Published online Jul 28, 2019. doi: 10.3748/wjg.v25.i28.3764
Peer-review started: March 4, 2019
First decision: April 8, 2019
Revised: May 24, 2019
Accepted: June 7, 2019
Article in press: June 8, 2019
Published online: July 28, 2019
Processing time: 147 Days and 0.5 Hours
Endoscopic en bloc resection of larger polyps is relevant because risk of advanced neoplasia or malignancy correlates with tumor size. Recurrence rates after piecemeal endoscopic mucosal resection (EMR) are high and endoscopic submucosal dissection (ESD) is associated with higher complication rates in the western world.
To develop a modified endoscopic en bloc resection technique using an external additional working channel and novel agent for submucosal injection.
EMR+ was considered as modified grasp and snare technique. For simultaneous use of a grasping and cutting device a novel additional working channel was used (AWC®, Ovesco Endoscopy, Tübingen, Germany). AWC® is installed on the outer surface of the endoscope, covered with a plastic sleeve and designed for single use. For submucosal injection a new agent consisting of poloxamers was used (LiftUp®, Ovesco Endoscopy, Tübingen, Germany). The agent is liquid at room temperature and forms a stable and permanent gel cushion after injection. Safety of LiftUp® has been shown in a pre-clinical study in domestic pigs. LiftUp® is commercially not yet available but approval is expected in early 2019. EMR+ was first developed ex vivo (explanted pig stomach) and subsequently evaluated in vivo (stomach, porcine model, 3 domestic pigs). Main outcome measurements were: Procedure time, macroscopic en bloc resection and adverse events.
Concept of EMR+ was first developed ex vivo (explanted pig stomach). Ex vivo, 22 resections were performed after technique was established. Median procedure time (measured from begin of injection to extraction of resection specimen) was 7 min (range 5-11, SD 1.68) and median size of resection specimens was 30 mm × 26 mm × 11 mm ex vivo. Subsequently 13 resections were performed in vivo (stomach, porcine model, 3 domestic pigs). In vivo, median procedure time (measured from begin of injection to extraction of resection specimen) was 5 min (range 3-12, SD 2.72) and median size of resection specimens was 35 mm × 35 mm × 11 mm. In vivo, resection was macroscopic complete in 92.3%, major adverse events were not observed. In one case (7.7%) minor periprocedural bleeding was observed and managed by coagulation.
EMR+ appeared to be effective and safe and was easy and fast to perform in the porcine model. EMR+ needs to be further evaluated clinically in comparative trials.
Core tip: We report on a novel modified grasp and snare technique (EMR+) forendoscopic en bloc resection. The technique was developed ex vivo (explanted pig stomach) and evaluated in vivo in a porcine model (stomach, 3 domestic pigs). EMR+ includes a novel additional working channel (AWC®) and a new agent (consisting of poloxamers) for submucosal injection (LiftUp®, approval expected in early 2019). EMR+ appeared to be effective and safe in the stomach and allowed for en bloc resection for lesions up to 40 mm. EMR+ needs to be further evaluated clinically in comparative trials.
- Citation: Meier B, Wannhoff A, Klinger C, Caca K. Novel technique for endoscopic en bloc resection (EMR+) - Evaluation in a porcine model. World J Gastroenterol 2019; 25(28): 3764-3774
- URL: https://www.wjgnet.com/1007-9327/full/v25/i28/3764.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i28.3764
Endoscopic resection (ER) of larger polyps is relevant because risk of advanced neoplasia or malignancy correlates with tumor size. En bloc resection is essential because main predictors for recurrency are tumor size > 20 mm and piecemeal resection[1]. Endoscopic mucosal resection (EMR) is only adequate for en bloc resection for lesions < 20 mm[2]. Recurrence rates after en bloc EMR are low and reported down to 3%[3]. For lesions > 20 mm piecemeal EMR[4,5] or endoscopic submucosal dissection (ESD) are available. However, recurrence rates after piecemeal EMR are reported between 15%-45%[3,6,7] and ESD still is an advanced technique associated with higher risks for bleeding or perforation in the western world.
Submucosal injection is well investigated and essential for EMR and ESD. By injection a liquid-filled cushion is created, so tumor is lifted and amenable for ER plus underlying tissue is protected against bleeding and perforation[8,9]. Different injection agents have been investigated but saline solution still is the standard solution used for ER[9]. Major limitation of isotonic saline solution is its absorption by the adjacent mucosa. In consequence, submucosal cushion disappears quickly[8-10], frequent re-injections are necessary and prolonged procedure times are the consequences. Different viscous and hypertonic solutions have been investigated to prolong maintenance of submucosal cushion and to reduce procedure time[8,10-13]. However, every agent has merits and limitations so optimal agent still is not identified. LiftUp® (Ovesco Endoscopy, Tübingen, Germany) is a new developed agent for submucosal injection consisting of poloxamers. Viscosity of LiftUp® is temperature-dependent and liquid at room temperature. After injection LiftUp® forms a stable and permanent gel cushion.
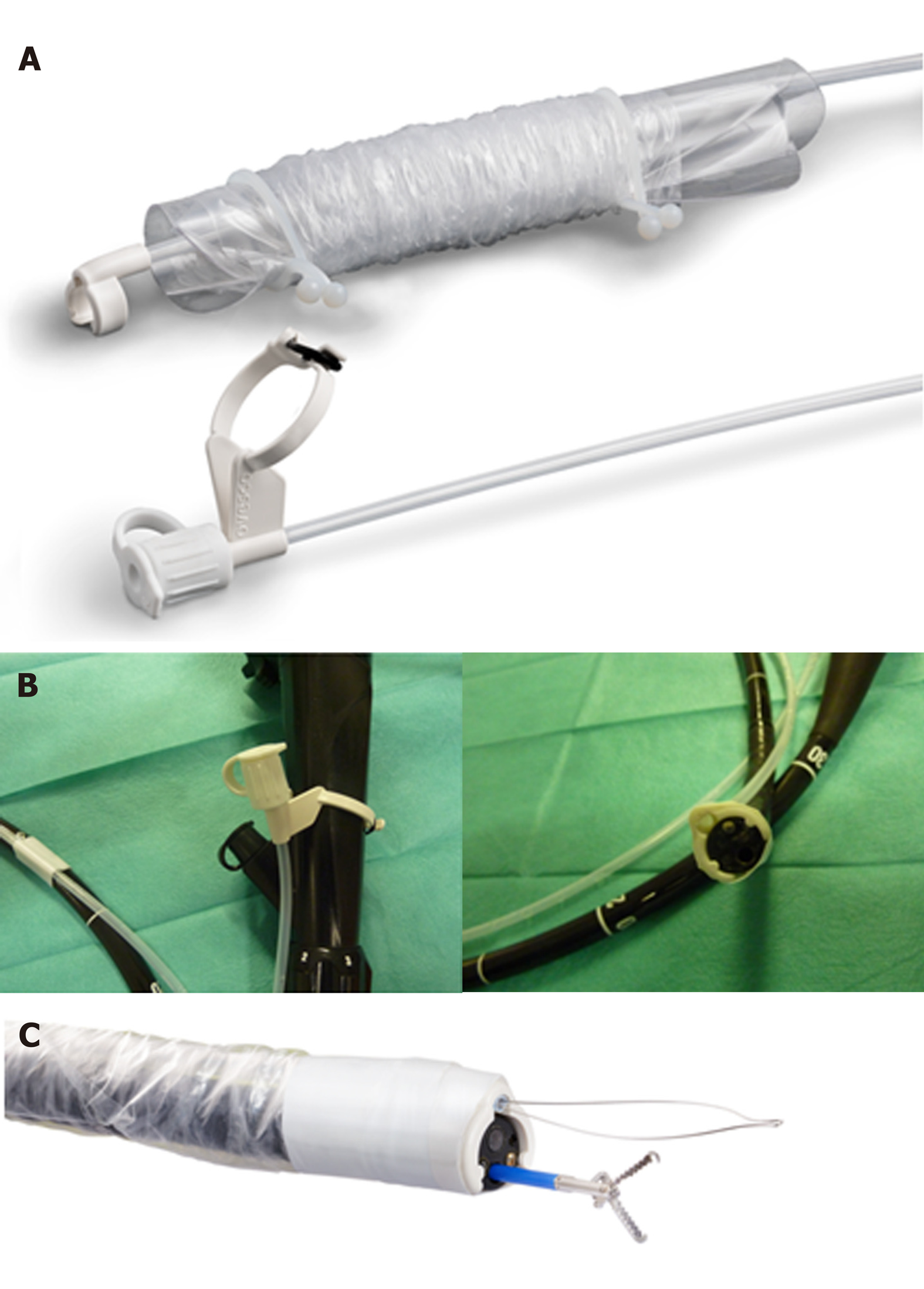
Grasp and snare techniques using double channel (DC) endoscopes have been investigated to optimize EMR procedure for larger or difficult (e.g., difficult location or reduced lifting-sign) lesions[14-17]. However, resection with DC endoscopes has not come to daily routine as instruments are more expensive and not widely available. The novel additional working channel (AWC®, Ovesco Endoscopy, Tübingen, Germany) is installed on the endoscope externally and designed for single use.
The aim of this study was to develop a novel technique for endoscopic en bloc resection for lesions up to 30 mm. The technique was considered as modified grasp and snare technique and included a new injection agent (LiftUp®) and novel additional working channel (AWC®). The technique was developed ex vivo and evaluated in vivo (porcine model).
For simultaneous use of a grasping and cutting device an external additional working channel (AWC) was used (AWC®, Ovesco Endoscopy, Tübingen, Germany). AWC® is available (currently in Europe and United States) for endoscopes with diameters 8.5-13.5 mm and shaft lengths 122 cm/185 cm. The device is installed on the outer surface of the endoscope, covered with a plastic sleeve and designed for single use. After attachment AWC® allows use of an additional instrument with diameter up to 2.8 mm (Figure 1). An anchor device (OTSC® Anchor, Ovesco Endoscopy, Tübingen, Germany) was advanced through the conventional working channel and used to improve positioning of the resection snare. For resection an oval monofilament snare (Olympus) with diameter of 35 mm was used and advanced through the AWC.
For submucosal injection a new agent was used (LiftUp®, Ovesco Endoscopy, Tübingen, Germany). Safety of LiftUp® has been shown in a pre-clinical study in domestic pigs. LiftUp® is commercially not yet available. Approval of LiftUp® is pending and expected in early 2019 in Europe. LiftUp® consists of poloxamers (nonionic tensides) with temperature-dependent viscosity. The agent is sterile and premixed with methylene blue and has liquid consistency at room temperature which allows submucosal injection. At body temperature the agent gels within seconds and forms a stable and permanent cushion. LiftUp® was stored in a refrigerator (6-8 degrees celcius) just before submucosal injection. First, 2 mL of saline solution were injected into the submucosa to facilitate injection of LiftUp®. Injection of LiftUp® was performed with an inflation device (Inflation Device, Accura Medizintechnik GmbH, Germany) and conventional injection needle (diameter 0.7 mm).
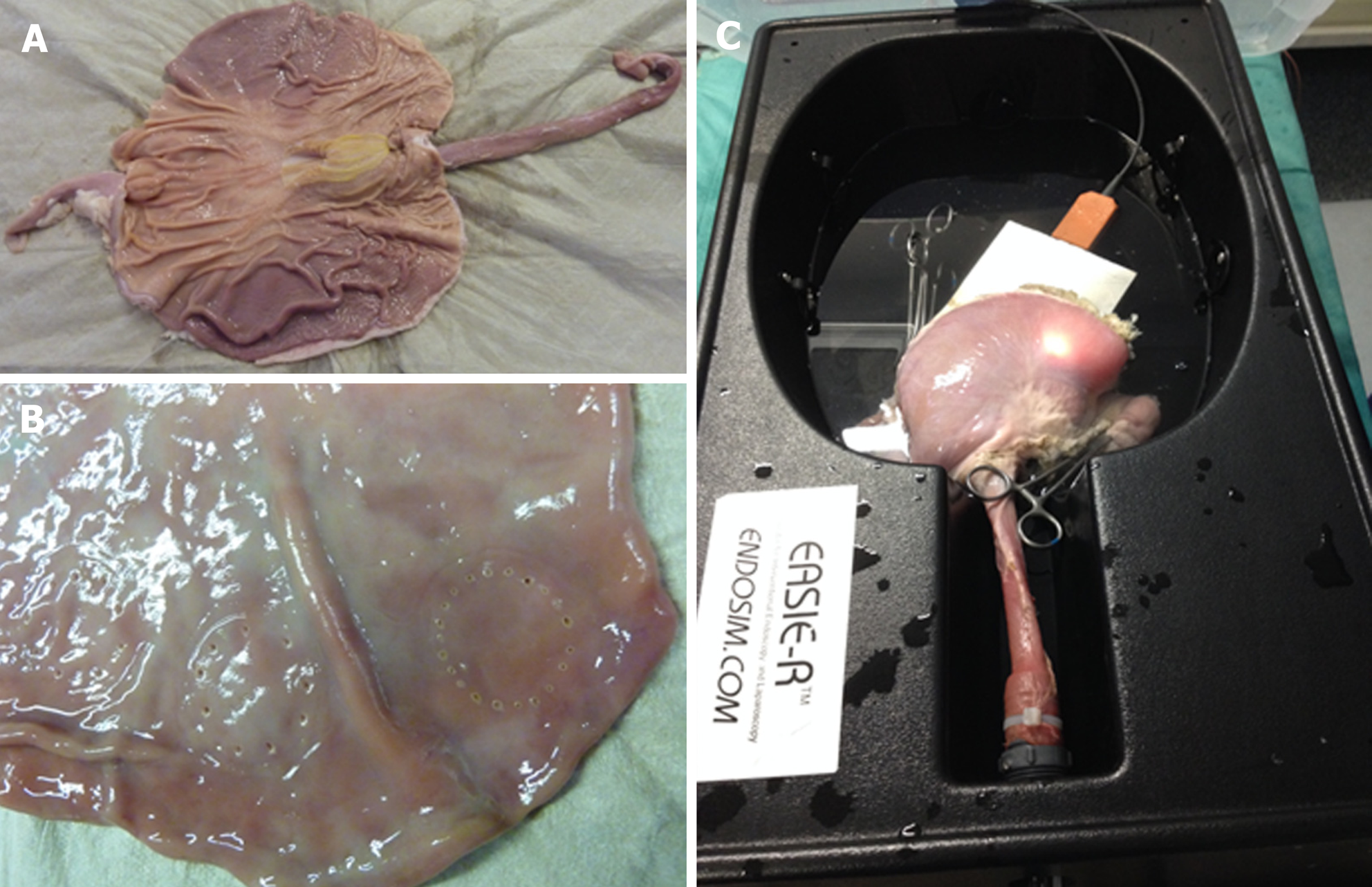
EMR+ was developed ex vivo (October – December 2017). Explanted pig stomach was opened by incision (Figure 2A) and imaginary lesions were created by coagulation (Figure 2B) using a template (circular, diameter 30 mm). After preparation stomach was closed and connected to EASIE-R1 simulator (EndoSim, Bolton, United States) to be accessible to endoscopy (Figure 2C). Primary goal in this setting was to develop a concept of EMR+ (e.g., positioning of instruments, injection/resection technique). EASIE-R 1 was filled with warm water and before resection the lesion (cushion) was additionally flushed with warm water endoscopically to ensure correct temperature. Before resection temperature was measured on the inner and outer surface of stomach.
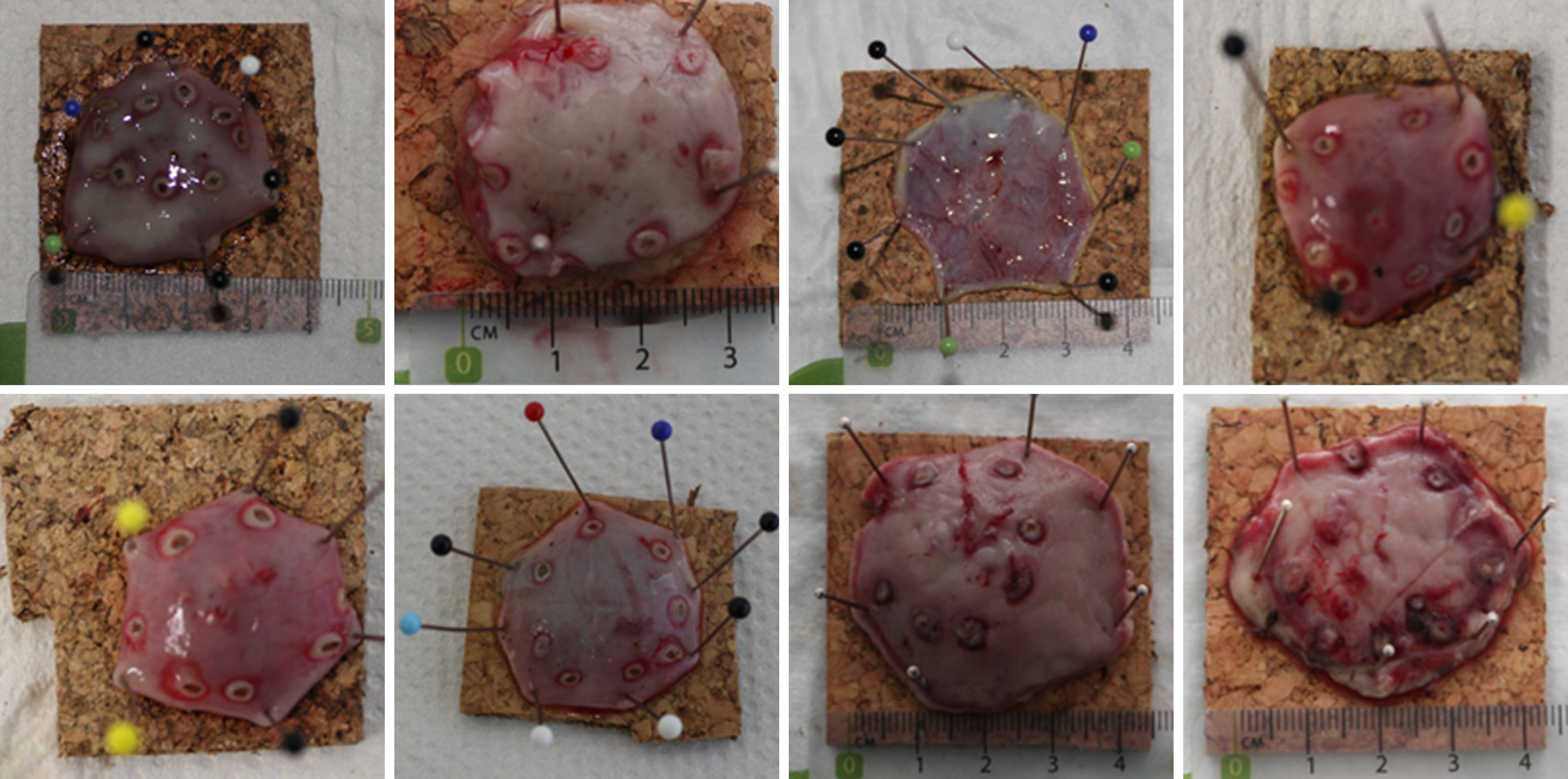
After developing concept of EMR+ ex vivo, technique was transferred and evaluated in vivo (domestic pigs, April – July 2018). Main outcome measurements were: Procedure time, macroscopic en bloc resection and adverse events. In vivo study was conducted at the facility of experimental surgery of the University of Tübingen, Germany (Institut für experimentelle Chirurgie, Universitätsklinikum Tübingen, Tübingen, Germany) after approval from the local authority/institutional animal care and use committee (Regierungspräsidium Baden-Württemberg, Germany, approval number C1/15). Three domestic pigs with a median weight of 81.5 kg were used. The animals were fasted from solid food for 48 hours prior to surgery but were allowed full access to water and milk. Preanesthesia sedation consisted of ketamine 2 mg/kg and xylazine 2 mg/kg. General anesthesia was achieved using isoflurane, nitrous oxide and oxygen following endotracheal intubation. Continuous pulse oximetry and electrocardiogram were carried out throughout the procedure. All procedures were performed with the animal in supine position. With the animal under general anesthesia, gastric lavage was performed and imaginary lesions were created by coagulation using a template (circular, diameter 30 mm). The template was introduced into the stomach endoscopically and extracted after coagulation. After resection, specimens were stretched and pinned onto a histology platform and examined for size and resection margins. Complications were managed endo-scopically. Periprocedural bleeding was managed by coagulation, perforations were managed by OTSC application. In the first animal additional laparotomy was used to further evaluate EMR+. One animal was used for several resections. All animals were euthanized immediately after the resections using intravenous pentobarbital.
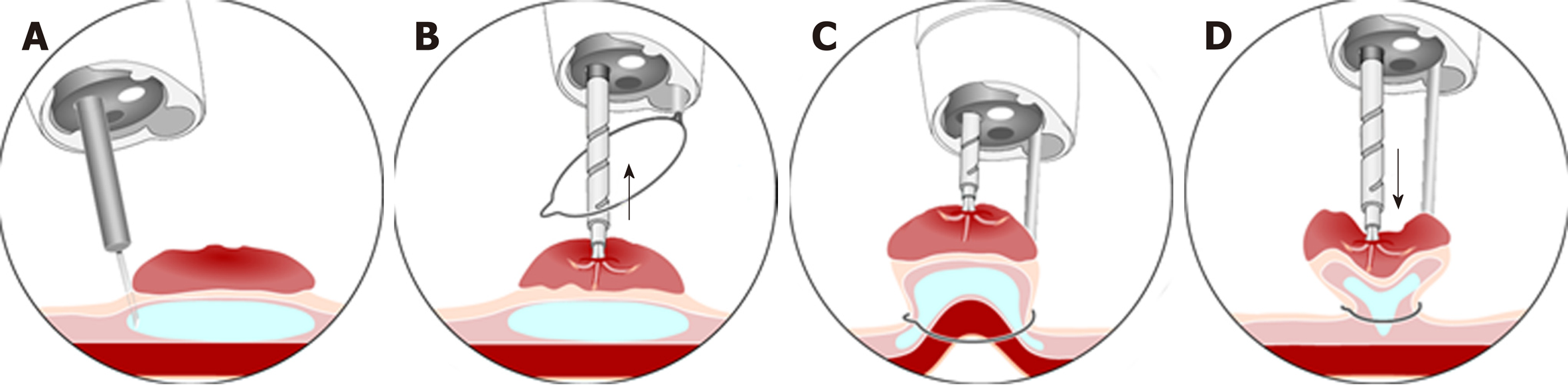
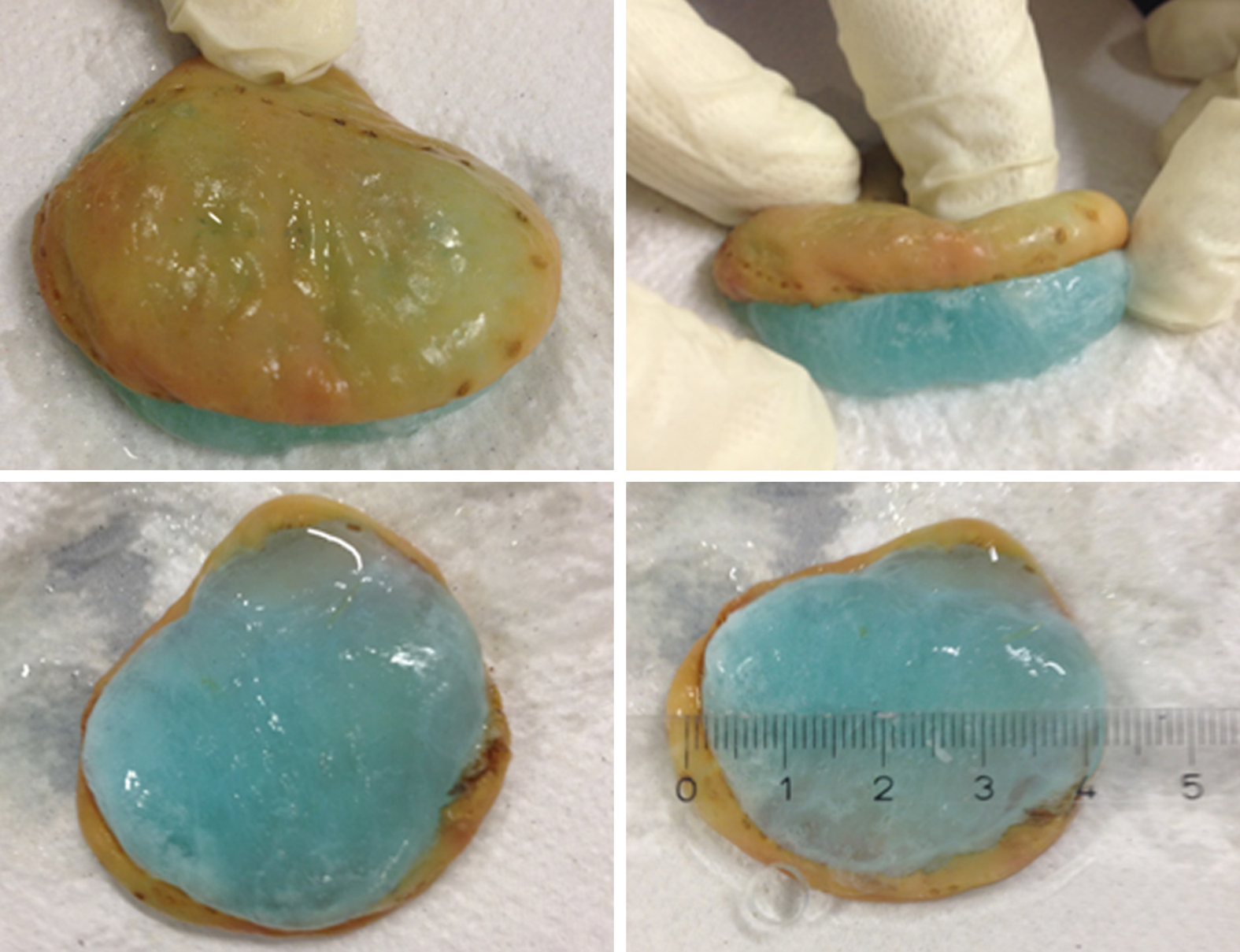
EMR+ was developed ex vivo (Figure 3). Resections were performed in the area of the greater curvature (endoscope in a relatively straight position). Initially, 2 ml of saline solution were injected into the submucosa to facilitate injection of LiftUp®. Then 5-8 mL of LiftUp® were used for submucosal injection to elevate the lesions (Figure 3A). The snare was advanced through the AWC. The anchor device (advanced through the conventional working channel) was used to improve positioning of the snare (Figure 3B). The lesion was pulled with the anchor and snare was closed (Figure 3C). Before resection the lesion was pushed back using the anchor to avoid perforation (Figure 3D). Using this protocol, 22 resections were performed ex vivo (Figure 4, Video 1). Median time for injection was 3 min (range 2-5, SD 0.86) and measured from injection to complete lifting of lesion and flushing with warm water. Median time for resection was 4 min (range 2-9, SD 1.57) and measured from snare opening to extraction of resection specimen. Median time of EMR+ (injection and resection) was 7 min (range 5-11, SD 1.68). Median size of specimen was 30 mm × 26 mm × 11 mm and ranged between 22 mm × 20 mm × 7 mm to 40 mm × 33 mm × 14.4 mm (Table 1).
| Resection | Specimen L × B × H (mm) | Time injection1 (min) | Time resection2 (min) | Time EMR+ (min) |
| 1 | 30 × 27 × 10 | 4 | 7 | 11 |
| 2 | 25 × 24 × 10.4 | 3 | 3 | 6 |
| 3 | 30 × 24 × 9.2 | 3 | 3 | 6 |
| 4 | 22 × 20 × 7 | 4 | 3 | 7 |
| 5 | 31 × 25 × 13.3 | 3 | 3 | 6 |
| 6 | 35 × 25 × 11.6 | 2 | 4 | 6 |
| 7 | 34 × 29 × 12.7 | 2 | 3 | 5 |
| 8 | 40 × 33 × 14.4 | 3 | 2 | 5 |
| 9 | 29 × 25 × 8.8 | 3 | 4 | 7 |
| 10 | 32 × 26 × 10.3 | 4 | 3 | 7 |
| 11 | 30 × 25 × 11.4 | 3 | 2 | 5 |
| 12 | 30 × 26 × 9.6 | 2 | 9 | 11 |
| 13 | 30 × 28 × 12,4 | 2 | 4 | 6 |
| 14 | 25 × 22 × 8.5 | 3 | 4 | 7 |
| 15 | 30 × 29 × 10.5 | 5 | 3 | 8 |
| 16 | 36 × 30 × 13.5 | 3 | 4 | 7 |
| 17 | 33 × 30 × 16.6 | 4 | 5 | 9 |
| 18 | 32 × 28 × 14.4 | 2 | 5 | 7 |
| 19 | 25 × 25 × 12.7 | 3 | 4 | 7 |
| 20 | 26 × 22 × 6.5 | 4 | 5 | 9 |
| 21 | 29 × 29 × 11.5 | 4 | 4 | 8 |
| 22 | 37 × 30 × 10.1 | 2 | 4 | 6 |
| Median | 30 × 26 × 11 | 3 | 4 | 7 |
After EMR+ was developed ex vivo the technique was transferred and evaluated in vivo (three domestic pigs). Resections were performed in the area of the greater curvature (endoscope in a relatively straight position). In the first animal perforations were observed due to excessive use of the anchor (Figure 3C). Perforations were managed by OTSC application. In consequence, laparotomy was used to further evaluate endoscopic technique in the same animal. It was observed that it is essential to push back the lesion with the anchor before resection (Video 2). The “Push Back” maneuver avoids inversion of the muscular layer into the lumen and subsequently protects from perforation (Figure 3D). After developing this last essential step of EMR+ in vivo no further perforations were observed.
13 resections were performed in vivo (animal two and three). Illustration of resection specimens and resection technique is shown in Figure 5 and Video 3. Median time for injection was 2 min (range 1-6, SD 1.23) and measured from injection until complete lifting of lesion. Median time for resection was 3 min (range 2-10, SD 2.47) and measured from snare opening to extraction of resection specimen. Median time of EMR+ (injection and resection) was 5 min (range 3-12, SD 2.72). Median size of specimen was 35 mm × 35 mm × 11 mm and ranged between 30 mm × 30 mm × 12 mm to 40 mm × 38 mm × 13.5 mm. Resection was macroscopic complete in 12/13 cases (92.3%). Major adverse events were not observed. In one case (7.7%) minor periprocedural bleeding was observed and managed by coagulation (Table 2).
| Resec-tion | SpecimenL × B × H (mm) | Time injection1 (min) | Time resection2 (min) | Time EMR+ (min) | Adverse events | Macroscopic complete |
| 1 | 40 × 35 × 10 | 2 | 6 | 8 | - | Yes |
| 2 | 40 × 35 × 11 | 6 | 3 | 9 | - | Yes |
| 3 | 40 × 38 × 13 | 2 | 6 | 8 | - | Yes |
| 4 | 40 × 38 × 13 | 2 | 10 | 12 | - | Yes |
| 5 | 30 × 30 × 12 | 2 | 6 | 8 | - | No |
| 6 | 35 × 35 × 11 | 2 | 4 | 6 | - | Yes |
| 7 | 40 × 40 × 11 | 2 | 2 | 4 | - | Yes |
| 8 | 35 × 35 × 9 | 1 | 2 | 3 | - | Yes |
| 9 | 35 × 35 × 13 | 2 | 2 | 4 | - | Yes |
| 10 | 35 × 38 × 10 | 3 | 2 | 5 | - | Yes |
| 11 | 40 × 35 × 14 | 1 | 2 | 3 | - | Yes |
| 12 | 35 × 35 × 9 | 2 | 3 | 5 | Minor bleeding3 | Yes |
| 13 | 35 × 35 × 8 | 2 | 2 | 4 | - | Yes |
| Median | 35 × 35 × 11 | 2 | 3 | 5 | - | - |
This study describes a novel resection technique for endoscopic en bloc resection (EMR+). The technique was considered as modified grasp and snare technique and included two major components. For submucosal injection a new agent (LiftUp®, Ovesco Endoscopy, Tübingen, Germany) with temperature-dependent viscosity was used. Efficacy and safety of LiftUp® has been shown recently in a preclinical study[18]. Once injected, LiftUp® forms a stable and permanent gel cushion which allows ER without re-injection. The agent is not yet commercially available but approval is pending and suspected in early 2019 in Europe. For resection a novel additional working channel (AWC®, Ovesco Endoscopy, Tübingen, Germany) was used. Successful clinical use of AWC® has been reported recently[19]. AWC® allows use of an additional working tool and is installed on the endoscope externally. Resection was performed as grasp and snare technique and included simultaneous use of an anchor device and monofilament resection snare. EMR+ was first developed and evaluated ex vivo (explanted pig stomach) and later transferred and evaluated in vivo in domestic pigs. In this study, EMR+ allowed for en bloc resection specimens up to 40 mm in diameter (median size ex vivo: 30 mm × 26 mm × 11 mm, median size in vivo: 35 mm × 35 mm × 11 mm). In vivo, macroscopic complete resection could be achieved in 92.3%. Median procedure time was fast (5 min in vivo). After developing final concept of EMR+ major adverse events were not observed. In one case (7.7%) minor periprocedural bleeding was observed in vivo and managed by coagulation.
Endoscopic en bloc and R0-resection is essential for adequate treatment of mucosal neoplasia and prevention of recurrency. However, EMR only is adequate for lesions > 20 mm and ESD is associated with higher risks for complications, especially in the western world. In consequence, new techniques for endoscopic en bloc resection for lesions > 20 mm are needed. Ideal resection technique should be effective and safe but as well fast and easy to perform.
Submucosal injection is essential for EMR and ESD. Different injection agents have been investigated but saline solution still is the standard solution used for ER[9]. Major limitation of isotonic saline solution is its fast absorption by the adjacent mucosa. To facilitate and maintain cushion formation other viscous and hypertonic solutions such as hydroxyethyl starch, sodium hyaluronate solution, 50% dextrose or succinylated gelatin have been investigated[8,10-13] but optimal agent is not defined or identified. Using viscous and hypertonic solution resulted in lower volumes to inject[10-12], longer duration of submucosal elevation and shorter procedure times[10,11] compared to saline solution. A recent meta-analysis (five randomized controlled trials, 504 patients) showed higher rates of en bloc resection and lower rates of residual lesions compared to saline solution when viscous and hypertonic solutions were used for EMR and polyps > 20 mm[9]. Rates of adverse events were similar.
Other agents with temperature-depended viscosity have been developed and investigated. Combination of hyaluronic acid, chondroitin sulfate and poloxamer 407 (Ziverel, Norgine, United Kingdom) showed prolonged submucosal elevation and absence of tissue damaging in a porcine model[20]. Combination of water, medium chain triglycerides, sodium chloride, polyoxyl-15-hydroxystearate and poloxamer 188 (Eleview®, Cosmo pharmaceuticals NV, Dublin, Ireland) showed prolonged submucosal elevation and safe application for EMR/ESD in preclinical[21] and clinical[22] trials. However, prolonged submucosal elevation (described up to 60 min) could not be confirmed clinically. Submucosal elevation was observed for 1-15 min and for ESD re-injections were still necessary[22]. Eleview® is approved as injection agent for ER in USA and Europe. In a recent study, Eleview® was compared with saline solution in a randomized double-blind setting[23]. Patients undergoing EMR for ≥ 20 mm colorectal non-pedunculated lesions were randomized 1:1 and 226 patients were included (mean lesion size 32 mm ± 12.4 mm). In the Eleview® arm total volume needed for EMR was significantly lower (approximately reduction of 50%). A trend for faster procedure times and higher en bloc resection rates was observed under Eleview® but statistical significance was not reached. Remarkably, macroscopic complete en bloc resection was only observed in 18.6% (Eleview®) vs 10.9% (saline solution). Rate of adverse events were similar in both arms. The agent for submucosal injection used in our study (LiftUp®) is comparable to Ziverel and Eleview® as agent includes poloxamers. In our ex vivo model duration of submucosal elevation using LiftUp® was observed for approximately one hour. However, submucosal lifting was not examined systematically and might be biased by inconsistent conditions of temperatures in the ex vivo model. In vivo, duration of submucosal lifting was not measured because study was focused on resection technique. The required volumes of LiftUp® were comparable to volumes of Eleview® used in the porcine model of Spadaccini et al[21].
Grasp and snare techniques have been investigated to optimize EMR procedure for lesions > 20 mm and were first described in 1976[24]. Double channel (DC) endoscopes allow simultaneous use of two different tools e.g. grasping device and resection snare. Using this technique, lesions in difficult locations or lesions with reduced lifting after submucosal injection can be resected[14-17]. The technique also allows reducing procedure time[25]. However, resection with DC endoscopes has not come to daily routine as instruments are more expensive and not widely available. The novel additional working channel (AWC®) used in our study provides an alternative option using two different endoscopic tools simultaneously. AWC® is designed for single use and installed on the endoscope externally. Different installations of AWC® allow variable positions of both working channels in contrast to DC endoscopes. Our modified grasp and snare technique (EMR+) could be accomplished with AWC® without observing technical problems.
Our study has strengths and limitations. Major strength of our study is a systematic development of a modified grasp and snare resection technique (EMR+) using two novel components (LiftUp® and AWC®). Major aim of this study was to develop a novel technique for endoscopic en bloc resection and proofing concept in vivo. Imaginary lesions had to be created in the stomach by circular coagulation. Major limitation of our study is the resection of regular mucosa in contrast to apparent mucosal neoplasia. Morphological features of lesions or existing fibrosis have a high impact on resectability. In consequence, clinical studies are needed to further evaluate EMR+. Notably, comparative trials (e.g., EMR+ vs ESD or EMR+ vs EMR with AWC® or EMR+ vs EMR with LiftUp®) are needed to further evaluate potential advantage of EMR+ over other resection techniques.
In conclusion, EMR+ is a novel modified grasp and snare technique for endoscopic en bloc resection. The technique includes two novel components (LiftUp® and AWC®) and was evaluated in vivo (porcine model). The technique appeared to be effective and safe and was easy and fast to perform in the porcine model. EMR+ needs to be further evaluated clinically in comparative trials.
Endoscopic en bloc and R0-resection is essential for adequate treatment of mucosal neoplasia. EMR is fast and safe but only adequate for lesions up to 20 mm of size. For lesions > 20 mm ESD is available. However, especially in the western world this technique might not be widely available and associated with higher risks for complications and longer procedure times.
To provide a fast and safe en bloc resection technique for lesions > 20 mm we developed a modified grasp and snare technique (EMR+) in a porcine model. We presumed that a novel technique might be interesting especially when ESD expertise is not available.
Major objective was to develop an effective, safe and fast technique for endoscopic en bloc resection for lesions > 20 mm of size.
EMR+ was first (October – December 2017) developed ex vivo in an explanted pig stomach. The technique included two novel components and was considered as a modified grasp and snare technique. We used an additional working channel (AWC®, Ovesco Endoscopy, Tübingen, Germany) to facilitate simultaneous application of a resection and grasping device. For submucosal injection we used a new agent with temperature-dependent viscosity (LiftUp®, Ovesco Endoscopy, Tübingen, Germany). EMR+ was then (April – July 2018) further evaluated in vivo (porcine model, stomach).
During the study period, 22 resections were performed ex vivo and 13 resections were performed in vivo. Median procedure time was fast (7 min ex vivo, 5 min in vivo) and median size of resections specimens was 30 mm × 26 mm × 11 mm/35 × 35 × 11 mm ex vivo/in vivo. Resection was macroscopically complete in vivo in 92.3%. Major adverse events were not observed.
EMR+ is a novel modified grasp and snare technique for endoscopic en bloc resection. The technique allowed safe and fast resection for lesions > 20 mm of size and was easy to perform in the porcine model. The novel injection agent allowed for sufficient protection of the muscular layer. Major limitation of our study was resection of regular mucosa in the stomach (imaginary lesions were created by circular coagulation).
To better define the role of EMR+ clinical and comparative trials are needed. Further studies need to address resection of apparent mucosal neoplasia in different anatomic locations.
Material support (endoscopic equipment, funding of the animal procedures and endotherapeutic material) for this study was provided by Ovesco Endoscopy, Tübingen, Germany.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Germany
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Harada H, Intagliata E S-Editor: Gong ZM L-Editor: A E-Editor: Zhang YL
| 1. | Woodward TA, Heckman MG, Cleveland P, De Melo S, Raimondo M, Wallace M. Predictors of complete endoscopic mucosal resection of flat and depressed gastrointestinal neoplasia of the colon. Am J Gastroenterol. 2012;107:650-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 2. | Ferlitsch M, Moss A, Hassan C, Bhandari P, Dumonceau JM, Paspatis G, Jover R, Langner C, Bronzwaer M, Nalankilli K, Fockens P, Hazzan R, Gralnek IM, Gschwantler M, Waldmann E, Jeschek P, Penz D, Heresbach D, Moons L, Lemmers A, Paraskeva K, Pohl J, Ponchon T, Regula J, Repici A, Rutter MD, Burgess NG, Bourke MJ. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2017;49:270-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 559] [Cited by in RCA: 765] [Article Influence: 95.6] [Reference Citation Analysis (0)] |
| 3. | Belderbos TD, Leenders M, Moons LM, Siersema PD. Local recurrence after endoscopic mucosal resection of nonpedunculated colorectal lesions: systematic review and meta-analysis. Endoscopy. 2014;46:388-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 293] [Cited by in RCA: 275] [Article Influence: 25.0] [Reference Citation Analysis (2)] |
| 4. | Matsuda T, Gotoda T, Saito Y, Nakajima T, Conio M. Our perspective on endoscopic resection for colorectal neoplasms. Gastroenterol Clin Biol. 2010;34:367-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Puli SR, Kakugawa Y, Gotoda T, Antillon D, Saito Y, Antillon MR. Meta-analysis and systematic review of colorectal endoscopic mucosal resection. World J Gastroenterol. 2009;15:4273-4277. [PubMed] |
| 6. | Gaglia A, Sarkar S. Evaluation and long-term outcomes of the different modalities used in colonic endoscopic mucosal resection. Ann Gastroenterol. 2017;30:145-151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Moss A, Williams SJ, Hourigan LF, Brown G, Tam W, Singh R, Zanati S, Burgess NG, Sonson R, Byth K, Bourke MJ. Long-term adenoma recurrence following wide-field endoscopic mucosal resection (WF-EMR) for advanced colonic mucosal neoplasia is infrequent: results and risk factors in 1000 cases from the Australian Colonic EMR (ACE) study. Gut. 2015;64:57-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 393] [Cited by in RCA: 367] [Article Influence: 36.7] [Reference Citation Analysis (0)] |
| 8. | Kishihara T, Chino A, Uragami N, Yoshizawa N, Imai M, Ogawa T, Igarashi M. Usefulness of sodium hyaluronate solution in colorectal endoscopic mucosal resection. Dig Endosc. 2012;24:348-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Yandrapu H, Desai M, Siddique S, Vennalganti P, Vennalaganti S, Parasa S, Rai T, Kanakadandi V, Bansal A, Titi M, Repici A, Bechtold ML, Sharma P, Choudhary A. Normal saline solution versus other viscous solutions for submucosal injection during endoscopic mucosal resection: a systematic review and meta-analysis. Gastrointest Endosc. 2017;85:693-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 71] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 10. | Katsinelos P, Kountouras J, Paroutoglou G, Chatzimavroudis G, Zavos C, Pilpilidis I, Gelas G, Paikos D, Karakousis K. A comparative study of 50% dextrose and normal saline solution on their ability to create submucosal fluid cushions for endoscopic resection of sessile rectosigmoid polyps. Gastrointest Endosc. 2008;68:692-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Fasoulas K, Lazaraki G, Chatzimavroudis G, Paroutoglou G, Katsinelos T, Dimou E, Geros C, Zavos C, Kountouras J, Katsinelos P. Endoscopic mucosal resection of giant laterally spreading tumors with submucosal injection of hydroxyethyl starch: comparative study with normal saline solution. Surg Laparosc Endosc Percutan Tech. 2012;22:272-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Moss A, Bourke MJ, Metz AJ. A randomized, double-blind trial of succinylated gelatin submucosal injection for endoscopic resection of large sessile polyps of the colon. Am J Gastroenterol. 2010;105:2375-2382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 101] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 13. | Yoshida N, Naito Y, Inada Y, Kugai M, Kamada K, Katada K, Uchiyama K, Ishikawa T, Takagi T, Handa O, Konishi H, Yagi N, Kokura S, Wakabayashi N, Yanagisawa A, Yoshikawa T. Endoscopic mucosal resection with 0.13% hyaluronic acid solution for colorectal polyps less than 20 mm: a randomized controlled trial. J Gastroenterol Hepatol. 2012;27:1377-1383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 42] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | de Melo SW, Cleveland P, Raimondo M, Wallace MB, Woodward T. Endoscopic mucosal resection with the grasp-and-snare technique through a double-channel endoscope in humans. Gastrointest Endosc. 2011;73:349-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Kwon KA. Is the double channel gastroscope useful in endoscopic mucosal resection for large sessile colon polyps? Clin Endosc. 2015;48:89-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Shetty A, Suarez AL, Dufault DL, Mcvey MC, Elmunzer BJ. Endoscopic mucosal resection with grasp-and-snare technique for challenging lesions. Gastrointest Endosc. 2016;84:738-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | von Renteln D, Schmidt A, Vassiliou MC, Rudolph HU, Caca K. Endoscopic mucosal resection using a grasp-and-snare technique. Endoscopy. 2010;42:475-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Wedi E, Ho CN, Conrad G, Weiland T, Freidinger S, Wehrmann M, Meining A, Ellenrieder V, Gottwald T, Schurr MO, Hochberger J. Preclinical evaluation of a novel thermally sensitive co-polymer (LiftUp) for endoscopic resection. Minim Invasive Ther Allied Technol. 2019;1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Walter B, Schmidbaur S, Krieger Y, Meining A. Improved endoscopic resection of large flat lesions and early cancers using an external additional working channel (AWC): a case series. Endosc Int Open. 2019;7:E298-E301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Fernández-Esparrach G, Cuatrecasas M, Rodríguez de Miguel C, Sánchez-Montes C, Córdova H. Efficacy and safety of a combination of hyaluronic acid, chondroitin sulfate, and poloxamer 407 as a submucosal injection solution for endoscopic resection: pilot study on a swine model. Endosc Int Open. 2017;5:E450-E454. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Spadaccini M, Hassan C, Maselli R, D'Amico F, Lamonaca L, Craviotto V, Repici A. Efficacy and safety of SIC-8000 (Eleview®) for submucosal injection for endoscopic mucosal resection and endoscopic submucosal dissection in an in vivo porcine model. Dig Liver Dis. 2018;50:260-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Girotra M, Triadafilopoulos G, Friedland S. Utility and performance characteristics of a novel submucosal injection agent (EleviewTM) for endoscopic mucosal resection and endoscopic submucosal dissection. Transl Gastroenterol Hepatol. 2018;3:32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 23. | Repici A, Wallace M, Sharma P, Bhandari P, Lollo G, Maselli R, Hassan C, Rex DK. A novel submucosal injection solution for endoscopic resection of large colorectal lesions: a randomized, double-blind trial. Gastrointest Endosc. 2018;88:527-535.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 49] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 24. | Martin TR, Onstad GR, Silvis SE, Vennes JA. Lift and cut biopsy technique for submucosal sampling. Gastrointest Endosc. 1976;23:29-30. [PubMed] |
| 25. | Voudoukis E, Tribonias G, Tavernaraki A, Theodoropoulou A, Vardas E, Paraskeva K, Chlouverakis G, Paspatis GA. Use of a double-channel gastroscope reduces procedural time in large left-sided colonic endoscopic mucosal resections. Clin Endosc. 2015;48:136-141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |