98%, non-Roma children 33% | Michos et al[36], 2008 | |
| Slovakia | 2008 | 667 cases reported to Epidemiological Information System database | 536 cases in “low hygienic standards” areas; considered Roma; 4/9 outbreaks in areas with mostly Roma population; Lomnička outbreak (99% Roma population): 298 cases, 297 < 18 years old | Hrivniaková et al[21], 2009 | |
| South Bulgaria | 2005-2008 | 3911 patients with hepatitis A treated in Clinics of Infectious Diseases, Plovdiv | Incidence rate in group living in poor hygienic conditions (mostly Roma): 450.66/100000; Outbreak in Stolipinovo quarter (2006); 1004 cases, mostly Roma | Stoycheva et al[24], 2011 | |
| San Sebastian, Spain | 1995 | 73 Roma, age 2-16 yr | Total anti-HAV 82.2 %, total anti-HAV 50% in children 2-5 yr, total anti-HAV 92.7% in children > 5 yr | Cilla et al[25], 1995 | |
| Eastern Slovakia (9 regions) | 2008-2009 | 59279 serum samples (13798were part of the pregnancy screening) | HBsAg overall 2.18%-9.07%; pregnant women 0.82%-4.13% | Kristian et al[33], 2013 | |
| Eastern Slovakia | 2011 | 452 Roma, adult population | HBsAg 12.4%; anti-HBc 52.8%; HBV DNA 94.3% | Drazilova et al[34], 2018 | |
| Sheffield, United Kingdom | 2007-2013 | 436 Slovak-Roma adult population | HBsAg 9.4%; anti-HBc 28% | Gregory et al[35], 2014 | |
| Western Athens, Greece | 2002 | 118 Roma children | HBsAg 4.2%; anti-HBs 13.6%; anti-HBc 22.0% | Michos et al[36], 2008 | |
| Serbia (Belgrade and Kragujevac) | 2010 | 240 Roma, age 20-24 yr | Anti-HCV 1.7% | Djonic et al[44], 2013 | |
| Eastern Slovakia, Košice region | 2011 | 441 Roma, age 18-55 yr | Anti-HCV 0.7% | Veselíny et al[32], 2014 | |
| Western Athens, Greece | 2002 | 216 children from two elementary schools, age 5-15 yr, 118 Roma | Anti-HCV 0% | Michos et al[36], 2008 | |
| Eastern Slovakia | 2011 | 195 Roma living in Roma settlements, age 18-55 yr | Total anti-HEV 21.5%, highest in Roma men–29.4% | Halánová et al[47], 2018 | |
| Košice, eastern Slovakia | 2018 | 175 patients hospitalized in Department of Infectology and Travel Medicine, age 19-94 yr, 11 Roma | Total anti-HEV 45.5% | Paraličová et al[48], 2020 |
The challenges in the Roma population are high. However, in the attempt to improve Roma's health and reduce health inequalities, viral hepatitis screening programs, facilitated linkage to care with access to affordable antivirals and vaccines should be continuously implemented through Roma communities. Effectively combating viral hepatitis may also reduce maternal and child mortality, as the mortality from non-communicable diseases. This strategy and its far-fetched implications may alleviate poverty and facilitate further development in terms of managing sanitation and water, reducing inequality in access to services, and promoting non-discrimination.
All European countries approved the WHO strategy, and now we have just one decade left to reach the goals and fulfill these promises.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Croatia
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Schiff ER S-Editor: Fan JR L-Editor: A P-Editor: Liu JH
| 1. | European Commission: Roma Health Report [Internet]. 2014 [cited 2020 Oct. 25]. Available from: https://ec.europa.eu/health/sites/health/files/social_determinants/docs/2014_roma_health_report_en.pdf. |
| 2. | Sepkowitz KA. Health of the world's Roma population. Lancet. 2006;367:1707-1708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 41] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Hajioff S, McKee M. The health of the Roma people: a review of the published literature. J Epidemiol Community Health. 2000;54:864-869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 175] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 4. | Vivian C, Dundes L. The crossroads of culture and health among the Roma (Gypsies). J Nurs Scholarsh. 2004;36:86-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | European Union Agency for Fundamental Rights. Roma and travellers in six countries [Internet]. 2020 [cited 2020 Oct. 25]. Available from: https://fra.europa.eu/sites/default/files/fra_uploads/fra-2020-roma-travellers-six-countries_en.pdf. |
| 6. | Jarcuska P, Bobakova D, Uhrin J, Bobak L, Babinska I, Kolarcik P, Veselska Z, Madarasova Geckova A; HEPA-META team. Are barriers in accessing health services in the Roma population associated with worse health status among Roma? Int J Public Health. 2013;58:427-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 7. | Rosicova K, Madarasova Geckova A, van Dijk JP, Kollarova J, Rosic M, Groothoff JW. Regional socioeconomic indicators and ethnicity as predictors of regional infant mortality rate in Slovakia. Int J Public Health. 2011;56:523-531. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Sedláková D. Low socioeconomic status and unhealthy lifestyle lead to high morbidity in young Roma of East Slovakia. Cent Eur J Public Health. 2014;22 Suppl:S3-S5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Babinská I, Gecková AM, Jarcuska P, Pella D, Mareková M, Stefková G, Veselská ZD; HepaMeta Team. Does the population living in Roma settlements differ in physical activity, smoking and alcohol consumption from the majority population in Slovakia? Cent Eur J Public Health. 2014;22 Suppl:S22-S27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Petek D, Rotar Pavlic D, Svab I, Lolić D. Attitudes of Roma toward smoking: qualitative study in Slovenia. Croat Med J. 2006;47:344-347. [PubMed] |
| 11. | Shaaf M. Roma Health Mediators: Successes and Challenges [Internet]. 2011 [cited 2020 Oct. 25]. Available from: https://www.opensocietyfoundations.org/publications/roma-health-mediators-successes-and-challenges#publications_download. |
| 12. | Janicko M, Senajová G, Drazilová S, Veselíny E, Fedacko J, Siegfried L, Kristian P, Virág L, Pella D, Mareková M, Gecková AM, Kalanin P, Jarcuska P, Halánová M; HepaMeta Team. Association between metabolic syndrome and hepatitis B virus infection in the Roma population in eastern Slovakia: a population-based study. Cent Eur J Public Health. 2014;22 Suppl:S37-S42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Gecková AM, Babinská I, Bobáková D, Veselská ZD, Bosáková L, Kolarcik P, Jarcuska P, Pella D, Halánová M; HepaMeta Team. Socioeconomic characteristics of the population living in Roma settlements and their association with health and health-related behaviour. Cent Eur J Public Health. 2014;22 Suppl:S57-S64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 14. | World Health Organization. Global health sector strategy on viral hepatitis, 2016–2021 [Internet]. 2016 [cited 2020 Oct. 25]. Available from: https://apps.who.int/iris/bitstream/handle/10665/246177/WHO-HIV-2016.06-eng.pdf?sequence=1. |
| 15. | European Centre for Disease Prevention and Control. Surveillance Atlas of Infectious Diseases [Internet]. 2020 [cited 2020 Oct. 6]. Available from: https://atlas.ecdc.europa.eu/public/index.aspx. |
| 16. | Vantarakis A, Nearxou A, Pagonidis D, Melegos F, Seretidis J, Kokkinos P, Zarkadis I, Parasidis T, Alamanos Y. An outbreak of hepatitis A in Roma populations living in three prefectures in Greece. Epidemiol Infect. 2010;138:1025-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Jacobsen KH, Wiersma ST. Hepatitis A virus seroprevalence by age and world region, 1990 and 2005. Vaccine. 2010;28:6653-6657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 394] [Cited by in RCA: 328] [Article Influence: 21.9] [Reference Citation Analysis (3)] |
| 18. | Jacobsen KH. Globalization and the Changing Epidemiology of Hepatitis A Virus. Cold Spring Harb Perspect Med. 2018;8:a031716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 103] [Article Influence: 14.7] [Reference Citation Analysis (1)] |
| 19. | Mellou K, Chrysostomou A, Sideroglou T, Kyritsi M, Georgakopoulou T, Tsiodras S, Hadjichristodoulou C. Epidemiology of hepatitis A in Greece in the last decade: management of reported cases and outbreaks and lessons learned. Epidemiol Infect. 2020;148:e58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Mellou K, Sideroglou T, Papaevangelou V, Katsiaflaka A, Bitsolas N, Verykouki E, Triantafillou E, Baka A, Georgakopoulou T, Hadjichristodoulou C. Considerations on the current universal vaccination policy against hepatitis A in Greece after recent outbreaks. PLoS One. 2015;10:e0116939. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Hrivniaková L, Sláciková M, Kolcunová S. Hepatitis A outbreak in a Roma village in eastern Slovakia, August-November 2008. Euro Surveill. 2009;14:19093. [PubMed] |
| 22. | Papamichail D, Petraki I, Arkoudis C, Terzidis A, Smyrnakis E, Benos A, Panagiotopoulos T. Low vaccination coverage of Greek Roma children amid economic crisis: national survey using stratified cluster sampling. Eur J Public Health. 2017;27:318-324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Rodrigues L, Pista A, Oliveira A, Agua-Doce I, Manita C, Paixão MT. Molecular epidemiology of hepatitis A virus in a group of Portuguese citizens living in Lisbon area. J Med Virol. 2007;79:483-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | Stoycheva M, Vatev N, Petrov A, Venchev C, Atanasova M. Epidemiological Study of Hepatitis A in Plovdiv Region – Bulgaria, 2005-2008. World J Vaccines. 2011;1:162-168. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 25. | Cilla G, Perez-Trallero E, Marimon JM, Erdozain S, Gutierrez C. Prevalence of hepatitis A antibody among disadvantaged gypsy children in northern Spain. Epidemiol Infect. 1995;115:157-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 26. | Stojanovski K, McWeeney G, Emiroglu N, Ostlin P, Koller T, Licari L, Kaluski DN. Risk factors for low vaccination coverage among Roma children in disadvantaged settlements in Belgrade, Serbia. Vaccine. 2012;30:5459-5463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Papaevangelou V, Alexopoulou Z, Hadjichristodoulou C, Kourlamba G, Katsioulis A, Theodoridou K, Spoulou V, Theodoridou M. Time trends in pediatric hospitalizations for hepatitis A in Greece (1999-2013): Assessment of the impact of universal infant immunization in 2008. Hum Vaccin Immunother. 2016;12:1852-1856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Polaris Observatory Collaborators. Global prevalence, treatment, and prevention of hepatitis B virus infection in 2016: a modelling study. Lancet Gastroenterol Hepatol. 2018;3:383-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1260] [Cited by in RCA: 1210] [Article Influence: 172.9] [Reference Citation Analysis (2)] |
| 29. | Zanetti AR, Van Damme P, Shouval D. The global impact of vaccination against hepatitis B: a historical overview. Vaccine. 2008;26:6266-6273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 286] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 30. | Nardone A, Anastassopoulou CG, Theeten H, Kriz B, Davidkin I, Thierfelder W, O'Flanagan D, Bruzzone B, Mossong J, Boot HJ, Butur D, Slaciková M, Panait ML, Hellenbrand W, DE Melker H, Sobotová Z, Icardi G, Andrews N, Pebody RG, VAN Damme P, Kafatos G, Miller E, Hatzakis A. A comparison of hepatitis B seroepidemiology in ten European countries. Epidemiol Infect. 2009;137:961-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 31. | Babinska I, Veselska ZD, Bobakova D, Pella D, Panico S, Reijneveld SA, Jarcuska P, Jarcuska P, Zezula I, Geckova AM; HEPA-META team. Is the cardiovascular risk profile of people living in Roma settlements worse in comparison with the majority population in Slovakia? Int J Public Health. 2013;58:417-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 32. | Veselíny E, Janicko M, Drazilová S, Siegfried L, Pastvová L, Schréter I, Kristian P, Viág L, Jarcuska P, Valková I, Cáriková K, Senajová G, Fedacko J, Pella D, Mareková M, Gecková AM, Jarcuska P; HepaMeta Team. High hepatitis B and low hepatitis C prevalence in Roma population in eastern Slovakia. Cent Eur J Public Health. 2014;22 Suppl:S51-S56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 33. | Kristian P, Veselská ZD, Paralicová Z, Jarcuska P, Virág L, Valková I, Schréter I. Regional and ethnic aspects of viral hepatitis B among pregnant women. Cent Eur J Public Health. 2013;21:22-25. [PubMed] |
| 34. | Drazilova S, Janicko M, Kristian P, Schreter I, Halanova M, Urbancikova I, Madarasova-Geckova A, Marekova M, Pella D, Jarcuska P; HepaMeta Team. Prevalence and Risk Factors for Hepatitis B Virus Infection in Roma and Non-Roma People in Slovakia. Int J Environ Res Public Health. 2018;15:1047. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 35. | Gregory A, Vedio A, Stone B, Green S, Bronsdon C. Targeted testing in primary care demonstrates high prevalence of hepatitis B infection within the Slovak-Roma population in Sheffield, UK. J Viral Hepat. 2014;21:e138-e139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 36. | Michos A, Terzidis A, Kalampoki V, Pantelakis K, Spanos T, Petridou ET. Seroprevalence and risk factors for hepatitis A, B, and C among Roma and non-Roma children in a deprived area of Athens, Greece. J Med Virol. 2008;80:791-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 37. | Medicines du Monde. Rapport d’enquête sur la couverture vaccinale des populations rroms rencontrées par les équipes de Médecins du Monde en France [Internet]. 2011 [cited 2020 Oct. 25]. Available from: https://fnasat.centredoc.fr/doc_num.php?explnum_id=208. |
| 38. | Drazilova S, Kristian P, Janicko M, Halanova M, Safcak D, Dorcakova PD, Marekova M, Pella D, Madarasova-Geckova A, Jarcuska P, HepaMeta Team. What is the Role of the Horizontal Transmission of Hepatitis B Virus Infection in Young Adult and Middle-Aged Roma Population Living in the Settlements in East Slovakia? Int J Environ Res Public Health. 2020;17:3293. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 39. | World Health Organization. Hepatitis C [Internet]. 2020 [cited 2020 Oct. 12]. Available from: https://www.who.int/news-room/fact-sheets/detail/hepatitis-c. |
| 40. | Cavlek TV, Margan IG, Lepej SZ, Kolaric B, Vince A. Seroprevalence, risk factors, and hepatitis C virus genotypes in groups with high-risk sexual behavior in Croatia. J Med Virol. 2009;81:1348-1353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 41. | Vilibic-Cavlek T, Kucinar J, Kaic B, Vilibic M, Pandak N, Barbic L, Stevanovic V, Vranes J. Epidemiology of hepatitis C in Croatia in the European context. World J Gastroenterol. 2015;21:9476-9493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 42. | Iraurgi I, Jiménez-Lerma JM, Landabaso MA, Arrazola X, Gutiérrez-Fraile M. Gypsies and drug addictions. Study of the adherence to treatment. Eur Addict Res. 2000;6:34-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 43. | Casals M, Pila P, Langohr K, Millet JP, Caylà JA; Roma Population Working Group. Incidence of infectious diseases and survival among the Roma population: a longitudinal cohort study. Eur J Public Health. 2012;22:262-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 44. | Djonic D, Djuric M, Bassioni-Stamenic F, McFarland W, Knezevic T, Nikolic S, Zivkovic V, Vallabhaneni S. HIV-related risk behaviors among Roma youth in Serbia: results of two community-based surveys. J Adolesc Health. 2013;52:234-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 45. | European Association for the Study of the Liver. EASL Clinical Practice Guidelines on hepatitis E virus infection. J Hepatol. 2018;68:1256-1271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 450] [Cited by in RCA: 441] [Article Influence: 63.0] [Reference Citation Analysis (0)] |
| 46. | Mrzljak A, Dinjar-Kujundzic P, Jemersic L, Prpic J, Barbic L, Savic V, Stevanovic V, Vilibic-Cavlek T. Epidemiology of hepatitis E in South-East Europe in the "One Health" concept. World J Gastroenterol. 2019;25:3168-3182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 25] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 47. | Halánová M, Veseliny E, Kalinová Z, Jarčuška P, Janičko M, Urbančíková I, Pella D, Dražilová S, Babinská I; HepaMeta Team. Seroprevalence of Hepatitis E Virus in Roma Settlements: A Comparison with the General Population in Slovakia. Int J Environ Res Public Health. 2018;15:904. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 48. | Paraličová Z, Halánová M, Schréter I, Kalinová Z, Novotný M, Sekula J, Paralič J, Kristian P. Seroprevalence of hepatitis E among hospitalized patients in Slovakia: first report. Cent Eur J Public Health. 2020;28:70-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |