Published online Dec 21, 2020. doi: 10.3748/wjg.v26.i47.7568
Peer-review started: September 15, 2020
First decision: November 3, 2020
Revised: November 16, 2020
Accepted: November 29, 2020
Article in press: November 29, 2020
Published online: December 21, 2020
Processing time: 94 Days and 16.9 Hours
Colonoscopy attendance is a key quality parameter in colorectal cancer population screening programmes. Within these programmes, educative interventions with bidirectional contact carried out by trained personnel have been proved to be an important tool for colonoscopy attendance improvement, and because of its huge clinical and economic impact, they have been widely implemented. However, outside of this population programmes, educative measures to improve colonoscopy attendance have been poorly studied and no navigation interventions are usually performed.
To investigate the clinical and economic impacts of an educational telephone intervention on colonoscopy attendance outside colorectal cancer screening programmes.
This randomized controlled trial included consecutive patients referred to colonoscopy from primary care centres from November 2017 to May 2018. The intervention group (IG) received a telephone intervention, while the control group (CG) did not. Patients assigned to the IG received an educational telephone call 7 d before the colonoscopy appointment. The intervention was carried out by two nurses with deep endoscopic knowledge who were previously trained for a telephone educational intervention for colonoscopy. The impact on patient compliance with preparedness protocols related to bowel cleansing, anti-thrombotic management, and sedation scheduling was also evaluated. A second call was conducted to assess patient satisfaction. Intention-to-treat (ITT) and per-protocol (PP) analyses were performed.
A total of 738 and 746 patients were finally included in the IG and CG respectively. Six hundred thirteen (83%) patients were contacted in the IG. The non-attendance rate was lower in the IG, both in the ITT analysis (IG 8.4% vs CG 14.3%, P < 0.001) and in the PP analysis (4.4% vs 14.3%, P < 0.001). In a multivariable analysis, belonging to the control group increased the risk of non-attendance in both, the ITT analysis (OR 1.81, 95%CI: 1.27 to 2.58, P = 0.001) and the PP analysis (OR 3.56, 95%CI: 2.25 to 5.64, P < 0.001). There was also a significant difference in compliance with preparedness protocols [bowel cleansing: IG 61.7% vs CG 52.6% (P = 0.001), antithrombotic management: IG 92.5% vs CG 62.8% (P = 0.001), and sedation scheduling: IG 78.8% vs CG 0% (P ≤ 0.001)]. We observed a net benefit of €55600/year after the intervention. The information given before the procedure was rated as excellent by 26% (CG) and 51% (IG) of patients, P ≤ 0.001.
Educational telephone nurse intervention improves attendance, protocol compliance and patient satisfaction in the non-screening colonoscopy setting and has a large economic impact, which supports its imple-mentation and maintenance over time.
Core Tip: This is the first randomized controlled trial that demonstrates that an educational intervention improves colonoscopy attendance in the non-screening colonoscopy setting. We found that bidirectional communication is the crucial point in reducing the non-attendance rate and telephone contact is a valid educational option. An endoscopy nurse is also a valid person to conduct the educational intervention and could be the ideal person to eliminate barriers that negatively influence the patient’s attendance. This educational intervention also improves protocol compliance and patient satisfaction and has a large economic impact, which supports its imple-mentation and maintenance over time.
- Citation: Seoane A, Font X, Pérez JC, Pérez R, Enriquez CF, Parrilla M, Riu F, Dedeu JM, Barranco LE, Duran X, Ibáñez IA, Álvarez MA. Evaluation of an educational telephone intervention strategy to improve non-screening colonoscopy attendance: A randomized controlled trial. World J Gastroenterol 2020; 26(47): 7568-7583
- URL: https://www.wjgnet.com/1007-9327/full/v26/i47/7568.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i47.7568
The substantial advance in colonoscopy quality in recent years has been achieved at the expense of population screening colonoscopy programmes, launched due to their very large clinical and economic impact on the decrease in colorectal cancer mortality. At the European level, these programmes have drawn on multiple performance measures, subsequently used to improve non-screening colonoscopy quality[1].
Colonoscopy appointment attendance is a key quality parameter in screening programmes, and different improvement strategies have been developed using educational material (mainly web-based approaches and mailed print communication) and administrative reminder systems[2-6]. Another approach is patient navigation throughout the screening process. This intervention allows bidirectional contact to help address common barriers to attending colonoscopy by eliminating misconceptions, changing negative attitudes and helping patients gain control over factors that concern them with regard to their ability to comply with preparedness protocols[7,8]. This patient navigation strategy in screening programmes has also been reported to be cost-effective and to have a positive influence on patient satisfaction[9-11].
However, little effort has been made to improve colonoscopy attendance outside screening programmes in daily clinical practice, and educational measures are not usually performed. There are also very few published studies on educational measures aimed at increasing attendance. Some studies have identified several factors related to the no-show rate of endoscopic procedures in general, but specific information on the attendance rate[12-16] in the context of non-screening colonoscopy is not well known. Non-educational reminder systems have been shown to result in little improvement in colonoscopy attendance[17-19]. Nevertheless, an educational telephone nurse intervention has been shown to have better efficacy in reducing the no-show rate, and the intervention was also cost-effective[20].
Effective educational patient interventions have also been applied in other endoscopy quality areas, such as patient compliance with achieving complete examinations[21] and bowel cleansing for improving adequacy, a successful strategy to improve the adenoma detection rate[22-24]. All these data suggest the suitability of implementing educational patient interventions in endoscopy units to improve non-screening colonoscopy quality.
We designed a randomized controlled trial (RCT) to conduct an educational telephone nurse intervention with bidirectional contact directed to increase colonoscopy attendance, similar to the patient navigation carried out in the population screening setting. Second, we assessed the economic impact and the potential benefit of the intervention in regard to compliance with patient preparedness protocols, cleansing adequacy, and patient satisfaction.
This is a prospective, RCT designed to assess the impact of an educational telephone intervention performed by digestive endoscopy nurses on colonoscopy attendance outside colorectal cancer screening programmes. This study was conducted in a tertiary centre at Hospital del Mar of Barcelona. The study was approved by the ethics committee of our centre (7739/I) in accordance with the Declaration of Helsinki, and the trial was registered at ClinicalTrials.gov (ID: NCT03458377).
All consecutive outpatients referred for colonoscopy from November 2017 to May 2018 from the primary care centres in our health area were included. The exclusion criteria were unwillingness to participate, inability to obtain the signed informed consent form, hospital admission during the study period, simultaneous participation in another clinical trial and/or impossibility to carry out the educational intervention (colonoscopy cancellation or not having a telephone). Patients routinely excluded in endoscopic studies for presenting pathologies that condition the colon preparation regimen or the sedation plan (history of subtotal colectomy, active inflammatory bowel disease, or high comorbidity), were not excluded in our study according to the main objective of evaluating the attendance rate.
An intervention group (IG) and a control group (CG) were designed. We performed a prerandomization method (Zelen’s method) with a complete-double-consent-design to eliminate selection bias created by contact with the patient prior to randomization in a study where assessing the applicability of contact is crucial, and to avoid the risk of non-participation and drop out of the study, given the attractiveness of the designed intervention.
Patients were randomized to the CG and the IG 10 d before the colonoscopy appointment using a computer-generated randomization list with a 1:1 allocation rate. In the IG, verbal consent was obtained in all patients after receiving a detailed explanation of the nature, aims, and consequences of the study, coinciding with the telephone call for intervention 7 d before the colonoscopy appointment. We obtained the signed informed consent form for both groups on the day of the colonoscopy. For those who did not attend the colonoscopy appointment, the signed informed consent form was obtained after later contact.
Patient preparedness protocols included bowel cleansing, antithrombotic management and sedation scheduling. We recommended a low fibre diet 48 h before the colonoscopy and laxative intake in a split dose regimen, with an interval of less than 4 h between the last laxative dose and the colonoscopy, according to the European Society of Gastrointestinal Endoscopy (ESGE) Guidelines[25]. In the case of antithrombotic drug intake, we followed the withdrawal ESGE guideline algorithm[26]. Sedation was administered by an anaesthesiologist if the patient had a high comorbidity burden; otherwise, a nurse directed by a gastroenterologist administered the sedation[27]. A high comorbidity burden was defined in cases of serious COPD, tracheostomy, severe ventricular function, Mobitz II-III atrioventricular block, implantable cardioverter defibrillator, severe mitral or aortic valvular stenosis, severe sleep apnoea or body mass index > 40, which were verified by the nurse after reviewing medical history and interviewing the patient.
All of the patients received information about patient preparedness protocols for colonoscopy in the primary care centres at the time of the colonoscopy referral. Additionally, the patients received a certified letter including the appointment time and a copy of bowel cleansing instructions.
Patients assigned to the IG received an educational telephone call 7 d before the colonoscopy appointment. The intervention was carried out by two nurses with deep endoscopic knowledge who were previously trained for a telephone educational intervention for colonoscopy[22,28,29] and instructed to evaluate the need for anaesthesia.
Special emphasis was placed on the attempt to eliminate socioeconomic, psychological and clinical barriers that could affect attendance. Rescheduling was performed in case of work conflict, and language translation help was requested when needed. After reviewing the clinical history, the nurses focused on explaining the importance of getting tested and the possibility of important conditions not being diagnosed in case of non-attendance. Efforts were made to eliminate fears and misconceptions related to first colonoscopies and previous negative experiences. Clinical aspects were approached by giving the patients instructions and tricks to help them successfully complete the preparedness protocols. Finally, other possible questions were addressed, and the intervention ended after confirmation of a complete understanding and willingness of the patient to attend the appointment. In the case of a disabled patient, the intervention was performed with the patient’s caretaker. Three attempts were made to locate the patient. Both mobile and landline telephones were considered for the intervention.
The primary outcome was the rate of non-attendance. Non-attendance was defined in case the patient did not show up to the colonoscopy appointment or in case of rescheduling or cancellation in the 3 d prior to the appointment, given the impossibility of preparing another patient in the remaining time and being able to fill the gap with another colonoscopy.
The secondary outcomes included compliance with patient preparedness protocols, bowel cleansing adequacy, patient satisfaction, and cost analysis derived from the nurse educational intervention.
To evaluate compliance with the cleansing protocols we asked the patient about the correct diet, taking the last dose of the laxative between 2 and 4 h, total intake of the cleansing agent, and split-dose regimen. According to the predominant social-economic low class of our patients, we preferred to measure the compliance with the bowel preparation protocol with a short face-to-face interview conducted by an endoscopy nurse before the colonoscopy, instead of a survey. Cleansing compliance was defined as an aggregate of the 4 previous cleansing variables.
Skilled endoscopists (> 1000 colonoscopies each) blinded to the randomization evaluated the adequacy according to the Boston Bowel Preparation Scale (BBPS). Cleansing adequacy was defined as all the colon segments scoring 2 or 3 points.
Compliance with the management of antithrombotic drugs was assessed according to ESGE guidelines. In the IG, patients with high comorbidity were referred to an endoscopy programme under anaesthesia. The appropriate scheduling according to the sedation administration was evaluated according to the presence of a high comorbidity burden. Disabled patients included any patient with physical or intellectual disability who needed help with colonoscopy preparedness.
Cost analysis was performed from the supplier’s perspective. We calculated the direct costs of the intervention compared with the cost of a colonoscopy that could not be billed. A colonoscopy service is invoiced based on its performance, which means it will not be charged if the patient does not show or there is a rescheduling need because of non-compliance with patient preparedness protocols. The cost of the colonoscopy was based on our hospital charges. The cost of the intervention was based on the nurse salary, according to our hospital’s collective agreement.
Patient satisfaction was quantified with the GHAA 9-me questionnaire from the ASGE[30] previously translated and validated into Spanish[31], including 7 items (waiting time until the appointment, waiting time on the day of examination, personal manner of staff, personal manner of the physician, adequacy of explanations given after the procedure, discomfort during examination and an overall rating of the visit). A specific item related to information given before the procedure was added (item 8). Each item was rated in an ordinal way (0-4), with 4 being the maximum satisfaction score, and satisfaction was assessed according to the score of the new item (0-4), the global score (0-32), and the percentage of patients who rated the information given before colonoscopy as excellent.
Demographic, clinical and endoscopic variables known to potentially impact attendance were recorded from the hospital electronic database and the telephone interview. The study nurses registered all relevant information regarding non-compliance with preparedness protocols in the endoscopy room before the colonoscopy. Endoscopists registered the BBPS in the endoscopy report. Patient satisfaction was assessed with a nurse-led telephone interview 30 d after the colonoscopy.
The statistical methods of the study were reviewed by Duran X from Consulting service on methodology for Biomedical Research. Hospital del Mar Medical Research Institute (IMIM). Barcelona. Spain.
The sample size was estimated to demonstrate the superiority of the educational intervention. We retrospectively obtained a non-attendance rate of 13.9% from November 2016 to May 2017, the same period of the study the year before. We use this figure to calculate the sample size because scarce published data on non-attendance in non-screening colonoscopies are available. Expecting a non-attendance rate of 13.9% in the CG and 8.9% in the IG to detect a 5% reduction as clinically significant and applying a significance level of 5%, a power of 80% for the comparison of two independent proportions and a 20% loss ratio, a sample size of 764 patients per group was calculated.
The intention-to-treat (ITT) analysis included all randomized patients. The per-protocol (PP) analysis included the participants who were finally contacted by telephone. Categorical variables were described through frequencies table (number and percentage). Quantitative variables were described through mean and standard deviation. The categorical variables were compared between groups by the Pearson chi-squared test or Fisher’s exact test if applicable and continuous variables by using Student’s t-test. Multivariate logistic regression was used to identify factors associated with non-attendance. The backward stepwise criterion was used for variable selection. A P value of > 0.1 as removal criteria and < 0.05 for inclusion criteria. The results are expressed as odds ratios (ORs). Stata software version 15.1 was used by our research statistician to perform the analysis.
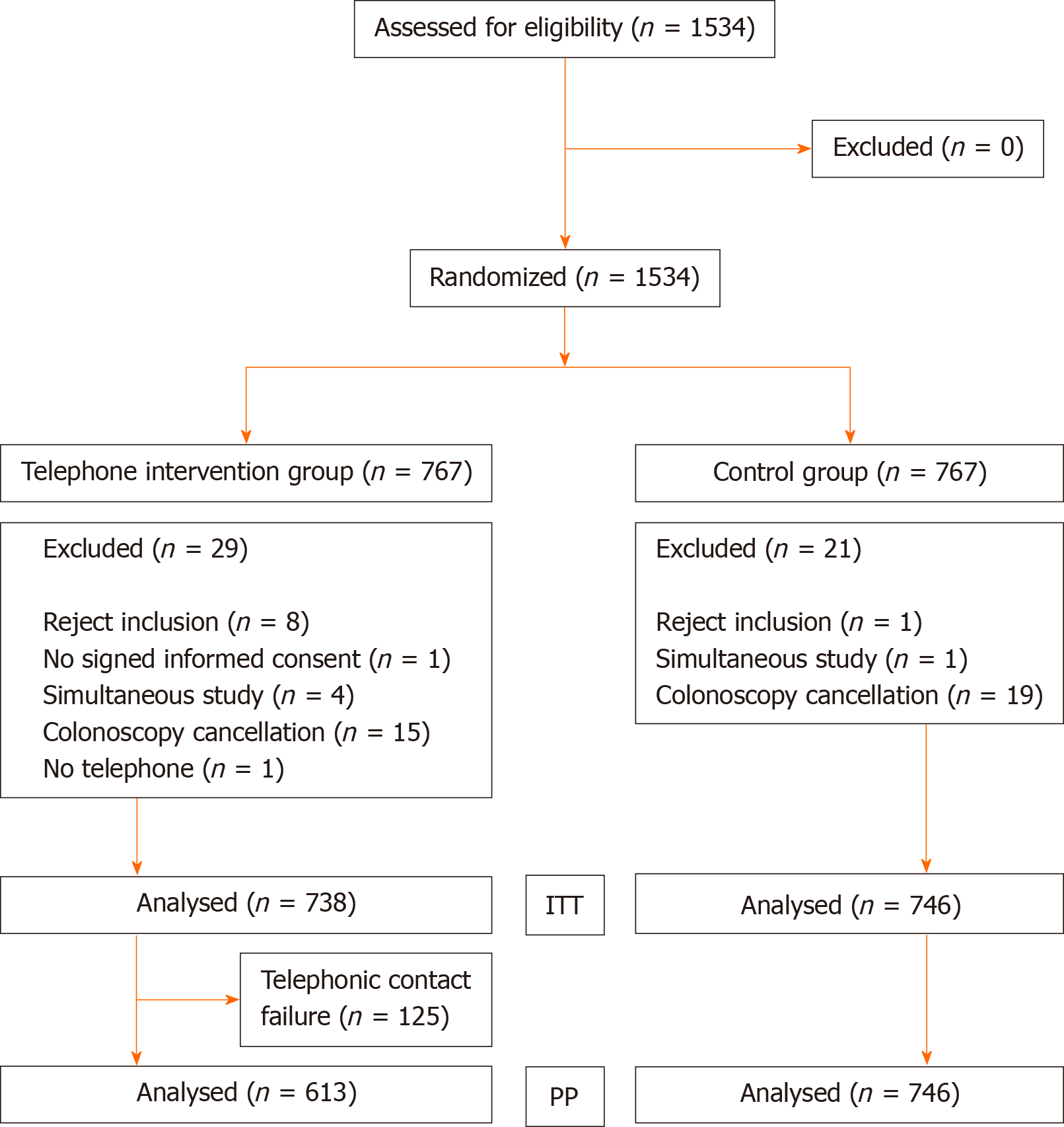
A total of 1485 patients (738 in the IG and 746 in the CG) were finally enrolled (Figure 1). Telephone contact was achieved in 613 (83%) patients in the IG. At baseline, the two groups did not differ in any of the variables analysed. Demographic, clinical and endoscopy data are shown in Table 1. The mean telephone time for the educational intervention was 12 min.
| Intervention (n = 738) | Control (n = 746) | P value | |
| Demographic variables | |||
| Age (yr), mean (SD) | 59.1 (16.2) | 59.9 (16.0) | 0.307 |
| Male sex, n (%) | 347 (47) | 363 (48.7) | 0.527 |
| Foreign nationality, n (%) | 94 (12.7) | 102 (13.7) | 0.594 |
| Advanced studies, n (%) | 148 (20.1) | 149 (20.0) | 0.834 |
| Language barrier, n (%) | 67 (9.1) | 53 (7.1) | 0.163 |
| Clinical variables | |||
| BMI, mean (SD) | 26.7 (4.7) | 26.9 (4.6) | 0.657 |
| Diabetes mellitus, n (%) | 126 (17.1) | 125 (16.8) | 0.871 |
| Abdominal/pelvic surgery, n (%) | 287 (38.9) | 292 (39.1) | 0.920 |
| Constipation, n (%) | 148 (20.1) | 161 (21.6) | 0.469 |
| Anxiety-depression syndrome, n (%) | 253 (34.3) | 253 (33.9) | 0.881 |
| Disabled condition, n (%) | 29 (3.9) | 33 (4.4) | 0.634 |
| Charlson index, mean (SD) | 0.5 (0.9) | 0.5 (0.9) | 0.322 |
| ASA classification III-IV, n (%) | 84 (11.4) | 100 (13.4) | 0.237 |
| High comorbidity burden, n (%) | 33 (4.5) | 42 (5.6) | 0.308 |
| Antiaggregants, n (%) | |||
| Aspirin | 73 (9.9) | 72(9.7) | 0.798 |
| Clopidogrel | 6 (0.8) | 9 (1.2) | |
| Dual APA | 1 (0.1) | 2 (0.3) | |
| VKA, n (%) | 24 (3.3) | 28 (3.8) | 0.600 |
| DOAC, n (%) | |||
| Rivaroxaban | 4 (0.5) | 4 (0.5) | 0.735 |
| Apixaban | 8 (1.1) | (1.2) | |
| Dabigatran | 3 (0.4) | 5 (0.7) | |
| Endoscopic variables | |||
| Previous endoscopy, n (%) | 335 (45.4) | 323 (49.1) | 0.417 |
| Previous non-attendance, n (%) | 77 (10.4) | 86 (11.5) | 0.500 |
| Referring physician, n (%) | |||
| Primary care | 668 (90.5) | 684 (91.7) | 0.128 |
| Gastroenterologist | 70 (9.5) | 62 (8.3) | |
| Indication, n (%) | |||
| Surveillance | 211 (28.6) | 197 (26.4) | 0.620 |
| Diagnostic | 456 (61.8) | (63.3) | |
| Family history of CRC | 71 (9.6) | 77 (10.3) | |
| Waiting time (d), mean (SD) | 60.7 (56.6) | 59.5 (60.9) | 0.701 |
| Afternoon timetable, n (%) | 467 (63.3) | 746 (67.3) | 0.104 |
| Laxative, n (%) | |||
| MCSP | 102 (15.1) | 80 (12.5) | 0.372 |
| PEG + ascorbate, 2 L | 158 (23.4) | 3.2) | |
| PEG, 4 L | 416 (61.5) | 411 (64.3) | |
| Previous cleansing problems, n (%) | 37 (5) | 44 (5.9) | 0.453 |
According to the ITT analysis, the non-attendance rate was higher in the CG than in the IG (14.3% vs 8.4%, P ≤ 0.001). The absolute risk reduction (ARR) was 5.9% (95%CI: 2.7% to 9.2%). In the PP analysis, there was a greater reduction in non-attendance (14.3% vs 4.4%, P ≤ 0.001), with an ARR of 9.9% (95%CI: 6.9% to 13%).
The study of variables related to non-attendance was assessed with a bivariable (Table 2) and a multivariable analysis (Table 3), in which 12 variables were found to be independent predictors, with the treatment group being an independent factor for non-attendance, both in the ITT analysis (OR 1.81, 95%CI: 1.27 to 2.58, P = 0.001) and the PP analysis (OR 3.56, 95%CI: 2.25 to 5.64, P ≤ 0.001).
| ITT | PP | |||||
| A | NA | P value | A | NA | P value | |
| Demographic risk factors | ||||||
| Group, n (%) | < 0.001 | < 0.001 | ||||
| Intervention | 676 (51.4) | 62 (36.7) | 586 (47.8) | 27 (20.1) | ||
| Control | 639 (48.6) | 107 (63.3) | 639 (52.2) | 107 (79.9) | ||
| Age (yr), mean (SD) | 60.2 (15.7) | 54.2 (18.0) | < 0.001 | 60.62 (15.6) | 53.45 (18.2) | < 0.001 |
| Sex, n (%) | 0.640 | 0.527 | ||||
| Female | 683 (51.9) | 91 (53.8) | 626 (51.1) | 75 (56) | ||
| Male | 632 (48.1) | 78 (46.2) | 599 (48.9) | 59 (44) | ||
| Nationality, n (%) | < 0.001 | < 0.001 | ||||
| Spanish | 1169 (88.9) | 119 (70.4) | 1092 (89.1) | 96 (71.6) | ||
| Foreign | 146 (11.1) | 50 (29.6) | 133 (10.9) | 38 (28.4) | ||
| Studies, n (%) | < 0.001 | < 0.001 | ||||
| Non-advanced | 1033 (78.6) | 154 (91.1) | 947 (77.3) | 121 (90.3) | ||
| Advanced | 282 (21.4) | 15 (8.9) | 278 (22.7) | 13 (9.7) | ||
| Language barrier, n (%) | 0.318 | 0.276 | ||||
| No | 1212 (92.2) | 152 (89.9) | 1130 (92.2) | 120 (89.6) | ||
| Yes | 103 (7.8) | 17(10.1) | 95 (7.8) | 14 (10.4) | ||
| Clinical risk factors | ||||||
| BMI, mean (SD) | 26.73 (4.6) | 27.76 (4.9) | 0.007 | 26.75 (4.5) | 27.84 (4.9) | 0.010 |
| Diabetes mellitus, n (%) | 0.758 | 0.528 | ||||
| No | 1094 (83.2) | 139 (82.2) | 1014 (82.8) | 108 (80.6) | ||
| Yes | 221 (16.8) | 30 (17.8) | 211 (17.2) | 26 (19.4) | ||
| Abdominal/pelvic surgery, n (%) | 0.046 | 0.465 | ||||
| No | 790 (60.1) | 115 (60.8) | 728 (59.4) | 84 (62.7) | ||
| Yes | 525 (39.9) | 54 (32.0) | 497 (40.6) | 50 (37.3) | ||
| Constipation, n (%) | 0.148 | 0.214 | ||||
| No | 1034 (78.6) | 141 (83.4) | 958 (78.2) | 11 (82.8) | ||
| Yes | 429 (32.6) | 77 (45.6) | 276 (21.8) | 23 (17.2) | ||
| Anxiety-depression syndrome, n (%) | 0.001 | 0.002 | ||||
| No | 886 (67.4) | 92 (54.4) | 832 (67.9) | 73 (54.5) | ||
| Yes | 429 (32.6) | 77 (45.6) | 393 (32.1) | 61 (45.5) | ||
| Disabled condition, n (%) | < 0.001 | 0.002 | ||||
| No | 1269 (96.5) | 153 (90.5) | 1182 (96.5) | 122 (91.0) | ||
| Yes | 46 (3.5) | 16 (9.5) | 43 (3.5) | 12 (9.0) | ||
| Charlson index, mean (SD) | 0.57 (0.9) | 0.54 (0.9) | 0.771 | 0.57 (0.9) | 0.50 (0.8) | 0.403 |
| ASA classification, n (%) | 0.813 | 0.834 | ||||
| I/II | 1151 (87.5) | 149 (88.2) | 1071 (87.4) | 118 (88.1) | ||
| III/IV | 164 (12.5) | 20 (11.8) | 154 (12.6) | 16 (11.9) | ||
| High comorbidity burden, n (%) | 0.840 | 0.769 | ||||
| No | 1248 (94.9) | 161 (95.3) | 1163 (94.9) | 128 (95.5) | ||
| Yes | 67 (5.1) | 8 (4.7) | 62 (5.1) | 6 (4.5) | ||
| Endoscopic risk factors | ||||||
| Previous endoscopy, n (%) | < 0.001 | < 0.001 | ||||
| No | 697 (53) | 129 (76.3) | 646 (52.7) | 98 (73.1) | ||
| Yes | 618 (47) | 40 (23.7) | 579 (47.3) | 36 (26.9) | ||
| Previous non-attendance, n (%) | < 0.001 | < 0.001 | ||||
| No | 1192 (90.6) | 129 (76.3) | 1111 (90.7) | 101 (75.4) | ||
| Yes | 123 (9.4) | 40 (23.7) | 114 (9.3) | 33 (24.6) | ||
| Referring physician, n (%) | 0.125 | 0.293 | ||||
| Primary care | 1178 (89.6) | 159 (94.1) | 1101 (89.9) | 125 (93.3) | ||
| Gastroenterologist | 122 (9.3) | 10 (5.9) | 109 (8.9) | 9 (6.7) | ||
| Other specialities | 15 (1.1) | 0 (0.0) | 15 (1.2) | 0 (0) | ||
| Indication, n (%) | < 0.001 | < 0.001 | ||||
| Surveillance | 338 (29.5) | 20 (11.8) | 357 (29.1) | 15 (11.2) | ||
| Diagnostic | 793 (60.3) | 135 (79.9) | 744 (60.7) | 107 (79.9) | ||
| Family history of CRC | 134 (10.2) | 14 (8.3) | 124 (10.1) | 12 (9) | ||
| Waiting time (d), mean (SD) | 59.3 (57.4) | 66.2 (68.6) | 0.149 | 58.3 (55.0) | 66.1 (72.4) | 0.134 |
| Endoscopy timetable, n (%) | 0.030 | 0.029 | ||||
| Morning | 469 (35.7) | 46 (27.2) | 436 (35.6) | 35 (26.1) | ||
| Afternoon | 846 (64.3) | 123 (72.8) | 789 (64.4) | 99 (73.9) | ||
| Previous cleansing problems, n (%) | 0.318 | 0.180 | ||||
| No | 1246 (94.8) | 157 (92.9) | 1159 (94.6) | 123 (91.8) | ||
| Yes | 69 (5.2) | 12 (7.1) | 66 (5.4) | 11 (8.2) | ||
| ITT | PP | |||||
| OR | 95%CI | P value | OR | 95%CI | P value | |
| Demographic risk factors | ||||||
| Group | ||||||
| Intervention | 1 | 1 | ||||
| Control | 1.81 | 1.27-2.58 | 0.001 | 3.56 | 2.25-5.64 | < 0.001 |
| Age | 0.98 | 0.97-0.99 | < 0.001 | 0.97 | 0.96-0.98 | < 0.001 |
| Nationality | ||||||
| Spanish | 1 | |||||
| Foreign | 2.69 | 1.77-4.10 | < 0.001 | 2.49 | 1.55-4.00 | < 0.001 |
| Studies level | ||||||
| Non-advanced | 1 | 1 | ||||
| Advanced | 0.47 | 0.27-0.83 | 0.010 | 0.51 | 0.27-0.94 | 0.031 |
| Clinical risk factors | ||||||
| BMI | 1.05 | 1.01-1.08 | 0.012 | 1.04 | 1.01-1.09 | 0.027 |
| Anxiety-depression syndrome | ||||||
| No | 1 | 1 | ||||
| Yes | 2.00 | 1.40-2.86 | < 0.001 | 2.02 | 1.35-3.02 | 0.001 |
| High comorbidity burden | ||||||
| No | 1 | 1 | ||||
| Yes | 2.82 | 0.86-9.24 | 0.087 | 3.87 | 1.17-12.85 | 0.027 |
| Disabled condition | ||||||
| No | 1 | 1 | ||||
| Yes | 3.39 | 1.68-6.84 | 0.001 | 3.37 | 1.50-7.58 | 0.003 |
| Endoscopic risk factors | ||||||
| Previous endoscopy | ||||||
| No | 1 | 1 | ||||
| Yes | 0.35 | 0.22-0.56 | < 0.001 | 0.46 | 0.28-0.77 | 0.003 |
| Previous non-attendance | ||||||
| No | 1 | 1 | ||||
| Yes | 2.94 | 1.89-4.58 | < 0.001 | 3.13 | 1.91-5.13 | < 0.001 |
| Previous cleansing problems | ||||||
| No | 1 | 1 | ||||
| Yes | 2.58 | 1.19-5.59 | 0.016 | 2.58 | 1.13-5.85 | 0.024 |
| Endoscopy timetable | ||||||
| Morning | 1 | 1 | ||||
| Afternoon | 1.52 | 1.03-2.23 | 0.033 | 1.62 | 1.04-2.51 | 0.031 |
In the IG, there was an improvement in all compliance-related variables (Table 4). It is important to highlight that there was a modest benefit in compliance with cleansing items. The benefit was much greater in regard to the management of antithrombotics and sedation scheduling.
| Intervention | Control | P value | |
| Compliance outcomes | |||
| Fasting 2-4 h, n/n (%) | |||
| ITT | 464/702 (66.2) | 427/720 (59.3) | 0.007 |
| PP | 408/583 (70.1) | 427/720 (59.3) | < 0.001 |
| Split regimen, n/n (%) | |||
| ITT | 622/702 (88.6) | 572/719 (79.6) | < 0.001 |
| PP | 544/583 (93.3) | 572/719 (79.6) | < 0.001 |
| Correct diet, n/n (%) | |||
| ITT | 633/702 (90.2) | 593/720 (82.4) | < 0.001 |
| PP | 553/583 (94.9) | 593/720 (82.4) | < 0.001 |
| Complete intake, n/n (%) | |||
| ITT | 597/702 (85) | 554/720 (76.9) | < 0.001 |
| PP | 522/583 (89.5) | 554/720 (76.9) | < 0.001 |
| Cleansing compliance, n/n (%) | |||
| ITT | 433/702 (61.7) | 379/720 (52.6) | 0.001 |
| PP | 383/583 (65.7) | 379/720 (52.6) | < 0.001 |
| Antithrombotic drugs, n/n (%) | |||
| ITT | 37/40 (92.5) | 27/43 (62.8) | 0.001 |
| PP | 33/35 (94.3) | 27/43 (62.8) | 0.001 |
| Endoscopy with anaesthesiologist, n/n (%) | |||
| ITT | 26/33 (78.8) | 0/42 (0) | < 0.001 |
| PP | 26/26 (100) | 0/42 (0) | < 0.001 |
| Rescheduling for non-compliance | |||
| Global rescheduling, n/n (%) | |||
| ITT | 2/676 (0.3) | 15/639 (2.3) | 0.001 |
| PP | 1/586 (0.2) | 15/639 (2.3) | 0.001 |
| Patient satisfaction questionnaire | |||
| Percentage of excellent (item 8), n/n (%) | |||
| ITT | 195/382 (51) | 97/373 (26) | < 0.001 |
| PP | 171/346 (49.4) | 97/373 (26) | < 0.001 |
| Information score (item 8) | |||
| ITT, mean (SD) | 3.29 (0.88) | 2.80 (1) | < 0.001 |
| PP, mean (SD) | 3.31 (0.89) | 2.80 (1) | < 0.001 |
| Total score of the questionnaire | |||
| ITT, mean (SD) | 26.12 (3.76) | 25.43 (3.82) | 0.01 |
| PP, mean (SD) | 26.18 (3.87) | 25.43 (3.82) | 0.008 |
Our hospital invoices €240.71 for a performed colonoscopy. The calculated nurse cost of the telephone intervention was €5.12 per patient. With a non-attendance rate of 14.3% and a non-compliance rescheduling rate of 2.3% (Table 4) the net income in the CG per 100 patients was €20075 (the result of subtracting €3442 for non-attendance and €554 for non-compliance to the total amount of €24071). According to the non-attendance and non-compliance figures in the IG of 8.4% and 0.3% respectively (Table 4), the net income in the IG per 100 patients was €21465 (the result of subtracting €2022 for non-attendance, €72 for non-compliance, and €512 for the nurse intervention to the total amount of €24071).
Therefore, the intervention was a cost-saving measure, as the benefit was greater in the IG, resulting in a net balance of €1390 (€21465-€20075) per 100 patients, €13.9 per patient. Since our centre performs approximately 4000 colonoscopies in a year, the implementation of the intervention would represent a benefit of €55600.
A total of 627 and 673 colonoscopies (584 in patients contacted) were finally performed in the CG and IG, respectively. The difference in cleansing adequacy did not reach statistical significance (CG 90.4% and IG 92.4%, P = 0.1); it also did not reach significance in the PP analysis (CG 90.4% and IG 93.2%, P = 0.08).
A total of 755 patients were contacted (50.8%). According to the total score and specific information item score, patient satisfaction improved with the intervention. The information was rated as excellent in 49.4% (IG) and 26% (CG) of patients, P ≤ 0.001 (Table 4).
This is the first RCT that demonstrates that an educational measure reduces non-attendance in non-screening colonoscopies with a significant clinical and economic impact, suggesting the suitability of its implementation in endoscopy units. In addition, the educational intervention also improved the need to reschedule the colonoscopy for non-compliance with patient preparedness protocols, such as antithrombotic management, sedation scheduling or bowel cleansing instructions.
The educational intervention was an important factor for non-attendance reduction. We believe that this is probably related to the fact that the educational measure is capable of dealing with medical aspects related to care that are impossible to address from an administrative perspective and that the figure of an educator truly impacts the patient, especially if it is a health-care provider in the endoscopy unit. The drastic reduction observed in the PP analysis (9.9%) suggests that the bidirectional conversation with the patient, dedicating the necessary time to carry out the educational intervention in a personal way, is the key point. This agrees with published results of educational patient interventions in which bidirectional communication with the patient was effective in improving colon cleansing adequacy[21-23]. On the other hand, other educational measures that do not allow a “human” interaction (booklets, mailed print resources, web pages, telephone applications, etc.) have failed to achieve optimal results[8].
Bidirectional communication may be achieved through other means, such as face-to-face interviews and video conferences. A personal interview allows for conversation and facilitates the transmission of concepts through verbal and non-verbal communication. However, there are no published comparisons between a telephone and a face-to-face interview to improve patient education. In any case, a personal interview has some logistical issues, such as the need for an interview room, a shorter agenda capability, the transport and access of the patients to hospitals and a higher cost than a telephone intervention. These limitations are even more important during the present COVID-19 pandemic. Furthermore, a video conference is a new and promising communication method that needs to be evaluated. However, its applicability is more limited than a telephone call because some patients do not have the technology or the knowledge to use it.
Regarding the person responsible for providing medical education, there are no published comparisons between the prescribing doctor, administrative personnel, a primary care nurse or an endoscopy nurse. Nevertheless, our study demonstrates that endoscopy nurses are capable of conducting telephone educational interventions, and because of their involvement, knowledge and immediate access to endoscopy experts, they could be the ideal person to eliminate the barriers that negatively influence the patient's attendance, with the additional benefit of improving compliance with patient preparedness protocols.
The multivariate analysis showed several independent risk factors for non-attendance. However, our intervention was the only modifiable factor. In this regard, when the patients were successfully contacted, the intervention was the most important predictor of attendance.
A quality improvement intervention is not implementable if despite generating a clinical improvement, it is not economically viable. It has been previously reported that the financial loss attributed to endoscopy non-attendance can be very high and can considerably decrease the expected net gain of outpatient procedure centres[32]. Similar to other educational studies[20,21], ours shows that non-attendance and rescheduling due to poor compliance are associated with a significant cost that nursing education intervention manages to reduce, providing data that support the conclusion that the educational intervention is not only cost-effective but also cost-saving.
Related to cleansing improvement, the intervention showed a numerically higher cleansing adequacy, but the difference was not statistically significant. However, this was not the main objective of our intervention. In any case, it must also be pointed out that both groups exceeded the 90% adequacy rate, which is over the quality recommendations[1], and it is possible that a ceiling effect is present.
We want to point out that our study has several strengths. First, this is the first RCT to evaluate an educational intervention to improve colonoscopy attendance outside colorectal screening programmes. Second, randomization was carried out with a large sample with broad inclusion criteria, which favours the extrapolation of the sample results from the study population. Third, we followed the most updated colonoscopy protocols recommended by the ESGE[26-28], allowing comparison with other studies. Finally, we performed a PP analysis and an economic study to measure the applicability of the intervention.
The main limitation of the study is the single centre design. There is room for improvement in the educational intervention since there are other independent factors that can help identify patients with high risk for non-attendance with whom to perform a more targeted intervention. It is also important to highlight that there are still several unknown factors to clarify regarding attendance outside population screening programmes. Studies are needed to determine the type and percentage of undiagnosed pathology and the prognostic and therapeutic implications of the diagnostic delay in the patients. We also do not know the effect that the intervention could have on attending future colonoscopies in this population although the satisfaction results observed in our study are promising in this regard.
Attendance is not currently considered a routine quality measurement parameter[1], but we believe this is arguable. Non-attendance, both in the diagnosis and in the surveillance of colonoscopies, has a significant clinical impact due to the diagnostic delay that it generates, which can be devastating in the case of colorectal cancer, which is mainly still diagnosed outside of colorectal screening programmes. Attendance is also a well-defined and reliable performance measure that is easy to measure and clearly susceptible to improvement. Its impact on the rest of the endoscopic procedures is also evident by increasing the waiting lists and making the endoscopic procedures more expensive. This means that attendance meets all the conditions that the European guideline considers as necessary to be able to include it as a key measure parameter for colonoscopy[1]. Colonoscopy quality parameters are not fixed and change over time based on data provided by new studies. We believe that our results support placing more importance on colonoscopy attendance as a routine quality measure parameter outside colorectal cancer screening programmes.
In conclusion, we found that an educational telephone intervention carried out by endoscopy nurses improves attendance outside colorectal cancer screening programmes, facilitates compliance with colonoscopy preparedness protocols, increases patient satisfaction and results in a beneficial economic impact, all of which support its implementation and maintenance over time. We believe that due to its characteristics as a quality measure parameter and given the significant clinical and economic impact observed, attendance measures should be routinely incorporated into endoscopy units.
Educative interventions with bidirectional contact to the patient have shown to improve colonoscopy attendance in colorectal cancer population screening programmes and because of its huge clinical and economic impact, they have been widely implemented. However, outside of this population programmes, educative measures to improve colonoscopy attendance have been poorly studied and no navigation interventions are usually performed.
We thought this lack of research needed attention, so we designed a randomized controlled trial to conduct an educational telephone nurse intervention with bidirectional contact directed to increase colonoscopy attendance, similar to the patient navigation carried out in the population screening setting.
The aim of the study was to determine the clinical and economic impact of this educational intervention.
We included all consecutive outpatients referred for colonoscopy from primary care centres in our health area. Patients randomized to the intervention group received a telephone call 7 d before colonoscopy appointment to eliminate socioeconomic, psychological and clinical barriers that could affect attendance. Baseline characteristics including demographics, clinical and endoscopic factors previously reported to be related to non-attendance were collected. The primary outcome was the attendance rate. The secondary outcomes included the economic impact and the potential benefit of the intervention in regard to compliance with patient preparedness protocols, cleansing adequacy, and patient satisfaction. We performed an intention-to-treat (ITT) and per-protocol (PP) analysis to measure the applicability of the telephone intervention.
A total of 738 and 746 patients were finally included in the intervention and control group (CG) respectively. Six hundred thirteen (83%) patients were contacted in the intervention group (IG). The non-attendance rate was lower in the IG, both in the ITT analysis (IG 8.4% vs CG 14.3%, P < 0.001) and in the PP analysis (4.4% vs 14.3%, P < 0.001). In a multivariable analysis, belonging to the CG increased the risk of non-attendance in both, the ITT analysis (OR 1.81, 95%CI: 1.27 to 2.58, P = 0.001) and the PP analysis (OR 3.56, 95%CI: 2.25 to 5.64, P < 0.001). There was also a significant difference in compliance with preparedness protocols [bowel cleansing: IG 61.7% vs CG 52.6% (P = 0.001), antithrombotic management: IG 92.5% vs CG 62.8% (P = 0.001), and sedation scheduling: IG 78.8% vs CG 0% (P ≤ 0.001)]. We observed a net benefit of €55600/year after the intervention. The information given before the procedure was rated as excellent by 26% (CG) and 51% (IG) of patients, P ≤ 0.001.
According to our results, non-attendance has a significant clinical and economic impact outside the population screening setting. This study proposes the necessity to routinely incorporate attendance measures into endoscopy units, not only in the population screening programmes but also in all colonoscopies. A telephone educative intervention by an endoscopy nurse seems to be a valid method.
Further multicentric studies on attendance outside colorectal cancer population screening programmes are needed. The type and percentage of undiagnosed pathology and the prognostic and therapeutic implications of the diagnostic delay in these patients have to be studied. We also do not know the effect that the intervention could have on attending future colonoscopies although the satisfaction results observed in our study are promising in this regard.
The authors would like to thank Serrano MC from The Epidemiology Department who assisted with the study design and Reguant FC for his help with the economic analysis.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: American Society for Gastrointestinal Endoscopy, No. 103506.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Spain
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Alsayid M, Ribeiro IB S-Editor: Huang P L-Editor: A P-Editor: Li JH
| 1. | Kaminski MF, Thomas-Gibson S, Bugajski M, Bretthauer M, Rees CJ, Dekker E, Hoff G, Jover R, Suchanek S, Ferlitsch M, Anderson J, Roesch T, Hultcranz R, Racz I, Kuipers EJ, Garborg K, East JE, Rupinski M, Seip B, Bennett C, Senore C, Minozzi S, Bisschops R, Domagk D, Valori R, Spada C, Hassan C, Dinis-Ribeiro M, Rutter MD. Performance measures for lower gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement Initiative. Endoscopy. 2017;49:378-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 337] [Cited by in RCA: 482] [Article Influence: 60.3] [Reference Citation Analysis (0)] |
| 2. | Weinberg DS, Keenan E, Ruth K, Devarajan K, Rodoletz M, Bieber EJ. A randomized comparison of print and web communication on colorectal cancer screening. JAMA Intern Med. 2013;173:122-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Helander S, Hakama M, Malila N. Effect of a pre-screening survey on attendance in colorectal cancer screening: a double-randomized study in Finland. J Med Screen. 2014;21:82-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Pisera M, Kaminski MF, Kraszewska E, Rupinski M, Regula J. Reinvitation to screening colonoscopy: a randomized-controlled trial of reminding letter and invitation to educational meeting on attendance in nonresponders to initial invitation to screening colonoscopy (REINVITE). Eur J Gastroenterol Hepatol. 2016;28:538-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Stratmann K, Bock H, Filmann N, Fister P, Weber C, Tacke W, Simonis B, Höftmann M, Schröder O, Hausmann J, Zeuzem S, Blumenstein I. Individual invitation letters lead to significant increase in attendance for screening colonoscopies: Results of a pilot study in Northern Hesse, Germany. United European Gastroenterol J. 2018;6:1082-1088. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Griffin JM, Hulbert EM, Vernon SW, Nelson D, Hagel EM, Nugent S, Baines Simon A, Bangerter A, van Ryn M. Improving endoscopy completion: effectiveness of an interactive voice response system. Am J Manag Care. 2011;17:199-208. [PubMed] |
| 7. | Dougherty MK, Brenner AT, Crockett SD, Gupta S, Wheeler SB, Coker-Schwimmer M, Cubillos L, Malo T, Reuland DS. Evaluation of Interventions Intended to Increase Colorectal Cancer Screening Rates in the United States: A Systematic Review and Meta-analysis. JAMA Intern Med. 2018;178:1645-1658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 242] [Article Influence: 34.6] [Reference Citation Analysis (0)] |
| 8. | Calderwood AH, Roy HK. Increasing colorectal cancer screening adherence: comment on "A randomized comparison of print and web communication on colorectal cancer screening". JAMA Intern Med. 2013;173:129-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Bernardo BM, Zhang X, Beverly Hery CM, Meadows RJ, Paskett ED. The efficacy and cost-effectiveness of patient navigation programs across the cancer continuum: A systematic review. Cancer. 2019;125:2747-2761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 102] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 10. | Hermann EA, Ashburner JM, Atlas SJ, Chang Y, Percac-Lima S. Satisfaction With Health Care Among Patients Navigated for Preventive Cancer Screening. J Patient Exp. 2018;5:225-230. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Post DM, McAlearney AS, Young GS, Krok-Schoen JL, Plascak JJ, Paskett ED. Effects of Patient Navigation on Patient Satisfaction Outcomes. J Cancer Educ. 2015;30:728-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Shuja A, Harris C, Aldridge P, Malespin M, de Melo SW Jr. Predictors of No-show Rate in the GI Endoscopy Suite at a Safety Net Academic Medical Center. J Clin Gastroenterol. 2019;53:29-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 13. | Laiyemo AO, Williams CD, Burnside C, Moghadam S, Sanasi-Bhola KD, Kwagyan J, Brim H, Ashktorab H, Scott VF, Smoot DT. Factors associated with attendance to scheduled outpatient endoscopy. Postgrad Med J. 2014;90:571-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Sola-vera J, Sáez J, Laveda R, Girona E, García-Sepulcre MF, Cuesta A, Vázquez N, Uceda F, Pérez E, Sillero C. Factors associated with non-attendance at outpatient endoscopy. Scand J Gastroenterol. 2008;43:202-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Chopra D, Hookey LC. Comorbid Illness, Bowel Preparation, and Logistical Constraints Are Key Reasons for Outpatient Colonoscopy Nonattendance. Can J Gastroenterol Hepatol. 2016;2016:2179354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Chang JT, Sewell JL, Day LW. Prevalence and predictors of patient no-shows to outpatient endoscopic procedures scheduled with anesthesia. BMC Gastroenterol. 2015;15:123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 17. | Lee CS, McCormick PA. Telephone reminders to reduce non-attendance rate for endoscopy. J R Soc Med. 2003;96:547-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Adams LA, Pawlik J, Forbes GM. Nonattendance at outpatient endoscopy. Endoscopy. 2004;36:402-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 61] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 19. | Downer SR, Meara JG, Da Costa AC. Use of SMS text messaging to improve outpatient attendance. Med J Aust. 2005;183:366-368. [PubMed] |
| 20. | Childers RE, Laird A, Newman L, Keyashian K. The role of a nurse telephone call to prevent no-shows in endoscopy. Gastrointest Endosc 2016; 84: 1010-1017. e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Abuksis G, Mor M, Segal N, Shemesh I, Morad I, Plaut S, Weiss E, Sulkes J, Fraser G, Niv Y. A patient education program is cost-effective for preventing failure of endoscopic procedures in a gastroenterology department. Am J Gastroenterol. 2001;96:1786-1790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 79] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Alvarez-Gonzalez MA, Flores-Le Roux JA, Seoane A, Pedro-Botet J, Carot L, Fernandez-Clotet A, Raga A, Pantaleon MA, Barranco L, Bory F, Lorenzo-Zuñiga V. Efficacy of a multifactorial strategy for bowel preparation in diabetic patients undergoing colonoscopy: a randomized trial. Endoscopy. 2016;48:1003-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 23. | Liu X, Luo H, Zhang L, Leung FW, Liu Z, Wang X, Huang R, Hui N, Wu K, Fan D, Pan Y, Guo X. Telephone-based re-education on the day before colonoscopy improves the quality of bowel preparation and the polyp detection rate: a prospective, colonoscopist-blinded, randomised, controlled study. Gut. 2014;63:125-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 133] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 24. | Kurlander JE, Sondhi AR, Waljee AK, Menees SB, Connell CM, Schoenfeld PS, Saini SD. How Efficacious Are Patient Education Interventions to Improve Bowel Preparation for Colonoscopy? PLoS One. 2016;11:e0164442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 25. | Hassan C, Bretthauer M, Kaminski MF, Polkowski M, Rembacken B, Saunders B, Benamouzig R, Holme O, Green S, Kuiper T, Marmo R, Omar M, Petruzziello L, Spada C, Zullo A, Dumonceau JM; European Society of Gastrointestinal Endoscopy. Bowel preparation for colonoscopy: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2013;45:142-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 311] [Article Influence: 25.9] [Reference Citation Analysis (1)] |
| 26. | Veitch AM, Vanbiervliet G, Gershlick AH, Boustiere C, Baglin TP, Smith LA, Radaelli F, Knight E, Gralnek IM, Hassan C, Dumonceau JM. Endoscopy in patients on antiplatelet or anticoagulant therapy, including direct oral anticoagulants: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guidelines. Endoscopy. 2016;48:385-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 138] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 27. | Dumonceau JM, Riphaus A, Schreiber F, Vilmann P, Beilenhoff U, Aparicio JR, Vargo JJ, Manolaraki M, Wientjes C, Rácz I, Hassan C, Paspatis G. Non-anesthesiologist administration of propofol for gastrointestinal endoscopy: European Society of Gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates Guideline--Updated June 2015. Endoscopy. 2015;47:1175-1189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 166] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 28. | Alvarez-Gonzalez MA, Pantaleon MA, Flores-Le Roux JA, Zaffalon D, Amorós J, Bessa X, Seoane A, Pedro-Botet J; PROCOLON group. Randomized Clinical Trial: A Normocaloric Low-Fiber Diet the Day Before Colonoscopy Is the Most Effective Approach to Bowel Preparation in Colorectal Cancer Screening Colonoscopy. Dis Colon Rectum. 2019;62:491-497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 29. | Alvarez-Gonzalez MA, Pantaleón Sánchez MÁ, Bernad Cabredo B, García-Rodríguez A, Frago Larramona S, Nogales O, Díez Redondo P, Puig Del Castillo I, Romero Mascarell C, Caballero N, Romero Sánchez-Miguel I, Pérez Berbegal R, Hernández Negrín D, Bujedo Sadornill G, Pérez Oltra A, Casals Urquiza G, Amorós Martínez J, Seoane Urgorri A, Ibáñez Zafón IA, Gimeno-García AZ. Educational nurse-led telephone intervention shortly before colonoscopy as a salvage strategy after previous bowel preparation failure: a multicenter randomized trial. Endoscopy. 2020;52:1026-1035. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 30. | Johanson JF, Schmitt CM, Deas TM Jr, Eisen GM, Freeman M, Goldstein JL, Jensen DM, Lieberman DA, Lo SK, Sahai A, Schoenfeld P, Morgan M. Quality and outcomes assessment in Gastrointestinal Endoscopy. Gastrointest Endosc. 2000;52:827-830. [PubMed] |
| 31. | Sánchez del Río A, Alarcón Fernández O, Baudet JS, Sainz Menéndez Z, Socas Méndez M. Reliability of the Spanish version of a brief questionnaire on patient satisfaction with gastrointestinal endoscopy. Rev Esp Enferm Dig. 2005;97:554-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | Berg BP, Murr M, Chermak D, Woodall J, Pignone M, Sandler RS, Denton BT. Estimating the cost of no-shows and evaluating the effects of mitigation strategies. Med Decis Making. 2013;33:976-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 76] [Article Influence: 6.3] [Reference Citation Analysis (0)] |