Published online Dec 21, 2019. doi: 10.3748/wjg.v25.i47.6813
Peer-review started: September 23, 2019
First decision: November 4, 2019
Revised: November 20, 2019
Accepted: December 7, 2019
Article in press: December 7, 2019
Published online: December 21, 2019
Processing time: 88 Days and 1.6 Hours
Ulcerative colitis (UC) is a chronic, nonspecific intestinal inflammatory disease with undefined pathogenesis. Non-SMC condensin I complex subunit D2 (NCAPD2) and non-SMC condensin II complex subunit D3 (NCAPD3) play pivotal roles in chromosome assembly and segregation during both mitosis and meiosis. To date, there has been no relevant report about the functional role of NCAPD2 and NCAPD3 in UC.
To determine the level of NCAPD2/3 in intestinal mucosa and explore the mechanisms of NCAPD2/3 in UC.
Levels of NCAPD2/3 in intestinal tissue were detected in 30 UC patients and 30 healthy individuals with in situ hybridization (ISH). In vitro, NCM60 cells were divided into the NC group, model group, si-NCAPD2 group, si-NCAPD3 group and si-NCAPD2+si-NCAPD3 group. Inflammatory cytokines were measured by ELISA, IKK and NF-κB were evaluated by western blot, and IKK nucleation and NF-κB volume were analyzed by immunofluorescence assay.
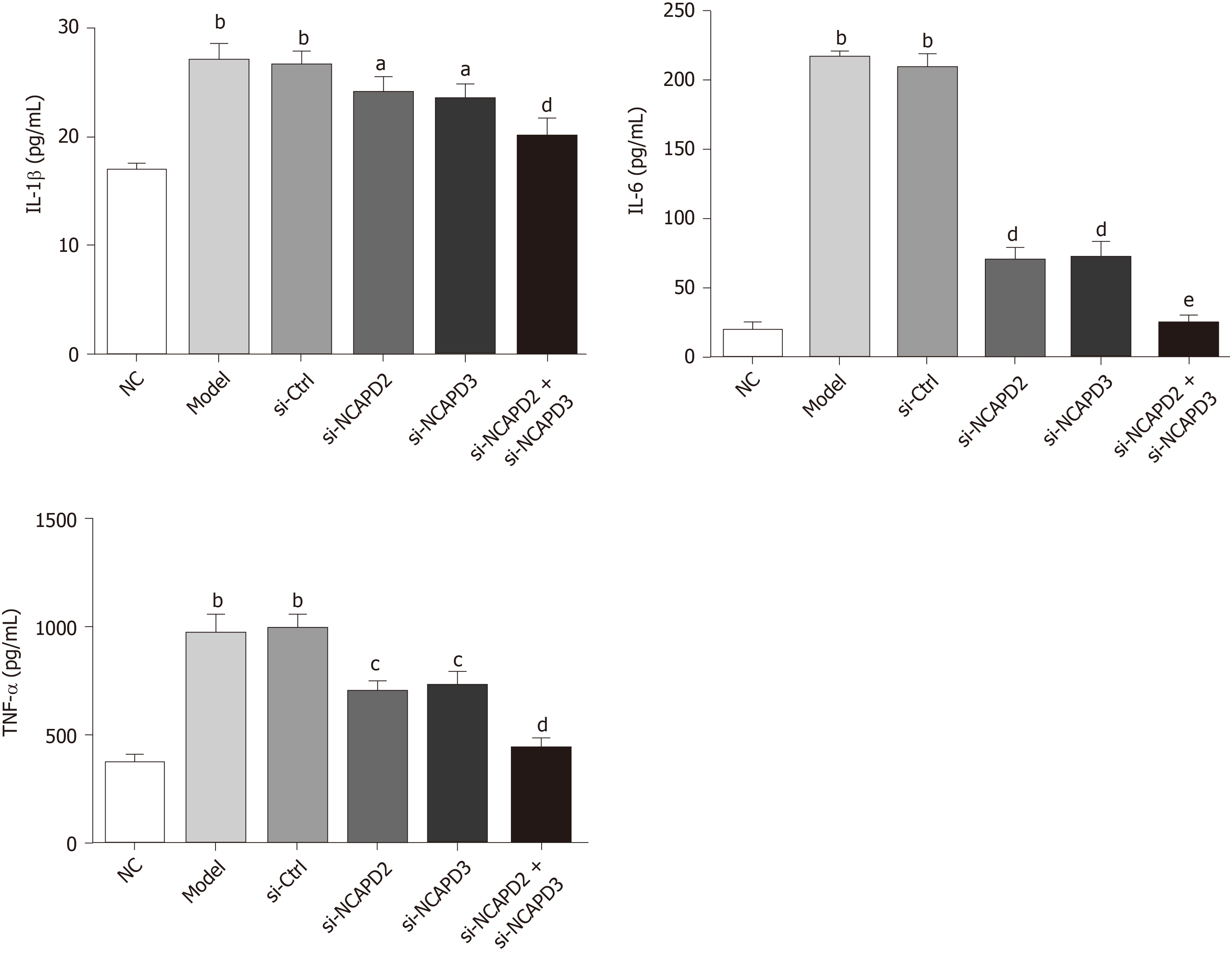
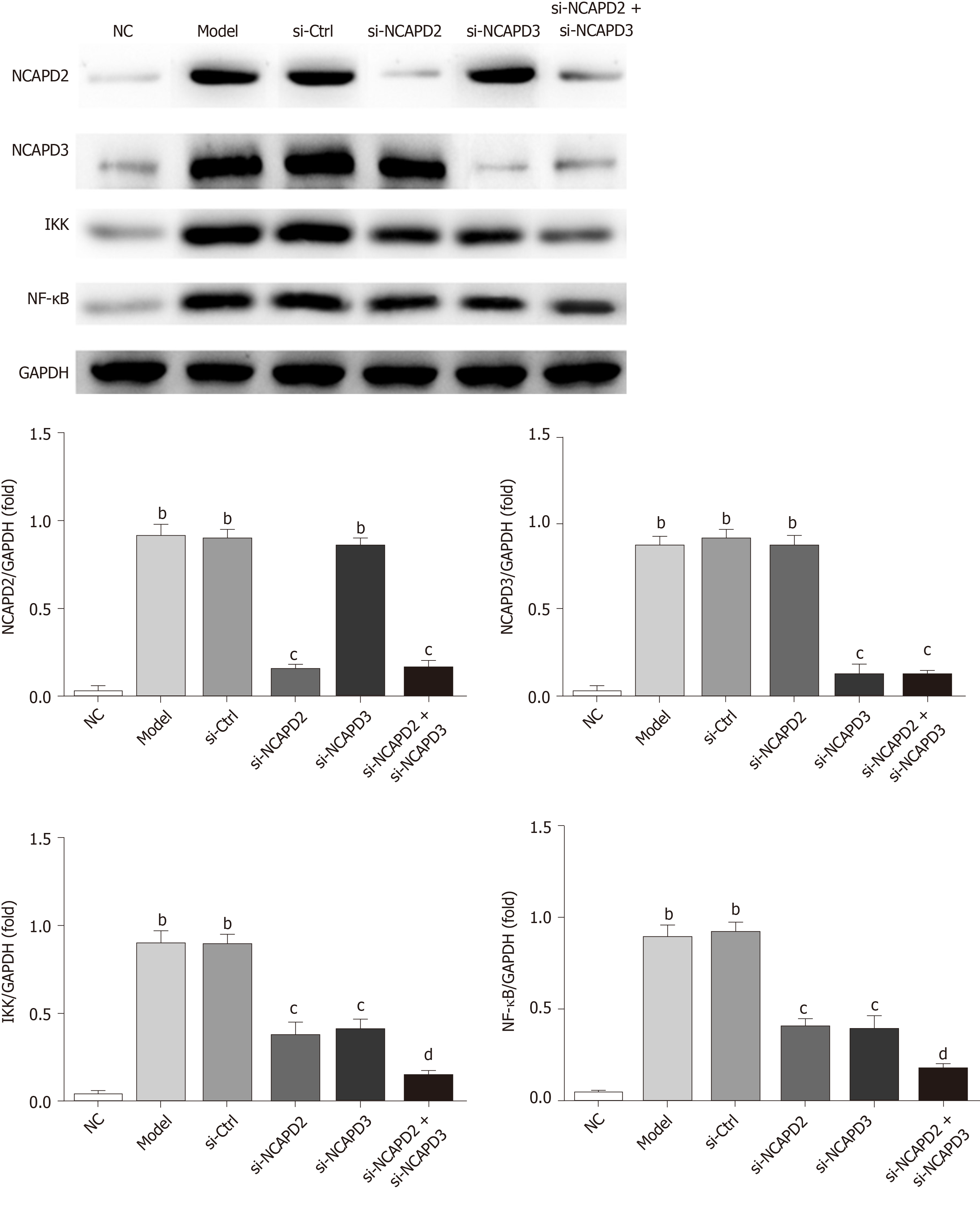
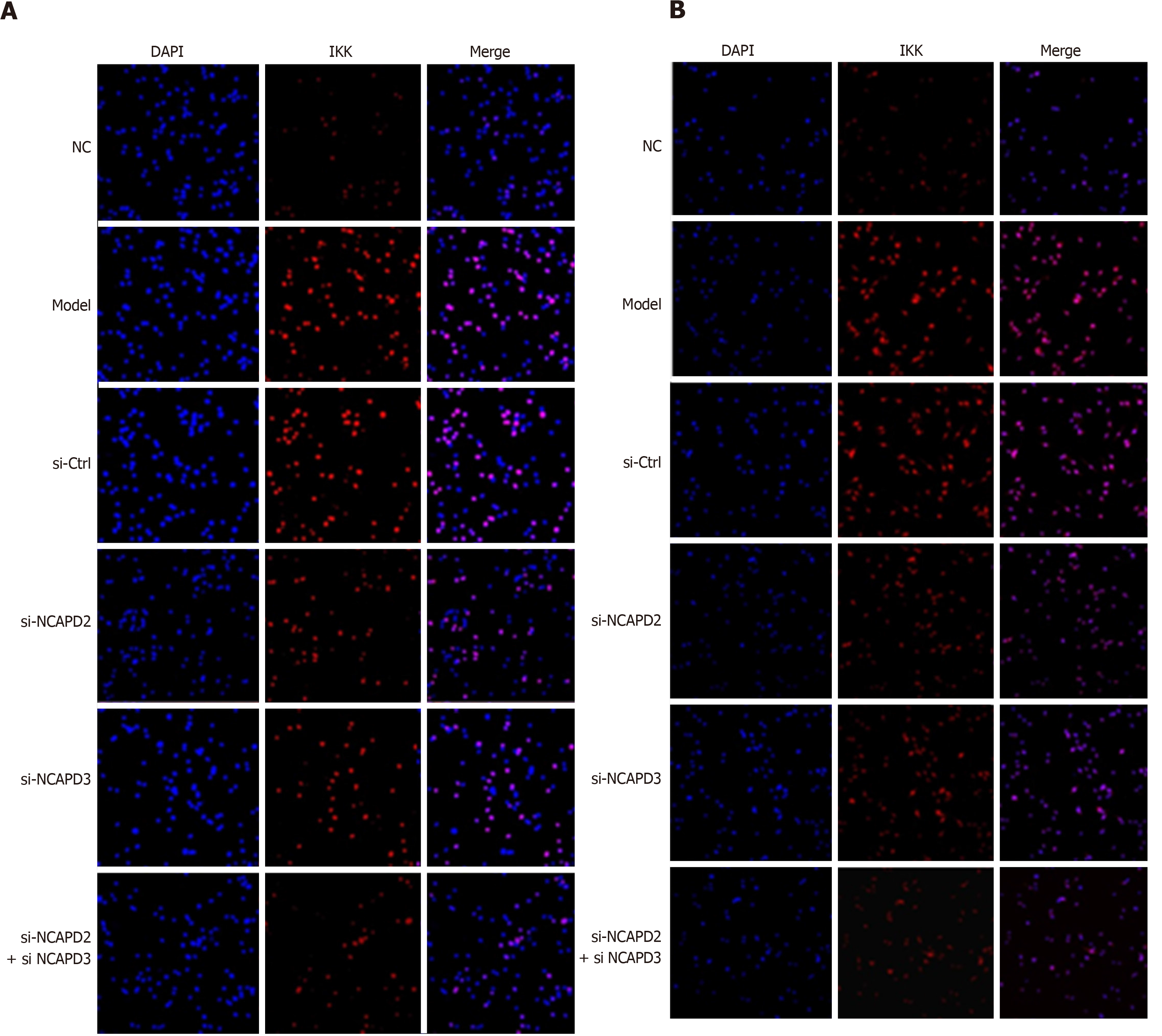
Compared with expression in healthy individuals, NCAPD2 and NCAPD3 expression in intestinal tissue was significantly upregulated (P < 0.001) in UC patients. Compared with levels in the model group, IL-1β, IL-6 and TNF-α in the si-NCAPD2, si-NCAPD3 and si-NCAPD2+si-NCAPD3 groups were significantly downregulated (P < 0.01). IKK and NF-κB protein expression in the si-NCAPD2, si-NCAPD3 and si-NCAPD2+si-NCAPD3 groups was significantly decreased (P < 0.01). Moreover, IKK nucleation and NF-κB volume were suppressed upon si-NCAPD2, si-NCAPD3 and si-NCAPD2+ si-NCAPD3 transfection.
NCAPD2/3 is highly expressed in the intestinal mucosa of patients with active UC. Overexpression of NCAPD2/3 promotes the release of pro-inflammatory cytokines by modulating the IKK/NF-κB signaling pathway.
Core tip: In this study, non-SMC condensin I complex subunit D2 (NCAPD2) and non-SMC condensin II complex subunit D3 (NCAPD3) expression levels have been confirmed to be significantly up-regulated in the intestinal mucosa of patients with active UC. In vitro, the data suggested that silencing NACPD2 and NACPD3 could depress the expression of IL-1β, IL-6 and TNF-α. Further, knockdown of NACPD2 and NACPD3 could remarkably suppress IKK nucleation and NF-κB volume. These results suggest that NACPD2 and NACPD3 are over-expressed in the intestinal mucosa of patients with UC, and overexpression of NCAPD2/3 promotes the release of pro-inflammatory cytokines by modulating the IKK/NF-κB signaling pathway.
- Citation: Yuan CW, Sun XL, Qiao LC, Xu HX, Zhu P, Chen HJ, Yang BL. Non-SMC condensin I complex subunit D2 and non-SMC condensin II complex subunit D3 induces inflammation via the IKK/NF-κB pathway in ulcerative colitis. World J Gastroenterol 2019; 25(47): 6813-6822
- URL: https://www.wjgnet.com/1007-9327/full/v25/i47/6813.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i47.6813
Inflammatory bowel disease (IBD) is a chronic, nonspecific intestinal inflammatory disease with undefined pathogenesis, and includes ulcerative colitis (UC) and Crohn’s disease[1]. The course of IBD is prolonged and repetitive. Although there are many medical treatments for the disease, the effects of treatment are unsatisfactory and the prognosis is poor, which seriously affects patient quality of life, exhausts many health resources and is one of the precancerous lesions of intestinal tumors[2,3].
One of the biggest problems in the diagnosis of IBD is the differential diagnosis of infectious intestinal disease, with the most difficult being the differential diagnosis of intestinal tuberculosis[4]. In recent years, many reports have found that serological markers have great value in the differential diagnosis of IBD. Therefore, the search and development of clinical biomarkers that can accurately diagnose IBD and monitor the status of IBD disease progression have important significance and value for improving the clinical treatment of IBD patients[5,6].
Non-SMC condensin I complex subunit D2 (NCAPD2) and non-SMC condensin II complex subunit D3 (NCAPD3) play key roles in chromosomal structural changes and separation during the process of eukaryotic cell mitosis[7,8]. NCAPD2 and 3 are subunits of condensin I and condensin II, respectively. Condensin is of vital importance in the contraction and separation of chromosomes during eukaryotic cell mitosis. When NCAPD2 and NCAPD3 function abnormally, abnormal chromosome structure can occur, leading to mitotic cell abnormalities. Studies have shown that the NCAPD2 gene is associated with Parkinson’s disease in Han Chinese people, and is correlated with gender and age[9]. Patients with high NCAPD3 expression have a lower postoperative recurrence rate after receiving prostatic cancer surgery. NCAPD3 can be used as a postoperative prognostic indicator of prostatic cancer[10]. Yin et al[11] found that high expression of NCAPH, a NCAPD3 homologous complex, promotes colonic cancerous cell proliferation. It has been reported that NCAPD3 plays an important role in microbial immunity and in the process of human intestinal epithelial cells to clear bacteria[12]. In this study, the role and possible mechanisms of NCAPD2/3 in the development of UC was explored.
Paraffin-embedded intestinal tissue specimens from colonoscopies were collected from 30 patients with active UC (Mayo endoscopic score > 2) and 30 age- and sex-matched healthy people (Mayo endoscopic score = 0) between October 2016 and September 2017. These samples were analyzed retrospectively using protocols approved by the ethics committee of the Affiliated Hospital of Nanjing University of Chinese Medicine (2018NL-170-02). The information regarding the tissue samples used for in situ Hybridization (ISH) in this study is provided in Table 1. As a retrospective study using discarded tissue, the ethics committee agreed to the use of these samples and waived informed consent.
| Normal control, n = 30 (%) | Ulcerative colitis1, n = 30 (%) | |
| Age in yr | ||
| A2 (18-40) | 16 (53.3) | 17 (56.7) |
| A3 (≥ 40) | 14 (46.7) | 13 (43.3) |
| Sex | ||
| Male | 15 (50.0) | 14 (46.7) |
| Female | 15 (50.0) | 16 (53.3) |
| Tissue sampling site | ||
| Transverse colon | 2 (6.7) | 3 (10.0) |
| Descending colon | 7 (23.3) | 6 (20.0) |
| Sigmoid colon | 13 (43.3) | 9 (30.0) |
| Rectum | 8 (26.7) | 12 (40.0) |
| Therapy | ||
| 5-ASA | N/A | 13 (43.4) |
| Corticosteroids | N/A | 4 (13.3) |
| 5-ASA/corticosteroids | N/A | 3 (10.0) |
| Immunomodulators/corticosteroids | N/A | 1 (3.3) |
| Chinese herbal medicine | N/A | 5 (16.7) |
| No treatment | N/A | 4 (13.3) |
Paraffin sections were routinely dewaxed with water, and 50 μL of levamisole was added, incubated at room temperature for 30 min and washed with high pressure water three times for 3 min each. Then, 50 μL of 1 × proteinase K was added, incubated at 37 °C for 20 min and washed with distilled water once for 3 min. For prehybridization, pre-hybrid solution was placed on each slide and incubated at 42 °C for 2-4 h. The excess liquid was drained, and 50 μL probe hybridization solution was added to each slide (NCAPD2 and NCAPD3 were purchased from Wuhan Boster Biological Technology Company) and hybridized at 42 °C overnight. SSC liquid elution was performed in a 37 °C water bath using the following parameters: 2 × SSC wash for 5 min twice, 0.5 × SSC wash for 15 min twice, and 0.2 × SSC wash for 15 min twice. Then, slides were incubated in 50 μL 1 × sealed protein solution at 37 °C for 30 min, and excess liquid was drained off without washing. The slides were incubated with 50 μL of rabbit anti-digoxin (1:100 dilution) at 37 °C for 1 h, followed by incubation with 50 μL of AP-sheep anti-rabbit IgG (1:100 dilution) at 37 °C for 1 h. NBT/BCIP was used for color development, and the reaction was stopped at any time by microscopy. Gradient ethanol was used for dehydration, xylene for transparence, and neutral gum to seal the slides. The probe-containing hybridization solution was replaced by a probe-free hybridization buffer solution for the negative control. Image-ProPlus 6.0 image analysis software was used for image analysis, and the average OD was calculated. Then, the average view value was used as the expression quantity of the specimen.
After normal recovery, NCM460 cells (ATCC, United States), which are normal colonic epithelial cells, were cultured in a thermostatic incubator using RPMI 1640 culture medium (37 °C, 5% CO2). NCM460 cells were divided into the normal control group (NC group), model group, si-NCAPD2 transfection group (si-NCAPD2 group), si-NCAPD3 transfection group (si-NCAPD3 group) and si-NCAPD2 plus si-NCAPD3 group (si-NCAPD2+si-NCAPD3 group). The NC group cells were cultured in normal culture medium. After transfection with si-NCAPD2 and si-NCAPD3 (Nanjing KeyGen Biotech Co., Ltd., Nanjing, China), the si-NCAPD2, si-NCAPD3 and si-NCAPD2+si-NCAPD3 groups, along with the model group, were stimulated with 50 ng/mL of LPS (Sigma, United States).
After 48 h of cell culture, cell culture medium from each group was collected. IL-1β, IL-6 and TNF-α levels in the culture medium of each group were detected according to the instructions for the IL-1β, IL-6 and TNF-α kits (Sigma, United States).
The cells were lysed using RIPA lysis buffer to collect protein. The total protein concentration was determined by BCA colorimetry assay. Then, 40 μg of protein was loaded into each well of the gel. After electrophoresis and transfer of proteins from the gel to a membrane, the membrane was blocked with 5% nonfat dried milk. The membrane was washed with TBST three times, and NCAPD2 (Abnova, Taiwan, China) (1: 1000), NCAPD3 (Proteintech Group, United States) (1:1000), IKK, NF-κB (Abeam, Cambridge, United Kingdom) (1:1000) and GAPDH antibodies (1: 1000) were added and incubated overnight at 4°C. After the membrane was washed with TBST three times, the second antibody (1:1000) was incubated for 1 hour and ECL was used for image development. Protein gray values in each group were read.
After being treated for 48 h, each group of cells was fixed with 4% paraformaldehyde for 30 min, ruptured with 0.01% Triton X-100 for 10 min, and blocked with 0.1% bovine serum albumin for 30 min. After washing with PBST, diluted primary IKK or NF-κB antibody (Abcam, Cambridge, United Kingdom) was added and incubated overnight at 4°C. Sheep anti-rabbit IgG-Cy3 (1:50) and sheep anti-mouse IgG-FITC (1:50) secondary antibodies were added and incubated at room temperature in the dark for 30 min. The nuclei were stained with DAPI, and the slides were sealed with glycerol. The staining results were observed under a laser scanning confocal microscope. Image analysis software IPP 6.0 was used to analyze the surface density, optical density, and number of positive cells in each image.
All numerical data were processed with SPSS 22.0. One-way analysis of variance was used for inter-group comparisons. Experimental data are expressed as the mean ± SD. P < 0.05 indicated that the difference was statistically significant.
Mucosal samples were taken during colonoscopy from inflamed rectal or colonic mucosa of 30 patients with active UC, as well as of 30 age- and sex-matched controls (Table 1). The patients with active UC were defined as having a Mayo endoscopic score > 2. Location of the samples acquired and the ongoing treatment are shown in Table 1. Compared with expression in healthy individuals, NCAPD2 and NCAPD3 expression in intestinal tissues of UC patients was significantly increased (P < 0.001) by ISH assay. The relevant data are shown in Figure 1.
ELISA results showed that the IL-1β, IL-6 and TNF-α concentrations of the Model and si-Ctrl groups were significantly upregulated compared with those of the NC group (P < 0.01). Upon si-NCAPD2 or/and si-NCAPD3 transfection, the IL-1β, IL-6 and TNF-α concentrations of the si-NCAPD2, si-NCAPD3 and si-NCAPD2+ si-NCAPD3 groups were significantly decreased compared with those of the Model group (P < 0.05, P < 0.01 and P < 0.001, respectively). The relevant data are shown in Figure 2.
To evaluate relative protein expression, we measured the expression of NCAPD2, NCAPD3, IKK and NF-κB by western blot (WB) assay. The results showed that NCAPD2, NCAPD3, IKK and NF-κB protein expression in the Model and si-Ctrl groups was significantly increased compared with that of the NC group (P < 0.001). Moreover, NCAPD2 protein expression in the si-NCAPD2 and si-NCAPD2+ si-NCAPD3 groups was significantly suppressed compared with that of the Model group (P < 0.01). NCAPD3 protein expression in the si-NCAPD3 and si-NCAPD2+ si-NCAPD3 groups was significantly suppressed compared with that of the Model group (P < 0.01). Protein expression of IKK and NF-κB in the si-NCAPD2, si-NCAPD3 and si-NCAPD2+si-NCAPD3 groups was significantly downregulated compared with that of the Model group (P < 0.01 and P < 0.001, respectively). The relevant data are shown in Figure 3.
Immunofluorescence results in Figure 4A show that the IKK nuclear volume increased in the Model and si-Ctrl groups compared with that of the NC group; however, with si-NCAPD2 or/and si-NCAPD3 transfection, the IKK nuclear volume was reduced. Figure 4B shows that the NF-κB volume increased in the Model and si-Ctrl groups compared with that of the NC group. However, upon si-NCAPD2 or/and si-NCAPD3 transfection, the NF-κB volume was reduced.
UC is a chronic nonspecific inflammatory disease of the rectum and colon that occurs due to intestinal immune abnormalities based on certain hereditary susceptibility, and is affected by environmental factors and enteric microorganisms[10,13]. Previous studies have found that NCAPD2/3 is closely related to the occurrence of various diseases[7,8]. Whether NCAPD2/3 is correlated with the development of UC remains unclear. In this study, the expression levels of NCAPD2 and NCAPD3 in UC intestinal tissues were first detected using ISH. The results showed that the expression levels of NCAPD2 and NCAPD3 were significantly increased in UC intestinal tissues, suggesting that the high expression of NCAPD2/3 might be the key factor leading to UC. Moreover, cell experiments found that the levels of IL-1β, IL-6, and TNF-α were significantly reduced after silencing NCAPD2/3, indicating that this approach can effectively improve the inflammatory reactions induced by UC.
The NF-κB pathway is the primary inflammatory signal transduction pathway, and is involved in the expression and regulation of a variety of inflammatory genes[14]. Under normal circumstances, NF-κB binds to the IκB protein, which normally resides in the cytoplasm in its inactive state[15]. However, under external stimuli (such as proinflammatory cytokines), IκB kinase becomes phosphorylated, resulting in the phosphorylation of IκB, which dissociates from NF-κB and enters the nucleus to regulate the secretion and expression of inflammatory factors[16]. Related studies have confirmed that the activation of IKK/NF-κB is an essential cause of severe inflammation[17-19]. The activation of IKK/NF-κB increases the secretion of the proinflammatory cytokines TNF-α and IL-6, which induces inflammatory reactions[20]. The results of this study revealed that activation of the IKK/NF-κB signaling pathway induced by LPS was effectively inhibited after NCAPD2/3 knockout, which may be one of the important mechanisms for reducing the levels of inflammatory factors (IL-1β, IL-6 and TNF-α).
In summary, we found for the first time that NCAPD2/3 are upregulated in the intestinal mucosa of patients with active UC, and that this mechanism may involve stimulating the secretion of inflammatory factors IL-1β, IL-6 and TNF-α by activating the IKK/NF-κB pathway. However, given the exploratory and retrospective design of our study, as well as the small clinical sample size, the result of these findings will need to be further validated. Future work will be aimed at deeply investigating the role of NCAPD2/3 in the onset and progression of IBD, including UC and Crohn’s disease.
Ulcerative colitis (UC) is a chronic, idiopathic inflammatory disease affecting the colon, and the precise molecular mechanisms are undefined. To date, some evidence suggested that non-SMC condensin I complex subunit D2 (NCAPD2) and non-SMC condensin II complex subunit D3 (NCAPD3) play important roles in mitosis and meiosis. Recently, it has been suggested in the literature that subunits of condensing I and condensin II are involved in human cancers, included colorectal cancer. Schuster et al[12] has reported that NCAPD3 down-regulates the transcription of genes that encode amino acid transporters (SLC7A5 and SLC3A2) to promote bacterial autophagy by colonic epithelial cells.
To date, there are few studies regarding the correlation of NCAPD2 and NCAPD3 with human diseases, especially in UC. We hypothesize that NCAPD2/3 can also be a potential pathogenic or diagnostic target for ulcerative colitis, and could be used as a new therapeutic target in the future.
In this study, we identified high expression of NCAPD2/3 in the intestinal mucosa of patients with UC. We also analyzed the NCM60 colonic epithelial cell line expressing inducible siRNAs targeting NCAPD2/3, and for the first time, we found that NCAPD2/3 may induce inflammation via the IKK/NF-κB pathway in UC. These findings reveal an important role for NCAPD2/3 in UC, thus providing a potential new direction for UC research.
We used in situ hybridization (ISH) to measure levels of NCAPD2/3 in intestinal tissue from patients with UC and healthy individuals. In vitro, the inflammatory cytokines IKK and NF-κB were evaluated by ELISA, WB and immunofluorescence assay with NCM60 cells expressing small hairpin RNAs against NCAPD2/3.
In this study, we found that NCAPD2 and NCAPD3 protein expression in intestinal tissue was significantly higher in UC patients than in healthy people. We also found that knockdown of NACPD2/3 in normal colonic epithelial cells (NCM460 cell) resulted in a significant downregulation of IL-1β, IL-6 and TNF-α, possibly by regulating the IKK/NF-κB signaling pathway.
Levels of NCAPD2/3 proteins are increased in patients with active UC. NCAPD2/3 promote the release of inflammatory cytokines such as IL-1β, IL-6 and TNF-α, which modulate the IKK/NF-κB signaling pathway.
Our findings indicate a critical role for NCAPD2/3 in the onset and progression of inflammatory bowel disease, as well as strategies to decrease NCAPD2/3 levels that might inhibit inflammation in patients with active UC.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Can G, Jamali R S-Editor: Wang J L-Editor: Filipodia E-Editor: Ma YJ
| 1. | Bonneau J, Dumestre-Perard C, Rinaudo-Gaujous M, Genin C, Sparrow M, Roblin X, Paul S. Systematic review: new serological markers (anti-glycan, anti-GP2, anti-GM-CSF Ab) in the prediction of IBD patient outcomes. Autoimmun Rev. 2015;14:231-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 54] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 2. | Rogler G, Biedermann L. Clinical Utility of Biomarkers in IBD. Curr Gastroenterol Rep. 2015;17:26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Ha CY, Katz S. Clinical implications of ageing for the management of IBD. Nat Rev Gastroenterol Hepatol. 2014;11:128-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 4. | Yang H, Li Y, Wu W, Sun Q, Zhang Y, Zhao W, Lv H, Xia Q, Hu P, Li H, Qian J. The incidence of inflammatory bowel disease in Northern China: a prospective population-based study. PLoS One. 2014;9:e101296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 69] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 5. | Soendergaard C, Seidelin JB, Steenholdt C, Nielsen OH. Putative biomarkers of vedolizumab resistance and underlying inflammatory pathways involved in IBD. BMJ Open Gastroenterol. 2018;5:e000208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 6. | Boden EK, Shows DM, Chiorean MV, Lord JD. Identification of Candidate Biomarkers Associated with Response to Vedolizumab in Inflammatory Bowel Disease. Dig Dis Sci. 2018;63:2419-2429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 7. | Zhang P, Liu L, Huang J, Shao L, Wang H, Xiong N, Wang T. Non-SMC condensin I complex, subunit D2 gene polymorphisms are associated with Parkinson's disease: a Han Chinese study. Genome. 2014;57:253-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Seipold S, Priller FC, Goldsmith P, Harris WA, Baier H, Abdelilah-Seyfried S. Non-SMC condensin I complex proteins control chromosome segregation and survival of proliferating cells in the zebrafish neural retina. BMC Dev Biol. 2009;9:40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Bouguen G, Chevaux JB, Peyrin-Biroulet L. Recent advances in cytokines: therapeutic implications for inflammatory bowel diseases. World J Gastroenterol. 2011;17:547-556. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 46] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 10. | Calderón M, Minckas N, Nuñez S, Ciapponi A. Inflammatory Bowel Disease in Latin America: A Systematic Review. Value Health Reg Issues. 2018;17:126-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | Yin L, Jiang LP, Shen QS, Xiong QX, Zhuo X, Zhang LL, Yu HJ, Guo X, Luo Y, Dong J, Kong QP, Yang CP, Chen YB. NCAPH plays important roles in human colon cancer. Cell Death Dis. 2017;8:e2680. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 63] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 12. | Schuster AT, Homer CR, Kemp JR, Nickerson KP, Deutschman E, Kim Y, West G, Sadler T, Stylianou E, Krokowski D, Hatzoglou M, de la Motte C, Rubin BP, Fiocchi C, McDonald C, Longworth MS. Chromosome-associated protein D3 promotes bacterial clearance in human intestinal epithelial cells by repressing expression of amino acid transporters. Gastroenterology. 2015;148:1405-1416.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Zhang Y, Gao W, Yang K, Tao H, Yang H. Salt-Inducible Kinase 1 (SIK1) is Induced by Alcohol and Suppresses Microglia Inflammation via NF-κB Signaling. Cell Physiol Biochem. 2018;47:1411-1421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Scheidereit C. IkappaB kinase complexes: gateways to NF-kappaB activation and transcription. Oncogene. 2006;25:6685-6705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 480] [Cited by in RCA: 538] [Article Influence: 28.3] [Reference Citation Analysis (0)] |
| 15. | Karin M. How NF-kappaB is activated: the role of the IkappaB kinase (IKK) complex. Oncogene. 1999;18:6867-6874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 894] [Cited by in RCA: 908] [Article Influence: 34.9] [Reference Citation Analysis (0)] |
| 16. | Alkalay I, Yaron A, Hatzubai A, Orian A, Ciechanover A, Ben-Neriah Y. Stimulation-dependent I kappa B alpha phosphorylation marks the NF-kappa B inhibitor for degradation via the ubiquitin-proteasome pathway. Proc Natl Acad Sci USA. 1995;92:10599-10603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 324] [Cited by in RCA: 341] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 17. | Cai D, Yuan M, Frantz DF, Melendez PA, Hansen L, Lee J, Shoelson SE. Local and systemic insulin resistance resulting from hepatic activation of IKK-beta and NF-kappaB. Nat Med. 2005;11:183-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1612] [Cited by in RCA: 1742] [Article Influence: 87.1] [Reference Citation Analysis (0)] |
| 18. | Yamamoto Y, Gaynor RB. Therapeutic potential of inhibition of the NF-kappaB pathway in the treatment of inflammation and cancer. J Clin Invest. 2001;107:135-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1137] [Cited by in RCA: 1166] [Article Influence: 48.6] [Reference Citation Analysis (0)] |
| 19. | Li R, Shen Q, Wu N, He M, Liu N, Huang J, Lu B, Yao Q, Yang Y, Hu R. MiR-145 improves macrophage-mediated inflammation through targeting Arf6. Endocrine. 2018;60:73-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 20. | Jadhav A, Tiwari S, Lee P, Ndisang JF. The heme oxygenase system selectively enhances the anti-inflammatory macrophage-M2 phenotype, reduces pericardial adiposity, and ameliorated cardiac injury in diabetic cardiomyopathy in Zucker diabetic fatty rats. J Pharmacol Exp Ther. 2013;345:239-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 69] [Article Influence: 5.8] [Reference Citation Analysis (0)] |