Published online Oct 14, 2020. doi: 10.3748/wjg.v26.i38.5884
Peer-review started: May 28, 2020
First decision: July 29, 2020
Revised: August 11, 2020
Article in press: September 11, 2020
Published online: October 14, 2020
Processing time: 139 Days and 3.2 Hours
Bowel ultrasound and magnetic resonance enterography (MRE) are decisive medical imaging modalities for diagnosing and locating bowel lesions with its extramural extent and complications. They assess the degree of activity, help clinicians to identify patients in need of surgery, and can be used for patient follow-up.
To compare the role of MRE and bowel ultrasound in diagnosis and follow-up of inflammatory bowel disease (IBD) patients in Egypt.
The study was conducted on 40 patients with IBD. All patients were subjected to clinical assessment, laboratory investigations, bowel ultrasound, MRE, and colonoscopy up to the terminal ileum with biopsies for histopathological examination.
This study was conducted on 14 patients (35%) with ulcerative colitis and 26 patients (65%) with Crohn's disease; 34 (85%) of these patients had active disease. Bowel ultrasound detected different bowel lesions with the following accuracies: ileum (85%), large bowel (70%), fistula (95%), stricture and proximal dilatation (95%) and abscesses (100%). Also, it showed that statistically significance of bowel ultrasound in differentiation between remission and activity of IBD in comparison to MRE and colonoscopy.
In comparison to MRE, bowel ultrasound is a useful, non-invasive, and feasible bedside imaging tool for the detection of inflammation, detection of complications, and follow-up of IBD patients when performed by the attending physician.
Core Tip: Crohn’s disease and ulcerative colitis are chronic, relapsing inflammatory bowel diseases (IBD). Medical imaging is decisive for diagnosis bowel lesions with its complications. Magnetic resonance enterography (MRE) is one of these imaging techniques. Also, bowel ultrasound is becoming progressively important in management of IBD. Our aim of work in our study is to compare between the role of MRE and bowel ultrasound in diagnosis and follow up of Egyptian IBD patients.
- Citation: Kamel S, Sakr M, Hamed W, Eltabbakh M, Askar S, Bassuny A, Hussein R, Elbaz A. Comparative study between bowel ultrasound and magnetic resonance enterography among Egyptian inflammatory bowel disease patients. World J Gastroenterol 2020; 26(38): 5884-5895
- URL: https://www.wjgnet.com/1007-9327/full/v26/i38/5884.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i38.5884
Crohn’s disease and ulcerative colitis are chronic, relapsing inflammatory bowel diseases (IBD). Medical imaging is decisive for diagnosis and locating the bowel lesion with its extramural extent and complications. It assesses its degree of activity, assigning patients in need for surgery and can be used for their follow-up.
Magnetic resonance enterography (MRE) is one specific imaging technique for such diseases[1]. T2W and T1W images after intravenous gadolinium have high accuracy for diagnosis and assessment of disease activity[2].
Bowel ultrasound is also becoming progressively important in IBD management. Ultrasonography is a noninvasive, non-radiating, cheap, and very available technique that is acceptable and tolerated by patients and can be used repeatedly for follow-up examinations. Ultrasonography for these patients needs higher frequency linear array probes (5-15 MHz) for assessment of the five-layer wall of the bowel[3].
Up until now, no previous comparative studies between bowel ultrasound and MRE for Egyptian patients who suffered/are suffering from IBD, either ulcerative colitis or Crohn’s disease, have been published.
Our study enrolled 40 patients who presented to our IBD center at Ain Shams University Hospital during the period from September 2017 to September 2018.
The study was approved by the medical ethics committee of Ain Shams University. The study population included adolescents who were over 18 years old. All patients provided written informed consent before enrollment. Patients were excluded if they had severe or uncontrolled comorbidities, such as cardio-respiratory, neurological, metabolic, liver, kidney diseases, claustrophobia, cardiac pacemaker, or implanted metal objects that prohibited use of MRE.
All patients reported a complete medical history, underwent thorough clinical examinations and laboratory investigations, including complete blood count, liver profile tests, renal profile tests, C-reactive protein, erythrocyte sedimentation rate, MRE, bowel ultrasound, and colonoscopy up to the terminal ileum with biopsies for histopathological examination.
Clinical activity score for Crohn's disease was assessed by The Crohn’s Disease Activity Index (CDAI). Clinical remission was determined if CDAI was < 150 points or no fistula drainage was found as assessed by the Fistula Drainage Assessment index[4]. Ulcerative colitis activity was assessed using the Truelove and Witts classification based on clinical and laboratory parameters, such as fever, frequency of bowel movements, rectal bleeding, tachycardia, anemia, and elevated erythrocyte sedimentation rate[5].
Colonoscopies were performed with a videoscope system from Olympus Exera II CV-180 after colonic preparation and fasting for six hours.
Bowel ultrasound was done by one examiner who had performed several previous general ultrasound examinations. This examiner was trained for several bowel ultrasound exams under supervision of an ultrasound gastroenterologist specialist at Sacco Hospital, Italy. Bowel ultrasound assessment was reviewed blindly compared to MRE and colonoscopy.
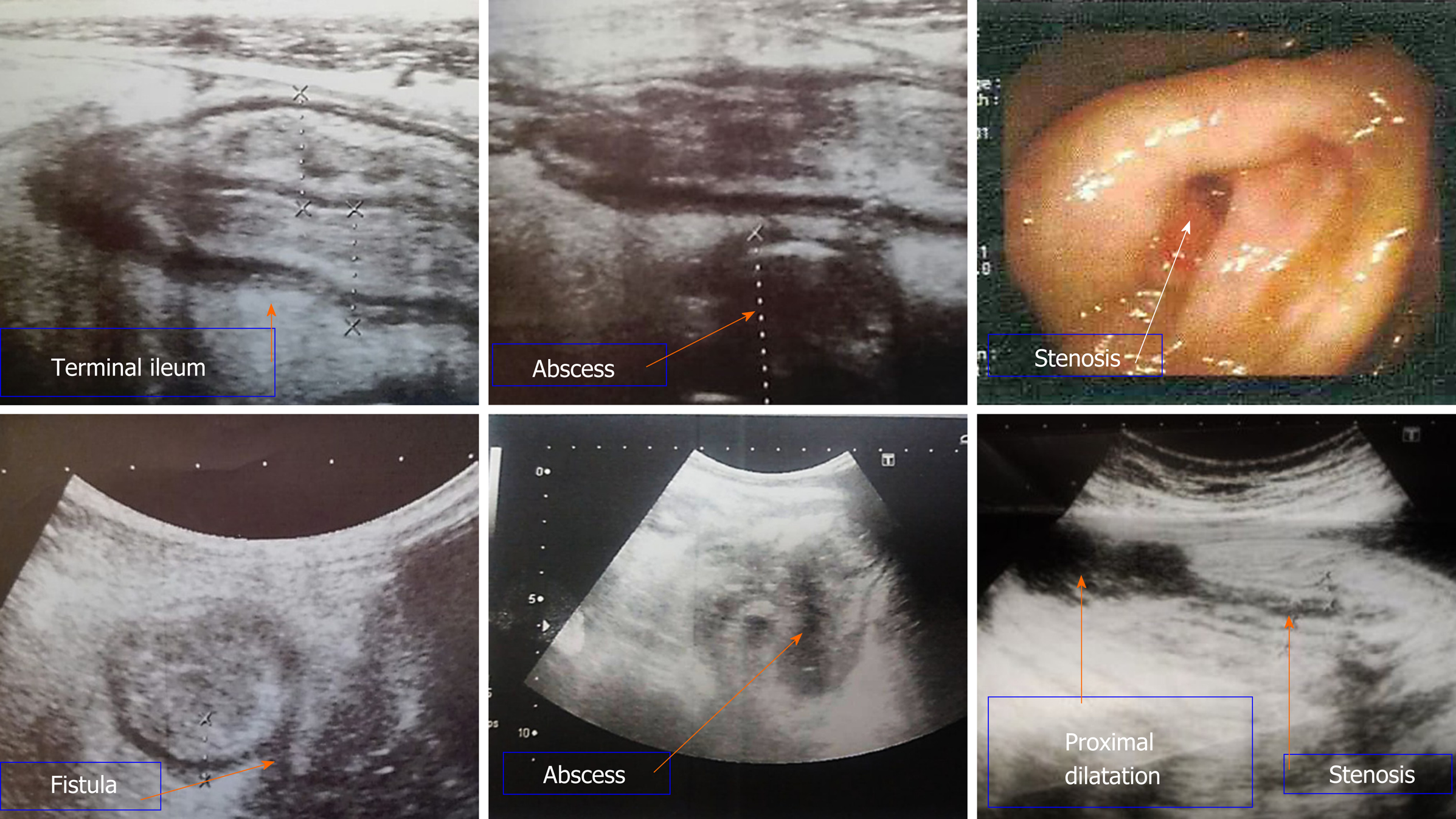
Patients were examined via ultrasound after a six-hour fasting period to minimize intestinal air contents. Examination was done by ultrasound machine (Toshiba Xario, Japan) with a low frequency curved-array transducer (2.5-4.5 MHz) to determine any pathological bowel motility or distension and any para-intestinal structures, such as abscesses, in all abdominal quadrants. Examination with a high-frequency linear-array transducer (6.0-8.4 MHz) was used for bowel wall examination starting with examination of the proximal colon followed with the distal one and then the small bowel[3]. This examination assessed criteria of inflammation such as thickness of bowel wall, inflammatory mesenteric fat and lymph nodes, hyperemia on color Doppler flow, and complications, such as stenosis, fistulas or inflammatory masses.
In the longitudinal direction, the bowel wall was measured for bowel thickness at its anterior wall or in an area in which it was more visible in order to avoid mucosal folds and haustrations. The cursor was placed at the end of the interface echo between the serosa and proper muscle to the start of the interface echo between the lumen and the mucosa[6,7].
Several criteria for stenosis diagnosis via ultrasound have been reported, such as thickened bowel wall, narrowing of the diameter of the lumen < 1 cm, hyperperistalsis of the pre-stenotic bowel, and proximal dilatation > 25-30 mm[8-10].
An abscess was indicated by bowel ultrasound as an irregular, avascular hypoechoic area with a small amount of internal echoes or air in the form of hyperechoic streaks[9].
The patient was instructed to have a low residue diet the day before the examination and was asked to fast at least 6 to 8 h before the onset of the procedure. Ingestion of 1 to 2 L of hyperosmolar oral contrast was performed for about 45 min before the magnetic resonance (MR) exam started. After full distension of the bowel, a spasmolytic medication was given to decrease bowel peristalsis to provide better bowel visualization. The examination was performed on 1.5-T MR machine, Achieva, Philips Medical System, Best, Netherlands in MRI Unit, Ain Shams University Hospital. The patient was laid in supine position using a multi-element phased array Torso coil (16 channels). A dedicated MR study was then performed as described in Table 1. Pixel-based apparent diffusion coefficient maps were generated on the off-line workstation (extended workspace ‘‘EWS’’), Pride software (Philips Medical Systems). Intravenous gadolinium contrast was given (0.2 mmol/kg body weight) in dynamic fashion obtaining three-dimensional enhanced T1 isotropic volume excitation (3D-eTHRIVE) coronal scans at 10 s, 20 s, 60 s, 70 s, and 90 s. The total MRE procedure took about 30 to 45 min.
| Imaging sequence and plane | TR/TE | Slice thickness (mm) | Gap | Field of view (mm) | Matrix |
| Coronal T2 SSFSE | 1200/115 | 6 | 1 | 375 × 375 | 268 × 234 |
| Coronal SSFP | 3.2/1.56 | 6 | 0 | 375 × 375 | 252 × 233 |
| Axial T2WI | 1200/115 | 7 | 1 | 375 × 336 | 268 × 208 |
| Axial DWI | 2743/65 | 7 | 1 | 375 × 302 | 124 × 100 |
| 3D-THRIVE | 4/1.9 | - | 0 | 410 × 377 | 196 × 178 |
| Axial post contrast fat-suppressed gradient-echo T1WI | 3.8/1.8 | - | 0 | 375 × 314 | 196 × 157 |
| Coronal post contrast fat-suppressed gradient-echo T1WI | 4/1.9 | - | 0 | 410 × 314 | 196 × 178 |
The images were interpreted by a radiologist with 12 years of experience in abdominal imaging and who was also blinded to the clinical and colonoscopy examination results.
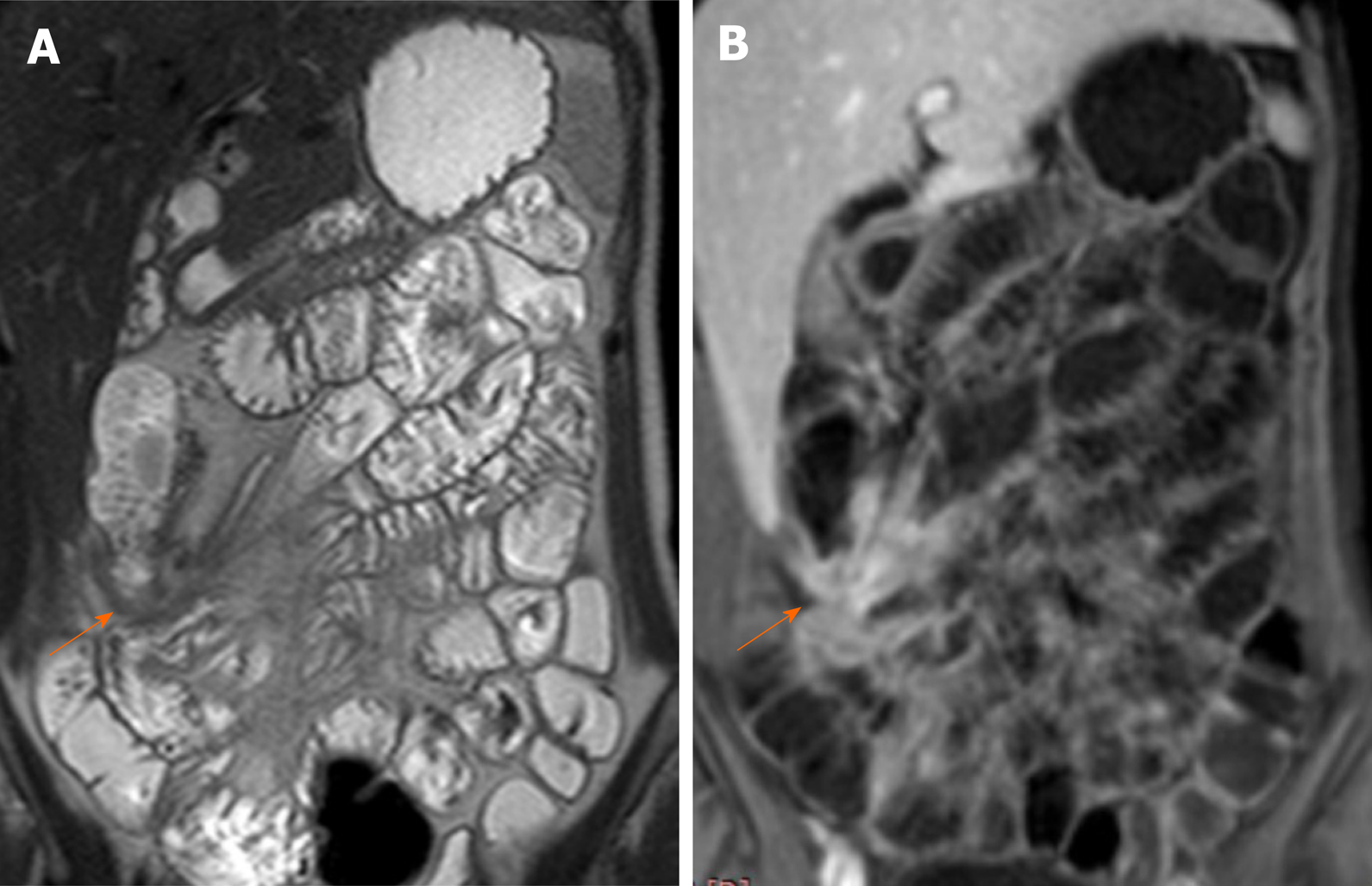
The MRE evaluated bowel wall thickening, mural edema, enlarged mesenteric lymph nodes, restricted diffusion, peri-enteric vascularization (comb sign), peri-enteric fluid, and presence of complications, such as abscesses or fistulas.
Statistical analysis was performed using the SPSS software (22.0 version: SSPS Inc., Chicago, IL. United States). Description of quantitative variables was expressed in the form of mean ± standard deviation (mean ± SD) or median and inter-quartile range. A description of qualitative variables was expressed by frequency and percentage. Comparison of qualitative variables was carried out using the chi-square test. P < 0.05 was taken as significant. The sensitivity, specificity, overall correctness of prediction, and positive and negative predictive values were calculated. Correlations were calculated using Pearson’s correlation coefficient. The receiver operating characteristic (ROC) curves and areas under the ROC (AUROC) curves were applied to evaluate the prognostic values (specificity and sensitivity).
The demographic profile, clinical and laboratory parameters are shown in Table 2. Most of the patients were middle-age females who usually presented with abdominal pain and diarrhea. The result indicated that 14 (35%) of our patients had ulcerative colitis, and 26 (65%) had Crohn's disease while 34 (85%) of them were inactive. Four (4%) of studied patients had pancolitis, and 18 (45%) of the studied cases had ileal lesions.
| Demographic characteristics, laboratory and colonscopic findings | n |
| Age (yr) | 33.50 ± 8.19 |
| Gender (male/female) | 16/24 |
| Symptoms | |
| Diarrhea | 14 (35%) |
| Diarrhea and bleeding | 10 (25%) |
| Bleeding | 4 (10%) |
| Abdominal pain | 36 (90%) |
| Total leukocyte count (103/cmm) | 7.32 ± 2.22 |
| Hemoglobin (g/dL) | 11.22 ± 1.86 |
| Total bilirubin (mg/dL) | 0.97 ± 0.14 |
| Alanine aminotransferase (IU/L) | 25.75 ± 10.49 |
| Total protein (g/dL) | 7.16 ± 0.73 |
| Albumin (g/dL) | 3.76 ± 0.44 |
| Blood urea nitrogen (mg/dL) | 22.10 ± 9.86 |
| Creatinine (mg/dL) | 0.87 ± 0.22 |
| Serum sodium (mmol/L) | 136.65 ± 6.19 |
| Serum Potassium (mmol/L) | 3.96 ± 0.55 |
| C-reactive protein (mg/L) | 28 (6–55) |
| Erythrocyte sedimentation rate (mm/h) | 45 (31.5–60) |
| Colonscopic findings | |
| Opacity of mucosa | 28 (70%) |
| Excess exudate | 24 (60%) |
| Cobble stone | 26 (65%) |
| Bleeding on touch | 20 (50%) |
| Aphthous ulcers | 30 (75%) |
| Diffuse ulceration | 20 (50%) |
| Pseudopolyps | 20 (50%) |
| Polyps | 30 (75%) |
| Site of involvement | |
| Rectum | 4 (10%) |
| Pancolitis | 4 (10%) |
| Descending colon | 4 (10%) |
| Rectum and sigmoid colon | 10 (25%) |
| Ileum | 18 (45%) |
| Type of disease | |
| Ulcerative colitis | 14 (35%) |
| Crohn's disease | 26 (65%) |
| Activity | |
| Remission | 6 (15%) |
| Activity | 34 (85%) |
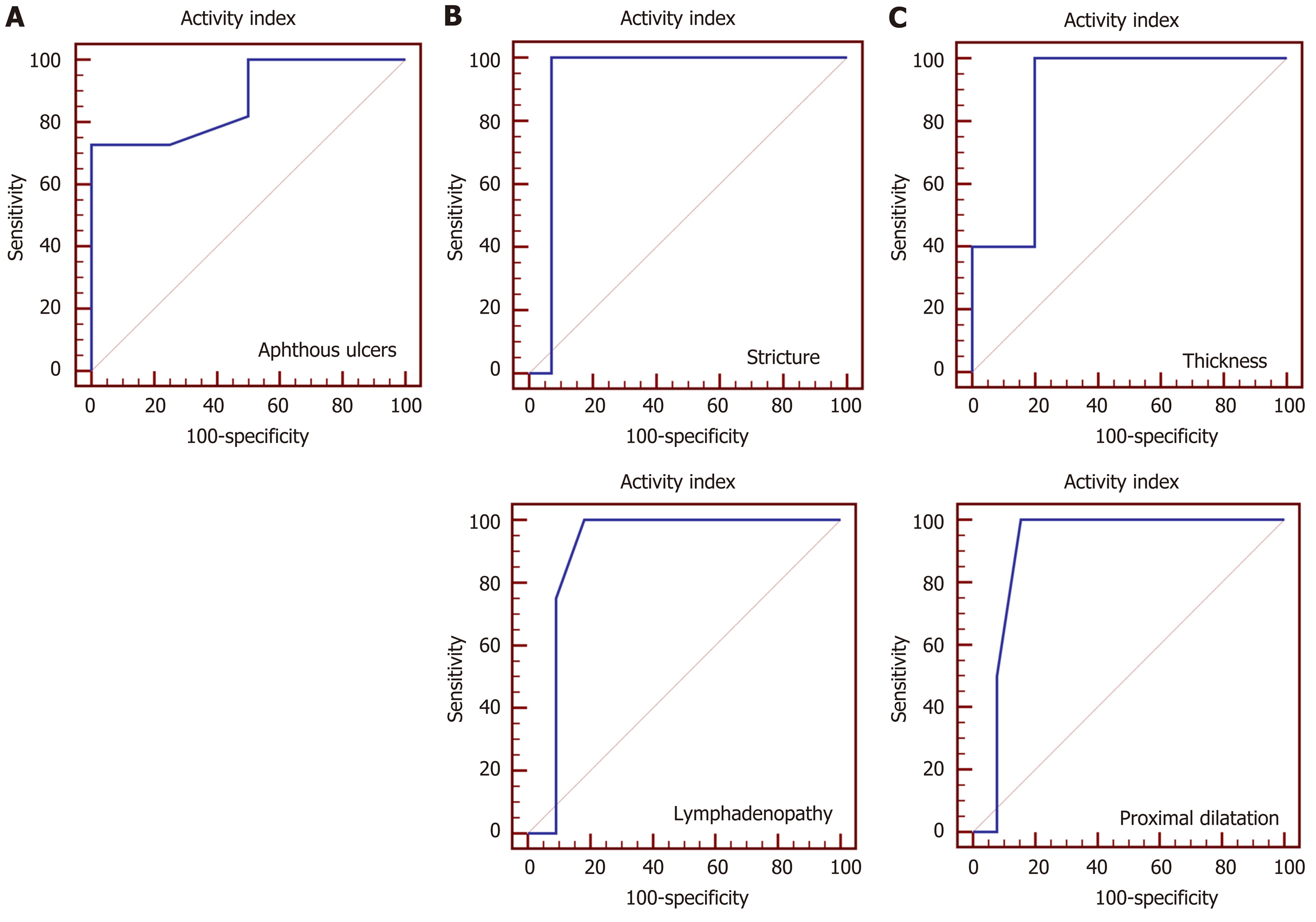
Table 3 indicates that the bowel ultrasound appeared to be a good predictor for detection of ileal affection with sensitivity, specificity, and diagnostic accuracy of 93.8%, 50%, and 85%, respectively. With respect to the large bowel, bowel ultrasound detected large bowel affection with sensitivity, specificity, and accuracy of 37.5%, 91.7%, and 70%, respectively. Also, bowel ultrasound was a good predictor for detection of thickness of affected segment with sensitivity, specificity, and accuracy of 83.3%, 50%, and 60% respectively. Also, bowel ultrasound was a good predictor for detection of fistulous track with sensitivity, specificity, and accuracy of 85.7%, 100%, and 95%, respectively, while sensitivity, specificity, and accuracy of 100%, 94.4%, and 95%, respectively, for detection of stricture and proximal dilatation were found. Abscess was detected by bowel ultrasound in six patients with high specificity, sensitivity, and accuracy (100%). Also, bowel ultrasound showed that no statistically significant differences between bowel ultrasound and disease activity index, which indicates that bowel ultrasound can differentiate between remission and active disease (Figure 1).
| Bowel ultrasound | Disease activity index | |||||||
| Sensitivity | Specificity | PPV | NPV | Accuracy | Remission | Activity | P value | |
| Large bowel | 37.5% | 91.7% | 75% | 68.8% | 0.700 | 0 (0) | 8 (23.5%) | 0.184 |
| Ileum | 93.8% | 50% | 88.2% | 66.7% | 0.850 | 6 (100%) | 28 (82.4%) | 0.264 |
| Thickness (> 3 mm) | 83.3% | 50% | 41.7% | 87.5% | 0.600 | 4 (66.7%) | 20 (58.8%) | 0.718 |
| Extent | 33.3% | 85.7% | 50% | 75% | 0.700 | 0 (0) | 8 (23.5%) | 0.184 |
| Mesenteric lymphadenopathy | 16.7% | 71.4% | 20% | 66.7% | 0.550 | 0 (0) | 10 (29.4%) | 0.125 |
| Fistula | 85.7% | 100% | 100% | 92.9% | 0.950 | 0 (0) | 12 (35.3%) | 0.082 |
| Stricture and proximal dilatation | 100% | 94.4% | 66.7% | 100% | 0.950 | 0 (0) | 6 (17.6%) | 0.264 |
| Abscess | 100% | 100% | 100% | 100% | 0.1 | 0 (0) | 6 (17.6%) | 0.264 |
Table 4 indicates that no statistically significant difference among bowel ultrasound, MRE, and colonoscopy for detection of activity of the disease was noted, indicating that bowel ultrasound and MRE can differentiate between remission and active IBD (Figure 2).
| Activity | Colonoscopy | Bowel ultrasound | MRE | P value |
| Remission | 6 (15%) | 6 (15%) | 6 (15%) | 1.000 |
| Activity | 34 (85%) | 34 (85%) | 34 (85%) | 1.000 |
Table 5 compares between clinical symptoms and imaging modalities bowel ultrasound and MRE. It indicates that bleeding per rectum is statistically significant in patients with strictures and proximal dilatation during assessment by bowel ultrasound, while diarrhea is statistically significant to the extent of the lesions when assessed by MRE.
| Abdominal pain | P value | Bleeding per rectum | P value | Diarrhea | P value | ||||||
| No, n (%) | Yes, n (%) | No, n (%) | Yes, n (%) | No, n (%) | Yes, n (%) | ||||||
| Bowel ultrasound | |||||||||||
| Large bowel | 0 (0) | 8 (22.2%) | 0.292 | 8 (25.0%) | 0 (0) | 0.114 | 2 (10.0%) | 6 (30.0%) | 0.114 | ||
| Ileum | 4 (100.0%) | 30 (83.3%) | 0.376 | 26 (81.2%) | 8 (100.0%) | 0.184 | 18 (90.0%) | 16 (80.0%) | 0.376 | ||
| Thickness (> 3 mm) | 4 (100.0%) | 20 (55.6%) | 0.085 | 18 (56.2%) | 6 (75.0%) | 0.333 | 14 (70.0%) | 10 (50.0%) | 0.197 | ||
| Extent | 0 (0) | 8 (22.2%) | 0.292 | 8 (25.0%) | 0 (0) | 0.114 | 2 (10.0%) | 6 (30.0%) | 0.114 | ||
| Lymphadenopathy | 0 (0) | 10 (27.8%) | 0.224 | 8 (25.0%) | 2 (25.0%) | 1.000 | 4 (20.0%) | 6 (30.0%) | 0.465 | ||
| Fistula | 0 (0) | 12 (33.3%) | 0.168 | 8 (25.0%) | 4 (50.0%) | 0.168 | 4 (20.0%) | 8 (40.0%) | 0.168 | ||
| Stricture and proximal dilatation | 0 (0) | 2 (5.6%) | 0.629 | 0 (0) | 2 (25.0%) | 0.004 | 0 (0) | 2 (10.0%) | 0.147 | ||
| Abscess | 2 (50.0%) | 6 (16.7%) | 0.114 | 6 (18.8%) | 2 (25.0%) | 0.693 | 6 (30.0%) | 2 (10.0%) | 0.114 | ||
| MRE | |||||||||||
| Large bowel | 0 (0) | 16 (44.4%) | 0.085 | 14 (43.8%) | 2 (25.0%) | 0.333 | 6 (30.0%) | 10 (50.0%) | 0.197 | ||
| Ileum | 4 (100.0%) | 28 (77.8%) | 0.292 | 24 (75.0%) | 8 (100.0%) | 0.114 | 16 (80.0%) | 16 (80.0%) | 1.000 | ||
| Thickness (> 3 mm) | 2 (50.0%) | 10 (27.8%) | 0.358 | 10 (31.2%) | 2 (25.0%) | 0.730 | 6 (30.0%) | 6 (30.0%) | 1.000 | ||
| Extent | 0 (0) | 12 (33.3%) | 0.168 | 10 (31.2%) | 2 (25.0%) | 0.730 | 2 (10.0%) | 10 (50.0%) | 0.006 | ||
| Lymphadenopathy | 0 (0) | 12 (33.3%) | 0.168 | 8 (25.0%) | 4 (50.0%) | 0.168 | 8 (40.0%) | 4 (20.0%) | 0.168 | ||
| Fistula | 0 (0) | 14 (38.9%) | 0.122 | 10 (31.2%) | 4 (50.0%) | 0.320 | 6 (30.0%) | 8 (40.0%) | 0.507 | ||
| Stricture and proximal dilatation | 0 (0) | 4 (11.1%) | 0.482 | 4 (12.5%) | 0 (0) | 0.292 | 2 (10.0%) | 2 (10.0%) | 1.000 | ||
| Abscess | 0 (0) | 6 (16.7%) | 0.376 | 6 (18.8%) | 0 (0) | 0.184 | 2 (10.0%) | 4 (20.0%) | 0.376 | ||
Endoscopy is still the most important diagnostic procedure as it permits taking biopsy for histological examination[11]. European guidelines have recommended imaging techniques, such as bowel ultrasound, computed tomography enterography, and MRE as complementary tools for IBD diagnosis that can help define its location, extension, and complications[12].
MRE is a cross-sectional non-ionizing imaging technique that can be used for IBD diagnosis and extrainstestinal assessment of disease activity and followup of patients. But MRE is available at certain centers only and it takes long time during scanning with sedation in some cases such as children to avoid motion artefacts besides non-compliance to contrast intake and breath-hold technique[13].
Assessment of gastrointestinal tract in IBD patients by intestinal ultrasound was evolved nowadays due to development of ultrasound devices and rising skillfullness of their examiners as radiologists and gastroenterologists. Major parts of the small and large intestine can be easily examined by bowel ultrasound while proximal part of jejunum and the rectum may be difficult in their assessment due to overlying structures. Inspite of different advantages of bowel ultrasound as a rapid bedside, inexpensive and non-radiating tolerable test but its results are subjective to the examiner's expertise[14].
Our results showed similar sensitivity for detection of ileal IBD in comparison to one previous study (92.7%) but with lower specificity than this study (88.2%). Regarding colonic IBD, our results showed lower sensitivity than observed in this previous study (81.8%) but with similar specificity (95.3%), a finding which may be explained by interobserver variability between examiners[13]. This variability can explain why one study concluded that bowel ultrasound is more accurate for assessment of IBD patients if combined with colonoscopy[16].
A bowel wall thickness cutoff value of 3 mm in our study showed sensitivity (83.3%), specificity (50%), and accuracy (60%) in comparison to other studies, which showed sensitivities of 88% to 94%; however, specificity (93%-97%,) and diagnostic accuracy (94%) were higher in previous studies than in our study[9,15]. This finding can be explained by the lack of international agreement about standardized measurement parameters, which leads to interobserver variability between examiners[18].
Mesenteric lymph nodes detected by bowel ultrasound in our study were non-sensitive and non-specific (16.7% and 71.4%, respectively) and insignificantly subsided during remission; therefore, lymph nodes detection was not a good parameter of activity in agreement with some previous studies[19,20].
Our study agreed with different trials in which it was shown that detection rate of fistulas, depending on their localization, had sensitivity between 67% and 82% and specificity between 90% and 100%[8,9,21-23].
Stricture in our study as detected by bowel ultrasound showed sensitivity, specificity, and accuracy (100%, 94.4%, and 95%, respectively) were similar to other studies[15,24-26].
The sensitivity for detecting abscesses in different studies varied between 80% and 100%, and specificity varied between 92% and 94%, which were similar results to ours[27-29].
Our study agreed with different trials in which it was shown that diagnosis of IBD and assessment of its activity cannot be dependent on clinical evaluation alone but should by combined with other investigations such as biomarkers, endoscopy, and imaging techniques such as bowel ultrasound and MRE[25,30].
Our results showed that aphthous ulcers at endoscopy, stricture and mesenteric lymphadenopathy at bowel ultrasound, thickness of bowel wall and proximal dilatation at MRE were significantly correlated to disease activity (Figure 3). Other studies showed that other different bowel ultrasound parameters such as bowel wall thickening and its extent showed a significant correlation with disease activity[26,31,32]. Regarding MRE results in our study agreed with some studies[33,34] and disagree with another[35].
This indicates that there is no clear gold standard imaging technique for IBD diagnosis including MRE or bowel ultrasound which could be used besides clinical history, biomarkers, endoscopy for diagnosis of IBD as agreed with previous studies[25,30,36].
Bowel ultrasound can be more helpful in follow-up of IBD patients and monitoring of their response to treatment away from its role of diagnosis by ultrasound guided biopsy.
In Egypt, both MRE and colonoscopy are available tools with estimated total cost of $93 dollars and $125 dollars respectively. Bowel ultrasound costs only 18$ dollars which is considered as a low cost alternative and has prospects for widespread clinical use.
Limitations of our study were the relatively small number of included patients, and comparative assessments of clinical decisions with and without bowel ultrasound were not available.
In comparison to MRE and colonoscopy, bowel ultrasound is a useful non-invasive and feasible bedside imaging tool for the detection of inflammation, complications, as screening tool and follow-up of IBD patients when performed by the attending physician.
Bowel ultrasound is a new tool for evaluation of inflammatory bowel.
Up until now, no previous published comparative studies between bowel ultrasound and magnetic resonance enterography (MRE) for Egyptian inflammatory bowel disease (IBD) patients.
Compare between the role of bowel ultrasound and MRE in Egyptian IBD patients.
The study was conducted on 40 patients presented to IBD center of Ainshams University Hospitals. The patients were subjected to clinical, laboratory, colonoscopic and radiological assessments including bowel ultrasound and MRE.
Bowel ultrasound was a good predictor of disease activity, fistula, stricture, and abscess formation with high sensitivity in ileum and more specificity in large bowel.
Bowel ultrasound is a useful bedside cheap imaging tool that can be used for diagnosis and follow-up of IBD patients.
Further studies to compare clinical decisions with and without bowel ultrasound.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Huang Z, Koga H, Sang LX, Zhuo ZQ S-Editor: Gao CC L-Editor: Webster JR P-Editor: Zhang YL
| 1. | Lunder AK, Bakstad LT, Jahnsen J, Borthne A, Hov JR, Vatn M, Negård A. Assessment of Bowel Inflammation and Strictures by Magnetic Resonance Enterography in Long-term Crohn's Disease. J Crohns Colitis. 2019;13:607-614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Maccioni F, Bruni A, Viscido A, Colaiacomo MC, Cocco A, Montesani C, Caprilli R, Marini M. MR imaging in patients with Crohn disease: value of T2- vs T1-weighted gadolinium-enhanced MR sequences with use of an oral superparamagnetic contrast agent. Radiology. 2006;238:517-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 187] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 3. | Strobel D, Goertz RS, Bernatik T. Diagnostics in inflammatory bowel disease: ultrasound. World J Gastroenterol. 2011;17:3192-3197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 36] [Reference Citation Analysis (0)] |
| 4. | Best WR, Becktel JM, Singleton JW. Rederived values of the eight coefficients of the Crohn's Disease Activity Index (CDAI). Gastroenterology. 1979;77:843-846. [PubMed] |
| 5. | TRUELOVE SC, WITTS LJ. Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J. 1955;2:1041-1048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1832] [Cited by in RCA: 1868] [Article Influence: 26.7] [Reference Citation Analysis (1)] |
| 6. | Nylund K, Hausken T, Ødegaard S, Eide GE, Gilja OH. Gastrointestinal wall thickness measured with transabdominal ultrasonography and its relationship to demographic factors in healthy subjects. Ultraschall Med. 2012;33:E225-E232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 7. | Nylund K, Maconi G, Hollerweger A, Ripolles T, Pallotta N, Higginson A, Serra C, Dietrich CF, Sporea I, Saftoiu A, Dirks K, Hausken T, Calabrese E, Romanini L, Maaser C, Nuernberg D, Gilja OH. EFSUMB Recommendations and Guidelines for Gastrointestinal Ultrasound. Ultraschall Med. 2017;38:e1-e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 71] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 8. | Calabrese E, Zorzi F, Onali S, Stasi E, Fiori R, Prencipe S, Bella A, Petruzziello C, Condino G, Lolli E, Simonetti G, Biancone L, Pallone F. Accuracy of small-intestine contrast ultrasonography, compared with computed tomography enteroclysis, in characterizing lesions in patients with Crohn's disease. Clin Gastroenterol Hepatol. 2013;11:950-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 9. | Castiglione F, Mainenti PP, De Palma GD, Testa A, Bucci L, Pesce G, Camera L, Diaferia M, Rea M, Caporaso N, Salvatore M, Rispo A. Noninvasive diagnosis of small bowel Crohn's disease: direct comparison of bowel sonography and magnetic resonance enterography. Inflamm Bowel Dis. 2013;19:991-998. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 10. | Coelho R, Ribeiro H, Maconi G. Bowel Thickening in Crohn's Disease: Fibrosis or Inflammation? Inflamm Bowel Dis. 2017;23:23-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 11. | Annese V, Daperno M, Rutter MD, Amiot A, Bossuyt P, East J, Ferrante M, Götz M, Katsanos KH, Kießlich R, Ordás I, Repici A, Rosa B, Sebastian S, Kucharzik T, Eliakim R; European Crohn's and Colitis Organisation. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis. 2013;7:982-1018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 640] [Cited by in RCA: 584] [Article Influence: 48.7] [Reference Citation Analysis (1)] |
| 12. | Gomollón F, Dignass A, Annese V, Tilg H, Van Assche G, Lindsay JO, Peyrin-Biroulet L, Cullen GJ, Daperno M, Kucharzik T, Rieder F, Almer S, Armuzzi A, Harbord M, Langhorst J, Sans M, Chowers Y, Fiorino G, Juillerat P, Mantzaris GJ, Rizzello F, Vavricka S, Gionchetti P; ECCO. 3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn's Disease 2016: Part 1: Diagnosis and Medical Management. J Crohns Colitis. 2017;11:3-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1585] [Cited by in RCA: 1448] [Article Influence: 181.0] [Reference Citation Analysis (0)] |
| 13. | Ramos López L, Hernández Camba A, Rodríguez-Lago I, Carrillo Palau M, Cejas Dorta L, Elorza A, Alonso Abreu I, Vela M, Hidalgo A, Hernández Álvarez-Builla N, Rodríguez GE, Rodríguez Y, Tardillo C, Díaz-Flórez L, Eiroa D, Aduna M, Garrido MS, Larena JA, Cabriada JL, Quintero Carrion E. Usefulness of magnetic resonance enterography in the clinical decision-making process for patients with inflammatory bowel disease. Gastroenterol Hepatol. 2020;:. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Rajagopalan A, Sathananthan D, An YK, Van De Ven L, Martin S, Fon J, Costello SP, Begun J, Bryant RV. Gastrointestinal ultrasound in inflammatory bowel disease care: Patient perceptions and impact on disease-related knowledge. JGH Open. 2020;4:267-272. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 15. | Calabrese E, Maaser C, Zorzi F, Kannengiesser K, Hanauer SB, Bruining DH, Iacucci M, Maconi G, Novak KL, Panaccione R, Strobel D, Wilson SR, Watanabe M, Pallone F, Ghosh S. Bowel Ultrasonography in the Management of Crohn's Disease. Inflamm Bowel Dis. 2016;22:1168-1183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 127] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 16. | Maconi G, Bolzoni E, Giussani A, Friedman AB, Duca P. Accuracy and cost of diagnostic strategies for patients with suspected Crohn's disease. J Crohns Colitis. 2014;8:1684-1692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 17. | Fraquelli M, Colli A, Casazza G, Paggi S, Colucci A, Massironi S, Duca P, Conte D. Role of US in detection of Crohn disease: meta-analysis. Radiology. 2005;236:95-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 207] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 18. | Calabrese E, Kucharzik T, Maaser C, Maconi G, Strobel D, Wilson SR, Zorzi F, Novak KL, Bruining DH, Iacucci M, Watanabe M, Lolli E, Chiaramonte C, Hanauer SB, Panaccione R, Pallone F, Ghosh S, Monteleone G. Real-time Interobserver Agreement in Bowel Ultrasonography for Diagnostic Assessment in Patients With Crohn's Disease: An International Multicenter Study. Inflamm Bowel Dis. 2018;24:2001-2006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 19. | Kucharzik T, Wittig BM, Helwig U, Börner N, Rössler A, Rath S, Maaser C; TRUST study group. Use of Intestinal Ultrasound to Monitor Crohn's Disease Activity. Clin Gastroenterol Hepatol. 2017;15:535-542.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 168] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 20. | Maconi G, Di Sabatino A, Ardizzone S, Greco S, Colombo E, Russo A, Cassinotti A, Casini V, Corazza GR, Bianchi Porro G. Prevalence and clinical significance of sonographic detection of enlarged regional lymph nodes in Crohn's disease. Scand J Gastroenterol. 2005;40:1328-1333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 59] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 21. | Onali S, Calabrese E, Petruzziello C, Zorzi F, Sica G, Fiori R, Ascolani M, Lolli E, Condino G, Palmieri G, Simonetti G, Pallone F, Biancone L. Small intestine contrast ultrasonography vs computed tomography enteroclysis for assessing ileal Crohn's disease. World J Gastroenterol. 2012;18:6088-6095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (1)] |
| 22. | Pallotta N, Vincoli G, Montesani C, Chirletti P, Pronio A, Caronna R, Ciccantelli B, Romeo E, Marcheggiano A, Corazziari E. Small intestine contrast ultrasonography (SICUS) for the detection of small bowel complications in crohn's disease: a prospective comparative study vs intraoperative findings. Inflamm Bowel Dis. 2012;18:74-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 77] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 23. | Kumar S, Hakim A, Alexakis C, Chhaya V, Tzias D, Pilcher J, Vlahos J, Pollok R. Small intestinal contrast ultrasonography for the detection of small bowel complications in Crohn's disease: correlation with intraoperative findings and magnetic resonance enterography. J Gastroenterol Hepatol. 2015;30:86-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 24. | Parente F, Maconi G, Bollani S, Anderloni A, Sampietro G, Cristaldi M, Franceschelli N, Bianco R, Taschieri AM, Bianchi Porro G. Bowel ultrasound in assessment of Crohn's disease and detection of related small bowel strictures: a prospective comparative study versus X ray and intraoperative findings. Gut. 2002;50:490-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 123] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 25. | Panes J, Bouhnik Y, Reinisch W, Stoker J, Taylor SA, Baumgart DC, Danese S, Halligan S, Marincek B, Matos C, Peyrin-Biroulet L, Rimola J, Rogler G, van Assche G, Ardizzone S, Ba-Ssalamah A, Bali MA, Bellini D, Biancone L, Castiglione F, Ehehalt R, Grassi R, Kucharzik T, Maccioni F, Maconi G, Magro F, Martín-Comín J, Morana G, Pendsé D, Sebastian S, Signore A, Tolan D, Tielbeek JA, Weishaupt D, Wiarda B, Laghi A. Imaging techniques for assessment of inflammatory bowel disease: joint ECCO and ESGAR evidence-based consensus guidelines. J Crohns Colitis. 2013;7:556-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 539] [Cited by in RCA: 478] [Article Influence: 39.8] [Reference Citation Analysis (0)] |
| 26. | Dong J, Wang H, Zhao J, Zhu W, Zhang L, Gong J, Li Y, Gu L, Li J. Ultrasound as a diagnostic tool in detecting active Crohn's disease: a meta-analysis of prospective studies. Eur Radiol. 2014;24:26-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 84] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 27. | Gasche C, Moser G, Turetschek K, Schober E, Moeschl P, Oberhuber G. Transabdominal bowel sonography for the detection of intestinal complications in Crohn's disease. Gut. 1999;44:112-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 143] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 28. | Kohn A, Cerro P, Milite G, De Angelis E, Prantera C. Prospective evaluation of transabdominal bowel sonography in the diagnosis of intestinal obstruction in Crohn's disease: comparison with plain abdominal film and small bowel enteroclysis. Inflamm Bowel Dis. 1999;5:153-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 29. | Maconi G, Sampietro GM, Parente F, Pompili G, Russo A, Cristaldi M, Arborio G, Ardizzone S, Matacena G, Taschieri AM, Bianchi Porro G. Contrast radiology, computed tomography and ultrasonography in detecting internal fistulas and intra-abdominal abscesses in Crohn's disease: a prospective comparative study. Am J Gastroenterol. 2003;98:1545-1555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 146] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 30. | Kucharzik T, Petersen F, Maaser C. Bowel Ultrasonography in Inflammatory Bowel Disease. Dig Dis. 2015;33 Suppl 1:17-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 31. | Ripollés T, Paredes Arquiola JM, Moreno-Osset E. Ultrasonography and Transmural Healing in Crohn's Disease. Clin Gastroenterol Hepatol. 2015;13:1549-1551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 32. | Parente F, Molteni M, Marino B, Colli A, Ardizzone S, Greco S, Sampietro G, Foschi D, Gallus S. Are colonoscopy and bowel ultrasound useful for assessing response to short-term therapy and predicting disease outcome of moderate-to-severe forms of ulcerative colitis? Am J Gastroenterol. 2010;105:1150-1157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 98] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 33. | Martínez MJ, Ripollés T, Paredes JM, Blanc E, Martí-Bonmatí L. Assessment of the extension and the inflammatory activity in Crohn's disease: comparison of ultrasound and MRI. Abdom Imaging. 2009;34:141-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 103] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 34. | Rimola J, Ordás I, Rodriguez S, García-Bosch O, Aceituno M, Llach J, Ayuso C, Ricart E, Panés J. Magnetic resonance imaging for evaluation of Crohn's disease: validation of parameters of severity and quantitative index of activity. Inflamm Bowel Dis. 2011;17:1759-1768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 367] [Cited by in RCA: 387] [Article Influence: 27.6] [Reference Citation Analysis (0)] |
| 35. | Ordás I, Rimola J, Rodríguez S, Paredes JM, Martínez-Pérez MJ, Blanc E, Arévalo JA, Aduna M, Andreu M, Radosevic A, Ramírez-Morros AM, Pinó S, Gallego M, Jauregui-Amezaga A, Ricart E, Panés J. Accuracy of magnetic resonance enterography in assessing response to therapy and mucosal healing in patients with Crohn's disease. Gastroenterology. 2014;146:374-82.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 294] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 36. | Schreiber-Dietrich D, Chiorean L, Cui XW, Braden B, Kucharzik T, Jüngert J, Kosiak W, Stenzel M, Dietrich CF. Particularities of Crohn's disease in pediatric patients: current status and perspectives regarding imaging modalities. Expert Rev Gastroenterol Hepatol. 2015;9:1313-1325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |