Published online Jul 28, 2019. doi: 10.3748/wjg.v25.i28.3787
Peer-review started: March 29, 2019
First decision: May 30, 2019
Revised: June 13, 2019
Accepted: July 5, 2019
Article in press: July 5, 2019
Published online: July 28, 2019
Processing time: 121 Days and 21 Hours
Congenital duodenal obstruction (CDO) can be complete (CCDO) or incomplete (ICDO). To date there is no outcome analysis available that compares both subtypes.
To quantify and compare the association between CCDO and ICDO with outcome parameters.
We retrospectively reviewed all patients who underwent operative repair of CCDO or ICDO in our tertiary care institution between January 2004 and January 2017. The demographics, clinical presentation, preoperative diagnostics and postoperative outcomes of 50 patients were compared between CCDO (n = 27; atresia type 1-3, annular pancreas) and ICDO (n = 23; annular pancreas, web, Ladd´s bands).
In total, 50 patients who underwent CDO repair were enrolled and followed for a median of 5.2 and 3.9 years (CCDO and ICDO, resp.). CCDO was associated with a significantly higher prenatal ultrasonographic detection rate (88% versus 4%; CCDO vs ICDO, P < 0.01), lower gestational age at birth, lower age and weight at operation, higher rate of associated congenital heart disease (CHD), more extensive preoperative radiologic diagnostics, higher morbidity according to Clavien-Dindo classification and comprehensive complication index (all P ≤ 0.01). The subgroup analysis of patients without CHD and prematurity showed a longer time from operation to the initiation of enteral feeds in the CCDO group (P < 0.01).
CCDO and ICDO differ with regard to prenatal detection rate, gestational age, age and weight at operation, rate of associated CHD, preoperative diagnostics and morbidity. The degree of CDO in mature patients without CHD influences the postoperative initiation of enteral feeding.
Core tip: Outcomes of complete congenital duodenal obstruction (CCDO) and incomplete (ICDO) have rarely been compared. The present study is the first to report on this issue based on a series of patients who represent a broad spectrum of pathologies in either group. The current results show significant differences between CCDO and ICDO with regard to prenatal detection rate, preoperative diagnostics, postoperative enteral feeds, length of hospital stay and morbidity according to Clavien-Dindo classification and the comprehensive complication index.
- Citation: Gfroerer S, Theilen TM, Fiegel HC, Esmaeili A, Rolle U. Comparison of outcomes between complete and incomplete congenital duodenal obstruction. World J Gastroenterol 2019; 25(28): 3787-3797
- URL: https://www.wjgnet.com/1007-9327/full/v25/i28/3787.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i28.3787
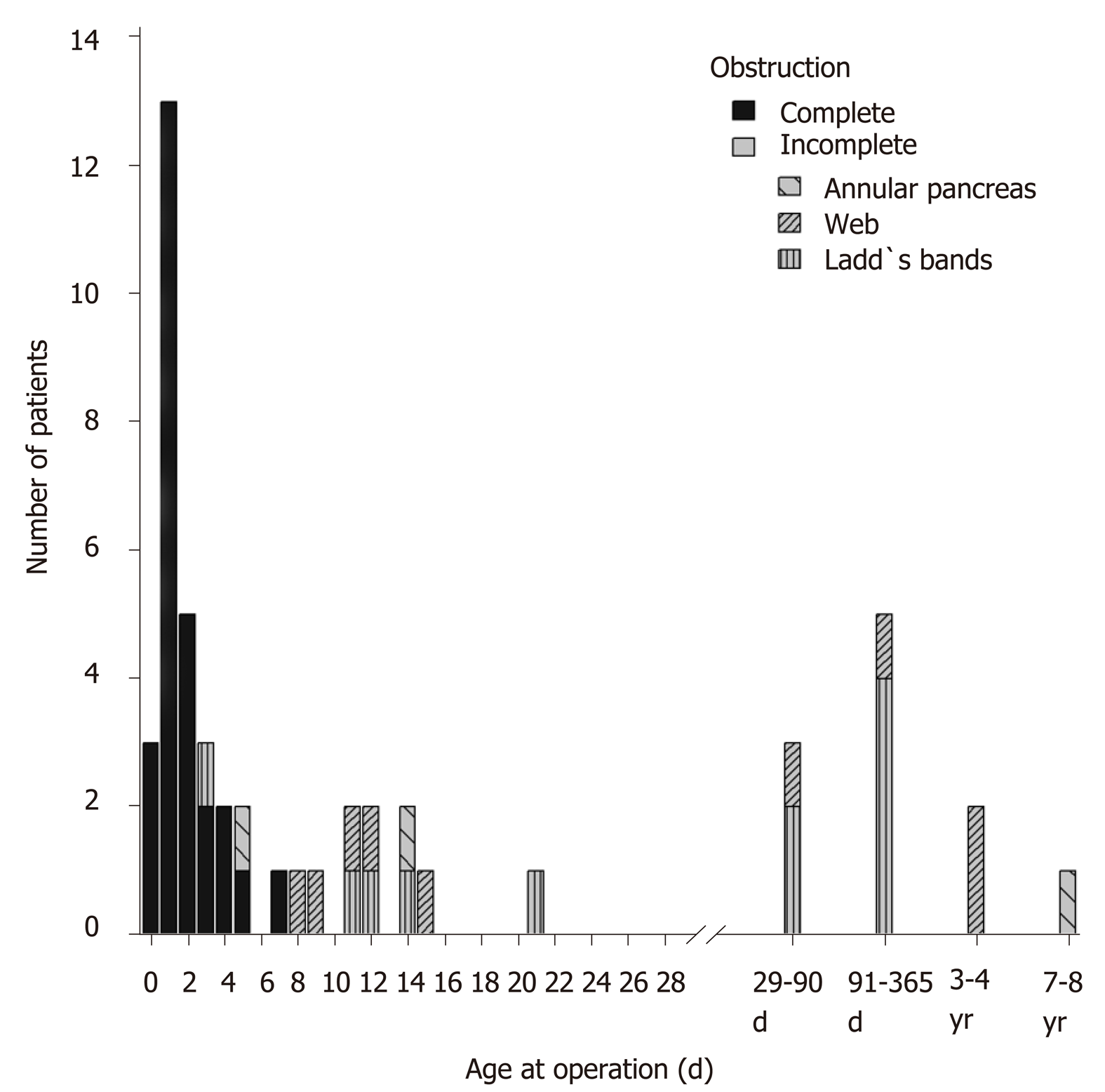
Congenital duodenal obstruction (CDO) accounts for approximately one-half of all intestinal obstructions in newborns and is reported to occur in 1 of 2500 to 10000 births[1,2]. CDO represents a spectrum of congenital anomalies. Corresponding duodenal pathologies are subdivided into congenital duodenal anomalies with either complete or incomplete obstruction (Figure 1). Complete congenital duodenal obstruction (CCDO) originates from duodenal atresia type 1 to 3 and annular pancreas. Incomplete congenital duodenal obstruction (ICDO) occurs on the basis of a web (perforated diaphragm), Ladd´s bands, annular pancreas, preduodenal portal vein, superior mesenteric artery syndrome and duplication cyst. CCDO is diagnosed antenatally to a varying degree based on the detection of a characteristic double bubble sign. However, ICDO is most often missed during prenatal ultrasound examination[3]. The overall neonatal survival rate of patients with CDO has gradually increased over past few decades[4]. Survival is currently reported to be approximately 96%[5,6]. Mortality is primarily attributed to complex congenital heart disease (CHD)[4]. Delayed transition to full enteral nutrition has been associated with CHD and prematurity[5]. In addition to CHD and prematurity influencing the postoperative course, there is limited evidence that the degree of duodenal obstruction may have an impact on postoperative outcome[7]. However, to date an outcome analysis comparing subgroups of patients with CCDO and ICDO is not yet available. The aim of this study was to clarify differences in clinical outcomes between CCDO and ICDO.
After approval of study protocols by the local institutional review board committee (number 85/17), we conducted a retrospective analysis of a series of 50 consecutive patients with CCDO or ICDO, as identified through International Classification of Diseases (ICD-10, Version 2017) codes, who underwent operative repair between January 2004 and January 2017 at our institution. Data including demographic data, preoperative clinical presentation and findings, pathologic findings, operative variables, postoperative outcomes and individual profile of postoperative adverse events, were retained in a database. Demographics included gender, gestational age at birth, age at operation, weight at operation and associated anomalies. Clinical presentations were specified and comprised vomiting, failure to thrive, intolerance of age-appropriate per oral intake, constipation, postprandial discomfort, acute life-threatening event and intolerance to solid food. Failure to thrive was defined as a child´s weight being below the 5th percentile, a drop of more than 2 major percentile lines, or a weight for height being lower than the 5th percentile[8]. Constipation was defined according to the Diagnostic Criteria for Functional Constipation (Rome IV)[9]. Preoperative diagnostics to indicate operative repair were plain abdominal X-ray, upper gastrointestinal (UGI) contrast study and gastroduodenoscopy. Pathologies of CCDO were allocated to diagnoses of atresia type 1 (membrane), atresia type 2 (fibrous cord), atresia type 3 (gap)[10] and annular pancreas. The findings of ICDO were assigned to annular pancreas, web and Ladd´s bands. Additional intestinal pathologies were specified by the following diagnoses: Intestinal malrotation, second distal stenosis and Meckel´s diverticulum. Intestinal malrotation was present when the duodenal loop and the cecocolic loop lacked their normal 270° counterclockwise rotation. Operative variables included operative time (abdominal incision to close of the abdominal wound; including time for correction of additional abdominal pathologies), operative procedures and additional operative procedures. In cases of malrotation where the dorsal peritoneal mesenteric fixation appeared narrow and put the bowel at risk for the development of a volvulus, Ladd´s procedure was per-formed. The question of whether to proceed with an appendectomy was an individual decision of the surgeon. The attending senior surgeon determined the operative approach. Laparoscopic repair of CDO was performed by the first author in patients weighing > 1700 g at operation. The operative approach was implemented irrespective of preoperative radiologic findings or associated congenital anomalies. Open access for CDO repair was achieved via a transverse right upper quadrant incision. Laparoscopic CDO repair was performed using a transumbilically placed 5 mm 30° camera and two 3.5 mm working trocars, one placed in the upper left quadrant and the second in the right mid abdomen. For duodenoduodenostomy, predominantly diamond-shaped anastomoses were performed; simple oblique[11] and parallel anastomoses[12] were also recently used depending on the individual duodenal anatomy. Tapering duodenoplasty was not performed in either group. All open procedures were performed by, or under the direct supervision of, the first, third or last author. Details of postoperative outcomes included the following parameters: time from operation to initiation of feeds (day of initiation of feeds was the day on which feeding per orally or via nasogastric tube was initiated); time from operation to full feeds (day of achievement of full feeds was the day on which parenteral nutrition was ceased); length of postoperative hospital stay (not including the day of operation, but including the day of discharge); reoperation rate (reoperation was defined as a repetition of a surgical operation undertaken due to lack of success of the first attempt). All postoperative adverse events were recorded in detail per patient and scored according to Clavien-Dindo classification[13]. The Clavien-Dindo classification consists of 7 grades (I, II, IIIa, IIIb, IVa, IVb and V); it focuses on the therapeutic consequences of the single most severe complication occurring in a patient in a given episode. In addition the comprehensive complication index (CCI) was calculated. The CCI represents a sensitive measure of the overall morbidity in a single score achieved by inclusion of all complications after surgery[14]. The CCI ranges from 0 (no complication) to 100 (death) and was calculated using the CCI calculator available online (http://www.assessurgery.com).
A nasogastric tube was left postoperatively for gastric decompression. All patients with an enterotomy were allowed nothing by mouth on the day of operation and were allowed to receive enteral feeding on postoperative day 1. All patients without an enterotomy were allowed to receive enteral feeding on the day of operation. After commencement of enteral feeding, all patients received nutritional increments based on clinical observations, irrespective of the operative approach. Green gastric fluid postoperatively during preprandial routine aspiration of the nasogastric tube in an otherwise unremarkable clinical course was regarded as a normal finding due to the insufficient closure of the pyloric muscle, and feeding increments were continued. UGI contrast studies were not performed on a routine basis postoperatively. Patients underwent clinical outpatient follow-up within 4 wk after discharge. All patients were scheduled for regular follow-up at least once per year.
A biomedical statistician performed the statistical review of the study. For the summary of normal distributed continuous variables, the mean and standard deviation were calculated. For comparison, we used two-sample t-tests. Continuous data with another type of distribution or an unknown distribution are presented as median with range, and the Wilcoxon rank sum test was applied for comparison. We used Fisher’s exact test to compare categorical variables. Testing was done based on a 5% significance level. Median follow-up was calculated using the reverse Kaplan-Meier estimate. We used statistical software R version 3.4.0 for analysis, R Foundation for Statistical Computing, Vienna, Austria (http://www.r-project.org).
A total of 50 patients underwent surgical repair of CDO. The patient cohort consisted of a group of 27 patients with CCDO and 23 patients with ICDO. Table 1 displays demographic data and the associated congenital anomalies of both groups. Patients with CCDO that underwent operative repair had a lower gestational age at birth, younger age and lower weight at operation, and had a higher rate of associated CHD. Figure 2 displays the absolute frequencies of operative repairs with the corresponding age at operation for 50 patients with CCDO or ICDO. Of the patients with ICDO, 48% (n = 11) were operated beyond the neonatal period. Patients´ diagnoses of this subgroup (n = 11) were Ladd´s bands (n = 6), duodenal web (n = 4) and annular pancreas (n = 1). Of the patients with ICDO, 13% underwent primary operative repair at 3.4 years or later. This late repair affected all pathologies of ICDO that were evident in this study. Table 2 compares the rates of prenatal ultrasonographic detections of CCDO and ICDO and lists preoperative diagnostics. Of patients with CDO, 49 of 50 had fetal ultrasound screening (98%). One pregnancy did not have prenatal maternal care. The overall prenatal detection rate of CDO was 49% (24 of 49 patients). For patients with CCDO, the prenatal detection rate was 88%; it was 4% for ICDO (P ≤ 0.01). In all patients with CCDO, preoperative plain abdominal X-ray was sufficient to indicate operative repair. In contrast, all patients with ICDO received a diagnostic UGI contrast study in which 4 patients (17%) underwent an additional diagnostic gastroduodenoscopy to indicate operation. In all patients with prenatally unsuspected CDO (complete group n = 4; incomplete group n = 22), postnatal clinical presentations were studied. Vomiting was the most frequent recorded preoperative finding (n = 24, 92%). All patients who vomited showed a yellow-greenish to green discoloration of the vomit at some point between birth and operation, as observed by parents or nursing staff. Table 3 displays intraoperative pathologic findings in the CCDO and ICDO group. Table 4 compares operative variables of the CCDO and ICDO group. Operative time was similar in both groups. Duodenoduodenostomy was the most frequent procedure in both the CCDO group (93%) and the ICDO group (35%, P < 0.01). Duodenal freeing from obstructive ligaments and the Ladd´s procedure were both performed as a single or an adjunct surgical maneuver. Table 5 shows variables of postoperative outcomes for patients with CCDO or ICDO. Durations from operation to initiation and completion of enteral feeds and length of hospital stay were longer in the CCDO group. Morbidity according to median (range) CCI was higher in the CCDO group [8.7 (0.0-100) vs 0.0 (0.0-33.7 in the ICDO group, P<0.01)]. In an attempt to reduce confounding a subgroup analysis was performed and outcome parameters were additionally calculated under exclusion of patients with CHD and prematurity. Subgroup analysis revealed a difference between the CCDO and ICDO groups with regard to the parameter time from operation to initiation of feeds. Table 6 lists all adverse events recorded during the entire individual follow-up period for 50 patients undergoing operative repair of CCDO or ICDO.
| Complete | Incomplete | P value | |
| n = 27 | n = 23 | ||
| Gender (male:female), n (%) | 12 (44):15 (56) | 12 (52):11 (48) | 0.78 |
| Gestational age at birth (wk) | 36.0 (31.3-42) | 38.7 (30.1-40.1) | 0.01a |
| No CHD + GA ≥ 37 wk (wk) | 38.6 (38.3-39.0), n = 4 | 39.3 (37.1-40.1), n = 15 | 0.34 |
| GA < 37 wks (patients), n (%) | 14 (52) | 5 (22) | < 0.05a |
| Age at operation, AO (d) | 1.0 (0-7) | 21.0 (3-2790) | < 0.01a |
| No CHD + GA ≥ 37 wk (d) | 1.0 (0-7), n = 4 | 21.0 (3-2790), n = 15 | < 0.01a |
| Weight at operation (kg) | 2.54 (1.48-3.84) | 3.27 (2.20-13.80) | < 0.01a |
| No CHD + GA ≥ 37 wk (kg) | 3.20 (2.98-3.45), n = 4 | 3.92 (2.48-12.80), n = 15 | 0.37 |
| Associated congenital anomalies (patients), n (%) | 20 (74) | 7 (30) | < 0.01a |
| Congenital heart disease (patients), n (%) | 18 (67) | 3 (13) | < 0.01a |
| Trisomy 21 (patients), n (%) | 11 (41) | 4 (17) | 0.12 |
| Other anomalies (patients), n (%) | 10 (37) | 6 (26) | 0.55 |
| Details | Butterfly vertebrae (1), esophageal atresia (1), hemolytic disease of the newborn (1), hydronephrosis, unilateral (1), bilateral (1), hypothyreosis (5), funnel trachea (1), polydactyly, unilateral (1), Hirschsprung disease (1), atopic eczema (1) | Pes calcaneus (1), biliary duct hypoplasia (1), celiac disease (1), Cornelia de Lange syndrom (1), sleep apnoea (1), ectrodactyly, bilateral (1), hypospadia (1), patent omphalomesenteric duct (1), glutaric aciduria type 1 (1) |
| Complete | Incomplete | P value | |
| n = 27 | n = 23 | ||
| Fetal US screening, n (%) | 261 (96) | 23 (100) | 1 |
| Prenatally suspected by US (yes:no), n (%) | 23 (88):3 (12) | 1 (4):22 (96) | < 0.01a |
| Clinical presentation all prenatally unknown CDO | n = 42 | n = 22 | |
| Vomiting, n (%) | 4 (100) | 20 (91) | 1 |
| Failure to thrive, n (%) | 13 (59) | ||
| Intolerance of age-appropriate p.o. intake, n (%) | 10 (45) | ||
| Constipation, n (%) | 1 (25) | 7 (32) | 1 |
| Postprandial discomfort/pain/restlessness, n (%) | 5 (23) | ||
| ALTE (aspiration, apnea, bradycardia), n (%) | 1 (5) | ||
| Intolerance to solid food, n (%) | 1 (5) | ||
| Preoperative diagnostics | n = 27 | n = 23 | |
| Plain abdominal X-ray, n (%) | 27 (100) | 1 (4) | < 0.01a |
| Upper GI contrast study, n (%) | 0 | 23 (100) | < 0.01a |
| Gastroduodenoscopy, n (%) | 0 | 4 (17) | 0.04a |
| Complete | Incomplete | P value | |
| n = 27 | n = 23 | ||
| Atresia type 1-membrane, n (%) | 10 (37) | ||
| Type 2-fibrous cord, n (%) | 1 (4) | ||
| Type 3-gap, n (%) | 3 (11) | ||
| Annular pancreas, n (%) | 15 (56) | 3 (13) | < 0.01a |
| additionally to type 3 atresia, n (%) | 2 (7) | ||
| Web, n (%) | 9 (39) | ||
| Ladd´s bands, n (%) | 11 (48) | ||
| Additional intestinal pathologies | |||
| Intestinal malrotation, n (%) | 16 (59) | 19 (83) | 0.12 |
| Second distal stenosis, n (%) | 0 | 1 (4) | |
| Meckel´s diverticulum, n (%) | 2 (7) | 2 (9) | 1 |
| Complete | Incomplete | P value | |
| n = 27 | n = 23 | ||
| Operative time (min), n (%) | 168 (75) | 163 (101) | 0.85 |
| Procedure | |||
| Duodenoduodenostomy, n (%) | 25 (93) | 8 (35) | < 0.01a |
| Excision of membrane/web and duodenoplasty (Mikulicz), n (%) | 2 (7) | 4 (17) | 0.39 |
| Duodenal freeing, n (%) | 15 (56) | 13 (57) | 1 |
| Ladd´s procedure, n (%) | 6 (22) | 9 (39) | 0.23 |
| Additional procedures | |||
| Jejunoplasty (Mikulicz) for second distal stenosis | 0 | 1 (4) | 0.46 |
| Appendectomy, n (%) | 5 (19) | 13 (57) | < 0.01a |
| Resection of Meckel`s diverticulum, n (%) | 2 (7) | 2 (9%) | 1 |
| Laparoscopic approach, n (%) | 12 (44) | 16 (70) | 0.09 |
| Conversion to open approach, n (%) | 1 (8) | 2 (13) | 1 |
| Complete | Incomplete | P value | |
| n = 261 | n = 23 | ||
| Time from OP to initiation of feeds (d) | 3.0 (0-12) | 1.0 (0-3) | < 0.01a |
| No CHD + GA ≥ 37 wk (d) | 4 (2-12), n = 4 | 1 (0-3), n = 15 | < 0.01a |
| Time from OP to full feeds (d) | 12.0 (5-22) | 6.0 (1-13) | < 0.01a |
| No CHD + GA ≥ 37 wk (d) | 10.5 (5-22), n = 4 | 6 (3-11), n = 15 | 0.09 |
| Length of postop. hospital stay (d) | 25 (7-40) | 9 (3-24) | < 0.01a |
| No CHD + GA ≥ 37 wk (d) | 15.5 (7-25), n = 4 | 8 (3-21), n = 15 | 0.14 |
| n = 27 | n = 23 | ||
| Morbidity (Clavien-Dindo grade I-V), n (%) | 15 (56) | 2 (9) | < 0.01a |
| No CHD + GA ≥ 37 wk, n (%) | 1 (25), n = 4 | 1 (7), n = 15 | 0.39 |
| Surgical morbidity, n (%) | 7 (26) | 1 (4) | 0.06 |
| No CHD + GA ≥ 37 wk, n (%) | 1 (25), n = 4 | 0 (0), n = 15 | 0.21 |
| Nonsurgical morbidity, n (%) | 12 (44) | 1 (4) | < 0.01a |
| No CHD + GA ≥ 37 wk, n (%) | 0 (0), n = 4 | 1 (7), n = 15 | 1 |
| Mortality, n (%) | 1 (3.7) | 0 (0) | 1 |
| Reoperation, n (%) | 3 (12) | 0 | 0.24 |
| Comprehensive complication index | 8.7 (0.0-100) | 0.0 (0.0-33.7) | < 0.01a |
| No CHD + GA ≥ 37 wk | 0 (0-58.4), n = 4 | 0 (0-8.7), n = 15 | 0.30 |
| Follow-up (yr) | 5.2 (0.4-13.8) | 3.9 (0.8-13.1) | 0.41 |
| Clavien-Dindo grade | Postoperative adverse event | Patient No. | Frequency of occurence, n (%) | |
| Complete | I | Icterus prolongatus | 5 | 1 (2) |
| Hyperbilirubinemia | 11 | 1 (2) | ||
| Transient trocar hernia | 16 | 1 (2) | ||
| II | Surgical site infection | 5 | 1 (2) | |
| Central line infection | 3, 6, 39 | 3 (6) | ||
| Enteritis, Dehydration | 2 | 1 (2) | ||
| Gastroesophageal reflux | 22, 32 | 2 (4) | ||
| Pneumonia | 27, 32 | 2 (4) | ||
| Pericardial effusion | 27 | 1 (2) | ||
| Cardiac insufficiency, ACE inhibitor | 31 | 1 (2) | ||
| Subclavian malpuncture, transfusion | 38 | 1 (2) | ||
| Enterocolitis | 43 | 1 (2) | ||
| IIIa | Gastric bleeding | 40 | 1 (2) | |
| IIIb | Colon perforation | 1, 25 | 2 (4) | |
| Colostomy closure | 1 | 1 (2) | ||
| Mesocolonic hernia | 1 | 1 (2) | ||
| Missed Ladd´s bands | 22, 32 | 2 (4) | ||
| Hematothorax, pleural drainage | 38 | 1 (2) | ||
| Anastomotic leakage | 40 | 1 (2) | ||
| IVb | Cardiac failure, multiorgan dysfunction | 40 | 1 (2) | |
| V | Death | 40 | 1 (2) | |
| Incomplete | I | Postoperative vomiting (> 7 d) | 46 | 1 (2) |
| IIIb | Diagnostic gastroduodenoscopy | 46 | 1 (2) | |
| IIIb | Incisional hernia | 2 | 1 (2) |
Our study suggests that outcomes of patients with CCDO and ICDO differ significantly. This article, to our knowledge, is the only paper focusing specifically on differences between patients with CCDO and ICDO. According to our results, patients with CCDO had a significantly higher prenatal detection rate, lower gestational age at birth and lower age and weight at operation. Operative repair in the CCDO group was indicated solely on the basis of a plain abdominal X-ray without the need for UGI contrast study. Patients with CCDO had a higher rate of associated CHD, had a longer duration from operation to both initiation and achievement of full feeds, had a longer hospital stay and had a higher morbidity according to Clavien-Dindo classification and CCI in comparison to patients in the ICDO group. In a subgroup of patients without associated CDH and prematurity patients with CCDO had a delayed initiation of enteral feeds in comparison with the ICDO group.
Our study is the first to deliver a differentiated prenatal detection rate of CCDO and ICDO based on an analysis of patients who underwent operative repair. While the overall detection rate was 48% we found a significant difference between CCDO and ICDO (detection rate 88% vs 4% respectively). Previously, several authors have conducted studies analyzing prenatal ultrasonographic findings of CDO. However, data based on a wide spectrum of CDO pathologies are scarce. Savran et al[15] analyzed 15 patients with duodenal atresia that had undergone operative repair over a period of 6 years at a single center. In their retrospective analysis, the calculated prenatal detection rate was 67%. Only 12 of 15 (80%) pregnant women had a prenatal ultrasonographic screening; ICDO was not analyzed. A study by Kim et al[16] reported a prenatal detection rate of 81.4% based on 59 pregnant women and neonates that underwent surgical repair of CDO. A limiting factor of the latter study was the restriction of patients to neonatal age. Our current study included all patients undergoing surgical repair of CDO irrespective of their age in order to gain a more realistic prenatal ultrasonographic detection rate. Due to the long period of observation, our data revealed a substantial number of patients with ICDO (23/50, 46%). The results of our present study suggest that a prenatal detection rate calculated on the basis of patients restricted to the neonatal period is likely to favor the depiction of CCDO. In our current case series, the proportion of patients with ICDO was slightly higher than previously reported (28%-37%)[1,5,17]. This may be attributed to the fact that in recent years, our surgical center has built up collaborations with regional pediatric hospitals, which do not employ pediatric surgeons.
An important finding of our study was that patients with ICDO frequently suffered a considerable delay between birth and diagnosis of CDO. Nearly one half of patients (48%) in the ICDO group underwent operative repair of CDO beyond the neonatal period; 13% were corrected beyond 3 years of age. In the literature, there is rare reporting of children that underwent delayed operative repair of CDO[18]. The results of our retrospective analysis raise the question whether delayed diagnoses of ICDO might be underreported. Patients presenting with chronic vomiting with or without failure to thrive and intolerance of age-appropriate per oral intake need to be assessed with conscious awareness of possible yet undiagnosed ICDO. This is equally attributable both to undiagnosed congenital lesions and the wide spectrum of acquired lesions of the adults` duodenum[19,20,21].
In our study, patients with CCDO had a lower gestational age at birth and lower age and weight at operation. In a previous study that compared duodenal atresia with duodenal web, age and weight at operation differed significantly, with those in the duodenal atresia group having the lowest age and weight and those with duodenal web having the highest age and weight[7]. However, no information was provided regarding differences in age and weight between the groups at birth.
Our finding that UGI contrast-enhanced X-ray examinations are frequently necessary to diagnose ICDO is in line with previous studies[1,22]. However, statistical analysis between ICDO and CCDO had not been previously performed. Our assessment of associated congenital anomalies corresponds well to a large previous analysis of patients with duodenal atresia and stenosis[4]. In simplified terms, approximately 50% of patients with CDO have associated congenital anomalies, CHD in 40% and trisomy 21 in 30%. However, previous studies did not differentiate between complete and incomplete duodenal obstruction.
A recent study of patients with CDO revealed that CHD and prematurity are most commonly associated with delayed enteral nutrition[5]. Consequently, in our outcome analysis, we additionally analyzed the subgroup of patients without CHD and prematurity (gestational age ≥ 37 wk). Our subgroup analysis demonstrated significant differences between groups with respect to postoperative initiation of feeds. Achievement of full feeds, length of postoperative hospital stay and morbidity did not differ between CCDO and ICDO in this subgroup. It appears that CHD and prematurity are predominant factors that widely influence postoperative outcome, while in contrast the degree of duodenal obstruction is limited to impact time from operation to initiation of enteral feeding.
The primary strength of this study was that it was based on data derived from a consecutive series of patients who underwent operative repair over a period of more than 13 years with a follow up period between 3.9 and 5.2 years. Duodenal pathologies of our series represented a wide spectrum of both CCDO and ICDO. Our analysis has several limitations, including the retrospective design of the study, small sample size, single institution and limited follow-up period. The difference of age at operation between groups may have influenced enteral feeding. Duodeno-duodenostomy had different frequencies in both groups, however differential impact on groups may be minor because operative time between groups was equal. Our study highlights differences in prenatal detection and postnatal outcome of patients with CCDO and ICDO. Our results suggest that future stratified outcome analyses of CDO should be performed with special attention to CHD, prematurity and the degree of duodenal obstruction.
In conclusion, our results indicate that outcome parameters between CCDO and ICDO differ significantly. Patients with CCDO have a longer postoperative hospital stay associated with more adverse events compared to ICDO. Patients with ICDO frequently suffer considerable delays to diagnosis and operative repair of their congenital malformation. Efforts should to be undertaken to improve pre- and postnatal detection of ICDO in order to reduce preoperative morbidity and the delay to operative repair.
Congenital duodenal obstruction (CDO) can be complete (CCDO) or incomplete (ICDO). To date there is no outcome analysis available that compares both subtypes.
Anatomically, CDO is subdevided into CCDO and ICDO. The clinical observation shows that outcomes between patients with CCDO and ICDO differ substantially.
The objective of this study was to analysis and compare the association between CCDO and ICDO with outcome parameters.
We retrospectively reviewed all patients who underwent operative repair of CCDO or ICDO in our tertiary care institution between January 2004 and January 2017. The demographics, clinical presentation, preoperative diagnostics and postoperative outcomes of 50 patients were compared between CCDO (n = 27) and ICDO (n = 23).
CCDO was associated with a significantly higher prenatal ultrasonographic detection rate, lower gestational age at birth, lower age and weight at operation, higher rate of associated congenital heart disease, more extensive preoperative radiologic diagnostics, higher morbidity according to Clavien-Dindo classification and comprehensive complication index. The subgroup analysis of patients without congenital heart disease (CHD) and prematurity showed a longer time from operation to the initiation of enteral feeds in the CCDO group.
This study showed that CCDO and ICDO differ with regard to prenatal detection rate, preoperative diagnostics, postoperative enteral feeds, length of hospital stay and morbidity according to the Clavien-Dindo classification and the comprehensive complication index. The degree of CDO in mature patients without CHD influences the postoperative initiation of enteral feeding.
Efforts should to be undertaken to improve pre- and postnatal detection of ICDO in order to reduce preoperative morbidity and the delay to operative repair.
The authors would like to acknowledge Emilia Salzmann-Manrique and Martin Hutter, Biomedical Statisticians, Devision for Pediatric Stem Cell Transplantation and Immunology, Department for Children and Adolescents, University Hospital Frankfurt, for the statistical analysis.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Germany
Peer-review report classification
Grade A (Excellent): A, A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chisthi MM, Corvino A, Marzano C S-Editor: Yan JP L-Editor: A E-Editor: Zhang YL
| 1. | Dalla Vecchia LK, Grosfeld JL, West KW, Rescorla FJ, Scherer LR, Engum SA. Intestinal atresia and stenosis: A 25-year experience with 277 cases. Arch Surg. 1998;133:490-6; discussion 496-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 321] [Cited by in RCA: 258] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 2. | Bales C, Liacouras CA. Intestinal atresia, stenosis and malrotation. 20th ed. Kliegman RM, Stanton BF, St Geme JW, Schor NF, editor. Nelson Textbook of pediatrics. Philadelphia: Elsevier Inc., 2016; 1800-1804. |
| 3. | Lawrence MJ, Ford WD, Furness ME, Hayward T, Wilson T. Congenital duodenal obstruction: Early antenatal ultrasound diagnosis. Pediatr Surg Int. 2000;16:342-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 39] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Grosfeld JL, Rescorla FJ. Duodenal atresia and stenosis: Reassessment of treatment and outcome based on antenatal diagnosis, pathologic variance, and long-term follow-up. World J Surg. 1993;17:301-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 105] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Bairdain S, Yu DC, Lien C, Khan FA, Pathak B, Grabowski MJ, Zurakowski D, Linden BC. A modern cohort of duodenal obstruction patients: Predictors of delayed transition to full enteral nutrition. J Nutr Metab. 2014;2014:850820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Choudhry MS, Rahman N, Boyd P, Lakhoo K. Duodenal atresia: Associated anomalies, prenatal diagnosis and outcome. Pediatr Surg Int. 2009;25:727-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 79] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 7. | Mustafawi AR, Hassan ME. Congenital duodenal obstruction in children: A decade's experience. Eur J Pediatr Surg. 2008;18:93-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Keane VA. Assessment of growth. 20th ed. Kliegman RM, Stanton BF, St Geme JW, Schor NF, editeor. Nelson Textbook of pediatrics. Philadelphia: Elsevier Inc., 2016; 84-89. |
| 9. | Benninga MA, Faure C, Hyman PE, St James Roberts I, Schechter NL, Nurko S. Childhood Functional Gastrointestinal Disorders: Neonate/Toddler. Gastroenterology. 2016;pii:S0016-5085(16)00182-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 395] [Cited by in RCA: 365] [Article Influence: 40.6] [Reference Citation Analysis (0)] |
| 10. | Skandalakis JE. Embryology for Surgeons: The Embryological Basis for the Treatment of Congenital Anomalies. Gray SW, editor. Philadelphia: Saunders 1972; 147-148. |
| 11. | Son TN, Liem NT, Kien HH. Laparoscopic simple oblique duodenoduodenostomy in management of congenital duodenal obstruction in children. J Laparoendosc Adv Surg Tech A. 2015;25:163-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Oh C, Lee S, Lee SK, Seo JM. Laparoscopic duodenoduodenostomy with parallel anastomosis for duodenal atresia. Surg Endosc. 2017;31:2406-2410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18532] [Cited by in RCA: 24858] [Article Influence: 1183.7] [Reference Citation Analysis (0)] |
| 14. | Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA. The comprehensive complication index: A novel continuous scale to measure surgical morbidity. Ann Surg. 2013;258:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 764] [Cited by in RCA: 1300] [Article Influence: 108.3] [Reference Citation Analysis (0)] |
| 15. | Savran B, Adigüzel Ü, Yüksel KB, Seven A, Fazli O, Kabil Kucur S, Öztürk Gözükara I. The importance of antenatal diagnosis of congenital duodenal obstruction. Ir J Med Sci. 2016;185:695-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Kim JY, You JY, Chang KH, Choi SJ, Oh SY, Seo JM, Roh CR, Kim JH. Association Between Prenatal Sonographic Findings of Duodenal Obstruction and Adverse Outcomes. J Ultrasound Med. 2016;35:1931-1938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Bailey PV, Tracy TF, Connors RH, Mooney DP, Lewis JE, Weber TR. Congenital duodenal obstruction: A 32-year review. J Pediatr Surg. 1993;28:92-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 103] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 18. | Mousavi SA, Karami H, Saneian H. Congenital duodenal obstruction with delayed presentation: Seven years of experience. Arch Med Sci. 2016;12:1023-1027. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Jayaraman MV, Mayo-Smith WW, Movson JS, Dupuy DE, Wallach MT. CT of the duodenum: An overlooked segment gets its due. Radiographics. 2001;21 Spec No:S147-S160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 80] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 20. | Campanile F, Maurea S, Mainenti P, Corvino A, Imbriaco M. Duodenal involvement by breast cancer. Breast J. 2012;18:615-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Juanpere S, Valls L, Serra I, Osorio M, Gelabert A, Maroto A, Pedraza S. Imaging of non-neoplastic duodenal diseases. A pictorial review with emphasis on MDCT. Insights Imaging. 2018;9:121-135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Chen QJ, Gao ZG, Tou JF, Qian YZ, Li MJ, Xiong QX, Shu Q. Congenital duodenal obstruction in neonates: A decade's experience from one center. World J Pediatr. 2014;10:238-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |