Published online Jan 28, 2019. doi: 10.3748/wjg.v25.i4.498
Peer-review started: September 30, 2018
First decision: November 15, 2018
Revised: December 3, 2018
Accepted: December 19, 2018
Article in press: December 20, 2018
Published online: January 28, 2019
Processing time: 118 Days and 16.6 Hours
To characterize esophageal endoluminal landmarks to permit radial and longitudinal esophageal orientation and accurate lesion location.
Distance from the incisors and radial orientation were estimated for the main left bronchus and the left atrium landmarks in 207 consecutive patients using white light examination. A sub-study was also performed using white light followed by endoscopic ultrasound (EUS) in 25 consecutive patients to confirm the findings. The scope orientation throughout the exam was maintained at the natural axis, where the left esophageal quadrant corresponds to the area between 6 and 9 o’clock. When an anatomical landmark was identified, it was recorded with a photograph and its quadrant orientation and distance from the incisors were determined. The reference points to obtain the distances and radial orientation were as follows: the midpoint of the left main bronchus and the most intense pulsatile zone of the left atrium. With the video processor system set to moderate insufflation, measurements were obtained at the end of the patients’ air expiration.
The left main bronchus and left atrium esophageal landmarks were identified using white light in 99% and 100% of subjects at a mean distance of 25.8 cm (SD 2.3), and 31.4 cm (SD 2.4) from the incisors, respectively. The left main bronchus landmark was found to be a tubular, concave, non-pulsatile, esophageal external compression, occupying approximately 1/4 of the circumference. The left atrium landmark was identified as a round, convex, pulsatile, esophageal external compression, occupying approximately 1/4 of the circumference. Both landmarks were identified using white light on the anterior esophageal quadrant. In the sub-study, the left main bronchus was identified in 24 (92%) patients at 25.4 cm (SD 2.1) and 26.7 cm (SD 1.9) from the incisors, by white light and EUS, respectively. The left atrium was recognized in all patients at 30.5 cm (SD 1.9), and 31.6 cm (SD 2.3) from the incisors, by both white light and EUS, respectively. EUS confirmed that the landmarks corresponded to these two structures, respectively, and that they were located on the anterior esophageal wall. The Bland-Altman plot demonstrated high agreement between the white light and EUS measurements.
This study provides an endoscopic characterization of esophageal landmarks corresponding to the left main bronchus and left atrium, to permit radial and longitudinal orientation and accurate lesion location.
Core tip: Although accurate photo documentation of endoscopic landmarks and a careful description of the location of an esophageal lesion are included in endoscopy quality guidelines, clinical practice lacks these essentials. This study characterized two esophageal landmarks to permit radial and longitudinal orientation and accurate lesion location. The left main bronchus and left atrium landmarks were identified in 99% and 100% of patients on the anterior esophageal quadrant and at a mean distance of 25.8 cm and 31.4 cm from the incisors, respectively. The endoscopic ultrasound sub-study confirmed these findings and the anterior orientation of the landmarks.
- Citation: Emura F, Gomez-Esquivel R, Rodriguez-Reyes C, Benias P, Preciado J, Wallace M, Giraldo-Cadavid L. Endoscopic identification of endoluminal esophageal landmarks for radial and longitudinal orientation and lesion location. World J Gastroenterol 2019; 25(4): 498-508
- URL: https://www.wjgnet.com/1007-9327/full/v25/i4/498.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i4.498
Esophageal lesions are traditionally described according to the distance from the incisors[1,2]. This measure, while helpful to roughly describe large lesions, lacks radial orientation and is inaccurate for precise location of dysplastic lesions and small flat tumors. Endoscopic resection/ablation procedures as well as newer advanced procedures, such as per-oral endoscopic myotomy (POEM), are facilitated by accurate longitudinal and radial anatomic orientation[3,4]. Furthermore, commonly used esophageal divisions comprising cervical, thoracic, and abdominal segments are unrecognized during an upper GI examination, making this surgical division meaningless for endoscopists[5,6]. As esophageal endoluminal anatomy has been poorly studied, current endoscopy practice lacks these essentials; offering vague lesion identification to a second intervening endoscopist. However, anatomical and cross-sectional radiological studies have identified two esophageal landmarks, the left main bronchus and the left atrium, and revealed their anterior location to the esophagus[7,8]. Although we recently postulated that these landmarks can be used to divide the esophageal length into three sections as part of the systematic alphanumeric coded endoscopic approach[9,10], an endoscopic study characterizing these landmarks has never been reported. The aim of this study was to determine the frequency of these landmarks, distance from the incisors and their quadrant orientation using white light endoscopy, and to confirm these findings by endoscopic ultrasound (EUS).
Two hundred and thirty-four patients were enrolled in the main study from March to December 2012 at EmuraCenter LatinoAmerica, Bogotá DC, Colombia. Endoscopy was indicated for both dyspeptic patients and screening purposes. Exclusion criteria consisted of patients with previous history of esophageal strictures, scleroderma, achalasia, Barrett’s esophagus, cardiac or esophageal motility disorders, and esophageal or gastric surgery. Those patients endoscopically diagnosed with peptic esophagitis, esophageal candidiasis, esophageal varices, and neoplastic lesions were also excluded from analysis. In the sub-study performed to confirm that the left main bronchus and left atrial indentations, truly represented those structures, 25 consecutive patients scheduled for upper EUS were enrolled between June and July 2016 at the Mayo Clinic, Jacksonville, FL, USA. Informed consent was obtained from all patients and this two-center study was approved by the respective institutional review boards.
The patients’ weight was determined using a digital weight scale and recorded in kilograms. Standing height from heel to vertex was determined using a conventional meter and estimated in centimeters. The BMI of each patient was determined by dividing the weight over the squared height.
White light examinations were performed by an expert endoscopist (FE) using an H180 or Q180 gastroscope (Olympus Optical, Tokyo, Japan), and an Olympus EVIS EXERA II HD video processor. An expert EUS endoscopist (MW) conducted the sub-study. White light examinations were performed with an H180 gastroscope, and EUS examinations with a 360° scanning range radial echoendoscope (Olympus America Inc., Center Valley, PA, United States), and an Olympus EVIS EXERA II HD video processor. All scopes had identical demarcations in centimeters, and visible numbers every five centimeters as reference. The video processor system was set to moderate insufflation mode (Mode M) during the entire procedure in all examinations. Once in the esophagus, the lumen was rinsed with water to remove any overlying surface mucous/saliva. Light conscious sedation with intravenous midazolam or propofol was used in selected subjects examined by white light endoscopy, and in all patients that underwent EUS.
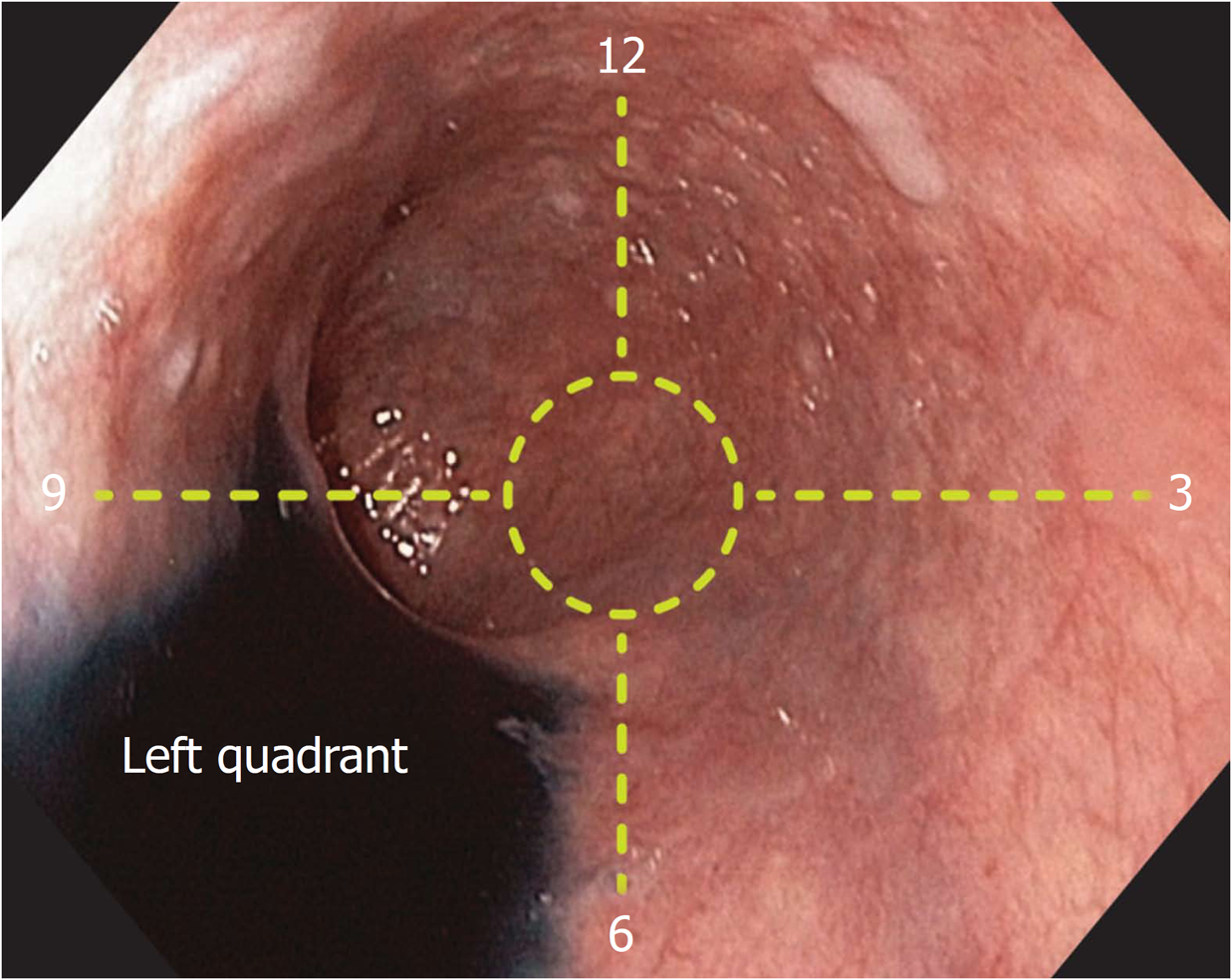
Once in the esophageal lumen, the endoscope was oriented with the left esophageal quadrant between 6 and 9 o’clock. This position was confirmed as follows: with the patient in the left lateral position, 3 mL of 0.25% Indigo Carmine (Chromoendoscopia, Colombia) was poured into the esophageal lumen using an irrigation catheter (PW-205V, Olympus, Japan). Utilizing gravity, the pooled water identified the left quadrant of the esophageal circumference (Figure 1). This endoluminal orientation, also known as the natural esophageal axis[8] was achieved when the examiner’s left hand maintained the head of the endoscope horizontally and the right hand slightly torqued to the right.
Esophageal quadrants during an upper GI examination were previously described by our team[9]. By positioning the left quadrant between 6 and 9 o’clock as previously mentioned, the other three quadrants were defined as follows: Anterior quadrant: the portion of the circumference between 9 and 12 o’clock; Right quadrant: the portion of the circumference contralateral to the left quadrant and located between 12 and 3 o’clock; Posterior quadrant: portion of the circumference contralateral to the anterior quadrant and located between 3 and 6 o’clock.
When an anatomical landmark was identified, the natural axis position of the endoscope was confirmed. It was then recorded with a photograph, and its quadrant orientation was identified. The reference points to obtain the distance from the incisors were as follows: the midpoint of the left main bronchus and the most protruded pulsatile zone of the left atrium. After identifying the radial orientation of the landmark, the distance from the incisors was calculated as follows: first, the endoscope tip was positioned immediately at the reference point, then, the distance was estimated using the standard demarcation of the endoscope located every 5 cm as a primary reference, and finally, for precise estimation, a flexible ruler marked in millimeters was positioned between the incisors and the closest endoscope mark. Each measurement was determined at the end of the patients’ air expiration.
Data were analyzed using the IBM-SPSS version 20 (IBM Corporation, Armonk, NY, United States). The results are presented as absolute numbers and proportions for qualitative variables and means ± SDs for continuous variables. The coefficient of variation was used as an additional statistic of measurement precision, and calculated as: standard deviation/mean. Differences between groups were analyzed using the chi-square test for categorical variables, and the one-way analysis of variance (ANOVA) or the Kruskal-Wallis test for continuous variables. A two-tailed P value < 0.05 was considered significant. The Bland-Altman plot was used to assess agreement between white light and EUS measurements (95%CI). The statistical methods used in this study were reviewed by a statistician (LG) of Universidad de La Sabana.
The sub-study sample size was calculated to detect differences ≥ 5% between the subjects with 95% confidence level, 80% power, 1:4 ratio and 2.5 cm SD.
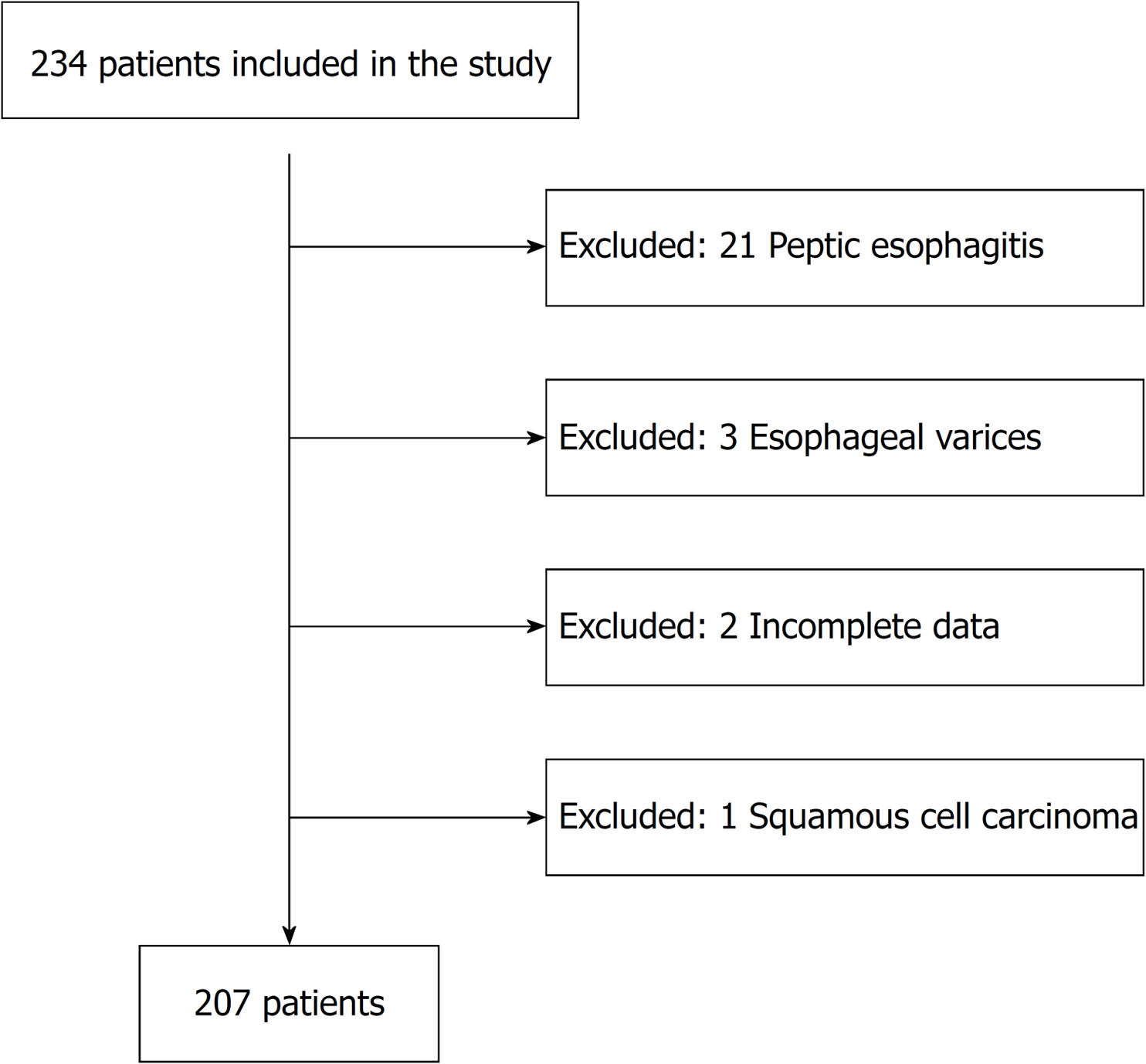
Two hundred and thirty-four patients were examined in the main study using white light endoscopy; 21 patients with peptic esophagitis, 3 with esophageal varices, 2 with incomplete data, and 1 with squamous cell carcinoma were excluded. Finally, a total of 207 subjects were analyzed (Figure 2). According to a calculated sample size of twenty-four for the sub-study, twenty-five subjects were enrolled and analyzed.
In the main study, the mean age of the patients was 54 years and the female:male ratio was 1.4:1. The mean weight, height and BMI were 162 cm, 66 kg and 25, respectively. In the sub-study, the mean age of the patients was 64 years and the female:male ratio was 1.8:1. The mean weight, height, and BMI were 170 cm, 79 kg and 27.3, respectively. Patients’ morphometric characteristics are shown in Table 1. There were no statistically significant differences between the groups.
| Factor | Study (n = 207), mean ± SD (CV) | Sub-study (n = 25), mean ± SD (CV) |
| Age (yr) | 54 ± 10 (0.2) | 64 ± 14 (0.2) |
| Height (cm) | 162 ± 9 (0.05) | 169 ± 8 (0.05) |
| Weight (kg) | 66 ± 12 (0.18) | 78 ± 16 (0.21) |
| BMI | 25 ± 4 (0.16) | 27 ± 4 (0.17) |
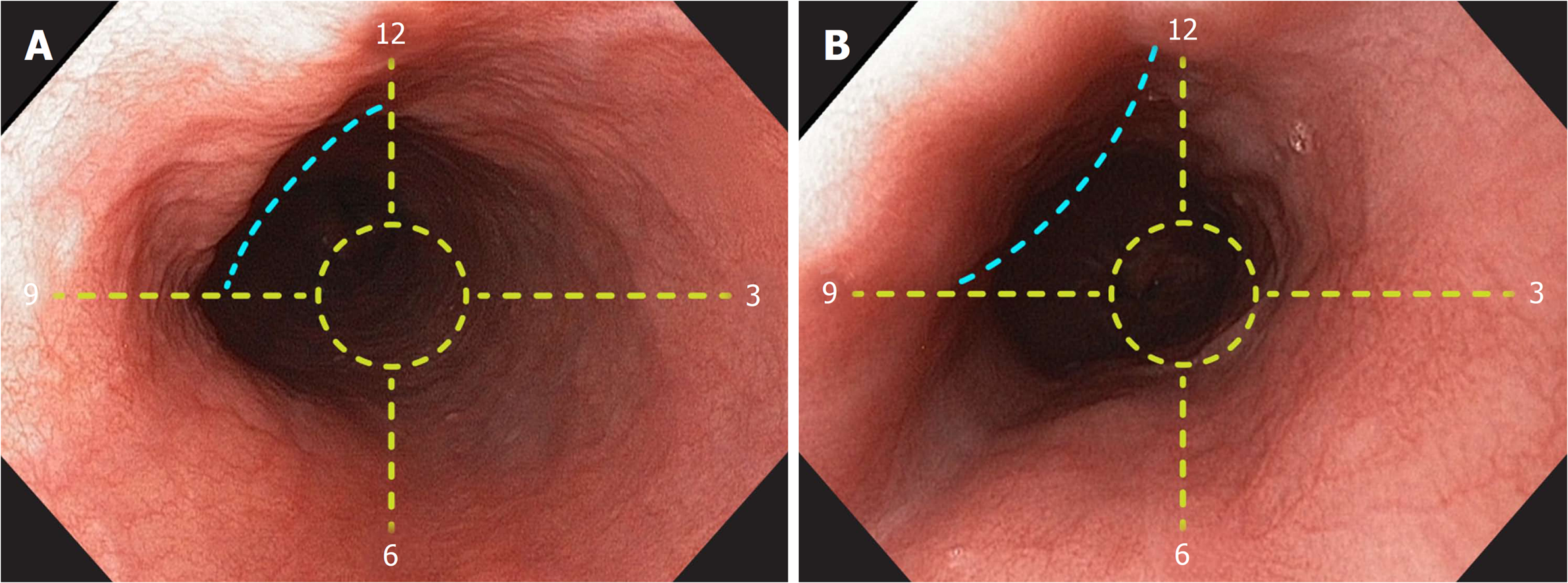
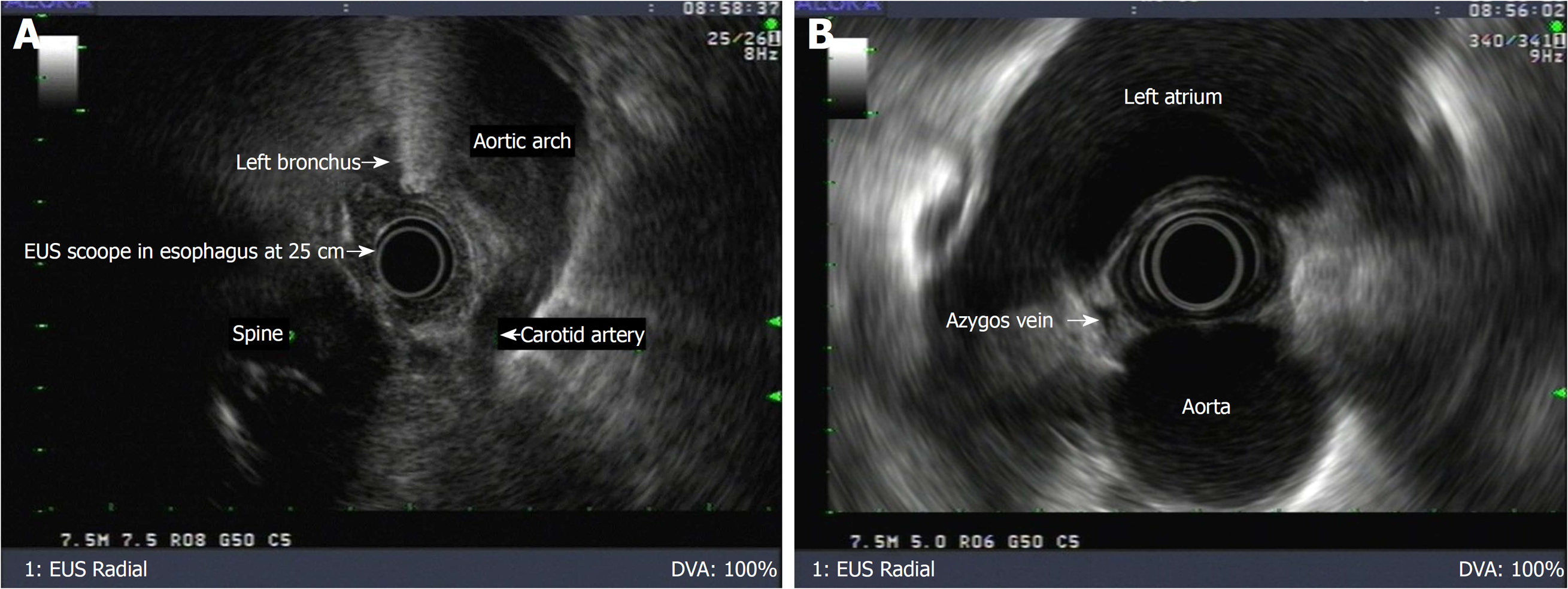
The left main bronchus and left atrium esophageal landmarks were endoscopically identified using white light in 205 (99%) and 100% of patients at a mean distance of 25.8 cm (SD 2.3), and 31.4 cm (SD 2.4) from the incisors, respectively. The left main bronchus landmark was found to be a tubular convex, non-pulsatile esophageal external compression, occupying approximately 1/4 of the circumference. The left atrium landmark was identified as a rounded concave, pulsatile esophageal external compression, also occupying approximately 1/4 of the circumference. In all subjects, the radial orientation of both landmarks was identified on the anterior esophageal quadrant (Figure 3). In the sub-study, the left main bronchus was identified in twenty-three (92%) patients at 25.4 cm (SD 2.1) and in twenty-four (96%) patients at 26.7 cm (SD 1.9) from the incisors, by white light and EUS, respectively. On the other hand, the left atrium was recognized in all patients at 30.5 cm (SD 1.9), and 31.6 cm (SD 2.3) from the incisors, by both white light and EUS, respectively. Both landmarks were also identified on the anterior esophageal quadrant. EUS confirmed that the landmarks corresponded to these two structures, respectively, and that they were located on the anterior esophageal wall (Figure 4). There were no significant differences between the distances measured by these methods (Table 2).
| Landmark | Study (n = 207) | Sub-study (n = 25) | P value | Power to detect differences > 4.5% (confidence 95%) | |
| WL, mean ± SD (CV) | WL, mean ± SD (CV) | EUS, mean ± SD (CV) | |||
| Left main bronchus | 25.8 ± 2.3 (0.09) | 25.4 ± 2.1 (0.08) | 26.7 ± 1.9 (0.07) | 0.16 | 82.9% |
| Left atrium | 31.4 ± 2.4 (0.08) | 30.5 ± 1.9 (0.06) | 31.6 ± 2.3 (0.07) | 0.1 | 80.1% |
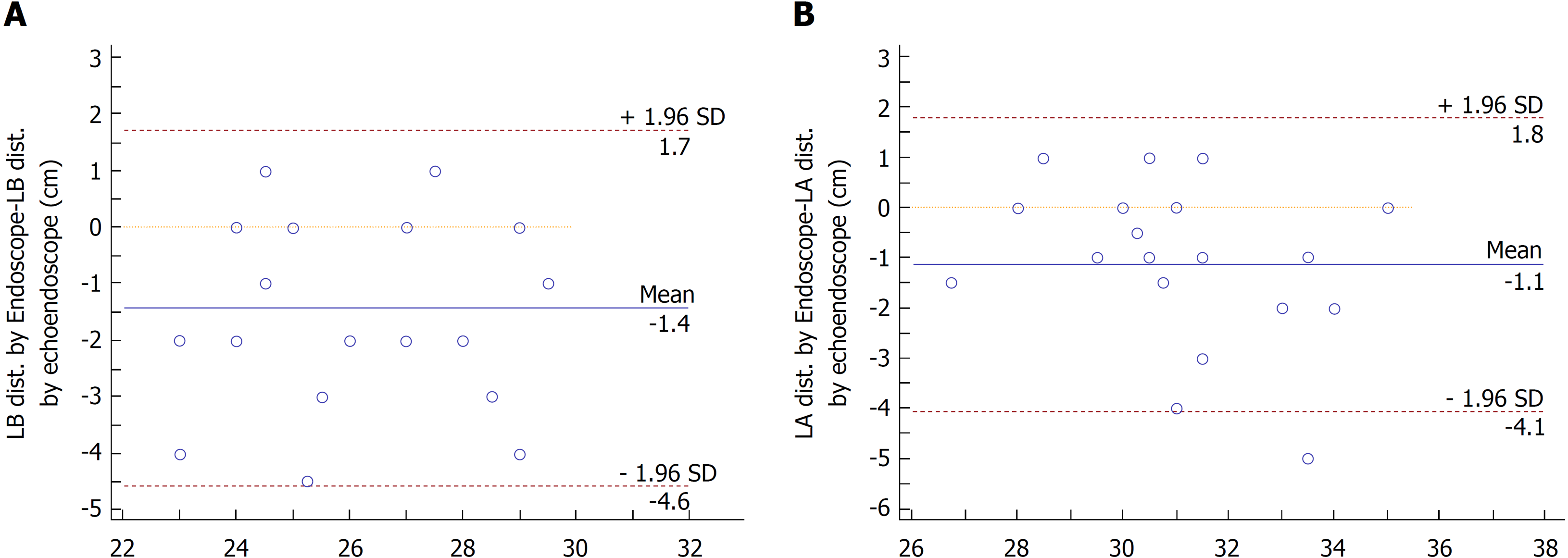
The Bland-Altman limits of agreement plot showed a mean difference of -1.1 and -1.4 cm for the left main bronchus and the left atrium when using white light and EUS, respectively (Figure 5).
This study, for the first time, characterized the endoscopic nature, frequency, distance from the incisors and quadrant orientation of two external compressions along the esophageal length.
There are several factors that reliably support the results obtained in this study. First, the evidence of previous anatomical and radiological studies that highlighted the existence of these landmarks[5,7,8]. Second, the reliable identification of these landmarks with consistent distances from the incisors, and third, the constant anterior radial orientation of the landmarks by white light, and their confirmation by EUS.
The distance measurements from the incisors were consistent between the three patient cohorts with similar coefficients of variation to those found as in any other anatomical study. Although some anatomical variations might explain the lack of observation of the left main bronchus landmark in two patients using white light in the main study, and in one patient using EUS, additional studies in larger subpopulations are warranted to further explain these findings. With regard to the two patients in which the left main bronchus was not observed using white light, but was seen during the subsequent EUS exam, a probable explanation was an unrecognized light extrinsic compression over the esophageal wall. However, further studies are also necessary to explain these observations.
In order to compare the differences between these measures, we carried out the Bland-Altman plot, which demonstrated high agreement between the white light and EUS measurements with an EUS mean difference of -1.1 cm and -1.4 cm measured for the left main bronchus and the left atrium, respectively. Although this small difference can be explained simply by human error, the major reason for this difference can be attributed to the type of radial echoendoscope used, which has an additional extension at the scope tip due to the ultrasound transducer, thereby explaining, in part, the difference obtained by EUS. Although cadaveric studies have estimated the esophageal relationship with external organs[5,11], no other endoscopic studies have been conducted to characterize the left atrium landmark. With regard to the left main bronchus landmark, a Korean study evaluated the endoscopic esophageal length in 196 individuals and reported a similar distance of 27.7 cm from the incisors[12].
In order to reliably identify the radial orientation of the landmarks, we first identified the anatomical distributions of the 4-quadrants by gravity identification of the left quadrant using Indigo Carmine, and then, defined other names according to described anatomical nomenclature[7]. After allocating the left quadrant between 6 and 9 o’clock, the right quadrant was therefore, allocated at the contralateral side between 12 and 3 o’clock, and the anterior and posterior quadrants were intercalated between the aforementioned quadrants. When the natural axis position was achieved, we applied clock face-distribution for precise quadrant identification. In all white light examinations, both identified landmarks were radially oriented at the anterior esophageal quadrant between 9 and 12 o’clock. We conducted EUS examinations to confirm these findings and obtained the same results.
Although anthropometric measurements in Colombian patients were lower compared to USA patients, there were no differences when the distances from the incisors were compared. Similar to a previous study that reported a direct association between height and esophageal total length[12,13], we found a direct association between height and both the left main bronchus and the left atrium measurements (P < 0.001). Further studies are warranted to predict esophageal length using height as the most relevant external parameter.
Although these endoscopic measurements need to be tested in further inter-observer validation studies, they are probably vulnerable to the same limitations as the measurements for human anatomical studies. For distance estimation, possible confounding influences are low or excessive insufflation of the esophagus, which could reduce endoluminal visibility and respiratory movements, which might modify the measurements.
Even when considerably fewer patients were examined in the sub-study compared to those examined using white light, the calculated statistical power was sufficient (> 80%), to detect differences > 4.5% between the methods, indicating that a larger sample was unnecessary. A limitation for clinical application is that, at present, endoscopists are not trained to recognize these anatomical landmarks and therefore, their identification and the consequent esophageal radial and longitudinal orientation require basic training.
The long tubular esophageal shape has limited our ability to accurately orientate and assess the location of esophageal lesions. Traditionally, esophageal lesions have been described according to the distance from the incisors[1,2] and their location, as proposed by surgeons, in cervical, thoracic or abdominal segments[5,6]. On the one hand, using only the estimation of distance from the incisors lacks accuracy to radially locate suspicious esophageal lesions and tumors, and on the other hand, the surgical esophageal divisions are unrecognizable during upper GI exams.
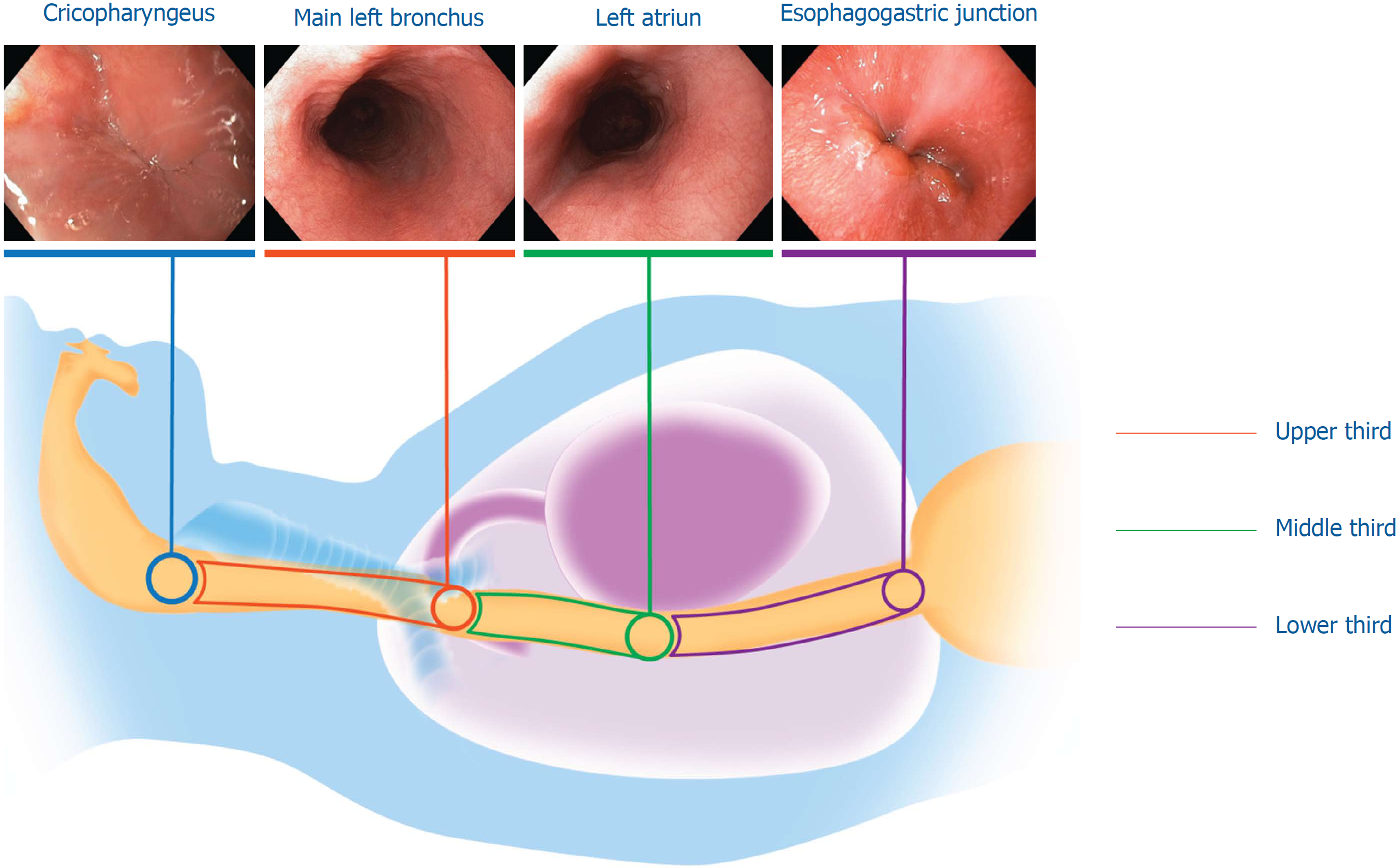
The two landmarks characterized herein, can potentially be used to overcome the above-mentioned limitations. First, when taken together along with the cricopharyngeal narrowing and the esophagogastric (EG) junction landmarks reported at a distance of 15.7 ± 1.4 cm and 40.9 ± 2.8 cm from the incisors, respectively[14,15], this constitutes the fundamentals for the systematic alphanumeric endoscopic proposal to evaluate the esophagus[9,10], and can be used, as reported by us, to improve longitudinal orientation by dividing the esophagus into three non-equal, but practical endoscopic sections: the upper third, located between the cricopharyngeal narrowing and the left main bronchus; the middle third, located between the left main bronchus and the left atrium; and the distal third, extending from the left atrium downward to the EG junction[9] (Figure 6). The potential usefulness of this endoscopic classification requires further study, but currently provides clinically relevant data to fulfill published guidelines by major gastroenterology societies, which recommend accurate photo documentation of endoscopic landmarks and a careful description of the location of a lesion to allow subsequent therapeutic applications and future surveillance[16,17]. Furthermore, appropriate recognition of the main left bronchus and/or the left atrium landmarks and their anterior location to the esophagus, may significantly improve radial quadrant orientation. Along with identification of the left esophageal quadrant as described herein, the landmarks can potentially be used to accurately distinguish the 4-quadrants in any esophageal portion including the EG junction. When accurate radial orientation is achieved, a clock face-distribution can be used to precisely locate any abnormalities in the esophageal circumference.
Previous studies have highlighted the importance of radial orientation at the EG junction, and reported a preponderance of mucosal erosive changes, high grade dysplasia and Barrett’s cancer between 12 and 3 o’clock[18,19]. However, in these observations, esophageal quadrants were not defined based on natural anatomy but according to the examiners’ view of the endoscopic field. Another study reported a preponderance of Barrett’s neoplasia at 2-5 o’clock and used the “neutral position” of the endoscope as a reference for radial orientation, emphasizing the lack of a universal standardized radial orientation[20]. Recent surveillance guidelines for Barrett’s esophagus recommend random 4-quadrant biopsies to be performed every 1 to 2 cm in the columnar segment together with biopsies of any visible lesions[21-23]. In our opinion, without accurate radial and longitudinal orientation and identification of anatomical quadrants, these recommendations cannot be fulfilled and are currently a source of confusion among practitioners.
These observations when externally validated, may fulfill in part, the lack of current reliable performance measures to gauge the quality of an esophageal endoscopy examination. Recognition of these landmarks can improve radial orientation for both standardization of anterior or posterior approaches in POEM procedures[3,4], and localization of Barrett’s esophagus with dysplasia and small squamous cell carcinomas, increasing the opportunity to diagnose and treat cancer in early stages[22,24,25].
In summary, this study provides an endoscopic identification of endoluminal esophageal landmarks corresponding to the left main bronchus and left atrium to permit radial and longitudinal orientation and accurate lesion location.
Esophageal lesions are traditionally described according to the distance from the incisors. This measure, while helpful in roughly describing large lesions, lacks radial orientation and is inaccurate for the precise location of dysplastic lesions and small flat tumors. Furthermore, commonly used esophageal divisions comprising cervical, thoracic, and abdominal segments are unrecognized during an upper GI examination, making this surgical division meaningless for endoscopists. As esophageal endoluminal anatomy has been poorly studied, current endoscopy practice lacks these essentials; offering vague lesion identification to a second intervening endoscopist.
Although anatomical and cross-sectional radiological studies, have identified two esophageal landmarks, the left main bronchus and the left atrium, and revealed their anterior location to the esophagus, the long tubular esophageal shape has limited our ability to accurately orientate and assess the location of esophageal lesions. Even though we have postulated that these landmarks can be used to divide the esophageal length into three sections as part of the upper systematic alphanumeric coded endoscopic approach, an endoluminal study characterizing these landmarks has never been reported.
Our study aimed to determine the frequency of these landmarks, distance from the incisors and their quadrant orientation using white light endoscopy, and to confirm these findings by endoscopic ultrasound (EUS).
Quadrant orientation and distance from the incisors were estimated in 207 consecutive patients using white light examination. A sub-study was also performed using white light followed by EUS in 25 consecutive patients to confirm the findings. Once in the esophageal lumen, the endoscope was oriented with the left esophageal quadrant between 6 and 9 o’clock. This position was confirmed as follows: with the patient in the left lateral position, 3 mL of 0.25% Indigo Carmine was poured into the esophageal lumen using an irrigation catheter. Utilizing gravity, the pooled water identified the left quadrant of the esophageal circumference. By positioning the left quadrant between 6 and 9 o’clock as previously mentioned, the other three quadrants were defined as follows: Anterior quadrant: the portion of the circumference between 9 and 12 o’clock; Right quadrant: the portion of the circumference contralateral to the left quadrant and located between 12 and 3 o’clock; Posterior quadrant: portion of the circumference contralateral to the anterior quadrant and located between 3 and 6 o’clock. This esophageal orientation was defined as the natural axis and was maintained throughout the exam. After identifying the radial orientation of the landmark, the distance from the incisors was estimated using the standard demarcation of the endoscope located every 5 cm as a primary reference, and finally, for precise estimation, a flexible ruler marked in millimeters was positioned between the incisors and the closest endoscope mark.
The left main bronchus and left atrium esophageal landmarks were identified using white light in 99% and 100% of subjects at a mean distance of 25.8 cm (SD 2.3), and 31.4 cm (SD 2.4) from the incisors, respectively. The left main bronchus landmark was found to be a tubular, concave, non-pulsatile, esophageal external compression, occupying approximately 1/4 of the circumference. The left atrium landmark was identified as a round, convex, pulsatile, esophageal external compression, occupying approximately 1/4 of the circumference. Both landmarks were identified using white light on the anterior esophageal quadrant. In the sub-study, the left main bronchus was identified in 24 (92%) patients at 25.4 cm (SD 2.1) and 26.7 cm (SD 1.9) from the incisors, by white light and EUS, respectively. The left atrium was recognized in all patients at 30.5 cm (SD 1.9), and 31.6 cm (SD 2.3) from the incisors, by both white light and EUS, respectively. EUS confirmed that the landmarks corresponded to these two structures, respectively, and that they were located on the anterior esophageal wall. The Bland-Altman plot demonstrated high agreement between the white light and EUS measurements.
Although these endoscopic measurements require further inter-observer validation studies, this study provides an endoscopic characterization of esophageal landmarks corresponding to the left main bronchus and left atrium, to permit radial and longitudinal orientation and accurate lesion location.
Endoscopic recognition of these two landmarks may have different clinical applications. First, when taken together along with the cricopharyngeal narrowing and the esophagogastric (EG) junction landmarks, these constitute the fundamentals for the systematic alphanumeric endoscopic proposal to evaluate the esophagus, and can be used, as reported by us, to improve longitudinal orientation by dividing the esophagus into three non-equal, but practical endoscopic sections: the upper third, located between the cricopharyngeal narrowing and the left main bronchus; the middle third, located between the left main bronchus and the left atrium; and the distal third, extending from the left atrium downward to the EG junction. The potential usefulness of this endoscopic classification requires further study, but currently provides clinically relevant data to fulfill published guidelines by major gastroenterology societies, which recommend accurate photo documentation of endoscopic landmarks and a careful description of the location of a lesion to allow subsequent therapeutic applications and future surveillance. Second, appropriate recognition of the main left bronchus and/or the left atrium landmarks and their anterior location to the esophagus, may significantly improve radial quadrant orientation for both standardization of anterior or posterior approaches in POEM procedures, and precise localization of Barrett’s esophagus with dysplasia and small squamous cell carcinomas. Furthermore, after identification of the left esophageal quadrant as described herein, these landmarks can potentially be used to properly distinguish the 4-quadrants in any esophageal portion including the EG junction. When accurate radial orientation is achieved, a clock face-distribution can be used to precisely locate any abnormalities in the esophageal circumference.
The authors would like to thank Harker Wade and Anne Shiwa for editing this manuscript.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Colombia
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
STROBE Statement: The authors have read the STROBE Statement-checklist of items, and the manuscript was prepared and revised according to the STROBE Statement-checklist of items
P- Reviewer: Guo YM, José Luis SS S- Editor: Gong ZM L- Editor: Webster JR E- Editor: Yin SY
| 1. | McClave SA, Boyce HW, Gottfried MR. Early diagnosis of columnar-lined esophagus: a new endoscopic diagnostic criterion. Gastrointest Endosc. 1987;33:413-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 154] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 2. | Csendes A, Maluenda F, Braghetto I, Csendes P, Henriquez A, Quesada MS. Location of the lower oesophageal sphincter and the squamous columnar mucosal junction in 109 healthy controls and 778 patients with different degrees of endoscopic oesophagitis. Gut. 1993;34:21-27. [PubMed] |
| 3. | Tan Y, Lv L, Wang X, Zhu H, Chu Y, Luo M, Li C, Zhou H, Huo J, Liu D. Efficacy of anterior versus posterior per-oral endoscopic myotomy for treating achalasia: a randomized, prospective study. Gastrointest Endosc. 2018;88:46-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (1)] |
| 4. | Ramchandani M, Nabi Z, Reddy DN, Talele R, Darisetty S, Kotla R, Chavan R, Tandan M. Outcomes of anterior myotomy versus posterior myotomy during POEM: a randomized pilot study. Endosc Int Open. 2018;6:E190-E198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 53] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 5. | Gray H, Susan S. Mediastinum. Susan S. Gray's Anatomy: The Anatomical Basis of Clinical Practice. Fortieth ed. New York: Churchill Livingstone Elsevier 2008; 939-957. |
| 6. | Vaezi M, Flint P. The esophagus: anatomy, physiology, and diseases. Flint P. Otolaryngology Head and Neck Surgery. Fifth ed. Philadelphia: Mosby - Elsevier 2010; 953-980. |
| 7. | Skandalakis JE, Skandalakis LJ, Skandalakis PN. Esophagus. Surgical Anatomy and Technique. New York, NY: Springer 2000; 257-309 [DOI.org/10.1007/978-1-4615-7993-9_6]. [DOI] [Full Text] |
| 8. | Chevallier JM, Vitte E, Derosier C, Aupart M, Jeanbourquin D, Sarcy JJ, Hannoun L, Parc R. The thoracic esophagus: sectional anatomy and radiosurgical applications. Surg Radiol Anat. 1991;13:313-321. [PubMed] |
| 9. | Emura F, Gralnek I, Sano Y, Baron TH. Improving early detection of gastric cancer: a novel systematic alphanumeric-coded endoscopic approach. Rev Gastroenterol Peru. 2013;33:52-58. [PubMed] |
| 10. | Machaca Quea NR, Emura F, Barreda Bolaños F, Salvador Arias Y, Arévalo Suárez FA, Piscoya Rivera A. Effectiveness of systematic alphanumeric coded endoscopy for diagnosis of gastric intraepithelial neoplasia in a low socioeconomic population. Endosc Int Open. 2016;4:E1083-E1089. [PubMed] |
| 11. | Netter FH. The Ciba collection of medical illustrations. 5th ed. 34. Summit, NJ: Ciba Pharmaceutical, 1979. . |
| 12. | Song TJ, Kim YH, Ryu HS, Hyun JH. Correlation of esophageal lengths with measurable external parameters. Korean J Intern Med. 1991;6:16-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Otsianyi WK, Mutie T, Kioko H. The Correlation of Esophageal Body Length with Measure of External Body Parameters. Int J Morphol. 2011;29:895-898. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (1)] |
| 14. | Sivarao DV, Goyal RK. Functional anatomy and physiology of the upper esophageal sphincter. Am J Med. 2000;108 Suppl 4a:27S-37S. [PubMed] |
| 15. | Boyce HW. Endoscopic definitions of esophagogastric junction regional anatomy. Gastrointest Endosc. 2000;51:586-592. [PubMed] |
| 16. | Bisschops R, Areia M, Coron E, Dobru D, Kaskas B, Kuvaev R, Pech O, Ragunath K, Weusten B, Familiari P, Domagk D, Valori R, Kaminski MF, Spada C, Bretthauer M, Bennett C, Senore C, Dinis-Ribeiro M, Rutter MD. Performance measures for upper gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement Initiative. Endoscopy. 2016;48:843-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 243] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 17. | Cohen J, Safdi MA, Deal SE, Baron TH, Chak A, Hoffman B, Jacobson BC, Mergener K, Petersen BT, Petrini JL, Rex DK, Faigel DO, Pike IM. Quality indicators for esophagogastroduodenoscopy. Gastrointest Endosc. 2006;63:S10-S15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 18. | Edebo A, Vieth M, Tam W, Bruno M, van Berkel AM, Stolte M, Schoeman M, Tytgat G, Dent J, Lundell L. Circumferential and axial distribution of esophageal mucosal damage in reflux disease. Dis Esophagus. 2007;20:232-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 56] [Article Influence: 3.1] [Reference Citation Analysis (2)] |
| 19. | Pech O, Gossner L, Manner H, May A, Rabenstein T, Behrens A, Berres M, Huijsmans J, Vieth M, Stolte M, Ell C. Prospective evaluation of the macroscopic types and location of early Barrett's neoplasia in 380 lesions. Endoscopy. 2007;39:588-593. [PubMed] |
| 20. | Kariyawasam VC, Bourke MJ, Hourigan LF, Lim G, Moss A, Williams SJ, Fanning SB, Chung AM, Byth K. Circumferential location predicts the risk of high-grade dysplasia and early adenocarcinoma in short-segment Barrett's esophagus. Gastrointest Endosc. 2012;75:938-944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 21. | Murphy SJ, Johnston BT, Murray LJ. British Society of Gastroenterology guidelines for the diagnosis of Barrett's oesophagus: are we casting the net too wide? Gut. 2006;55:1821-1822. [PubMed] |
| 22. | Wang KK, Sampliner RE; Practice Parameters Committee of the American College of Gastroenterology. Updated guidelines 2008 for the diagnosis, surveillance and therapy of Barrett's esophagus. Am J Gastroenterol. 2008;103:788-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 850] [Cited by in RCA: 786] [Article Influence: 46.2] [Reference Citation Analysis (1)] |
| 23. | American Gastroenterological Association; Spechler SJ, Sharma P, Souza RF, Inadomi JM, Shaheen NJ. American Gastroenterological Association medical position statement on the management of Barrett's esophagus. Gastroenterology. 2011;140:1084-1091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 383] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 24. | Hirota WK, Zuckerman MJ, Adler DG, Davila RE, Egan J, Leighton JA, Qureshi WA, Rajan E, Fanelli R, Wheeler-Harbaugh J, Baron TH, Faigel DO; Standards of Practice Committee, American Society for Gastrointestinal Endoscopy. ASGE guideline: the role of endoscopy in the surveillance of premalignant conditions of the upper GI tract. Gastrointest Endosc. 2006;63:570-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 369] [Cited by in RCA: 315] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 25. | ASGE Standards of Practice Committee; Evans JA, Early DS, Fukami N, Ben-Menachem T, Chandrasekhara V, Chathadi KV, Decker GA, Fanelli RD, Fisher DA, Foley KQ, Hwang JH, Jain R, Jue TL, Khan KM, Lightdale J, Malpas PM, Maple JT, Pasha SF, Saltzman JR, Sharaf RN, Shergill A, Dominitz JA, Cash BD; Standards of Practice Committee of the American Society for Gastrointestinal Endoscopy. The role of endoscopy in Barrett's esophagus and other premalignant conditions of the esophagus. Gastrointest Endosc. 2012;76:1087-1094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 242] [Article Influence: 18.6] [Reference Citation Analysis (1)] |