Published online Aug 14, 2019. doi: 10.3748/wjg.v25.i30.4199
Peer-review started: April 10, 2019
First decision: May 9, 2019
Revised: May 28, 2019
Accepted: July 2, 2019
Article in press: July 3, 2019
Published online: August 14, 2019
Processing time: 128 Days and 7.6 Hours
The huge prognostic difference between early and late stage hepatocellular carcinoma (HCC) is a challenging diagnostic problem. Alpha-fetoprotein is the mostly widely used biomarker for HCC used in the clinic, however it’s sensitivity and specificity of is not optimal. The development and application of multiple biotechnologies, including next generation sequencing, multiple “omics” data, that include genomics, epigenomics, transcriptomics, proteomics, metabolomics, metagenomics has been used for HCC diagnostic biomarker screening. Effective biomarkers/panels/models have been identified and validated at different clinical levels. A large proportion of these have a good diagnostic performance for HCC, especially for early HCC. In this article, we reviewed the various HCC biomarkers derived from “omics” data and discussed the advantages and disadvantages for diagnosis HCC.
Core tip: Compared to traditional biomarkers, high throughput technologies provide novel insights and mechanistic understanding of hepatocellular carcinoma (HCC). In this article, recent genomic, epigenomic, transcriptomic, proteomic, metabolomics, and metagenomics based HCC diagnostic biomarkers and their performance was evaluated. The advantages and disadvantages of these HCC diagnostic biomarkers are also discussed.
- Citation: Liu XN, Cui DN, Li YF, Liu YH, Liu G, Liu L. Multiple “Omics” data-based biomarker screening for hepatocellular carcinoma diagnosis. World J Gastroenterol 2019; 25(30): 4199-4212
- URL: https://www.wjgnet.com/1007-9327/full/v25/i30/4199.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i30.4199
In 2018, hepatocellular carcinoma (HCC) was the sixth most common cancer and the fourth leading cause of deaths worldwide. It is estimated that about 841000 new cases and 78000 deaths will occur each year. The incidence of HCC varies regionally but is the most common cancer in thirteen geographically countries[1].
HCC accounts for 75% to 85% of all liver cancers[1]. HCC is a multifactorial disease due to a variety of risk factors. Chronic infection with hepatitis B virus (HBV) or hepatitis C virus, aflatoxin-contaminated food, heavy alcohol intake, obesity, smoking, and type 2 diabetes are the main risk factors for HCC[2,3]. The occurrence of HCC results from a combination of virus-specific factors, immune mechanisms, environmental factors and genetics[4]. Due to the complicated etiology of liver cancer and the different molecular subtypes observed in individuals, early diagnosis is difficult[5]. As a result, the majority of patients are diagnosed with late-stage HCC, with a five-year survival rate of only 10.1%[6]. Thus, early diagnosis is necessary to improve HCC patient survival.
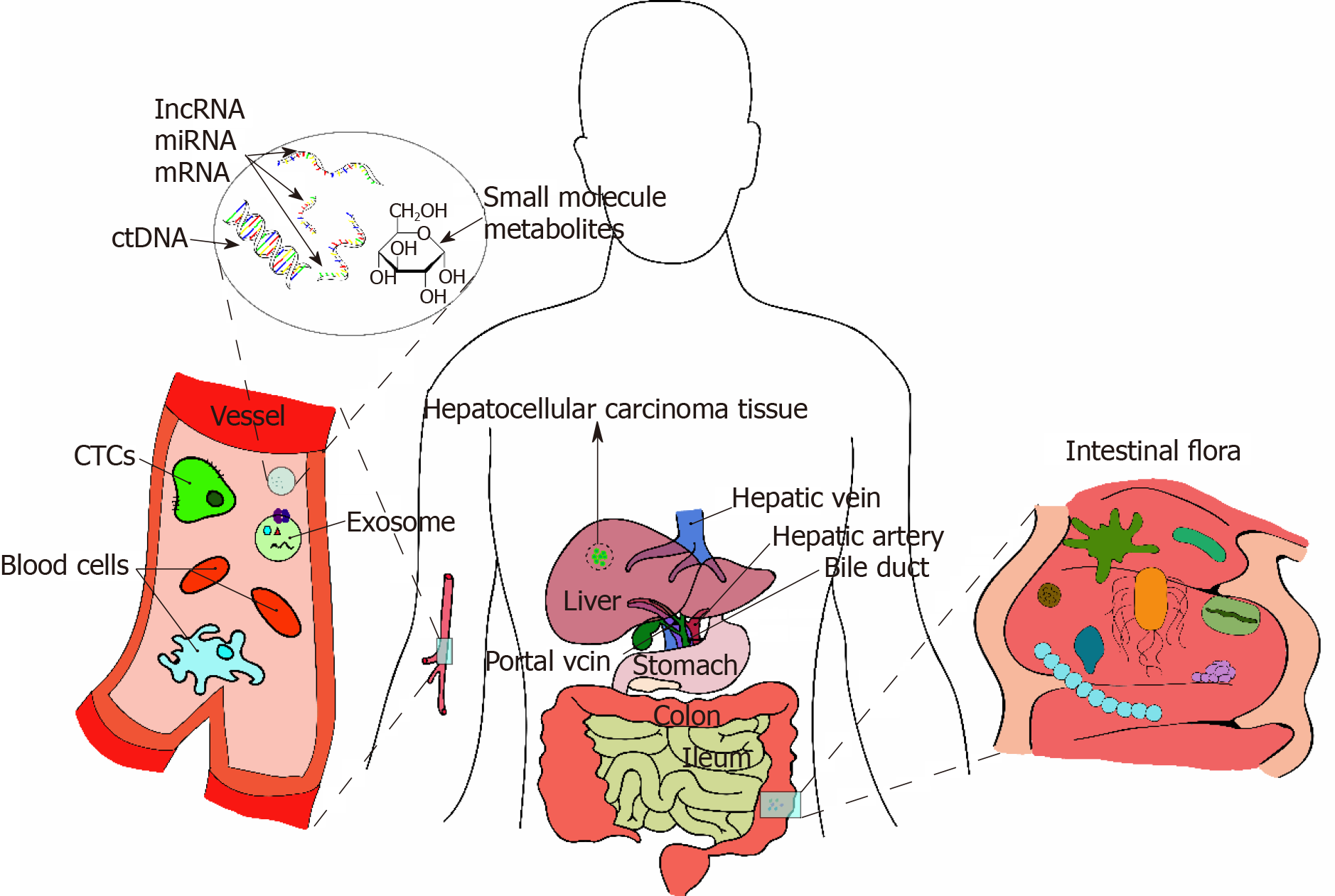
Early screening is essential for the early detection and treatment of HCC. Diagnostic methods for HCC include clinical, imaging, molecular marker and omics diagnosis[7]. Clinical symptom, Imaging diagnosis[8], and molecular biomarkers are the most com-monly used evidences for HCC detection. The molecular markers commonly used for the diagnosis of HCC are alpha-fetoprotein (AFP)[9], desaturation-γ-lock-up-thrombin (DCP)[10], and phosphatidylinositol proteoglycan-3 (GPC-3)[10-12]. HCC heterogeneity significantly limits the diagnosis and treatment of HCC patients[13-15], making the efficiency of diagnosis and treatment very low. With the advent of next generation sequencing and the development of precision medicine, individual heterogeneity-based histological diagnosis makes it possible for individualized diagnosis and targeted HCC therapy[16,17]. Omics data, including but not limited to genomic, epigenomic, transcriptomic, proteomic and metabolomic, identifies biological heterogeneity and has provided novel insights for HCC diagnosis, as shown in Figure 1. With regards to genomics, circulating tumor DNA (ctDNA)[18] has been recognized as omics diagnostic markers. Currently, ctDNA can be extracted using a small amount of peripheral blood from patients and is minimally invasive. ctDNA can reveal genetic and epigenetic changes associated with specific cancers and their metastatic potential, and provides unique insights for the continuous monitoring of tumor genomes in a non-invasive, convenient, and accurate way[18]. With regards to epigenomics, methylation patterns in ctDNA could be used for the diagnosis of HCC[19]. Using transcriptomics, circulating miRNAs has been demonstrated to have unique expression patterns for various tumors including HCC[10,20,21]. In addition, circulating miRNAs combined with conventional AFP and ultrasound screening tools have great application prospects for the prediction and prevention of HCC in high-risk populations[5,22]. Proteomic markers such as AFP, AFP-L3, DCP, GPC3, Golgi protein-73 (GP73)[9] etc. are considered diagnostic markers for HCC, however they have poor sensitivity and specificity[9,23]. In addition to the diagnostic tools mentioned above, metabolomics and metagenomics has also contributed to the diagnosis of HCC. This review will focus on the omics based HCC diagnosis.
Circulating tumor cells (CTCs) are generally considered to be the “seeds” of tumors that migrate from carcinomas in situ to the peripheral blood or lymphatic system[24]. This process takes place at every stage of tumor development. Hence, CTCs may be a good tool for HCC diagnosis.
CTCs can be separated and enriched using methods based on their physical and biological properties. The physical characteristics including size, density, migration capacity, and charge and are independent of the expression of established cancer epitopes. However, the separation and enrichment of CTCs are less cancer-specific[25]. Various bio-based technologies rely on specific antibodies that bind to CTC surface markers, including but not limited to epithelial cell adhesion molecule (EpCAM), human epidermal growth factor receptor, members of the cytokeratin (CK) family (CK8, CK18 and CK19) and mesenchymal markers (N-cadherin and vimentin)[26]. Various technologies based on the physical or biological properties of CTCs have been used for CTC detection. These include, the CellSearch® system (CSS: Veridex LLC, NJ, United States)[27], RT-PCR method, the CanPatrol CTC analysis platform (SurExam, China)[28], the ISET technology (segregation by the size of epithelial tumor cells)[29], flow cytometry[30], and CTC-Chip[31,32].
Numerous studies have been performed to investigate the diagnostic value of CTCs using these approaches. Guo et al[33] found that the rate of detectable EpCAMmRNA+ CTCs using their optimized qRT-PCR–based platform was significantly higher in HCC patients compared to healthy controls (P < 0.05), while the area under the curve (AUC) for EpCAMmRNA+ CTCs combined with AFP levels for discriminating HCC vs controls was 0.857, with a sensitivity of 73.0% and specificity of 93.4%. In addition, it was accurate for detecting early stage and AFP-negative HCC. Guo et al[34] demon-strated the clinical significance of CTC with stem-like phenotypes for diagnosing HBV–related HCC using an optimized qPCR-based detection platform. They found that using a panel containing four putative stem cell biomarkers (EpCAM, CD90, CD133, and CK19) outperformed EpCAM alone for the diagnosis of HCC and had an AUC of 0.88 and 0.93 in the training set and the validation set, respectively. CTCs may induce metastases in distal organs and hence may play a significant role in prognosis[35-37]. Qi et al[37] demonstrated that the percentages of CTC and mesenchymal-CTC were significantly associated with early recurrence, multi-intrahepatic recur-rence, and lung metastasis.
Exosomes are cell-derived vesicles about 30-100 nm in size. They are intraluminal vesicles formed by the inward budding of the endosomal membrane, and secreted out of the cell by the fusion of MVEs with the cell surface[25]. Exosomes are released into the extracellular space by multiple cell types, and are present in many eukaryotic fluids including blood, urine, cerebrospinal fluid and cultured cell culture media[38,39]. Exosomes are currently a good tool for the HCC diagnosis. Several exosomes isolation technologies are used clinically, such as ultracentrifugation, sucrose-gradient centrifugation, and immune-magnetic isolation[40].
mRNA, microRNA, and lncRNA in exosomes are prevented from being degraded by RNases due to the exosome lipid layer. Several studies have recommended serum exosomes and exosomes enclosed RNAs as HCC screening biomarkers[21,40]. Xu et al[41] using 301 patient samples demonstrated that the combination of exosomal ENSG00000258332.1, LINC00635 and serum AFP has an AUC of 0.885-0.894 for HCC diagnosis. The combination of exosomal miR-122, miR-148a, and serum AFP increased the AUC to 0.931 for distinguishing early HCC from liver cirrhosis. Additionally, exosomal miR-122 was the best for differentiating HCC from NC (AUC = 0.990)[42]. Furthermore, serum exosomal heterogeneous nuclear ribonucleoprotein H1, LINC00161, and miRNA224 were also able to distinguish HCC patients from healthy controls (AUC = 0.865; AUC = 0.794; AUC = 0.91, respectively)[43-45]. Studies have also demonstrated that exosome enclosed RNAs had the potential for HCC prognosis[46,47].
Circulating cell-free DNA is defined as extracellular DNA present in plasma or serum samples. ctDNA is specifically released from tumor cells undergoing metabolic secretion, apoptosis or necrosis. ctDNA carries with it tumor-specific genetic or epigenetic changes, such as DNA methylation, point mutations, copy number variation, etc[18]. A recent study using minimally invasive examination of ctDNA harvested from a small amount of patient peripheral blood demonstrated genetic and epigenetic changes associated with specific cancers and their metastatic status. This provides a unique insight for the continuous monitoring of tumor genomes in a non-invasive and precise way.
The methylation pattern of ctDNAs is applicable for the early detection of HCC. Methylation changes occur in many genes that are involved in the initiation and progression of HCC. Several studies have demonstrated changes in DNA methylation in tumor tissues of HCC patients, including the aberrant methylation of the glutathione S-transferase P1 (GSTP1) promoter region[48,49] and the cyclin-dependent kinase inhibitor p15 and p16[50,51]. Hypermethylated GSTP1[52], p15[53] and p16[54] in ctDNA from HCC patients have been observed. The study conducted by Wang et al[52] demonstrated GSTP1 promoter CpG island hypermethylation in 23 of 26 (88.5%) tumor tissues and 18 of 26 (69%) corresponding non-tumor tissues. Huang et al[19] analyzed the methylation status of four genes (APC, GSTP1, RASSF1A and SFRP1) in plasma and demonstrated sufficient diagnostic value of ctDNAs. The combination of these four genes increased the AUC to 0.933 with 92.7% sensitivity and 81.9% specificity for distinguishing HCC patients from normal healthy controls. MS-PCR has been widely used in methylation studies and provides a quick and easy method with high sensitivity and accuracy. The tissue specificity of methylation patterns in ctDNA may help determine original tumor location. The above results indicate that comprehensive assessment of circulating methylated DNA may be a promising tool for HCC diagnosis and management.
In addition to changes in methylation patterns, other genetic or epigenetic changes have been demonstrated in ctDNAs. These include microsatellite changes, point mutations, chromosomal rearrangements, and viral DNA which may contribute to the early diagnosis of HCC. Comparative genomic hybridization technology has enabled scientists to study microsatellite changes in HCC, such as chromosome 8p, 17p and 19p deletions[55]. The loss of 8p has been reported in eight metastatic tumors, but only in three corresponding primary tumors (P = 0.03)[56]. Droplet digital PCR[57] and whole-genome high-throughput sequencing[58] has been used to accurately detect rare and multiple types of mutations in circulating DNA. Point mutations that inactivated tumor suppressor genes or activate proto-oncogenes can be detected in ctDNA using these technologies. Ser249 of TP53 is the most frequently reported mutation hotspot in HCC patients, that results in a loss of specific DNA binding capacity[59]. Recent studies have demonstrated that TP53 Ser249 mutations are highly correlated with cirrhosis and HCC in China and Africa[60]. In addition, high recurring hotspot mutations have been detected for TP53 R249S, CTNNB1 amino acids D32, S33, S37, T41 and S45, and TERT c.-124C> T promoter mutations[61-63] and may be regarded as potential markers for HCC diagnosis. Additionally, genomic sequencing revealed several recurrent chromosomal rearrangements in HCC, including deletions, insertions, amplifications, translocations, and more complex rearrangements. Detection of these chromosomal rearrangements in ctDNA requires highly sensitive PCR. This has only been successfully applied in a small group of patients, mostly with hematological malignancies[18]. However, whole-genome sequencing of ctDNA provides an opportunity to identify changes in chromosomal rearrangements or copy number in HCC patients and will ultimately become a reliable and robust method for HCC detection. Although ctDNA has been associated with disease stages and is easy to measure, it lacks the sensitivity and specificity[64]. Additional case-control and clinical studies should be performed to validate its utility, especially for diagnosis of early stage HCC.
Among the diagnostic biomarkers of HCC, serum RNAs, including mRNAs, circular RNAs, long non-coding RNAs and micro-RNAs have garnered recent attention, while studies using urine RNAs have been seldomly reported. In this section, we will mainly focus on long non-coding RNAs and micro-RNAs.
Micro-RNA are non-coding RNAs consisting of approximately 22 nucleotides. miRNAs are not chemically stable, however circulating miRNAs in plasma makes them ideal biomarkers to be studied for HCC. Using TLDA Chips, Yang et al. reported that eight miRNAs were dysregulated in HCC. The AUC of the eight-miRNAs for HCC diagnosis reached 0.802 for their patient cohort[65] in their phase three study. In addition, four lncRNAs (miR-20a-5p, miR-320a, miR-324-3p and miR-375) have been used as preclinical biomarkers for HCC. Another study demonstrated that plasma miR-224 was significantly expressed in HCC patients. They found that the AUC for diagnosis was 0.888-0.899 for early HCC patients[66]. Similar studies on miR-106b[67], miRNAs 21, 199-a[68] and microRNA-21[69] have also reported their diagnostic value for HCC, especially early HCC, with AUCs of 0.885, 0.865, and 0.943 respectively, with some having prognostic value. However, the diagnostic and prognostic value of these miRNA have not been replicated in other studies. The performance of these miRNAs needs further validation before clinical use.
Long non-coding RNAs were usually more than 200 nucleotides. They function in RNA stability, protein and DNA binding. Several circulating lncRNAs have demonstrated diagnostic values for HCC. For example, Li et al[70] reported that by combining circulating lncRNAs HULC and Linc00152, the AUC for HCC diagnosis was 0.87, while combining them with AFP, the AUC could reach 0.89. Another study combined three plasma lncRNAs (LINC00152, RP11-160H22.5 and XLOC014172) as a model to discriminate healthy/chronic hepatitis patients from HCC patients and had an AUC of 0.985-0.986[71]. Additional lncRNAs, including p34822, have also been reported to have diagnostic value[72].
Metabolomics is an “omics” method for the high-throughput identification, quantifi-cation and characterization of small metabolites (metabolites with an atomic mass < 1.5 kDa)[73]. Metabolomics provides direct information on metabolites produced by both endogenously and exogenously[74]. Two major analytical platforms have been used in HCC metabolomics studies: Nuclear magnetic resonance spectroscopy and mass spectrometry (MS)[75]. The latter is generally equipped with different separation instruments, that comprise liquid chromatography (LC), gas chromatography (GC), and capillary electrophoresis[63,74] capabilities.
Blood, urine, and feces can be easily obtained from individuals and are generally used in human metabolomic studies. Several metabolomics studies using blood and urine have been reported for HCC diagnosis. Di Poto et al[76] performed GC coupled MS (GC-MS)-based metabolomics on plasma samples from 128 individuals (63 HCC cases and 65 cirrhotic controls). They demonstrated that a panel consisting of 11 metabolites and three clinical factors (AFP, Child–Pugh score, and etiologic factors) had a higher area under the ROC curve (AUC = 0.985) compared to AFP alone. Luo et al[77] performed LC-MS-based metabolomics on serum samples from 1448 individuals (healthy controls and patients with chronic HBV infection, liver cirrhosis, and HCC), and identified a biomarker panel (phenylalanyl-tryptophan and glycocholate) that had a better diagnostic value (AUC = 0.807) compared to AFP (AUC = 0.650) for distinguishing HCC patients from a high-risk cohort of cirrhosis patients. In addition, Lu et al[78] found that serum acetylcarnitine was able to discriminate HCC patients from patients with cirrhosis (AUC = 0.808-0.887). In addition, other biomarker panels have been identified using different metabolites to discriminate HCC patients from non-HCC patients[79-81].
AFP, AFP-L3, DCP, Glypican-3 (GPC3), Osteopontin (OPN), Midkine (MDK), GP73, Annexin A2, squamous cell carcinoma antigen, soluble urokinase plasminogen activator receptor, and thioredoxin have been shown to have value for the early diagnosis of liver cancer. An introduction for each protein and its sensitivity and specificity for the early diagnosis of HCC have been compiled from literature and is shown in Table 1. It is worth mentioning that AFP is regarded as the most useful biomarker for HCC diagnosis, and the only biomarker evaluated in randomized controlled trials[82]. Most of the biomarkers were evaluated in case-control studies for the detection of early stage HCC[83].
| Biomarker | Full name | Sensitivity (%) | Specificity (%) | Ref. | Description |
| AFP | α-fetoprotein | 66 | 82 | [9] | A glycoprotein with a molecular weight of approximately 70 kDa that transports a variety of molecules, including bilirubin, fatty acids, steroids, and various drugs |
| 65 | 94 | [107] | |||
| AFP-L3 | AFP-L3 (binding fraction) | 28 | 97 | [9] | One of the three glycoforms of AFP. AFP-L3 is only derived from cancer cells and has a higher specificity than AFP |
| 37 | 92 | [108] | |||
| DCP | Des-γ-carboxyprothrombin | 77 | 82 | [23] | Prothrombin, Des-γ-carboxyprothrombin (DCP), induced by vitamin K deletion II (PIVKAII), is an abnormal prothrombin molecule that is increased in HCC |
| 61 | 70 | [9] | |||
| GPC3 | Glypican-3 | 55.2 | 84.2 | [11] | Glypican-3 (GPC3) belongs to the glypican family of heparan sulfate proteoglycans. GPC3 is involved in cell proliferation, survival and tumor suppression |
| GP73 | Golgi protein-73 | 62 | 88 | [9] | It is a type II Golgi-specific membrane protein that is normally expressed in epithelial cells of various human tissues, but not in hepatocytes. However, GP73 is detected in the serum of patients with liver disease, especially HCC |
| OPN | Osteopontin | 75 | 62 | [99] | Also known as transformation-associated protein phosphatase, a glycophosphoprotein that binds to integrin, which is overexpressed in many different types of malignancies, including lung, breast and colon cancers |
| MDK | Midkine | 92.5 | 83.3 | [109] | Midkine is a heparin-binding growth factor, originally identified as a retinoic acid response gene that plays a key role in cell growth, survival, migration, angiogenesis and carcinogenesis |
| SCCA | Squamous cell carcinoma antigen | 56.1 | 74.9 | [110] | It is the member of the high molecular weight family of serine protease inhibitors, highly expressed in epithelial tumors, and protects tumor cells from apoptosis |
| Annexin A2 | 83.2 | 67.5 | [111] | A calcium-dependent phospholipid binding protein that is present on endothelial cells and on the surface of most epithelial cells. It is up-regulated in many tumor types and has multiple roles in various tumorigenic processes | |
| suPAR | Soluble urokinase plasminogen activator receptor | 76.0 | 90.4 | [112] | A glycophosphatidylinositol-linked membrane protein, a circulating form of the urokinase-type plasminogen activator receptor (uPAR). Recently, suPAR has been established as a biomarker of immune system activation and cancer metastasis level |
| TRXs | Thioredoxins | 74.9 | 87.5 | [113] | Thiol oxidoreductase is ubiquitously expressed and involved in several biological processes, such as regulation of protein status, apoptosis and proliferation, and protection against oxidative stress. |
Early and accurate diagnosis of HCC patients is critical for patient prognosis. Several studies have successfully identified promising biomarkers for the diagnosis of HCC. However, current studies suggest that a single biomarker alone may not have the best sensitivity and specificity for detecting HCC, especially for detecting early stage HCC. Several studies have reported that combining several biomarkers complements to improve the early diagnosis rate[84]. A study demonstrated that the sensitivity and specificity of serum GP73 for HCC was 74.6% and 97.4% respectively, while for AFP it was 58.2% and 85.3%. Combining both GP73 and AFP increased the sensitivity to 89.2% (95%CI: 86.7-91.5%) and its specificity to 85.2% (95%CI: 83.4%-86.4%)[84]. Adding clinical variables (such as age and gender) into the model based on biomarker combinations can further increase the predictive performance for HCC detection. It is worth noting that GALAD score, which is the combination of clinical factors (gender, age) and biomarkers (AFP, AFP-L3 and Des-carboxyprothrombin), has been validated to improve the performance of discerning between HCC and cirrhosis[85]. More randomized control trials to validate the optimal combination of biomarkers will contribute to better detection of early stage HCC.
About 80 percent of normal human microbes are concentrated in the intestinal tract, with a number of more than 100 trillion[86]. The symbiotic microbial flora in the human body is closely related to the health of the host[87]. including carcinogenesis. Intestinal microorganisms cause tumorigenesis by integrating carcinogenic genes into the host genome, affecting the stability of the host genome, breaking the balance between the host immune systems, and inhibiting the host immune system. Liver inflammation, increase and inhibition of anti-tumor immunity are affected by intestinal leakage, intestinal flora imbalance, microbe-associated molecular patterns and microbial metabolites, which promotes the occurrence of HCC[88-90].
Therefore, intestinal microorganisms are powerful biomarkers for early diagnosis of HCC. Bacteroides, Clostridium cluster XVIII,Prevotella and Oscillibacter were increased in HCC group compared to control group, while Prevotella, Streptococcus and Bifidobacterium were decreased in animal studies as Yamada et al[91], Li et al[92] reported. Escherichia coli was regarded as microbiome factor in clinical trials as Grat et al[93,94] reported, which was enriched in HCC patients. Escherichia-Shigella, Enterococcus, Proteus and Veillonella were increased in HBV-related HCC versus HBV-related HCC. On the other hand, Faecalibacterium, Ruminococcus, Ruminoclostridium, Pseudobutyrivibrio, Lachnoclostridium and Phascolarctobacterium were decreased as Liu et al[95] reported. Loomba et al[96] set a Random Forest model found that Proteobacteria, Escherichia coli and Firmicutes were microbial diagnostic markers. This model had a robust and statistically significant diagnostic accuracy, with AUC 93.60%. Currently, Ren et al[97] reported that faecal microbial diversity was increased from cirrhosis to early HCC. Phylum Actinobacteria was increased in early HCC vs cirrhosis. And 13 genera including Gemmiger and Parabacteroides were enriched in early HCC versus cirrhosis. Butyrate-producing genera were decreased, while genera producing-lipopolysaccharide were increased in early HCC versus controls. The AUC of this diagnostic model was 80.64%.
Some biomarkers mentioned above have been validated their ability of HCC diagnosis in different phases of clinical trials. Pepe et al[83] summarized five phases of biomarker development and the only biomarker that has undergone five phases of HCC biomarker development is AFP[98]. Three biomarkers, OPN[99], MDK[100] and GALAD score[85], have passed phase III validation. More biomarkers are under phase II biomarker development, such as AFP-L3[9], Dickkopf-1[101], and Glypican-3[102], etc. The description of the phases (I, II, III) of biomarker development and the corresponding candidate biomarkers are shown in Table 2.
| Phases | Description | Biomarkers | Ref. |
| Phase I | Preclinical exploratory studies | miRNA | [114] |
| Metabolomic | [115] | ||
| Cell-free DNA | [116] | ||
| Phase II | Clinical essay and validation | AFP-L3 | [9] |
| Dickkopf-1 | [101] | ||
| DCP(Des-carboxyprothrombin) | [9] | ||
| GPC3 (Glypican-3) | [102] | ||
| Golgi protein-73 | [117] | ||
| Squamous cell carcinoma antigen | [118] | ||
| miRNA | [114] | ||
| Phase III | Retrospective longitudinal studies | Osteopontin | [99] |
| Midkine | [100] | ||
| GALAD score | [85] |
Historically verification has been limited due to the lack of large-scale vertical cohorts and available test samples. Fortunately, serial samples from several longitudinal cohorts in the United States are being collected to allow for extensive validation of these biomarkers[103]. In the next few years, through the improved big data techniques and appropriate validation, the biomarker-based precision screening method may become the main method for early detection of HCC.
Theoretically, the human body is an exquisitely organized system, while blood is responsible for carrying the substances from tissues to tissues, to maintain the complex functions. During carcinogenesis, the cells, organelles, macromolecules and metabolites are inevitably altered to different degrees. Due to the rapid development of high-throughput technologies, HCC biomarker screening is now feasible and necessary, by detecting these cells, organelles, macromolecules and metabolites. However, the genetic and environmental heterogeneity makes the carcinogenesis of individuals unique. Therefore, the alteration on these biological levels varies, which makes it difficult to develop an almighty biomarker for diagnosis. Technically, due to the limitation of detection methods and the nature of targets, each method has its own drawbacks and advantages. Plus, it is taken for granted that early-staged HCC has less huge impact on the body, which makes the early HCC diagnosis difficult. Thus, HCC diagnosis on different platforms is worth trying.
Protein biomarkers for HCC is mostly widely recognized in clinical practice, However, the diagnostic value of several biomarkers has shown inconsistent results. For example, the sensitivity and specificity of DCP reported by Sawada et al[23] was 77% and 82%, while it was 61% and 70% as reported by Marrero et al[9], which may result from different parameter selection or system errors.
ctDNA analysis is convenient, non-invasive and has a precise diagnostic capability. But serious technical hurdles in the detection and analysis of ctDNA, there has been limited progress in determining its clinical applicability for HCC diagnosis. The low levels of ctDNA, HCC heterogeneity and poorly characterized DNA alterations in HCC are the three main challenges for using ctDNA technology for the early detection of HCC[18].
CTCs are effective tools for diagnosing HCC as they are the “seeds” of tumors. One study[37] detected low levels of CTCs in two of 12 HBV patients, and subsequently detected small HCC tumors during the next 5 mo. This suggested that CTCs may be a valuable tool for HCC early-diagnosis. But the precision of HCC diagnosis using CTCs varies across cohorts and studies[33,34,104]. Exosomal cargo is protected from degradation by its lipid bilayer which makes it a good HCC diagnostic tool. Although several technology platforms have been developed for exosome enrichment, there is still no standard separation technology that is widely used[105]. Plus, the expensive extraction methods hinders the study of exosomes[40]. Cheaper and faster extraction methods are needed to fully explore its utility. Although several studies have used paneled metabolites for HCC screening, there have been no new markers or panels that have been clinically utilized. This is because of the absence of standard sample processing and analytical procedures that has led to metabolomics studies being unable to be replicated[106]. Secondly the metabolomics detection platforms are not mature enough to robustly and accurately detect metabolites.
Rapid high-throughput sequencing makes HCC diagnosis, especially early HCC diagnosis more feasible, and studies concerning omics data-based HCC diagnosis is still increasing. The most studies collected samples with a small sample size from single or few cohorts. The sample processing steps are different in cohorts, and the analyzing method even in same platforms still varies. These studies limited the clinical utilization of biomarkers. It is believed that with the development and maturity of techniques, omics data-based biomarker screening will finally become clinically utilized tool for cancers, including but not limited to HCC.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Aoki T, Chau GY, Lee HC, Tchilikidi KY, Vradelis S S-Editor: Yan JP L-Editor: Tian-Qi Wang E-Editor: Wu YXJ
| 1. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 55853] [Article Influence: 7979.0] [Reference Citation Analysis (132)] |
| 2. | Singal AG, El-Serag HB. Hepatocellular Carcinoma From Epidemiology to Prevention: Translating Knowledge into Practice. Clin Gastroenterol Hepatol. 2015;13:2140-2151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 394] [Cited by in RCA: 408] [Article Influence: 40.8] [Reference Citation Analysis (0)] |
| 3. | Gomes MA, Priolli DG, Tralhão JG, Botelho MF. Hepatocellular carcinoma: Epidemiology, biology, diagnosis, and therapies. Rev Assoc Med Bras (1992). 2013;59:514-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 4. | Ružić M, Pellicano R, Fabri M, Luzza F, Boccuto L, Brkić S, Abenavoli L. Hepatitis C virus-induced hepatocellular carcinoma: A narrative review. Panminerva Med. 2018;60:185-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 5. | Fu J, Wang H. Precision diagnosis and treatment of liver cancer in China. Cancer Lett. 2018;412:283-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 224] [Article Influence: 32.0] [Reference Citation Analysis (1)] |
| 6. | Zeng H, Zheng R, Guo Y, Zhang S, Zou X, Wang N, Zhang L, Tang J, Chen J, Wei K, Huang S, Wang J, Yu L, Zhao D, Song G, Chen J, Shen Y, Yang X, Gu X, Jin F, Li Q, Li Y, Ge H, Zhu F, Dong J, Guo G, Wu M, Du L, Sun X, He Y, Coleman MP, Baade P, Chen W, Yu XQ. Cancer survival in China, 2003-2005: A population-based study. Int J Cancer. 2015;136:1921-1930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 415] [Cited by in RCA: 499] [Article Influence: 49.9] [Reference Citation Analysis (0)] |
| 7. | Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet. 2012;379:1245-1255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3249] [Cited by in RCA: 3597] [Article Influence: 276.7] [Reference Citation Analysis (4)] |
| 8. | Chedid MF, Kruel CRP, Pinto MA, Grezzana-Filho TJM, Leipnitz I, Kruel CDP, Scaffaro LA, Chedid AD. Hepatocellular carcinoma: Diagnosis and operative management. Arq Bras Cir Dig. 2017;30:272-278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 9. | Marrero JA, Feng Z, Wang Y, Nguyen MH, Befeler AS, Roberts LR, Reddy KR, Harnois D, Llovet JM, Normolle D, Dalhgren J, Chia D, Lok AS, Wagner PD, Srivastava S, Schwartz M. Alpha-fetoprotein, des-gamma carboxyprothrombin, and lectin-bound alpha-fetoprotein in early hepatocellular carcinoma. Gastroenterology. 2009;137:110-118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 583] [Cited by in RCA: 571] [Article Influence: 35.7] [Reference Citation Analysis (0)] |
| 10. | Mitchell PS, Parkin RK, Kroh EM, Fritz BR, Wyman SK, Pogosova-Agadjanyan EL, Peterson A, Noteboom J, O'Briant KC, Allen A, Lin DW, Urban N, Drescher CW, Knudsen BS, Stirewalt DL, Gentleman R, Vessella RL, Nelson PS, Martin DB, Tewari M. Circulating microRNAs as stable blood-based markers for cancer detection. Proc Natl Acad Sci USA. 2008;105:10513-10518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5636] [Cited by in RCA: 6315] [Article Influence: 371.5] [Reference Citation Analysis (0)] |
| 11. | Jia X, Liu J, Gao Y, Huang Y, Du Z. Diagnosis accuracy of serum glypican-3 in patients with hepatocellular carcinoma: A systematic review with meta-analysis. Arch Med Res. 2014;45:580-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Li J, Wang T, Jin B, Li W, Wang Z, Zhang H, Song Y, Li N. Diagnosis accuracy of serum glypican-3 level in patients with hepatocellular carcinoma: A systematic review with meta-analysis. Int J Biol Markers. 2018;1724600818784409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Fattovich G, Stroffolini T, Zagni I, Donato F. Hepatocellular carcinoma in cirrhosis: Incidence and risk factors. Gastroenterology. 2004;127:S35-S50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1691] [Cited by in RCA: 1793] [Article Influence: 85.4] [Reference Citation Analysis (2)] |
| 14. | Arzumanyan A, Reis HM, Feitelson MA. Pathogenic mechanisms in HBV- and HCV-associated hepatocellular carcinoma. Nat Rev Cancer. 2013;13:123-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 581] [Cited by in RCA: 634] [Article Influence: 52.8] [Reference Citation Analysis (0)] |
| 15. | Tu T, Budzinska MA, Maczurek AE, Cheng R, Di Bartolomeo A, Warner FJ, McCaughan GW, McLennan SV, Shackel NA. Novel aspects of the liver microenvironment in hepatocellular carcinoma pathogenesis and development. Int J Mol Sci. 2014;15:9422-9458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 64] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 16. | Schork NJ. Personalized medicine: Time for one-person trials. Nature. 2015;520:609-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 693] [Cited by in RCA: 702] [Article Influence: 70.2] [Reference Citation Analysis (0)] |
| 17. | Cyranoski D. China embraces precision medicine on a massive scale. Nature. 2016;529:9-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 18. | Tang JC, Feng YL, Guo T, Xie AY, Cai XJ. Circulating tumor DNA in hepatocellular carcinoma: Trends and challenges. Cell Biosci. 2016;6:32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 19. | Huang ZH, Hu Y, Hua D, Wu YY, Song MX, Cheng ZH. Quantitative analysis of multiple methylated genes in plasma for the diagnosis and prognosis of hepatocellular carcinoma. Exp Mol Pathol. 2011;91:702-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 88] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 20. | Zhou J, Yu L, Gao X, Hu J, Wang J, Dai Z, Wang JF, Zhang Z, Lu S, Huang X, Wang Z, Qiu S, Wang X, Yang G, Sun H, Tang Z, Wu Y, Zhu H, Fan J. Plasma microRNA panel to diagnose hepatitis B virus-related hepatocellular carcinoma. J Clin Oncol. 2011;29:4781-4788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 430] [Cited by in RCA: 498] [Article Influence: 35.6] [Reference Citation Analysis (0)] |
| 21. | Chen X, Ba Y, Ma L, Cai X, Yin Y, Wang K, Guo J, Zhang Y, Chen J, Guo X, Li Q, Li X, Wang W, Zhang Y, Wang J, Jiang X, Xiang Y, Xu C, Zheng P, Zhang J, Li R, Zhang H, Shang X, Gong T, Ning G, Wang J, Zen K, Zhang J, Zhang CY. Characterization of microRNAs in serum: A novel class of biomarkers for diagnosis of cancer and other diseases. Cell Res. 2008;18:997-1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3218] [Cited by in RCA: 3554] [Article Influence: 209.1] [Reference Citation Analysis (0)] |
| 22. | Li L, Chen J, Chen X, Tang J, Guo H, Wang X, Qian J, Luo G, He F, Lu X, Ding Y, Yang Y, Huang W, Hou G, Lin X, Ouyang Q, Li H, Wang R, Jiang F, Pu R, Lu J, Jin M, Tan Y, Gonzalez FJ, Cao G, Wu M, Wen H, Wu T, Jin L, Chen L, Wang H. Serum miRNAs as predictive and preventive biomarker for pre-clinical hepatocellular carcinoma. Cancer Lett. 2016;373:234-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 23. | Sawada Y, Yoshikawa T, Nobuoka D, Shirakawa H, Kuronuma T, Motomura Y, Mizuno S, Ishii H, Nakachi K, Konishi M, Nakagohri T, Takahashi S, Gotohda N, Takayama T, Yamao K, Uesaka K, Furuse J, Kinoshita T, Nakatsura T. Phase I trial of a glypican-3-derived peptide vaccine for advanced hepatocellular carcinoma: Immunologic evidence and potential for improving overall survival. Clin Cancer Res. 2012;18:3686-3696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 233] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 24. | Yin CQ, Yuan CH, Qu Z, Guan Q, Chen H, Wang FB. Liquid Biopsy of Hepatocellular Carcinoma: Circulating Tumor-Derived Biomarkers. Dis Markers. 2016;2016:1427849. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 25. | Mann J, Reeves HL, Feldstein AE. Liquid biopsy for liver diseases. Gut. 2018;67:2204-2212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 78] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 26. | Alix-Panabières C, Pantel K. Challenges in circulating tumour cell research. Nat Rev Cancer. 2014;14:623-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 917] [Cited by in RCA: 1013] [Article Influence: 92.1] [Reference Citation Analysis (0)] |
| 27. | Allard WJ, Matera J, Miller MC, Repollet M, Connelly MC, Rao C, Tibbe AG, Uhr JW, Terstappen LW. Tumor cells circulate in the peripheral blood of all major carcinomas but not in healthy subjects or patients with nonmalignant diseases. Clin Cancer Res. 2004;10:6897-6904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1810] [Cited by in RCA: 1955] [Article Influence: 97.8] [Reference Citation Analysis (0)] |
| 28. | Wang Z, Luo L, Cheng Y, He G, Peng B, Gao Y, Jiang ZS, Pan M. Correlation Between Postoperative Early Recurrence of Hepatocellular Carcinoma and Mesenchymal Circulating Tumor Cells in Peripheral Blood. J Gastrointest Surg. 2018;22:633-639. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 57] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 29. | Vona G, Sabile A, Louha M, Sitruk V, Romana S, Schütze K, Capron F, Franco D, Pazzagli M, Vekemans M, Lacour B, Bréchot C, Paterlini-Bréchot P. Isolation by size of epithelial tumor cells: A new method for the immunomorphological and molecular characterization of circulatingtumor cells. Am J Pathol. 2000;156:57-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 827] [Cited by in RCA: 801] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 30. | Xu W, Cao L, Chen L, Li J, Zhang XF, Qian HH, Kang XY, Zhang Y, Liao J, Shi LH, Yang YF, Wu MC, Yin ZF. Isolation of circulating tumor cells in patients with hepatocellular carcinoma using a novel cell separation strategy. Clin Cancer Res. 2011;17:3783-3793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 122] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 31. | Sequist LV, Nagrath S, Toner M, Haber DA, Lynch TJ. The CTC-chip: An exciting new tool to detect circulating tumor cells in lung cancer patients. J Thorac Oncol. 2009;4:281-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 144] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 32. | Kalinich M, Bhan I, Kwan TT, Miyamoto DT, Javaid S, LiCausi JA, Milner JD, Hong X, Goyal L, Sil S, Choz M, Ho U, Kapur R, Muzikansky A, Zhang H, Weitz DA, Sequist LV, Ryan DP, Chung RT, Zhu AX, Isselbacher KJ, Ting DT, Toner M, Maheswaran S, Haber DA. An RNA-based signature enables high specificity detection of circulating tumor cells in hepatocellular carcinoma. Proc Natl Acad Sci USA. 2017;114:1123-1128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 129] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 33. | Guo W, Yang XR, Sun YF, Shen MN, Ma XL, Wu J, Zhang CY, Zhou Y, Xu Y, Hu B, Zhang X, Zhou J, Fan J. Clinical significance of EpCAM mRNA-positive circulating tumor cells in hepatocellular carcinoma by an optimized negative enrichment and qRT-PCR-based platform. Clin Cancer Res. 2014;20:4794-4805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 93] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 34. | Guo W, Sun YF, Shen MN, Ma XL, Wu J, Zhang CY, Zhou Y, Xu Y, Hu B, Zhang M, Wang G, Chen WQ, Guo L, Lu RQ, Zhou CH, Zhang X, Shi YH, Qiu SJ, Pan BS, Cao Y, Zhou J, Yang XR, Fan J. Circulating Tumor Cells with Stem-Like Phenotypes for Diagnosis, Prognosis, and Therapeutic Response Evaluation in Hepatocellular Carcinoma. Clin Cancer Res. 2018;24:2203-2213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 106] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 35. | Sun YF, Xu Y, Yang XR, Guo W, Zhang X, Qiu SJ, Shi RY, Hu B, Zhou J, Fan J. Circulating stem cell-like epithelial cell adhesion molecule-positive tumor cells indicate poor prognosis of hepatocellular carcinoma after curative resection. Hepatology. 2013;57:1458-1468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 305] [Article Influence: 25.4] [Reference Citation Analysis (0)] |
| 36. | Schulze K, Gasch C, Staufer K, Nashan B, Lohse AW, Pantel K, Riethdorf S, Wege H. Presence of EpCAM-positive circulating tumor cells as biomarker for systemic disease strongly correlates to survival in patients with hepatocellular carcinoma. Int J Cancer. 2013;133:2165-2171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 192] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 37. | Qi LN, Xiang BD, Wu FX, Ye JZ, Zhong JH, Wang YY, Chen YY, Chen ZS, Ma L, Chen J, Gong WF, Han ZG, Lu Y, Shang JJ, Li LQ. Circulating Tumor Cells Undergoing EMT Provide a Metric for Diagnosis and Prognosis of Patients with Hepatocellular Carcinoma. Cancer Res. 2018;78:4731-4744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 214] [Article Influence: 30.6] [Reference Citation Analysis (0)] |
| 38. | Keller S, Sanderson MP, Stoeck A, Altevogt P. Exosomes: From biogenesis and secretion to biological function. Immunol Lett. 2006;107:102-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 592] [Cited by in RCA: 671] [Article Influence: 35.3] [Reference Citation Analysis (0)] |
| 39. | Chaput N, Théry C. Exosomes: Immune properties and potential clinical implementations. Semin Immunopathol. 2011;33:419-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 417] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 40. | Chen R, Xu X, Tao Y, Qian Z, Yu Y. Exosomes in hepatocellular carcinoma: A new horizon. Cell Commun Signal. 2019;17:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 100] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 41. | Xu H, Chen Y, Dong X, Wang X. Serum Exosomal Long Noncoding RNAs ENSG00000258332.1 and LINC00635 for the Diagnosis and Prognosis of Hepatocellular Carcinoma. Cancer Epidemiol Biomarkers Prev. 2018;27:710-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 127] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 42. | Wang Y, Zhang C, Zhang P, Guo G, Jiang T, Zhao X, Jiang J, Huang X, Tong H, Tian Y. Serum exosomal microRNAs combined with alpha-fetoprotein as diagnostic markers of hepatocellular carcinoma. Cancer Med. 2018;7:1670-1679. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 124] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 43. | Sun L, Su Y, Liu X, Xu M, Chen X, Zhu Y, Guo Z, Bai T, Dong L, Wei C, Cai X, He B, Pan Y, Sun H, Wang S. Serum and exosome long non coding RNAs as potential biomarkers for hepatocellular carcinoma. J Cancer. 2018;9:2631-2639. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 79] [Cited by in RCA: 105] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 44. | Xu H, Dong X, Chen Y, Wang X. Serum exosomal hnRNPH1 mRNA as a novel marker for hepatocellular carcinoma. Clin Chem Lab Med. 2018;56:479-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 96] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 45. | Cui Y, Xu HF, Liu MY, Xu YJ, He JC, Zhou Y, Cang SD. Mechanism of exosomal microRNA-224 in development of hepatocellular carcinoma and its diagnostic and prognostic value. World J Gastroenterol. 2019;25:1890-1898. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 60] [Cited by in RCA: 80] [Article Influence: 13.3] [Reference Citation Analysis (1)] |
| 46. | Lee YR, Kim G, Tak WY, Jang SY, Kweon YO, Park JG, Lee HW, Han YS, Chun JM, Park SY, Hur K. Circulating exosomal noncoding RNAs as prognostic biomarkers in human hepatocellular carcinoma. Int J Cancer. 2019;144:1444-1452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 202] [Article Influence: 28.9] [Reference Citation Analysis (0)] |
| 47. | Sugimachi K, Matsumura T, Hirata H, Uchi R, Ueda M, Ueo H, Shinden Y, Iguchi T, Eguchi H, Shirabe K, Ochiya T, Maehara Y, Mimori K. Identification of a bona fide microRNA biomarker in serum exosomes that predicts hepatocellular carcinoma recurrence after liver transplantation. Br J Cancer. 2015;112:532-538. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 212] [Cited by in RCA: 243] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 48. | Tchou JC, Lin X, Freije D, Isaacs WB, Brooks JD, Rashid A, De Marzo AM, Kanai Y, Hirohashi S, Nelson WG. GSTP1 CpG island DNA hypermethylation in hepatocellular carcinomas. Int J Oncol. 2000;16:663-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 30] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 49. | Zhong S, Tang MW, Yeo W, Liu C, Lo YM, Johnson PJ. Silencing of GSTP1 gene by CpG island DNA hypermethylation in HBV-associated hepatocellular carcinomas. Clin Cancer Res. 2002;8:1087-1092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 50. | Matsuda Y, Ichida T, Matsuzawa J, Sugimura K, Asakura H. p16(INK4) is inactivated by extensive CpG methylation in human hepatocellular carcinoma. Gastroenterology. 1999;116:394-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 145] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 51. | Roncalli M, Bianchi P, Bruni B, Laghi L, Destro A, Di Gioia S, Gennari L, Tommasini M, Malesci A, Coggi G. Methylation framework of cell cycle gene inhibitors in cirrhosis and associated hepatocellular carcinoma. Hepatology. 2002;36:427-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 87] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 52. | Wang J, Qin Y, Li B, Sun Z, Yang B. Detection of aberrant promoter methylation of GSTP1 in the tumor and serum of Chinese human primary hepatocellular carcinoma patients. Clin Biochem. 2006;39:344-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 70] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 53. | Wong IH, Lo YM, Yeo W, Lau WY, Johnson PJ. Frequent p15 promoter methylation in tumor and peripheral blood from hepatocellular carcinoma patients. Clin Cancer Res. 2000;6:3516-3521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 54. | Wong IH, Lo YM, Zhang J, Liew CT, Ng MH, Wong N, Lai PB, Lau WY, Hjelm NM, Johnson PJ. Detection of aberrant p16 methylation in the plasma and serum of liver cancer patients. Cancer Res. 1999;59:71-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 55. | Ren N, Qin LX, Tu H, Liu YK, Zhang BH, Tang ZY. The prognostic value of circulating plasma DNA level and its allelic imbalance on chromosome 8p in patients with hepatocellular carcinoma. J Cancer Res Clin Oncol. 2006;132:399-407. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 58] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 56. | Qin LX, Tang ZY, Sham JS, Ma ZC, Ye SL, Zhou XD, Wu ZQ, Trent JM, Guan XY. The association of chromosome 8p deletion and tumor metastasis in human hepatocellular carcinoma. Cancer Res. 1999;59:5662-5665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 57. | Kinugasa H, Nouso K, Miyahara K, Morimoto Y, Dohi C, Tsutsumi K, Kato H, Matsubara T, Okada H, Yamamoto K. Detection of K-ras gene mutation by liquid biopsy in patients with pancreatic cancer. Cancer. 2015;121:2271-2280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 181] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 58. | Takai E, Totoki Y, Nakamura H, Morizane C, Nara S, Hama N, Suzuki M, Furukawa E, Kato M, Hayashi H, Kohno T, Ueno H, Shimada K, Okusaka T, Nakagama H, Shibata T, Yachida S. Clinical utility of circulating tumor DNA for molecular assessment in pancreatic cancer. Sci Rep. 2015;5:18425. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 134] [Cited by in RCA: 149] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 59. | Kirk GD, Camus-Randon AM, Mendy M, Goedert JJ, Merle P, Trépo C, Bréchot C, Hainaut P, Montesano R. Ser-249 p53 mutations in plasma DNA of patients with hepatocellular carcinoma from The Gambia. J Natl Cancer Inst. 2000;92:148-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 115] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 60. | Hosny G, Farahat N, Tayel H, Hainaut P. Ser-249 TP53 and CTNNB1 mutations in circulating free DNA of Egyptian patients with hepatocellular carcinoma versus chronic liver diseases. Cancer Lett. 2008;264:201-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 61. | Guichard C, Amaddeo G, Imbeaud S, Ladeiro Y, Pelletier L, Maad IB, Calderaro J, Bioulac-Sage P, Letexier M, Degos F, Clément B, Balabaud C, Chevet E, Laurent A, Couchy G, Letouzé E, Calvo F, Zucman-Rossi J. Integrated analysis of somatic mutations and focal copy-number changes identifies key genes and pathways in hepatocellular carcinoma. Nat Genet. 2012;44:694-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 962] [Cited by in RCA: 1150] [Article Influence: 88.5] [Reference Citation Analysis (0)] |
| 62. | Fujimoto A, Furuta M, Totoki Y, Tsunoda T, Kato M, Shiraishi Y, Tanaka H, Taniguchi H, Kawakami Y, Ueno M, Gotoh K, Ariizumi S, Wardell CP, Hayami S, Nakamura T, Aikata H, Arihiro K, Boroevich KA, Abe T, Nakano K, Maejima K, Sasaki-Oku A, Ohsawa A, Shibuya T, Nakamura H, Hama N, Hosoda F, Arai Y, Ohashi S, Urushidate T, Nagae G, Yamamoto S, Ueda H, Tatsuno K, Ojima H, Hiraoka N, Okusaka T, Kubo M, Marubashi S, Yamada T, Hirano S, Yamamoto M, Ohdan H, Shimada K, Ishikawa O, Yamaue H, Chayama K, Miyano S, Aburatani H, Shibata T, Nakagawa H. Whole-genome mutational landscape and characterization of noncoding and structural mutations in liver cancer. Nat Genet. 2016;48:500-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 465] [Cited by in RCA: 538] [Article Influence: 59.8] [Reference Citation Analysis (0)] |
| 63. | Cancer Genome Atlas Research Network. Electronic address: wheeler@bcm.edu.; Cancer Genome Atlas Research Network. Comprehensive and Integrative Genomic Characterization of Hepatocellular Carcinoma. Cell. 2017;169:1327-1341.e23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1578] [Cited by in RCA: 1732] [Article Influence: 216.5] [Reference Citation Analysis (1)] |
| 64. | Liao W, Mao Y, Ge P, Yang H, Xu H, Lu X, Sang X, Zhong S. Value of quantitative and qualitative analyses of circulating cell-free DNA as diagnostic tools for hepatocellular carcinoma: A meta-analysis. Medicine (Baltimore). 2015;94:e722. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 55] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 65. | Wen Y, Han J, Chen J, Dong J, Xia Y, Liu J, Jiang Y, Dai J, Lu J, Jin G, Han J, Wei Q, Shen H, Sun B, Hu Z. Plasma miRNAs as early biomarkers for detecting hepatocellular carcinoma. Int J Cancer. 2015;137:1679-1690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 173] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 66. | Okajima W, Komatsu S, Ichikawa D, Miyamae M, Kawaguchi T, Hirajima S, Ohashi T, Imamura T, Kiuchi J, Arita T, Konishi H, Shiozaki A, Moriumura R, Ikoma H, Okamoto K, Taniguchi H, Itoh Y, Otsuji E. Circulating microRNA profiles in plasma: Identification of miR-224 as a novel diagnostic biomarker in hepatocellular carcinoma independent of hepatic function. Oncotarget. 2016;7:53820-53836. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 51] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 67. | Shi BM, Lu W, Ji K, Wang YF, Xiao S, Wang XY. Study on the value of serum miR-106b for the early diagnosis of hepatocellular carcinoma. World J Gastroenterol. 2017;23:3713-3720. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 68. | Amr KS, Ezzat WM, Elhosary YA, Hegazy AE, Fahim HH, Kamel RR. The potential role of miRNAs 21 and 199-a in early diagnosis of hepatocellular carcinoma. Gene. 2016;575:66-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 69. | Wang X, Zhang J, Zhou L, Lu P, Zheng ZG, Sun W, Wang JL, Yang XS, Li XL, Xia N, Zhang N, Dou KF. Significance of serum microRNA-21 in diagnosis of hepatocellular carcinoma (HCC): Clinical analyses of patients and an HCC rat model. Int J Clin Exp Pathol. 2015;8:1466-1478. [PubMed] |
| 70. | Li J, Wang X, Tang J, Jiang R, Zhang W, Ji J, Sun B. HULC and Linc00152 Act as Novel Biomarkers in Predicting Diagnosis of Hepatocellular Carcinoma. Cell Physiol Biochem. 2015;37:687-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 165] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 71. | Yuan W, Sun Y, Liu L, Zhou B, Wang S, Gu D. Circulating LncRNAs Serve as Diagnostic Markers for Hepatocellular Carcinoma. Cell Physiol Biochem. 2017;44:125-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 60] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 72. | Wang C, Ren T, Wang K, Zhang S, Liu S, Chen H, Yang P. Identification of long non-coding RNA p34822 as a potential plasma biomarker for the diagnosis of hepatocellular carcinoma. Sci China Life Sci. 2017;60:1047-1050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 73. | Wishart DS, Tzur D, Knox C, Eisner R, Guo AC, Young N, Cheng D, Jewell K, Arndt D, Sawhney S, Fung C, Nikolai L, Lewis M, Coutouly MA, Forsythe I, Tang P, Shrivastava S, Jeroncic K, Stothard P, Amegbey G, Block D, Hau DD, Wagner J, Miniaci J, Clements M, Gebremedhin M, Guo N, Zhang Y, Duggan GE, Macinnis GD, Weljie AM, Dowlatabadi R, Bamforth F, Clive D, Greiner R, Li L, Marrie T, Sykes BD, Vogel HJ, Querengesser L. HMDB: The Human Metabolome Database. Nucleic Acids Res. 2007;35:D521-D526. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2058] [Cited by in RCA: 2245] [Article Influence: 124.7] [Reference Citation Analysis (0)] |
| 74. | Guo W, Tan HY, Wang N, Wang X, Feng Y. Deciphering hepatocellular carcinoma through metabolomics: From biomarker discovery to therapy evaluation. Cancer Manag Res. 2018;10:715-734. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 75. | Cox IJ, Aliev AE, Crossey MM, Dawood M, Al-Mahtab M, Akbar SM, Rahman S, Riva A, Williams R, Taylor-Robinson SD. Urinary nuclear magnetic resonance spectroscopy of a Bangladeshi cohort with hepatitis-B hepatocellular carcinoma: A biomarker corroboration study. World J Gastroenterol. 2016;22:4191-4200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 23] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 76. | Di Poto C, Ferrarini A, Zhao Y, Varghese RS, Tu C, Zuo Y, Wang M, Nezami Ranjbar MR, Luo Y, Zhang C, Desai CS, Shetty K, Tadesse MG, Ressom HW. Metabolomic Characterization of Hepatocellular Carcinoma in Patients with Liver Cirrhosis for Biomarker Discovery. Cancer Epidemiol Biomarkers Prev. 2017;26:675-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 77. | Luo P, Yin P, Hua R, Tan Y, Li Z, Qiu G, Yin Z, Xie X, Wang X, Chen W, Zhou L, Wang X, Li Y, Chen H, Gao L, Lu X, Wu T, Wang H, Niu J, Xu G. A Large-scale, multicenter serum metabolite biomarker identification study for the early detection of hepatocellular carcinoma. Hepatology. 2017;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 193] [Cited by in RCA: 284] [Article Influence: 40.6] [Reference Citation Analysis (0)] |
| 78. | Lu Y, Li N, Gao L, Xu YJ, Huang C, Yu K, Ling Q, Cheng Q, Chen S, Zhu M, Fang J, Chen M, Ong CN. Acetylcarnitine Is a Candidate Diagnostic and Prognostic Biomarker of Hepatocellular Carcinoma. Cancer Res. 2016;76:2912-2920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 80] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 79. | Liu Y, Hong Z, Tan G, Dong X, Yang G, Zhao L, Chen X, Zhu Z, Lou Z, Qian B, Zhang G, Chai Y. NMR and LC/MS-based global metabolomics to identify serum biomarkers differentiating hepatocellular carcinoma from liver cirrhosis. Int J Cancer. 2014;135:658-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 105] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 80. | Zeng J, Yin P, Tan Y, Dong L, Hu C, Huang Q, Lu X, Wang H, Xu G. Metabolomics study of hepatocellular carcinoma: Discovery and validation of serum potential biomarkers by using capillary electrophoresis-mass spectrometry. J Proteome Res. 2014;13:3420-3431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 102] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 81. | Liang Q, Liu H, Wang C, Li B. Phenotypic Characterization Analysis of Human Hepatocarcinoma by Urine Metabolomics Approach. Sci Rep. 2016;6:19763. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 82. | Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol. 2004;130:417-422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 960] [Cited by in RCA: 945] [Article Influence: 45.0] [Reference Citation Analysis (1)] |
| 83. | Pepe MS, Etzioni R, Feng Z, Potter JD, Thompson ML, Thornquist M, Winget M, Yasui Y. Phases of biomarker development for early detection of cancer. J Natl Cancer Inst. 2001;93:1054-1061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1150] [Cited by in RCA: 1140] [Article Influence: 47.5] [Reference Citation Analysis (0)] |
| 84. | Xu WJ, Guo BL, Han YG, Shi L, Ma WS. Diagnostic value of alpha-fetoprotein-L3 and Golgi protein 73 in hepatocellular carcinomas with low AFP levels. Tumour Biol. 2014;35:12069-12074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 85. | Johnson PJ, Pirrie SJ, Cox TF, Berhane S, Teng M, Palmer D, Morse J, Hull D, Patman G, Kagebayashi C, Hussain S, Graham J, Reeves H, Satomura S. The detection of hepatocellular carcinoma using a prospectively developed and validated model based on serological biomarkers. Cancer Epidemiol Biomarkers Prev. 2014;23:144-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 229] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 86. | Wan MLY, El-Nezami H. Targeting gut microbiota in hepatocellular carcinoma: Probiotics as a novel therapy. Hepatobiliary Surg Nutr. 2018;7:11-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 87] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 87. | Garrett WS. Cancer and the microbiota. Science. 2015;348:80-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 901] [Cited by in RCA: 975] [Article Influence: 97.5] [Reference Citation Analysis (1)] |
| 88. | Yu LX, Schwabe RF. The gut microbiome and liver cancer: Mechanisms and clinical translation. Nat Rev Gastroenterol Hepatol. 2017;14:527-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 334] [Cited by in RCA: 414] [Article Influence: 51.8] [Reference Citation Analysis (0)] |
| 89. | Tripathi A, Debelius J, Brenner DA, Karin M, Loomba R, Schnabl B, Knight R. The gut-liver axis and the intersection with the microbiome. Nat Rev Gastroenterol Hepatol. 2018;15:397-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 872] [Cited by in RCA: 975] [Article Influence: 139.3] [Reference Citation Analysis (0)] |
| 90. | Tsilimigras MC, Fodor A, Jobin C. Carcinogenesis and therapeutics: The microbiota perspective. Nat Microbiol. 2017;2:17008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 104] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 91. | Yamada S, Takashina Y, Watanabe M, Nagamine R, Saito Y, Kamada N, Saito H. Bile acid metabolism regulated by the gut microbiota promotes non-alcoholic steatohepatitis-associated hepatocellular carcinoma in mice. Oncotarget. 2018;9:9925-9939. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 102] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 92. | Li J, Sung CY, Lee N, Ni Y, Pihlajamäki J, Panagiotou G, El-Nezami H. Probiotics modulated gut microbiota suppresses hepatocellular carcinoma growth in mice. Proc Natl Acad Sci U S A. 2016;113:E1306-E1315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 425] [Article Influence: 47.2] [Reference Citation Analysis (0)] |
| 93. | Grąt M, Wronka KM, Krasnodębski M, Masior Ł, Lewandowski Z, Kosińska I, Grąt K, Stypułkowski J, Rejowski S, Wasilewicz M, Gałęcka M, Szachta P, Krawczyk M. Profile of Gut Microbiota Associated With the Presence of Hepatocellular Cancer in Patients With Liver Cirrhosis. Transplant Proc. 2016;48:1687-1691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 145] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 94. | Gupta H, Youn GS, Shin MJ, Suk KT. Role of Gut Microbiota in Hepatocarcinogenesis. Microorganisms. 2019;7:pii: E121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 87] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 95. | Liu Q, Li F, Zhuang Y, Xu J, Wang J, Mao X, Zhang Y, Liu X. Alteration in gut microbiota associated with hepatitis B and non-hepatitis virus related hepatocellular carcinoma. Gut Pathog. 2019;11:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 148] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 96. | Loomba R, Seguritan V, Li W, Long T, Klitgord N, Bhatt A, Dulai PS, Caussy C, Bettencourt R, Highlander SK, Jones MB, Sirlin CB, Schnabl B, Brinkac L, Schork N, Chen CH, Brenner DA, Biggs W, Yooseph S, Venter JC, Nelson KE. Gut Microbiome-Based Metagenomic Signature for Non-invasive Detection of Advanced Fibrosis in Human Nonalcoholic Fatty Liver Disease. Cell Metab. 2017;25:1054-1062.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 551] [Cited by in RCA: 754] [Article Influence: 94.3] [Reference Citation Analysis (0)] |
| 97. | Ren Z, Li A, Jiang J, Zhou L, Yu Z, Lu H, Xie H, Chen X, Shao L, Zhang R, Xu S, Zhang H, Cui G, Chen X, Sun R, Wen H, Lerut JP, Kan Q, Li L, Zheng S. Gut microbiome analysis as a tool towards targeted non-invasive biomarkers for early hepatocellular carcinoma. Gut. 2019;68:1014-1023. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 542] [Cited by in RCA: 509] [Article Influence: 84.8] [Reference Citation Analysis (0)] |
| 98. | Bruix J, Sherman M; American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: An update. Hepatology. 2011;53:1020-1022. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5972] [Cited by in RCA: 6573] [Article Influence: 469.5] [Reference Citation Analysis (1)] |
| 99. | Shang S, Plymoth A, Ge S, Feng Z, Rosen HR, Sangrajrang S, Hainaut P, Marrero JA, Beretta L. Identification of osteopontin as a novel marker for early hepatocellular carcinoma. Hepatology. 2012;55:483-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 247] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 100. | Vongsuvanh R, van der Poorten D, Iseli T, Strasser SI, McCaughan GW, George J. Midkine Increases Diagnostic Yield in AFP Negative and NASH-Related Hepatocellular Carcinoma. PLoS One. 2016;11:e0155800. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 101. | Jang ES, Jeong SH, Kim JW, Choi YS, Leissner P, Brechot C. Diagnostic Performance of Alpha-Fetoprotein, Protein Induced by Vitamin K Absence, Osteopontin, Dickkopf-1 and Its Combinations for Hepatocellular Carcinoma. PLoS One. 2016;11:e0151069. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 77] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 102. | Qiao SS, Cui ZQ, Gong L, Han H, Chen PC, Guo LM, Yu X, Wei YH, Ha SA, Kim JW, Jin ZT, Li S, Peng JR, Leng XS. Simultaneous measurements of serum AFP, GPC-3 and HCCR for diagnosing hepatocellular carcinoma. Hepatogastroenterology. 2011;58:1718-1724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 103. | Sengupta S, Parikh ND. Biomarker development for hepatocellular carcinoma early detection: Current and future perspectives. Hepat Oncol. 2017;4:111-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 104. | Li J, Han X, Yu X, Xu Z, Yang G, Liu B, Xiu P. Clinical applications of liquid biopsy as prognostic and predictive biomarkers in hepatocellular carcinoma: Circulating tumor cells and circulating tumor DNA. J Exp Clin Cancer Res. 2018;37:213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 88] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 105. | Im H, Lee K, Weissleder R, Lee H, Castro CM. Novel nanosensing technologies for exosome detection and profiling. Lab Chip. 2017;17:2892-2898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 65] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 106. | Chen J, Zhang P, Lv M, Guo H, Huang Y, Zhang Z, Xu F. Influences of Normalization Method on Biomarker Discovery in Gas Chromatography-Mass Spectrometry-Based Untargeted Metabolomics: What Should Be Considered? Anal Chem. 2017;89:5342-5348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 107. | Gupta S, Bent S, Kohlwes J. Test characteristics of alpha-fetoprotein for detecting hepatocellular carcinoma in patients with hepatitis C. A systematic review and critical analysis. Ann Intern Med. 2003;139:46-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 108. | Sterling RK, Jeffers L, Gordon F, Venook AP, Reddy KR, Satomura S, Kanke F, Schwartz ME, Sherman M. Utility of Lens culinaris agglutinin-reactive fraction of alpha-fetoprotein and des-gamma-carboxy prothrombin, alone or in combination, as biomarkers for hepatocellular carcinoma. Clin Gastroenterol Hepatol. 2009;7:104-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 104] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 109. | Shaheen KY, Abdel-Mageed AI, Safwat E, AlBreedy AM. The value of serum midkine level in diagnosis of hepatocellular carcinoma. Int J Hepatol. 2015;2015:146389. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 110. | Giannelli G, Fransvea E, Trerotoli P, Beaugrand M, Marinosci F, Lupo L, Nkontchou G, Dentico P, Antonaci S. Clinical validation of combined serological biomarkers for improved hepatocellular carcinoma diagnosis in 961 patients. Clin Chim Acta. 2007;383:147-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 71] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 111. | Sun Y, Gao G, Cai J, Wang Y, Qu X, He L, Liu F, Zhang Y, Lin K, Ma S, Yang X, Qian X, Zhao X. Annexin A2 is a discriminative serological candidate in early hepatocellular carcinoma. Carcinogenesis. 2013;34:595-604. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 56] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 112. | Chounta A, Ellinas C, Tzanetakou V, Pliarhopoulou F, Mplani V, Oikonomou A, Leventogiannis K, Giamarellos-Bourboulis EJ. Serum soluble urokinase plasminogen activator receptor as a screening test for the early diagnosis of hepatocellular carcinoma. Liver Int. 2015;35:601-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 113. | Li J, Cheng ZJ, Liu Y, Yan ZL, Wang K, Wu D, Wan XY, Xia Y, Lau WY, Wu MC, Shen F. Serum thioredoxin is a diagnostic marker for hepatocellular carcinoma. Oncotarget. 2015;6:9551-9563. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 114. | Zekri AN, Youssef AS, El-Desouky ED, Ahmed OS, Lotfy MM, Nassar AA, Bahnassey AA. Serum microRNA panels as potential biomarkers for early detection of hepatocellular carcinoma on top of HCV infection. Tumour Biol. 2016;37:12273-12286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 75] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 115. | Chen T, Xie G, Wang X, Fan J, Qiu Y, Zheng X, Qi X, Cao Y, Su M, Wang X, Xu LX, Yen Y, Liu P, Jia W. Serum and urine metabolite profiling reveals potential biomarkers of human hepatocellular carcinoma. Mol Cell Proteomics. 2011;10:M110.004945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 246] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 116. | Julich-Haertel H, Urban SK, Krawczyk M, Willms A, Jankowski K, Patkowski W, Kruk B, Krasnodębski M, Ligocka J, Schwab R, Richardsen I, Schaaf S, Klein A, Gehlert S, Sänger H, Casper M, Banales JM, Schuppan D, Milkiewicz P, Lammert F, Krawczyk M, Lukacs-Kornek V, Kornek M. Cancer-associated circulating large extracellular vesicles in cholangiocarcinoma and hepatocellular carcinoma. J Hepatol. 2017;67:282-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 131] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 117. | Marrero JA, Romano PR, Nikolaeva O, Steel L, Mehta A, Fimmel CJ, Comunale MA, D'Amelio A, Lok AS, Block TM. GP73, a resident Golgi glycoprotein, is a novel serum marker for hepatocellular carcinoma. J Hepatol. 2005;43:1007-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 256] [Cited by in RCA: 285] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 118. | Giannelli G, Marinosci F, Trerotoli P, Volpe A, Quaranta M, Dentico P, Antonaci S. SCCA antigen combined with alpha-fetoprotein as serologic markers of HCC. Int J Cancer. 2005;117:506-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 2.3] [Reference Citation Analysis (0)] |