Published online Mar 28, 2021. doi: 10.3748/wjg.v27.i12.1161
Peer-review started: December 18, 2020
First decision: January 10, 2021
Revised: January 20, 2021
Accepted: March 13, 2021
Article in press: March 13, 2021
Published online: March 28, 2021
Processing time: 96 Days and 12.3 Hours
The impact of perioperative blood transfusion on short- and long-term outcomes in pediatric living donor liver transplantation (PLDLT) must still be ascertained, mainly among young children. Clinical and surgical postoperative complications related to perioperative blood transfusion are well described up to three months after adult liver transplantation.
To determine whether transfusion is associated with early and late postoperative complications and mortality in small patients undergoing PLDLT.
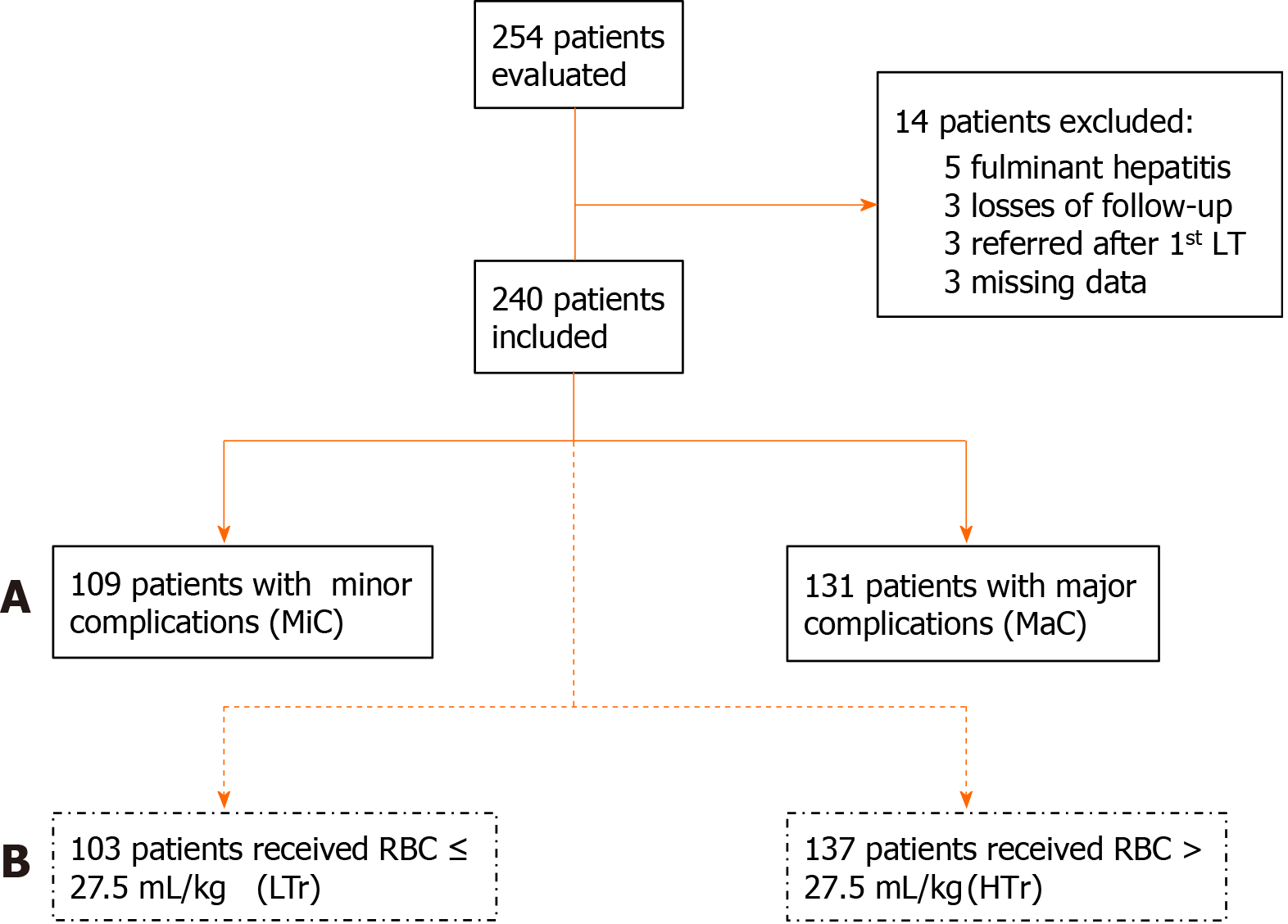
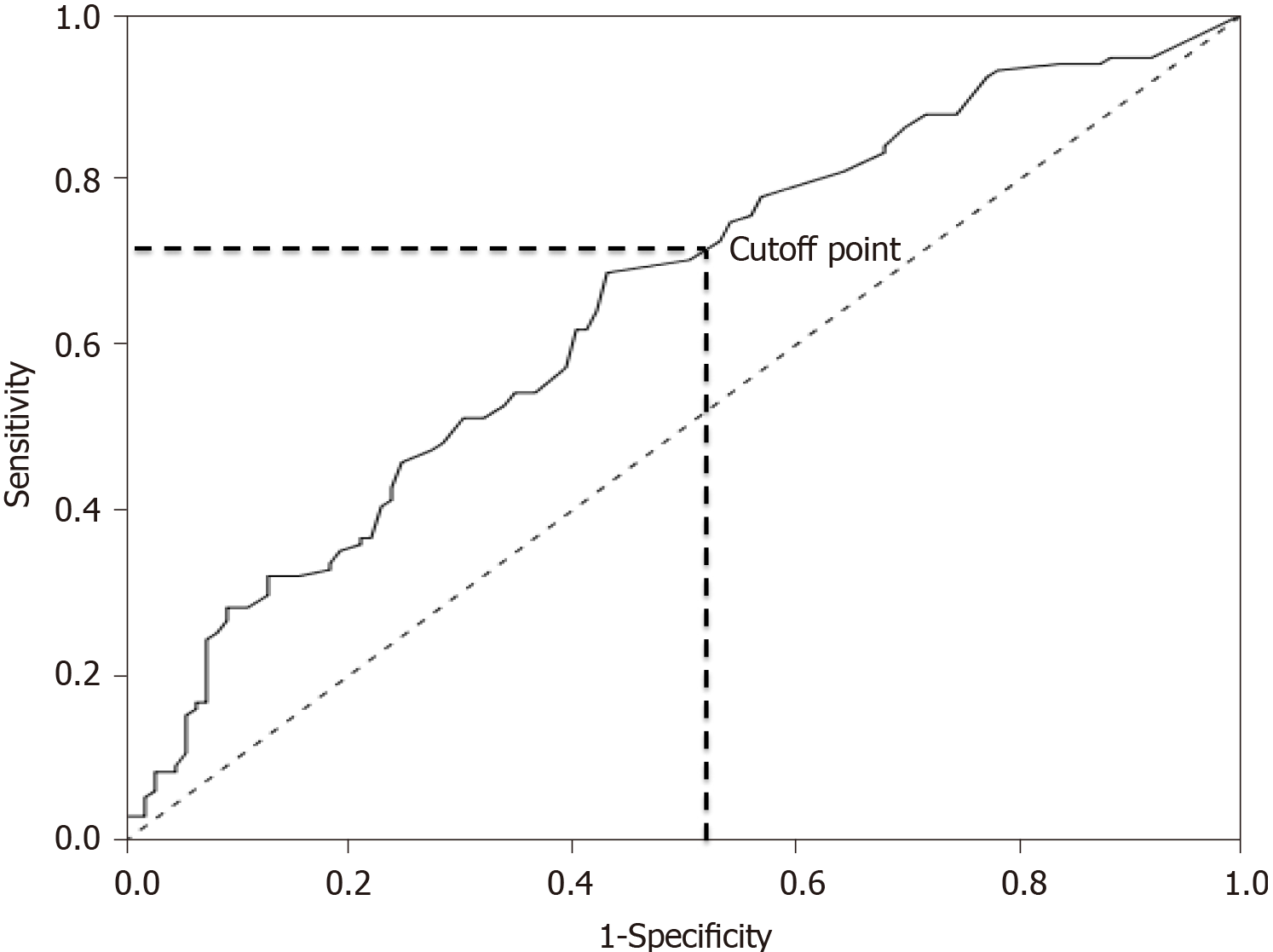
We evaluated the effects of perioperative transfusion on postoperative complications in recipients up to 20 kg of body weight, submitted to PLDLT. A total of 240 patients were retrospectively allocated into two groups according to postoperative complications: Minor complications (n = 109) and major complications (n = 131). Multiple logistic regression analysis identified the volume of perioperative packed red blood cells (RBC) transfusion as the only independent risk factor for major postoperative complications. The receiver operating characteristic curve was drawn to identify the optimal volume of the perioperative RBC transfusion related to the presence of major postoperative complications, defining a cutoff point of 27.5 mL/kg. Subsequently, patients were reallocated to a low-volume transfusion group (LTr; n = 103, RBC ≤ 27.5 mL/kg) and a high-volume transfusion group (HTr; n = 137, RBC > 27.5 mL/kg) so that the outcome could be analyzed.
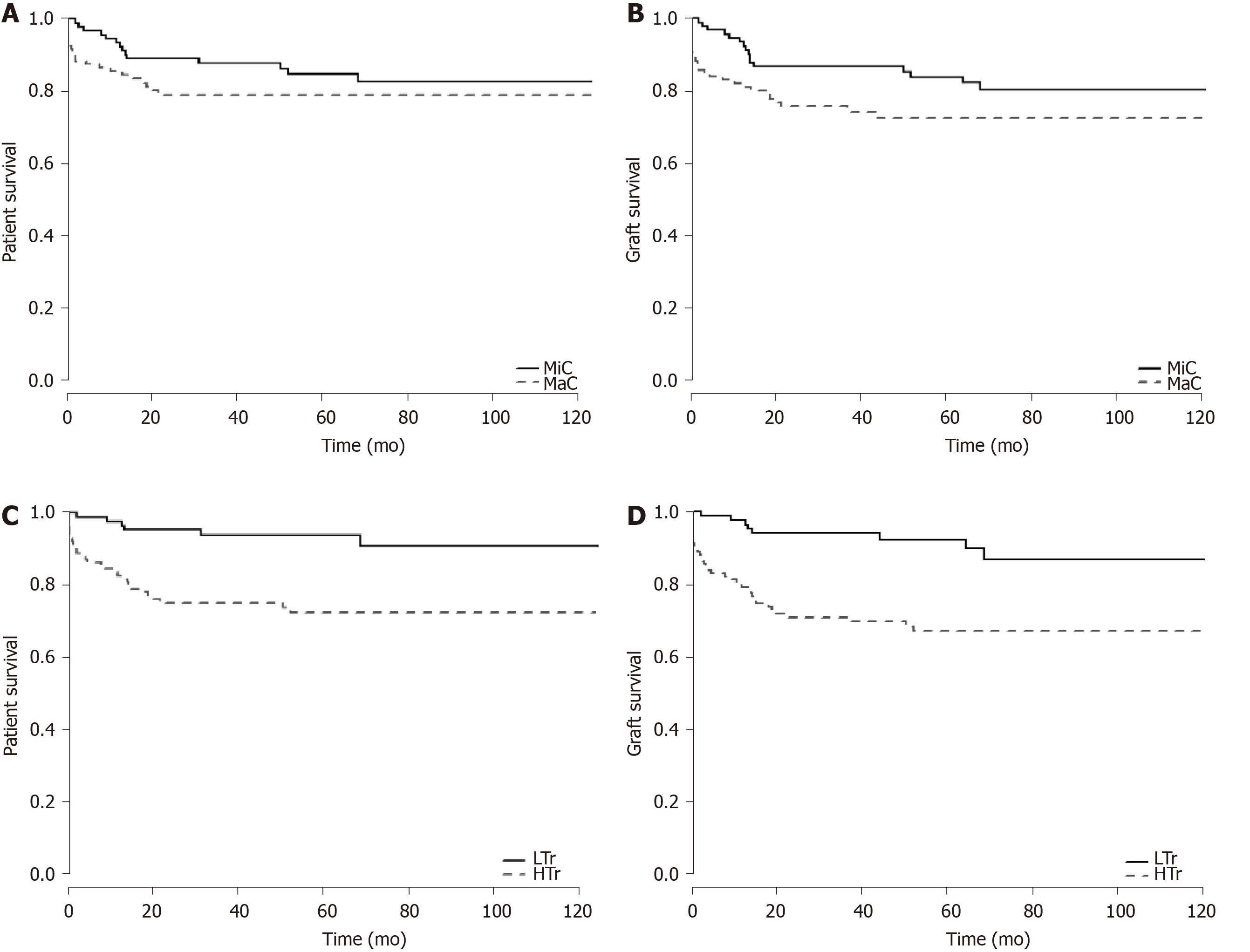
High-volume transfusion was associated with an increased number of major complications and mortality during hospitalization up to a 10-year follow-up period. During a short-term period, the HTr showed an increase in major infectious, cardiovascular, respiratory, and bleeding complications, with a decrease in rejection complications compared to the LTr. Over a long-term period, the HTr showed an increase in major infectious, cardiovascular, respiratory, and minor neoplastic complications, with a decrease in rejection complications. Additionally, Cox hazard regression found that high-volume RBC transfusion increased the mortality risk by 3.031-fold compared to low-volume transfusion. The Kaplan-Meier survival curves of the studied groups were compared using log-rank tests and the analysis showed significantly decreased graft survival, but with no impact in patient survival related to major complications. On the other hand, there was a significant decrease in both graft and patient survival, with high-volume RBC transfusion.
Transfusion of RBC volume higher than 27.5 mL/kg during the perioperative period is associated with a significant increase in short- and long-term postoperative morbidity and mortality after PLDLT.
Core Tip: This study aimed to assess whether perioperative transfusion is associated with early and late postoperative complications and mortality in small patients undergoing pediatric living donor liver transplantation (PLDLT). The volume of perioperative packed red blood cell (RBC) transfusion was the only independent risk factor for major postoperative complications. The perioperative volume of RBC > 27.5 mL/kg was an independent risk factor for mortality, increasing the risk by 3.031-fold, and was directly related to reduced patient and graft survival. In conclusion, not even massive transfusion, in the perioperative period, was associated with a significant increase in short- and long-term postoperative morbimortality after PLDLT.
- Citation: Gordon K, Figueira ERR, Rocha-Filho JA, Mondadori LA, Joaquim EHG, Seda-Neto J, da Fonseca EA, Pugliese RPS, Vintimilla AM, Auler Jr JOC, Carmona MJC, D'Alburquerque LAC. Perioperative blood transfusion decreases long-term survival in pediatric living donor liver transplantation. World J Gastroenterol 2021; 27(12): 1161-1181
- URL: https://www.wjgnet.com/1007-9327/full/v27/i12/1161.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i12.1161
Blood transfusion has been associated with increased morbimortality rates in major surgical procedures such as hepatic resection[1,2], cardiac[3] and non-cardiac major thoracoabdominal surgeries[4], and adult liver transplantation (LT)[5,6]. Regarding adult LT, Boyd et al[7] showed that intraoperative red blood cell (RBC) transfusion volume, a positive history of anti-RBC alloantibodies, and the immunosuppressive regimen used are associated with patient mortality. De Boer et al[5] reported that the indication for LT and the number of platelets or RBC units transfused during surgery are risk factors for 1-year graft survival; additionally, the number of RBC or platelet units transfused during surgery, cold ischemia time, and surgical team experience are risk factors for 5-year graft survival. Also, RBC transfusion has been associated with an increased rate of cancer recurrence. Indeed, the relative risk of digestive cancer recurrence has been reported to increase by 2.1-fold after the administration of ≥ 3 units[8]. Storage time and the timing of the transfusion related to surgery may also play a role[8]. In patients undergoing adult LT, all blood products (BP) are related to increased postoperative complications[9,10]; consequently, there is a trend towards reducing their use[11-13].
The harmful effects of perioperative transfusion in small pediatric patients are unclear pediatric LT. López Santamaría et al[11] suggested decreased graft survival associated with massive intraoperative blood transfusion, which was defined in their study as a loss greater than four volemias. They found four independent risk factors for mortality: Recipient’s age < 3 years, retransplantation, severity of the underlying disease, and the transplant team’s experience. Blood transfusion was not among them, however. To date, few reports have addressed the risks of transfusion in pediatric LT. In 2012, Nacoti et al[14] found that perioperative transfusion of fresh frozen plasma (FFP) RBC are independent risk factors for decreasing 1-year patient and graft survival. Nacoti et al[15] reported that intraoperative platelet and RBC transfusion are independent risk factors for developing major complications in the first year after pediatric LT.
Fanna et al[16] showed that high intraoperative bleeding is associated with pre-LT abdominal surgeries, factor V level ≤ 30%, and ex-situ parenchymal transection of the liver graft. Jin et al[17] identified high white blood cell count, low platelet count, and a deceased donor as independent risk factors for massive transfusion, which was defined as the administration of RBC volume ≥ 100% of the total blood volume (TBV). Although the graft failure incidence was higher in the massive group compared to the non-massive group, they found no difference in survival between the groups. Huang et al[18] evaluated pediatric living donor liver transplantation (LDLT) procedures and observed that younger patients with a lower weight, shorter stature, and preoperative prolonged international normalized ratio (INR) required larger blood transfusion volumes. Notwithstanding, preoperative INR was the only risk factor for massive blood transfusion. Kloesel et al[19] identified predictors of massive intraoperative bleeding (estimated blood loss of > TBV within a 24 h period): Preoperative hemoglobin (Hb) < 8.5 g/dL, INR > 1.5, platelet count < 100.000/mm3, and surgery length > 10 h. Except for a longer intensive care unit (ICU) stay, there was no other correlation between massive transfusion and morbimortality.
Pediatric LT includes patients less than 18 years of age with either chronic or acute liver diseases involving deceased and living donors. Underlying pathologies may vary, and even the severity score is different under 12 years old [Pediatric end-stage liver disease (PELD) score]. Importantly, previous studies did not exclusively include young children. In addition, the grafts came from split and whole organs from deceased donors in most samples. Massive transfusion definitions vary across pediatric studies as BP transfusion from one[18] to four[11] volemias. There is still much controversy regarding the type, volume, and timing of BP transfusion and its association with postoperative morbimortality. Thus, this study assessed whether perioperative transfusion is associated with early and late postoperative complications and mortality in small patients undergoing pediatric LDLT (PLDLT).
The Institutional Research Ethics Committees of ACCamargo Cancer Center and the University of São Paulo School of Medicine approved this observational, retrospective, and analytical cohort study according to the Helsinki Statement. All data were completely anonymized before they were accessed, and both committees waived the requirement for informed consent.
We investigated 254 pediatric patients weighing up to 20 kg with non-acute liver diseases who underwent first LDLT performed at the ACCamargo Cancer Center over 10 years. Fourteen patients were excluded: Five had fulminant hepatitis, three had their first transplant performed in other center, three were lost to follow-up, and three had missing data. All 240 enrolled patients underwent standardized procedures and techniques (total intravenous general anesthesia, piggyback inferior vena cava clamping, and exclusive use of hepatic left lateral segment grafts).
Based on the severity of postoperative complications (graded according to the Clavien-Dindo classification during hospital stay), a total of 240 patients were initially allocated into two groups (Figure 1A): The minor complications (MiC) group (n = 109, either with no complications or with grade I-IIIa complications) and the major complications (MaC) group (n = 131, with at least one grade IIIb-V complication). Subsequently, all patients were reallocated into two further groups according to the RBC volume transfused during the perioperative period from 24 h before to 48 h after LT: The low-volume transfusion group (LTr n = 103, RBC ≤ 27.5 mL/kg) and the high-volume transfusion group (HTr n = 137, RBC > 27.5 mL/kg) (Figure 1B).
The Clavien-Dindo classification was applied to assess the relationship between blood transfusion and postoperative complications. In this pediatric population, general anesthesia was ostensibly required to ensure stillness and safety for diagnostic and treatment procedures. Thus, the original grade III was modified and subdivided into IIIa and IIIb according to the complexity of the procedures as low and high, respectively (Table 1). Data on mortality and complications were collected over a 10-year period post-LT. Patients who failed to attend outpatient follow-up after hospital discharge were considered lost to follow-up.
| Grade | Definition |
| I | Complication that requires the use of simple analgesics, antipyretics, anti-emetics, diuretics, electrolytes and physiotherapy |
| II | Complication requiring other drugs, different from grade I, blood transfusion or parenteral nutrition |
| III | Complication requiring surgical, endoscopic or radiologic intervention under any kind of anesthesia |
| IIIa | Low complexity procedures: Small and medium surgery, endoscopy and colonoscopy, US, CT, ERCP or PTCD, arteriography and angioplasty of portal vein or suprahepatic veins and hepatic artery, biopsies, simple teeth extractions, drainages, ostomies and central catheter passage for medication, dialysis or chemotherapy |
| IIIb | High complexity procedures: Large surgery, multiple teeth extractions, vascular and biliodigestive re-anastomosis, laparotomy and thoracotomy |
| IV | Life-threatening complication (including CNS1 complications) requiring ICU admission |
| IVa | Dysfunction of one organ (including dialysis) |
| IVb | Dysfunction of two or more organs |
| V | Death of patient |
Complications were categorized by clinical presentation in 14 types: (1) Bleeding: Epistaxis, gastrointestinal, surgical wound, drains, and systemic hemorrhages due to portal hypertension or coagulopathy with or without need for surgery; (2) Cardiovascular: Systemic arterial hypertension, mismatches of cardiac rhythm, heart failure, hemodynamic instability, and cardiorespiratory arrest; (3) Dermatologic: Skin manifestations of drugs, food, and environmental factors; (4) Gastrointestinal: Malnutrition with weight-for-age z-score, height-for-age z-score[20], weight-for-height z-score, or body-mass-index z-score (BMIZ) ≤ -2 standard deviation, need for enteral or parenteral diet, persistent vomiting or diarrhea ≥ 3 wk, gastroesophageal reflux disease with or without brochoaspiration, visceromegaly, or ascites caused by maintained portal hypertension; (5) Infectious: Positive cultures with clinical or laboratory manifestations except from respiratory infections; (6) Malignancy: Post-transplant lymphoprolipherative disease (PTLD), lymphomas, skin tumors, and relapse of tumors; (7) Metabolic: Hydro-electrolytic serum changes such as hyponatremia (sodium < 133 mEq/L), hypernatremia (sodium > 147 mEq/L), hypokalemia (potassium < 3.0 mEq/L), hyperkalemia (potassium > 5.4 mEq/L), hypocalcemia (ionic calcium < 1.17 mmol/Lol/L), hypomagnesemia (magnesium < 1.8 mg/dL), hypophosphatemia (phosphorus < 2.5 mg/dL), arterial blood gases with pH < 7.2, acidosis and pH > 7.5, alkalosis, hyperlactatemia (lactate > 22 mg/dL), oliguria (diuresis < 0.5 mL/kg/h), adrenal insufficiency, diabetes mellitus, obesity (BMIZ > 2 standard deviations), or dyslipidemia (total cholesterol > 170 mg/dL, LDL fraction > 130 mg/dL, and triglycerides > 130 mg/dL); (8) Miscellaneous: Accidental injuries linked to LT procedure or postoperative follow-up; (9) Neuropsychiatric: Headache, vertigo, seizures, sedation withdrawal syndrome, delayed neuropsychomotor development, school learning difficulties, behavioral changes with psychomotor agitation, attention deficit, mood lability, anxiety, or depression; (10) Primary non-function (PNF) of the graft; (11) Rejection: Clinical and laboratory responsiveness to pulse therapy with methylprednisolone or anatomopathological documentation of acute or chronic rejection; (12) Renal: Renal failure was considered a decay of at least 50% of the estimated glomerular filtration rate (eGFR) applying the simplified revised Schwartz formula[21]; (13) Respiratory: Upper airway infections (rhinitis, sinusitis, otitis, tonsillitis, epiglottitis, pharyngolaryngitis), lower airway infections (tracheitis, bronchopneumonia, pneumonia), prolonged intubations (over 48 h), bronchospasm, atelectasis, effusions, pleural fistulas, hemothorax, pneumothorax, pneumomediastinum, non-cardiogenic edema, or acute respiratory failure; and (14) Surgical: LT specific complications (vascular thrombosis, biliary stenosis and fistulas, reoperation or retransplantation), hernias, dehiscence of anastomoses, or need for exploratory laparotomy except if caused by bleeding.
Multiple logistic regression analysis was performed to identify risk factors for major postoperative complications. The stepwise method was used for the selection of the variables. A perioperative RBC transfusion volume was identified as a single risk factor. A receiver operating characteristic curve was constructed using the perioperative RBC transfusion volume, and the occurrence of major complications were input parameters. A cutoff point of 27.5 mL/kg was identified using Youden’s index (Figure 2).
Student’s t-test or the Mann-Whitney test was used for quantitative variables while the chi-square test or Fisher’s exact test was used for qualitative variables. Independent risk factors for mortality were identified using simple and multiple Cox regression analyses. Overall patient and graft survival analyses were performed using Kaplan–Meier survival curves, which were compared using the log-rank test. A P value level < 0.05 was used to define statistical significance. Statistical analyses were performed using SPSS version 23 (IBM Corp., Armonk, NY, United States) and R program version 3.2.1 (R Foundation for Statistical Computing, Vienna, Austria).
Of the 240 patients included in the study, 136 (56.7%) were females. The median patient age, weight, and stature were 12.4 mo, 8.07 kg, and 70 cm, respectively. Biliary atresia was found in 151 patients (62.9% of the underlying diseases) in our cohort. The Kasai procedure was previously performed in 111 cases (46.3%). The average pre-LT PELD score was 16 (± 7.7).
The overall incidence of major complications was 54.6%. In the MaC, all anthropometric measures, eGFR, Hb, sodium, and albumin levels were significantly lower. The INR, graft-to-body-weight ratio, and transfused BP volume were significantly higher than in the MiC. However, the only independent risk factor for major complications was perioperative RBC transfusion volume (Table 2).
| Variables | mean ± SD or No (%) | P value | OR | 95%CI | P value | |
| MiC, n = 109 | MaC, n = 131 | |||||
| Male gender | 54 (49.5) | 52 (39.7) | 0.081 | |||
| Age (d) | 632 ± 440 | 512 ± 490 | < 0.001 | |||
| Weight (kg) | 9.67 ± 2.91 | 8.61 ± 3.09 | < 0.001 | |||
| Height (cm) | 76.6 ± 11.2 | 71.9 ± 11.6 | < 0.001 | |||
| WAZ | -1.28 ± 1.24 | -1.49 ± 1.31 | 0.105 | |||
| HAZ | -0.28 ± 1.15 | -0.54 ± 1.24 | 0.012 | |||
| WHZ | -1.60 ± 1.34 | -2.43 ± 1.48 | < 0.001 | |||
| BMIZ | -0.20 ± 1.11 | -0.36 ± 1.39 | 0.001 | |||
| Ascites | 78 (71.6) | 108 (82.4) | 0.057 | |||
| PELD score | 16.2 ± 7.0 | 17.8 ± 8.2 | 0.14 | |||
| Kasai surgery | 50 (45.9) | 61 (46.6) | 0.698 | |||
| Portal hypertension | 97 (88.9) | 131 (100.0) | 0.132 | |||
| Hepatopulmonary syndrome | 16 (14.7) | 15 (11.5) | 0.414 | |||
| Infections 30 d pre-LT | 0.4 ± 0.6 | 0.6 ± 0.7 | 0.081 | |||
| eGFR (mL/min/1.73 m2)1 | 228 ± 121 | 187 ± 104 | 0.006 | |||
| Hemoglobin (g/dL)2 | 10.2 ± 1.5 | 9.3 ± 1.5 | < 0.001 | |||
| Platelets (× 103/mm3)2 | 196 ± 112 | 193 ± 118 | 0.789 | |||
| INR2 | 1.24 ± 0.25 | 1.49 ± 0.56 | < 0.001 | |||
| Sodium (mEq/L)2 | 137 ± 2.7 | 135 ± 4.3 | < 0.001 | |||
| Potassium (mEq/L)2 | 4.4 ± 0.5 | 4.3 ± 0.7 | 0.613 | |||
| Glucose (mEq/L)2 | 104 ± 59 | 92 ± 60 | 0.313 | |||
| Albumin (g/dL)2 | 2.9 ± 0.9 | 2.5 ± 0.8 | 0.002 | |||
| Total Bilirubin (g/dL)2 | 11.9 ± 7.3 | 13.4 ± 8.8 | 0.304 | |||
| GBWR (%) | 3.3 ± 1.1 | 3.7 ± 1.2 | 0.035 | |||
| RBC (mL/kg)3 | 31.1 ± 25.4 | 46.7 ± 39.7 | < 0.001 | 1.018 | 1.007-1.028 | 0.001 |
| FFP (mL/kg)3 | 0.3 ± 2.6 | 3.0 ± 11.5 | 0.015 | |||
| Platelets (mL/kg)3 | 0.1 ± 0.8 | 1.2 ± 6.0 | 0.021 | |||
| Cryoprecipitate (mL/kg)3 | 0.0 ± 0.0 | 0.1 ± 1.2 | 0.196 | |||
The HTr had lower Hb and sodium levels but significantly higher INR during the intraoperative period than the LTr. Additionally, the HTr had longer anesthetic and surgery time, a higher volume of crystalloids and colloids, higher diuresis rates, a lower incidence of extubation in the operating room, a longer intubation time, and a longer ICU and in-hospital stay than the LTr (Table 3).
| Variables | mean ± SD or No. (%) | P value | |
| LTr, n = 103 | HTr, n = 137 | ||
| Male gender | 48 (46.6) | 58 (42.3) | 0.565 |
| Age (d) | 764 ± 544 | 419 ± 350 | < 0.001 |
| Weight (kg) | 10.67 ± 3.20 | 7.88 ± 2.29 | < 0.001 |
| Height (cm) | 80.0 ± 12.1 | 69.4 ± 8.7 | < 0.001 |
| WAZ | -0.90 ± 1.20 | -1.75 ± 1.21 | < 0.001 |
| HAZ | -0.11 ± 1.41 | -0.54 ± 1.24 | 0.012 |
| WHZ | -1.60 ± 1.34 | -2.43 ± 1.48 | < 0.001 |
| BMIZ | 0.20 ± 1.20 | -0.36 ± 1.39 | 0.001 |
| Ascites | 72 (69.9) | 115 (83.9) | 0.036 |
| PELD score | 14.1 ± 6.2 | 19.1 ± 7.9 | < 0.001 |
| Extra-hepatic cholestasis | 67 (65.0) | 105 (76.6) | 0.029 |
| Intrahepatic cholestasis | 13 (12,6) | 5 (3.6) | 0.002 |
| Cirrhosis | 6 (5.8) | 12 (8.8) | 0.373 |
| Metabolic diseases | 7 (6.8) | 10 (7.3) | 0.852 |
| Malignant diseases | 7 (6.8) | 3 (2.2) | 0.159 |
| Miscellany | 3 (2.9) | 2 (1.5) | 0.751 |
| Kasai surgery | 40 (38.8) | 74 (54.0) | 0.016 |
| Portal hypertension | 96 (93.2) | 132 (96.3) | 0.132 |
| Hepatopulmonary syndrome | 19 (18.4) | 12 (8.7) | 0.043 |
| Infections ≤ 30 d pre-LT | 0 ± 1 | 1 ± 1 | 0.01 |
| eGFR (mL/min/1.73 m2)1 | 229 ± 121 | 188 ± 105 | 0.006 |
| Hemoglobin (g/dL)2 | 10.2 ± 1.5 | 9.3 ± 1.5 | < 0.001 |
| Platelets (× 103/mm3)2 | 196 ± 112 | 193 ± 118 | 0.789 |
| INR2 | 1.24 ± 0.25 | 1.49 ± 0.56 | < 0.001 |
| Sodium (mEq/L)2 | 137 ± 2.6 | 135 ± 4.4 | < 0.001 |
| Potassium (mEq/L)2 | 4.3 ± 0.5 | 4.4 ± 0.6 | 0.613 |
| Glucose (mEq/L)2 | 104 ± 59 | 92 ± 60 | 0.313 |
| Albumin (g/dL)2 | 2.9 ± 0.9 | 2.5 ± 0.8 | 0.002 |
| Total bilirubin (g/dL)2 | 11.9 ± 7.3 | 13.4 ± 8.8 | 0.304 |
| Hemoglobin (g/dL)3 | 8.6 ± 1.5 | 7.6 ± 1.2 | < 0.001 |
| INR3 | 1.23 ± 0.42 | 1.67 ± 0.75 | < 0.001 |
| Sodium (mEq/L)3 | 135 ± 8 | 134 ± 5 | 0.002 |
| Warm ischemia time (min) | 42.2 ± 12.9 | 42.9 ± 11.4 | 0.515 |
| Cold ischemia time (min) | 53.3 ± 34.8 | 67.1 ± 56.3 | 0.118 |
| Anesthetic time (h) | 9.7 ± 1.6 | 10.8 ± 1.9 | < 0.001 |
| Surgical time (h) | 7.8 ± 1.5 | 9.0 ± 1.9 | 0.001 |
| Crystalloid (mL/kg)4 | 179 ± 67 | 251 ± 105 | 0.015 |
| Colloid (mL/kg)4 | 33.6 ± 20.8 | 43.1 ± 19.7 | < 0.001 |
| Diuresis (mL/kg)4 | 47.5 ± 22.9 | 61.3 ± 36.6 | 0.013 |
| GBWR (%) | 2.9 ± 1.0 | 3.9 ± 1.1 | < 0.001 |
| Extubation in OR | 24 (23.1) | 16 (11.8) | 0.014 |
| Intubation period ≥ 48 h | 7 (6.7) | 35 (25.7) | < 0.001 |
| ICU length of stay (d) | 4 ± 5 | 8 ± 13 | 0.001 |
| Hospital length of stay (d) | 17 ± 13 | 23 ± 21 | 0.010 |
During hospitalization, the incidence of major complications per patient and the proportion of major complications were significantly higher in the HTr compared to the LTr (Table 4). Metabolic complications accounted for 28.2% of the complications during hospitalization. Additionally, complications such as gastrointestinal, malignancy, miscellany, neuropsychiatric, PNF, renal, and surgical were observed but with no significant difference between transfusion groups. The HTr had significantly more bleeding, respiratory, major cardiovascular, and major infectious complications but less dermatologic complications and rejections than the LTr (Table 5). Early LT-specific complications include PNF (2.1%), biliary fistula (6.2%), hepatic artery thrombosis (HAT) (3.3%), portal venous thrombosis (PVT) (9.2%), and retransplantation (1.2%); these were not related to a higher perioperative transfusion volume (Table 6). In terms of RBC transfusion volume, there was a significantly higher rate of 30 d reoperation (26.3% × 8.7%, P < 0.001) and 30 d mortality rate (6.6% × 0.0%, P < 0.001) in the HTr vs LTr, respectively (Table 6).
| Variables | All patients, n = 240 | ||
| All complications during hospitalization, n = 783 | |||
| mean ± SD or No. (%) | P value | ||
| LTr, n = 103 | HTr, n = 137 | ||
| Patients with any complication | 95 (92.2) | 132 (96.4) | 0.264 |
| Patients with major complications (IIIb-V) | 41 (39.8) | 90 (65.7) | < 0.001 |
| Complications per patient | 2.5 ± 1.7 | 3.8 ± 3.6 | 0.007 |
| Number of major complications (IIIb-V) | 54/262 (20.6) | 207/521 (39.7) | < 0.001 |
| Median of the highest degrees of complication | IIIa (I-IVb) | IVa (I-V) | < 0.001 |
| Median grade of complications per patient | II (I-IIIb) | II (I-V) | < 0.001 |
| Complication | Hospitalization | 1 yr | 5 yr | 10 yr | |||||||||
| Type | Grade | LTr | HTr | P value | LTr | HTr | P value | LTr | HTr | P value | LTr | HTr | P value |
| Bleeding (%) | Minor | 1(0.4) | 6(1.1) | 0.252 | 5(0.9) | 11(1.3) | 0.61 | 5(0.5) | 13(0.9) | 0.237 | 5(0.5) | 13(0.9) | 0.236 |
| Major | 0(0) | 9(1.8) | 0.211 | 1(0.2) | 9(1.0) | 0.465 | 1(0.1) | 9(0.7) | 0.467 | 1(0.1) | 9(0.6) | 0.297 | |
| Subtotal | 1(0.4) | 15(2.9) | 0.016 | 6(1.1) | 20(2.3) | 0.178 | 6(0.6) | 22(1.6) | 0.052 | 6(0.6) | 22(1.4) | 0.068 | |
| Cardiovascular (%) | Minor | 17(6.5) | 29(5.6) | 0.754 | 19(3.6) | 32(3.6) | 0.662 | 24(2.6) | 39(2.8) | 0.518 | 25(2.5) | 42(2.7) | 0.381 |
| Major | 0(0) | 17(3.3) | 0.028 | 0(0) | 18(2.0) | 0.017 | 0(0) | 18(1.3) | 0.005 | 0(0) | 18(1.2) | 0.005 | |
| Subtotal | 17(6.5) | 46(8.9) | 0.319 | 19(3.6) | 50(5.8) | 0.098 | 24(2.6) | 57(4.1) | 0.075 | 25(2.5) | 60(3.9) | 0.282 | |
| Dermatologic (%) | Minor | 9(3.4) | 5(1.0) | 0.093 | 25(4.7) | 16(1.8) | 0.009 | 52(5.6) | 58(4.1) | 0.322 | 59(5.8) | 71(4.6) | 0.583 |
| Major | 0(0) | 1(0.2) | 1 | 1(0.2) | 1(0.1) | 0.406 | 7(0.8) | 10(0.7) | 0.168 | 8(0.8) | 10(0.7) | 0.114 | |
| Subtotal | 9(3.4) | 6(1.2) | 0.049 | 26(4.9) | 17(1.9) | 0.003 | 59(6.4) | 68(4.8) | 0.134 | 67(6.6) | 81(5.3) | 0.209 | |
| Gastrointestinal (%) | Minor | 5(1.9) | 13(2.5) | 0.336 | 15(2.8) | 30(3.4) | 0.353 | 30(3.3) | 44(3.1) | 0.721 | 33(3.2) | 49(3.2) | 0.65 |
| Major | 0(0) | 1(0.2) | 1 | 1(0.2) | 4(0.5) | 1 | 3(0.3) | 6(0.5) | 0.704 | 3(0.3) | 6(0.4) | 0.713 | |
| Subtotal | 5(1.9) | 14(2.7) | 0.627 | 16(3.0) | 34(3.9) | 0.488 | 33(3.6) | 50(3.6) | 1 | 36(3.5) | 55(3.6) | 1 | |
| Infectious (%) | Minor | 21(8) | 32(6.1) | 1 | 86(16.2) | 116(13.2) | 0.577 | 188(20.3) | 235(16.7) | 0.434 | 207(20.3) | 257(16.8) | 0.394 |
| Major | 32(12.2) | 82(15.8) | 0.013 | 43(8.1) | 106(12.1) | 0.028 | 56(6.0) | 132(9.4) | 0.02 | 60(5.9) | 133(8.7) | 0.022 | |
| Subtotal | 53(20.2) | 114(21.9) | 0.66 | 129(24.3) | 222(25.3) | 0.729 | 244(26.3) | 367(26.1) | 0.948 | 267(26.2) | 390(25.5) | 0.743 | |
| Malignancy (%) | Minor | 0(0) | 0(0) | 1 | 4(0.8) | 9(1.0) | 0.576 | 13(1.4) | 32(2.3) | 0.067 | 13(1.3) | 35(2.3) | 0.027 |
| Major | 0(0) | 0(0) | 1 | 4(0.8) | 3(0.3) | 0.058 | 9(1.0) | 13(0.9) | 0.137 | 11(1.1) | 14(0.9) | 0.07 | |
| Subtotal | 0(0) | 0(0) | 1 | 8(1.6) | 12(1.4) | 1 | 22(2.4) | 45(3.2) | 0.296 | 24(2.4) | 49(3.2) | 0.253 | |
| Metabolic (%) | Minor | 86(32.8) | 134(25.7) | 0.786 | 89(16.8) | 140(16.0) | 0.494 | 96(10.4) | 146(10.4) | 0.329 | 102(10.0) | 151(9.9) | 0.416 |
| Major | 1(0.4) | 0(0) | 0.207 | 2(0.4) | 0(0) | 0.052 | 2(0.2) | 0(0) | 0.069 | 2(0.2) | 0(0) | 0.077 | |
| Subtotal | 87(33.2) | 134(25.7) | 0.085 | 91(17.2) | 140(16.0) | 0.605 | 98(10.6) | 146(10.4) | 0.942 | 104(10.2) | 151(9.9) | 0.846 | |
| Miscellany (%) | Minor | 8(3.1) | 25(4.8) | 0.067 | 30(5.7) | 48(5.5) | 0.093 | 66(7.2) | 71(5.1) | 0.179 | 73(7.2) | 74(4.8) | 0.1 |
| Major | 1(0.4) | 5(1.0) | 1 | 3(0.6) | 7(0.8) | 0.702 | 4(0.4) | 14(1.0) | 0.792 | 5(0.5) | 14(0.9) | 1 | |
| Subtotal | 9(3.5) | 30(5.8) | 0.217 | 33(6.3) | 55(6.3) | 1 | 70(7.6) | 85(6.1) | 0.18 | 78(7.7) | 88(5.8) | 0.07 | |
| Neuropsyquiatric (%) | Minor | 3(1.1) | 2(0.4) | 0.391 | 7(1.3) | 4(0.5) | 0.135 | 17(1.8) | 14(1.0) | 0.2 | 24(2.4) | 23(1.5) | 0.297 |
| Major | 1(0.4) | 1(0.2) | 0.371 | 1(0.2) | 1(0.1) | 0.406 | 1(0.1) | 1(0.1) | 0.459 | 2(0.2) | 1(0.1) | 0.188 | |
| Subtotal | 4(1.5) | 3(0.6) | 0.169 | 8(1.5) | 5(0.6) | 0.134 | 18(1.9) | 15(1.1) | 0.116 | 26(2.6) | 24(1.6) | 0.109 | |
| PNF (%) | Minor | 0(0) | 0(0) | 1 | 0(0) | 0(0) | 1 | 0(0) | 0(0) | 1 | 0(0) | 0(0) | 1 |
| Major | 0(0) | 5(1.0) | 0.587 | 0(0) | 5(0.6) | 0.593 | 0(0) | 5(0.4) | 0.332 | 0(0) | 5(0.3) | 0.329 | |
| Subtotal | 0(0) | 5(1.0) | 0.175 | 0(0) | 5(0.6) | 0.164 | 0(0) | 5(0.4) | 0.164 | 0(0) | 5(0.3) | 0.164 | |
| Rejection (%) | Minor | 40(15.3) | 32(6.1) | 0.004 | 73(13.8) | 66(7.5) | 0.003 | 111(12.0) | 102(7.3) | 0.106 | 117(11.5) | 125(8.2) | 0.03 |
| Major | 0(0) | 1(0.2) | 1 | 1(0.2) | 4(0.5) | 1 | 4(0.4) | 8(0.6) | 0.526 | 5(0.5) | 8(0.5) | 0.363 | |
| Subtotal | 40(15.3) | 33(6.3) | <0.001 | 74(14.0) | 70(8.0) | <0.001 | 115(12.4) | 110(7.9) | <0.001 | 122(12.0) | 133(8.7) | <0.001 | |
| Renal (%) | Minor | 2(0.8) | 3(0.6) | 1 | 3(0.6) | 3(0.3) | 0.693 | 4(0.4) | 3(0.2) | 0.469 | 4(0.4) | 4(0.3) | 0.731 |
| Major | 2(0.8) | 5(1.0) | 0.637 | 2(0.4) | 7(0.8) | 1 | 5(0.5) | 9(0.7) | 0.535 | 5(0.5) | 9(0.6) | 0.547 | |
| Subtotal | 4(1.6) | 8(1.6) | 1 | 5(1.0) | 10(1.1) | 0.796 | 9(0.9) | 12(0.9) | 0.945 | 9(0.9) | 13(0.9) | 1 | |
| Respiratory (%) | Minor | 8(3.1) | 24(4.6) | 0.093 | 75(14.2) | 110(12.6) | 0.934 | 161(17.4) | 247(17.6) | 0.141 | 177(17.4) | 261(17.1) | 0.106 |
| Major | 7(2.7) | 36(6.9) | 0.539 | 9(1.7) | 53(6.0) | 0.096 | 14(1.5) | 70(5.0) | 0.029 | 15(1.5) | 71(4.7) | 0.017 | |
| Subtotal | 15(5.8) | 60(11.5) | 0.014 | 84(15.9) | 163(18.6) | 0.217 | 175(18.9) | 317(22.6) | 0.038 | 192(18.9) | 332(21.8) | 0.041 | |
| Surgical (%) | Minor | 8(3.1) | 9(1.8) | 0.617 | 19(3.6) | 23(2.6) | 0.631 | 33(3.6) | 49(3.5) | 0.732 | 43(4.2) | 66(4.3) | 0.487 |
| Major | 10(3.8) | 44(8.4) | 0.711 | 12(2.3) | 51(5.8) | 0.509 | 20(2.2) | 56(4.0) | 1 | 20(2.0) | 58(3.8) | 0.682 | |
| Subtotal | 18(6.9) | 53(10.2) | 0.166 | 31(5.9) | 74(8.4) | 0.092 | 53(5.8) | 105(7.5) | 0.118 | 63(6.2) | 124(8.1) | 0.079 | |
| Total minor complications (%) | 208(79.4) | 314(60.3) | <0.001 | 450(84.9) | 608(69.3) | <0.001 | 800(86.4) | 1053(75.0) | <0.001 | 882(86.6) | 1171(76.7) | <0.001 | |
| Total major complications (%) | 54(20.6) | 207(39.7) | 80(15.1) | 269(30.7) | 126(13.6) | 351(25.0) | 137(13.4) | 356(23.3) | |||||
| Total complications per group (%) | 262(33,5) | 521(66,5) | 530(37,7) | 877(62,3) | 926(39,7) | 1404(60,3) | 1019(40,0) | 1527(60,0) | |||||
| Total complications per period (%) | 783(30,8) | 1407(55,3) | 2330(91,5) | 2546(100) | |||||||||
| Variables | Early complications | Late complications | ||||
| No. (%) | No. (%) | P value | No. (%) | No. (%) | P value | |
| LTr, n = 103 | HTr, n = 137 | LTr, n = 103 | HTr, n = 137 | |||
| PNF | 0 (0.0) | 5 (3.6) | 0.072 | 0 (0.0) | 0 | NA |
| Biliary fistula | 4 (3.9) | 10 (7.3) | 0.267 | 0 (0.0) | 1 (0.7) | NA |
| Biliary stenosis | 0 | 0 | NA | 15 (14.6) | 14 (10.2) | 0.307 |
| Hepatic arthery thrombosis | 2 (1.9) | 6 (4.4) | 0.478 | 0 (0.0) | 3 (2.2) | 0.261 |
| Portal vein thrombosis | 6 (5.1) | 16 (11.7) | 0.113 | 3 (2.9) | 6 (4.4) | 0.554 |
| Reoperation | 9 (8.7) | 36 (26.3) | < 0.001 | 4 (3.9) | 13 (9.5) | 0.298 |
| Retransplantation | 0 (0.0) | 3 (2.2) | 0.262 | 2 (1.9) | 4 (2.9) | 0.306 |
| 30 d mortality | 0 (0.0) | 9 (3.6) | 0.008 | NA | NA | NA |
| 10 yr mortality | NA | NA | NA | 8 (7.8) | 26 (19.0) | 0.137 |
Major cardiac complications were more frequent at 1, 5, and 10 years post-LT; major respiratory complications were more frequent at 5 and 10 years post-LT in the HTr than in the LTr. Dermatologic complications were less frequent up to 1 year in the HTr than in the LTr. Major infectious complications were more frequent, and rejections were less frequent in the HTr than in the LTr from 1 to 10 years post-LT. Minor neoplastic complications were more frequent at later points in follow-up in the HTr than in the LTr (Table 5).
Late LT-specific complications were observed after 30 d over 10 years of follow-up, as biliary stenosis (12.1%), HAT (1.2%), PVT (3.7%), reoperation (7.1%) and retransplantation (2.5%), none of these were related to perioperative transfusion (Table 6). Overall, 10-years mortality rate, with respect to RBC transfusion volume, was significantly higher (25.5% vs 7.8%, P < 0.001), respectively, in the HTr compared to the LTr (Table 6).
Simple and multiple Cox regression analysis identified perioperative RBC volume > 27.5 mL/kg and preoperative eGFR as independent risk factors for mortality over 10 years of follow-up after LT (Table 7).
| All patients n = 240 | ||||||
| Variables | Estimative | HR | 95%CI | P value | HR | P value |
| Univariate | Multivariate | |||||
| Male gender | -0.062 | 0.94 | 0.514-1.718 | 0.841 | ||
| Age (d) | -0.024 | 0.977 | 0.950-1.004 | 0.095 | ||
| Weight (kg) | -0.17 | 0.844 | 0.738-0.964 | 0.012 | ||
| Height (cm) | -0.044 | 0.957 | 0.924-0.990 | 0.013 | ||
| WAZ | -0.243 | 0.784 | 0.623-0.986 | 0.037 | ||
| HAZ | -0.085 | 0.918 | 0.734-1.148 | 0.455 | ||
| WHZ | -0.235 | 0.791 | 0.649-0.963 | 0.019 | ||
| BMIZ | -0.084 | 0.919 | 0.723-1.168 | 0.49 | ||
| PELD score | 0.022 | 1.022 | 0.982-1.064 | 0.282 | ||
| Biliary Atresia | -0.426 | 0.653 | 0.357-1.195 | 0.167 | ||
| Kasai surgery | -0.214 | 0.808 | 0.440-1.483 | 0.491 | ||
| Infections ≤ 30 d pre-LT | 0.348 | 1.416 | 1.023-1.960 | 0.036 | ||
| eGFR (mL/min/1.73 m2)1 | -0.005 | 0.995 | 0.991-0.999 | 0.010 | 0.995 | 0.023 |
| Surgical time (hours) | 0.012 | 1.013 | 0.856-1.197 | 0.884 | ||
| Hemoglobin (g/dL)2 | -0.206 | 0.814 | 0.657-1.008 | 0.059 | ||
| INR2 | 0.259 | 1.295 | 0.722-2.322 | 0.386 | ||
| Sodium (mEq/L)2 | -0.014 | 0.986 | 0.916-1.061 | 0.704 | ||
| Albumin (g/dL)2 | -0.116 | 0.89 | 0.615-1.290 | 0.539 | ||
| Lactate (mmoL/L)3 | -0.021 | 0.979 | 0.914-1.048 | 0.541 | ||
| GBWR (%) | 0.149 | 1.16 | 0.909-1.481 | 0.232 | ||
| RBC > 27.5 mL/kg | 1.316 | 3.73 | 1.730-8.042 | 0.001 | 3.031 | 0.009 |
| Presence of major complication | 0.384 | 1.469 | 0.799-2.701 | 0.261 |
The overall patient survival rates were 87.1%, 81.5%, and 80.3%, whereas the overall graft survival rates were 87.1%, 77.7%, and 75.6% at 1, 5, and 10 years post-LT, respectively. The graft survival rates were significantly lower in the MaC than in the MiC at 1, 5, and 10 years post-LT (81.5% vs 94.4%, 73.8% vs 84.6, and 72.2% vs 81%, respectively); however, no significant difference was seen in the patient survival rates between the MaC and the MiC. The patient survival rates were significantly lower in the HTr than in the LTr at 1, 5, and 10 years post-LT: 82.7% vs 97.7%, 73.9% vs 93.8%, and 72.6% vs 90.9%, respectively. Likewise, the graft survival rates were significantly lower in the HTr than in the LTr at 1, 5, and 10 years post-LT: 79.5% vs 97.7%, 67.2% vs 92.3%, and 67.2% vs 87%, respectively (Figure 3).
Determining predictive factors for complications of pediatric LT may be hindered by patient heterogeneity and a lack of standardization in the definition of complications. This study is the first retrospective study to assess short- and long-term transfusion-associated postoperative complications in a large number of small pediatric patients with chronic liver diseases who received the same type of graft from living donors.
The Clavien-Dindo classification[22] was first used by Clavien et al[23] to assess postoperative complications in adult LT patients and has been increasingly used in most pediatric surgical areas with some adaptations[24]. Beck-Schimmer et al[25] classified post-LT complications as minor and major providing the basis for the use of this modified classification primarily because general anesthesia was induced for almost all procedures in this pediatric population (e.g., imaging exams, biopsies, catheter insertions, and other minor invasive procedures).
We defined the interval from 24 h pre- to 48 h post-LT as the perioperative period. Over this period, patients had a greater need for transfusion. Our transfusion goals throughout this period were to keep Hb > 8 and < 10g/dL, INR < 3.5, platelet count > 45 × 103/mm3, and fibrinogen level > 80 mg/dL. Viscoelastic methods were unavailable at our center at this time. Only 16 study participants were not transfused during the perioperative period. Of the 224 transfused patients, 7.1%, 98.8%, and 37.5% received RBC before, during, and after surgery, respectively. Some patients remained within a suitable range during the intraoperative period yet this level dropped during the early postoperative period requiring subsequent transfusion. In this study, the average volume of transfusion of other BP was minimal compared to RBC.
Massive bleeding is usually defined as the loss of 100% or more of circulating TBV within 24 h[26]. Massive transfusion can also be defined as the transfusion of over 10% of TBV per minute or 50% in 3 h[27]. Nevertheless, TBV in pediatrics depends on the child’s age and weight ranging from 65 to 100 mL/kg. In our study, the child’s average age was 567 d (1.5 years) corresponding to a TBV of 75 mL/kg. The mean perioperative RBC volume transfused in the HTr was 57.7 mL/kg. A cutoff point of 27.5 mL/kg was used when the perioperative RBC volume represented less than 37% of TBV transfused within 96 h. Therefore, most of our patients did not meet the definition for massive bleeding or transfusion. Though there was no massive transfusion in the perioperative period in most patients; this lower volume has already been associated with major postoperative complications in PLDLT.
This study identified a perioperative transfusion volume of RBC > 27.5 mL/kg and preoperative eGFR as independent risk factors for mortality in PLDLT patients. A perioperative RBC transfusion volume higher than 27.5 mL/kg was a strong independent risk factor for mortality and increased the risk by 3.031-fold vs lower or equal volumes. This volume of RBC is definitely below that reported in other studies, which analyzed risk factors for survival in LT.
Matinlauri et al[28] identified transfusion of RBC > 20 units as a risk factor for graft survival post-LT in adults. Nacoti et al[14] evaluated the effect of transfusion on 1-year patient and graft survival in pediatric LT and estimated a mortality risk of 3.15 for ≥ 3 units of RBC. Preoperative eGFR was a weak risk factor for mortality in our study probably because malnourished children tend to have underestimated serum creatinine values, and the simplified revised formula [eGFR = 0.413 × Height (cm)/serum creatinine (mL/min/1.73 m2)] increases the error of the results at higher GFR values[29]. In the meantime, serum creatinine is known to be an independent risk factor for mortality in adult LT[30] and in pediatric LT with deceased donor[15].
Though LDLT is currently a standard treatment with good outcomes for young children with end-stage liver diseases, the postoperative complication rate can lead to a high morbimortality[31]. Among the 240 children, early postoperative complications were observed in 94.6% of patients of whom 54.6% had major complications associated with higher rates of graft loss. Although, the 1-year survival rate of 87.1 was slightly lower than in other centers that reported overall survival higher than 90%, the 5 and 10-year survival rates of 81.5% and 80.3%, respectively, are comparable to rates higher than 80%, reported by others[32-34]. This could be attributed to the fact that we studied exclusively small children, with inherent risks of early childhood, in comparison to other studies that include patients aged up to 18 years. In this study, the only risk factor for major postoperative complications after PLDLT was the volume of perioperative RBC transfused.
Transfusion was more frequently employed for younger and undernourished patients with extrahepatic cholestasis, previous Kasai procedure, increased rates of ascites, higher preoperative INR, lower Hb and sodium levels, and worse pulmonary and renal function. These findings are consistent with many reports on adult LT[35-37].
BP transfusion has often been reported to be associated with increased rates of both early and late LT complications[38,39]. Our sample consisted of 234 (97.5%) outpatients and 6 (2.5%) patients previously admitted to the ICU. During hospitalization, the total complication rates were similar between patients of the LTr and HTr groups (92.2% vs 96.4%). The HTr had more patients with severe complications (65.7% vs 39.8%), a higher average of complications per patient (3.8 ± 3.6 vs 2.5 ± 1.7), and a higher median number of major complications (IIIa vs IVa). Although the median grade of complications per patient was equal in the groups (II), there was a greater variability (I-V vs I-IIIb) in the HTr than in the LTr. Higher transfusion volumes were associated with longer anesthetic and surgery time, prolonged intubation, and longer ICU and in-hospital stays; these conclusions are corroborated by the findings of Massicotte et al[39] and Ramos et al[40] in adult LT patient studies.
Other specific complications might be related to perioperative BP transfusion in LT patients. Feltracco et al[41] reported that intraoperative BP transfusion was a risk factor for early postoperative pulmonary complications. Li et al[9] observed an increase in infectious complications during in-hospital and ICU stays among LDLT adults in the early postoperative period. Furthermore, Pereboom et al[12] reported a higher incidence and mortality associated with intraoperative platelet transfusion and acute lung injury related to transfusion. Benson et al[42] also reported similar findings with plasma containing BP and a higher incidence of early postoperative infections with dose-dependent RBC transfusion in adult LT.
During hospitalization occurred 30.8% of the total complications observed within the 10 years of follow-up. Minor metabolic complications (e.g., hydro electrolytic disorders, hypo- or hyper-glycemia, acidosis) were the most common. Nevertheless, no association between this type of complication and RBC transfusion volume was observed. Renal complications were not significantly different between groups, and dialysis was performed in seven patients during this period. HTr patients exhibited a higher frequency of major infectious complications (15.7% of complications, e.g., severe sepsis, with hemodynamic instability), general respiratory complications (11.5% of complications, e.g., pulmonary edema, pleural effusion, bronchospasm, pneumonia, and acute respiratory distress syndrome), general bleeding (2.8% of complications, e.g., oozing and draining with a need for reoperation), and major cardiovascular complications (2.1% of complications, e.g., hemodynamic instability requiring vasoactive drugs, severe arrhythmias, and cardiorespiratory arrest) than LTr patients. HTr patients had a lower frequency of rejections (6.3% of complications, e.g., mild acute cellular reaction) and dermatologic complications (1.2% of complications, e.g., oral ulceration and dermatitis.
Kloesel et al[19] did not observe significant differences in perioperative complications between the major and minor transfusion groups within the hospitalization period in pediatric LT patients despite an incidence rate of 43% for massive bleeding. In this last study, conflicting results might be attributed to the fact that all patients received an RBC transfusion and 88% of them received FFP transfusion thus creating a bias in the comparison between groups. Aside from increasing the risk of complications, RBC transfusion is a predictive factor for survival in adult[28] and pediatric LT[43]. In our study, patients with MaC presented reduced graft survival but patient survival was not affected relative to patients with no or MiC. Meanwhile, patients who underwent a HTr showed both worse graft and patient survival relative to patients of LTr.
The late period had 69.2% of the total complications with 55.3% up to the first year. Among the late postoperative complications of LT, infections are the leading cause of death[44]. In line with this, the frequency of major complications in HTr patients was higher at 1 up to 10 years post-LT. The most frequent major complications were infectious (15.8%-8.7% of complications, e.g., severe sepsis), pulmonary (5.0%-4.7% of complications, e.g., severe pneumonia requiring mechanical ventilation), and cardiovascular (2.0%-1.2% of complications, e.g., cardiorespiratory arrest). In the HTr patients, the frequency of minor neoplastic complications was significantly higher at 10 years (2.3% of complications, e.g., PTLD) than in LTr patients. The frequency of rejections was lower in the HTr at 1 to 10 years post-LT (8.0%-8.7% of complications, e.g., mild acute cellular reaction) than in the LTr. Renal complications were still not different between groups, and dialysis was necessary in 14 patients up to 10 years. Dermatological complications are common among LT patients and are related to genetics, allergic factors, and the side effects of immunosuppressive drugs. Surprisingly, patients with HTr had fewer dermatological complications than patients with LTr up to 1 year after LT (1.9%). This could be attributed to a lower frequency of rejections and, consequently, less of a need for immunosuppressive drugs. However, this would fail to explain why the rate of dermatological complications does not differ significantly afterward while rejections remained lower in HTr throughout the study. A higher-volume transfusion of RBC might have had some influence. Notwithstanding the fact that such complications are usually related to LT[45], there is no strong evidence of the association of perioperative BP transfusion and long-term outcomes in pediatric LT. We found a significant difference in 30 d and 10-year postoperative mortality rates between the LTr and the HTr (0 vs 6.6% and 7.8 vs 25.5%), respectively, confirming that HTr patients generally experienced more severe complications.
Concerning LT-specific complications, the incidence of PNF corresponded to 2.1% and was not related to transfusion. This is consistent with others who reported an incidence of 0.9%-8.5%[46]. Hypercoagulability is a risk factor for vascular thrombosis in LT, mainly in children, as determined by rebalanced hemostasis in cirrhosis, technical vascular issues, inflammatory response to trauma, and massive transfusion[47,48]. Incidences of HAT have been reported to be 4%-8% and PVT of 5%-10%[49-51]. In our study, the overall incidence of HAT and PVT was 4.6% and 13.3%, respectively. Nevertheless, no relation between transfusion volume and an increase in arterial or venous thrombosis were observed, in both, short- and long-term periods. The lower incidence of HAT is likely related to the microsurgical anastomosis technique whereas the higher incidence of PVT may be attributed to previous portal hypoplasia frequently observed in patients with biliary atresia-this was the most prevalent underlying disease in our cohort. Portal vein graft interposition was employed in 37 (15.4%) patients of the total cohort, and only three cases evolved with PVT. Biliary complications accounted for 18.3% of the total cases, and neither fistulas nor stenosis were related to RBC transfusion. The incidence rate of biliary complications in PLDLT has been reported to be 10%-20%[52], depending on the size of the graft and subsequent technical difficulties. Reoperations corresponded to 25.8%, which is consistent with others who reported an incidence of 8%-29%[33] in PLDLT. In the short-term period, reoperation (18.7%) was three-fold higher in the patients who received an RBC volume higher than 27.5 mL/kg (HTr), due mostly to bleeding and intestinal injuries. In the long-term period, reoperations were not related to perioperative transfusion. Retransplantation corresponded to 3.8% and was not related to RBC transfusion. The incidence was below the historical average of 9%-29%[53], probably because of the lower incidence of total hip arthroplasty and the good quality of the grafts. Although the HTr had fewer minor rejection episodes, such as a mild acute cellular reaction over 10 years, this fact did not impact the retransplantation rate in both, short- and long-term periods.
Immunosuppression associated with blood transfusion occurs via a decrease in the number and function of natural killer cells, a decrease in cytotoxic T-cell function, an increase in the number of suppressor T-cells, and a reduction in macrophage and monocyte function[54]. Blood transfusion may induce immunomodulatory effects (both proinflammatory and immunosuppressive) that are of variable intensity and long-term duration. These antagonistic effects are associated with a decrease in rejection episodes[55] as well as an increase in the frequency of infection[56], neoplasia[57], and tumor recurrence[8]. We essentially found that HTr patients displayed more major infections and fewer rejections during early and late postoperative periods and more minor neoplastic complications in the late postoperative period than LTr patients.
Detailing the type, severity, and chronology of postoperative complications is of paramount importance for a better understanding of the clinical evolution. It can assist in the implementation of preventive measures that may positively impact the outcome of PLDLT.
Several strategies have been adopted to decrease perioperative transfusion in adult LT patients. They can be classified into three groups of measures: (1) Prophylactic such as the recognition of patients at risk for bleeding and the previous suspension of drugs that interfere with coagulation; (2) Technical such as maintenance of low central venous pressure, controlled hypotension, use of vascular clamping, ultrasonic or argon scalpels, and capture and reuse of blood lost; guided fluid therapy by multiparametric data, reduction of transfusion trigger values, and viscoelastic tests; and (3) Pharmacological such as erythropoietin, desmopressin, vasopressin, antifibrinolytics, prothrombin complex, lyophilized fibrinogen, recombinant factor VIIa, fibrin sealants, and vasoactive drugs[58,59]. Certainly, not all of them apply to this population, that remain to be a challenge in conducting LT. Fluid management in small children undergoing LT cannot be guided by minimally invasive multiparametric monitors. These are of limited use, once their softwares are designed for adult patients. Nonetheless, the analysis of the trend curves can assist in decision-making, there is a lack of accuracy in the assessment of volemia, hemodynamic state and effect of vasoactive drugs during the perioperative period of pediatric LT. Besides, techniques as hemodilution and controlled hypotension are not validated in this group. Hemodilution increases hydrostatic pressure in the portal vein and inferior vena cava system and worsens the coagulopathy, exacerbating surgical bleeding. Controlled hypotension is a debatable issue and might be of potential risk for target organ damage. It is crucial to recognize that small children with chronic liver disease have a tenuous rebalance of the hemostatic system, not entirely understood, which might be easily disrupted by hasted interventions, pushing the patient towards hemorrhage and/or thrombosis. Prophylactic use of FFP is not advised, because it can increase intravascular pressure and increase RBC transfusion. Routine prophilatic use of antifibrinolytic drugs is no longer recommended, tranexamic acid and aminocaproic acid are possibly useful for patients in hyperfibrinolysis, demonstrated by microvascular oozing or viscoelastic tests. Prophylactic use of recombinant factor VIIa, should be avoided in all, except for highest-risk procedures[60]. Although, preoperative blood transfusion has been demonstraded to be independently associated to morbidity up to 30 d of postoperative period and harmful in neonates undergoing general pediatric surgery, neurosurgery, otolaringology, cardiothoracic, plastics and urology surgery[61], no strong evidence is found in pediatric LT in the long-term period. Concurrent transfusion of “red” and “yellow” BP, in adult liver resection with compromised function, was associated with a significantly higher risk of postoperative morbidity compared to only RBC or only FFP transfusion, what might be attributed to synergistic effects[2]. Though, no similar study was conducted in pediatric LT. If there is an absence of universal definition of massive bleeding or massive transfusion and a scarcity of studies relating survival to specifc BP dosages, ratios, timing and guidance even in adult trauma victims[62], let alone pediatric LT in small children. Specific transfusion trigger thresholds in pediatric LT have not been validated and need to be determined by prospective controlled studies that seek to standardize patient samples, according to age or weight, underlying diseases, type of donor and type of graft.
This study does have some limitations. First, this was a retrospective study performed in a single center. Second, the collection of data was refined on an ongoing basis since the implementation of the LT program; the learning curve may have influenced the results. Third, and most importantly, complications due to increased transfusion volume may be an epiphenomenon related to a sicker patient and of higher technical difficulty, or, indeed, a risk factor for postoperative morbimortality. Nonetheless, this study has several strengths, such as the size and homogeneity of the sample as well as the standardization of the anesthetic/surgical approaches and the immunosuppression regimen. The follow-up was conducted in the same center, which included facilities for patients and their families to remain close during local treatment thus improving patient recruitment and reducing loss to follow-up throughout the study period.
In this study, blood transfusion volumes less than one total blood volume, though not considered massive transfusions, were already associated with a higher incidence of more serious complications and mortality as assessed by hospitalization up to 10 years after PLDLT. A perioperative RBC transfusion volume higher than 27.5 mL/kg is associated with not only increased rates of infectious, cardiovascular, respiratory, and neoplastic complications but also decreased frequency of rejection episodes. Furthermore, a perioperative volume of RBC transfusion higher than 27.5 mL/kg is an independent risk factor for mortality and is directly related to reduced patient and graft survival in PLDLT. These results underscore the need for more restrictive criteria to guide the use of blood transfusion in PLDLT patients to prevent potentially related postoperative complications.
Appropriate protocols should be tailored to each center according to the infrastructure, clinical staff experience, and patient’s profile. Indeed, some strategies to reduce blood consumption should be implemented. An accurate nutritional assessment with specific dietary support and early supplementation is mandatory. Treatment with iron and vitamins should be considered. Prophylaxis of digestive bleeding and treatment of renal dysfunction and infection can decrease the incidence of preoperative anemia. The use of recombinant human erythropoietin therapy is controversial. Reduce blood tests and perform microsampling. During surgery, a more restrictive fluid management and a reduction of Hb trigger values to less than 8.0 g/dL, could reduce blood transfusion especially when combined with low doses of continuous infusion of norepinephrine. This could mitigate fluid overload, reduce portal hypertension, restore splanchnic and central circulatory imbalances and optimize tissue oxygenation. Assessment of coagulation with viscoelastic tests to improve blood management in pediatric surgery is feasible, but specific algorithms must be developed. The goals are to optimize the erythrocyte mass, minimize blood loss, increase tolerance to anemia and maintain hemostatic balance. As demonstrated, a small reduction in perioperative RBC transfusion volume may determine a better outcome in the short- and long-term postoperative periods. The evaluation of risk, effectiveness, and cost-benefit assessment of these strategies in young children with liver diseases is outside the scope of the present study and should be carried out in future research.
Pediatric living donor liver transplantation (PLDLT) is a multidisciplinary procedure of high complexity and potential risk of bleeding. The association between transfusion and short- and long-term postoperative complications is poorly established especially in small children. Blood transfusion is frequently indicated in the perioperative period of liver transplant, though there is little robust evidence of associated postoperative complications. Given the good survival results, in the past decade, it is now necessary to identify risk factors for complications in order to improve the long-term evolution.
To study in depth the short- and long-term evolution of this specific group of highly fragile pediatric patients, in order to improve the proficiency acquired in 20 years of working with PLDLT, and to be able to share knowledge.
This study assessed whether perioperative transfusion is associated with early and late postoperative complications and mortality in small patients undergoing PLDLT.
Postoperative complications along 10 years of follow up were graduated with Clavien-Dindo modified classification in order to assess relationship between blood transfusion and postoperative complications. Multiple logistic regression analysis identified risk factors for major postoperative complications. Perioperative red blood cells volume was identified as a single risk factor and a receiver operating characteristic curve identified a cutoff point of 27.5 mL/kg. Cox regression analyses identified independent risk factors for mortality. Overall patient and graft survival analyses was performed using Kaplan–Meier survival curves, which were compared using the log-rank test and a P < 0.05 was considered statistically significant.
In terms of red blood cells (RBC) transfusion volume, there was a significantly higher rate of 30 d reoperation (26.3% × 8.7%, P < 0.001) and 30 d mortality rate (6.6% × 0.0%, P < 0.001) in the high-volume transfusion (HTr) vs low-volume transfusion (LTr), respectively. Early liver transplantation (LT)-specific complications include primary non-function, biliary complications, vascular thrombosis, and retransplantation that were not related to a higher perioperative transfusion volume. Over 10 years of follow-up, with respect to RBC transfusion volume, there was a significantly higher rate of reoperation (36.5% × 12.6%, P < 0.001) and mortality (25.5% × 7.8%, P < 0.001), respectively, in the HTr compared to the LTr. Perioperative RBC volume > 27.5 mL/kg and preoperative estimated glomerular filtration rate were identified as independent risk factors for mortality over 10 years of follow-up after LT. The patient survival rates were significantly lower in the HTr than in the LTr at 1, 5, and 10 years post-LT: 82.7% vs 97.7%, 73.9% vs 93.8%, and 72.6% vs 90.9%, respectively. Likewise, the graft survival rates were significantly lower in the HTr than in the LTr at 1, 5, and 10 years post-LT: 79.5% vs 97.7%, 67.2% vs 92.3%, and 67.2% vs 87%, respectively.
A perioperative RBC transfusion volume > 27.5 mL/kg is associated with not only increased rates of infectious, cardiovascular, respiratory, and neoplastic complications but also decreased frequency of rejection episodes. Furthermore, a perioperative volume of RBC transfusion higher than 27.5 mL is an independent risk factor for mortality, and is directly related to reduced patient and graft survival in PLDLT.
The detailed analysis of this study allows the construction of strategy protocols to reduce the need for transfusion of patients undergoing PLDLT improving short- and long-term outcome.
The authors would like to thank Dr. Vinicius Fernando Calsavara, statistical researcher at the International Research Center of AC Camargo Cancer Center, professor at the postgraduation course of Antonio Prudente Foundation and member of the Research Ethics Committee of AC Camargo Cancer Center for performing the statistical analysis and providing vital technical support.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: El Kassas M, Kutluturk K, Xu X S-Editor: Fan JR L-Editor: A P-Editor: Wang LL
| 1. | Schiergens TS, Rentsch M, Kasparek MS, Frenes K, Jauch KW, Thasler WE. Impact of perioperative allogeneic red blood cell transfusion on recurrence and overall survival after resection of colorectal liver metastases. Dis Colon Rectum. 2015;58:74-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 97] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 2. | Lu Q, Zhang J, Gao WM, Lv Y, Zhang XF, Liu XM. Intraoperative Blood Transfusion and Postoperative Morbidity Following Liver Resection. Med Sci Monit. 2018;24:8469-8480. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Bhaskar B, Dulhunty J, Mullany DV, Fraser JF. Impact of blood product transfusion on short and long-term survival after cardiac surgery: more evidence. Ann Thorac Surg. 2012;94:460-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 130] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 4. | Glance LG, Dick AW, Mukamel DB, Fleming FJ, Zollo RA, Wissler R, Salloum R, Meredith UW, Osler TM. Association between intraoperative blood transfusion and mortality and morbidity in patients undergoing noncardiac surgery. Anesthesiology. 2011;114:283-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 375] [Cited by in RCA: 411] [Article Influence: 29.4] [Reference Citation Analysis (0)] |
| 5. | de Boer MT, Christensen MC, Asmussen M, van der Hilst CS, Hendriks HG, Slooff MJ, Porte RJ. The impact of intraoperative transfusion of platelets and red blood cells on survival after liver transplantation. Anesth Analg. 2008;106:32-44, table of contents. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 237] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 6. | Rana A, Petrowsky H, Hong JC, Agopian VG, Kaldas FM, Farmer D, Yersiz H, Hiatt JR, Busuttil RW. Blood transfusion requirement during liver transplantation is an important risk factor for mortality. J Am Coll Surg. 2013;216:902-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 7. | Boyd SD, Stenard F, Lee DK, Goodnough LT, Esquivel CO, Fontaine MJ. Alloimmunization to red blood cell antigens affects clinical outcomes in liver transplant patients. Liver Transpl. 2007;13:1654-1661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 51] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Cata JP, Wang H, Gottumukkala V, Reuben J, Sessler DI. Inflammatory response, immunosuppression, and cancer recurrence after perioperative blood transfusions. Br J Anaesth. 2013;110:690-701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 291] [Cited by in RCA: 336] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 9. | Li C, Mi K, Wen TF, Yan LN, Li B, Wei YG, Yang JY, Xu MQ, Wang WT. Risk factors and outcomes of massive red blood cell transfusion following living donor liver transplantation. J Dig Dis. 2012;13:161-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | de Morais BS, Sanches MD, Ribeiro DD, Lima AS, de Abreu Ferrari TC, Duarte MM, Cançado GH. [Association between the use of blood components and the five-year mortality after liver transplant]. Rev Bras Anestesiol. 2011;61:286-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | López Santamaría M, Gámez M, Murcia J, Díez Pardo JA, Leal N, Frauca E, Camarena C, Hierro L, de la Vega A, Díaz MC, Jara P, Tovar J. [Prognostic factors in pediatric liver transplantation. Multivariate analysis]. Cir Pediatr. 2003;16:175-180. [PubMed] |
| 12. | Pereboom IT, de Boer MT, Haagsma EB, Hendriks HG, Lisman T, Porte RJ. Platelet transfusion during liver transplantation is associated with increased postoperative mortality due to acute lung injury. Anesth Analg. 2009;108:1083-1091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 156] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 13. | Lopez-Plaza I. Transfusion guidelines and liver transplantation: time for consensus. Liver Transpl. 2007;13:1630-1632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Nacoti M, Cazzaniga S, Lorusso F, Naldi L, Brambillasca P, Benigni A, Corno V, Colledan M, Bonanomi E, Vedovati S, Buoro S, Falanga A, Lussana F, Barbui T, Sonzogni V. The impact of perioperative transfusion of blood products on survival after pediatric liver transplantation. Pediatr Transplant. 2012;16:357-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 15. | Nacoti M, Cazzaniga S, Colombo G, Corbella D, Fazzi F, Fochi O, Gattoni C, Zambelli M, Colledan M, Bonanomi E. Postoperative complications in cirrhotic pediatric deceased donor liver transplantation: Focus on transfusion therapy. Pediatr Transplant. 2017;21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Fanna M, Baptiste A, Capito C, Ortego R, Pacifico R, Lesage F, Moulin F, Debray D, Sissaoui S, Girard M, Lacaille F, Telion C, Elie C, Aigrain Y, Chardot C. Preoperative risk factors for intra-operative bleeding in pediatric liver transplantation. Pediatr Transplant. 2016;20:1065-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Jin SJ, Kim SK, Choi SS, Kang KN, Rhyu CJ, Hwang S, Lee SG, Namgoong JM, Kim YK. Risk factors for intraoperative massive transfusion in pediatric liver transplantation: a multivariate analysis. Int J Med Sci. 2017;14:173-180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Huang CJ, Cheng KW, Chen CL, Wu SC, Shih TH, Yang SC, Jawan B, Wang CH. Predictive factors for pediatric patients requiring massive blood transfusion during living donor liver transplantation. Ann Transplant. 2013;18:443-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Kloesel B, Kovatsis PG, Faraoni D, Young V, Kim HB, Vakili K, Goobie SM. Incidence and predictors of massive bleeding in children undergoing liver transplantation: A single-center retrospective analysis. Paediatr Anaesth. 2017;27:718-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Otte M, Andree C, Hagouan M, Richrath P, Abu-Ghazaleh A, Munder B. [The DIEP Flap as Method of Choice in Breast Reconstruction - Results and Protocol for Succesful Reconstruction]. Handchir Mikrochir Plast Chir. 2015;47:222-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Squires RH, Ng V, Romero R, Ekong U, Hardikar W, Emre S, Mazariegos GV. Evaluation of the pediatric patient for liver transplantation: 2014 practice guideline by the American Association for the Study of Liver Diseases, American Society of Transplantation and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. Hepatology. 2014;60:362-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 144] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 22. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18532] [Cited by in RCA: 24849] [Article Influence: 1183.3] [Reference Citation Analysis (0)] |
| 23. | Clavien PA, Camargo CA Jr, Croxford R, Langer B, Levy GA, Greig PD. Definition and classification of negative outcomes in solid organ transplantation. Application in liver transplantation. Ann Surg. 1994;220:109-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 280] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 24. | Sethi MV, Zimmer J, Ure B, Lacher M. Prospective assessment of complications on a daily basis is essential to determine morbidity and mortality in routine pediatric surgery. J Pediatr Surg. 2016;51:630-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Beck-Schimmer B, Bonvini JM, Schadde E, Dutkowski P, Oberkofler CE, Lesurtel M, DeOliveira ML, Figueira ER, Rocha Filho JA, Auler JO Jr, D'Albuquerque LA, Reyntjens K, Wouters P, Rogiers X, Debaerdemaeker L, Ganter MT, Weber A, Puhan MA, Clavien PA, Breitenstein S. Conditioning With Sevoflurane in Liver Transplantation: Results of a Multicenter Randomized Controlled Trial. Transplantation. 2015;99:1606-1612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 26. | Stainsby D, MacLennan S, Hamilton PJ. Management of massive blood loss: a template guideline. Br J Anaesth. 2000;85:487-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 131] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 27. | Diab YA, Wong EC, Luban NL. Massive transfusion in children and neonates. Br J Haematol. 2013;161:15-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 74] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 28. | Matinlauri IH, Nurminen MM, Höckerstedt KA, Isoniemi HM. Risk factors predicting survival of liver transplantation. Transplant Proc. 2005;37:1155-1160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 29. | Zachwieja K, Korohoda P, Kwinta-Rybicka J, Miklaszewska M, Moczulska A, Bugajska J, Berska J, Drożdż D, Pietrzyk JA. Which equations should and which should not be employed in calculating eGFR in children? Adv Med Sci. 2015;60:31-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 30. | Jo YY, Choi YS, Joo DJ, Yoo YC, Nam SG, Koh SO. Pretransplant mortality predictors in living and deceased donor liver transplantation. J Chin Med Assoc. 2014;77:16-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 31. | Farmer DG, Venick RS, McDiarmid SV, Ghobrial RM, Gordon SA, Yersiz H, Hong J, Candell L, Cholakians A, Wozniak L, Martin M, Vargas J, Ament M, Hiatt J, Busuttil RW. Predictors of outcomes after pediatric liver transplantation: an analysis of more than 800 cases performed at a single institution. J Am Coll Surg. 2007;204:904-14; discussion 914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 63] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 32. | Kim JJ, Marks SD. Long-term outcomes of children after solid organ transplantation. Clinics (Sao Paulo). 2014;69 Suppl 1:28-38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 33. | Yazigi NA. Long term outcomes after pediatric liver transplantation. Pediatr Gastroenterol Hepatol Nutr. 2013;16:207-218. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 34. | Cuenca AG, Kim HB, Vakili K. Pediatric liver transplantation. Semin Pediatr Surg. 2017;26:217-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 80] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 35. | Massicotte L, Denault AY, Beaulieu D, Thibeault L, Hevesi Z, Nozza A, Lapointe R, Roy A. Transfusion rate for 500 consecutive liver transplantations: experience of one liver transplantation center. Transplantation. 2012;93:1276-1281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 97] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 36. | Makroo RN, Walia RS, Aneja S, Bhatia A, Chowdhry M. Preoperative predictors of blood component transfusion in living donor liver transplantation. Asian J Transfus Sci. 2013;7:140-146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 37. | De Santis GC, Brunetta DM, Nardo M, Oliveira LC, Souza FF, Cagnolati D, Mente ÊD, Sankarankutty AK, Covas DT, de Castro e Silva O. Preoperative variables associated with transfusion requirements in orthotopic liver transplantation. Transfus Apher Sci. 2014;50:99-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 38. | Boin IF, Leonardi MI, Luzo AC, Cardoso AR, Caruy CA, Leonardi LS. Intraoperative massive transfusion decreases survival after liver transplantation. Transplant Proc. 2008;40:789-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 61] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 39. | Massicotte L, Sassine MP, Lenis S, Seal RF, Roy A. Survival rate changes with transfusion of blood products during liver transplantation. Can J Anaesth. 2005;52:148-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 122] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 40. | Ramos E, Dalmau A, Sabate A, Lama C, Llado L, Figueras J, Jaurrieta E. Intraoperative red blood cell transfusion in liver transplantation: influence on patient outcome, prediction of requirements, and measures to reduce them. Liver Transpl. 2003;9:1320-1327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 199] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 41. | Feltracco P, Carollo C, Barbieri S, Pettenuzzo T, Ori C. Early respiratory complications after liver transplantation. World J Gastroenterol. 2013;19:9271-9281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 80] [Cited by in RCA: 94] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 42. | Benson AB, Burton JR Jr, Austin GL, Biggins SW, Zimmerman MA, Kam I, Mandell S, Silliman CC, Rosen H, Moss M. Differential effects of plasma and red blood cell transfusions on acute lung injury and infection risk following liver transplantation. Liver Transpl. 2011;17:149-158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 100] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 43. | Barcelona SL, Thompson AA, Coté CJ. Intraoperative pediatric blood transfusion therapy: a review of common issues. Part II: transfusion therapy, special considerations, and reduction of allogenic blood transfusions. Paediatr Anaesth. 2005;15:814-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 44] [Article Influence: 2.2] [Reference Citation Analysis (1)] |
| 44. | Fonseca-Aten M, Michaels MG. Infections in pediatric solid organ transplant recipients. Semin Pediatr Surg. 2006;15:153-161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 30] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 45. | Gallegos-Orozco JF, Charlton MR. Predictors of Cardiovascular Events After Liver Transplantation. Clin Liver Dis. 2017;21:367-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 46. | Chen XB, Xu MQ. Primary graft dysfunction after liver transplantation. Hepatobiliary Pancreat Dis Int. 2014;13:125-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 93] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 47. | Clevenger B, Mallett SV. Transfusion and coagulation management in liver transplantation. World J Gastroenterol. 2014;20:6146-6158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 124] [Cited by in RCA: 124] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 48. | De Pietri L, Montalti R, Nicolini D, Troisi RI, Moccheggiani F, Vivarelli M. Perioperative thromboprophylaxis in liver transplant patients. World J Gastroenterol. 2018;24:2931-2948. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 39] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 49. | Spada M, Riva S, Maggiore G, Cintorino D, Gridelli B. Pediatric liver transplantation. World J Gastroenterol. 2009;15:648-674. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 125] [Cited by in RCA: 121] [Article Influence: 7.6] [Reference Citation Analysis (2)] |
| 50. | Nacoti M, Corbella D, Fazzi F, Rapido F, Bonanomi E. Coagulopathy and transfusion therapy in pediatric liver transplantation. World J Gastroenterol. 2016;22:2005-2023. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 29] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 51. | Kohli R, Cortes M, Heaton ND, Dhawan A. Liver transplantation in children: state of the art and future perspectives. Arch Dis Child. 2018;103:192-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 52. | Rawal N, Yazigi N. Pediatric Liver Transplantation. Pediatr Clin North Am. 2017;64:677-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 67] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 53. | Dreyzin A, Lunz J, Venkat V, Martin L, Bond GJ, Soltys KA, Sindhi R, Mazariegos GV. Long-term outcomes and predictors in pediatric liver retransplantation. Pediatr Transplant. 2015;19:866-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 54. | de Boer MT, Molenaar IQ, Porte RJ. Impact of blood loss on outcome after liver resection. Dig Surg. 2007;24:259-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 111] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 55. | Ghosh PK, Kochhar P, Kochhar RS. Effect of Blood Transfusion on Subsequent Organ Transplantation. Blood Transfusion in Clinical Practice. InTech, 2012: 245-254. [DOI] [Full Text] |
| 56. | Freire MP, Soares Oshiro IC, Bonazzi PR, Guimarães T, Ramos Figueira ER, Bacchella T, Costa SF, Carneiro D'Albuquerque LA, Abdala E. Surgical site infections in liver transplant recipients in the model for end-stage liver disease era: an analysis of the epidemiology, risk factors, and outcomes. Liver Transpl. 2013;19:1011-1019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 57. | Muszynski JA, Spinella PC, Cholette JM, Acker JP, Hall MW, Juffermans NP, Kelly DP, Blumberg N, Nicol K, Liedel J, Doctor A, Remy KE, Tucci M, Lacroix J, Norris PJ; Pediatric Critical Care Blood Research Network (Blood Net). Transfusion-related immunomodulation: review of the literature and implications for pediatric critical illness. Transfusion. 2017;57:195-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 102] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 58. | Trzebicki J, Flakiewicz E, Kosieradzki M, Blaszczyk B, Kołacz M, Jureczko L, Pacholczyk M, Chmura A, Lagiewska B, Lisik W, Wasiak D, Kosson D, Kwiatkowski A, Lazowski T. The use of thromboelastometry in the assessment of hemostasis during orthotopic liver transplantation reduces the demand for blood products. Ann Transplant. 2010;15:19-24. [PubMed] |
| 59. | Gurusamy KS, Pissanou T, Pikhart H, Vaughan J, Burroughs AK, Davidson BR. Methods to decrease blood loss and transfusion requirements for liver transplantation. Cochrane Database Syst Rev. 2011: CD009052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 60. | Raffini L, Witmer C. Pediatric transplantation: managing bleeding. J Thromb Haemost. 2015;13 Suppl 1:S362-S369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 61. | Dukleska K, Vinocur CD, Brenn BR, Lim DJ, Keith SW, Dirnberger DR, Berman L. Preoperative Blood Transfusions and Morbidity in Neonates Undergoing Surgery. Pediatrics. 2020;146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 62. | Abuzeid AM, O'Keeffe T. Review of massive transfusion protocols in the injured, bleeding patient. Curr Opin Crit Care. 2019;25:661-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |