Published online Jun 21, 2020. doi: 10.3748/wjg.v26.i23.3271
Peer-review started: February 14, 2020
First decision: April 9, 2020
Revised: May 9, 2020
Accepted: May 29, 2020
Article in press: May 29, 2020
Published online: June 21, 2020
Processing time: 128 Days and 5 Hours
During the perioperative period, the characteristic therapy of traditional Chinese medicine is effective in improving postoperative rehabilitation. In large-scale hospitals practicing traditional Chinese medicine, there is accumulating experience related to the promotion of fast recovery in the perioperative period.
To evaluate the efficacy and safety of Yikou-Sizi powder hot compress on Shenque acupuncture point combined with rapid rehabilitation technique.
This prospective, multicenter, randomized, controlled study included two groups: Treatment group and control group. The patients in the treatment group and control group received Yikou-Sizi powder hot compress on Shenque acupuncture point combined with rapid rehabilitation technique and routine treatment, respectively. Clinical observation regarding postoperative recovery of gastrointestinal function was performed, including the times to first passage of flatus, first defecation, and first normal bowel sounds. The comparison between groups was conducted through descriptive analysis, χ2, t, F, and rank-sum tests.
There was a statistically significant difference in the time to postoperative first defecation between the treatment and control group (87.16 ± 32.09 vs 109.79 ± 40.25 h, respectively; P < 0.05). Similarly, the time to initial recovery of bowel sounds in the treatment group was significantly shorter than that in the control group (61.17 ± 26.75 vs 79.19 ± 33.35 h, respectively; P < 0.05). However, there was no statistically significant difference in the time to initial exhaust between the treatment and control groups (51.54 ± 23.66 vs 62.24 ± 25.95 h, respectively; P > 0.05). The hospitalization expenses for the two groups of patients were 62283.45 ± 12413.90 and 62059.42 ± 11350.51 yuan, respectively. Although the cost of hospitalization was decreased in the control group, the difference was not statistically significant (P > 0.05). This clinical trial was safe without reports of any adverse reaction or event.
The rapid rehabilitation technique with integrated traditional Chinese and Western medicine promotes the recovery of postoperative gastrointestinal function and is significantly better than standard approach for patients after colorectal surgery.
Core tip: Gastrointestinal recovery is key for rapid rehabilitation during the perioperative period. Modern medicine recognizes the importance of postoperative gastrointestinal function recovery, but an effective and safe treatment for this disorder has proven limited. During the perioperative period, the characteristic therapy of traditional Chinese medicine is effective in improving postoperative rehabilitation. The aim of this prospective, randomized, controlled study was to investigate the efficacy and safety of rapid rehabilitation technique with integrated traditional Chinese and Western medicine in the recovery of gastrointestinal function in 111 patients who underwent laparoscopic surgery for colorectal cancer.
- Citation: Cao LX, Chen ZQ, Jiang Z, Chen QC, Fan XH, Xia SJ, Lin JX, Gan HC, Wang T, Huang YX. Rapid rehabilitation technique with integrated traditional Chinese and Western medicine promotes postoperative gastrointestinal function recovery. World J Gastroenterol 2020; 26(23): 3271-3282
- URL: https://www.wjgnet.com/1007-9327/full/v26/i23/3271.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i23.3271
In recent years, rapid rehabilitation during the perioperative period is attracting considerable attention. Gastrointestinal recovery is key for rapid recovery during this period. Considering the effects of surgical stress, anesthesia, and trauma inflammation, gastrointestinal dysfunction after abdominal surgery is mainly manifested as intestinal paralysis. This condition is characterized by abdominal distention, abdominal pain, nausea and vomiting, and abnormal anal exhaust and defecation. Modern medicine recognizes the importance of postoperative gastrointestinal function recovery. For this purpose, measures are taken to improve preoperative preparation and operative techniques, reduce trauma and irritation, and maintain electrolyte balance and postoperative gastrointestinal decompression. However, the method of active intervention to promote the rapid recovery of gastrointestinal function after operation remains insufficient. During the perioperative period, the characteristic therapy of traditional Chinese medicine (TCM) is effective in improving postoperative rehabilitation. In large-scale hospitals practicing TCM, there is accumulating experience related to the promotion of fast recovery in the perioperative period.
This prospective, multicenter, randomized, controlled trial assessed the efficacy and safety of Yikou-Sizi powder hot compress on Shenque acupuncture point combined with rapid rehabilitation technique in patients who underwent laparoscopic surgery for colorectal cancer.
This study was approved by the Second Affiliated Hospital of Guangzhou University of Chinese Medicine Ethics Review Committee. The registration number of the clinical study is ChiCTR-IOR-14005744. The full trial protocol can be accessed in the journal named MEDICINE.
Patients: We enrolled the patients who underwent laparoscopic surgery for colorectal cancer from December 2014 to June 2017 at four institutions, namely, the Second Affiliated Hospital of Guangzhou University of Chinese Medicine, the First Affiliated Hospital of Guangzhou University of Chinese Medicine, the Guangdong Provincial Integrative Chinese and Western Medicine Hospital, and Zhongshan Hospital of Chinese Medicine.
The inclusion criteria were: (1) Patients who had undergone laparoscopic surgery for colorectal cancer; (2) Patients aged 40–75 years; (3) The duration of surgery was 1-4 h; (4) The time of anesthesia was 1.5-4.5 h; (5) The TCM pattern belonged to the Qi stagnation and Qi deficiency; and (6) The patients provided informed consent.
The exclusion criteria were: (1) Extremely weak patients with malignant fluids in the late stage of cancer; (2) Patients with malignant tumors who required extensive radical surgery; (3) Patients with cardiovascular, liver, kidney, brain, lung, or other serious diseases, or patients with poor control of hypertension or diabetes; (4) Patients with mental illness; (5) Patients who were allergic to drugs; (6) Patients during pregnancy or lactation; (7) Patients with severe dystrophy, serum albumin < 21 g/L, or prealbumin < 0.10 g/L; (8) Repeated abdominal surgery with severe intestinal adhesion; (9) Intraoperative blood loss > 400 mL and requirement for blood transfusion during or after surgery; (10) Occurrence of severe complications within 6 h after operation, or transfer of the patient to the intensive care unit after operation due to diseases, such as multiple organ dysfunction; (11) Emergency surgery; (12) Necessity to administer a drug or therapy, known to exert effects on the gastrointestinal function after operation; (13) Patients who participated in other clinical trials within one month prior to participation in this study; and (14) Patients who were unsuitable to participate in this clinical study according to the evaluation performed by the researchers.
The elimination criteria were: (1) Patients not randomly allocated according to the regulations; (2) Patients participating in the study more than once; and (3) Patients unsuitable to participate in this study according to the screening conditions.
The exit criteria were: (1) Deterioration of the condition and lack of improvement within 3 d; (2) Development of treatment-related complications, such as severe anaphylaxis or serious adverse events; (3) Presence of severe complications or severe infection, or requirement for secondary operation during the observation period due to various reasons; and (4) The patient was no longer willing to participate in the clinical trial.
Random implementation method: The patients who met the inclusion criteria were enrolled in the clinical trial. They were randomly assigned to two groups through the central random allocation interactive network operation system. Sequentially numbered containers were used to implement the random allocation sequence. The statistical review of the study was performed by a biomedical statistician.
Sample size determination: The sample size was estimated using the two sample mean comparison method. Based on the results of the preliminary test, the times to defecation after operation in the control group and treatment group were mean1 = 134.2 h, SD1 = 31.1 and mean2 = 109.9 h, SD2 = 42.1, respectively. The above data were used to calculate the value of the overall parameter. When α = 0.05 and β = 0.10, the data were inserted into the Package for Encyclopaedia of Medical Statistics 3.1 for Windows software package (Department of Health Statistics, Huaxi School of public health, Sichuan University, China). The calculated sample size in each group was 50 patients. Accounting for a potential 15% discontinuation rate, the total estimated sample size for this study was 116 patients (58 patients per group).
The study included two groups, namely, a rapid rehabilitation treatment with integrated traditional Chinese and Western medicine group (treatment group) and a control group.
Control group: Routine basic treatment, including antibiotics, fluid support treatment, etc., was applied.
Treatment group: The preoperative, intraoperative, and postoperative patients were treated by the rapid rehabilitation technique with the TCM treatment Yikou-Sizi powder hot compress.
The technical plan for rapid rehabilitation surgery was determined according to the relevant literature[1-9] and discussions among the investigators of this study (Table 1). The TCM treatment of Yikou-Sizi powder hot compress was applied to the Shenque acupuncture point on the first day after the operation. The treatment was used twice daily (i.e., at 9:00 and 16:00) for 30 min each time. The drugs were replaced every 3 d and the treatment lasted for 7 d after surgery.
| Serial number | Measures | Treatment group (fast track surgery) | Control group |
| Preoperation | |||
| 1 | Mission | Explaining the process of rapid rehabilitation surgery to relieve patient tension: (1) Communicating with the patient prior to the operation to reduce the fear of the unfamiliar environment; (2) Explaining the preparation and cooperation prior to and after the operation, how to get out of bed for exercising as soon as possible after operation, and how to restore early drinking and eating; (3) Informing the patient regarding the time of discharge from the hospital after the operation; and (4) Performing all necessary psychological nursing to relieve anxiety in the patients prior to operation | Appropriate care for the psychological problems of the patients, health management for the disease, and adequate sleep |
| 2 | Fasting, water prohibition | Fasting 6 h, water prohibition 4 h | Overnight water prohibition and fasting prior to the operation |
| 3 | Basic disease control and support therapy | Routine treatment | Routine treatment |
| 4 | Intestinal preparation | Cleansing of intestines at 18:00 one night prior to the operation | Cleansing of intestines at 18:00 one night prior to the operation at night |
| Intraoperation | |||
| 5 | Anesthesia | General anesthesia for endotracheal intubation | General anesthesia for endotracheal intubation |
| 6 | Intraoperative heat preservation | Stabilization of the heat (i.e., use of a heated quilt to maintain the body temperature and warm distilled water to wash the wound) | Normal temperature treatment in the operation room |
| 7 | Drainage tube | Unconventional placement | Conventional placement |
| 8 | Gastric tube | Unconventional placement | Conventional placement |
| Postoperation | |||
| 9 | Restrictive rehydration | Limiting the amount of infusion, especially the intake of salt, in principle not parenteral nutrition | Conventional rehydration |
| 10 | Analgesia | Intravenous analgesia and avoidance of morphine and opioid drugs. Reference scheme: PCIA scheme 1: sulfentanyl 50–80 μg + kyffin 200 mg, initial dose: sulfentanyl 5 μg + kyffin 50 mg; PCIA scheme 2: sulfentanyl 50 μg + dezocine 30–40 mg, initial dose: sulfentanyl 5 μg + dezocine 5 mg | Intravenous analgesia and avoidance of morphine and opioid drugs. Reference scheme: PCIA scheme 1: sulfentanyl 50–80 μg + kyffin 200 mg, initial dose: sulfentanyl 5 μg + kyffin 50 mg; PCIA scheme 2: sulfentanyl 50 μg + dezocine 30–40 mg, initial dose: sulfentanyl 5 μg + dezocine 5 mg |
| 11 | Early feeding | Early enteral nutrition, initiation of liquid diet on the first day after the operation, if no discomfort; gradual recovery of semi flow diet and general diet | A full-flow diet after the anal exhaust; recovery of half-flow diet after defecation; restoration of general diet 7 d after the operation |
| 12 | Early activity | Initiation of activities on the first day after the operation | Gradual initiation of activities based on the patient’s will and recovery |
| 13 | Catheter | Removal of catheter on the first day after the operation, in the absence of prostatic hyperplasia or another urinary tract obstruction | Catheter was removed in the second day after the operation if it is not prostatic presence of hyperplasia or another urinary tract obstruction |
| 14 | Drainage tube | Removal of the tube if the drainage is < 50 mL | Regular placement for 5 to 7 d |
| 15 | Gastric tube | Removal on the second day after the operation | Routine placement until exhaust and defecation |
| 16 | Antibiotic | Use according to the principles for the clinical application of antimicrobial agents established by the Ministry of Health | Use according to the principles for the clinical application of antimicrobial agents established by the Ministry of Health |
| 17 | Medication | Conventional treatment + Yikou-Sizi powder hot compress. No use of gastrointestinal motility medicine, Chinese medicine decoction, or Chinese patent medicine. No enema treatment performed within 3 d after operation. No use of parenteral nutrition in principle | Conventional treatment, No use of gastrointestinal motility medicine, Chinese medicine decoction, or Chinese patent medicine. No enema treatment performed within 3 d after operation. No use of parenteral nutrition in principle |
Patient characteristics: Background information (i.e., name, sex, age, course of disease, medical history, etc.) was provided by the patients after admission.
Conditions and operative conditions: Such information was recorded after the operation and included the diagnosis, type and time of operation, type of anesthesia, etc.
Safety observation: Routine blood and urine tests, liver and kidney function tests, and electrocardiography were performed prior to the operation, on the first and third days after the operation, and prior to hospital discharge. The occurrence of adverse reactions/adverse events was recorded at all times. According to the normal reference values of laboratory indicators, the treating physicians judged whether the results were abnormal or had clinical significance.
Therapeutic observation: (1) Gastrointestinal function index. This included the times to recovery of first bowel sounds, first anal exhaust, and defecation, and the incidence of complications. Observations were performed by doctors every morning after treatment, on the day of surgery, and 1–7 d after surgery. The times for first anal exhaust and first defecation were recorded by the patient or families. Time to recovery of bowel sounds was calculated as time to the first normal bowel sounds minus the end time of the surgery. Time to first exhaust was calculated as time to the first exhaust minus the end time of the surgery. Time to first defecation was calculated as time to the first defecation minus the end time of the surgery.
(2) Hospitalization expenses index. This determined the total cost of hospitalization during the treatment of each patient. The discharge from hospital was based on certain criteria as follows: (a) The patients resumed a normal diet and intestinal function generally, without positive sign in abdominal examination; and (b) The patients had a normal temperature, with results of relevant laboratory tests being basically normal. Once these criteria were met, the patients were deemed safe to be discharged from hospital.
Compliance to treatment (percentage) was calculated by dividing the times of actual treatment by the times of planned treatment (i.e., twice daily).
The TCM treatment used in the study was volatile. Thus, it was difficult to perform a blinded study. The postoperative exhaust and defecation time were recorded by the patients and their families. In addition, the patients and their families were thoroughly informed by the treating physicians prior to the operation to ensure the accuracy of records. The research data were processed by a third party (New Drug Research Office in Guangdong Hospital of Traditional Chinese Medicine) to ensure an objective and accurate evaluation.
Data entry was double-checked. Statistical analyses were performed by an independent third-party statistical center.
Through the use of descriptive statistical analysis, count data are calculated as constituent ratio and frequency, and were compared between groups using the χ2 or Fisher’s exact test. Measurement data are calculated as mean ± SD, min, max, and median, and were compared between two groups using the t-test for those with normal distribution and uniform variance, or the rank-sum test for those with either non-normal distribution or non-uniform variance. The test level was α = 0.05. The statistical methods of this study were reviewed by Ai-Hua Ou from the big data research team of traditional Chinese medicine in The Second Affiliated Hospital of Guangzhou University of Chinese Medicine.
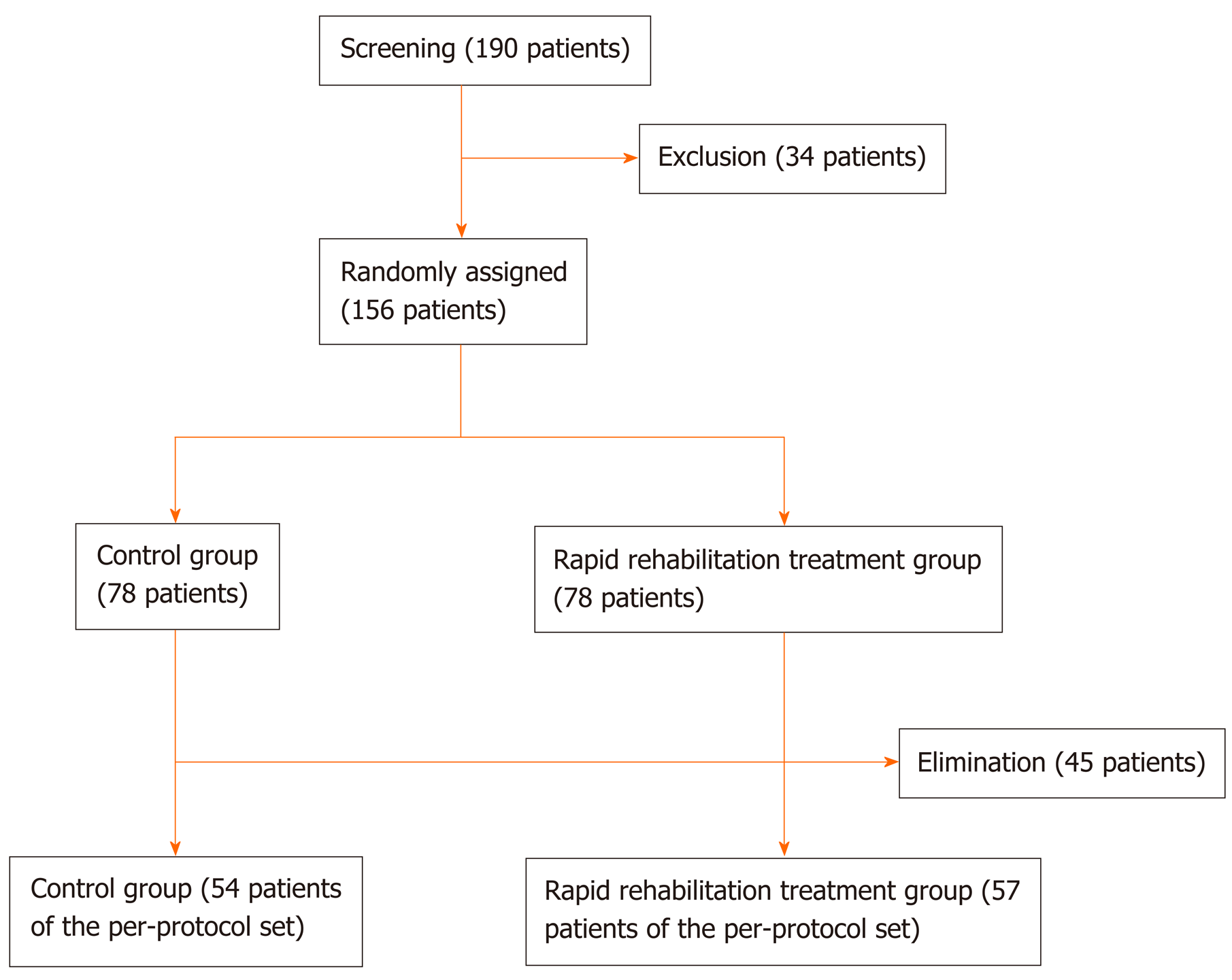
A total of 156 patients were enrolled in this study and randomly assigned to the two groups. Of those, 45 patients were excluded. Therefore, the final analysis included a total of 111 patients (Figure 1).
There was no statistically significant difference in gender, age, or operative data (i.e., anesthesia time, operative time, and intraoperative blood loss) between the two groups (P > 0.05). As shown in Table 2 and 3, the population at baseline was homogeneous.
| Control group (n = 51) | Treatment group (n = 60) | χ2 | P value | ||||
| n | % | n | % | ||||
| Sex | Male (n = 61) | 28 | 51.9 | 33 | 57.9 | 0.409 | 0.522 |
| Female (n = 50) | 26 | 48.1 | 24 | 42.1 | |||
| Control group (n = 54) | Treatment group (n = 57) | Z | P value | |
| Age (yr) | 58.28 ± 10.28 | 58.96 ± 10.95 | 0.387 | 0.699 |
| Time of anesthesia (h) | 4.71 ± 0.78 | 4.42 ± 1.07 | 1.317 | 0.188 |
| Time of operation (h) | 3.75 ± 0.76 | 3.57 ± 0.85 | 0.980 | 0.327 |
| Intraoperative bleeding (mL) | 81.93 ± 60.46 | 81.3 ± 47.31 | 0.546 | 0.585 |
Comparison of postoperative recovery of gastrointestinal function: There was a statistically significant difference in the time to postoperative first defecation between the treatment and control groups [87.16 ± 32.09 h vs 109.79 ± 40.25 h, respectively (P < 0.05)]. Similarly, there was a statistically significant difference in the time to initial recovery of bowel sounds [61.17 ± 26.75 h vs 79.19 ± 33.35 h, respectively (P < 0.05)]. However, there was no statistically significant difference in the time to initial exhaust between the two groups after the operation (P > 0.05) (Table 4, Table 5, Table 6).
| Number of patients | Time to initial exhaust after surgery (h) | Z | P value | |
| Treatment group | 57 | 51.54 ± 23.66 | 1.791 | 0.073 |
| Control group | 54 | 62.24 ± 25.95 |
| Number of patients | Time to first defecation after surgery (h) | Z | P value | |
| Treatment group | 57 | 87.16 ± 32.09 | 2.746 | 0.006a |
| Control group | 54 | 109.79 ± 40.25 |
| Number of patients | Time to initial postoperative recovery of bowel sound (h) | Z | P value | |
| Treatment group | 57 | 61.17 ± 26.75 | 3.263 | 0.001a |
| Control group | 54 | 79.19 ± 33.35 |
Comparison of hospitalization expenses: According to the analysis of variance, the total hospitalization expenses for patients in the two groups showed homogeneity; thus, we performed an independent sample t-test. The analysis revealed a non-significant reduction in hospitalization costs in the control group compared with those in the treatment group (P > 0.05) (Table 7).
| Number of patients | Total hospitalization expenses (yuan) | t | P value | |
| Treatment group | 57 | 62283.45 ± 12413.90 | 0.099 | 0.921 |
| Control group | 54 | 62059.42 ± 11350.51 |
General situation: During the period of clinical observation, there were no adverse reactions observed in either group. There were no abnormal changes in the three routine examinations, biochemical indicators, stress indicators, inflammatory markers, or electrocardiogram.
Complications: In terms of complications, there was one case in the treatment group and four cases in the control group (Table 8).
| Category | Treatment group (57 patients) | Control group (54 patients) |
| Postoperative anastomotic fistula | 0 | 0 |
| Postoperative ileus | 0 | 1 |
| Postoperative abdominal infection | 0 | 1 |
| Postoperative infection of incisional incision | 1 | 1 |
| Postoperative pulmonary infection | 0 | 0 |
| Postoperative urinary tract infection | 0 | 1 |
| Postoperative deep venous thrombosis | 0 | 0 |
| Other postoperative complications | 0 | 0 |
| Total | 1 | 4 |
According to the 2015 National Cancer Statistics announced by the Chinese National Cancer Center, the incidence of colorectal cancer and mortality associated with this disease in China has shown a gradually ascending trend. Colorectal cancer ranks fifth[10] among all malignant tumors in terms of incidence and mortality. Surgery is the most effective treatment for colorectal cancer. At present, the diagnosis and treatment of colorectal cancer are based on the combination of surgery with multiple treatment modalities, including radiotherapy, chemotherapy, biological therapy, immunotherapy, targeted therapy, etc. Minimally invasive surgery is the preferred mode of operation. With the increasing interest in the concept of rapid rehabilitation, rapid rehabilitation programs for patients with colorectal surgery have been developed and widely recognized. Using various means of treatment and rehabilitation supported by clinical evidence, these programs reduce the stress response and related complications.
During the perioperative period, the characteristic therapy of TCM is also effective in improving postoperative rehabilitation. In large-scale hospitals practicing TCM, there is accumulating experience related to the promotion of fast recovery in the perioperative period. The results of previous clinical research showed that the external treatment of TCM (i.e., Evodia rutaecarpa hot compress in the Shenque acupoint plus electroacupuncture in the Zusanli acupoint) was safe and effective in promoting the recovery of gastrointestinal function in patients who underwent abdominal surgery[11]. Therefore, by employing the latest advances in TCM and Western medicine, we combined external therapy with the rapid rehabilitation program to form a perioperative fast recovery technique. In addition, we selected laparoscopic surgery for colorectal cancer as the model for this prospective, randomized, and controlled trial to explore the role of this rapid rehabilitation technique in early rehabilitation. We observed that the combined rapid rehabilitation technique promoted the recovery of gastrointestinal function after laparoscopic colorectal surgery.
This study had some limitations. First, the TCM treatment used in the study was volatile. Thus, it was difficult to perform a blinded study, which may have impact on the primary outcomes and secondary outcomes. Moreover, early postoperative enteral feeding and mobilization after surgery could be essential for the study results, which were different in ERAS surgical protocols. Finally, painkillers were used for postoperative pain management, including opioids, tramadol, dexmedetomidine, and so on. The medication relieving pain for the patients was individualized. However, it could take effects on monitored symptoms which were recorded by the doctors and patients.
Optimization of Yikou-Sizi powder: The external treatment of TCM used in previous studies was Evodia rutaecarpa hot compress on the Shenque acupoint plus electroacupuncture in the Zusanli acupoint. Prior to this study, we initially optimized the prescription and appearance of the external application package of the TCM. The prescription was as follows: 150 g of Fructus Evodiae (Wu Zhu Yu), 200 g of Fructus Amomum tsaoko (Cao Guo), 100 g of Alpiniae katsumadai (Cao Dou Kou), and 100 g of Fructus Alpiniae oxyphyllae (Yi Zhi Ren).
Fructus Evodiae (Wu Zhu Yu) tending to warm and diffuse is helpful for the recovery of the gastrointestinal function.
Fructus Amomum tsaoko (Cao Guo) is the dried ripe fructus of the Zingiberaceae vegetation tsaoko. It is spicy and bitter with special flavor. The pungent, warm, and fiery nature of Fructus Amomum tsaoko promotes the recovery of gastrointestinal function.
Alpiniae katsumadai (Cao Dou Kou) is the dried nearly mature seed of the Zingiberaceae vegetation Alpiniae katsumadai. It is fragrant, spicy, and bitter. It is efficacious in warming the stomach and preventing vomiting.
Fructus Alpiniae oxyphyllae (Yi Zhi Ren) is the dried ripe fructus of the Zingiberaceae vegetation Alpiniae oxyphyllae, also known as Yi Zhi Zi, Zhi Ren, and Yi Zhi. With its special aroma, and pungent and bitter taste, it regulates gastrointestinal function.
The application of a hot compress on the Shenque acupoint may promote the recovery of gastrointestinal function. The external application package of the Yikou-Sizi powder is shown as Figure 2.
Point selection on the Shenque: Shenque is a common acupoint used in the external application of TCM. The Shenque is located in the center of the umbilical fossa. According to TCM, the umbilical fossa is a congenital cord and acquired Qi shelter between the middle and lower Jiao. The Shenque acupoint is most closely related to the spleen, stomach, and kidneys. By stimulating the point to follow the umbilicus meridian access to disease, it exerts its influence through dredging of the meridians, adjustment of organ function, and relaxing the bowels. Because the Shenque acupoint belongs to the Ren channel and its anatomic sites is located in the center of the abdomen, and the adjacent organs of the stomach, liver, gallbladder, pancreas, and intestines belong to the digestive system, the Shenque acupoint plays an important role in the treatment of diseases of the digestive system. Because it is a special acupoint, it is usually not needled, and TCM hot compress or moxibustion is often used.
We performed an analysis of the times to postoperative first exhaust, defecation, and recovery of bowel sounds. The results showed that in the treatment group using the rapid rehabilitation technique, the time to the first exhaust and time to the first defecation were 51.54 ± 23.66 h and 87.16 ± 32.09 h, respectively. In the control group, these values were 62.24 ± 25.95 h and 109.79 ± 40.25 h, respectively. These findings showed that the times to exhaust and defecation in the treatment group were shortened compared with those in the control group. Notably, the difference in the time to first defecation was statistically significant (P < 0.05). The times to recovery of bowel sounds in the treatment and control groups were 61.17 ± 26.75 h and 79.19 ± 33.35 h, respectively, and the difference was statistically significant (P < 0.05). Furthermore, according to the report, the inevitable recovery obstacle time of gastrointestinal function after abdominal operation is 0–1 d in the small intestine, 1–2 d in the stomach, and 2–3 d in the colon[12,13]. In the present study, the recovery time of gastrointestinal function in the treatment group was reduced significantly compared with that reported in the control group. This finding demonstrates that the rapid rehabilitation technique with integrated TCM and Western medicine exerts a beneficial effect on the recovery of gastrointestinal function after operation.
The cost of hospitalization in the treatment group was 62283.45 ± 12413.90 yuan, while that in the control group was 62059.42 ± 11350.51 yuan. Although the hospitalization expenses in the control group were lower than those in the treatment group, the difference between the two groups was not statistically significant (P > 0.05).
Safety is a key indicator of the applicability of a technology to the clinic. During the period of clinical observation, there were no abnormal changes noted in the three routine examinations, biochemical indices, and electrocardiograms between the two groups. This indicated that the patients in the two groups exhibited a favorable safety profile during the perioperative period, without obvious adverse reactions. Regarding complications, one patient in the treatment group developed postoperative incision infection. In the control group, the following complications were observed: One incision infection, one abdominal infection, one ileus, and one urinary tract infection. The symptoms in patients with complications were controlled and improved after symptomatic treatment.
This clinical study showed that the rapid rehabilitation technique with integrated YiKou-Sizi powder hot compress and Western Medicine significantly shortened the times to first defecation and initial recovery of bowel sounds, without increasing hospitalization expenses. And there was no abnormal change in safety indexes in the two groups. In conclusion, the rapid rehabilitation technique with integrated TCM and Western Medicine exerts positive effects on postoperative gastrointestinal function recovery with a favorable safety profile and is significantly better than standard approach for patients after colorectal surgery. Therefore, this rapid rehabilitation technique with integrated TCM and Western Medicine is worthy of further clinical investigation.
In recent years, rapid rehabilitation during the perioperative period is attracting considerable attention. Gastrointestinal dysfunction is key for rapid recovery during this period. Modern medicine recognizes the importance of postoperative gastrointestinal function recovery. However, the method of active intervention to promote the rapid recovery of gastrointestinal function after surgery remains insufficient. Therefore, it is essential to find an effective and safe method that promotes postoperative gastrointestinal function recovery.
During the perioperative period, the characteristic therapy of traditional Chinese medicine is effective in improving postoperative rehabilitation and rapid rehabilitation technique has been developed and widely recognized. Therefore, the combination of these two methods is the best treatment.
To evaluate the efficacy and safety of Yikou-Sizi powder hot compress on Shenque acupuncture point combined with rapid rehabilitation technique.
In this prospective, multicenter, randomized, and controlled study, the patients in a treatment group received Yikou-Sizi powder hot compress in Shenque acupuncture point combined with rapid rehabilitation technique, and routine treatments were applied to patients in a control group. Clinical observation regarding postoperative recovery of gastrointestinal function was performed, including the times to first passage of flatus, first defecation, and first normal bowel sounds.
Patients had shortened times to postoperative first defecation and initial recovery of bowel sounds in the treatment group compared with those in the control group. There was no statistically significant difference in the time to initial exhaust and hospitalization expenses between treatment group and control group. This clinical trial was safe without reports of any adverse reaction or event.
The rapid rehabilitation technique with integrated traditional Chinese and Western medicine promotes the recovery of postoperative gastrointestinal function and is significantly better than standard approach for patients after colorectal surgery.
Our study suggests that Yikou-Sizi powder hot compress in Shenque acupuncture point combined with rapid rehabilitation technique is effective in improving postoperative rehabilitation. Further studies are required to conduct in multiple centers to promote and apply the treatment so that more patients can recover fully and rapidly.
We wish to acknowledge Professor Ai-Hua Ou, who gave us much help with statistical methodology.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification:
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Madalinski M S-Editor: Zhang L L-Editor: Wang TQ E-Editor: Zhang YL
| 1. | Li L, Jin J, Min S, Liu D, Liu L. Compliance with the enhanced recovery after surgery protocol and prognosis after colorectal cancer surgery: A prospective cohort study. Oncotarget. 2017;8:53531-53541. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 39] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 2. | Price BA, Bednarski BK, You YN, Manandhar M, Dean EM, Alawadi ZM, Bryce Speer B, Gottumukkala V, Weldon M, Massey RL, Wang X, Qiao W, Chang GJ. Accelerated enhanced Recovery following Minimally Invasive colorectal cancer surgery (RecoverMI): a study protocol for a novel randomised controlled trial. BMJ Open. 2017;7:e015960. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | van Zelm R, Coeckelberghs E, Sermeus W, De Buck van Overstraeten A, Weimann A, Seys D, Panella M, Vanhaecht K. Variation in care for surgical patients with colorectal cancer: protocol adherence in 12 European hospitals. Int J Colorectal Dis. 2017;32:1471-1478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 4. | Venara A, Barbieux J, Mucci S, Talbot MF, Lermite E, Hamy A. Short-Term Outcomes of Colorectal Resection for Cancer in Elderly in the Era of Enhanced Recovery. Scand J Surg. 2018;107:31-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Brescia A, Tomassini F, Berardi G, Sebastiani C, Pezzatini M, Dall'Oglio A, Laracca GG, Apponi F, Gasparrini M. Development of an enhanced recovery after surgery (ERAS) protocol in laparoscopic colorectal surgery: results of the first 120 consecutive cases from a university hospital. Updates Surg. 2017;69:359-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Shah PM, Johnston L, Sarosiek B, Harrigan A, Friel CM, Thiele RH, Hedrick TL. Reducing Readmissions While Shortening Length of Stay: The Positive Impact of an Enhanced Recovery Protocol in Colorectal Surgery. Dis Colon Rectum. 2017;60:219-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 57] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 7. | ERAS Compliance Group. The Impact of Enhanced Recovery Protocol Compliance on Elective Colorectal Cancer Resection: Results From an International Registry. Ann Surg. 2015;261:1153-1159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 415] [Cited by in RCA: 476] [Article Influence: 52.9] [Reference Citation Analysis (0)] |
| 8. | van Zelm R, Janssen I, Vanhaecht K, de Buck van Overstraeten A, Panella M, Sermeus W, Coeckelberghs E. Development of a model care pathway for adults undergoing colorectal cancer surgery: Evidence-based key interventions and indicators. J Eval Clin Pract. 2018;24:232-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Moya P, Soriano-Irigaray L, Ramirez JM, Garcea A, Blasco O, Blanco FJ, Brugiotti C, Miranda E, Arroyo A. Perioperative Standard Oral Nutrition Supplements Versus Immunonutrition in Patients Undergoing Colorectal Resection in an Enhanced Recovery (ERAS) Protocol: A Multicenter Randomized Clinical Trial (SONVI Study). Medicine (Baltimore). 2016;95:e3704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 88] [Cited by in RCA: 96] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 10. | Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11444] [Cited by in RCA: 13210] [Article Influence: 1467.8] [Reference Citation Analysis (3)] |
| 11. | Chen Z, Cao L, Wen Z, Cui N, Li N, Xie J, Tan Z, Luo Z, Wang S, Qin Y, Chen X, Xu Z, Ou A, Shang W, Jiang Z, Chen Q. Study of Evodia hot compress plus electro-acupuncture in patients who have undergone abdominal surgery. Int J Clin Exp Med. 2015;8:16167-16174. [PubMed] |
| 12. | Holte K, Kehlet H. Postoperative ileus: a preventable event. Br J Surg. 2000;87:1480-1493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 395] [Cited by in RCA: 373] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 13. | Livingston EH, Passaro EP Jr. Postoperative ileus. Dig Dis Sci. 1990;35:121-132. [PubMed] |