Published online Aug 7, 2020. doi: 10.3748/wjg.v26.i29.4372
Peer-review started: April 7, 2020
First decision: April 29, 2020
Revised: May 9, 2020
Accepted: July 15, 2020
Article in press: July 15, 2020
Published online: August 7, 2020
Processing time: 122 Days and 2.4 Hours
Epithelioid angiosarcoma is a vascular neoplasm that is among the most aggressive subtypes of sarcomas. Its involvement in the gastrointestinal tract is rare. We here report a case of multifocal gastrointestinal epithelioid angiosarcomas presenting with gastrointestinal bleeding.
A 77-year-old woman was admitted because of melena and dizziness for three months. Gastroscopy and colonoscopy were performed, revealing a centrally ulcerated hemorrhagic polypoid lesion in the gastric body and multiple polypoid lesions with blood clots and hemorrhagic tendency in the colon. Histopathological examination of routine endoscopic biopsy samples showed inflammation in the gastric mucosa and tubular adenomas in the colon. The polypoid lesions were removed by endoscopic mucosal resection. Immunohistochemistry suggested a final diagnosis of epithelioid angiosarcomas. The patient refused chemotherapy and died after three months.
Epithelioid angiosarcomas are characterized by highly vascular nature and tendency to cause gastrointestinal bleeding. Efforts to obtain histological findings using endoscopic mucosal resection are of great importance.
Core tip: Gastrointestinal epithelioid angiosarcoma is extremely rare, which is only described in individual case reports and case series. Most reported cases appeared as centrally ulcerated, hemorrhagic, highly erythematous or purpuric nodules. Histopathology is the golden standard for diagnosis. Endoscopic biopsy often obtains insufficient specimens, while endoscopic mucosal resection of suspected lesions is satisfactory for histopathological examination. We here report a case of gastrointestinal bleeding which was finally diagnosed as multifocal epithelioid angiosarcomas in the gastrointestinal tract.
- Citation: Chen YW, Dong J, Chen WY, Dai YN. Multifocal gastrointestinal epithelioid angiosarcomas diagnosed by endoscopic mucosal resection: A case report. World J Gastroenterol 2020; 26(29): 4372-4377
- URL: https://www.wjgnet.com/1007-9327/full/v26/i29/4372.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i29.4372
Epithelioid angiosarcoma is a sporadic, highly aggressive malignancy that originates from a variety of locations, most commonly from the skin and soft tissue[1]. This type of tumor occasionally occurs in the liver, spleen, ovary, breast and adrenal gland[2]. Primary gastrointestinal angiosarcoma is extremely rare[3,4]. Here, we present a case of multifocal epithelioid angiosarcomas involved in the gastrointestinal tract.
A previous healthy 77-year-old woman presented with a 3-mo history of melena and dizziness and was admitted to our hospital.
The physical examination was unremarkable except for pale conjunctiva. Her hemoglobin level was 65 g/L. The platelet count, coagulation function, and blood biochemistry were within normal limits. The antinuclear antibody titre was 1:1000, while the anti-SSA (Ro60) antibodies were weakly positive. Autoimmune diseases were ruled out by rheumatologists because there were no related symptoms. Abdominal computed tomography angiography revealed nothing remarkable.
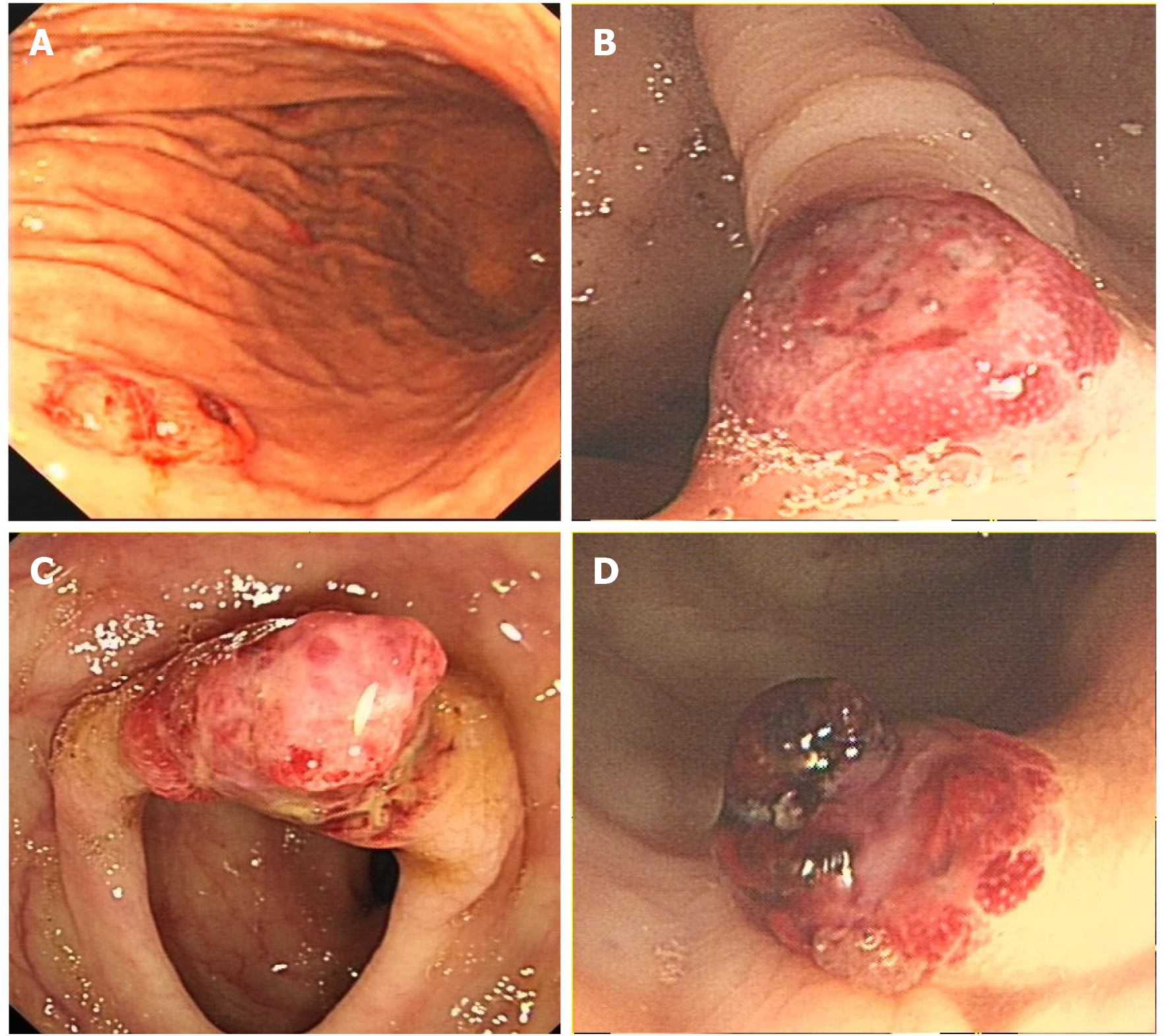
Gastroscopy demonstrated a centrally ulcerated haemorrhagic polypoid lesion in the gastric body (Figure 1A). Colonoscopy revealed multiple polypoid lesions with blood clots and hemorrhagic tendency in the ileocecum, ascending colon, transverse colon and sigmoid colon (Figure 1B-D). Routine endoscopic biopsies showed inflammatory infiltration in the gastric mucosa and tubular adenomas with low-grade intraepithelial neoplasia and local eosinophilic changes in the colon. Nevertheless, the pathologic findings did not conform to the endoscopic appearance of the foci. Subsequently, the lesions were resected en bloc by endoscopic mucosal resection for further diagnosis.
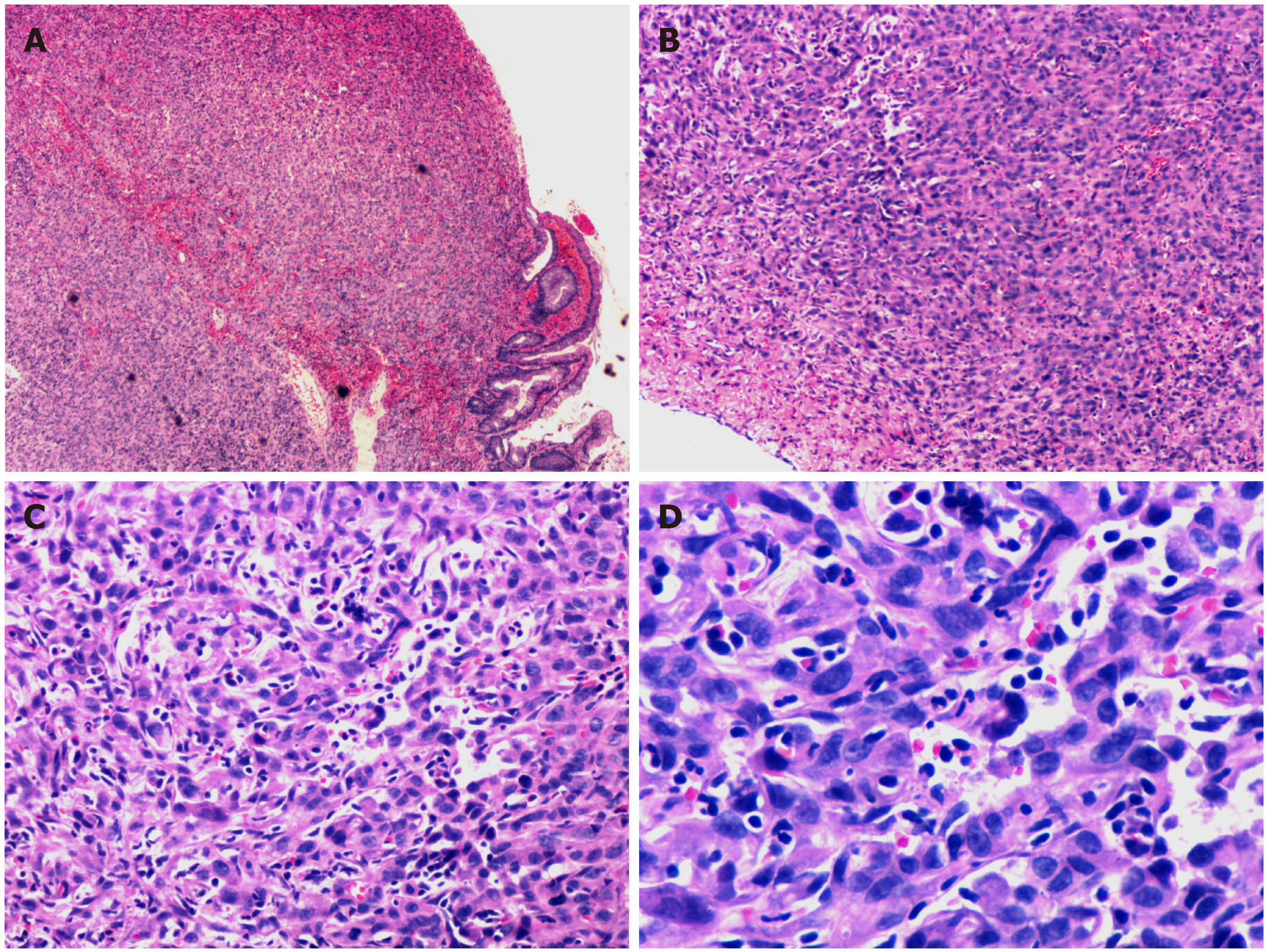
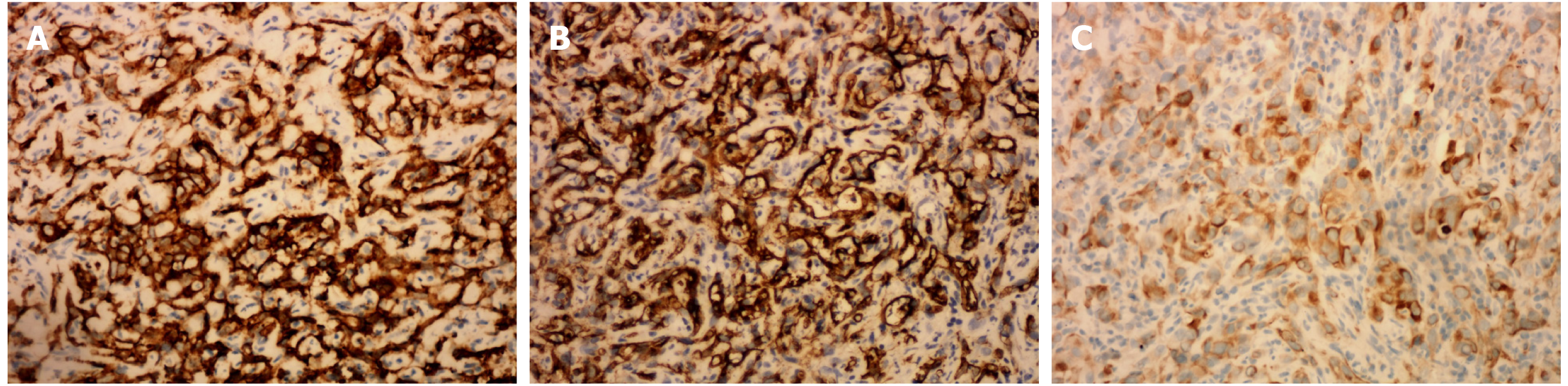
Microscopically, hematoxylin and eosin staining showed areas of epithelioid cells with abundant eosinophilic cytoplasm, which was morphologically similar to undifferentiated carcinoma or poorly differentiated adenocarcinoma (Figure 2). Immunohistochemical staining (Figure 3) demonstrated that the tumor cells were positive for pan-cytokeratin (AE1/AE3), CD31, CD34, EMA, vimentin and Ki67 (60% positive) and negative for hepatocytes, S100, CD117, DOG1, CD56, SYN, CgA, LCA, desmin or ALK. The final pathological diagnosis was epithelioid angiosarcoma.
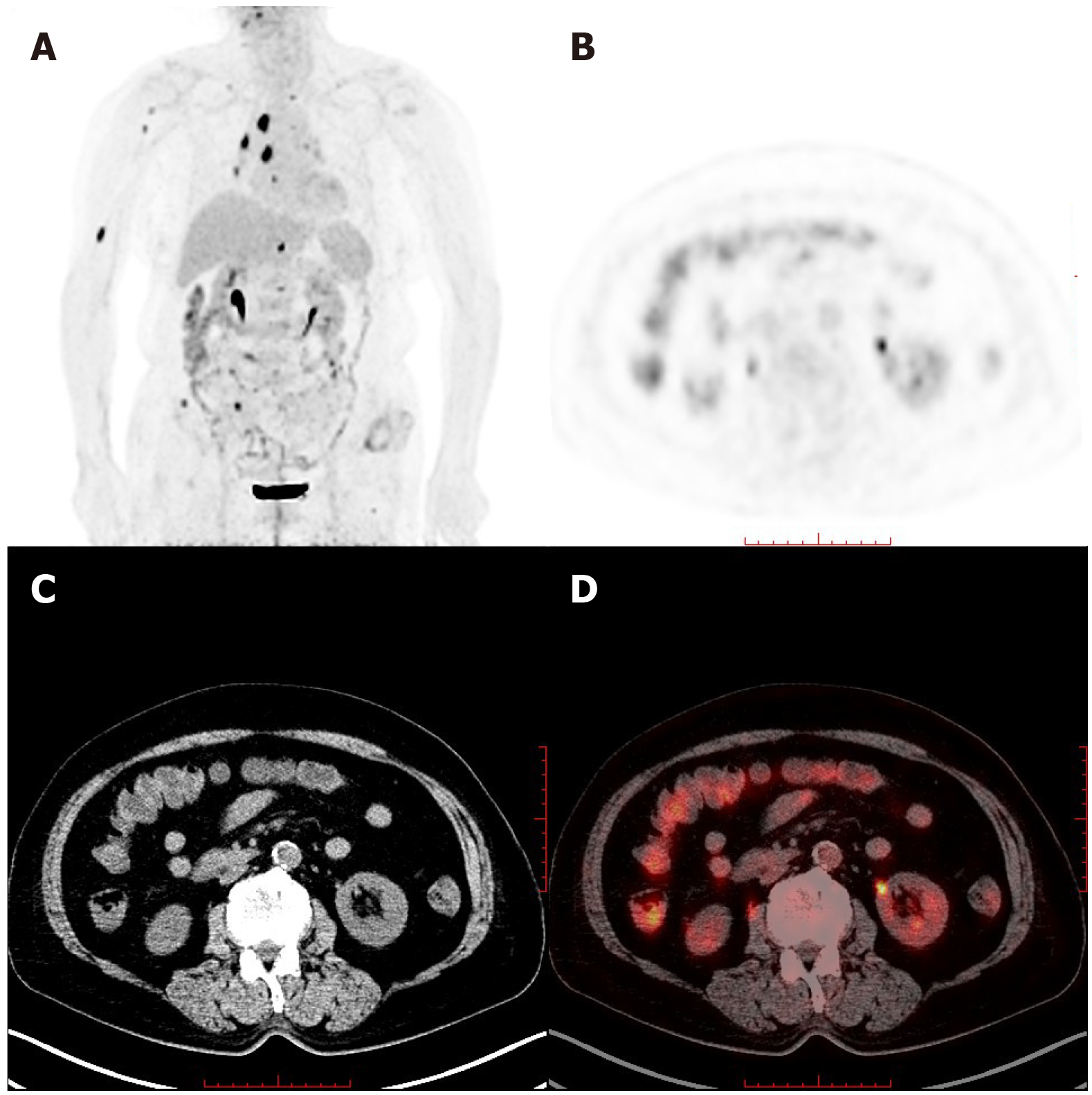
To determine whether distant metastasis occurred, additional F-18 fluorodeoxyglucose positron emission tomography/computed tomography (PET/CT) was performed. PET/CT showed tubular hypermetabolic lesions in the colon, suggesting malignancy. Furthermore, numerous hypermetabolic hilar and mediastinal lymph nodes, as well as multiple node-like foci with active F-18 fluorodeoxyglucose metabolism in the bones, were observed, revealing lymphatic and osseous metastasis (Figure 4).
Multifocal gastrointestinal epithelioid angiosarcomas with lymphatic and osseous metastasis.
The patient refused chemotherapy and died after three months due to gastrointestinal bleeding.
Angiosarcomas may arise in any part of the body, but commonly occur in skin and superficial soft tissues, with its predilection sites in the head and neck[5]. Epithelioid angiosarcoma of the gastrointestinal tract is an extremely rare neoplasm, which is only described in individual case reports and case series[6-9], with a lack of demographic morbidity data. According to literatures, vascular tumors of the stomach constitute only 0.9%-3.3% of all gastric cancers[10], while colorectal angiosarcomas represent less than 0.001% of all colorectal neoplasms[11].
Epithelioid angiosarcoma is characterized by an extremely aggressive course, leading to a very poor prognosis[12]. Even for localized disease, patients without any therapy had a 0% survival rate at 2 years[5]. Due to the infiltrative nature of this neoplasm, recurrence and metastasis are frequent after surgical resection, even for localized disease. Cytotoxic chemotherapy can be effective in a subset of patients for a limited period, but metastatic angiosarcomas remain incurable and even fatal[5]. Targeted therapy with tyrosine kinase inhibitors usually resulted in significant responses, but these tumors are prone to developing resistance[5].
In most cases of gastrointestinal angiosarcoma, the symptoms are nonspecific, including abdominal pain, weight loss and anorexia. Overt bleeding with melena or hematochezia is less common. The patient in the present report had positive antinuclear antibody and anti-SSA, which might be secondary to the tumor. Nevertheless, until now, there is no evidence that the positivity of autoimmune antibodies has association with angiosarcomas. Further studies are needed to clarify their relationships.
Almost all reported lesions that occurred in the gastrointestinal tract appeared endoscopically as centrally ulcerated, hemorrhagic, highly erythematous or purpuric nodules/masses[13]. Endoscopy with direct visualization and biopsy is crucial for diagnosis. However, endoscopic biopsy often obtains insufficient specimens and leads to the possibility of a missed diagnosis[14], similar to this case. It is well known that invasive carcinomas are likely to be covered by normal epithelium or intraepithelial neoplasm. Consequently, findings of the biopsy on their surface usually do not reflect the invasive components. Possible efforts to obtain additional histopathological findings must be made. In the present case, en bloc endoscopic mucosal resection of the suspected lesions in the colon was satisfactory for the histopathological examination. Due to the confirmation of malignant angiosarcomas, the patient refused to have another large-scale biopsy of the gastric lesion, in which the endoscopic performance was similar and typical.
Epithelioid angiosarcoma mimics carcinoma morphologically and contains numerous vasoformative structures. Because of the high architectural and cytological variability, pathological diagnosis is difficult. Immunoreactivity for endothelial and epithelial cell markers can confirm the diagnosis. This innate characteristic of epithelioid angiosarcoma corresponds to the tendency of gastrointestinal bleeding. PET/CT has been reported to detect primary uterine and pulmonary epithelioid angiosarcoma[15,16] and is of great value in identifying metastases.
We report a case of gastrointestinal bleeding that was finally diagnosed as multifocal epithelioid angiosarcomas involved in the gastrointestinal tract. The endoscopic characteristics of the lesions were highlighted and corresponded to the propensity of gastrointestinal bleeding. En bloc endoscopic mucosal resection contributed to the final histopathological diagnosis.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Perrotti S, Zhang YX S-Editor: Zhang L L-Editor: MedE-Ma JY E-Editor: Li JH
| 1. | Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ. Angiosarcoma. Lancet Oncol. 2010;11:983-991. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 538] [Cited by in RCA: 668] [Article Influence: 44.5] [Reference Citation Analysis (0)] |
| 2. | Chou JW, Cheng KS, Chen SF. Primary hepatic angiosarcoma with multifocal metastases in the gastrointestinal tract. Endoscopy. 2013;45 Suppl 2 UCTN:E319-E320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Zhai ZZ, Wang L, Zuo XL. A Rare Cause of Gastrointestinal Bleeding in a Patient With a History of Alcoholic Cirrhosis. Gastroenterology. 2019;156:e6-e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Louie J, Tejaswi S, Matsukuma K. Colonic Angiosarcoma: A Rare Gastrointestinal Malignancy. Clin Gastroenterol Hepatol. 2020;18:e75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Florou V, Wilky BA. Current and Future Directions for Angiosarcoma Therapy. Curr Treat Options Oncol. 2018;19:14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 77] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 6. | Jayaraman V, Wilkinson MN, Nagula S, Siebel M, Bucobo JC, Zee S, Buscaglia JM. Primary jejunal angiosarcoma: an extremely rare tumor diagnosed by means of anterograde spiral enteroscopy. Endoscopy. 2011;43 Suppl 2 UCTN:E219-E220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Leong J, Rascon MA, Kaushik N. Multifocal angiosarcoma of the gastrointestinal tract. Endoscopy. 2008;40 Suppl 2:E252-E253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Coumaros D, Tsesmeli N. Epithelioid angiosarcoma in the duodenal bulb. Endoscopy. 2009;41 Suppl 2:E232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Al Ali J, Ko HH, Owen D, Steinbrecher UP. Epithelioid angiosarcoma of the small bowel. Gastrointest Endosc. 2006;64:1018-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Tai CM, Hung CM, Lee TC, Chang HC, Wang HP. Primary gastric angiosarcoma presenting as an asymptomatic gastric submucosal tumor. J Formos Med Assoc. 2007;106:961-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Al Beteddini OS, Brenez D, Firket C, Algaba R, Tabech A. Colonic angiosarcoma: A case report and review of literature. Int J Surg Case Rep. 2013;4:208-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Grewal JS, Daniel AR, Carson EJ, Catanzaro AT, Shehab TM, Tworek JA. Rapidly progressive metastatic multicentric epithelioid angiosarcoma of the small bowel: a case report and a review of literature. Int J Colorectal Dis. 2008;23:745-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Saad A, Cappell MS, Amin M. Endoscopic findings with GI angiosarcoma correspond with the propensity of these vascular tumors to cause GI bleeding: two case reports and review of the literature. Dig Dis Sci. 2013;58:1797-1801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Lee CK, Chung IK, Lee SH, Kim SP, Lee SH, Lee TH, Kim HS, Park SH, Kim SJ, Lee JH, Cho HD, Oh MH. Is endoscopic forceps biopsy enough for a definitive diagnosis of gastric epithelial neoplasia? J Gastroenterol Hepatol. 2010;25:1507-1513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 15. | Treglia G, Cardillo G, Graziano P. A rare case of primary pulmonary epithelioid angiosarcoma detected by (18)F-FDG PET/CT. Clin Nucl Med. 2014;39:450-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Hwang JP, Lim SM. Uterine Epithelioid Angiosarcoma on F-18 FDG PET/CT. Nucl Med Mol Imaging. 2013;47:134-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |