Published online Oct 7, 2019. doi: 10.3748/wjg.v25.i37.5702
Peer-review started: May 30, 2019
First decision: July 21, 2019
Revised: July 30, 2019
Accepted: September 9, 2019
Article in press: September 9, 2019
Published online: October 7, 2019
Processing time: 124 Days and 10.5 Hours
Irritable bowel syndrome (IBS) is a prevalent and debilitating gastrointestinal condition. Research has reported persistent, low-grade mucosal inflammation and significant overlaps between patients with IBS and those with dyspepsia, suggesting a possible pathogenic role of Helicobacter pylori (H. pylori) in IBS. This study therefore aimed to provide the first systematic review and meta-analysis on the association between H. pylori infection and IBS.
To investigate the association between H. pylori infection and IBS.
Using the keywords “H. pylori OR Helicobacter OR Helicobacter pylori OR infection” AND “irritable bowel syndrome OR IBS”, a preliminary search of PubMed, Medline, Embase, Cochrane Database of Systematic Reviews, Web of Science, Google Scholar and WanFang databases yielded 2924 papers published in English between 1 January 1960 and 1 June 2018. Attempts were also made to search grey literature.
A total of 13 clinical studies were systematically reviewed and nine studies were included in the final meta-analysis. Random-effects meta-analysis found a slight increased likelihood of H. pylori infection in patients with IBS, albeit this was not statistically significant (pooled odds ratio 1.47, 95% confidence interval: 0.90-2.40, P = 0.123). It must also be acknowledged that all of the available studies reported only crude odd ratios. H. pylori eradication therapy also does not appear to improve IBS symptoms. Although publication bias was not observed in the funnel plot, there was a high degree of heterogeneity amongst the studies included in the meta-analysis (I2 = 87.38%).
Overall, current evidence does not support an association between IBS and H. pylori infection. Further rigorous and detailed studies with larger sample sizes and after H. pylori eradication therapy are warranted.
Core tip: This is the first systematic review to examine the association of Helicobacter pylori (H. pylori) infection and irritable bowel syndrome (IBS). 13 clinical studies were systematically reviewed and nine studies were included in the final meta-analysis. Random-effects meta-analysis suggests a tenuous association between the two (pooled odds ratio 1.47, 95% confidence interval: 0.90-2.40, P = 0.123). H. pylori eradication therapy also does not appear to improve IBS symptoms in the limited studies available. Further detailed trials with larger sample sizes and after H. pylori eradication therapy are necessary to elucidate the relationship between H. pylori infection and IBS pathogenesis.
- Citation: Ng QX, Foo NX, Loke W, Koh YQ, Seah VJM, Soh AYS, Yeo WS. Is there an association between Helicobacter pylori infection and irritable bowel syndrome? A meta-analysis. World J Gastroenterol 2019; 25(37): 5702-5710
- URL: https://www.wjgnet.com/1007-9327/full/v25/i37/5702.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i37.5702
Irritable bowel syndrome (IBS) is one of the most common gastrointestinal (GI) disorders, characterized by chronic abdominal pain and a change in the frequency or form of stool[1]. It affects an estimated 10% to 15% of the global population[2] and carries a significant disease burden in terms of decreased productivity, increased healthcare costs and reduced health-related quality of life[3].
Despite the global prevalence of IBS, its pathophysiology remains unclear. Studies have reported disturbances in gut microbiota and persistent, subclinical systemic and mucosal inflammation in individuals with IBS[4]. Significant overlaps also exist between patients with IBS and those with dyspepsia[5], hinting at a possible pathogenic role of Helicobacter pylori (H. pylori) in IBS. H. pylori is a prevalent gram-negative bacterium that grows in the gut of more than half of the world’s population, and it is even more common in developing countries[6]. The mode of transmission of H. pylori is unclear, but believed to be fecal-oral. H. pylori, especially strains that produce cytotoxin-associated gene A (CagA) protein, causes chronic inflammation in the stomach and duodenum, microbial dysbiosis[7] as well as elevated systemic inflammation[8]. H. pylori infection has been linked to several conditions, including dyspepsia and even hyperemesis gravidarum[9].
However, its role in the pathogenesis of IBS remains largely unknown. Some studies have highlighted increased rates of H. pylori infection in patients with IBS compared to healthy controls[10,11], while others have disputed this and found no association between H. pylori infection and IBS[12]. This association has been challenged as H. pylori is thought to affect mainly the upper GI trait instead of the lower GI tract. Some also contend that the association is merely fortuitous given the widespread prevalence of H. pylori infection globally[6]. This meta-analysis thus aimed to investigate and better clarify the role of H. pylori in the pathogenesis of IBS. A better understanding of the pathogenesis of IBS has important clinical implications.
Literature search was performed in accordance with Meta-analysis of Observational Studies in Epidemiology (MOOSE) and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. By using the keywords “H. pylori OR Helicobacter OR Helicobacter pylori OR infection” AND ”irritable bowel syndrome OR IBS”, a preliminary search of PubMed, Medline, Embase, Cochrane Database of Systematic Reviews, Web of Science, Google Scholar and WanFang databases yielded 2924 papers published in English between 1 January 1960 and 1 June 2018. Attempts were made to search grey literature as well, using Google search engine and the Open System for Information on Grey Literature in Europe database. Title/abstract screening were performed independently by three researchers (Q.X.N., N.X.F. and W.R.L.) to identify articles of interest. For relevant abstracts, full articles were obtained, reviewed and also checked for references of interest. If necessary, the authors of the articles were contacted to provide additional data.
Full articles were obtained for all selected abstracts and reviewed by four researchers (Q.X.N., N.X.F, W.R.L. and Y.Q.K.) for inclusion. The inclusion criteria for this review were: (1) Published case-control or cross-sectional study; (2) patients with IBS; and (3) confirmed/laboratory testing for presence of H. pylori infection. Any disagreement was resolved by discussion and consensus amongst the three researchers. Each study was carefully reviewed and the primary outcome measure of interest was the proportion of H. pylori infection in patients with IBS compared to a control group. Odds ratio (OR) were calculated for each individual study, and estimates were pooled and where appropriate, 95% confidence intervals (95%CI) and P-values were calculated.
Heterogeneity amongst the different studies pooled was examined using the I2 statistic and Cochran’s Q test. Publication bias was assessed using a funnel plot and Egger test. All analyses were performed using MedCalc Statistical Software version 14.8.1 (MedCalc Software bvba, Ostend, Belgium; http://www.medcalc.org; 2014) and STATA version 13.0 (2000; STATA Corp., College Station, TX, United States).
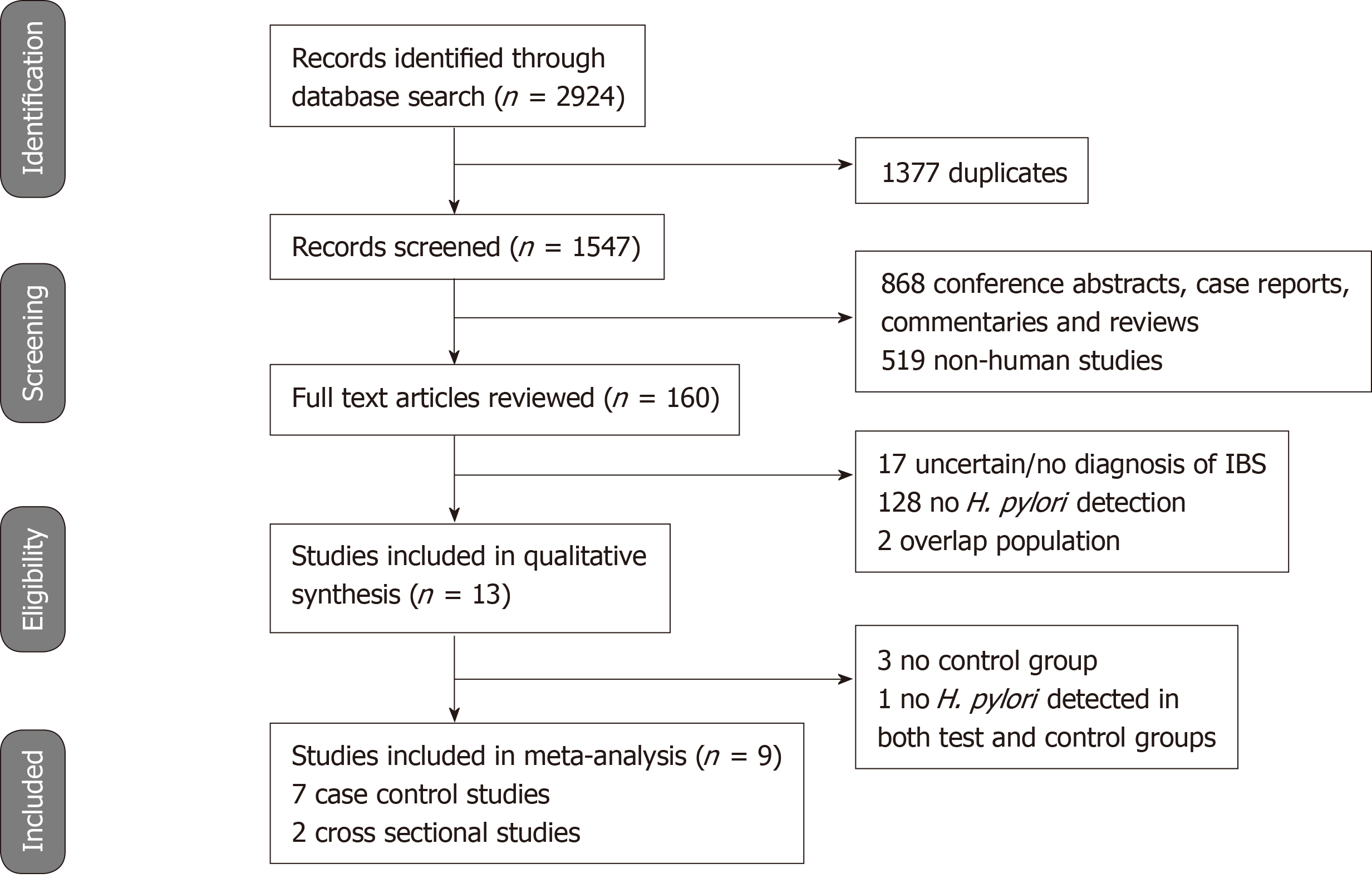
The literature search and abstraction process (and reasons for exclusion) was detailed in Figure 1. The key details of each study were extracted and summarized in Table 1[10-22]. A total of 13 studies were systematically reviewed. Four studies were excluded from the final meta-analysis as three did not have a control group while one did not detect H. pylori infection in either patients with IBS or healthy controls, hence no OR could be calculated.
| First author, Year | Study design | Study sample (n) | Country | Diagnosis of IBS | Method of H. pylori detection | Odds ratio (95%CI) | Conclusions |
| Abdelrazak et al[10], 2015 | Case control | 550 | Egypt | Rome III criteria | Stool antigen test or 13C-urea breath test positive | 8.56 (4.06, 18.05) | Significantly higher rate of H. pylori detection in pediatric patients with IBS compared to healthy controls |
| Agreus et al[13], 1995 | Case control | 150 | Sweden | More than 2 of the following symptoms (feeling of incomplete defecation, mucous stools, abdominal distension, abdominal pain or discomfort on defecation or relieved by defecation) and diarrhoea/constipation/or alternating diarrhoea and constipation and abdominal discomfort | Serum IgG by ELISA | 0.56 (0.25, 1.25) | No association between H. pylori seropositivity and dyspepsia or IBS |
| Corsetti et al[14], 2004 | Case control | 309 | Belgium | Rome II criteria | Gastric biopsy specimens | 0.74 (0.36, 1.51) | The prevalence of H. pylori infection did not differ between patients with functional dyspepsia alone and patients with functional dyspepsia and IBS |
| El-Badry et al[15], 2018 | Cross sectional | 115 | Egypt | Rome III criteria | H. pylori stool coproantigen | NA | H. pylori was detected in 55.7% of patients with IBS |
| Gerards et al[16], 2001 | Case control | 46 | Germany | Not specified | 13C-urea breath test | 0.96 (0.24, 3.87) | Rectal distension produced abdominal pain only in patients with IBS and who were H. pylori infected. H. pylori may contribute to visceral hypersensitivity |
| Hasan et al[17], 2017 | Cross sectional | 184 | Iraq | Based on clinical and ultrasonography results | Serum IgG by ELISA | 0.54 (0.278, 1.03) | Rate of H. pylori infection similar between patients with IBS and healthy controls |
| Locke et al[18], 2000 | Cross sectional | 148 | United States | Abdominal pain with at least two of six Manning criteria symptoms | Serum IgG by ELISA and CagA IgG | 7.22 (2.91, 17.9) | After adjusting for age, CagA-positivity but not H. pylori seropositivity was associated with IBS |
| Malinen et al[12], 2005 | Case control | 49 | Finland | Rome II criteria | Real-time PCR analysis of fecal samples | NA | H. pylori was not detected in any of the control or test subjects. PCR assay may lack sensitivity |
| McDonald et al[19], 2017 | Cross sectional | 112 | Peru | Rome III criteria | Endoscopy specimens | NA | H. pylori infection was detected in 58 (57.4%) of patients with IBS |
| Su et al[20], 2000 | Cross sectional | 69 | Taiwan | Rome I criteria | 13C-urea breath test and endoscopy specimens | NA | H. pylori infection was detected in 33 (47.8%) of patients with IBS |
| Xiong et al[21], 2016 | Case control | 502 | China | Rome III criteria | Not specified (presumably seropositivity) | 0.96 (0.77, 1.19) | The prevalence of H. pylori infection in patients with IBS-D was similar to the general population and eradication therapy did not improve symptoms |
| Yakoob et al[22], 2012 | Case control | 330 | Pakistan | Rome III criteria | Gastric biopsy specimens | 1.76 (1.12, 2.75) | H. pylori infection was common in patients with IBS-D, and was associated with predominantly cagAs1-positive strains |
| Yang et al[11], 2017 | Case control | 670 | China | Rome III criteria | Positive for rapid urease test and 14C-urea breath test | 1.62 (1.19, 2.20) | The rate of H. pylori infection was significantly higher in patients with IBS-D than healthy controls, however, eradication of H. pylori did not improve symptoms |
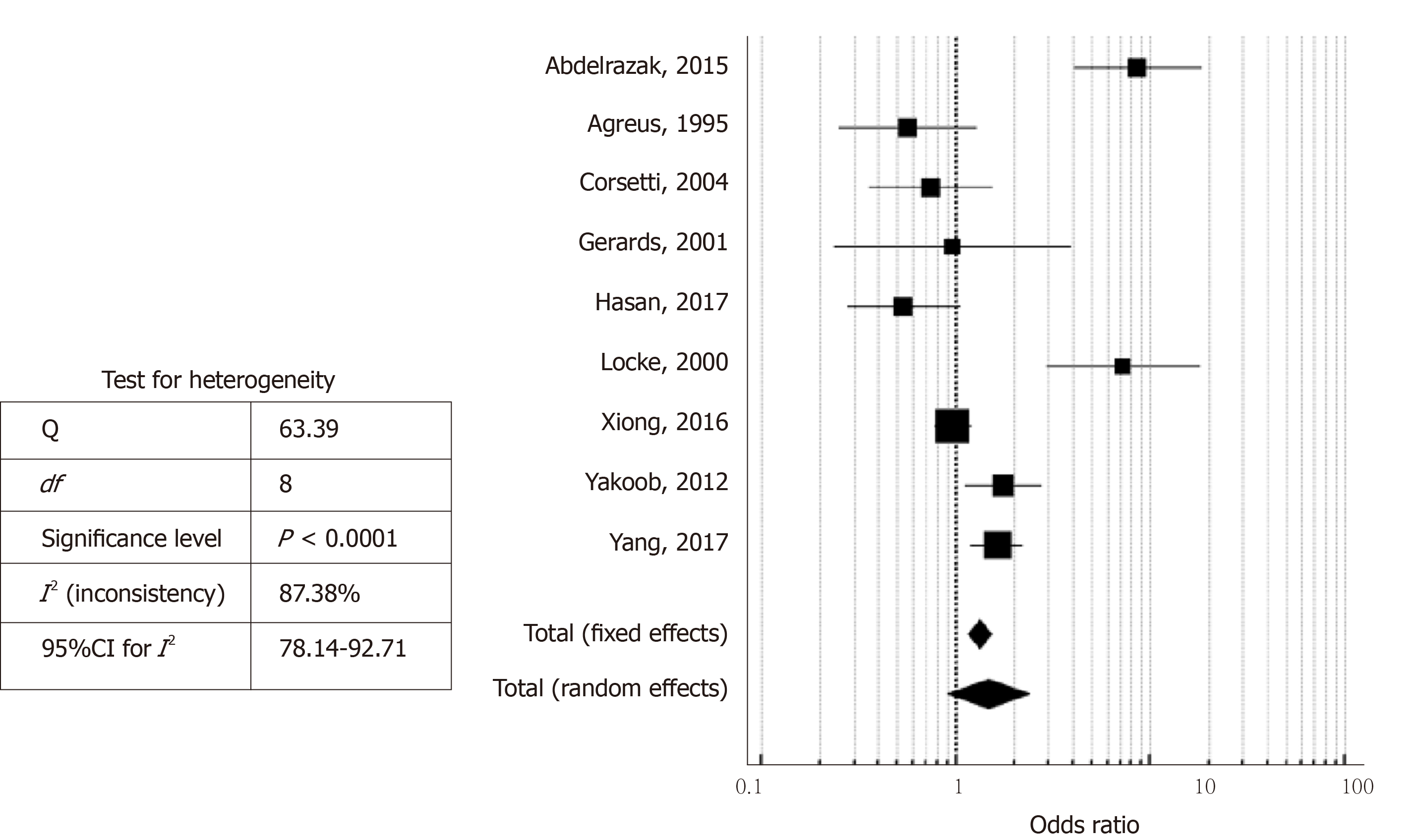
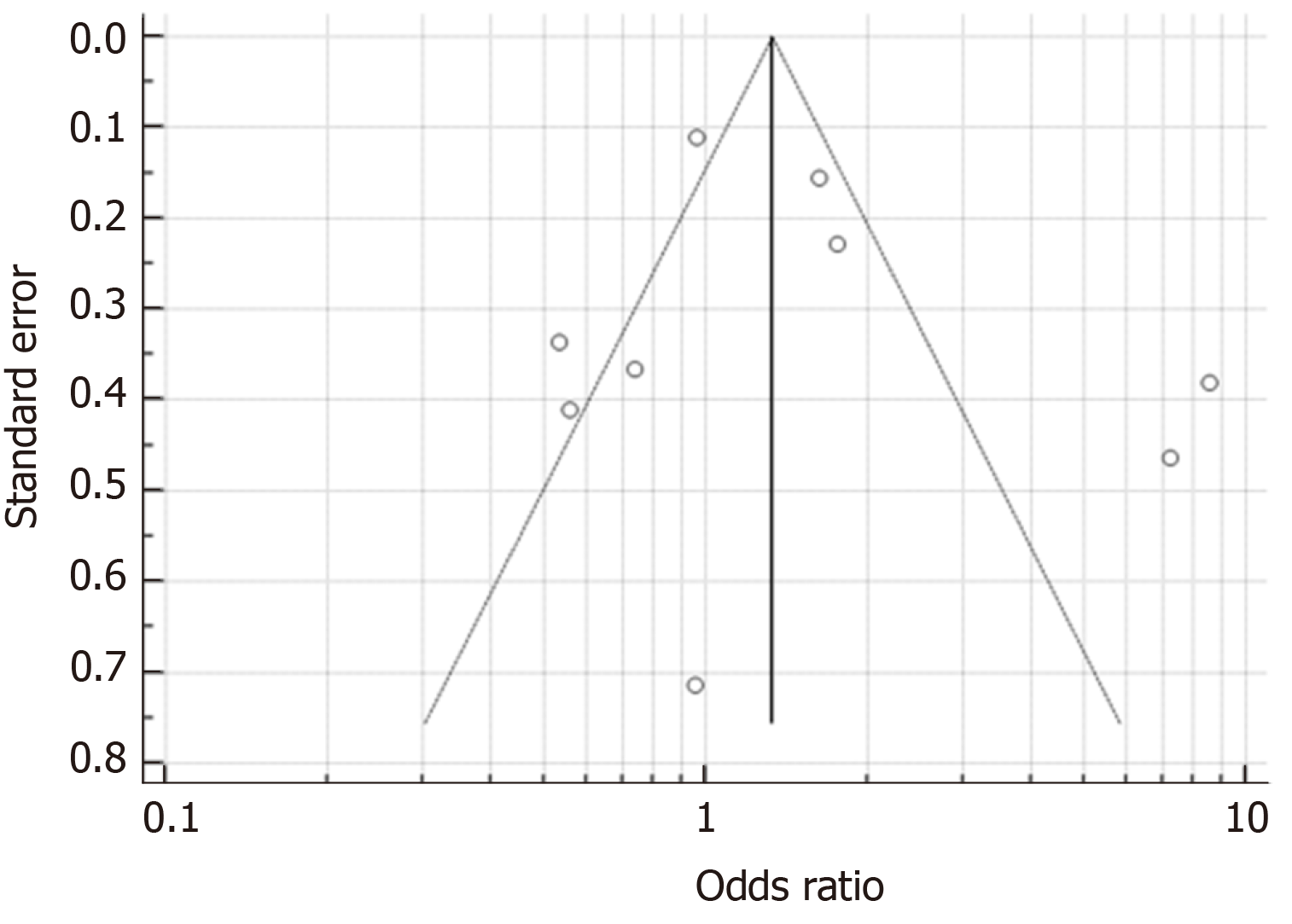
As seen in Figure 2, the studies had an overall high degree of heterogeneity (I2 = 87.38%), likely due to the different study designs and method of detection of H. pylori employed. Random-effects meta-analysis found that patients with IBS did not have a significantly increased likelihood of H. pylori infection, as the pooled OR was 1.47 (95%CI: 0.90-2.40, P = 0.123). Separate subgroup analyses and sensitivity analyses were likely underpowered and hence, were not conducted due to the small number of studies available. With regard to the possibility of publication bias, visual inspection of the funnel plot revealed a roughly symmetrical distribution of studies (Figure 3) and encouragingly, Egger test was not significant for publication bias (P = 0.189).
Overall, current evidence suggests that patients with IBS may have an increased likelihood of H. pylori infection, but this is not statistically significant (pooled OR 1.47, 95%CI: 0.90-2.40, P = 0.123). It must also be acknowledged that all of the available studies reported only crude odd ratios and did not adjust for potential confounders, further weakening any potential association between IBS and H. pylori infection. To the best of our knowledge, this review is the first to examine the association between IBS and H. pylori infection. The current meta-analysis is therefore a novel and significant contribution to current literature.
It is well demonstrated that H. pylori infection leads to chronic inflammation and is involved in the etiopathogenesis of atrophic gastritis, intestinal metaplasia and peptic ulcers[23]. Patients with IBS have been found to have increased lamina propria immune cells in the colonic mucosa[24] and significantly reduced levels of oleoylethanolamide (a fatty acid amide with anti-inflammatory properties) when compared to healthy controls[25]. These are suggestive of chronic, subclinical inflammation at the microscopic level[26]. Increased infiltration of mucosal mast cells have also been reported in the GI tract of patients with IBS when compared to healthy controls[27]. In considering the possible pathogenic mechanisms of H. pylori in relation to IBS, H. pylori infection has been associated with elevated inflammatory markers[8], increased mast cell activation[28] and gastric mucosal and neural remodeling[29]. Vacuolating cytotoxin A[30] and the neutrophil-activating protein[28] of H. pylori are both potent mast cell stimulators. Although a definite and consistent pattern of immune dysregulation has yet to be established in patients with IBS, increased mast cell activation and immune activity in the gut may correlate with symptoms of visceral hypersensitivity[31].
Furthermore, in a study utilizing the rectal barostat to elicit abdominal symptoms in patients with IBS, positive results were seen almost exclusively in H. pylori-positive patients with IBS, suggesting a potential role of H. pylori in stimulating visceral hypersensitivity[16]. Preclinical and clinical studies have often reported a link between increased intestinal mucosal inflammation and changes in sensory-motor function[32,33]. As such, H. pylori infection may result in gastric dysmotility and neuroplastic changes in the afferent neural pathways, giving rise to visceral hypersensitivity and prototypical IBS symptoms.
On the other hand, contrary findings have also been reported. A study on patients with functional dyspepsia found no association between H. pylori infection and increased pain perception of gastric distension[34]. Studies that investigated the effect of H. pylori eradication therapy on IBS symptoms also found no significant differences at follow-up[11,21]. However, the relationship is difficult to analyse as it may be confounded by the fact that H. pylori is eradicated with antibiotics, which is also associated with a significantly increased risk of developing IBS[35] and may also aggravate IBS symptoms[36].
A fundamental understanding of the pathogenesis of IBS is still lacking. Additionally, psychological factors such as stress, depression and anxiety are known to contribute to the pathogenesis[37]. Our study investigated another potential contributory factor. Patients with IBS may have an increased likelihood of H. pylori infection albeit this is not statistically significant. The role of H. pylori eradication therapy is also unclear as it does not appear to improve IBS symptoms in the limited studies available.
Other limitations of current evidence that must be discussed include the fact that some of the available studies[13,18] used a self-report symptom questionnaire in the diagnosis of IBS. There is a known wide variability in the definition of constipation and diarrhoea[38], and the subjectivity and inter-study variability in the diagnosis of IBS could further affect the reliability of current findings. Also, some of the studies[13,18] included in the meta-analysis did not investigate study participants for organic disease that may contribute to IBS-like symptoms. Limited studies also performed CagA testing. In one study[18], CagA antibody positivity but not H. pylori seropositivity was found to be significantly associated with IBS. Future studies should examine the effect of CagA positivity as the CagA toxin is an important H. pylori virulence factor associated with a greater inflammatory response[39]. There was also a significant degree of heterogeneity amongst the various studies included in the meta-analysis (I2 = 87.38%). This could stem from the subjectivity and different definitions used in the diagnosis of IBS as previously discussed, as well as the differing tests used to detect H. pylori infection, e.g., serum IgG antibodies, urea breath test and stool antigen assay. Moreover, the commonly-used serologic test is unable to distinguish between current and previous H. pylori infection as it remains positive for years, even after H. pylori eradication therapy[40]. Although some studies carefully selected only individuals who have no history of previous H. pylori eradication therapy[16], it was less clear in other studies. The duration of H. pylori infection may also affect our analysis as study subjects with more longstanding infection may have greater mucosal inflammation and more significant GI symptoms.
Last but not least, the influence of H. pylori on the composition of distal gut microbiota is an important area that deserves further study. Microbial dysbiosis is a known hallmark of IBS[41]. However, it is unclear how H. pylori, which is thought to affect mainly the upper GI tract, may affect the lower GI tract[42].
In conclusion, current evidence does not support an association between IBS and H. pylori infection. Patients with IBS may have a slight increased likelihood of H. pylori infection albeit this is not statistically significant. This relationship is complicated by admittedly problematic study designs and potential confounding factors. The role of H. pylori eradication therapy also remains unclear as it does not appear to improve IBS symptoms. Further rigorous and detailed studies with larger sample sizes, carefully selected subjects, and after H. pylori eradication therapy are warranted. The influence of H. pylori on gut microbiota should also be investigated.
Helicobacter pylori (H. pylori) is a prevalent gram-negative bacterium found in the human gut. H. pylori infection has been linked to several conditions, including dyspepsia and even hyperemesis gravidarum. However, its role in the pathogenesis of irritable bowel syndrome (IBS) remains largely unknown.
An improved understanding of the pathogenic mechanisms of IBS may lead to more effective therapeutics.
To investigate the association between H. pylori infection and IBS.
A comprehensive search of PubMed, Medline, Embase, Cochrane Database of Systematic Reviews, Web of Science, Google Scholar and WanFang databases was performed using the keywords “H. pylori OR Helicobacter OR Helicobacter pylori OR infection” AND “irritable bowel syndrome OR IBS”.
A total of 13 clinical studies were systematically reviewed and nine studies were included in the final meta-analysis. Random-effects meta-analysis found a slight increased likelihood of H. pylori infection in patients with IBS, albeit this was not statistically significant (pooled odds ratio 1.47, 95% confidence interval: 0.90-2.40, P = 0.123). H. pylori eradication therapy also does not appear to improve IBS symptoms in the limited studies available.
Current evidence does not support an association between IBS and H. pylori infection. This relationship is complicated by admittedly problematic study designs and potential confounding factors. H. pylori is eradicated with antibiotics, which is also associated with a significantly increased risk of developing IBS and may also aggravate IBS symptoms.
Further rigorous and detailed trials with larger sample sizes, carefully selected subjects, and after H. pylori eradication therapy are warranted. The influence of H. pylori on gut microbiota also remains unknown and should be investigated.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Singapore
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Grawish ME, Jadallah KA, Tsukanov V, Yang SS S-Editor: Yan JP L-Editor: A E-Editor: Ma YJ
| 1. | Drossman DA. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV. Gastroenterology. 2016;pii: S0016-5085(16)00223-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1366] [Cited by in RCA: 1383] [Article Influence: 153.7] [Reference Citation Analysis (1)] |
| 2. | Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol. 2012;10:712-721.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1251] [Cited by in RCA: 1415] [Article Influence: 108.8] [Reference Citation Analysis (2)] |
| 3. | Akehurst RL, Brazier JE, Mathers N, O'Keefe C, Kaltenthaler E, Morgan A, Platts M, Walters SJ. Health-related quality of life and cost impact of irritable bowel syndrome in a UK primary care setting. Pharmacoeconomics. 2002;20:455-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 148] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 4. | Barbara G, Cremon C, De Giorgio R, Dothel G, Zecchi L, Bellacosa L, Carini G, Stanghellini V, Corinaldesi R. Mechanisms underlying visceral hypersensitivity in irritable bowel syndrome. Curr Gastroenterol Rep. 2011;13:308-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 101] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 5. | Agréus L, Svärdsudd K, Nyrén O, Tibblin G. Irritable bowel syndrome and dyspepsia in the general population: overlap and lack of stability over time. Gastroenterology. 1995;109:671-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 459] [Cited by in RCA: 449] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 6. | Hooi JKY, Lai WY, Ng WK, Suen MMY, Underwood FE, Tanyingoh D, Malfertheiner P, Graham DY, Wong VWS, Wu JCY, Chan FKL, Sung JJY, Kaplan GG, Ng SC. Global Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology. 2017;153:420-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1361] [Cited by in RCA: 2047] [Article Influence: 255.9] [Reference Citation Analysis (0)] |
| 7. | Kim YJ, Chung WC, Kim BW, Kim SS, Kim JI, Kim NJ, Yoo J, Kim SH. Is Helicobacter pylori Associated Functional Dyspepsia Correlated With Dysbiosis? J Neurogastroenterol Motil. 2017;23:504-516. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Jackson L, Britton J, Lewis SA, McKeever TM, Atherton J, Fullerton D, Fogarty AW. A population-based epidemiologic study of Helicobacter pylori infection and its association with systemic inflammation. Helicobacter. 2009;14:108-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 69] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 9. | Ng QX, Venkatanarayanan N, De Deyn MLZQ, Ho CYX, Mo Y, Yeo WS. A meta-analysis of the association between Helicobacter pylori (H. pylori) infection and hyperemesis gravidarum. Helicobacter. 2018;23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Abdelrazak MA, Walid F, Abdelrahman M, Mahmoud M. Interrelation between helicobacter pylori infection, infantile colic, and irritable bowel syndrome in pediatric patients. J Gastrointest Dig Syst. 2015;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Yang Y, Chen LF. Role of Helicobacter pylori Eradication in Diarrhea-predominant Irritable Bowel Syndrome. Wei Chang Bing Xue. 2017;22:482-485. [DOI] [Full Text] |
| 12. | Malinen E, Rinttilä T, Kajander K, Mättö J, Kassinen A, Krogius L, Saarela M, Korpela R, Palva A. Analysis of the fecal microbiota of irritable bowel syndrome patients and healthy controls with real-time PCR. Am J Gastroenterol. 2005;100:373-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 502] [Cited by in RCA: 498] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 13. | Agréus L, Engstrand L, Svärdsudd K, Nyrén O, Tibblin G. Helicobacter pylori seropositivity among Swedish adults with and without abdominal symptoms. A population-based epidemiologic study. Scand J Gastroenterol. 1995;30:752-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 47] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Corsetti M, Caenepeel P, Fischler B, Janssens J, Tack J. Impact of coexisting irritable bowel syndrome on symptoms and pathophysiological mechanisms in functional dyspepsia. Am J Gastroenterol. 2004;99:1152-1159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 125] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 15. | El-Badry AA, Abd El Wahab WM, Hamdy DA, Aboud A. Blastocystis subtypes isolated from irritable bowel syndrome patients and co-infection with Helicobacter pylori. Parasitol Res. 2018;117:127-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 16. | Gerards C, Leodolter A, Glasbrenner B, Malfertheiner P. H. pylori infection and visceral hypersensitivity in patients with irritable bowel syndrome. Dig Dis. 2001;19:170-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Hasan AS, Jaafer AM, Athab AM. Rate of Helicobacter pylori infection among patients with irritable bowel syndrome. Gulf Med J. 2017;6:16-21. |
| 18. | Locke CR, Talley NJ, Nelson DK, Haruma K, Weaver AL, Zinsmeister AR, Melton LJ. Helicobacter pylori and dyspepsia: a population-based study of the organism and host. Am J Gastroenterol. 2000;95:1906-1913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | McDonald K, Shopinski S, Wilkinson A, Meza C, Cok J, Bussalleu A, Valdivieso M. Correlation between functional gastrointestinal disorders and gastric mucosa histopathology findings, including Helicobacter pylori infection, in Lima, Peru. Revista de Gastroenterología del Perú. 2017;. |
| 20. | Su YC, Wang WM, Wang SY, Lu SN, Chen LT, Wu DC, Chen CY, Jan CM, Horowitz M. The association between Helicobacter pylori infection and functional dyspepsia in patients with irritable bowel syndrome. Am J Gastroenterol. 2000;95:1900-1905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Xiong F, Xiong M, Ma Z, Huang S, Li A, Liu S. Lack of Association Found between Helicobacter pylori Infection and Diarrhea-Predominant Irritable Bowel Syndrome: A Multicenter Retrospective Study. Gastroenterol Res Pract. 2016;2016:3059201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | Yakoob J, Abbas Z, Naz S, Islam M, Jafri W. Virulence markers of Helicobacter pylori in patients with diarrhoea-dominant irritable bowel syndrome. Br J Biomed Sci. 2012;69:6-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Crowe SE. Helicobacter infection, chronic inflammation, and the development of malignancy. Curr Opin Gastroenterol. 2005;21:32-38. [PubMed] |
| 24. | Salzmann JL, Peltier-Koch F, Bloch F, Petite JP, Camilleri JP. Morphometric study of colonic biopsies: a new method of estimating inflammatory diseases. Lab Invest. 1989;60:847-851. [PubMed] |
| 25. | Cremon C, Stanghellini V, Barbaro MR, Cogliandro RF, Bellacosa L, Santos J, Vicario M, Pigrau M, Alonso Cotoner C, Lobo B, Azpiroz F, Bruley des Varannes S, Neunlist M, DeFilippis D, Iuvone T, Petrosino S, Di Marzo V, Barbara G. Randomised clinical trial: the analgesic properties of dietary supplementation with palmitoylethanolamide and polydatin in irritable bowel syndrome. Aliment Pharmacol Ther. 2017;45:909-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 91] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 26. | Ng QX, Soh AYS, Lim DY, Yeo WS. Agomelatine, a novel therapeutic option for the management of irritable bowel syndrome. J Clin Pharm Ther. 2018;43:752-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 27. | O'Sullivan M, Clayton N, Breslin NP, Harman I, Bountra C, McLaren A, O'Morain CA. Increased mast cells in the irritable bowel syndrome. Neurogastroenterol Motil. 2000;12:449-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 340] [Cited by in RCA: 340] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 28. | Montemurro P, Nishioka H, Dundon WG, de Bernard M, Del Giudice G, Rappuoli R, Montecucco C. The neutrophil-activating protein (HP-NAP) of Helicobacter pylori is a potent stimulant of mast cells. Eur J Immunol. 2002;32:671-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 29. | Stead RH, Hewlett BR, Lhotak S, Colley ECC, Frendo M, Dixon MF. Do gastric mucosal nerves remodel in H. pylori gastritis? In: Hunt RH, Tytgat GNJ, eds. Helicobacter pylori. Springer, Dordrecht; 1994; 281-291. |
| 30. | Supajatura V, Ushio H, Wada A, Yahiro K, Okumura K, Ogawa H, Hirayama T, Ra C. Cutting edge: VacA, a vacuolating cytotoxin of Helicobacter pylori, directly activates mast cells for migration and production of proinflammatory cytokines. J Immunol. 2002;168:2603-2607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 123] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 31. | Ohman L, Simrén M. Pathogenesis of IBS: role of inflammation, immunity and neuroimmune interactions. Nat Rev Gastroenterol Hepatol. 2010;7:163-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 399] [Cited by in RCA: 443] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 32. | Rao SS, Read NW, Brown C, Bruce C, Holdsworth CD. Studies on the mechanism of bowel disturbance in ulcerative colitis. Gastroenterology. 1987;93:934-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 132] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 33. | Stanghellini V, Barbara G, de Giorgio R, Tosetti C, Cogliandro R, Cogliandro L, Salvioli B, Corinaldesi R. Review article: Helicobacter pylori, mucosal inflammation and symptom perception--new insights into an old hypothesis. Aliment Pharmacol Ther. 2001;15 Suppl 1:28-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 34. | Mearin F, de Ribot X, Balboa A, Salas A, Varas MJ, Cucala M, Bartolomé R, Armengol JR, Malagelada JR. Does Helicobacter pylori infection increase gastric sensitivity in functional dyspepsia? Gut. 1995;37:47-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 93] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 35. | Ianiro G, Tilg H, Gasbarrini A. Antibiotics as deep modulators of gut microbiota: between good and evil. Gut. 2016;65:1906-1915. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 357] [Cited by in RCA: 442] [Article Influence: 49.1] [Reference Citation Analysis (0)] |
| 36. | Maxwell PR, Rink E, Kumar D, Mendall MA. Antibiotics increase functional abdominal symptoms. Am J Gastroenterol. 2002;97:104-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 113] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 37. | Grinsvall C, Törnblom H, Tack J, Van Oudenhove L, Simrén M. Psychological factors selectively upregulate rectal pain perception in hypersensitive patients with irritable bowel syndrome. Neurogastroenterol Motil. 2015;27:1772-1782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 38. | Soh AYS, Kang JY, Siah KTH, Scarpignato C, Gwee KA. Searching for a definition for pharmacologically refractory constipation: A systematic review. J Gastroenterol Hepatol. 2018;33:564-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 39. | Jafarzadeh A, Hassanshahi GH, Nemati M. Serum levels of high-sensitivity C-reactive protein (hs-CRP)in Helicobacter pylori-infected peptic ulcer patients and its association with bacterial CagA virulence factor. Dig Dis Sci. 2009;54:2612-2616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 40. | Ricci C, Holton J, Vaira D. Diagnosis of Helicobacter pylori: invasive and non-invasive tests. Best Pract Res Clin Gastroenterol. 2007;21:299-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 143] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 41. | Collins SM. A role for the gut microbiota in IBS. Nat Rev Gastroenterol Hepatol. 2014;11:497-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 261] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 42. | Schulz C, Koch N, Schütte K, Pieper DH, Malfertheiner P. H. pylori and its modulation of gastrointestinal microbiota. J Dig Dis. 2015;16:109-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |