Published online Sep 7, 2019. doi: 10.3748/wjg.v25.i33.4985
Peer-review started: June 17, 2019
First decision: July 21, 2019
Revised: July 30, 2019
Accepted: August 19, 2019
Article in press: August 19, 2019
Published online: September 7, 2019
Processing time: 82 Days and 5.5 Hours
Hepatitis B virus (HBV) DNA polymerase mutations usually occur to long term use of nucleos(t)ide analogues (NAs), but they can occur spontaneously in treatment-naïve chronic hepatitis B (CHB) patients. The naturally occurring HBV DNA polymerase mutations might complicate antiviral therapy with NAs, leading to the generation of drug-resistant viral mutants and disease progression. The most common substitutions are known to be YMDD-motif mutations, but their prevalence and the influence on antiviral therapy is unclear.
To investigate prevalence of the naturally occurring rtM204I mutations in treatment-naïve CHB genotype C2 patients and their influence on antiviral therapy.
A total of 410 treatment-naïve CHB patients infected with HBV genotype C2 strains were enrolled in this retrospective study. Among the 410 patients, 232 were treated with NAs for at least 12 mo. Significant fibrosis was defined as fibrosis-4 index > 3.25 or aspartate aminotransferase to platelet ratio index > 1.5. Complete viral response (CVR) during NAs was defined as undetectable serum HBV DNA (< 24 IU/mL). The rtM204I variants were analyzed by a newly developed locked nucleotide probe (LNA probe) based real-time PCR (LNA-RT-PCR) method.
The LNA-RT-PCR could discriminate rtM204I mutant-type (17 patients, 4.2%) from rtM204 wild-type (386 patients, 95.8%) in 403 of 410 patients (98.3% sensitivity). Multivariate analysis showed that naturally occurring rtM204I variants were more frequently detected in patients with significant fibrosis [odd-ratio (OR) 3.397, 95% confidence-interval (CI) 1.119-10.319, P = 0.031]. Of 232 patients receiving NAs, multivariate analysis revealed that achievement of CVR was reversely associated with naturally occurring rtM204I variants prior to NAs treatment (OR 0.014, 95%CI 0.002-0.096, P < 0.001). Almost patients receiving tenofovir achieved CVR at 12 mo of tenofovir, irrespective of pre-existence of naturally occurring rtM204I mutations (CVR rates: patients with rtM204I, 100%; patients without rtM204I, 96.6%), whereas, pre-existence of naturally-occurring rtM204I-mutations prior to NAs significantly affects CVR rates in patients receiving entecavir (at 12 mo: Patients with rtM204I, 16.7%; patients without rtM204I, 95.6%, P < 0.001).
The newly developed LNA-RT-PCR method could detect naturally occurring rtM204I mutations with high-sensitivity. Theses mutations were more frequent in patients with liver fibrosis. Tenofovir is a more suitable treatment than entecavir for CHB patients carrying the naturally occurring rtM204I mutations.
Core tip: Hepatitis B virus (HBV) DNA polymerase mutations have been known to be prevalent in treatment-naïve chronic hepatitis B (CHB) patients infected with HBV genotype C2 strains. The newly developed locked nucleotide probe based real-time PCR method could discriminate the naturally-occurring rtM204I mutations from wild type with high sensitivity in treatment-naïve patients. Multivariate analyses showed that the naturally-occurring rtM204I variants were more frequently pre-existed in patients with liver fibrosis, and the pre-existence of the naturally-occurring rtM204I variants were significantly associated with incomplete viral response to nucleos(t)ide analogues. Tenofovir is a more suitable nucleos(t)ide analogues than entecavir for treatment-naïve CHB patients carrying the naturally occurring rtM204I mutations.
- Citation: Choe WH, Kim K, Lee SY, Choi YM, Kwon SY, Kim JH, Kim BJ. Tenofovir is a more suitable treatment than entecavir for chronic hepatitis B patients carrying naturally occurring rtM204I mutations. World J Gastroenterol 2019; 25(33): 4985-4998
- URL: https://www.wjgnet.com/1007-9327/full/v25/i33/4985.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i33.4985
Hepatitis B virus (HBV) infection is a global health issue because of its worldwide distribution and is a potential leading cause of adverse outcomes, including liver cirrhosis (LC), hepatic decompensation, and hepatocellular carcinoma (HCC)[1,2]. Nucleos(t)ide analogues (NAs) are recommended by international guidelines for suppressing HBV replication and have been shown to decrease the rate of complications[3,4]. While NAs are well tolerated and effective in suppressing viral replication, long-term treatment with oral antiviral drugs can lead to the emergence of drug resistance mutations[5]. For instance, rtM204I is a classic mutation reducing susceptibility to mono-therapy by NAs with low genetic barriers, such as lamivudine (LAM), telbivudine (L-dT) and clevudine (CLV)[6].
HBV is an enveloped, partially double stranded DNA virus containing a genome that is approximately 3.2 kb in length and contains 4 overlapping open reading frames encoding the polymerase, core, surface antigen, and X protein[7]. The polymerase gene includes four domains, the terminal protein, spacer, ribonuclease H, and reverse transcriptase (RT) regions. The RT region replicates the HBV genome through its DNA polymerase activity using RNA intermediates as a template. Since the RT lacks proofreading activity during viral replication, the error rate of HBV genome synthesis has been found to be 10-7 per nucleotide, which is 10-fold higher than those of other DNA viruses[8]. The high rate of mutations in the HBV genome complicates antiviral therapy with NAs, leading to the generation of drug-resistant viral strains and disease progression[9].
Previous studies have reported the existence of HBV DNA polymerase mutations in chronic hepatitis B (CHB) individuals prior to NA treatment; however, the prevalence varies from 0 to 30%[10-13]. This wide range might may be due to several factors including different study designs, regions, ethnicities, mutation detection methods, sample sizes, etc.[9,14,15]. Because of the high replication rate of HBV, viral mutations, including mixed wild-type and mutant populations in a single host, are commonly seen, but a low sensitivity assay could not enable the discrimination between wild and mutant types.
The purpose of this study was to determine the prevalence and clinical characteristics of naturally occurring rtM204I mutations in treatment-naïve patients infected with HBV genotype C2 strains by using a newly developed locked nucleotide probe (LNA probe) based real time PCR (LNA-RT-PCR) method, which can detect subspecies at 5% of the circulating HBV population.
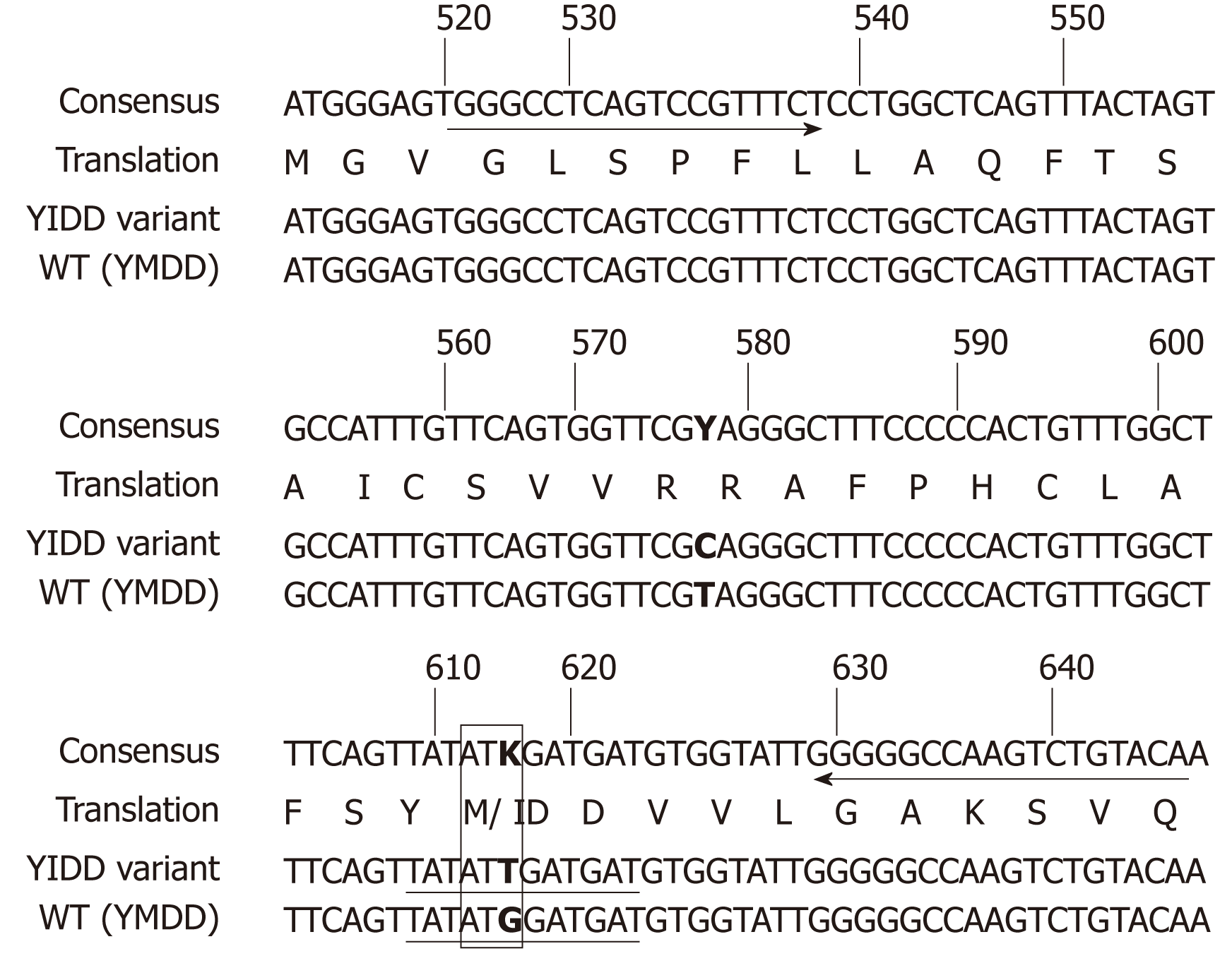
We designed two different LNA probes for the specific simultaneous detection in a single reaction of wild type (WT) and rtM204I variant of HBV. We used LC PDS (version 2.0) software for the probe design and referred to the design guidelines of LNA manufacturer (Integrated DNA technologies). We attached two different reporter dyes, FAM to probe for rtM204I variant, and Hex to probe for WT, respectively, to differentially identify rtM204I variant and WT HBV DNA. The primer and probe specificity for detection of rtM204I variant was further analyzed using Primer-Blast at NCBI (http://www.ncbi.nlm.nih.gov/tools/primer-blast/) and the Oligo software version 6.5. There were no PCR products formed by Primer-blast with the designed primer sequences in Homo sapiens, bacteria, and viruses other than HBV. Probe sequences were exclusively found in the amplicon sequence analyzed by the Oligo software with an HBV DNA sequence. The sequences of primers and LNA probes are shown in Figure 1 and Table 1. The LNA probes were purchased from Integrated DNA technologies, and primers from Macrogen.
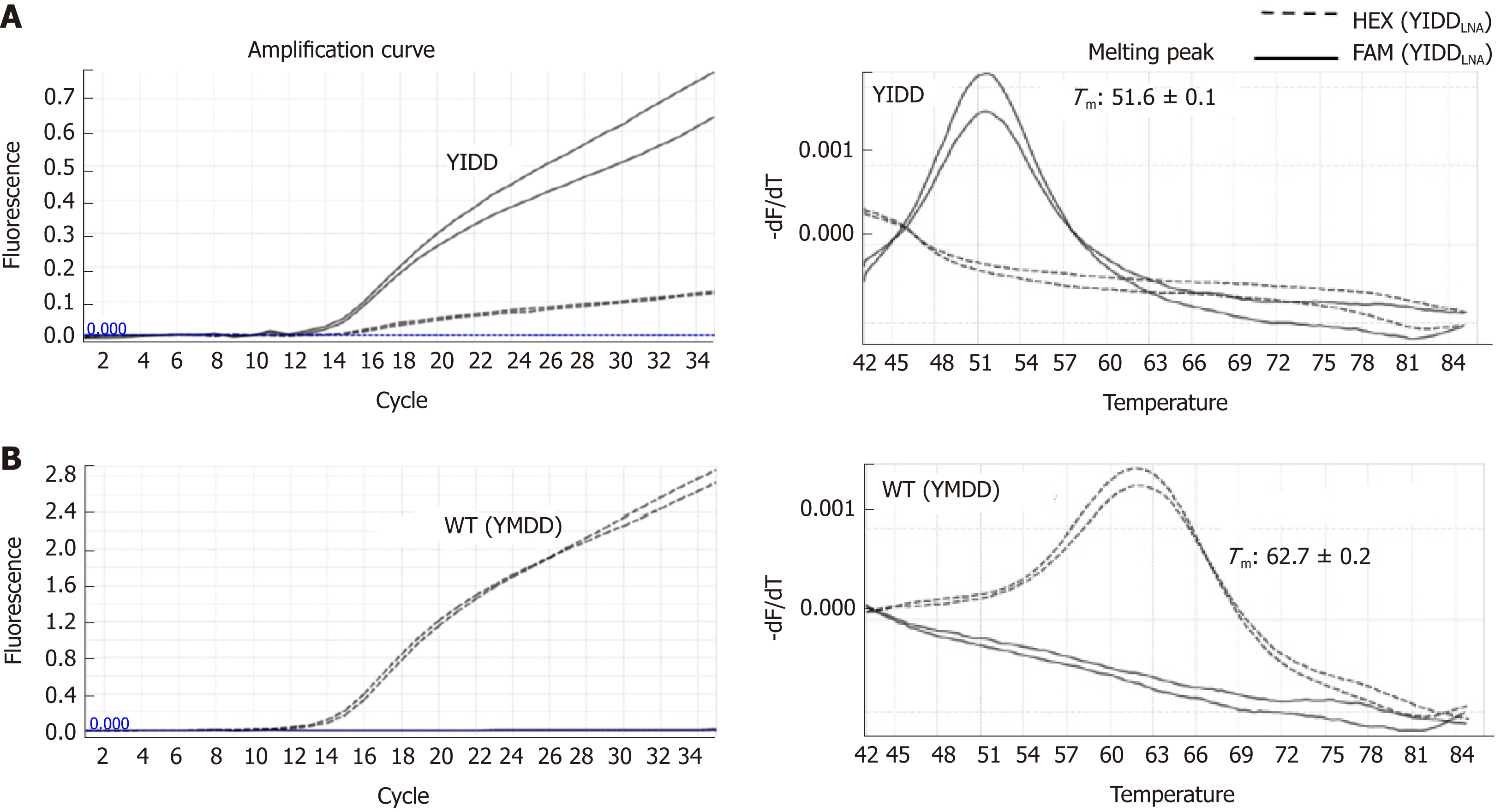
A LightCycler Version 96 system (Roche) was used for LNA probe-based real-time PCR, and two channels were used for the experiment. Optimal reaction mixture was established for the sensitive and specific detection of target sequences. A 10-μL reaction mixture was prepared for each sample as follows: 1 μl PCR reaction buffer for Taq (Bioneer E-3150 buffer), 4.25 mM MgCl2, 0.425 mM deoxynucleoside triphosphate mixture (Takara), 0.3 μM forward primer, 1 μM reverse primer, 0.25 μM LNA FAM probe (rtM204I variant), 0.25 μM LNA Hex probe (rtM204I variant), 0.6 U Hot Start Taq (Bioneer E-3150), 1 mg/mL bovine serum albumin (Ambion, Lifetechnologies), 2 μL template DNA, and PCR-grade water (Roche). The cycling conditions were 300 s at 95 °C and 15 cycles of 10 s at 95 °C, 15 s at 58 °C, and 40 s at 75 °C, followed by 32 cycles of 10 s at 95 °C, 15 s at 47 °C (single acquisition of fluorescence signals), 15 s at 62 °C, and 40 s at 75 °C at a ramping speed of 1.1 °C/s. Melting curve analysis was subsequently continued without any pause by use of cycling for 10 s at 95 °C and 60 s at 43 °C, and the temperature was then increased from 43 °C to 85 °C at a temperature transition rate of 0.17 °C/s, during which the fluorescence signal was continuously acquired by three readings per degrees Celsius. All the following LNA real-time PCR experiments were done in quadruplicate with positive control DNAs and mixtures of WT and rtM204I at a variety of ratios and concentrations as aforementioned. The experiments were all repeated to examine inter-assay reliability.
DNAs of a total of 410 human sera were tested for the identification of WT and rtM204I variant of HBV RT gene by LNA real-time PCR in duplicate. Tm, melting peak height, and quantification cycle (Cq) produced by WT- and rtM204I -targeting LNA probes with a sample DNA were measured. Identification of WT and rtM204I variant was determined by comparing their Tm s obtained from their specific channel (FAM for rtM204I, HEX for WT) with their diagnostic Tm ranges obtained from standard assays. Positive identification of WT and rtM204I variant was recorded only when distinct melting peak formation with their diagnostic Tm is recognized.
Throughout the real-time PCR assay, two rtM204I positive controls with high copies (2400000) and low copies (2400), two rtM204I positive controls with high copies (2400000) and low copies (2400), and two non-template controls were included in each run to monitor validity of Cqs, Tm s, and cross-contamination for inter-assays. Comparison of LNA real-time PCR and direct sequencing for identification of rtM204I variant and WT DNA.
Data were collected retrospectively from a total of 410 treatment-naïve HBV patients who were followed in the Digestive Disease Center of Konkuk University Hospital, Korea, between March 2011 and February 2014. All of the patients were diagnosed with CHB and confirmed to have not taken any NAs or interferon. The inclusion criteria for the CBH patients included hepatitis B surface antigen (HBsAg) positive for more than 6 months and HBV-DNA viral loads were detectable, while the exclusion criteria included hepatitis C virus or human immunodeficiency virus coinfection, autoimmune liver disease, and alcohol or drug abuse. Prior to antiviral treatments, sera were collected from patients for analyses of the pre-existence of antiviral variants prior to NAs. This study was approved by the Institutional Review Board of Konkuk University Hospital.
In all cases, demographic, clinical, biochemical and virologic data were collected. A diagnosis of LC was made clinically when a patient had at least two of the following three criteria: cirrhotic configuration of the liver (nodular liver surface or caudate lobe hypertrophy) and/or splenomegaly confirmed on imaging studies, thrombocytopenia (< 100000 platelets/mm3), or the presence of varices detected by esophago-gastroduodenoscopy. Liver fibrosis was assessed using noninvasive biomarkers to calculate two composite scores The Fibrosis-4 index (FIB-4) score was calculated using age, aspartate aminotransferase (AST), alanine aminotransferase (ALT), and platelet count in the following formula: FIB-4 = [age (years) × AST (IU/L)] / [platelets (109/L) × ALT (IU/L)]. The AST to platelet ratio index (APRI) score was calculated using AST and platelet counts in the following formula: APRI = [AST level (IU/L) / AST upper limit of normal (IU/L) / platelet count (109/L)] × 100. Significant fibrosis of liver was defined as FIB-4 > 3.25 or APRI > 1.5[16]. The diagnosis of HCC was made based on histological evidence or typical radiological findings (the presence of arterial phase enhancement and portal venous phase wash-out of a nodule 1 cm or more in size)[17].
A complete viral response (CVR) was regarded as HBV-DNA levels being lower than detectable levels (24 IU/mL) at 12 mo of antiviral therapy, and incomplete (suboptimal) responders were defined as individuals having detectable HBV-DNA levels after at least 12 mo of treatment[18].
Data were mainly expressed as the mean and standard deviation (SD). Fisher's exact test was used to compare categorical variables. One-way ANOVA and Duncan's multiple comparison tests were used to compare continuous variables among the groups, and Student's t-test was for the analysis between the groups. Logistic regression analyses were performed to identify the independent factors for the presence of naturally occurring rtM204I mutations, or antiviral responsiveness. The Statistical Package for Social Science (SPSS Inc., Chicago, IL, United States), version 15.0 was used for all analyses.
Identification of WT and rtM204I variants was performed by LNA real-time PCR melting curve analysis by the observation of melting peak formation and specific Tm measurements in the specified channels (Figure 2, Table 2). LNA real-time PCR with samples of rtM204I positive control DNAs (n = 48) in amounts ranging from 24 to 2400000 copies resulted in a 100% positive detection rate and 100% specificity showing a distinct melting peak formation at the FAM channel in all of the rtM204I control DNA samples with Tms ranging from 51.3 to 52.2 °C (mean, 51.7 ± 0.2 °C) but no significant melting peak formation at the HEX channel (WT detection channel). LNA real-time PCR with samples of WT control DNAs (n = 48) in amounts ranging from 24 to 2400000 copies resulted in a 95.8% positive detection rate and 100% specificity showing a distinct melting peak formation at the HEX channel in all of the WT control DNA samples with Tms ranging from 61.9 to 63.3 °C (mean, 62.6 ± 0.4 °C) but no significant melting peak formation at the FAM channel (rtM204I detection channel). Two WT control DNA samples that had the lowest copy numbers were not detected. This suggests high sensitivity and specificity of our newly developed LNA RT-PCR assay.
| Sample (copies, number of samples n) | Measured Tm (°C) at channel | |||||
| FAM | HEX | |||||
| Min | Max | Mean ± SD (number of positives) | Min | Max | Mean ± SD (number of positives) | |
| YIDD positive control DNA (24-2400000, n = 48) | 51.3 | 52.2 | 51.7 ± 0.2 (48, 100%) | (-) | (-) | (-) |
| WT positive control DNA (24-2400000, n = 48) | (-) | (-) | (-) | 61.9 | 63.3 | 62.6 ± 0.4 (46, 95.8%) |
| YIDD and WT standard mixtures (24-2400000, n = 280) | 50.1 | 52.6 | 51.5 ± 0.3 (280, 100%) | 61.9 | 64.0 | 63.0 ± 0.4 (280, 100%) |
| YIDD and WT standard mixtures (24, n = 56) | 49.9 | 51.9 | 51.2 ± 0.5 (45, 80.3%) | 60.9 | 63.8 | 63.0 ± 0.5 (44, 78.6%) |
| YIDD of clinical samples in duplicate (82-180000, n = 17) | 49.6 | 51.9 | 51.3 ± 0.5 | (-) | (-) | (-) |
| YMDD of clinical samples in duplicate (65-13000000, n = 397) | (-) | (-) | (-) | 61.1 | 64.0 | 62.8 ± 0.3 |
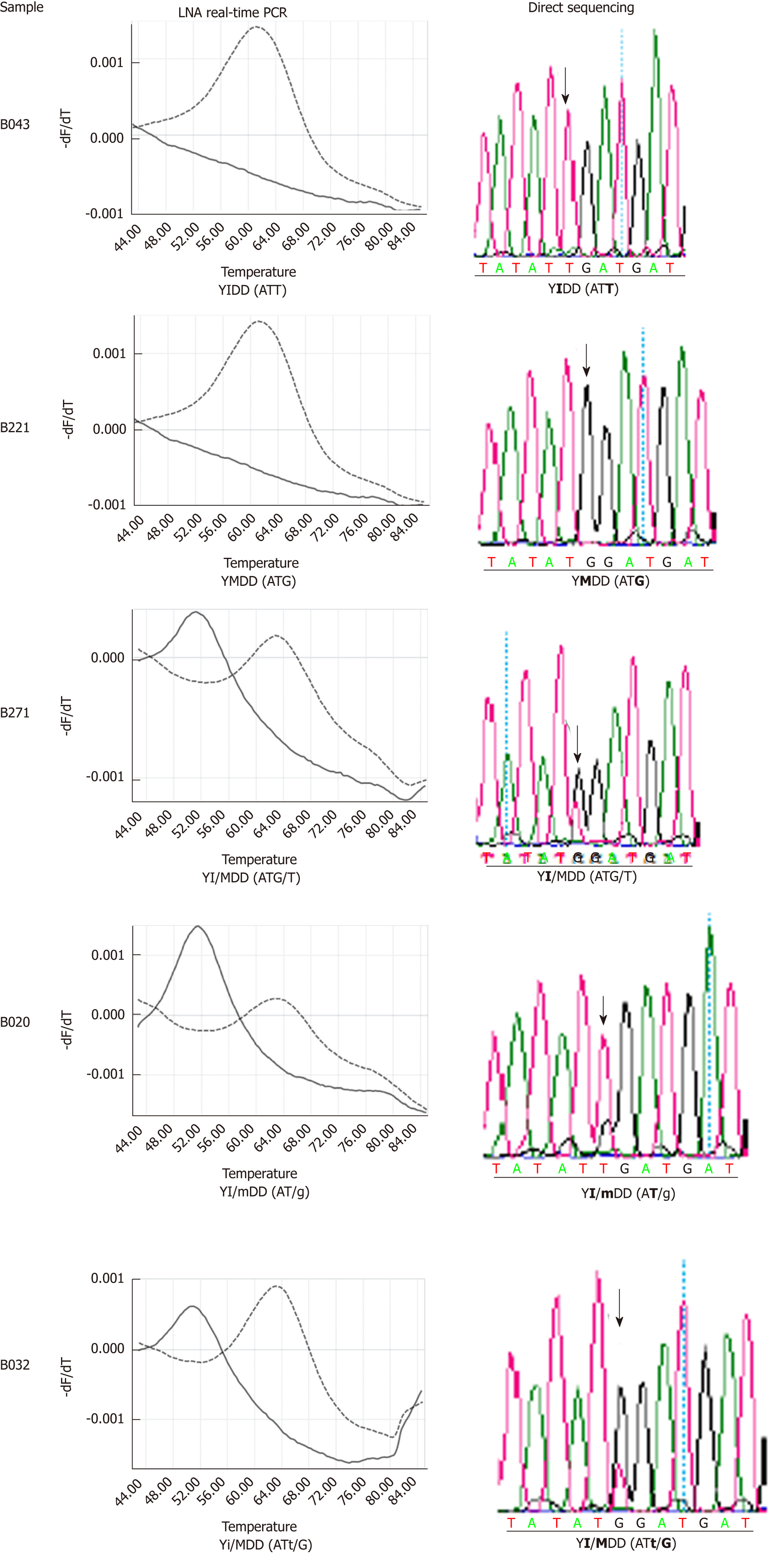
Of 410 clinical samples tested in duplicate by our LNA real-time PCR method, 403 samples (98.3%) were positively identified as WT and/or rtM204I variants, with two samples found to be mixed with presumably unknown variants with non-typable Tms. Of the seven unidentified samples, two samples were amplified but non-typable due to their non-diagnostic melting temperatures (50.4 °C, 57.9 °C) at the HEX channel and five samples did not show any positive signals. Thus, only four samples among all clinical samples tested carried non-typable Tms in this study.
Among the positively identified samples, all of the samples produced a distinct melting peak or peaks with a Tm or Tms being in the diagnostic Tm range for WT or rtM204I. Among all clinical samples, seventeen samples (4.1%) were identified as carrying rtM204I variants and among these samples, nine samples were rtM204I variant exclusively and eight samples were rtM204I variant coexistent with WT. Among these, in four samples, rtM204I was dominant over WT; in one sample, codominant; in three samples, WT was dominant over rtM204I (Table 3). Overall, thirteen samples carried the rtM204I variant predominantly and one sample co-dominantly with WT. The majority of the clinical samples were WT.
| Type of detection | No. of samples | Percentage |
| Clinical samples | 410 | 100% |
| Identified | 403 | 98.3% |
| YIDD | 17 | 4.1% |
| YIDD exclusively | 9 | 2.2% |
| YIDD + YMDD | 3 | 0.7% |
| YIDD + YMDD + YIDD with ATA codon1 | 1 | 0.2% |
| YIDD + YMDD | 1 | 0.5% |
| YIDD + YMDD | 3 | 0.7% |
| YMDD | 394 | 96.3% |
| YMDD exclusively | 385 | 93.9% |
| YMDD + unknown variant | 1 | 0.2% |
| Unidentified | 7 | 1.7% |
| Non-target Tm | 2 | 0.5% |
| HEX 50.4 °C; YVDD1 | 1 | 0.2% |
| HEX 57.9 °C; YMDD with Y of TAC codon1 | 1 | 0.2% |
| No positive signal | 5 | 1.2% |
Three of the four samples that showed Tms out of the WT-diagnostic Tm range were sequenced by direct sequencing of their PCR products. The one sample with a Tm of 50.4 °C was identified as a YVDD variant with a GTG codon and the other sample with a Tm of 57.9 °C was YMDD but had a TAC codon for the Y amino acid. The third sample that showed three melting peaks was revealed to have an additional codon for isoleucine of rtM204I. The results of direct PCR sequencing of thirty clinical samples randomly chosen among positively identified samples by LNA real-time PCR had results identical to those of our LNA real-time PCR assay, proving its reliability for screening for pre-existing rtM204I variants from treatment naïve CHB patients (Figure 3).
Four hundred and three treatment-naïve patients with chronic HBV infection that could be typed by LNA real-time PCR comprising 244 men and 159 women with a mean age of 43.9 ± 12.5 years were included. Baseline characteristics were shown in Table 4. Two hundred thirty-eight (59.1%) patients had HBeAg-positive CHB and 165 (40.9%) patients had HBeAg-negative CHB. Eighty-seven patients had LC, and fifty-one patients had HCC. One hundred fifty-seven had significant fibrosis (defined as FIB-4 score > 3.25, or APRI score > 1.5). Of the 403 treatment-naïve patients, 232 patients were treated with NAs over a period of 1 year. One-hundred ninety-two patients were treated with agents that had a high genetic barrier to resistance (95 patients were treated with tenofovir, and 97 patients were tread with entecavir), and 40 patients were treated with low genetic barrier agents [9, 19, and 12 patients were treated with LAM, adefovir (ADV), and LAM-ADV combination, respectively]. As it is well known that HBV genotype C is the universal type in almost all Korean chronic carriers, HBV genotyping is not routinely carried out in Korea. In our study, HBV genotyping was performed for 40 patients and all (100%) had genotype C2 strains.
| Characteristics | Pre-existing rtM204I n = 17 | Wild type rtM204 n = 386 | P value |
| Gender (M/F) | 14/3 | 230/156 | 0.060 |
| Age (yr) | 48.8 ± 9.3 | 43.7 ± 12.6 | 0.101 |
| HBeAg (positive/negative) | 10/7 | 228/158 | 0.984 |
| HBV-DNA (log10 IU/mL) | 6.33 ± 0.66 | 6.06 ± 1.77 | 0.519 |
| qHBsAg (log 10 IU/mL) | 3.43 ± 0.30 | 3.59 ± 0.70 | 0.334 |
| AST (IU/L) | 104.7 ± 40.9 | 78.7 ± 65.2 | 0.103 |
| ALT (IU/L) | 77.8 ± 29.4 | 85.4 ± 84.1 | 0.709 |
| Total bilirubin (mg/dL) | 0.93 ± 0.33 | 0.88 ± 0.60 | 0.743 |
| Albumin (g/dL) | 4.02 ± 0.43 | 4.14 ± 0.52 | 0.338 |
| Prothrombin time (INR) | 1.07 ± 0.10 | 1.02 ± 0.16 | 0.246 |
| Platelet count (× 103/mm3) | 155.7 ± 55.6 | 181.4 ± 64.4 | 0.106 |
| FIB-4 | 4.38 ± 2.33 | 2.91 ± 2.92 | 0.041 |
| APRI | 1.94 ± 0.98 | 1.34 ± 1.35 | 0.068 |
| Significant fibrosis1 (presence/absence) | 12/5 | 145/241 | 0.006 |
| Liver cirrhosis (presence/absence) | 7/10 | 80 / 306 | 0.045 |
| HCC (presence/absence) | 5/12 | 46 / 340 | 0.034 |
The pre-existing rtM204I variants prior to NAs were detected in 17 of 403 treatment-naïve CHB patients (4.2%). The pre-existing rtM204I variants were more frequently detected in subjects with higher FIB-4 scores. These variants were more often detected in subjects with significant fibrosis, LC, and HCC (Table 4). Among the clinical factors (age, sex, HBeAg status, HBV-DNA titers, HBsAg quantitative levels, AST, ALT, total bilirubin, albumin, prothrombin time, platelet counts, presence of significant fibrosis, LC or HCC), univariate analysis showed that pre-existing rtM204I variants were more frequently detected in patients with significant fibrosis, or patients with HCC. Logistic multivariate analysis showed that pre-existing rtM204I variants were significantly more frequent in patients with significant fibrosis (odd ratio 3.397, 95% confidence interval 1.119-10.319, P = 0.031) (Table 5).
| Pre-existing rtM204I (n = 17) | Wild type rtM204 (n = 386) | Univariate | Multivariate | |||||
| OR | 95%CI | P value | OR | 95%CI | P value | |||
| Gender (male) | 14 (82.4%) | 230 (59.6%) | 3.165 | (0.895-11.197) | 0.074 | |||
| Age, yr | 48.8 ± 9.3 | 43.7 ± 12.6 | 1.033 | (0.993-1.074) | 0.105 | |||
| HBeAg status (positive) | 10 (58.8%) | 228 (59.1%) | 0.990 | (0.369-2.656) | 0.984 | |||
| HBV-DNA, log10 IU/mL | 6.33 ± 0.66 | 6.06 ± 1.77 | 1.098 | (0.827-1.458) | 0.519 | |||
| qHBsAg, log10 IU/mL | 3.43 ± 0.30 | 3.59 ± 0.70 | 0.555 | (0.336-0.916) | 0.021 | |||
| AST, IU/L | 104.7 ± 40.9 | 78.7 ± 65.2 | 1.005 | (0.999-1.011) | 0.109 | |||
| ALT, IU/L | 77.8 ± 29.4 | 85.4 ± 84.1 | 0.999 | (0.992-1.005) | 0.709 | |||
| Total bilirubin, mg/dL | 0.93 ± 0.33 | 0.88 ± 0.60 | 1.140 | (0.522-2.487) | 0.742 | |||
| Albumin, g/dL | 4.02 ± 0.43 | 4.14 ± 0.52 | 0.655 | (0.275-1.559) | 0.339 | |||
| Prothrombin time, INR | 1.07 ± 0.10 | 1.02 ± 0.16 | 4.625 | (0.339-63.020) | 0.250 | |||
| Platelet count, × 103/mm3 | 155.7 ± 55.6 | 181.4 ± 64.4 | 0.993 | (0.985-1.001) | 0.108 | |||
| Significant fibrosis1 | 12 (70.6%) | 145 (37.6%) | 3.989 | (1.377-11.553) | 0.011 | 3.397 | (1.119-10.319) | 0.031 |
| Liver cirrhosis | 7 (41.2%) | 80 (20.7%) | 2.677 | (0.988-7.255) | 0.053 | |||
| HCC | 5 (29.4%) | 46 (11.9%) | 3.080 | (1.038-9.139) | 0.043 | 1.961 | (0.626-6.143) | 0.248 |
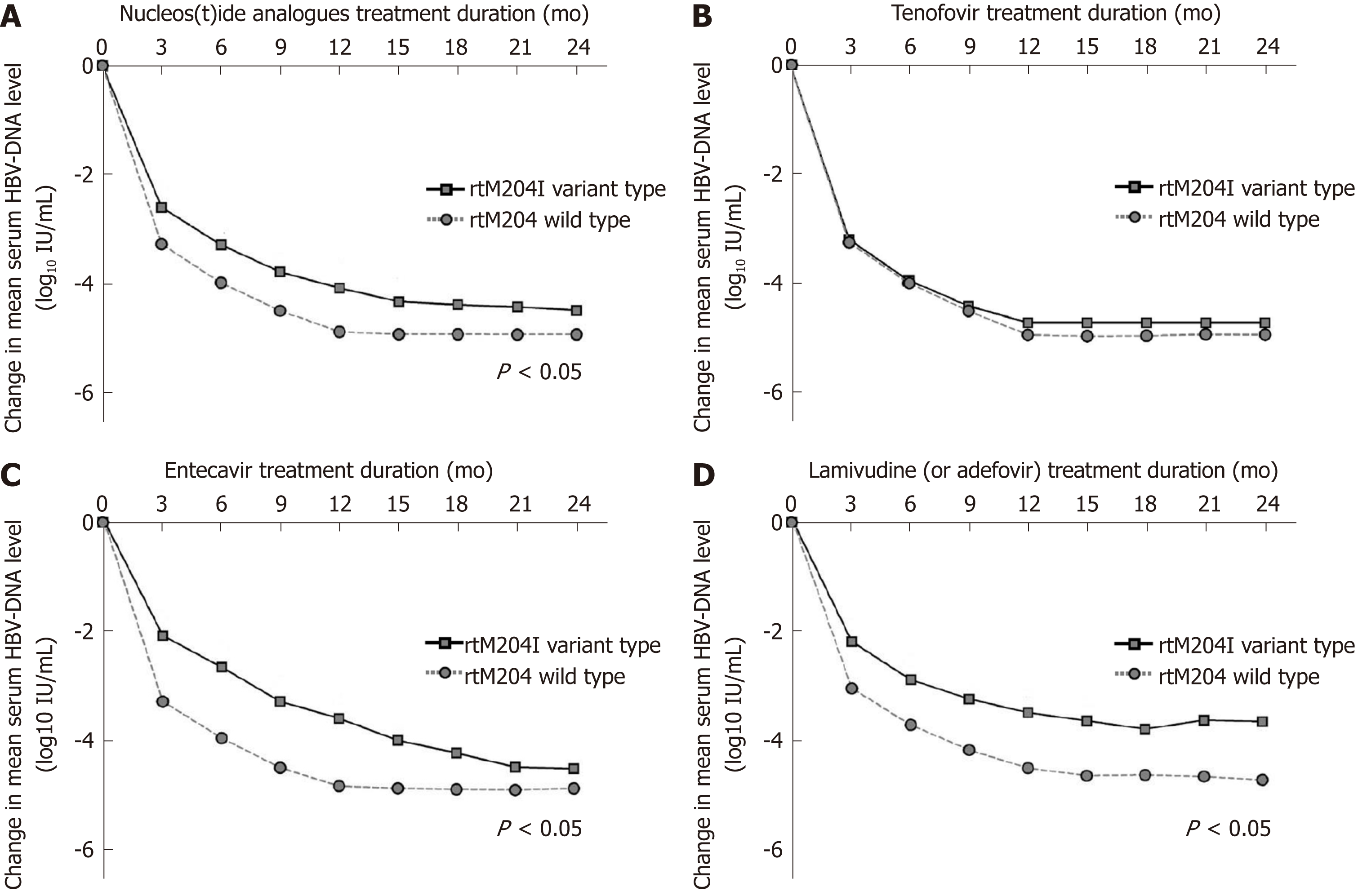
Two hundred and thirty-two patients were treated with oral NAs over a period of 12 mo, and their antiviral responsiveness to NAS was evaluated. One hundred and ninety-nine patients achieved a CVR at 12 months of anti-HBV therapy, whereas thirty-three patients had suboptimal (incomplete) responses. Logistic multivariate regression analysis revealed that achievement of CVR was reversely associated with higher HBV-DNA titers, treatment with low genetic barrier drugs, and, infection with pre-existing rtM204I variants prior to NAs (odds ratio 0.014, 95% confidence interval 0.002-0.096, P < 0.001; Table 6). Figure 4 shows the mean changes in the HBV-DNA level at each point. The decrease in HBV-DNA was significantly less prominent in patients infected with pre-existing rtM204I variants than in patients infected without pre-existing rtM204I variants, at 3, 6, 9, and 12 mo of antiviral treatments (all P < 0.05).
| Complete response (n = 199) | Incomplete response (n = 33) | Univariate | Multivariate | |||||
| OR | 95%CI | P value | OR | 95%CI | P value | |||
| Gender (male) | 130 (65.3%) | 20 (60.6%) | 1.225 | (0.575-2.610) | 0.600 | |||
| Age, yr | 47.3 ± 11.9 | 43.6 ± 10.9 | 1.028 | (0.996-1.062) | 0.087 | |||
| HBeAg status (positive) | 106 (53.3%) | 30 (90.9%) | 0.114 | (0.034-0.386) | < 0.001 | 0.438 | (0.086-2.226) | 0.320 |
| HBV-DNA, log10 IU/mL | 5.97 ± 1.40 | 7.69 ± 1.13 | 0.402 | (0.290-0.559) | < 0.001 | 0.185 | (0.083-0.412) | < 0.001 |
| qHBsAg, log10 IU/mL | 3.46 ± 0.57 | 3.89 ± 0.74 | 0.270 | (0.134-0.544) | < 0.001 | 1.492 | (0.501-4.447) | 0.473 |
| AST, IU/L | 94.6 ± 69.5 | 83.0 ± 47.2 | 1.003 | (0.997-1.009) | 0.361 | |||
| ALT, IU/L | 103.5 ± 92.7 | 91.6 ± 57.5 | 1.002 | (0.997-1.006) | 0.474 | |||
| Total bilirubin, mg/dL | 0.95 ± 0.57 | 0.76 ± 0.30 | 2.201 | (0.964-5.024) | 0.061 | |||
| Albumin, g/dL | 4.06 ± 0.53 | 4.14 ± 0.44 | 0.743 | (0.351-1.573) | 0.438 | |||
| Prothrombin time, INR | 1.05 ± 0.16 | 1.01 ± 0.10 | 8.323 | (0.444-155.931) | 0.156 | |||
| Platelet count, × 103/mm3 | 164.6 ± 63.8 | 182.6 ± 53.0 | 0.995 | (0.990-1.001) | 0.128 | |||
| Significant fibrosis | 105 (52.8%) | 13 (39.4%) | 1.718 | (0.810-3.644) | 0.158 | |||
| Liver cirrhosis | 58 (29.1%) | 6 (18.2%) | 1.851 | (0.726-4.720) | 0.197 | |||
| HCC | 33 (16.6%) | 3 (9.1%) | 1.988 | (0.573-6.899) | 0.279 | |||
| High genetic barrier | 180 (90.5%) | 12 (36.4%) | 16.579 | (7.069-38.882) | < 0.001 | 82.076 | (14.945-450.760) | < 0.001 |
| Pre-existing rtM204I | 9 (4.5%) | 8 (24.2%) | 0.148 | (0.052-0.419) | < 0.001 | 0.014 | (0.002-0.096) | < 0.001 |
Among 95 patients treated with tenofovir, all seven patients with pre-existing rtM204I variants (7/7, 100%) as well as almost patients without pre-existing rtM204I variants (85/88, 96.6%) achieved CVR at 12 mo of tenofovir. Among 97 patients treated with entecavir, only one of six patients with pre-existing rtM204I variants (1/6, 16.7%) achieved CVR at 12 mo of entecavir, whereas almost patients without pre-existing rtM204I variants (87/91, 95.6%) achieved CVR at 12 mo entecavir (87/91, 95.6%). Among 40 patients treated with low genetic barriers, one of four patients with pre-existing rtM204I variants (1/4, 25.0%) and half of patients without pre-existing rtM204I variants (18/36, 50.0%) achieved CVR at 12 mo of low genetic barriers.
Table 7 shows the mean changes in the HBV-DNA levels and cumulative probabilities of CVR in 17 patients with pre-existing rtM204I variants. The cumulative probability of CVR at 12 mo of tenofovir was significantly higher than those of entecavir and low genetic barriers (the Fisher’s exact test: tenofovir vs entecavir, P = 0.005; tenofovir vs low genetic barrier, P = 0.024).
| Outcome | Tenofovir (n = 7) | Entecavir (n = 6) | Low genetic barriers1 (n = 4) | P value |
| Reduction of HBV-DNA (log10 IU/mL), mean ± SD | ||||
| Mo 3 | -3.22 ± 0.74 | -2.12 ± 0.532 | -2.22 ± 0.402 | 0.011 |
| Mo 6 | -3.97 ± 0.75 | -2.71 ± 0.432 | -2.92 ± 0.512 | 0.005 |
| Mo 9 | -4.44 ± 0.70 | -3.33 ± 0.482 | -3.28 ± 0.352 | 0.004 |
| Mo 12 | -4.75 ± 0.59 | -3.65 ± 0.432 | -3.52 ± 0.602 | 0.003 |
| Complete virologic response, cumulative incidence | ||||
| Mo 12 | 100% | 16.7%2 | 25%2 | 0.021 |
Although antiviral resistance mutations occur secondarily to long term use of NAs, they can occur spontaneously in NAs-naïve patients. Since the HBV genome lacks a proofreading function on the RT region of the DNA polymerase, mutations can naturally occur due to random incorrect substitution of nucleos(t)ides. The most common substitutions are methionine at amino acid position 204 to either isoleucine (rtM204I, YIDD mutations) or valine (rtM204V, YVDD mutations)[19,20]. Many studies have revealed that YMDD-motif mutations can emerge naturally in treatment-naïve CHB patients, but their reported prevalence vary greatly (0% to approximately 30%) or are even contradictory[10-13].
Our group recently analyzed the RT region of the HBV polymerase by full-length HBV RT sequences in NAs-naive CHB patients, and we found that approximately 60% of them had antiviral resistant variants with substitutions at T184, M204, L180, or L80 prior to NAs therapy[14]. Among these variants, spontaneous rtM204I/V variants were detected in approximately 1.5% of NAs-native patients, and the rtM204I variant was the dominant type. Additionally, they were more frequently detected in patients with HCC than in patients without HCC. Thus, in this research, we focused on the spontaneous rtM204I variants, and they were evaluated using an LNA-RT-PCR method, which is a more sensitive method than sequence analysis. We also tripled the sample number of NAs-naïve patients with various phases of CHB genotype C infection.
In this study, we have confirmed that spontaneous rtM204I mutations exist in NAs-naïve patients with CHB genotype C infection, and their prevalence is approximately 4%. Spontaneous M204I mutations were more frequently detected in patients with higher scores on the FIB-4 index, which is considered to be a noninvasive marker of liver fibrosis, and multivariate analysis showed that pre-existing M204I mutations were more frequently detected in patients with significant fibrosis[21]. These data suggest that spontaneous rtM204I variants might be risk factors for the progression of liver fibrosis. Although the mechanism is unclear, a possible reason for the significant association between spontaneous rtM204I variants and liver fibrosis might also be related to HBV genotype C. Many studies have demonstrated that naturally occurring mutations, such as variants in the pre-S region, are associated with LC and HCC development in CHB patients, especially those infected with genotype C[22,23]. Hence, this study suggested that progression of fibrosis might be related to spontaneous occurrence of rtM204I mutations prior to NAs, as well as infection with naturally occurring pre-S variants, in treatment-naïve patients infected with HBV genotype C2 strains.
Another finding of this study is that spontaneous rtM204I variants could affect antiviral responsiveness in treatment-naïve patients when they are treated with NAs. Our data showed that CVR rate to antiviral therapy was significantly lower in patients infected with spontaneous rtM204I variants. Indeed, rtM204I variants are the predominant mutations causing resistance to NAs with low genetic barriers, such as LAM, L-dT, and CLV[6,24]. These variants can also reduce the susceptibility to entecavir therapy and induce entecavir resistance[25]. This study also revealed that all seven patients carrying pre-existing rtM204I mutations achieved CVR to tenofovir, which can effectively suppress not only WT HBV strains but also rtM204I variants. In contrast, only one of six patients carrying pre-existing rtM204I mutations achieved CVR at 12 mo of entecavir treatment, and one of four patients achieved CVR at 12 mo of low genetic barrier agents. Therefore, tenofovir is the preferred treatment since its higher barrier to resistance provides the best chance for successful long-term therapy in treatment-naïve patients carrying spontaneous rtM204I variants.
Recently, a Korean population-based cohort study demonstrated that tenofovir treatment was associated with a significantly lower risk of HCC compared with entecavir treatment[26]. This result might be related to the fact that tenofovir therapy can more effectively suppress HBV-DNA compared to entecavir therapy and consequently decrease the risk of LC progression or HCC development in Korean patients infected with HBV genotype C strains, some of whom have spontaneous rtM204I variants.
In conclusion, the LNA-RT-PCR method can detect pre-existing rtM204I variants with high sensitivity in NAs-naïve CHB patients. rtM204I mutations can occur spontaneously with a rate of approximately 4% in treatment-naïve patients infected with HBV genotype C2. The rtM204I variants more frequently pre-existed in patients with significant fibrosis, and the pre-existence of rtM204I variants was associated with incomplete responses to NAs. Therefore, the detection of pre-existing rtM204I variants with the newly developed LNA-RT-PCR method could play a relevant role in the clinical management of NA-naïve patients with CHB genotype C2 infection.
Hepatitis B virus (HBV) DNA polymerase mutations usually occur to long term use of nucleos(t)ide analogues (NAs), but they can occur spontaneously in treatment-naïve chronic hepatitis B (CHB) patients. The naturally occurring HBV-DNA polymerase mutations might complicate antiviral therapy with NAs, leading to the generation of drug-resistant viral mutants and disease progression. The most common substitutions are known to be YMDD-motif mutations, but their prevalence and the influence on antiviral therapy is unclear.
HBV DNA polymerase mutations have been known to be prevalent in treatment-naïve CHB patients infected with HBV genotype C2 strains. But there is still controversy regarding prevalence of the naturally occurring rtM204I mutations prior to antiviral treatments. Moreover, the clinical characteristics of the naturally occurring rtM204I mutations have not been fully elucidated.
The objective of this study was to determine the prevalence and clinical characteristics of naturally occurring rtM204I mutations in treatment-naïve patients infected with HBV genotype C2 strains by using a newly developed locked nucleotide probe (LNA probe) based real time PCR (LNA-RT-PCR) method, which can detect subspecies at 5% of the circulating HBV population.
The retrospective study enrolled a total of 410 treatment-naïve CHB patients infected with HBV genotype C2 strains. Among the 410 patients, 232 were treated with NAs for at least 12 mo. Significant fibrosis was defined as fibrosis-4 index > 3.25 or aspartate aminotransferase to platelet ratio index > 1.5. Complete viral response (CVR) during NAs was defined as undetectable serum HBV DNA (< 24 IU/mL). The rtM204I variants were analyzed by a newly developed LNA RT-PCR method.
The LNA-RT-PCR could discriminate rtM204I mutant-type (17 patients, 4.2%) from rtM204 wild-type (386 patients, 95.8%) in 403 of 410 patients (98.3% sensitivity). Multivariate analysis showed that naturally occurring rtM204I variants were more frequently detected in patients with significant fibrosis [odd-ratio (OR) 3.397, 95% confidence-interval (CI) 1.119-10.319, P = 0.031]. Of 232 patients receiving NAs, multivariate analysis revealed that achievement of CVR was reversely associated with naturally occurring rtM204I variants prior to NAs treatment (OR 0.014, 95%CI 0.002-0.096, P < 0.001). Almost patients receiving tenofovir achieved CVR at 12 mo of tenofovir, irrespective of pre-existence of naturally occurring rtM204I mutations (CVR rates: patients with rtM204I, 100%; patients without rtM204I, 96.6%), whereas, pre-existence of naturally-occurring rtM204I-mutations prior to NAs significantly affects CVR rates in patients receiving entecavir (at 12 mo: Patients with rtM204I, 16.7%; patients without rtM204I, 95.6%, P < 0.001).
The newly developed LNA-RT-PCR method can detect pre-existing rtM204I variants with high sensitivity in NAs-naïve CHB patients. rtM204I mutations can occur spontaneously with a rate of approximately 4% in treatment-naïve patients infected with HBV genotype C2. The rtM204I variants more frequently pre-existed in patients with significant fibrosis, and the pre-existence of rtM204I variants was associated with incomplete responses to NAs. Tenofovir is a more suitable treatment than entecavir for CHB patients carrying the naturally occurring rtM204I mutations.
The detection of pre-existing rtM204I variants with the newly developed LNA-RT-PCR method could play a relevant role in the clinical management of NA-naïve patients with CHB genotype C2 infection. Further prospective studies should be performed to verify our conclusions.
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (Grant No., 2016932422 and 2019R1A2C1084511).
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: South Korea
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Jain M, Komatsu H, Xu XY, Zheng SJ S-Editor: Yan JP L-Editor: A E-Editor: Ma YJ
| 1. | Dienstag JL. Hepatitis B virus infection. N Engl J Med. 2008;359:1486-1500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 689] [Cited by in RCA: 689] [Article Influence: 40.5] [Reference Citation Analysis (0)] |
| 2. | Wong GL. Management of chronic hepatitis B patients in immunetolerant phase: What latest guidelines recommend. Clin Mol Hepatol. 2018;24:108-113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 3. | European Association for the Study of the Liver. EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection. J Hepatol. 2017;67:370-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3745] [Cited by in RCA: 3773] [Article Influence: 471.6] [Reference Citation Analysis (1)] |
| 4. | Terrault NA, Bzowej NH, Chang KM, Hwang JP, Jonas MM, Murad MH; American Association for the Study of Liver Diseases. AASLD guidelines for treatment of chronic hepatitis B. Hepatology. 2016;63:261-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1532] [Cited by in RCA: 1578] [Article Influence: 175.3] [Reference Citation Analysis (2)] |
| 5. | Pawlotsky JM, Dusheiko G, Hatzakis A, Lau D, Lau G, Liang TJ, Locarnini S, Martin P, Richman DD, Zoulim F. Virologic monitoring of hepatitis B virus therapy in clinical trials and practice: Recommendations for a standardized approach. Gastroenterology. 2008;134:405-415. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 180] [Cited by in RCA: 174] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 6. | Bartholomeusz A, Locarnini SA. Antiviral drug resistance: Clinical consequences and molecular aspects. Semin Liver Dis. 2006;26:162-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 100] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 7. | Glebe D, Bremer CM. The molecular virology of hepatitis B virus. Semin Liver Dis. 2013;33:103-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 122] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 8. | Locarnini S, Zoulim F. Molecular genetics of HBV infection. Antivir Ther. 2010;15 Suppl 3:3-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 131] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 9. | Kim BJ. Hepatitis B virus mutations related to liver disease progression of Korean patients. World J Gastroenterol. 2014;20:460-467. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 31] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 10. | Tan Y, Ding K, Su J, Trinh X, Peng Z, Gong Y, Chen L, Cui Q, Lei N, Chen X, Yu R. The naturally occurring YMDD mutation among patients chronically infected HBV and untreated with lamivudine: A systematic review and meta-analysis. PLoS One. 2012;7:e32789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Heo J, Cho M, Kim HH, Shin YM, Jang HJ, Park HK, Kim CM, Kim GH, Kang DH, Song GA, Yang US. Detection of YMDD motif mutants by oligonucleotide chips in lamivudine-untreated patients with chronic hepatitis B virus infection. J Korean Med Sci. 2004;19:541-546. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Horgan M, Brannigan E, Crowley B, Levis J, Fanning LJ. Hepatitis B genotype and YMDD profiles in an untreated Irish population. J Clin Virol. 2006;35:203-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Kirishima T, Okanoue T, Daimon Y, Itoh Y, Nakamura H, Morita A, Toyama T, Minami M. Detection of YMDD mutant using a novel sensitive method in chronic liver disease type B patients before and during lamivudine treatment. J Hepatol. 2002;37:259-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 73] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Choi YM, Lee SY, Kim BJ. Naturally occurring hepatitis B virus reverse transcriptase mutations related to potential antiviral drug resistance and liver disease progression. World J Gastroenterol. 2018;24:1708-1724. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 37] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 15. | Kim H, Jee YM, Song BC, Hyun JW, Mun HS, Kim HJ, Oh EJ, Yoon JH, Kim YJ, Lee HS, Hwang ES, Cha CY, Kook YH, Kim BJ. Analysis of hepatitis B virus quasispecies distribution in a Korean chronic patient based on the full genome sequences. J Med Virol. 2007;79:212-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Xiao G, Yang J, Yan L. Comparison of diagnostic accuracy of aspartate aminotransferase to platelet ratio index and fibrosis-4 index for detecting liver fibrosis in adult patients with chronic hepatitis B virus infection: A systemic review and meta-analysis. Hepatology. 2015;61:292-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 338] [Cited by in RCA: 389] [Article Influence: 38.9] [Reference Citation Analysis (0)] |
| 17. | Yu SJ. A concise review of updated guidelines regarding the management of hepatocellular carcinoma around the world: 2010-2016. Clin Mol Hepatol. 2016;22:7-17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 185] [Cited by in RCA: 225] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 18. | Sarin SK, Kumar M, Lau GK, Abbas Z, Chan HL, Chen CJ, Chen DS, Chen HL, Chen PJ, Chien RN, Dokmeci AK, Gane E, Hou JL, Jafri W, Jia J, Kim JH, Lai CL, Lee HC, Lim SG, Liu CJ, Locarnini S, Al Mahtab M, Mohamed R, Omata M, Park J, Piratvisuth T, Sharma BC, Sollano J, Wang FS, Wei L, Yuen MF, Zheng SS, Kao JH. Asian-Pacific clinical practice guidelines on the management of hepatitis B: A 2015 update. Hepatol Int. 2016;10:1-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1985] [Cited by in RCA: 1947] [Article Influence: 216.3] [Reference Citation Analysis (0)] |
| 19. | Tsubota A. How do naturally occurring YMDD-motif mutants influence the clinical course of lamivudine-naïve patients with chronic hepatitis B virus infection? J Gastroenterol Hepatol. 2006;21:1769-1771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Keeffe EB, Dieterich DT, Pawlotsky JM, Benhamou Y. Chronic hepatitis B: Preventing, detecting, and managing viral resistance. Clin Gastroenterol Hepatol. 2008;6:268-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 57] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 21. | Houot M, Ngo Y, Munteanu M, Marque S, Poynard T. Systematic review with meta-analysis: Direct comparisons of biomarkers for the diagnosis of fibrosis in chronic hepatitis C and B. Aliment Pharmacol Ther. 2016;43:16-29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 22. | Kim H, Kim BJ. Association of preS/S Mutations with Occult Hepatitis B Virus (HBV) Infection in South Korea: Transmission Potential of Distinct Occult HBV Variants. Int J Mol Sci. 2015;16:13595-13609. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 23. | Kim H, Lee SA, Do SY, Kim BJ. Precore/core region mutations of hepatitis B virus related to clinical severity. World J Gastroenterol. 2016;22:4287-4296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 36] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (1)] |
| 24. | Zeng Y, Li D, Wang W, Su M, Lin J, Chen H, Jiang L, Chen J, Yang B, Ou Q. Establishment of real time allele specific locked nucleic acid quantitative PCR for detection of HBV YIDD (ATT) mutation and evaluation of its application. PLoS One. 2014;9:e90029. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Gish R, Jia JD, Locarnini S, Zoulim F. Selection of chronic hepatitis B therapy with high barrier to resistance. Lancet Infect Dis. 2012;12:341-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 106] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 26. | Choi J, Kim HJ, Lee J, Cho S, Ko MJ, Lim YS. Risk of Hepatocellular Carcinoma in Patients Treated With Entecavir vs Tenofovir for Chronic Hepatitis B: A Korean Nationwide Cohort Study. JAMA Oncol. 2019;5:30-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 230] [Article Influence: 38.3] [Reference Citation Analysis (0)] |