Published online Oct 28, 2020. doi: 10.3748/wjg.v26.i40.6279
Peer-review started: June 21, 2020
First decision: August 21, 2020
Revised: August 26, 2020
Accepted: September 23, 2020
Article in press: September 23, 2020
Published online: October 28, 2020
Processing time: 128 Days and 22.8 Hours
Pit pattern classification using magnifying chromoendoscopy is the established method for diagnosing colorectal lesions. The Japan Narrow-band-imaging (NBI) Expert Team (JNET) classification is a novel NBI magnifying endoscopic classification that focuses on the vessel, and surface patterns.
To determine the diagnostic efficacy of each category of the JNET and Pit pattern classifications for colorectal lesions.
A systematic literature search was performed using PubMed, Embase, the Cochrane Library, and Web of Science databases. The pooled sensitivity, specificity, diagnostic odds ratio, and area under the summary receiver operating characteristic curve of each category of the JNET and Pit pattern classifications were calculated.
A total of 19227 colorectal lesions in 31 studies were included. The diagnostic performance of the JNET classification was equivalent to the Pit pattern classification in each corresponding category. The pooled sensitivity, specificity, and area under the curve (AUC) for each category of the JNET classification were as follows: 0.73 (95%CI: 0.55-0.85), 0.99 (95%CI: 0.97-1.00), and 0.97 (95%CI: 0.95-0.98), respectively, for Type 1; 0.88 (95%CI: 0.78-0.94), 0.72 (95%CI: 0.64-0.79), and 0.84 (95%CI: 0.81-0.87), respectively, for Type 2A; 0.56 (95%CI: 0.47-0.64), 0.91 (95%CI: 0.79-0.96), and 0.72 (95%CI: 0.68-0.76), respectively, for Type 2B; 0.51 (95%CI: 0.42-0.61), 1.00 (95%CI: 1.00-1.00), and 0.90 (95%CI: 0.87-0.93), respectively, for Type 3.
This meta-analysis suggests that the diagnostic efficacy of the JNET classification may be equivalent to that of the Pit pattern classification. However, due to its simpler and clearer clinical application, the JNET classification should be promoted for the classification of colorectal lesions, and to guide the treatment strategy.
Core Tip: This systematic review and meta-analysis examined the diagnostic efficacy of each category of the Japan Narrow-band imaging Expert Team (JNET) and Pit pattern classifications for colorectal lesions. The pooled analyses of 19227 colorectal lesions from 31 studies were performed. The sensitivity, specificity, diagnostic odds ratio, and area under the summary receiver operating characteristic curve of each category of the JNET and Pit pattern classifications were calculated. The results suggest that the diagnostic efficacy of the JNET classification may be equivalent to that of the Pit pattern classification. However, due to its simpler and clearer clinical application, the JNET classification should be promoted for classification of colorectal lesions, and to guide the treatment strategy.
- Citation: Zhang Y, Chen HY, Zhou XL, Pan WS, Zhou XX, Pan HH. Diagnostic efficacy of the Japan Narrow-band-imaging Expert Team and Pit pattern classifications for colorectal lesions: A meta-analysis. World J Gastroenterol 2020; 26(40): 6279-6294
- URL: https://www.wjgnet.com/1007-9327/full/v26/i40/6279.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i40.6279
Colorectal cancer (CRC) is one of the most common malignant tumors in the world[1]. Accurate identification and treatment of early CRC have significantly reduced its incidence and mortality[2]. However, early CRC is generally asymptomatic, and coloscopy allows the direct visual inspection of the intestinal tract and same-session detection, biopsy, and subsequent removal of lesions. Endoscopic evaluation of colorectal lesions is important to guide the selection of an appropriate treatment. The ideal endoscopic management of colorectal lesions involves two steps. First, any mucosal lesions need to be detected. Second, the lesions need to be characterized based on histological characteristics assessed via endoscopic evaluation; which forms the basis of the endoscopic judgment on whether the lesions need to be resected. In general, there is a consensus that low-grade dysplasias (LGDs), high-grade dysplasias (HGDs), and superficial submucosal invasive (SM-s) carcinomas are considered appropriate for endoscopic resection, while observation is recommended for hyperplastic polyps (HPs), in contrast, surgery is recommended for deep submucosal invasive (SM-d) carcinomas[3].
Kudo et al[4] first proposed the “Pit patterns” (the opening shape of a colorectal crypt) based on the classification of colorectal lesions via magnifying endoscopy, and indigo carmine dye contrast[4]. Pit pattern diagnosis (Type I-V) is clinically significant as it can differentiate between neoplasia and non-neoplasia, characterize the degree of histological atypia in a tumor, and reveal the invasion depth of early carcinoma.
Usually, standard magnification requires the use of chromoagents (e.g., indigo carmine, crystal violet, or methylene blue) to clarify the pit structures in these diagnostic procedures. However, with the emergence of electronic staining endoscopic equipment, chemical staining endoscopy has gradually been replaced. In addition, simpler and more convenient procedures are desirable for magnifying procedures. It has been suggested that narrow-band-imaging (NBI) technology is as effective as chromoendoscopy in differentiating the gross type of colorectal lesions[5]. The Colon Tumor NBI Interest Group proposed the NBI International Colorectal Endoscopic (NICE) classification in 2010, which is based on non-magnifying NBI observations[6]. However, the NICE classification cannot distinguish between benign adenoma and superficial mucosal carcinoma, therefore, it plays a limited role in guiding endoscopic treatment strategies. As more endoscopic devices are being equipped with a magnifying function, NBI combined with magnifying endoscopy is increasingly being used, which further improves the diagnostic efficiency, and plays an important role in estimating the invasion depth of the lesion. In order to better guide the endoscopic treatment strategy, in 2014, the Japan NBI Expert Team (JNET) proposed the JNET classification as a universal NBI magnifying endoscopic classification[7]. The JNET classification focuses on vessel and surface patterns to diagnose colorectal lesions as Types 1, 2A and B, 3.
Recently, several studies have proposed that the JNET classification of colorectal lesions via NBI magnifying endoscopy is a useful and objective tool for differentiating the gross type of colorectal lesions. However, differences in the diagnostic performance of the JNET classification have not been reported according to each gross type. Although several investigators now accept the application of the JNET classification for colorectal lesions, to what extent we can trust the results of the JNET classification, and whether the Pit pattern classification can be replaced by the JNET classification are aspects that remain unclear.
Few studies have compared the diagnostic efficacy of the JNET and Pit pattern classifications for each gross type of lesion, and determined the correlation between endoscopic features and pathological findings, and, to our knowledge, there are no meta-analyses on this topic. Accordingly, we performed a systematic review and meta-analysis to analyze the data on existing magnifying endoscopy trials using the JNET classification and the Pit pattern classification for characterization of colorectal lesions, and, to obtain a statistically convincing conclusion on the diagnostic accuracy, and practicability of these two comparable methods.
We performed a systematic literature search of articles in PubMed, Web of Science, Embase and the Cochrane Library (January 1990 to May 2020) containing quantitative data, and manually searched the reference lists of retrieved articles. The following search terms were used: “Japan Narrow-Band Imaging Expert Team”, “Japan NBI Expert Team”, JNET, “Pit pattern”, “Kudo’s classification”, “Colorectal Neoplasm” “Neoplasm, Colorectal”, “Colorectal Carcinoma”, “Carcinoma, Colorectal”, “Carcinomas, Colorectal”, “Colorectal Carcinomas”, “Colorectal Cancer”, “Cancer, Colorectal”, “Cancers, Colorectal”, “Colorectal Cancers”, “Colorectal Tumors”, “Colorectal Tumor”, “Tumor, Colorectal”, “Tumors, Colorectal”, “Neoplasms, Colorectal”, “Colon polyps”, “Colorectal polyps”, and “Colorectal lesions”. The queries used are displayed in the supplementary materials. All similar possible word variations were also searched. The attained records were retrieved and managed with EndNote X 9.0 (Bld 10136, Thomson Reuters, New York, NY, United States).
Studies were included when all of the following conditions were met: (1) Studies in which all participants received the JNET or Pit pattern classification for colorectal lesions diagnosed via endoscopy; (2) Histological diagnosis was chosen as the gold standard; and (3) Studies in which sufficient data were reported to calculate true positive (TP), false positive (FP), false negative (FN), and true negative (TN) results. In addition, we included only the latest-published article when the same population was reported in more than one article. However, conference papers and duplicate published studies that fulfilled the above two criteria were excluded. This meta-analysis was performed in compliance with the preferred reporting items for systematic reviews and meta-analyses statement (PRISMA)[8].
Data from the included studies were extracted and cross-checked by 2 authors independently (Zhang Y and Pan HH). If there was a discrepancy in their opinions, it was discussed with other authors to achieve a consistent result. The extracted data included the name of the first author, year of publication, demographics of the population, type of endoscope, number of included patients, number of colorectal lesions examined, design of the study, and the type of classification for colorectal lesions. The number of TP, FP, TN, and FN results for the JNET, and Pit pattern classifications were the main statistics extracted from the studies. We computed sensitivity [TP/(TP + FN)] and specificity [TN/(TN + FP)] for each technique separately.
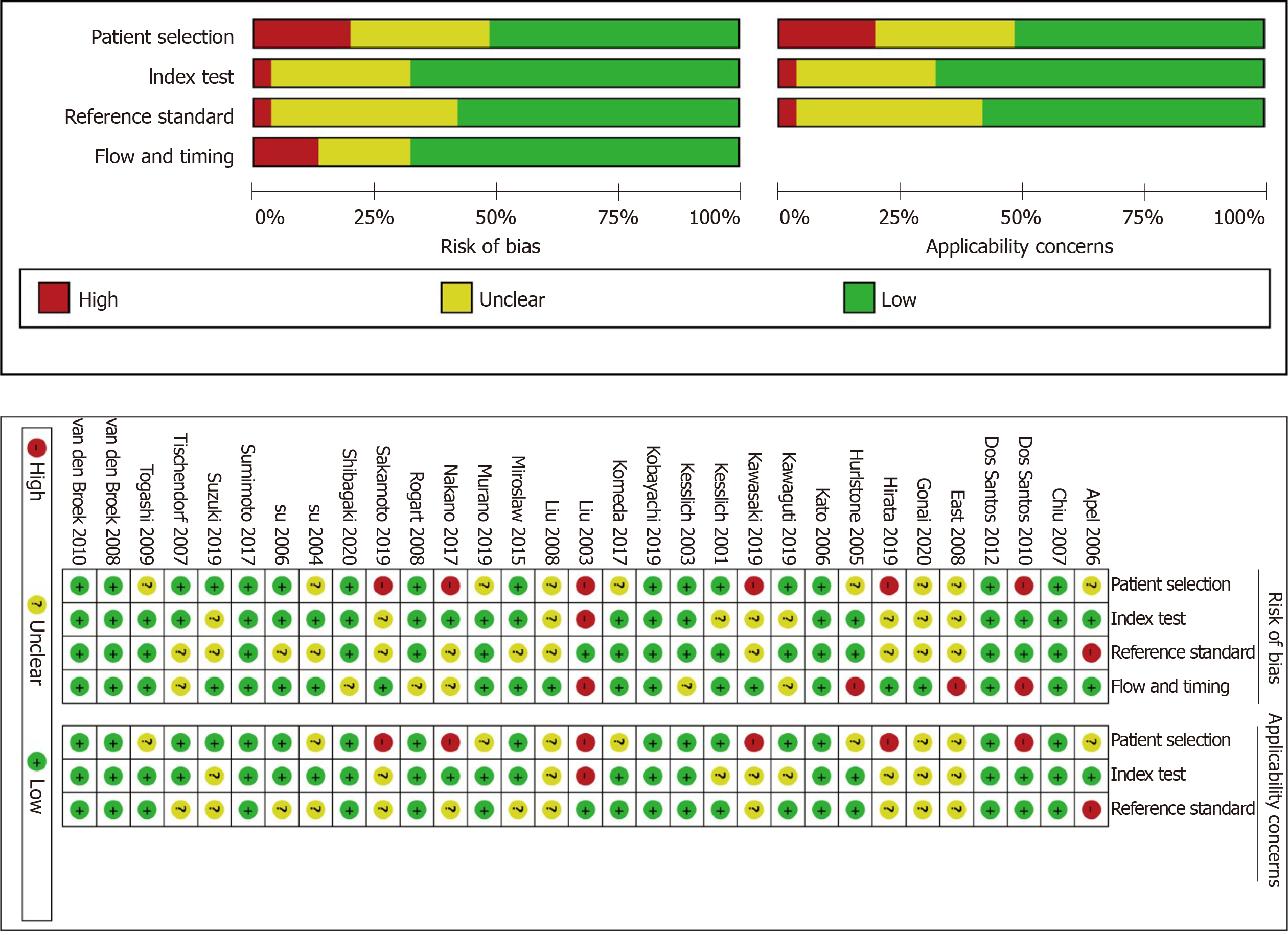
The quality of the included studies was independently assessed by 2 authors independently (Zhou XX and Chen HY) using the quality assessment of diagnostic accuracy studies II (QUADAS-II) tool[9].
The original data from each study (TP, FP, TN and FN) were integrated through meta-analysis, and the pooled sensitivity, specificity, positive likelihood ratio, and diagnostic odds ratio (DOR) of both the JNET and Pit pattern classifications were calculated by the DerSimonian Laird random effects model[10]. The heterogeneity of pooled sensitivity and specificity was calculated using the I2 statistic, and a high degree of heterogeneity was set at I2 > 50%[11]. Mose's constant linear model was used to perform the summary receiver operating characteristic curve[12]. Cochrane’s Q test was used to evaluate the accuracy of the JNET and Pit pattern classifications in the diagnosis of colorectal lesions. When heterogeneity was present, the Spearman correlation coefficient, and the P value or heterogeneity ratio caused by the threshold effect were calculated. Meta-regression was conducted to explore the existing source of heterogeneity. Publication bias was assessed using the Deeks’ Funnel Plot Asymmetry Test. The t-test was used to compare the statistical significance of the area under the curve (AUC) and pooled sensitivity, with the significance set at P < 0.05. The statistical software used for the diagnostic accuracy test was Stat 15.1. Revman5.3 was used to evaluate the quality of the included studies.
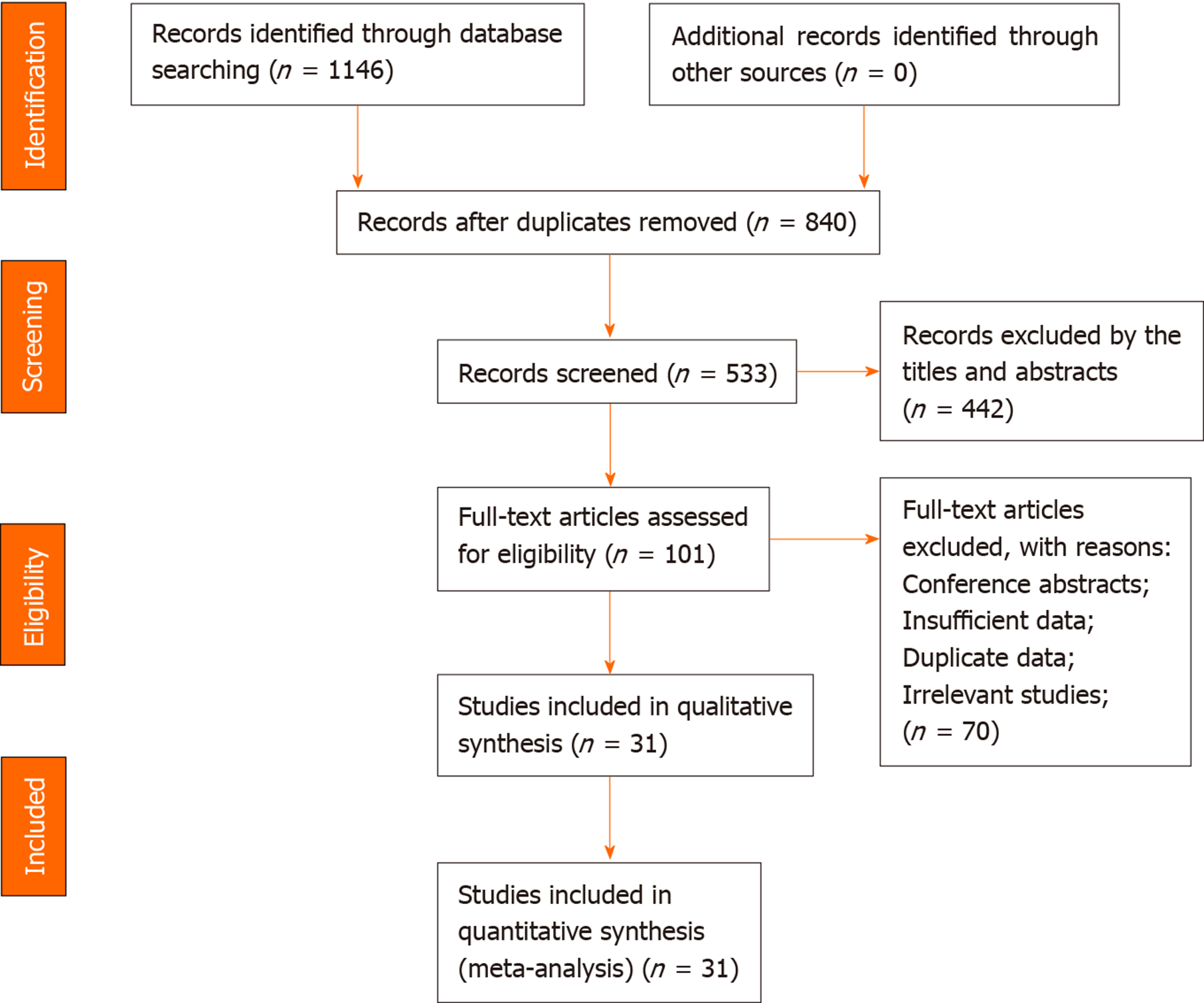
A total of 1146 articles were initially searched (351 in Web of Science, 241 in PubMed, 44 in Cochrane Library, and 510 in Embase), and 31 studies[5,13-42] with a total of 14674 patients were ultimately included in this meta-analysis. 1114 studies were excluded of which 306 studies were duplicate references, 442 studies were excluded based on title and abstract, and 70 studies were excluded after full-text review. A detailed PRISMA flow diagram is shown in Figure 1.
All studies used the JNET or Pit pattern classifications as the diagnostic criteria for colorectal lesions examined via endoscopy. The JNET classified colorectal lesions into four categories: Type 1 is a hyperplastic polyp (HP)/sessile serrated lesion (SSL), Type 2A is a LGD/adenoma, Type 2B is a HGD/M-SM-s and Type 3 is a SM-d[5]. The Pit pattern classification has five corresponding categories: Type I is normal mucosa, Type II is hyperplasia/SSL, Types IIIL/IV are LGD/adenomas, Types IIIS/VI-L, and VI-H/VN are associated with HGD/M-SM-s lesions, and SM-d lesions, respectively[13]. The detailed interpretation criteria are shown in Table 1. Our study was restricted to only cross-sectional outcomes such as sensitivity and specificity, and the screening tests were compared to the reference standard (histopathological diagnosis). General information on the included studies is presented in Table 2. Of the 31 studies[5,13-42], 11 were retrospective [5,13-22], and 20 were prospective[23-42]. Seven studies[14-20] used the JNET classification alone, 21 studies[22-42] used the Pit pattern classification alone, and only 3 studies[5,13,21] used both the JNET and Pit pattern classifications in the same population. Thirteen studies[5,13-16,18-21,24,28,35,41] used narrow-band imaging magnifying endoscopy (NBI-ME), 13 studies used magnifying chromoendoscopy[22,25-27,29,30,32-35,37,38,42], and the other studies used BLI-magnification[17,23] (n = 2), NBI[31,39] (n = 2), and chromoendoscopy[36,40] (n = 2). The QUADAS-II quality assessment for each study is presented in Figure 2.
| Interpretation | JNET | Pit pattern | Histological diagnosis | Therapeutic strategy |
| Non-neoplastic | I | Normal mucosa | ||
| Type 1 | II | Hyperplastic/SSL | Follow-up observation | |
| Neoplastic | Type 2A | IIIL + IV | Adenoma/LGD | Endoscopic resection (polypectomy/EMR) |
| Type 2B | IIIS + VI-L | HGD/M-SM-s cancer | Endoscopic resection (ESD) | |
| Type 3 | VN + VI-H | SM-d cancer | Surgery |
| Ref. | Year | Country | Study design | Patients (n) | Lesions (n) | Type of endoscopy | Typeof classification | Category |
| Shibagaki et al[13] | 2020 | Japan | Retrospective | 432 | 718 | A-NBI-ME | JNET/Pit pattern | 1/2A/2B/3; I, II, III/IV, VI-L, VI-H, VN |
| Kobayashi et al[5] | 2019 | Japan | Retrospective | 750 | 1402 | NBI-ME | JNET/Pit pattern | 1/2A/2B/3; I, II, IIIL, IIIS, IV, IVH, VI-L, VI-H, VN |
| Sumimoto et al[14] | 2017 | Japan | Retrospective | 1901 | 2933 | NBI-ME | JNET | 1/2A/2B/3 |
| Murano et al[15] | 2019 | Japan | Retrospective | 680 | 1472 | NBI-ME | JNET | 1/2A/2B/3 |
| Komeda et al[16] | 2017 | Japan | Retrospective | 199 | 199 | NBI-ME | JNET | 1/2A/2B/3 |
| Suzuki et al[17] | 2019 | Japan | Retrospective | 145 | 185 | BLI-ME | JNET | 1/2A/2B/3 |
| Hirata et al[18] | 2019 | Japan | Retrospective | 6138 | 6138 | NBI-ME | JNET | 1/2A/2B/3 |
| Sakamoto et al[19] | 2019 | Japan | Retrospective | 246 | 246 | NBI-ME | JNET | 1/2A/2B/3 |
| Gonai et al[20] | 2020 | Japan | Retrospective | 153 | 169 | NBI-ME | JNET | 2A/2B/3 |
| Kawasaki et al[21] | 2019 | Japan | Retrospective | 17 | 17 | NBI-ME | JNET/Pit pattern | 1/2A/2B/3; III, IV, VI-L, VI-H, VN |
| Nakano et al[23] | 2017 | Japan | Prospective | 506 | 799 | BLI-ME | Pit pattern | II, IIIL, IIIS/IV, VI-L, VI-H/VN |
| Miroslaw et al[24] | 2015 | Poland | Prospective | 270 | 386 | WL, NBI-ME | Pit pattern | I/II/IIIL/IIIS/IV/V |
| Su et al[25] | 2004 | China | Prospective | 230 | 270 | Magnifying chromoendoscopy | Pit pattern | I/II/IIIS/IIIL/IV/V |
| Kiesslich et al[26] | 2001 | Germany | Prospective | 100 | 283 | Magnifying chromoendoscopy | Pit pattern | I/II/IIIS/IIIL/IV/V |
| Kawaguti et al[27] | 2019 | Brazil | Prospective | 121 | 123 | Magnifying chromoendoscopy | Pit pattern | II/IIIS/IIIL/IV/V |
| East et al[28] | 2008 | United Kingdom | Prospective | 62 | 116 | NBI-ME | Pit pattern | I/II/IIIS/IIIL/IV/V |
| Liu et al[29] | 2003 | China | Prospective | 948 | 954 | Magnifying chromoendoscopy | Pit pattern | I/II/IIIL/IIIS/IV/V |
| Kato et al[30] | 2006 | Japan | Prospective | 180 | 210 | Magnifying chromoendoscopy | Pit pattern | Neoplastic/non-neoplastic |
| Van den Broek et al[31] | 2011 | Netherlands | Prospective | 48 | 153 | NBI | Pit pattern | Neoplastic/non-neoplastic |
| Togashi et al[32] | 2009 | Japan | Prospective | 50 | 107 | Magnifying chromoendoscopy | Pit pattern | Neoplastic/non-neoplastic |
| Kiesslich et al[33] | 2003 | Germany | Prospective | 84 | 118 | Magnifying chromoendoscopy | Pit pattern | Neoplastic/non-neoplastic |
| Hurlstone et al[34] | 2005 | United Kingdom | Prospective | 350 | 288 | Magnifying chromoendoscopy | Pit pattern | Neoplastic/non-neoplastic |
| Tischendorf et al[35] | 2007 | Germany | Prospective | 52 | 100 | NBI-ME | Pit pattern | Neoplastic/non-neoplastic |
| Tischendorf et al[35] | 2007 | Germany | Prospective | 47 | 100 | Magnifying chromoendoscopy | Pit pattern | Neoplastic/non-neoplastic |
| Su et al[36] | 2006 | China | Prospective | 79 | 110 | Chromoendoscopy | Pit pattern | Neoplastic/non-neoplastic |
| Dos Santos et al[37] | 2012 | Brazil | Prospective | 69 | 120 | Magnifying chromoendoscopy | Pit pattern | Neoplastic/non-neoplastic |
| Dos Santos et al[38] | 2010 | Brazil | Prospective | 72 | 137 | Magnifying chromoendoscopy | Pit pattern | Neoplastic/non-neoplastic |
| Rogart et al[39] | 2008 | United States | Prospective | 131 | 265 | NBI | Pit pattern | Neoplastic/non-neoplastic |
| Apel et al[40] | 2006 | Germany | Prospective | 158 | 273 | Chromoendoscopy | Pit pattern | Neoplastic/non-neoplastic |
| Van den Broek et al[41] | 2008 | Netherlands | Prospective | 50 | 98 | NBI-ME | Pit pattern | Neoplastic/non-neoplastic |
| Chiu et al[42] | 2007 | China | Prospective | 133 | 180 | Magnifying chromoendoscopy | Pit pattern | Neoplastic/non-neoplastic |
| Liu et al[22] | 2008 | China | Retrospective | 223 | 451 | Magnifying chromoendoscopy | Pit pattern | Neoplastic/non-neoplastic |
In total, 19227 colorectal lesions in 14674 patients were identified in the 31 included studies. Table 3 summarizes the pooled sensitivity, specificity, DOR, and AUC in each category of the JNET and Pit pattern classifications corresponding to the pathological results.
| JNET | Sensitivity | Specificity | DOR | AUC | Pit pattern | Sensitivity | Specificity | DOR | AUC |
| 1 | 0.73 [0.55, 0.85] | 0.99 [0.97, 1.00] | 245 [64, 936] | 0.97 [0.95, 0.98] | II | 0.76 [0.62, 0.86] | 0.96 [0.88, 0.98] | 68 [15, 309] | 0.92 [0.90, 0.94] |
| 2A | 0.88 [0.78, 0.94] | 0.72 [0.64, 0.79] | 19 [11, 33] | 0.84 [0.81, 0.87] | IIIL + IV | 0.80 [0.67, 0.89] | 0.80 [0.74, 0.86] | 17 [8, 34] | 0.87 [0.83, 0.89] |
| 2B | 0.56 [0.47, 0.64] | 0.91 [0.79, 0.96] | 13 [7, 24] | 0.72 [0.68, 0.76] | IIIS + VI-L | 0.45 [0.23, 0.69] | 0.88 [0.75, 0.94] | 6 [1, 26] | 0.79 [0.75, 0.82] |
| 3 | 0.51 [0.42, 0.61] | 1.00 [1.00, 1.00] | 801 [267, 2398] | 0.90 [0.87, 0.93] | VN + VI-H | 0.73 [0.55, 0.85] | 0.99 [0.98, 1.00] | 449 [93, 2182] | 0.98 [0.97, 0.99] |
| Non-neoplastic | 0.73 [0.55, 0.85] | 0.99 [0.97, 1.00] | 245 [64, 936] | 0.97 [0.95, 0.98] | Non-neoplastic | 0.86 [0.81, 0.90] | 0.94 [0.90, 0.96] | 88 [48, 156] | 0.95 [0.93, 0.97] |
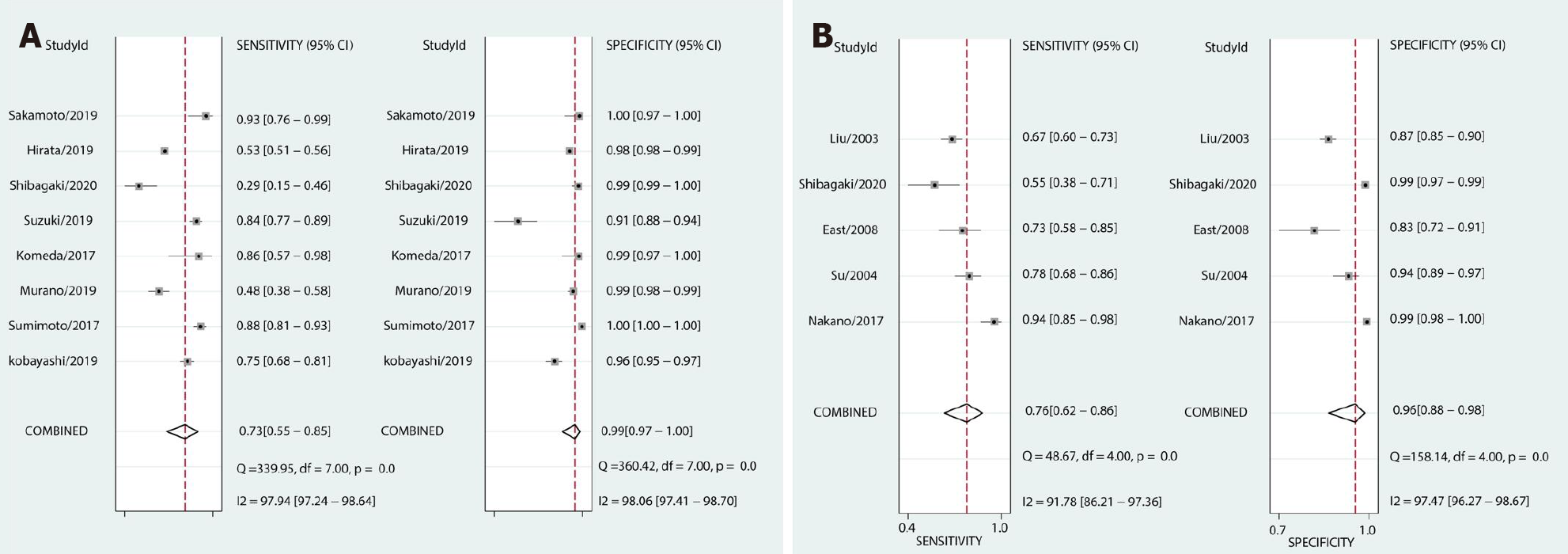
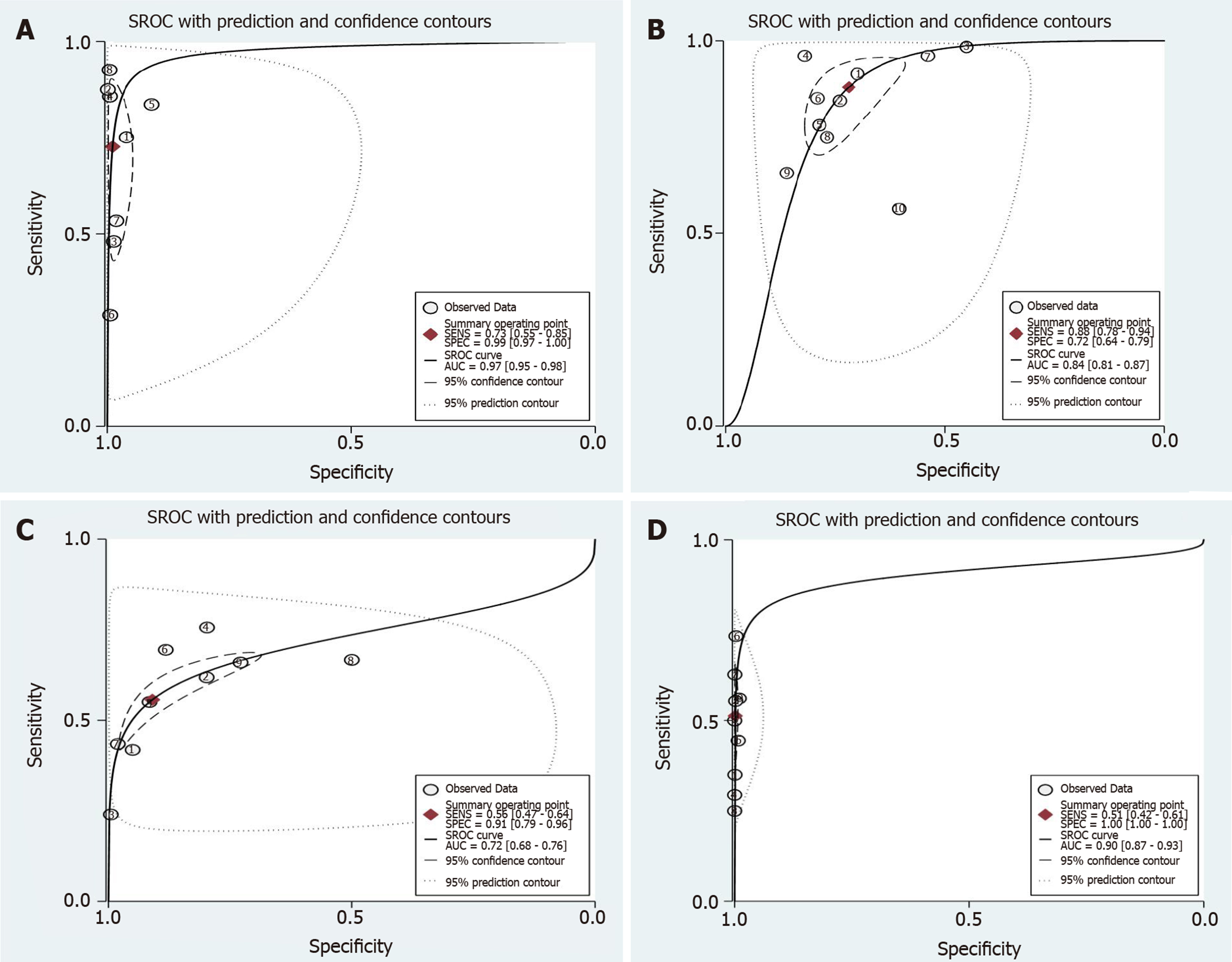
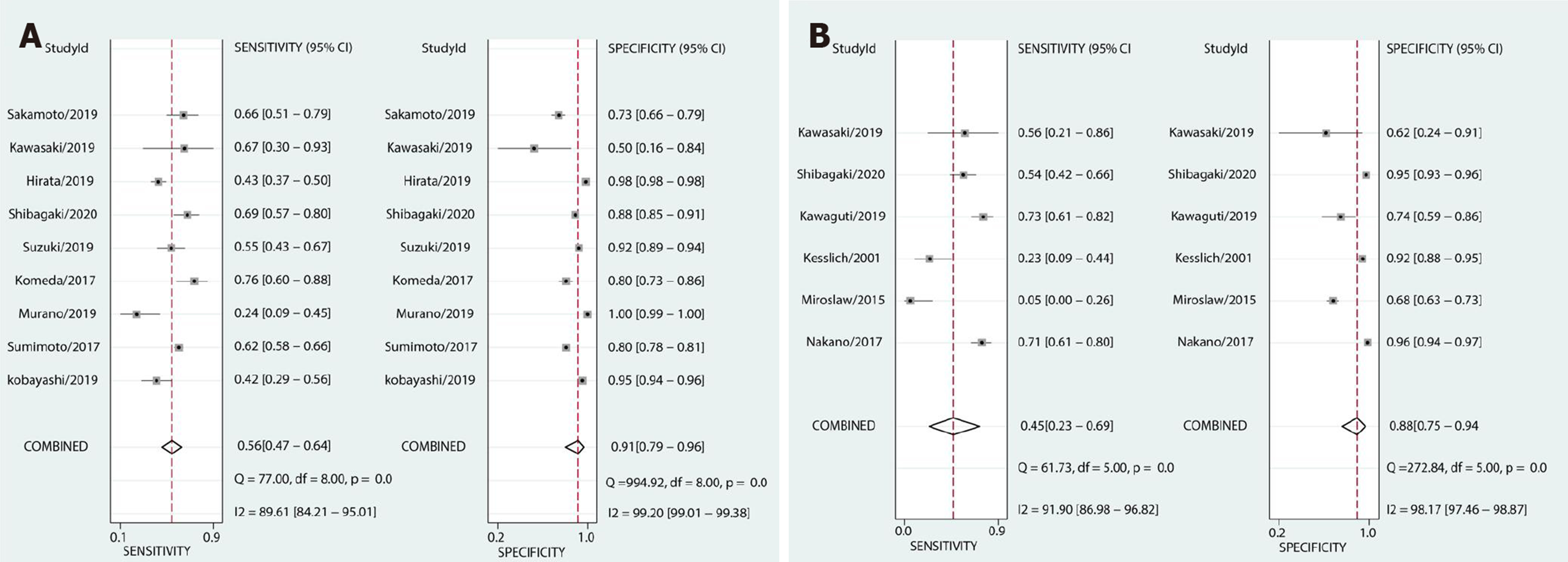
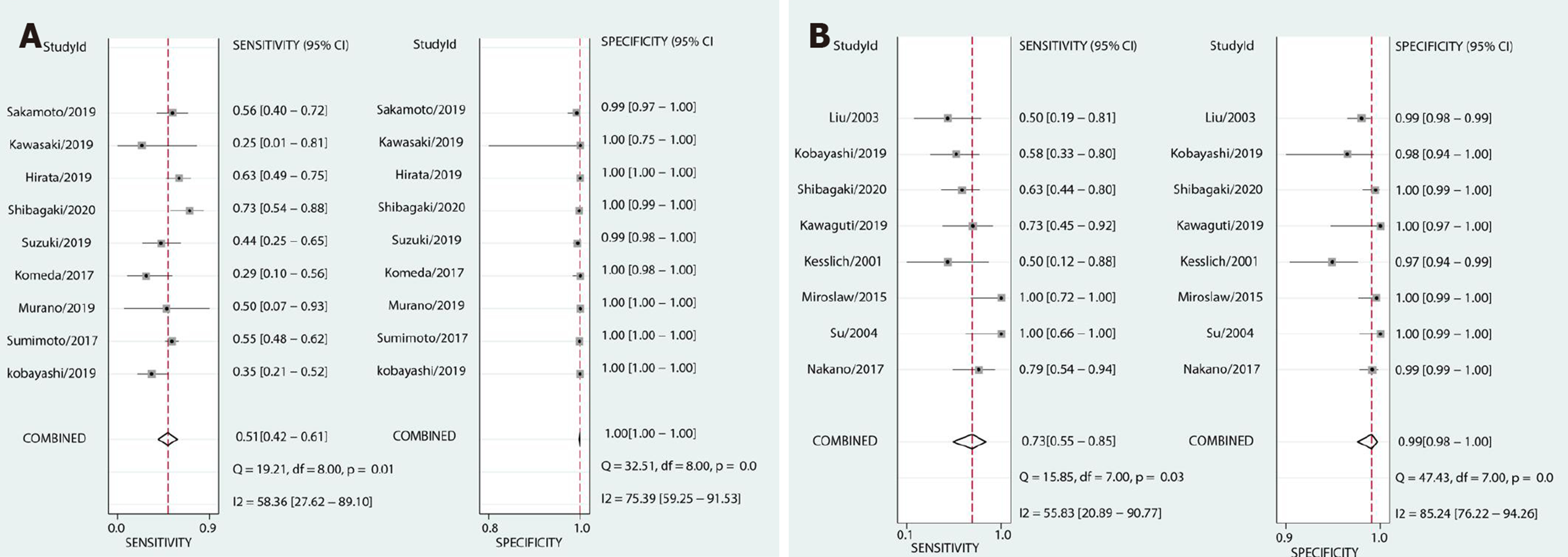
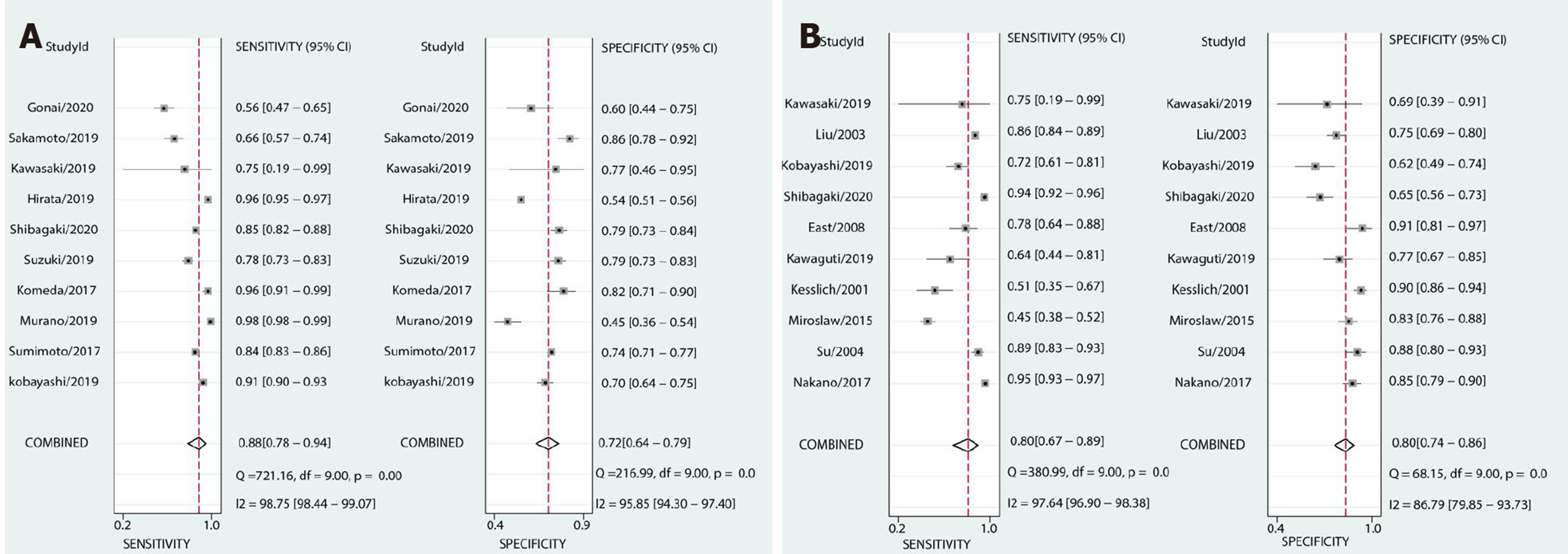
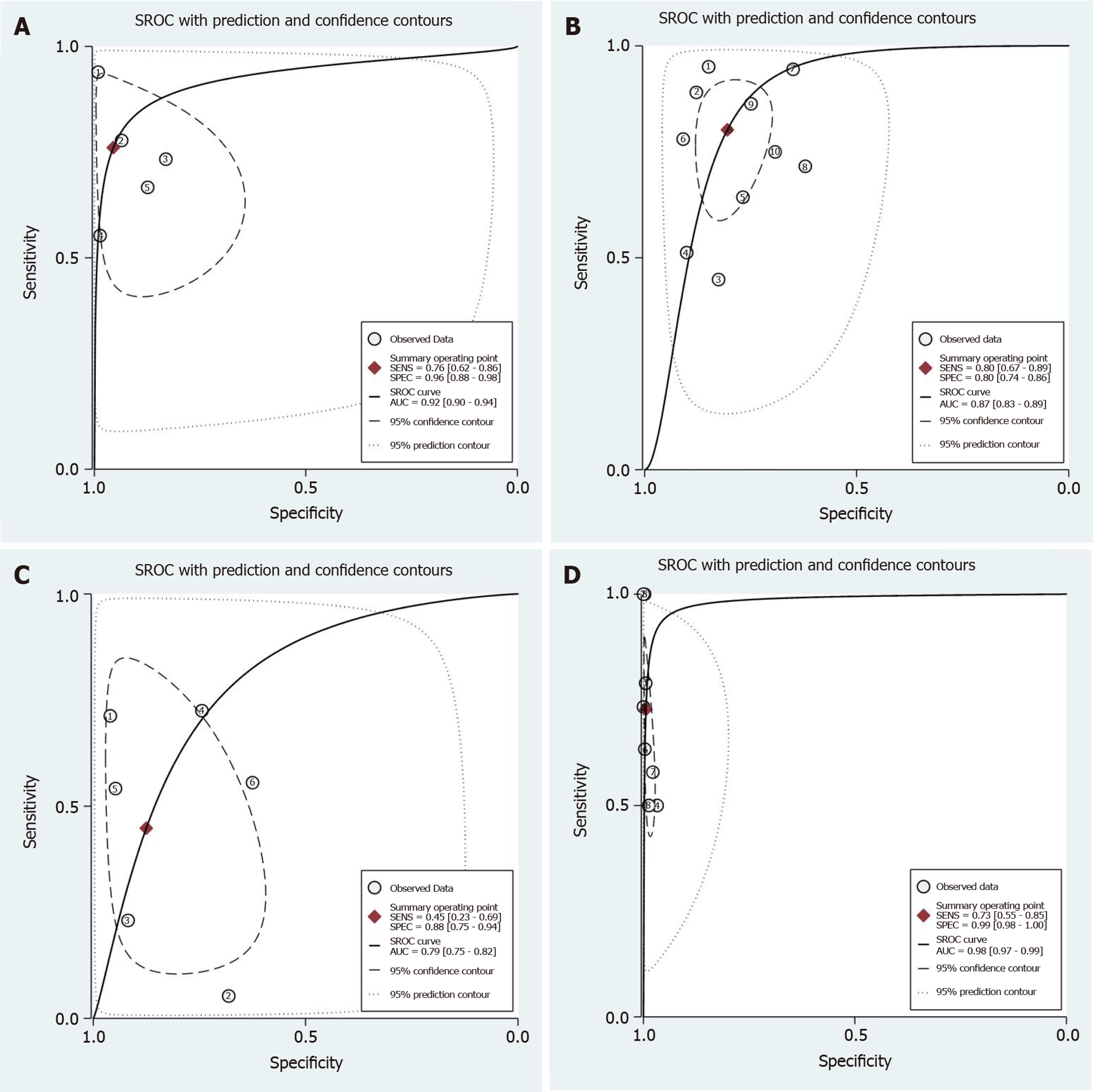
Ten studies[5,13-21] involving 13479 colorectal lesions reported the diagnostic efficacy of the JNET classification. The pooled values for each category were as follows. Type 1 (non-neoplastic): Sensitivity, 0.73 (95%CI: 0.55-0.85); specificity, 0.99 (95%CI: 0.97-1.00) (Figure 3A); DOR, 245 (95%CI: 64-936); and AUC, 0.97 (95%CI: 0.95-0.98) (Figure 4A). Type 2A: sensitivity, 0.88 (95%CI: 0.78-0.94); specificity, 0.72 (95%CI: 0.64-0.79) (Figure 8A); DOR, 19 (95%CI: 11-33); and AUC, 0.84 (95%CI: 0.81-0.87) (Figure 4B). Type 2B: sensitivity, 0.56 (95%CI: 0.47-0.64); specificity, 0.91 (95%CI: 0.79-0.96) (Figure 5A); DOR, 13 (95%CI: 7-24); and AUC, 0.72 (95%CI: 0.68-0.76) (Figure 4C); Type 3: sensitivity, 0.51 (95%CI: 0.42-0.61); specificity, 1.00 (95%CI: 1.00-1.00) (Figure 6A); DOR, 801 (95%CI: 267-2398); and AUC, 0.90 (95%CI: 0.87-0.93) (Figure 4D).
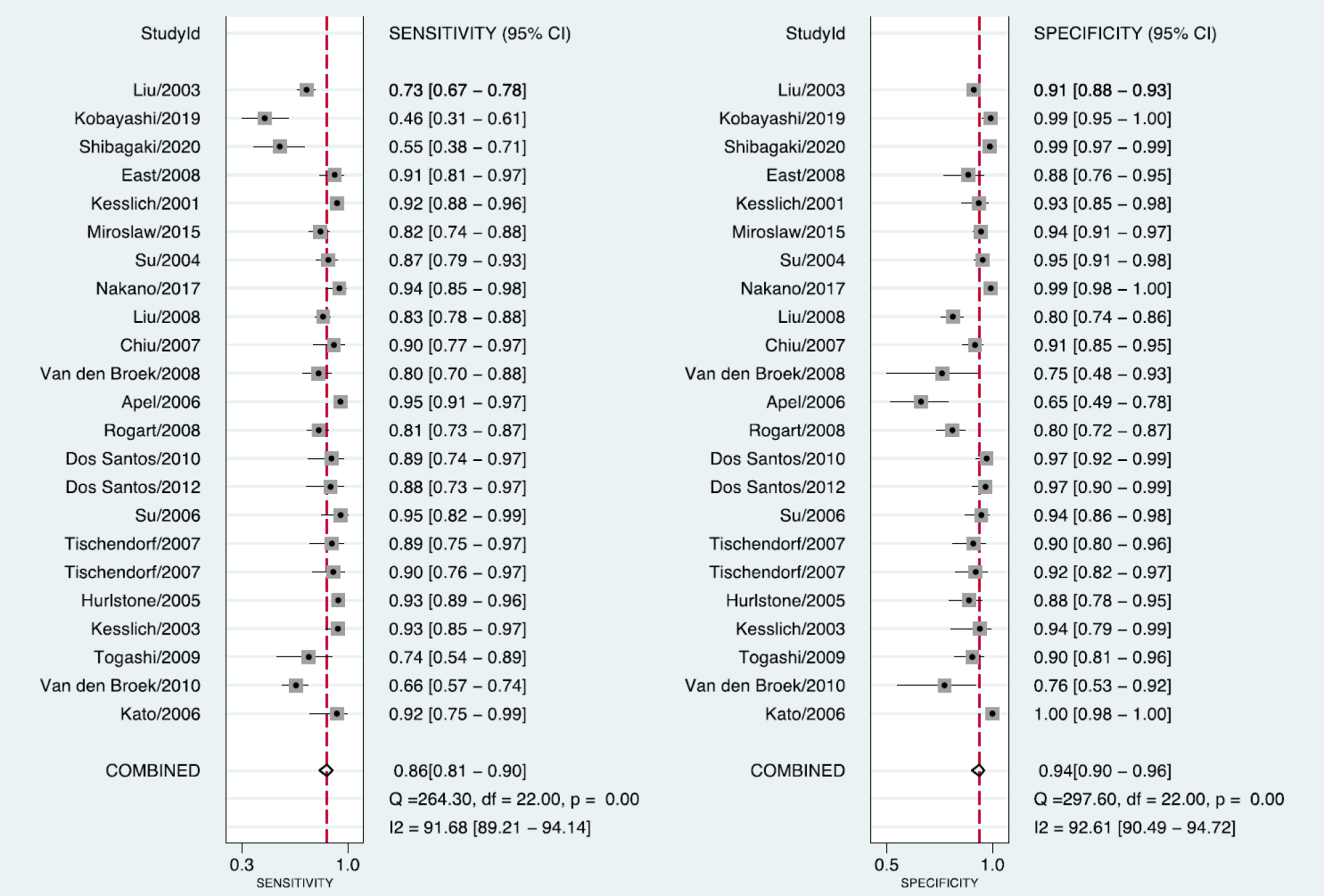
Twenty-one studies[5,13,21-42] involving 6150 colorectal lesions reported the diagnostic value of the Pit pattern classification. The pooled values for each category were as follows. Types I + II (non-neoplastic): sensitivity, 0.86 (95%CI: 0.81-0.90); specificity, 0.94 (95%CI: 0.90-0.96) (Figure 7); DOR, 88 (95%CI: 48-156); and AUC, 0.95 (95%CI: 0.93-0.97) (Figure 9A). Types IIIL + IV: sensitivity, 0.80 (95%CI: 0.67-0.89); specificity, 0.80 (95%CI: 0.74-0.86) (Figure 8B); DOR, 17 (95%CI: 8-34); and AUC, 0.87 (95%CI: 0.83-0.89) (Figure 9B). Types IIIS + VI-L: sensitivity, 0.45 (95%CI: 0.23-0.69); specificity, 0.88 (95%CI: 0.75-0.94) (Figure 5B); DOR, 6 (95%CI: 1-26); and AUC, 0.79 (95%CI: 0.75-0.82) (Figure 9C). Types VN + VI-H: sensitivity, 0.73 (95%CI: 0.55-0.85); specificity, 0.99 (95%CI: 0.98-1.00) (Figure 6B); DOR, 449 (95%CI: 93-2182); and AUC, 0.98 (95%CI: 0.97-0.99) (Figure 9D).
The Student’s t-test was used to compare the sensitivities, specificities, and AUCs of each corresponding category of these two classifications. A statistically significant difference was found in sensitivity between JNET Type 3, and Pit pattern Types VN + VL-H (P < 0.05), however, no significant difference was found in specificity, and AUC. The results showed that no significant differences was found between the remaining categories among sensitivities, specificities, and AUCs: JNET Type 1 (non-neoplastic) vs Pit pattern Types I + II (non-neoplastic), JNET Type 2A vs Pit pattern Types IIIL + IV, and JNET Type 2B vs Pit pattern Types IIIS + VI-L.
Significant heterogeneity existed among the included studies. Estimation of Spearman’s correlation coefficient (coef) and the P-value for each category of the JNET and Pit pattern classifications are shown in Table 4. Significant differences were noted for JNET Type 1 (non-neoplastic) (coef. = 0.14, P = 0.02), JNET Type 3 (coef. = -0.17, P = 0.03), and Pit pattern Types I + II (non-neoplastic) (coef. = -0.12, P = 0.02), while for the remaining subtypes of these two classifications, there were no significant differences. These results indicated the threshold effect existed in JNET Types 1, 3, and Pit pattern Types I + II. Additionally, for the non-threshold effect, we performed meta-regression analysis, including the population in the study (Asian or non-Asian), design of the study (retrospective or prospective), patient sample size (≥ 100 or < 100), QUADAS-2 score (≥ 7 or < 7), publication year (before, or after 2014), as well as the type of endoscopy as covariates. The sources of potential heterogeneity in the sensitivity and specificity were detected by univariate regression analysis, and the results are shown in Table 5. Deeks’ Funnel Plot Asymmetry Test revealed no publication bias in each category of these two classifications (Table 6).
| JNET (type) | Coef | P value | Pit pattern (type) | Coef | P value |
| Non-neoplastic | -0.12 | 0.02 | |||
| Type 1 (Non-neoplastic) | 0.14 | 0.02 | II | 0.45 | 0.20 |
| Type 2A | -0.70 | 0.49 | IIIL + IV | -0.24 | 0.06 |
| Type 2B | -1.00 | 1.00 | IIIS + VI-L | 0.41 | 0.17 |
| Type 3 | -0.17 | 0.03 | VN + VI-H | 1.00 | 1.00 |
| Classification | Type | P value | ||||||
| Prodesign | Sampsize | Qscore | Endoscopy | Category | Country | Pubyear | ||
| JNET | Type 1 | 0.26 | 0.63 | 0.06 | ||||
| Type 2A | 0.88 | 0.58 | 0.76 | 0.00 | ||||
| Type 2B | ||||||||
| Type 3 | 0.57 | 0.12 | 0.19 | |||||
| Pit pattern | II | 0.52 | 0.00 | 0.04 | 0.35 | 0.00 | ||
| IIIL + IV | 0.63 | 0.77 | 0.41 | 0.33 | 0.77 | 0.00 | 0.09 | |
| IIIS + VI-L | 0.35 | 0.35 | 0.66 | 0.35 | 0.35 | 0.21 | 0.02 | |
| VN + VI-H | ||||||||
| Non-neoplastic | 0.49 | 0.60 | 0.04 | 0.52 | 0.05 | 0.03 | 0.00 | |
| JNET (type) | n of study | Pubbias (P value) | Pit pattern (type) | No. of study | Pubbias (P value) |
| Type 1 | 8 | 0.26 | II | 5 | 0.54 |
| Type 2A | 10 | 0.62 | IIIL + IV | 10 | 0.41 |
| Type 2B | 9 | 0.52 | IIIS + VI-L | 6 | 0.09 |
| Type 3 | 9 | 0.50 | VN + VI-H | 8 | 0.91 |
| Non-neoplastic | 8 | 0.26 | Non-neoplastic | 23 | 0.13 |
To best of our knowledge, no meta-analysis has been reported that systematically compared the diagnostic efficacy of detailed histologic characteristics and interobserver diagnostic agreements between the JNET and Pit pattern classifications. The present meta-analysis compared and evaluated the diagnostic outcomes of each category of these two classifications corresponding to the histological diagnosis. Our results revealed that the diagnostic performance of the JNET classification is equivalent to the Pit pattern classification in each corresponding category. We also proposed a treatment strategy for colorectal lesions using the JNET classification with its confidence level.
Endoscopic diagnosis via magnification colonoscopy has been reported to provide high diagnostic accuracy and improve the prognosis of colorectal lesions. The Pit pattern classification is the most frequently used criteria for the accurate diagnosis of colorectal neoplasms. To date, several trials[5,13-21] have evaluated the efficacy of the JNET classification, which provides useful criteria for optical-histologic diagnoses of colorectal lesions. Whereas, JNET Types 1 and 2A correspond to Pit pattern Types I + II, and Type IIIL + IV, respectively; JNET Type 2B and 3 correspond to Pit pattern Types IIIS + VI-L and VI-H + VN, respectively. However, there are some differences between the JNET classification and Pit pattern classification. The Pit pattern classification is only based on the surface structure of lesions, while the JNET classification is based on the surface structure combined with the microvascular structure of lesions. In addition, the JNET classification is more concise in terms of guiding appropriate treatment strategies. According to our proposed treatment strategy, most JNET Type 1 lesions are HPs, which generally do not require resection and could be followed up by endoscopy. However, whether using the JNET classification or Pit pattern classification, it is difficult to distinguish between HP and SSL with endoscopy. Endoscopic resection is also recommended if the colorectal lesion is large or tends to enlarge obviously with endoscopy follow-up. Type 2A lesions could be resected by polypectomy or endoscopic mucosal resection (EMR). Type 2B lesions should be resected en bloc by endoscopic submucosal dissection (ESD) to obtain a precise histologic diagnosis concerning the invasion depth and determine endoscopic curability. If the lesion is relatively small, EMR is also recommended. Lastly, surgical resection is recommended for Type 3 lesions. However, few studies[5,13-21] have been published that have used the JNET classification for treatment of colorectal lesions in practice.
The JNET Type 1 is considered to have as high diagnostic efficacy as the Pit pattern Type II, moreover, no significant difference was found between these categories in this meta-analysis, which implies that the magnification technology could accurately distinguish non-neoplastic from neoplastic lesions and guide clinicians to formulate the appropriate treatment.
In this study, JNET Type 2B had a relatively low pooled sensitivity and AUC of 0.56 and 0.72, respectively. Interestingly, similar results were also obtained for Pit pattern Types IIIS + VI-L, with a sensitivity of 0.45 and AUC of 0.79. Through data analysis, it was found that, in these two categories, the evaluation regarding the dysplasia of some lesions was too low, or the depth of invasion was too shallow. Firstly, one reason might be that a large lesion often contained several pathological features, for example, a lesion contained two or more histological features of HGD, SM-s carcinoma, and SM-d carcinoma at the same time. Most of the surface structures showed the features of HGD, or SM-s carcinoma, while, only a focal, or the deep part of these lesions showed the features of SM-d carcinoma; therefore, the lesions were identified as Type 2B. Secondly, due to the large size, or the special location of the lesions, the endoscopist might be unable to observe the full picture of these lesions, which might be one reason for the low sensitivity. In addition, due to the spontaneous or contact bleeding of some large lesions, the blood might be attached to the surface of the lesions and then affect the judgment of pathological Types. Therefore, for large lesions, special location lesions and pedicled lesions, endoscopists are required to observe carefully, to obtain the whole picture of the lesions, and make a comprehensive judgement, which might be helpful in improving sensitivity.
Generally, SM-d carcinomas correspond to JNET Type 3. Our meta-analysis showed that JNET Type 3 has a lower sensitivity than that of Pit pattern Type VN + VL-H. Some polypoid advanced lesions could have a slightly less irregular NBI appearance than Type 3 because the surface microvillous structure persisted, which might be classified into JNET Type 2B. Thus, it has been proposed that Type 2B can be divided into two subtypes, Type 2B-low, and Type 2B-high[14]. The classification subtypes help to optimize the choice of treatment strategies, which also indicates that the JNET classification may need to be updated and optimized by experts to further improve the sensitivity of diagnosis. In addition, two studies[5,14] suggested that the endoscopist needed to perform an additional Pit pattern diagnosis using chromoendoscopy to differentiate Type 2B from Type 3, which might help to improve sensitivity; however, this requires further validation. In terms of specificity, compared with the Pit pattern classification, the overall JNET types were slightly higher, which was attributed to the evaluation of vessel structure by NBI-ME.
There are several limitations to this meta-analysis. First, the high degree of statistical heterogeneity with a high I2 value could not be avoided. The quality of endoscopic images, type of endoscopy, size of the population, year of publication, and experience of the endoscopists (expert or non-expert) possibly affected the heterogeneity of the included studies. For the Pit pattern classification, chemical staining magnifications were used in most of the included studies, but several studies used electronic staining magnification, and a few studies also used non-magnifying technology, which might have affected the results. Second, previous studies of the JNET classification were all retrospective single-center studies and the included populations were all Japanese. This indicates a potential need for large-scale prospective multi-center validation studies of the JNET classification in the future. Additionally, it is better to compare the JNET classification with the Pit pattern classification in the same endoscopic and histopathologic center.
In conclusion, this meta-analysis has shown that the diagnostic efficacy of the JNET classification is equivalent to that of the Pit pattern classification as both classifications are divided into four major categories according to similar histopathology. The sensitivity of JNET Type 2B can be further improved by differentiating subtypes and combining it with the Pit pattern classification. Due to its simpler and clearer application, it is easier to guide the choice of treatment strategy, which suggests that we can promote the application of the JNET classification for colorectal lesions in the clinic. However, future prospective multi-center studies with a uniform endoscopic and histopathology protocol are required to validate our results.
The Pit pattern classification using magnifying chromoendoscopy is the established and traditional choice for diagnosing colorectal lesions. The Japan Narrow-band imaging (NBI) Expert Team (JNET) classification is a novel NBI magnifying endoscopic classification, which focuses on vessel and surface patterns to diagnose colorectal lesions. However, the comparative diagnostic efficacy of the JNET classification is inconclusive.
Several studies have proposed that the JNET classification of colorectal lesions via NBI magnifying endoscopy is a useful and objective tool for differentiating the gross type of colorectal lesions. However, to what extent we can trust the results of the JNET classification, and whether the Pit pattern classification can be replaced by the JNET classification are aspects that remain unclear.
To perform a systematic review and meta-analysis on the diagnostic efficacy of each category of the JNET and Pit pattern classifications for colorectal lesions.
A systematic literature search was performed using PubMed, Embase, the Cochrane Library and Web of Science. The pooled sensitivity, specificity, diagnostic odds ratio, and area under the curve (AUC) of each category of the JNET and Pit pattern classifications were calculated.
A total of 19227 colorectal lesions in 31 studies were included. The diagnostic performance of the JNET classification was equivalent to the Pit pattern classification in each corresponding category. The pooled sensitivity, specificity, and AUC for each category of the JNET classification were as follows: 0.73 (95%CI: 0.55-0.85), 0.99 (95%CI: 0.97-1.00), and 0.97 (95%CI: 0.95-0.98), respectively, for Type 1; 0.88 (95%CI: 0.78-0.94), 0.72 (95%CI: 0.64-0.79), and 0.84 (95%CI: 0.81-0.87), respectively, for Type 2A; 0.56 (95%CI: 0.47-0.64), 0.91 (95%CI: 0.79-0.96), and 0.72 (95%CI: 0.68-0.76), respectively, for Type 2B; 0.51 (95%CI: 0.42-0.61), 1.00 (95%CI: 1.00-1.00), and 0.90 (95%CI: 0.87-0.93), respectively, for Type 3.
Our study found that the diagnostic efficacy of the JNET classification is equivalent to that of the Pit pattern classification as both classifications are divided into four major categories according to similar histopathology.
The JNET classification is easier for guiding the choice of treatment strategy, which suggests that we can promote the application of the JNET classification for colorectal lesions in the clinic. However, future prospective multi-center studies with uniform endoscopic and histopathology protocol are required to validate our results.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chiba H S-Editor: Yan JP L-Editor: Webster JR P-Editor: Liu JH
| 1. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 55814] [Article Influence: 7973.4] [Reference Citation Analysis (132)] |
| 2. | Lin JS, Piper MA, Perdue LA, Rutter CM, Webber EM, O'Connor E, Smith N, Whitlock EP. Screening for Colorectal Cancer: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2016;315:2576-2594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 598] [Cited by in RCA: 558] [Article Influence: 62.0] [Reference Citation Analysis (0)] |
| 3. | Tanaka S, Kashida H, Saito Y, Yahagi N, Yamano H, Saito S, Hisabe T, Yao T, Watanabe M, Yoshida M, Kudo SE, Tsuruta O, Sugihara KI, Watanabe T, Saitoh Y, Igarashi M, Toyonaga T, Ajioka Y, Ichinose M, Matsui T, Sugita A, Sugano K, Fujimoto K, Tajiri H. JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2015;27:417-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 359] [Cited by in RCA: 436] [Article Influence: 43.6] [Reference Citation Analysis (0)] |
| 4. | Kudo S, Tamura S, Nakajima T, Yamano H, Kusaka H, Watanabe H. Diagnosis of colorectal tumorous lesions by magnifying endoscopy. Gastrointest Endosc. 1996;44:8-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 721] [Cited by in RCA: 708] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 5. | Kobayashi S, Yamada M, Takamaru H, Sakamoto T, Matsuda T, Sekine S, Igarashi Y, Saito Y. Diagnostic yield of the Japan NBI Expert Team (JNET) classification for endoscopic diagnosis of superficial colorectal neoplasms in a large-scale clinical practice database. United European Gastroenterol J. 2019;7:914-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 75] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 6. | Tanaka S, Sano Y. Aim to unify the narrow band imaging (NBI) magnifying classification for colorectal tumors: current status in Japan from a summary of the consensus symposium in the 79th Annual Meeting of the Japan Gastroenterological Endoscopy Society. Dig Endosc. 2011;23 Suppl 1:131-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 96] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 7. | Sano Y, Tanaka S, Kudo SE, Saito S, Matsuda T, Wada Y, Fujii T, Ikematsu H, Uraoka T, Kobayashi N, Nakamura H, Hotta K, Horimatsu T, Sakamoto N, Fu KI, Tsuruta O, Kawano H, Kashida H, Takeuchi Y, Machida H, Kusaka T, Yoshida N, Hirata I, Terai T, Yamano HO, Kaneko K, Nakajima T, Sakamoto T, Yamaguchi Y, Tamai N, Nakano N, Hayashi N, Oka S, Iwatate M, Ishikawa H, Murakami Y, Yoshida S, Saito Y. Narrow-band imaging (NBI) magnifying endoscopic classification of colorectal tumors proposed by the Japan NBI Expert Team. Dig Endosc. 2016;28:526-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 455] [Cited by in RCA: 402] [Article Influence: 44.7] [Reference Citation Analysis (1)] |
| 8. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6253] [Cited by in RCA: 7636] [Article Influence: 477.3] [Reference Citation Analysis (1)] |
| 9. | Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM; QUADAS-2 Group. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6953] [Cited by in RCA: 9570] [Article Influence: 683.6] [Reference Citation Analysis (0)] |
| 10. | DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26739] [Cited by in RCA: 30408] [Article Influence: 779.7] [Reference Citation Analysis (0)] |
| 11. | Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch V. Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from: https://training.cochrane.org/cochrane-handbook-systematic-reviews-interventions#how-to-access. |
| 12. | Moses LE, Shapiro D, Littenberg B. Combining independent studies of a diagnostic test into a summary ROC curve: data-analytic approaches and some additional considerations. Stat Med. 1993;12:1293-1316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 983] [Cited by in RCA: 1021] [Article Influence: 31.9] [Reference Citation Analysis (0)] |
| 13. | Shibagaki K, Ishimura N, Yuki T, Taniguchi H, Aimi M, Kobayashi K, Kotani S, Yazaki T, Yamashita N, Tamagawa Y, Mishiro T, Ishihara S, Yasuda A, Kinshita Y. Magnification endoscopy in combination with acetic acid enhancement and narrow-band imaging for the accurate diagnosis of colonic neoplasms. Endosc Int Open. 2020;8:E488-E497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Sumimoto K, Tanaka S, Shigita K, Hayashi N, Hirano D, Tamaru Y, Ninomiya Y, Oka S, Arihiro K, Shimamoto F, Yoshihara M, Chayama K. Diagnostic performance of Japan NBI Expert Team classification for differentiation among noninvasive, superficially invasive, and deeply invasive colorectal neoplasia. Gastrointest Endosc. 2017;86:700-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 59] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 15. | Murano T, Ikematsu H, Shinmura K, Ito R, Minamide T, Sato D, Yamamoto Y, Takashima K, Kadota T, Yoda Y, Hori K, Oono Y, Yano T. Endoscopic prediction of advanced histology in colorectal lesions sized <10 mm using the Japan Narrow-band imaging Expert Team classification. Dig Endosc. 2019;32:785-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (2)] |
| 16. | Komeda Y, Kashida H, Sakurai T, Asakuma Y, Tribonias G, Nagai T, Kono M, Minaga K, Takenaka M, Arizumi T, Hagiwara S, Matsui S, Watanabe T, Nishida N, Chikugo T, Chiba Y, Kudo M. Magnifying Narrow Band Imaging (NBI) for the Diagnosis of Localized Colorectal Lesions Using the Japan NBI Expert Team (JNET) Classification. Oncology. 2017;93 Suppl 1:49-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 63] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 17. | Suzuki H, Yamamura T, Nakamura M, Hsu CM, Su MY, Chen TH, Chiu CT, Hirooka Y, Goto H. An International Study on the Diagnostic Accuracy of the Japan Narrow-Band Imaging Expert Team Classification for Colorectal Polyps Observed with Blue Laser Imaging. Digestion. 2020;101:339-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Hirata D, Kashida H, Iwatate M, Tochio T, Teramoto A, Sano Y, Kudo M. Effective use of the Japan Narrow Band Imaging Expert Team classification based on diagnostic performance and confidence level. World J Clin Cases. 2019;7:2658-2665. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Sakamoto T, Takamaru H, Sekiguchi M, Yamada M, Matsuda T, Saito Y. Reliability of Japan Narrow-Band Imaging Expert Team Classification for the Diagnosis of Colorectal Neoplasms: A Pilot Study. Digestion. 2019;1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Gonai T, Kawasaki K, Nakamura S, Yanai S, Akasaka R, Sato K, Toya Y, Asakura K, Urushikubo J, Fujita Y, Eizuka M, Uesugi N, Sugai T, Matsumoto T. Microvascular density under magnifying narrow-band imaging endoscopy in colorectal epithelial neoplasms. Intest Res. 2020;18:107-114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Kawasaki K, Nakamura S, Esaki M, Kurahara K, Eizuka M, Nuki Y, Kochi S, Fujiwara M, Oshiro Y, Sugai T, Matsumoto T. Clinical usefulness of magnifying colonoscopy for the diagnosis of ulcerative colitis-associated neoplasia. Dig Endosc. 2019;31 Suppl 1:36-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Liu YX, Huang LY, Bian XP, Cui J, Xu N, Wu CR. Fuji Intelligent Chromo Endoscopy and staining technique for the diagnosis of colon tumor. Chin Med J (Engl). 2008;121:977-982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | Nakano A, Hirooka Y, Yamamura T, Watanabe O, Nakamura M, Funasaka K, Ohno E, Kawashima H, Miyahara R, Goto H. Comparison of the diagnostic ability of blue laser imaging magnification versus pit pattern analysis for colorectal polyps. Endosc Int Open. 2017;5:E224-E231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 24. | Szura M, Pasternak A, Bucki K, Urbańczyk K, Matyja A. Two-stage optical system for colorectal polyp assessments. Surg Endosc. 2016;30:204-214. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 25. | Su MY, Ho YP, Chen PC, Chiu CT, Wu CS, Hsu CM, Tung SY. Magnifying endoscopy with indigo carmine contrast for differential diagnosis of neoplastic and nonneoplastic colonic polyps. Dig Dis Sci. 2004;49:1123-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 48] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 26. | Kiesslich R, von Bergh M, Hahn M, Hermann G, Jung M. Chromoendoscopy with indigocarmine improves the detection of adenomatous and nonadenomatous lesions in the colon. Endoscopy. 2001;33:1001-1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 158] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 27. | Kawaguti FS, Franco MC, Martins BC, Segateli V, Marques CFS, Nahas CSR, Pinto RA, Safatle-Ribeiro AV, Ribeiro-Junior U, Nahas SC, Maluf-Filho F. Role of Magnification Chromoendoscopy in the Management of Colorectal Neoplastic Lesions Suspicious for Submucosal Invasion. Dis Colon Rectum. 2019;62:422-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 28. | East JE, Suzuki N, Bassett P, Stavrinidis M, Thomas HJ, Guenther T, Tekkis PP, Saunders BP. Narrow band imaging with magnification for the characterization of small and diminutive colonic polyps: pit pattern and vascular pattern intensity. Endoscopy. 2008;40:811-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 99] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 29. | Liu HH, Kudo SE, Juch JP. Pit pattern analysis by magnifying chromoendoscopy for the diagnosis of colorectal polyps. J Formos Med Assoc. 2003;102:178-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Kato S, Fu KI, Sano Y, Fujii T, Saito Y, Matsuda T, Koba I, Yoshida S, Fujimori T. Magnifying colonoscopy as a non-biopsy technique for differential diagnosis of non-neoplastic and neoplastic lesions. World J Gastroenterol. 2006;12:1416-1420. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 63] [Cited by in RCA: 52] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 31. | van den Broek FJ, Fockens P, van Eeden S, Stokkers PC, Ponsioen CY, Reitsma JB, Dekker E. Narrow-band imaging versus high-definition endoscopy for the diagnosis of neoplasia in ulcerative colitis. Endoscopy. 2011;43:108-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 131] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 32. | Togashi K, Osawa H, Koinuma K, Hayashi Y, Miyata T, Sunada K, Nokubi M, Horie H, Yamamoto H. A comparison of conventional endoscopy, chromoendoscopy, and the optimal-band imaging system for the differentiation of neoplastic and non-neoplastic colonic polyps. Gastrointest Endosc. 2009;69:734-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 65] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 33. | Kiesslich R, Fritsch J, Holtmann M, Koehler HH, Stolte M, Kanzler S, Nafe B, Jung M, Galle PR, Neurath MF. Methylene blue-aided chromoendoscopy for the detection of intraepithelial neoplasia and colon cancer in ulcerative colitis. Gastroenterology. 2003;124:880-888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 616] [Cited by in RCA: 557] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 34. | Hurlstone DP, Sanders DS, Lobo AJ, McAlindon ME, Cross SS. Indigo carmine-assisted high-magnification chromoscopic colonoscopy for the detection and characterisation of intraepithelial neoplasia in ulcerative colitis: a prospective evaluation. Endoscopy. 2005;37:1186-1192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 185] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 35. | Tischendorf JJ, Wasmuth HE, Koch A, Hecker H, Trautwein C, Winograd R. Value of magnifying chromoendoscopy and narrow band imaging (NBI) in classifying colorectal polyps: a prospective controlled study. Endoscopy. 2007;39:1092-1096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 155] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 36. | Su MY, Hsu CM, Ho YP, Chen PC, Lin CJ, Chiu CT. Comparative study of conventional colonoscopy, chromoendoscopy, and narrow-band imaging systems in differential diagnosis of neoplastic and nonneoplastic colonic polyps. Am J Gastroenterol. 2006;101:2711-2716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 185] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 37. | Dos Santos CE, Malaman D, Lopes CV, Pereira-Lima JC, Parada AA. Digital chromoendoscopy for diagnosis of diminutive colorectal lesions. Diagn Ther Endosc. 2012;2012:279521. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 38. | dos Santos CE, Lima JC, Lopes CV, Malaman D, Salomão AD, Garcia AC, Teixeira CR. Computerized virtual chromoendoscopy versus indigo carmine chromoendoscopy combined with magnification for diagnosis of small colorectal lesions: a randomized and prospective study. Eur J Gastroenterol Hepatol. 2010;22:1364-1371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 39. | Rogart JN, Jain D, Siddiqui UD, Oren T, Lim J, Jamidar P, Aslanian H. Narrow-band imaging without high magnification to differentiate polyps during real-time colonoscopy: improvement with experience. Gastrointest Endosc. 2008;68:1136-1145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 95] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 40. | Apel D, Jakobs R, Schilling D, Weickert U, Teichmann J, Bohrer MH, Riemann JF. Accuracy of high-resolution chromoendoscopy in prediction of histologic findings in diminutive lesions of the rectosigmoid. Gastrointest Endosc. 2006;63:824-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 41. | van den Broek FJ, Fockens P, van Eeden S, Reitsma JB, Hardwick JC, Stokkers PC, Dekker E. Endoscopic tri-modal imaging for surveillance in ulcerative colitis: randomised comparison of high-resolution endoscopy and autofluorescence imaging for neoplasia detection; and evaluation of narrow-band imaging for classification of lesions. Gut. 2008;57:1083-1089. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 193] [Cited by in RCA: 190] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 42. | Chiu HM, Chang CY, Chen CC, Lee YC, Wu MS, Lin JT, Shun CT, Wang HP. A prospective comparative study of narrow-band imaging, chromoendoscopy, and conventional colonoscopy in the diagnosis of colorectal neoplasia. Gut. 2007;56:373-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 242] [Article Influence: 13.4] [Reference Citation Analysis (0)] |