Published online Sep 14, 2019. doi: 10.3748/wjg.v25.i34.5210
Peer-review started: March 25, 2019
First decision: April 11, 2019
Revised: July 14, 2019
Accepted: August 7, 2019
Article in press: August 7, 2019
Published online: September 14, 2019
Processing time: 174 Days and 4.2 Hours
Bilateral vs unilateral biliary stenting is used for palliation in malignant biliary obstruction. No clear data is available to compare the efficacy and safety of bilateral biliary stenting over unilateral stenting.
To assess the efficacy and safety of bilateral vs unilateral biliary drainage in inoperable malignant hilar obstruction.
PubMed, Embase, Scopus, and Cochrane databases, as well as secondary sources (bibliographic review of selected articles and major GI proceedings), were searched through January 2019. The primary outcome was the re-intervention rate. Secondary outcomes were a technical success, early and late complications, and stent malfunction rate. Pooled odds ratio (OR) and 95% confidence interval (CI) were calculated for each outcome.
A total of 9 studies were included (2 prospective Randomized Controlled Study, 5 retrospective studies, and 2 abstracts), involving 782 patients with malignant hilar obstruction. Bilateral stenting had significantly lower re-intervention rate compared with unilateral drainage (OR = 0.59, 95%CI: 0.40-0.87, P = 0.009). There was no difference in the technical success rate (OR = 0.7, CI: 0.42-1.17, P = 0.17), early complication rate (OR = 1.56, CI: 0.31-7.75, P = 0.59), late complication rate (OR = 0.91, CI: 0.58-1.41, P = 0.56) and stent malfunction (OR = 0.69, CI: 0.42-1.12, P = 0.14) between bilateral and unilateral stenting for malignant hilar biliary strictures.
Bilateral biliary drainage had a lower re-intervention rate as compared to unilateral drainage for high grade inoperable malignant biliary strictures, with no significant difference in technical success, and early or late complication rates.
Core tip: Biliary drainage is useful to control jaundice and cholangitis in patients with inoperable malignant hilar strictures. No consensus guidelines are available to decide if bilateral stenting has any advantage over unilateral stenting. This meta-analysis adds to the growing body of evidence that bilateral stenting is technically feasible with similar early and late complications and leads to lower re-intervention rates.
- Citation: Ashat M, Arora S, Klair JS, Childs CA, Murali AR, Johlin FC. Bilateral vs unilateral placement of metal stents for inoperable high-grade hilar biliary strictures: A systemic review and meta-analysis. World J Gastroenterol 2019; 25(34): 5210-5219
- URL: https://www.wjgnet.com/1007-9327/full/v25/i34/5210.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i34.5210
Unresectable malignant hilar obstruction (UMHO) is associated with very poor prognosis. Five-year survival is < 10% with most patients dying within 1 year of diagnosis[1,2]. Compared to plastic stents, self-expanding metallic stents (SEMS) have shown to be more cost effective and provides advantage with longer stent patency and less re-intervention rate in patients with non-operable malignancy with score of II to IV on Bismuth-Corlette classification and Hilar cholangiocarcinoma who have a predicted the life expectancy of > 3 mo[3-5]. Biliary stenting also plays a role in the management of obstructive jaundice and cholangitis and is important in enhancing the quality of life of patients with UMHO.
Although endoscopic stenting is widely favored in cases of UMHO, there is currently no consensus on whether the placement of bilateral biliary stents has any advantage for these patients over unilateral stenting. Although some experts believe in measuring the volume of the liver to be drained to determine the type of stent to be used, quantification of the liver volume is clinically challenging. Furthermore, there have been conflicting data regarding the technical success and outcomes of bilateral and unilateral stenting. While some authors believe that unilateral stenting renders increased technical success rate with concomitant lower complications[6-8]; bilateral stenting, on the other hand, will drain higher liver volume, may have longer stent patency, and hence may require less re-intervention[9-11].
The aim of the meta-analysis was to systematically review the current literature and compare the efficacy of unilateral vs bilateral stenting in achieving successful stent placement, comparing re-intervention rate, technical success, and early and late procedure-related complications for unresectable malignant hilar strictures.
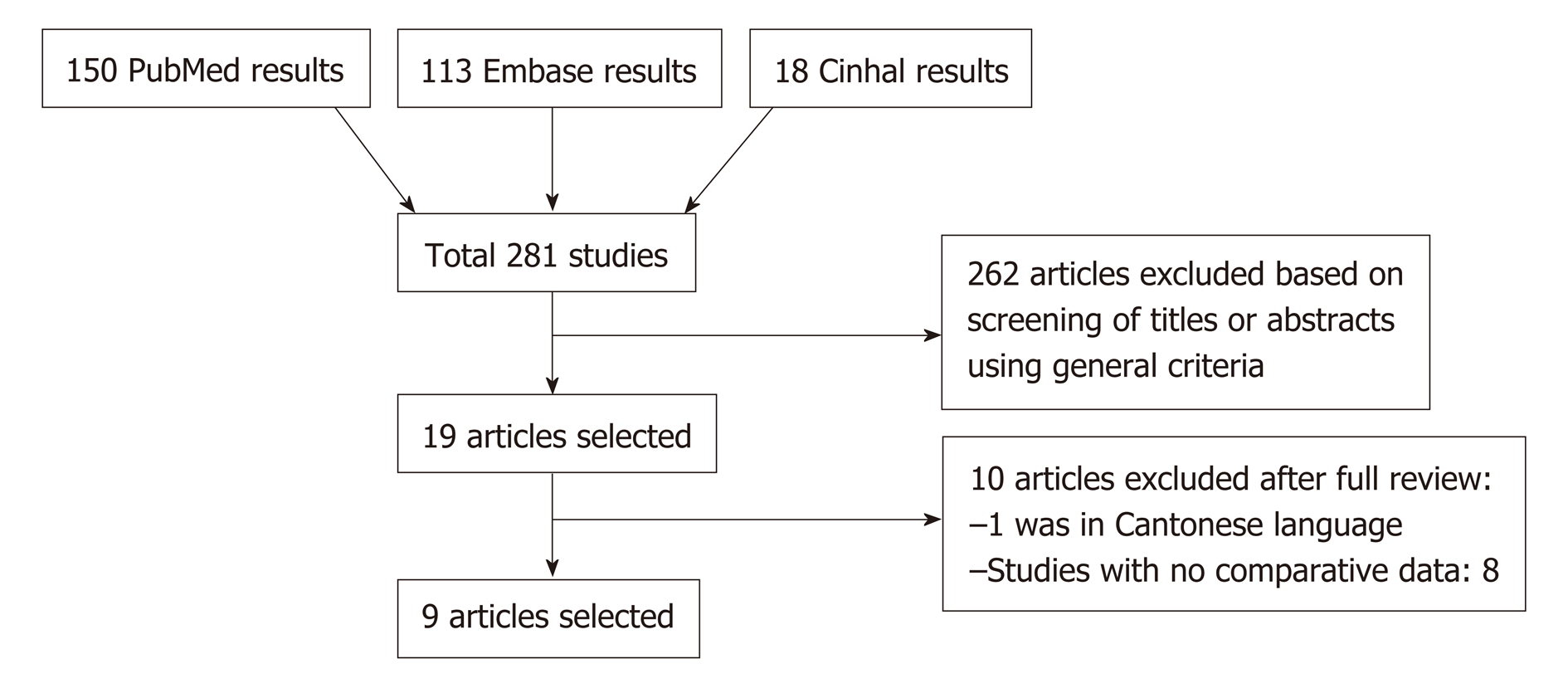
Search strategies were developed with the assistance of a health sciences librarian with expertise in searching for systematic reviews. Comprehensive search strategies using index and keywords were constructed for PubMed, Embase (Elsevier), and Cinhal (EBSCO). No database filters were used at any time during the searching process. All searches were conducted during January 2019 and the number of citations found in each database can be found in the flow diagram (Figure 1). The searches combined the following concepts: Unilateral SEMS and bilateral SEMS with biliary stents. Within the results for those combined concepts, additional filters, publication types, and keyword strategies were used to identify and exclude the most common articles types that do not report trial results (reviews and case studies). An exhaustive forward search tool was used for the Web of Science database to capture all possible studies of interest. The databases were searched for publications dates 1995 to present. Language limits were applied to search for articles in English only. To identify further articles, references were hand searched. All results were downloaded into EndNote (Thompson ISI Research Soft, Philadelphia, PA, United States), a bibliographic database manager, and duplicate citations were identified and removed. In addition, abstracts from Digestive Disease Week, annual meetings of American College of Gastroenterology, and United European Gastroenterology Week from the last 5 years were also searched.
Prospective studies, retrospective studies, and abstracts published in the English language were included if they compared unilateral vs bilateral SEMS biliary stent placement, for one or more of the clinical outcomes: Re-intervention rate, technical success, complication rate, and stent malfunction.
Studies were excluded when there was no comparison between unilateral and bilateral stents. We also excluded studies that did not evaluate the required pre-defined endpoints. Furthermore, duplicate studies, case reports, animal studies, and letters to editors were excluded.
Two authors (Ashat M and Arora S) independently extracted the data according to a pre-specified protocol from all the included studies. All discrepancies were resolved after discussion with a third reviewer.
Cohort studies were assessed using the Newcastle-Ottawa Scale and for randomized control trials, Cochrane tool was used to assess for risk of bias[12,13]. Risk of publication bias for each end-point was assessed using the funnel plots.
The data collected from eligible studies included following data points-publication year, authors, country of publication, study design, mean age of study participants, a total number of patients in each unilateral stenting and bilateral stenting category and type of malignancy, complications rates, and type of complications Supplemental (Table 1).
Primary end-point of the study was the re-intervention rate. This was defined as an endoscopic or percutaneous intervention that was done for stent failure and to increase biliary drainage or for recurrent jaundice, or for management of dilated intra-hepatic bile duct revealed by imaging or management of immediate adverse event of successfully inserted SEMS. Secondary outcomes were (1) Technical success was defined by the successful placement of bilateral or unilateral SEMS across stricture site, confirmed by the flow of contrast or bile through SEMS; (2) Early adverse event rate- defined as early stent-related complications within 4 wk. Early complications included cholangitis, cholecystitis, pancreatitis, bleeding, and liver abscess; (3) Late adverse events were defined as any stent-related complication that occurred after 4 wk of stent insertion. Late complication included cholangitis, cholecystitis, liver abscess; and (4) Stent malfunction defined as stent obstruction due to sludge or stone formation, cholangitis, tumor in-growth, or development of a liver abscess, or biloma.
Review Manager 5.3 (The Cochrane Collaboration, Oxford, United Kingdom) was used to analyze the data for the meta-analysis. Pooled odds ratios (ORs) and 95% confidence interval (CI) of study end-points were calculated using the Mantel-Haenszel method. In order to access of heterogeneity, we used X2 test (Cochran Q statistic). In case there was significant heterogeneity, a random-effect model was used. Funnel plots were obtained to assess the risk of bias.
Using pre-defined parameters and removing duplicate publications our search strategy identified 281 articles. Another 2 articles were identified by manual search. A total of 262 articles were excluded based on our exclusion criterion. Based on our inclusion criterions, 9 studies were selected (Figure 1). Of these 9 studies, 7 were published manuscripts and 2 were published as abstracts. All the baseline characteristics of each individual studies are highlighted in Supplemental Table 1.
The characteristics of the studies, and of the patients in the selected studies are shown in Supplemental Table 1. A total of 9 studies were enrolled in the current study of which 2 were randomized control trial’s (RCT), and 7 were retrospective trials (5 complete manuscripts and 2 abstracts). Although the study by Mukai et al[14] was an RCT, for our analysis we used only bilateral stents subgroup of the study which was not randomized. A total of 782 patients were included in the analysis of bilateral vs unilateral biliary stenting.
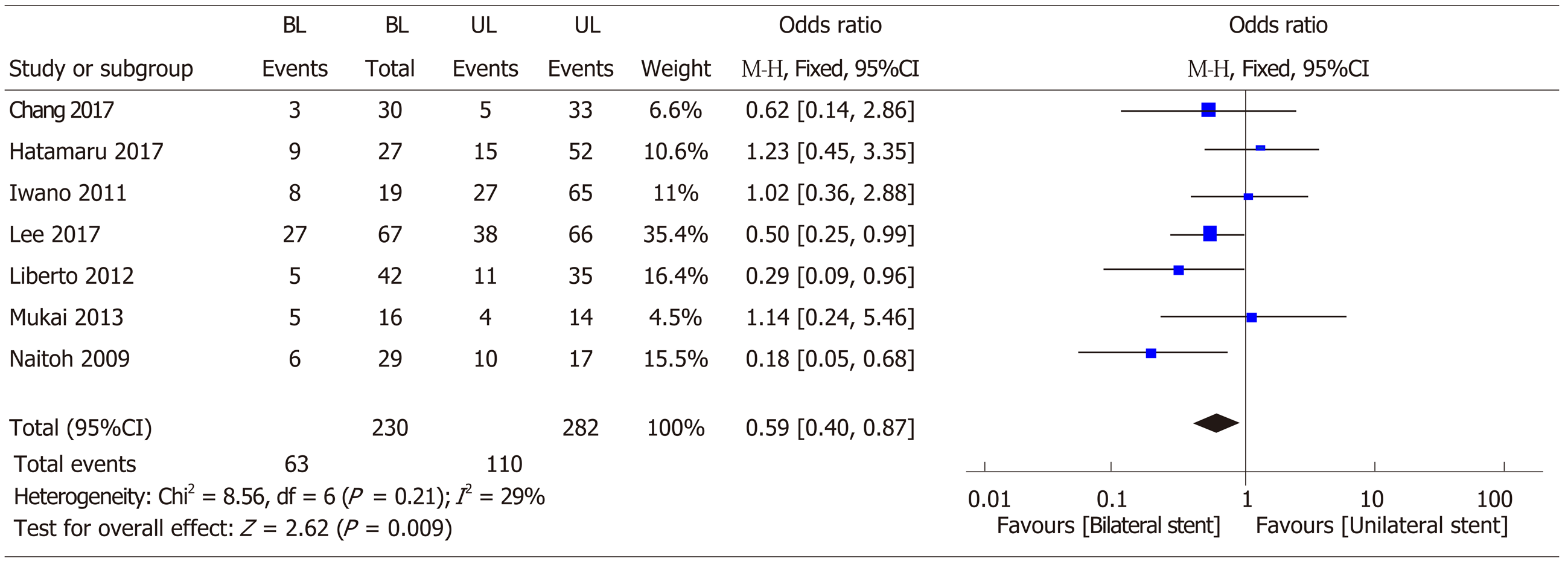
Primary end-point: Re-intervention rate: A total of 7 studies involving 513 patients was included in this analysis[7,10,14-18]. Bilateral stenting required significantly lower re-intervention as compared to unilateral stenting (OR = 0.59, 95%CI: 0.40-0.87, P = 0.009) (Figure 2). The funnel plot showed no asymmetry (Figure 3).
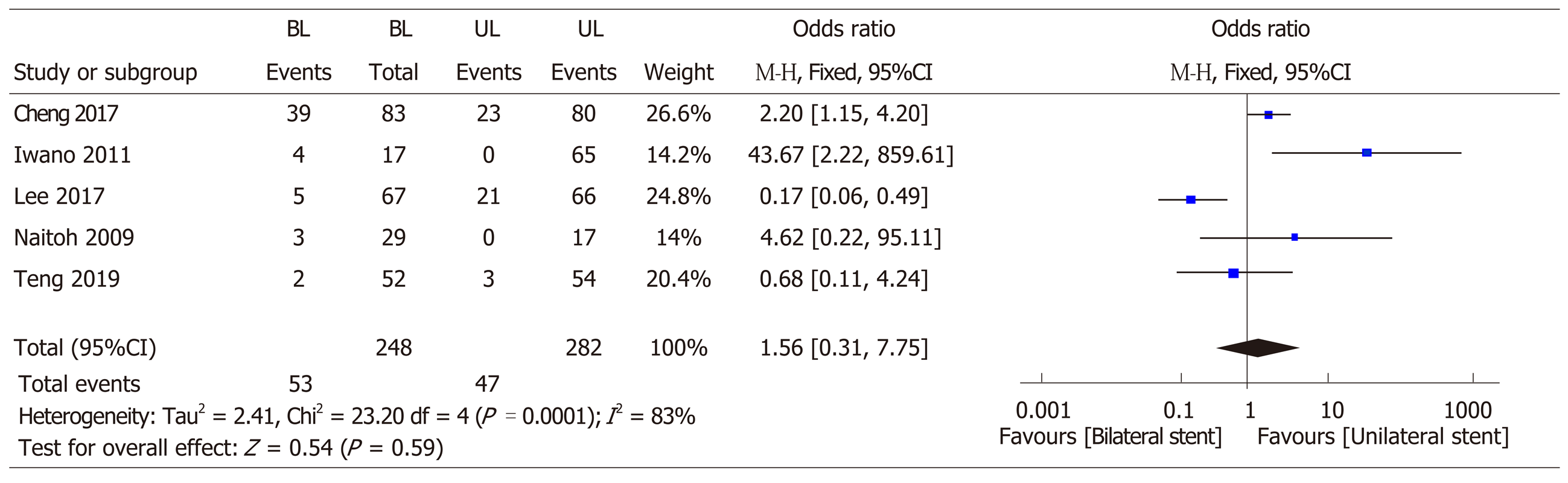
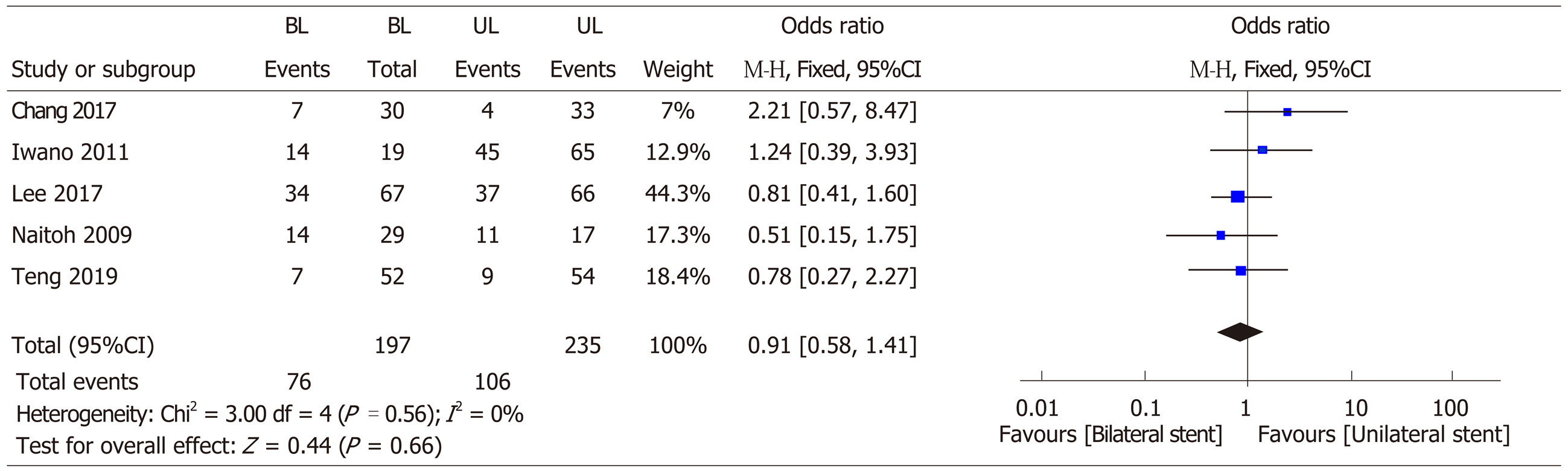
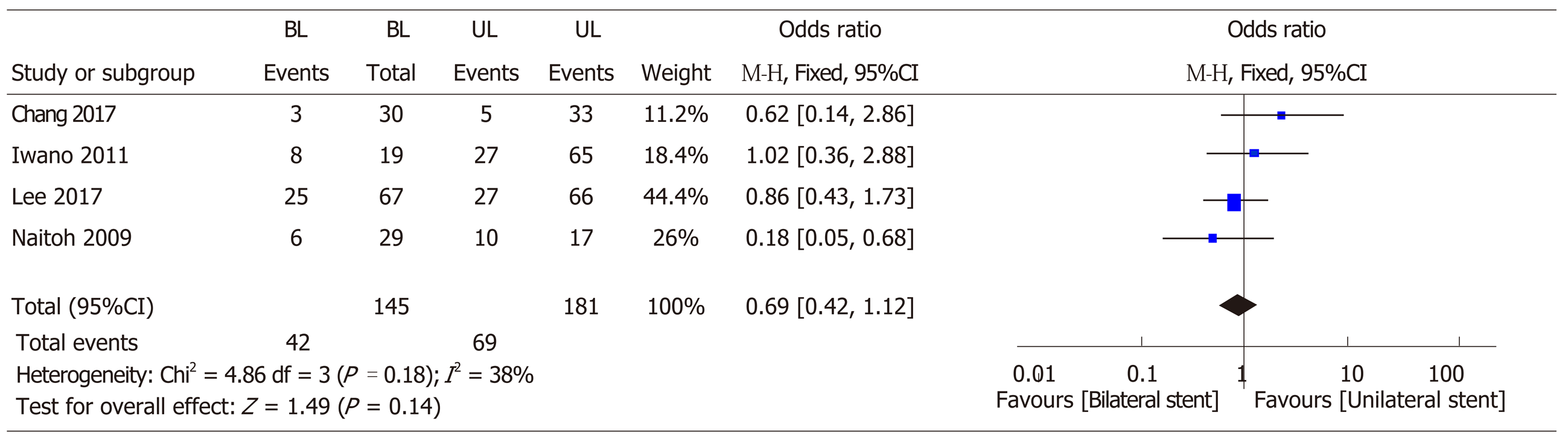
Secondary end-points: (1) Technical success: A total of 8 studies involving 745 patients was included in this analysis[7,10,14,15,17-20]. There was no significant difference in the technical success rate with bilateral stenting as compared to unilateral stenting (OR = 0.7, 95%CI: 0.42-1.17, P = 0.17) (Figure 4). There was mild heterogeneity; (2) Early complications: A total of 5 studies involving 530 patients were included in this analysis[7,10,18-20]. There was no difference between early complications (OR = 1.56, 95%CI: 0.31-7.75, P = 0.0001) (Figure 5); (3) Late complications: A total of 5 studies involving 430 patients were included in this analysis[7,10,15,18,20]. There was no difference in late complication rate (OR = 0.91, 95%CI: 0.58-1.41, P = 0.56) (Figure 6); and (4) Stent malfunction: A total of 4 studies involving 324 patients was included in this analysis[7,10,15,18]. There was no difference in stent malfunction rates (OR = 0.69, 95%CI: 0.42-1.12, P = 0.14) (Figure 7).
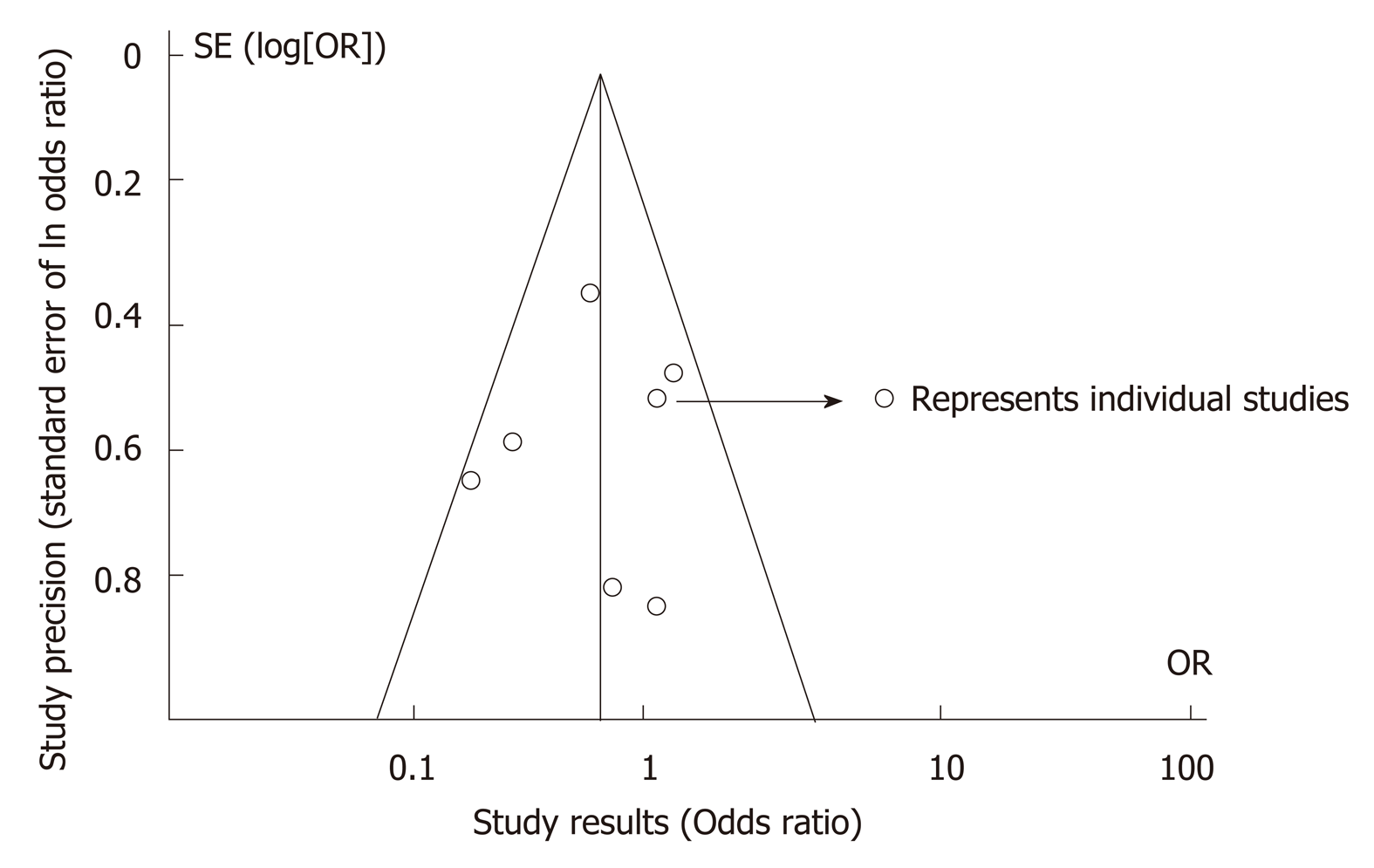
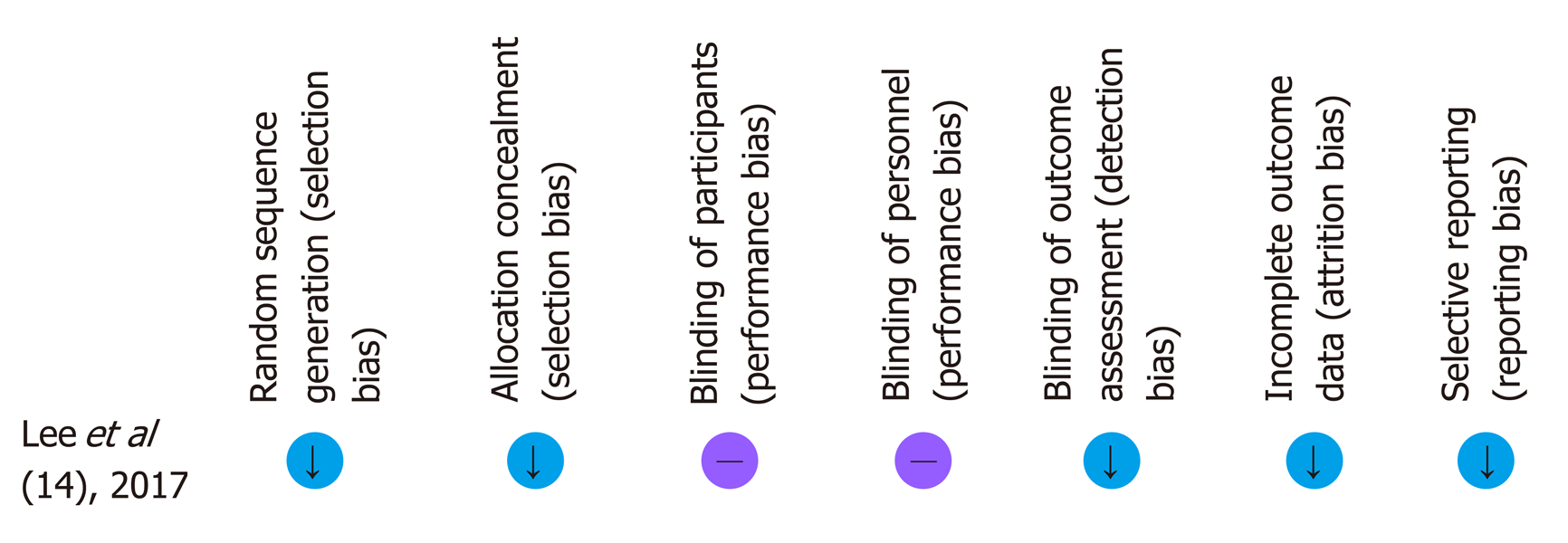
The Newcastle Ottawa Scale score has been provided for all retrospective studies in Supplemental Table 1. The Cochrane collaboration tool assessment of bias for the RCT has been provided in Figure 8. Funnel plots to estimate bias revealed no asymmetry (Figure 3).
Endoscopic biliary drainage is the intervention of choice in patients with UMHO. Besides providing symptomatic relief to patients with pruritis it also has therapeutic implications with a reduction in total bilirubin which permits the use of subsequent chemotherapy, radiotherapy or photodynamic therapy. This may be important in prolonging the life of patients with unresectable malignant biliary strictures. Over the past decade, multiple studies have found using metallic stents over plastic stents as more cost-effective in hilar cholangiocarcinoma[4,14,21,22]. However, the data comparing bilateral vs unilateral stenting in UMHO is sparse. There has been conflicting data in regards to the outcomes of placement of bilateral vs unilateral SEMS stents[7,8,10,18,23,24]. Therefore, we designed this meta-analysis to review the data, thus-far available, comparing bilateral vs unilateral SEMS placement for UMHO. Our meta-analysis shows that bilateral stenting as compared to unilateral stenting is associated with a lower re-intervention rate, but has a comparable technical success rate, early and late complication rates.
Bilateral stenting was associated with a statistically significant 41% reduction in re-intervention rate. There has been marked variability in results among published literature. A prospective trial by Mukai et al[14] demonstrated 50% re-intervention rate in bilateral SEMS group compared to 29% in unilateral SEMS group. However, the study groups were not treated similarly in their study, as patients who received bilateral stent received sphincterotomy while patients receiving unilateral stent did not. In the prospective RCT by Lee et al[10], the authors showed a statistically significant lower re-intervention rate at 3 mo for bilateral SEMS group vs unilateral SEMS group (10.9% vs 33.3%). The ability to reduce the number of interventions is of paramount importance in patients with non-operable malignant hilar strictures and an average life expectancy < 12 mo, thus avoiding multiple hospitalizations, which in-return could mean an overall more cost-effective approach and also will have an impact on improving the quality of life for patients[18,25]. Further, restoration of bile flow with bilateral stenting is physiologically more superior to unilateral stenting. Approximately 25%-30% liver needs to be drained in order to satisfactorily reduce jaundice[8,26]. Though unilateral stent should be able to drain at-least 25% of the liver, clinical evidence suggests that up to 30% cases of hilar cholangiocarcinoma are associated with hepatic lobar atrophy[27], and thus in such a situation, unilateral stenting may not provide an appropriate therapeutic response and may increase primary re-intervention rates. Furthermore, a study by Vienne et al[28] suggested that draining more than 50% of the liver volume is an important predictor of the effectiveness of biliary drainage especially in malignant hilar strictures.
The conflicting data is further complicated by the technical difficulties associated with the placement of bilateral stents. Thus, multiple newer stent delivery systems have been developed to overcome this technical challenge. In our study, there was no significant difference in the technical success between bilateral biliary stenting and unilateral biliary stenting. A meta-analysis by Hong W et al[24] concluded higher success with unilateral stenting. However, their meta-analysis included studies involving plastic biliary stents which may have affected the results. Our results are similar to results by Naitoh et al[18] and Iwano et al[7] who had similar technical success for bilateral and unilateral stents. Bilateral stents could be placed by either stent-in-stent technique (SIS) or side-by-side technique (SBS). Naitoh et al use stent in stent technique and Iwano et al used SIS technique respectively in their patients Although, this meta-analysis did not specifically compare the two techniques of bilateral stenting, a meta-analysis by Naitoh et al[18] showed longer stent patency time with SBS group when compared to SIS group. Provider expertise could also account for the variability in the technical success rate among the studies. Thus, based on our results, we believe that bilateral stenting may be preferable for providers who are technically adept at placing both bilateral and unilateral stent.
Stent malfunction could be driving our primary outcome of stent re-intervention rates. The rate of reintervention was influenced by stent malfunction, however, not all studies defined the cause of stent malfunction clearly (Supplemental Table 2) and hence we only included stent malfunction as a secondary outcome. There was a trend towards decreased stent malfunction with bilateral drainage as compared to unilateral drainage though this was not statistically different. Earlier studies seemed to suggest that bilateral stents could lead to increased stent-related early complications. SBS was associated with increased cholangitis rates and portal vein occlusion because of excessive expansion of the bile duct by parallel stents[18]. SIS deployment could lead to increased sludge formation at the site of stent overlap as a result of a reduction in bile inflow and increase the incidence of tumor ingrowth if the stent mesh is expanded in the area of overlap[17]. In contrast, most recent RCT by Lee et al[10] has shown no difference in rates of cholangitis and liver abscess after bilateral stent placement. Similarly, in our meta-analysis, there was no difference with stent-related early or late complication rates between the two groups.
There are several limitations to this meta-analysis. The main limitation is that only two studies included in our meta-analysis are RCT’s. Most studies are retrospective studies which could have led to selection bias. Nevertheless, the retrospective studies are reasonable quality cohort studies, as determined by the Modified Newcastle Ottawa quality assessment scale of cohort studies. Another limitation is the presence of significant heterogeneity in some of the analysis. This is likely due to the significant clinical heterogeneity among the studies the differences in the study population, the location of malignant strictures, technical expertise of the providers, and the difference in the duration. However, importantly, there was only mild heterogeneity in the analysis of our primary end-point analysis of re-intervention rate and in the analysis for technical success. For analysis with significant heterogeneity, we used a random effects model to partly account for the clinical heterogeneity. This highlights the need for further research on this topic and the importance of our meta-analysis based on available data.
In conclusion, bilateral biliary stenting for UMHO may decrease the re-intervention rate in patients with malignant hilar strictures, without increasing early or late complication rate. To the best of our knowledge, this is the first meta-analysis so far comparing the outcomes of SEMS bilateral vs unilateral stenting. Further RCT’s are needed to confirm our findings.
Inoperable malignant biliary strictures comes with a very high mortality rate. Self expanding metal stents (SEMS) not only offers symptomatic relief but also gives an opportunity for these patients to receive chemotherapy once bilirubin starts to trend down. Unilateral biliary SEMS have long been thought to be adequate and probably better than bilateral SEMS as it comes with lower complication rates. However, with newer endoscopic techniques and most recent prospective trials, the efficacy of bilateral SEMS has shown to be better than unilateral SEMS and with similar complication rates. This meta-analysis highlights the growing body of evidence in support of bilateral stenting versus unilateral stenting.
Over the past few years, newer randomized control trials (RCTs have been published showing the overall advantage of bilateral biliary stenting over unilateral stenting in a subset of patients with inoperable hilar malignant strictures. No meta-analysis was done on this topic with newer study data points.
We aimed to conduct a meta-analysis to compare the role of bilateral stenting vs unilateral stenting in inoperable malignant hilar strictures.
A detailed literature search was conducted to find all the relevant articles. Two reviewers independently analyzed all the selected studies. All discrepancies were discussed independently with the third reviewer and consensus was achieved. We used Pooled odds ratio (OR) and 95% confidence intervals (CIs) were calculated for each outcome.
A total of 782 patients form nine studies were included for analysis. Bilateral stenting had significantly lower re-intervention rate compared with unilateral drainage (OR = 0.59, 95%CI: 0.40-0.87, P = 0.009). There was no difference in the technical success rate (OR = 0.7, CI: 0.42-1.17, P = 0.17), early complication rate (OR = 1.56, CI: 0.31-7.75, P = 0.59), late complication rate (OR = 0.91, CI: 0.58-1.41, P = 0.56) and stent malfunction (OR = 0.69, CI: 0.42-1.12, P = 0.14) between bilateral and unilateral stenting for malignant hilar biliary strictures.
Older studies that have shown the ease of putting unilateral stenting with fewer complications over bilateral stenting in inoperable malignant hilar strictures. However, with new RCTs showing the higher success of bilateral biliary stenting with lower re-intervention rates, bilateral stenting could offer an overall advantage over unilateral stenting. Our study highlights the overall advantage of bilateral stenting over unilateral stenting.
Biliary stenting is very important modality in the overall management of inoperable malignant hilar strictures. Bilateral stenting offers an advantage over unilateral stenting, however more RCT is required to further support this conclusion.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Neri V, Sugimoto M S-Editor: Ma RY L-Editor: A E-Editor: Zhang YL
| 1. | Bismuth H, Castaing D, Traynor O. Resection or palliation: priority of surgery in the treatment of hilar cancer. World J Surg. 1988;12:39-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 237] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 2. | Black K, Hanna SS, Langer B, Jirsch DW, Rider WD. Management of carcinoma of the extrahepatic bile ducts. Can J Surg. 1978;21:542-545. [PubMed] |
| 3. | Rerknimitr R, Angsuwatcharakon P, Ratanachu-ek T, Khor CJ, Ponnudurai R, Moon JH, Seo DW, Pantongrag-Brown L, Sangchan A, Pisespongsa P, Akaraviputh T, Reddy ND, Maydeo A, Itoi T, Pausawasdi N, Punamiya S, Attasaranya S, Devereaux B, Ramchandani M, Goh KL; Asia-Pacific Working Group on Hepatobiliary Cancers. Asia-Pacific consensus recommendations for endoscopic and interventional management of hilar cholangiocarcinoma. J Gastroenterol Hepatol. 2013;28:593-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 186] [Article Influence: 15.5] [Reference Citation Analysis (1)] |
| 4. | Dumonceau JM, Tringali A, Papanikolaou IS, Blero D, Mangiavillano B, Schmidt A, Vanbiervliet G, Costamagna G, Devière J, García-Cano J, Gyökeres T, Hassan C, Prat F, Siersema PD, van Hooft JE. Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline - Updated October 2017. Endoscopy. 2018;50:910-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 529] [Cited by in RCA: 479] [Article Influence: 68.4] [Reference Citation Analysis (0)] |
| 5. | Dumonceau JM, Tringali A, Blero D, Devière J, Laugiers R, Heresbach D, Costamagna G; European Society of Gastrointestinal Endoscopy. Biliary stenting: indications, choice of stents and results: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy. 2012;44:277-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 290] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 6. | Polydorou AA, Chisholm EM, Romanos AA, Dowsett JF, Cotton PB, Hatfield AR, Russell RC. A comparison of right vs left hepatic duct endoprosthesis insertion in malignant hilar biliary obstruction. Endoscopy. 1989;21:266-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 71] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Iwano H, Ryozawa S, Ishigaki N, Taba K, Senyo M, Yoshida K, Sakaida I. Unilateral vs bilateral drainage using self-expandable metallic stent for unresectable hilar biliary obstruction. Dig Endosc. 2011;23:43-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 73] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 8. | De Palma GD, Galloro G, Siciliano S, Iovino P, Catanzano C. Unilateral vs bilateral endoscopic hepatic duct drainage in patients with malignant hilar biliary obstruction: results of a prospective, randomized, and controlled study. Gastrointest Endosc. 2001;53:547-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 290] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 9. | Kogure H, Isayama H, Kawakubo K, Sasaki T, Yamamoto N, Hirano K, Sasahira N, Tsujino T, Tada M, Koike K. Endoscopic bilateral metallic stenting for malignant hilar obstruction using newly designed stents. Journal of Hepato-Biliary-Pancreatic Sciences. 2011;18:653-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Lee TH, Kim TH, Moon JH, Lee SH, Choi HJ, Hwangbo Y, Hyun JJ, Choi JH, Jeong S, Kim JH, Park DH, Han JH, Park SH. Bilateral vs unilateral placement of metal stents for inoperable high-grade malignant hilar biliary strictures: a multicenter, prospective, randomized study (with video). Gastrointest Endosc. 2017;86:817-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 146] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 11. | Kogure H, Isayama H, Nakai Y, Tsujino T, Matsubara S, Yashima Y, Ito Y, Hamada T, Takahara N, Miyabayashi K, Mizuno S, Mohri D, Kawakubo K, Sasaki T, Yamamoto N, Hirano K, Sasahira N, Tada M, Koike K. High single-session success rate of endoscopic bilateral stent-in-stent placement with modified large cell Niti-S stents for malignant hilar biliary obstruction. Dig Endos. 2014;26:93-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savović J, Schulz KF, Weeks L, Sterne JAC. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18487] [Cited by in RCA: 24774] [Article Influence: 1769.6] [Reference Citation Analysis (3)] |
| 13. | Stang A; Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8858] [Cited by in RCA: 12615] [Article Influence: 841.0] [Reference Citation Analysis (0)] |
| 14. | Mukai T, Yasuda I, Nakashima M, Doi S, Iwashita T, Iwata K, Kato T, Tomita E, Moriwaki H. Metallic stents are more efficacious than plastic stents in unresectable malignant hilar biliary strictures: a randomized controlled trial. J Hepatobiliary Pancreat Sci. 2013;20:214-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 165] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 15. | Chang G, Xia FF, Li HF, Niu S, Xu YS. Unilateral vs bilateral stent insertion for malignant hilar biliary obstruction. Abdom Radiol (NY). 2017;42:2745-2751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Hatamaru K, Yamashita Y, Uenoyama Y. Tu1448 The Study of Endoscopic Treatment for Unresectable Malignant Hilar Biliary Obstruction. Gastrointest Endosc. 2017;85:AB626. [DOI] [Full Text] |
| 17. | Liberato MJ, Canena JM. Endoscopic stenting for hilar cholangiocarcinoma: efficacy of unilateral and bilateral placement of plastic and metal stents in a retrospective review of 480 patients. BMC Gastroenterol. 2012;12:103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 112] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 18. | Naitoh I, Ohara H, Nakazawa T, Ando T, Hayashi K, Okumura F, Okayama Y, Sano H, Kitajima Y, Hirai M, Ban T, Miyabe K, Ueno K, Yamashita H, Joh T. Unilateral vs bilateral endoscopic metal stenting for malignant hilar biliary obstruction. J Gastroenterol Hepatol. 2009;24:552-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 155] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 19. | Cheng S, Jianfeng y, Zhang X. Tu1408 A Comparison of Unilateral Vs Bilateral Endoscopic Biliary Stenting for Bismuth-Corlette II-IV Malignant Hilar Strictures. Gastrointest Endosc. 2017;85:AB613. [DOI] [Full Text] |
| 20. | Teng F, Xian YT, Lin J, Li Y, Wu AL. Comparison of Unilateral With Bilateral Metal Stenting for Malignant Hilar Biliary Obstruction. Surg Laparosc Endosc Percutan Tech. 2019;29:43-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Perdue DG, Freeman ML, DiSario JA, Nelson DB, Fennerty MB, Lee JG, Overby CS, Ryan ME, Bochna GS, Snady HW, Moore JP; ERCP Outcome Study ERCOST Group. Plastic vs self-expanding metallic stents for malignant hilar biliary obstruction: a prospective multicenter observational cohort study. J Clin Gastroenterol. 2008;42:1040-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 144] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 22. | Sangchan A, Kongkasame W, Pugkhem A, Jenwitheesuk K, Mairiang P. Efficacy of metal and plastic stents in unresectable complex hilar cholangiocarcinoma: a randomized controlled trial. Gastrointest Endosc. 2012;76:93-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 183] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 23. | De Palma GD, Pezzullo A, Rega M, Persico M, Patrone F, Mastantuono L, Persico G. Unilateral placement of metallic stents for malignant hilar obstruction: a prospective study. Gastrointest Endosc. 2003;58:50-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 130] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 24. | Hong W, Sun X, Zhu Q. Endoscopic stenting for malignant hilar biliary obstruction: should it be metal or plastic and unilateral or bilateral? Eur J Gastroenterol Hepatol. 2013;25:1105-1112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 25. | Abraham NS, Barkun JS, Barkun AN. Palliation of malignant biliary obstruction: a prospective trial examining impact on quality of life. Gastrointest Endosc. 2002;56:835-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 26. | Larghi A, Tringali A, Lecca PG, Giordano M, Costamagna G. Management of hilar biliary strictures. Am J Gastroenterol. 2008;103:458-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 81] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 27. | Gwon DI, Ko GY, Sung KB, Yoon HK, Shin JH, Hyoung Kim J, Kim J, Oh JY. Percutaneous biliary metallic stent placement in patients with unilobar portal vein occlusion caused by advanced hilar malignancy: outcome of unilateral vs bilateral stenting. AJR Am J Roentgenol. 2011;197:795-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 28. | Vienne A, Hobeika E, Gouya H, Lapidus N, Fritsch J, Choury AD, Chryssostalis A, Gaudric M, Pelletier G, Buffet C, Chaussade S, Prat F. Prediction of drainage effectiveness during endoscopic stenting of malignant hilar strictures: the role of liver volume assessment. Gastrointest Endosc. 2010;72:728-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 219] [Article Influence: 14.6] [Reference Citation Analysis (0)] |