Published online Jun 28, 2019. doi: 10.3748/wjg.v25.i24.3091
Peer-review started: March 1, 2019
First decision: April 5, 2019
Revised: May 3, 2019
Accepted: May 31, 2019
Article in press: June 1, 2019
Published online: June 28, 2019
Processing time: 121 Days and 11.4 Hours
Endoscopic retrograde cholangiopancreatography (ERCP) in patients with Billroth II gastrectomy has been considered a challenging procedure due to the surgically altered gastrointestinal anatomy. However, there has been a paucity of comparative studies regarding ERCP in Billroth II gastrectomy cases because of procedure-related morbidity and mortality and practical and ethical limitations. This systematic and comprehensive review was performed to obtain a recent perspective on ERCP in Billroth II gastrectomy patients.
To systematically review the literature regarding ERCP in Billroth II gastrectomy patients.
A systematic review was performed on the literature published between May 1975 and January 2019. The following electronic databases were searched: PubMed, EMBASE, and Cochrane Library. The outcomes of successful afferent loop intubation and successful selective cannulation and occurrence of adverse events were assessed.
A total of 43 studies involving 2669 patients were included. The study designs were 36 (83.7%) retrospective cohort studies, 4 (9.3%) retrospective comparative studies, 2 (4.7%) prospective comparative studies, and 1 (2.3%) prospective cohort study. Of a total of 2669 patients, there were 1432 cases (55.6%) of side-viewing endoscopy, 664 (25.8%) cases of forward-viewing endoscopy, 171 (6.6%) cases of balloon-assisted enteroscopy, 169 (6.6%) cases of anterior oblique-viewing endoscopy, 64 (2.5%) cases of dual-lumen endoscopy, 31 (1.2%) cases of colonoscopy, and 14 (0.5%) cases of multiple bending endoscopy. The overall success rate of afferent loop intubation was 91.3% (2437/2669), and the overall success rate of selective cannulation was 87.9% (2346/2437). A total of 195 cases (7.3%) of adverse events occurred. The success rates of afferent loop intubation and the selective cannulation rate for each type of endoscopy were as follows: side-viewing endoscopy 98.2% and 95.3%; forward-viewing endoscopy 97.4% and 95.2%; balloon-assisted enteroscopy 95.4% and 97.5%; oblique-viewing endoscopy 94.1% and 97.5%; and dual-lumen endoscopy 82.8% and 100%, respectively. The rate of bowel perforation was slightly higher in side-viewing endoscopy (3.6%) and balloon-assisted enteroscopy (4.1%) compared with forward-viewing endoscopy (1.7%) and anterior oblique-viewing endoscopy (1.2%). Mortality only occurred in side-viewing endoscopy (n = 9, 0.6%).
The performance of ERCP in the Billroth II gastrectomy population has been improving with choice of various type of endoscope and sphincter management. More comparative studies are needed to determine the optimal strategy to perform safe and effective ERCP in Billroth II gastrectomy patients.
Core tip: Endoscopic retrograde cholangiopancreatography (ERCP) in Billroth II gastrectomy anatomy has been considered a difficult procedure due to the surgical alteration. To date, there has been a paucity of comparative studies regarding ERCP in Billroth II gastrectomy patients. In current study, we systematically and comprehensively reviewed the literatures regarding ERCP in Billroth II gastrectomy cases. The performance of ERCP in the Billroth II gastrectomy has been improving with choice of various type of endoscope and sphincter therapy. More comparative studies are required to perform effective and safe ERCP in Billroth II gastrectomy population.
- Citation: Park TY, Song TJ. Recent advances in endoscopic retrograde cholangiopancreatography in Billroth II gastrectomy patients: A systematic review. World J Gastroenterol 2019; 25(24): 3091-3107
- URL: https://www.wjgnet.com/1007-9327/full/v25/i24/3091.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i24.3091
Billroth II gastrectomy commonly encounters a challenging surgically altered anatomy when performing endoscopic retrograde cholangiopancreatography (ERCP). The difficulties in performing ERCP in patients with Billroth II gastrectomy include the identification and intubation of the afferent loop, visualization of the papilla, selective cannulation of the desired biliary or pancreatic duct, and sphincter therapy due to the reverse direction of the papilla[1,2]. As a result, the safety and failure of ERCP have always been a major concern in Billroth II gastrectomy patients.
For successful and safe ERCP in Billroth II gastrectomy patients, there have been many choices for the selection of endoscopy other than conventional side-viewing endoscopy, such as forward-viewing endoscopy (with or without cap-fitting)[3,4], balloon-assisted enteroscopy (single-balloon or double-balloon)[5,6], anterior oblique-viewing endoscopy (with or without overtube-assisted)[7,8], dual-lumen endoscopy[9], and multiple bending endoscopy[10]; choices for sphincter therapy, such as endoscopic sphinc-terotomy (EST), endoscopic papillary balloon dilation (EPBD), and endoscopic papillary large balloon dilation (EPLBD)[11-13]; and choices for accessories, such as a needle knife (NK) and rotatable or dedicated inverted papillotome[14,15].
To date, there has been a paucity of comparative studies regarding ERCP in Billroth II gastrectomy cases because of procedure-related morbidity and mortality and practical and ethical limitations. To obtain a more recent perspective on ERCP in Billroth II gastrectomy, we systematically and comprehensively reviewed the literature regarding ERCP in Billroth II gastrectomy patients. In detail, the aims of our study were: (1) To assess the success rate of afferent loop intubation, the success rate of selective cannulation, and rate of adverse events in ERCP in Billroth II gastrectomy patients; (2) To assess these outcomes according to each type of endoscopy; (3) To assess clinical efficacy according to each type of sphincter management methods.
This systematic review was conducted according to the PRISMA guidelines[16]. Electronic databases, including MEDLINE (PubMed), EMBASE, and Cochrane Library, were searched for all studies published from May 1975 to January 2019. The search terms included “Billroth II gastrectomy” or “Billroth II operation,” or “gastrectomy” and “endoscopic retrograde cholangiopancreatography” or “endoscopic retrograde” combined with “cholangiopancreatography,” or “ERCP.” Two investigators (T.Y.P. and T.J.S.) independently performed the search of the electronic databases and assessed the eligibility of all the studies searched from the databases according to the predetermined selection criteria. Disagreements between evaluators were resolved through discussion.
Studies were included in the systematic review if they met all of the following criteria: (1) Relevant clinical studies of ERCP in patients with prior Billroth II gastrectomy; (2) Studies that enrolled at least 10 Billroth II gastrectomy patients; (3) Studies with full text available; (4) Studies with available information on the patient number, indications for the ERCP, type of endoscopy, type of sphincter therapy, success rate of afferent loop intubation, success rate of selective cannulation, occurrence of adverse events including bowel perforation, post-ERCP pancreatitis, bleeding, cardiopulmonary events and mortality; and (5) Studies written in English. Studies were excluded from the current review if they met any of the following criteria: (1) Irrelevancy to ERCP in Billroth II gastrectomy patients; (2) Fewer than ten patients; (3) Review, abstract only article, commentary, and letter; (4) Non-human study; and (5) Languages other than English.
Data of the sample size, study design, indications for the procedure, type of endoscopy (side-viewing endoscopy, forward-viewing endoscopy, double-balloon enteroscopy, single-balloon enteroscopy, anterior oblique-viewing endoscopy, overtube-assisted endoscopy, multi-bending endoscopy, or dual-lumen endoscopy), type of sphincter therapy (EST, EPBD, EPLBD, NK), success rate of afferent loop intubation, success rate of selective cannulation, occurrence of adverse events including bowel perforation, post-ERCP pancreatitis, procedure-related bleeding, cardiopulmonary events, and mortality were extracted from the included studies. Subgroup analysis of successful afferent loop intubation, successful selective cannulation, bowel perforation, post-ERCP pancreatitis, bleeding, and mortality according to the type of endoscopy was performed. And clinical outcomes according to the type of sphincter therapy was also evaluated. Clinical success was defined as the achievement of the planned therapeutic goals including bile duct stone clearance, endobiliary biopsy, biliary stent or nasobiliary catheter insertion. Data extraction was carried out by two independent reviewers (T.Y.P. and T.J.S.) using a standardized table. Discrepancies were resolved by discussion.
The primary outcome was to assess the efficacy of ERCP in Billroth II gastrectomy patients by afferent loop intubation and the selective cannulation of the desired duct as well as the safety according to procedure-related adverse events, such as bowel perforation, post-ERCP pancreatitis, bleeding, cardiopulmonary events, and mortality. The secondary outcome was to compare the rate of afferent loop intubation, selective cannulation, and adverse events according each type of endoscope. The categorical variables were reported as the frequency with respective proportions (percentages). The pooled rate of outcome measures was calculated by dividing the percentage of patients or procedures from the included studies.
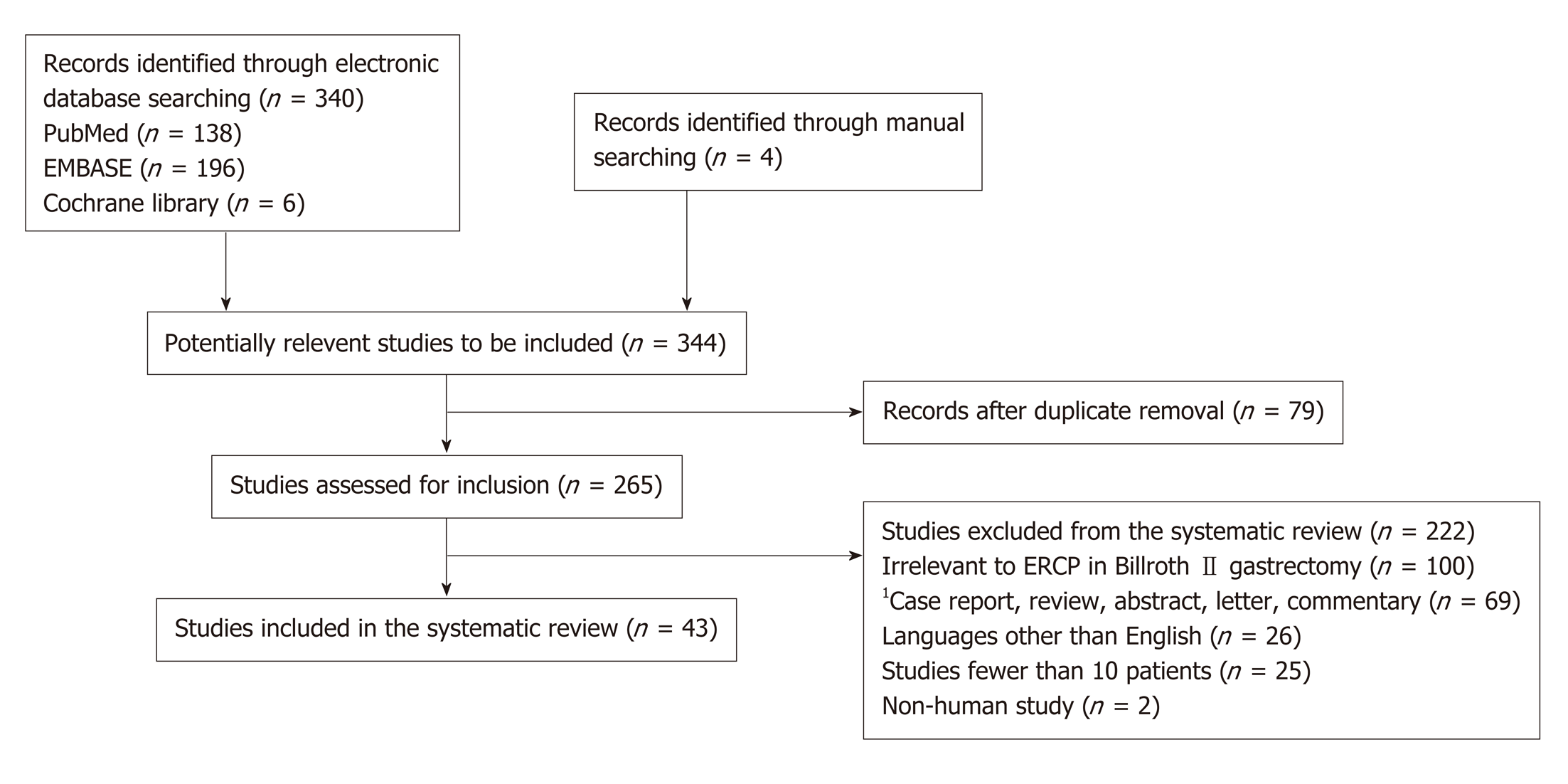
The flow diagram of the study identification, screening, eligibility, and inclusion process is shown in Figure 1. A total of 344 studies were identified through an electronic search of 3 databases and manual search of the relevant bibliographies. Of them, 79 duplicate studies were removed during the initial screening. Then, through a review of the titles and abstracts, 100 studies irrelevant to ERCP in Billroth II gastrectomy patients were excluded. After a thorough review of 265 relevant studies, 222 studies were excluded from the systematic review. The reasons for study exclusion were as follows: Case report (n = 28), languages other than English (n = 26), fewer than 10 patients (n = 25), review (n = 15), abstract (n = 13), letter (n = 7), commentary (n = 6), and non-human study (n = 2). The remaining 43 studies were included in the final analysis.
The characteristics of the 43 studies are listed in Table 1. The published year ranged from 1984 to 2018. Most of the studies were retrospective single-arm studies, and the most common indications for ERCP were common bile duct (CBD) stones and pancreaticobiliary malignancies. There were six studies that included more than 100 Billroth II gastrectomy patients and, among them, three studies[17-19] were published in recent years. The detailed characteristics of the recently published studies including more than 100 Billroth II gastrectomy cases are summarized in Table 2.
| Study | Study design | No. | Indications for ERCP | Type of endoscope | Sphincter therapy | A-loop intubation, No. (%) | Selective cannulation, No. (%) | Adverse events |
| Forbes and Cotton[1], 1984 | Retrospective cohort | 53 | N/A | S | EST | 45/53 (84.9) | 35/45 (77.8) | Bowel perforation (n = 1, 1.9%) |
| Osnes et al[2], 1986 | Retrospective cohort | 147 | N/A | S | EST | 134/147 (91.2) | 134/134 (100) | Bowel perforation (n = 1, 0.7%) |
| Pancreatitis (n = 1, 0.7%) | ||||||||
| Bleeding (n = 1, 0.7%) | ||||||||
| Mortality (n = 2, 1.4%) | ||||||||
| Hintze et al[31], 1997 | Retrospective cohort | 59 | CBD stone | S | EST | 54/59 (91.5) | 54/54 (100) | Bowel perforation (n = 1, 1.7%) |
| Papillary stenosis | Mortality (n = 1, 1.7%) | |||||||
| Tumor stenosis | ||||||||
| Juxtapapillary diverticulum | ||||||||
| Kim et al[3], 1997 | Prospective comparative | 45 | N/A | F (n = 23) | EST±NK | 44/45 | 36/44 (80.0) | Bowel perforation (n = 4, 8.9%) |
| (97.8) | ||||||||
| S (n = 22) | Pancreatitis (n = 3, 2.2%) | |||||||
| Lin et al[32], 1999 | Retrospective cohort | 56 | CBD stone | F | EST | 43/56 (76.6) | 35/43 (81.3) | Bleeding (n = 3, 5.4%) |
| CBD dilation | ||||||||
| RUQ pain with cholestasis | ||||||||
| Faylona et al[33], 1999 | Retrospective cohort | 110 | Cholangitis (n = 58) | S | EST | 2132/185 (71.4) | 2122/132 (92.4) | Bowel perforation (n = 11, 5.9%) |
| CBD stone (n = 41) | Pancreatitis (n = 1, 0.5%) | |||||||
| Jaundice (n = 28) | ||||||||
| CBD dilation (n = 19) | Bleeding (n = 3, 1.6%) | |||||||
| Pancreatitis (n = 9) | Mortality (n = 2, 1.1%) | |||||||
| Others (n = 30) | ||||||||
| Bergman et al[11], 2001 | Prospective comparative | 34 | CBD stone (n = 34) | S | EST/EPBD | N/A | 28/34 (82.4) | Bowel perforation (n = 1, 2.9%) |
| Pancreatitis (n = 1, 2.9%) | ||||||||
| Bleeding (n = 3, 8.8%) | ||||||||
| Respiratory insufficiency (n = 1, 2.9%) | ||||||||
| Swarnkar et al[34], 2005 | Retrospective cohort | 41 | CBD stone (n = 16) | S | EST | 242/48 (87.5) | 241/42 (97.6) | Bowel perforation (n = 1, 2.1%) |
| CBD dilation (n = 9) | ||||||||
| Pancreatitis (n = 4) | ||||||||
| Gastric cancer (n = 3) | ||||||||
| Pancreatic cancer (n = 2) | ||||||||
| Others (n = 7) | ||||||||
| Bleeding (n = 2, 4.2%) | ||||||||
| Kikuyama et al[35], 2005 | Retrospective cohort | 24 | CBD stone (n = 14) | AOE | EST | 24/24 (100) | 22/24 (91.7) | Bowel perforation (n = 1, 4.2%) |
| Pancreaticobiliary malignancy (n = 8) | Pancreatitis (n = 1, 4.2%) | |||||||
| Bleeding (n = 1, 4.2%) | ||||||||
| Others (n = 2) | ||||||||
| Ciçek et al[36], 2006 | Retrospective cohort | 52 | CBD stone (n = 27) | S | EST±NK | 45/52 (94.2) | 43/45 (95.6) | Bowel perforation (n = 6, 11.5%) |
| Jaundice (n = 11) | Bleeding (n = 3, 1.6%) | |||||||
| Pancreatico-biliary malignancy (n = 10) | ||||||||
| (n = 2, 3.8%) | ||||||||
| Bile leakage (n = 2) | ||||||||
| Others (n = 2) | ||||||||
| Park et al[37], 2007 | Retrospective cohort | 10 | CBD stone (n = 9) | 1F | EST | 10/10 (100) | 10/10 (100) | None |
| CBD stricture (n = 1) | ||||||||
| Dolay and Soylu[38], 2008 | Retrospective cohort | 11 | S | EST | 11/11 (100) | 11/11 (100) | None | |
| Nakahara et al[39], 2009 | Retrospective comparative | 43 | CBD stone (n = 43) | AOE | EST/EPBD±NK | 38/43 (88.4) | 36/38 (94.7) | None |
| Koo et al[10], 2009 | Retrospective cohort | 14 | CBD stone (n = 8) | Multiple bending endoscope | EST/EPBD | 14/14 (100) | 13/14 (92.9) | None |
| Biliary pancreatitis (n = 2) | ||||||||
| Pancreatico-biliary malignancy (n = 3) | ||||||||
| Bile leakage after cholecystectomy (n = 1) | ||||||||
| Shimatani et al[40], 2009 | Retrospective cohort | 17 | N/A | DBE | EST/EPBD | 222/22 (100) | 222/22 (100) | None |
| Kikuyama et al[41], 2009 | Retrospective cohort | 11 | CBD stone (n = 8) | AOE with over tube | EST/EPBD | 210/15 (66.7) | 210/10 (100) | None |
| Pancreatico-biliary malignancy (n = 3) | ||||||||
| Chronic pancreatitis (n = 1) | ||||||||
| Lin et al[42], 2010 | Retrospective cohort | 32 | N/A | S (n = 22) | EPBD | 30/32 (68.8) | 28/30 (93.3) | Bowel perforation (n = 2, 6.3%) |
| DBE (n = 8) | ||||||||
| Itoi et al[12], 2010 | Retrospective cohort | 11 | CBD stone (n = 11) | F (n = 8) | EST+EPLBD | 11/11 (100) | 11/11 (100) | None |
| S (n = 1) | ||||||||
| AOE (n = 1) | ||||||||
| SBE (n = 1) | ||||||||
| Lee et al[30], 2012 | Retrospective cohort | 13 | CBD stone (n = 13) | 1F | EPLBD | 13/13 (100) | 12/13 (92.3) | Bleeding (n = 1, 7.7%) |
| Byun et al[43], 2012 | Retrospective cohort | 46 | CBD stone (n = 37) | F | EST+EPBD | 42/46 (91.3) | 42/42 (100) | Bowel perforation (n = 1, 2.2%) |
| Pancreatico-biliary malignancy (n = 5) | Pancreatitis (n = 1, 2.2%) | |||||||
| Benign biliary stricture (n = 4) | ||||||||
| Choi et al[44], 2012 | Retrospective comparative | 26 | CBD stone (n = 26) | S (n = 13) | EST±EPBD | 26/26 (100) | 26/26 (100) | None |
| F (n = 13) | ||||||||
| Kianicka et al[45], 2012 | Retrospective cohort | 120 | Cholestasis (n = 100) | F | EST | 109/120 (90.8) | 109/120 (90.8) | Bowel perforation (n = 1, 0.8%) |
| Biliary pancreatitis (n = 12) | Pancreatitis (n = 2, 1.7%) | |||||||
| Acute cholangitis (n = 6) | Bleeding (n = 2, 1.7%) | |||||||
| Bile leakage (n = 2) | ||||||||
| Osoegawa et al[27], 2012 | Retrospective cohort | 15 | N/A | DBE | EST/EPBD±NK | 218/19 (94.7) | 216/18 (88.9) | Bowel perforation (n = 1, 0.5%) |
| Sen-Yo et al[46], 2012 | Retrospective comparative | 65 | CBD stone (n = 38) | AOE | EST/EPBD±NK | 60/65 (92.3) | 60/60 (100) | Bowel perforation (n = 1, 1.5%) |
| Pancreatico-biliary malignancy (n = 17) | Pancreatitis (n = 3, 4.6%) | |||||||
| Cholangitis (n = 2, 3.0%) | ||||||||
| Other malignancy (n = 2) | ||||||||
| Chronic pancreatitis (n = 2) | ||||||||
| Bile leakage (n = 2) | ||||||||
| Others (n = 4) | ||||||||
| Jang et al[47], 2013 | Retrospective cohort | 40 | CBD stones (n = 40) | S | EPLBD±NK | 40/40 (100) | 40/40 (100) | Pancreatitis (n = 2, 5.0%) |
| Yao et al[9], 2013 | Retrospective cohort | 46 | CBD stone (n = 38) | Dual-lumen gastroscope | EST/EPBD | 38/46 (82.6) | 38/38 (100) | None |
| Biliary stricture (n = 3) | ||||||||
| Pancreatico-biliary malignancy (n = 5) | ||||||||
| Kawamura et al[48], 2013 | Retrospective comparative | 65 | CBD stone (n = 49) | F (n = 56) | N/A | 61/65 (93.8) | 51/61 (83.6) | Bowel perforation (n = 2, 3.1%) |
| Pancreatico-biliary malignancy (n = 26) | S (n = 2) | Pancreatitis (n = 4, 6.2%) | ||||||
| SBE (n = 3) | ||||||||
| Others (n = 4) | Bleeding (n = 1, 1.5%) | |||||||
| Benign biliary stricture (n = 1) | ||||||||
| Kim et al[49], 2014 | Retrospective cohort | 30 | CBD stone (n = 30) | S | EPLBD±EST | 30/30 (100) | 30/30 (100) | Pancreatitis (n = 2, 6.7%) |
| Bleeding (n = 2, 6.7%) | ||||||||
| Iwai et al[50], 2014 | Retrospective comparative | 19 | N/A | SBE | N/A | 18/19 (95) | 18/18 (100) | None |
| Cheng et al[51], 2015 | Retrospective cohort | 77 | CBD stone (n = 77) | DBE | EPLBD/ EPBD±NK | 73/77 (95) | 67/73 (92) | Bowel perforation (n = 3, 3.8%) |
| Intestinal mucosal tear (n = 2, 2.6%) | ||||||||
| Jang et al[52], 2015 | Retrospective cohort | 36 | CBD stone (n = 28) | 1F | EPBD± EST | 36/36 (100) | 32/36 (88.9) | Bowel perforation (n = 3, 8.3%) |
| Benign biliary stricture (n = 6) | Pancreatitis ((n = 2, 5.6%) | |||||||
| Pancreatico-biliary malignancy (n = 1) | ||||||||
| Post-operative bile leakage (n = 1) | ||||||||
| Ki et al[53], 2015 | Retrospective cohort | 72 | CBD stone (n = 55) | 1F | EST/EPBD | 2125/126 (99.2) | 2125/125 (100) | Bowel perforation (n = 1, 0.7%) |
| Cholangitis (n = 11) | ||||||||
| CBD stricture (n = 7) | ||||||||
| Pancreatico-biliary malignancy (n = 3) | ||||||||
| IHD stone (n = 2) | ||||||||
| Pancreatitis (n = 3, 2.2%) | ||||||||
| Bleeding (n = 8, 5.9%) | ||||||||
| Nakahara et al[54], 2015 | Retrospective cohort | 25 | CBD stone (n = 15) | AOE | EST/EPBD | 226/30 (86.7) | 226/26 (100) | Pancreatitis (n = 1, 3.3%) |
| Pancreatico-biliary malignancy (n = 7) | ||||||||
| Chronic pancreatitis (n = 3) | ||||||||
| Bove et al[17], 2015 | Retrospective cohort | 713 | CBD stone (n = 365) | S (n = 600) | EST | 618/713 (86.7) | 580/618 (93.8) | Bowel perforation (n = 22, 3.1%) |
| F (n = 18) | ||||||||
| Obstructive jaundice (n = 177) | Pancreatitis (n = 5, 0.7%) | |||||||
| Acute cholangitis (n = 61) | ||||||||
| Chronic pancreatitis (n = 55) | Bleeding (n = 11, 1.5%) | |||||||
| Biliary pancreatitis (n = 21) | ||||||||
| Mortality (n = 2, 0.3%) | ||||||||
| Benign biliary stricture (n = 9) | ||||||||
| Others (n = 5) | ||||||||
| Wu et al[18], 2016 | Retrospective cohort | 135 | CBD stone/cholangitis | S | EST+EPBD | 120/135 (88.8) | 117/135 (86.3) | 2Bowel perforation (n = 1, 0.7%) |
| Benign biliary stricture | Pancreatitis (n = 9, 4.1%) | |||||||
| Bleeding (n = 2, 0.9%) | ||||||||
| Park et al[19], 2016 | Retrospective cohort | 165 | CBD stone (n = 133) | 1F | EPBD±NK | 151/165 | 144/151 | Bowel perforation (n = 3, 1.8%) |
| Benign biliary stricture (n = 21) | (91.5) | (95.4) | Pancreatitis (n = 13, 7.9%) | |||||
| Pancreatico-biliary malignancy (n = 11) | ||||||||
| Hyperamylasemia (n = 22, 13.3%) | ||||||||
| Wang et al[28], 2016 | Retrospective cohort | 18 | CBD stone (n = 15) | Dual-lumen gastroscope | EST/EPBD | 15/18 (83.3) | 15/15 (100) | Pancreatitis (n = 2, 11.1%) |
| Pancreatico-biliary malignancy (n = 3) | Bleeding (n = 1, 5.6%) | |||||||
| Wang et al[29], 2016 | Retrospective cohort | 52 | CBD stone (n = 38) | C (n = 31) | EST/EPBD±NK | 50/52 (96.2) | 50/52 (96.2) | Pancreatitis (n = 2, 3.8%) |
| Biliary stricture (n = 9) | F (n = 13) | Hyperamylasemia (n = 2, 3.8%) | ||||||
| Pancreatico-biliary malignancy (n = 5) | S (n = 11) | |||||||
| Shimatani et al[25], 2016 | Prospective cohort | 26 | Cholangitis (n = 13) | DBE | EST | 25/26 (96.2) | 25/25 (100) | Bowel perforation (n = 2, 7.7%) |
| Hepatobiliary disorder (n = 4) | Pancreatitis (n = 5, 19.2%) | |||||||
| Obstructive jaundice (n = 4) | Cholangitis (n = 1, 3.8%) | |||||||
| CBD stone (n = 2) | ||||||||
| Aspiration pneumonia (n = 1, 3.8%) | ||||||||
| Others (n = 3) | ||||||||
| Shimatani et al[55], 2017 | Retrospective cohort | 11 | CBD stone (n = 7) | DBE | EST | 11/11 (100) | 11/11 (100) | None |
| Obstructive jaundice (n = 2) | ||||||||
| Others (n = 2) | ||||||||
| Yane et al[26], 2017 | Retrospective cohort | 20 | CBD stone | SBE | N/A | 20/20 (100) | 19/20 (95) | Bowel perforation (n = 2, 1.0%) |
| Bile duct stricture | Pancreatitis (n = 3, 1.5%) | |||||||
| Aanstomosis site stricture | Cholangitis (n = 4, 2.0%) | |||||||
| Cholecystitis (n = 1, 0.5%) | ||||||||
| Li et al[56], 2017 | Retrospective cohort | 49 | CBD stone (n = 49) | S | EPBD | N/A | 42/49 (85.7) | Pancreatitis (n = 3, 6.1%) |
| Han et al[57], 2018 | Retrospective cohort | 15 | CBD stone (n = 15) | 1F | EST/EPBD±NK | 15/15 (100) | 15/15 (100) | Pancreatitis (n = 1, 6.7%) |
| Bove et al[17], 2015 | Wu et al[18], 2016 | Park et al[19], 2016 | |
| (n = 713) | (n = 135) | (n = 165) | |
| Study design | Retrospective cohort in single center | Retrospective cohort in single center | Retrospective cohort in 5 centers |
| Male gender, n (%) | 567 (79.5) | N/A | 116 (70.3) |
| Age (yr), n (%) or mean ± SD | > 60 yr, 565 (79.2) | N/A | 71.1 ± 10.0 |
| Type of endoscope | Side-viewing or forward-viewing | Side-viewing | Cap-fitting forward- viewing |
| Type of sphincter therapy | EST | EST | EPBD±NK |
| Success of afferent loop intubation, n (%) | 618/713 (86.7) | 120/135 (88.8) | 151/165 (91.5) |
| Success of selective cannulation, n (%) | 580/618 (93.8) | 117/120 (97.5) | 144/151 (95.4) |
| Bowel perforation, n (%) | 22/713 (3.1) | 1/135 (0.7) | 3/165 (1.8) |
| Post-ERCP pancreatitis, n (%) | 5/713 (0.7) | N/A | 13/165 (7.9) |
| Bleeding, n (%) | 11/713 (1.5) | N/A | - |
| Mortality, n (%) | 2/713 (0.3) | - | - |
The results of the current systematic review are shown in Table 3. Of the 43 included studies, there were 36 (83.7%) retrospective cohort studies, 4 (9.3%) retrospective comparative studies, 2 (4.7%) prospective comparative studies, and 1 (2.3%) prospective cohort study. There were 2669 identified patients in total. Conventional side-viewing endoscopy (n = 1432, 55.6%) and forward-viewing endoscopy with or without cap-fitting (n = 664, 25.8%) were the most frequently used types of endoscopy when performing ERCP in Billroth II gastrectomy patients. The other types of endoscopy that were used were balloon-assisted enteroscopy in 171 cases (6.6%), anterior oblique-viewing endoscopy in 169 cases (6.6%), dual-lumen endoscopy in 64 cases (2.5%), colonoscopy in 31 (1.2%), and multiple bending endoscopy in 14 cases (0.5%). The overall success rate of afferent loop intubation was 91.3% (2437/2669), and the overall success rate of selective cannulation was 87.9% (2346/2437). A total of 195 cases (7.3%) of adverse events occurred. These events were bowel perforations in 74 cases (2.8%), post-ERCP pancreatitis in 65 cases (2.4%), bleeding in 37 cases (1.4%), mortality in 9 cases (0.3%), cholangitis in 7 cases (0.1%), respiratory insufficiency in 1 case (0.04%), aspiration pneumonia in 1 case (0.04%), and cholecystitis in 1 case (0.04%). All the mortality cases (n = 9, 0.3%) occurred in procedures using conventional side-viewing endoscopy.
| No. (%) | |
| Study design, n (%) | |
| Retrospective cohort | 36/43 (83.7) |
| Retrospective comparative | 4/43 (9.3) |
| Prospective comparative | 2/43 (4.7) |
| Prospective cohort | 1/43 (2.3) |
| Total number of identified patients | 2669 |
| 1Type of endoscope, n (%) | |
| Side-viewing endoscope | 1432/2575 (55.6) |
| Forward-viewing endoscope | 664/2575 (25.8) |
| Balloon-assisted enteroscope | 197/2575 (7.7) |
| Anterior oblique-viewing endoscope | 169/2575 (6.6) |
| Dual-lumen endoscope | 64/2575 (2.5) |
| Colonoscope | 31/2575 (1.2) |
| Multiple bending endoscope | 14/2575 (0.5) |
| Others | 4/2575 (0.2) |
| Overall success of afferent loop intubation, n (%) | 2437/2669 (91.3) |
| Overall success of selective cannulation, n (%) | 2346/2437 (87.9) |
| Overall adverse events, n (%) | 195 (7.3) |
| Bowel perforation | 74 (2.8) |
| Post-ERCP pancreatitis | 65 (2.4) |
| Bleeding | 37 (1.4) |
| Mortality | 9 (0.3) |
| 2Others | 10 (0.4) |
The subgroup analysis according to the type of endoscopy is summarized in Table 4. The success rates of afferent loop intubation by each type of endoscopy ranged from 82.8% to 98.2%. The success rates of selective cannulation ranged from 95.2% to 100%. The occurrence rate of adverse events by each type of endoscopy ranged from 3.6% to 7.9%. The rates of afferent loop intubation, selective cannulation, and adverse events were similar between side-viewing endoscopy and forward-viewing endoscopy, which are the most frequently used types of endoscopy in ERCP in patients with Billroth II gastrectomy. The rates of bowel perforation were slightly higher in side-viewing endoscopy (3.6%) and balloon-assisted enteroscopy (4.1%) compared with forward-viewing endoscopy (1.7%) and anterior oblique-viewing endoscopy (1.2%). Mortality only occurred in side-viewing endoscopy (n = 9, 0.6%).
| Side-viewing endoscope | Forward-viewing endoscope | Balloon-assisted enteroscope | Oblique-viewing endoscope | Dual-lumen endoscope | |
| (n = 1432) | (n = 664) | (n = 197) | (n = 169) | (n = 64) | |
| Afferent loop intubation, n (%) | 1406 (98.2) | 647 (97.4) | 188 (95.4) | 159 (94.1) | 53(82.8) |
| Selective cannulation, n (%) | 1340 (95.3) | 616 (95.2) | 179 (97.5) | 155 (97.5) | 53 (100) |
| Adverse events, n (%) | 113 (7.9) | 47 (7.1) | 14 (7.1) | 6 (3.6) | 3 (4.7) |
| Bowel perforation, n (%) | 51 (3.6) | 11 (1.7) | 8 (4.1) | 2 (1.2) | 2 (3.1) |
| Post-ERCP pancreatitis, n (%) | 26 (1.8) | 27 (4.1) | 6 (3.0) | 3 (1.8) | 1 (1.6) |
| Bleeding, n (%) | 27(1.9) | 9 (1.4) | - | 1 (0.6) | - |
| Mortality, n (%) | 9 (0.6) | - | - | - | - |
The subgroup analysis by each type of sphincter management summarized in Table 5. The clinical success rates of achievement for the planned therapeutic goals according to the sphincter management ranged from 85.8% to 93.6%. The overall rate of adverse events according to the sphincter therapy ranged from 5.8% to 8.5%. The rate of bowel perforation ranged from 1.3% to 3.5%. The most cases of post-ERCP pancreatitis occurred in patients who underwent EPBD (6.5%). Most of the bleeding occurred in whom EST was used (EST, n = 25; EST+EPBD, n = 8; EPBLD, n = 3).
| EST | EST+EPBD | EPBD | EPLBD | |
| (n = 1478) | (n = 598) | (n = 246) | (n = 171) | |
| 1Clinical success, n (%) | 1268 (85.8) | 546 (91.3) | 214 (87.0) | 160 (93.6) |
| Adverse events, n (%) | 103 (7.0) | 38 (6.4) | 21 (8.5) | 10 (5.8) |
| Bowel perforation, n (%) | 51 (3.5) | 8 (1.3) | 5 (2.0) | 3 (1.8) |
| Post-ERCP pancreatitis, n (%) | 18 (1.2) | 22 (3.7) | 16 (6.5) | 4 (2.3) |
| Bleeding, n (%) | 25 (1.7) | 8 (1.3) | - | 3 (1.8) |
| Mortality, n (%) | 9 (0.6) | - | - |
The gastric bypass surgery was first introduced in 1879 by Jules Emile Pean and 1880 by Ludwik Rydygier[20]. The gastrectomy with gastrojejunal anastomosis (Billroth II gastrectomy) is the most modern form of gastric bypass surgery, which was first performed in 1885 by Theodor Billroth[21]. Now, Billroth II gastrectomy has been widely used to treat gastric malignancy, refractory peptic ulcer disease with pyloric stenosis, or peptic ulcer perforation[22]. There are several types of Billroth II anastomosis according to reconstruction following partial gastrectomy such as antecolic or retrocolic, anisoperistaltic or isoperistaltic with or without Roux-en-Y anastomosis.
ERCP in Billroth II gastrectomy patients is a challenging procedure. The difficulties in performing ERCP in Billroth II gastrectomy are selective intubation of the endoscope into the afferent loop due to the acute angulation of the remnant stomach and small bowel, identification of papilla behind the mucosal fold, selective cannulation of the desired pancreaticobiliary duct, and optimal sphincter therapy due to the inverted position[23]. Particularly, because of procedure-related morbidity and mortality, there has been a paucity of prospective controlled studies in this population, and the treatment strategy or instrument decision, including the choice of endoscope or sphincter therapy, has been determined according to the endoscopists’ preference based on their education and experience.
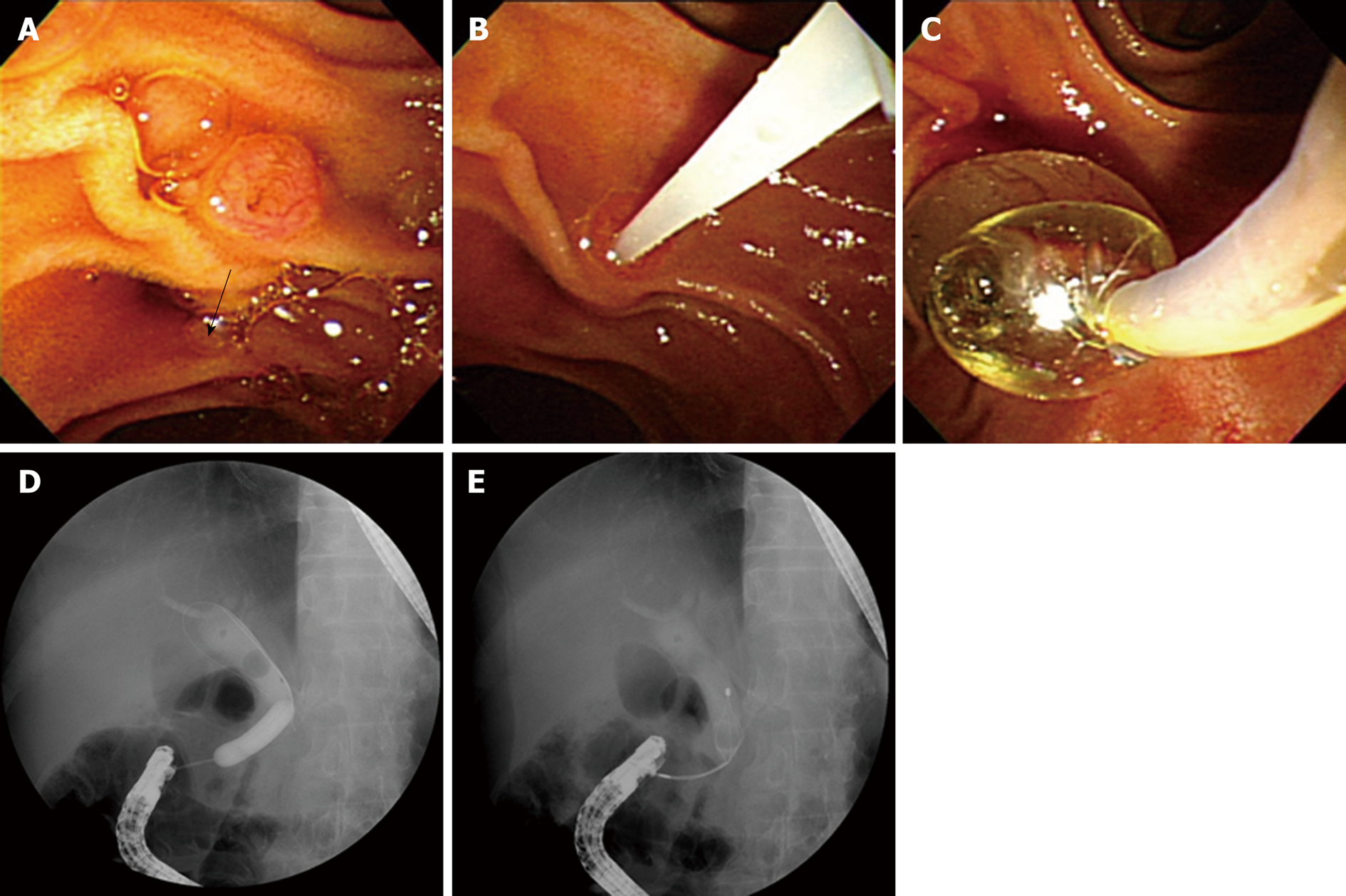
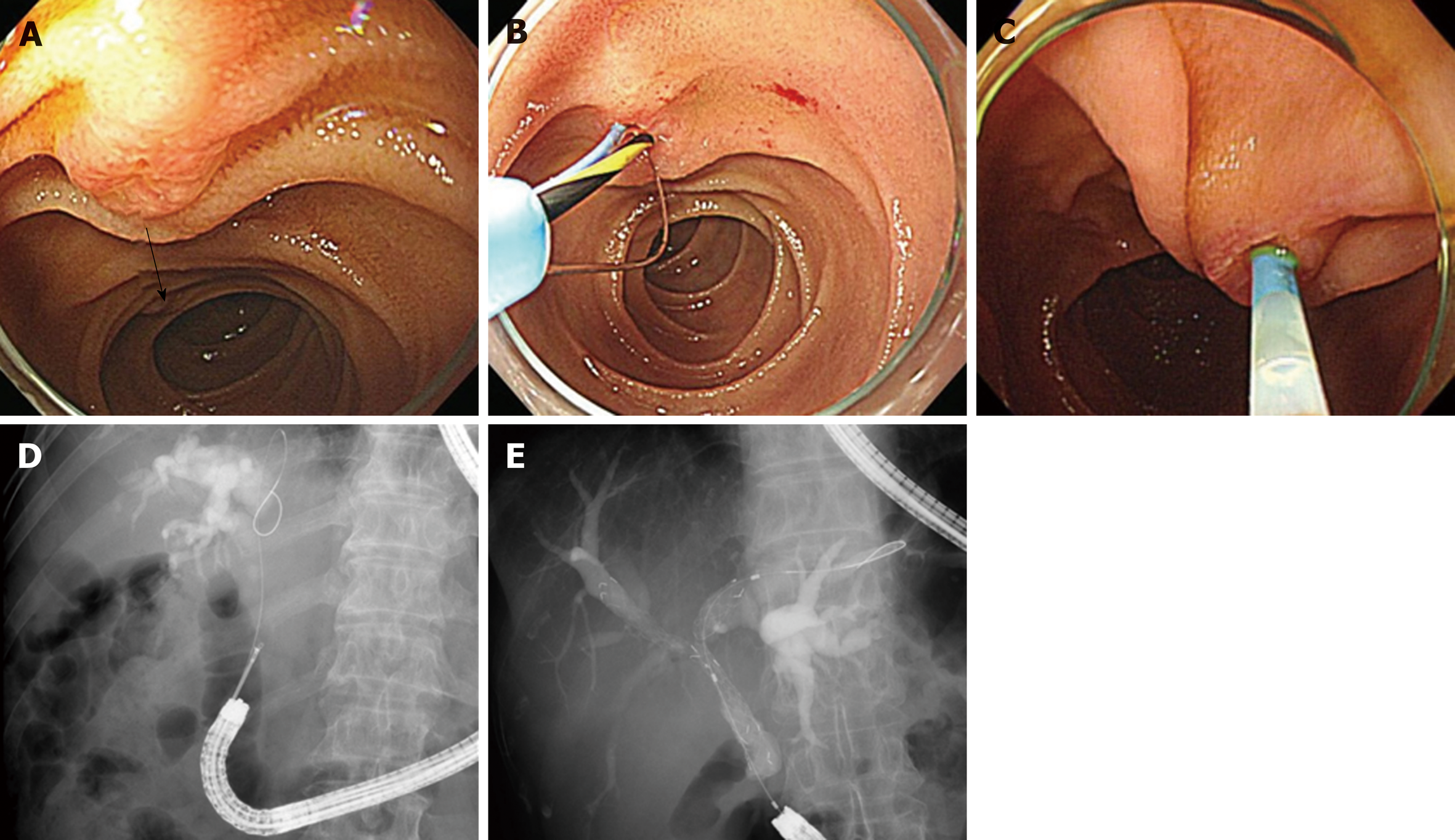
The choice of endoscopy has always been a matter of controversy, and there is no consensus on the issues. Experienced endoscopists usually recommend using a conventional side-viewing endoscope because it has an elevator and a large working channel. However, a side-viewing endoscope has some limitations when used on Billroth II gastrectomy patients because of its limited visibility due to presenting a side view, rigidity and relatively large diameter of the scope. Therefore, in Billroth II gastrectomy patients, ERCP using a side-viewing endoscope may sometimes be difficult, and it may be associated with a risk of small bowel or an anastomosis site perforation, particularly for inexperienced endoscopists. By contrast, insertion of a forward-viewing endoscope may be relatively easy and safe, and various interventions can also be performed safely. Consequently, the use of a forward-viewing endoscope with or without cap-fitting has become more frequent and now is the second most common type of endoscope for ERCP in Billroth II gastrectomy patients despite its disadvantages, such as absence of an elevator, small working channel, and difficulty in obtaining an en face view of the papilla (Figures 2 and 3).
Recently, a meta-analysis[24] that focused on the efficacy and safety of forward-viewing endoscopy for ERCP in Billroth II gastrectomy compared with conventional side-viewing endoscopy was reported. The meta-analysis showed a higher success rate for afferent loop intubation in forward-viewing endoscopy (with or without cap-fitting) compared to that for conventional side-viewing endoscopy (90.3% vs 86.8%). Furthermore, the success rate of selective cannulation in cap-fitting forward-viewing endoscopy has been reported up to 93.7%. This result suggested that forward-viewing endoscopy with or without cap-fitting can be a potential alternative type of endoscopy for ERCP in Billroth II gastrectomy cases, particularly when conventional side-viewing endoscopy fails and balloon-assisted enteroscopy is unavailable. A forward-viewing endoscopy with or without cap-fitting could be the initial choice of endoscopy for an inexperienced endoscopist to minimize the risk of adverse events, such as bowel perforation. However, the studies included in this meta-analysis were non-comparative and had a retrospective design, and therefore, the applicability of their pooled estimate results to general practice might be limited.
As an introduction to balloon-assisted endoscopy, the double-balloon enteroscope or single-balloon enteroscope have been increasingly used to perform ERCP in surgically altered anatomy, including Billroth II gastrectomy[5,6]. The success rates of ERCP in Billroth II gastrectomy cases by balloon-assisted enteroscopy have been reported from 95.0% to 100%, and seem to be comparable with those of conventional side-viewing endoscopy or forward-viewing endoscopy[25,26]. Balloon-assisted enteroscope has significant benefit to overcome the sharp curve of the anastomosis site and advance much deeper into the small intestine than conventional side-viewing endoscope or forward-viewing endoscope[5,27]. However, ERCP by balloon-assisted enteroscopy is technically demanding and requires expertise and specialized equipments. Balloon-assisted enteroscope is also forward-viewing instrument, which has disadvantages of difficulty in obtaining an en face view of the papilla. Therefore, a head to head comparison of outcomes between different types of endoscopy with a randomized controlled trial (RCT) is needed in the future.
Recently, the advent of new types of endoscopes, such as a dual lumen or multiple bending endoscope, has allowed successful afferent loop intubation and selective cannulation[10,28]. The use of dual lumen endoscope has potential advantage that the cooperation of two instruments through different channels can facilitate papillary cannulation in cases with difficult anatomy such as periampullary diverticulum and surgical altered anatomy. Unfortunately, the success rate of these procedures is not significantly higher than that of conventional side-viewing endoscopy, easily available forward-viewing endoscopy or standard colonoscopy (dual lumen endoscope, 82.8%; multiple bending endoscope, 92.9% vs conventional side-viewing endoscopy, 93.8%-97.5%; forward-viewing endoscopy, 95.4%; standard colonoscopy, 96.2%)[9,10,17-19,28,29]. Until now, there has been no large-scale retrospective cohort study or prospective comparative study. Therefore, the new types of endoscopes are practically and economically limited for widespread use.
Another issue, the choice of sphincter therapy, has also been a matter of debate regarding ERCP with Billroth II gastrectomy patients. Traditionally, the performance of sphincterotomy in Billroth II cases is difficult due to its revere position of the biliary and pancreatic duct. The difficulty of sphincterotomy in optimal direction is associated with the risk of bowel perforation or bleeding. So, there have been continued considerable efforts to perform effective and safe sphincter therapy. Dedicated sphincterotomes for Billroth II anatomy such as inverted sphincterotome or S-shaped sphincterotome have been developed and widely used. Recently, the use of EPBD for sphincter management in Billroth II patients has been on the increase. EPBD is particularly useful in ERCP with a forward-viewing endoscope since sphincterotomy may be difficult with this scope which does not have an elevator. Furthermore, in cases with large CBD stones, application of EPLBD can help to efficiently remove these stones in Billroth II gastrectomy cases[12,30]. Therefore, the increasing use of balloon dilator has been the general trend in sphincter therapy in recent years.
This study has potential limitations that should be discussed. First, in this study, it is not sufficiently and clearly described a recent trend toward a better outcome with novel technologies in ERCP in Billroth II gastrectomy patients. Because most of studies regarding novel technologies were case report, case series, and animal study, they were excluded from current systematic review. This point is major limitation of current study. Second, the studies included in the current systematic review were retrospective, observatory publications from more than 30 years with heterogenous indications for ERCP. The performance bias of ERCP according to the endoscopist’s experience and technique and operative consideration, including the duration and type of Billroth II operation (antecolic or retrocolic, anisoperitacltic or isoperistaltic), were not described. The older studies can lead to bias because there are the difference of the technological advance such as endoscopic instruments and skill, overall knowledge and experience of endoscopists in performing ERCP of Billroth II gastrectomy patients between the past and the present.
In summary, conventional side-viewing endoscopy remains the most commonly used type of endoscopy for ERCP in Billroth II gastrectomy cases. Forward-viewing endoscopy has been increasingly used to perform ERCP in Billroth II gastrectomy cases because of its advantages, including easy availability and good visual field, as well as the additional advantage of the transparent cap being fitted to the distal end of the endoscope. In recent years, new types of endoscopy, including balloon-assisted enteroscopy, anterior oblique-viewing endoscopy, dual-lumen endoscopy, and multiple bending endoscopy, have been introduced and performed with ERCP safely and effectively. There have also been various types of sphincter therapy applied, including EST, EPBD, and EPLBD, with or without precutting by NK, and the use of diverse types of accessories. As considerable efforts of worldwide investigators have been applied for safe and effective ERCP in this population, the success rate of the procedure and occurrence of adverse events have been improving. In addition, a RCT is required to evaluate the optimal type of endoscopy and sphincter therapy for ERCP in Billroth II gastrectomy patients in the future.
Endoscopic retrograde cholangiopancreatography (ERCP) in patients who have a Billroth II gastrectomy has been considered a difficult procedure due to the surgically altered anatomy. The difficulties of ERCP in patients with Billroth II gastrectomy include the intubation of the afferent loop, visualization of the papilla, selective cannulation of the bile duct, and optimal sphincter management due to the reverse direction of the papilla. To perform safe and effective ERCP in Billroth II gastrectomy cases, considerable efforts have been put in several ways including the choice of endoscope and sphincter management. However, there has been a paucity of comparative studies on the efficacy and safety regarding ERCP in Billroth II gastrectomy.
At present, comparative studies on the efficacy and safety of ERCP in Billroth II gastrectomy cases are lacking because of practical and ethical limitations due to procedure-related morbidity and mortality. This systematic and comprehensive review was performed to obtain a recent perspective on ERCP in Billroth II gastrectomy patients.
The main objective of the study was to assess the efficacy and safety of ERCP in Billroth II gastrectomy patients. In detail, the assessment of success rate of afferent loop intubation and selective cannulation, and rate of adverse events including bowel perforation, post-ERCP pancreatitis, bleeding, cardiopulmonary events, and mortality was performed. In addition, the assessment of these outcomes according to each type of endoscopy and sphincter management methods was performed.
A systematic review was performed on the literatures that evaluated the outcomes of ERCP in Billroth II gastrectomy patients. Electronic databases were searched, including PubMed, EMBASE, and Cochrane Library. The outcomes of afferent loop intubation and selective cannulation, and occurrence of adverse events were assessed.
A total of 43 studies involving 2669 patients were included. The overall success rate of afferent loop intubation was 91.3% (2437/2669), and the overall success rate of selective cannulation was 87.9% (2346/2437). A total of 195 cases (7.3%) of adverse events occurred. Bowel perforations occurred in 74 cases (2.8%), post-ERCP pancreatitis in 65 cases (2.4%), bleeding in 37 cases (1.4%), mortality in 9 cases (0.3%).
This systematic review showed that the performance of ERCP in the Billroth II gastrectomy patients has been improving with choice of endoscope and sphincter management. To determine the optimal method to perform safe and effective ERCP in Billroth II gastrectomy patients, more comparative studies are needed in the future.
The success of ERCP in Billroth II gastrectomy has been improving with technical advance. Future research is needed to explore the optimal approach in performance of ERCP in Billroth II gastrectomy cases.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: South Korea
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Anderloni A, Arcidiacono PG, Karagyozov P, Liu-Ye H, Karagyozov N S-Editor: Yan JP L-Editor: A E-Editor: Zhang YL
| 1. | Forbes A, Cotton PB. ERCP and sphincterotomy after Billroth II gastrectomy. Gut. 1984;25:971-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 69] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Osnes M, Rosseland AR, Aabakken L. Endoscopic retrograde cholangiography and endoscopic papillotomy in patients with a previous Billroth-II resection. Gut. 1986;27:1193-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 77] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Kim MH, Lee SK, Lee MH, Myung SJ, Yoo BM, Seo DW, Min YI. Endoscopic retrograde cholangiopancreatography and needle-knife sphincterotomy in patients with Billroth II gastrectomy: A comparative study of the forward-viewing endoscope and the side-viewing duodenoscope. Endoscopy. 1997;29:82-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 81] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Lee YT. Cap-assisted endoscopic retrograde cholangiopancreatography in a patient with a Billroth II gastrectomy. Endoscopy. 2004;36:666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Chu YC, Su SJ, Yang CC, Yeh YH, Chen CH, Yueh SK. ERCP plus papillotomy by use of double-balloon enteroscopy after Billroth II gastrectomy. Gastrointest Endosc. 2007;66:1234-1236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Itoi T, Ishii K, Sofuni A, Itokawa F, Tsuchiya T, Kurihara T, Tsuji S, Ikeuchi N, Umeda J, Moriyasu F. Single-balloon enteroscopy-assisted ERCP in patients with Billroth II gastrectomy or Roux-en-Y anastomosis (with video). Am J Gastroenterol. 2010;105:93-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 124] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 7. | Law NM, Freeman ML. ERCP by using a prototype oblique-viewing endoscope in patients with surgically altered anatomy. Gastrointest Endosc. 2004;59:724-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Wagh MS, Draganov PV. Prospective evaluation of spiral overtube-assisted ERCP in patients with surgically altered anatomy. Gastrointest Endosc. 2012;76:439-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Yao W, Huang Y, Chang H, Li K, Huang X. Endoscopic Retrograde Cholangiopancreatography Using a Dual-Lumen Endogastroscope for Patients with Billroth II Gastrectomy. Gastroenterol Res Pract. 2013;2013:146867. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Koo HC, Moon JH, Choi HJ, Ko BM, Hong SJ, Cheon YK, Cho YD, Lee JS, Lee MS, Shim CS. The utility of a multibending endoscope for selective cannulation during ERCP in patients with a Billroth II gastrectomy (with video). Gastrointest Endosc. 2009;69:931-934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Bergman JJ, van Berkel AM, Bruno MJ, Fockens P, Rauws EA, Tijssen JG, Tytgat GN, Huibregtse K. A randomized trial of endoscopic balloon dilation and endoscopic sphincterotomy for removal of bile duct stones in patients with a prior Billroth II gastrectomy. Gastrointest Endosc. 2001;53:19-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 100] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 12. | Itoi T, Ishii K, Itokawa F, Kurihara T, Sofuni A. Large balloon papillary dilation for removal of bile duct stones in patients who have undergone a billroth ii gastrectomy. Dig Endosc. 2010;22 Suppl 1:S98-S102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Dickey W, Jacob S, Porter KG. Balloon dilation of the papilla via a forward-viewing endoscope: An aid to therapeutic endoscopic retrograde cholangiopancreatography in patients with Billroth-II gastrectomy. Endoscopy. 1996;28:531-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Costamagna G, Mutignani M, Perri V, Gabrielli A, Locicero P, Crucitti F. Diagnostic and therapeutic ERCP in patients with Billroth II gastrectomy. Acta Gastroenterol Belg. 1994;57:155-162. [PubMed] |
| 15. | Kim GH, Kang DH, Song GA, Heo J, Park CH, Ha TI, Kim KY, Lee HJ, Kim ID, Choi SH, Song CS. Endoscopic removal of bile-duct stones by using a rotatable papillotome and a large-balloon dilator in patients with a Billroth II gastrectomy (with video). Gastrointest Endosc. 2008;67:1134-1138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ. 2009;339:b2535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18665] [Cited by in RCA: 17528] [Article Influence: 1095.5] [Reference Citation Analysis (1)] |
| 17. | Bove V, Tringali A, Familiari P, Gigante G, Boškoski I, Perri V, Mutignani M, Costamagna G. ERCP in patients with prior Billroth II gastrectomy: Report of 30 years' experience. Endoscopy. 2015;47:611-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 56] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 18. | Wu WG, Mei JW, Zhao MN, Zhang WJ, Gu J, Tao YJ, Liu YB, Wang XF. Use of the Conventional Side-viewing Duodenoscope for Successful Endoscopic Retrograde Cholangiopancreatography in Postgastrectomy Patients. J Clin Gastroenterol. 2016;50:244-251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Park TY, Kang JS, Song TJ, Lee SS, Lee H, Choi JS, Kim HJ, Jang JW. Outcomes of ERCP in Billroth II gastrectomy patients. Gastrointest Endosc. 2016;83:1193-1201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 20. | Santoro E. The history of gastric cancer: Legends and chronicles. Gastric Cancer. 2005;8:71-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Robinson JO. The history of gastric surgery. Postgrad Med J. 1960;36:706-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Weil PH, Buchberger R. From Billroth to PCV: A century of gastric surgery. World J Surg. 1999;23:736-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 23. | Rosseland AR, Osnes M, Kruse A. Endoscopic sphincterotomy (EST) in patients with Billroth II Gastrectomy. Endoscopy. 1981;13:19-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Park TY, Bang CS, Choi SH, Yang YJ, Shin SP, Suk KT, Baik GH, Kim DJ, Yoon JH. Forward-viewing endoscope for ERCP in patients with Billroth II gastrectomy: A systematic review and meta-analysis. Surg Endosc. 2018;32:4598-4613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 25. | Shimatani M, Hatanaka H, Kogure H, Tsutsumi K, Kawashima H, Hanada K, Matsuda T, Fujita T, Takaoka M, Yano T, Yamada A, Kato H, Okazaki K, Yamamoto H, Ishikawa H, Sugano K; Japanese DB-ERC Study Group. Diagnostic and Therapeutic Endoscopic Retrograde Cholangiography Using a Short-Type Double-Balloon Endoscope in Patients With Altered Gastrointestinal Anatomy: A Multicenter Prospective Study in Japan. Am J Gastroenterol. 2016;111:1750-1758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 118] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 26. | Yane K, Katanuma A, Maguchi H, Takahashi K, Kin T, Ikarashi S, Sano I, Yamazaki H, Kitagawa K, Yokoyama K, Koga H, Nagai K, Nojima M. Short-type single-balloon enteroscope-assisted ERCP in postsurgical altered anatomy: Potential factors affecting procedural failure. Endoscopy. 2017;49:69-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 27. | Osoegawa T, Motomura Y, Akahoshi K, Higuchi N, Tanaka Y, Hisano T, Itaba S, Gibo J, Yamada M, Kubokawa M, Sumida Y, Akiho H, Ihara E, Nakamura K. Improved techniques for double-balloon-enteroscopy-assisted endoscopic retrograde cholangiopancreatography. World J Gastroenterol. 2012;18:6843-6849. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 47] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 28. | Wang S, Liu W, Sun S, Wang G, Liu X, Ge N, Guo J. Clinical evaluation of double-channel gastroscope for endoscopic retrograde cholangiopancreatography in patients with Billroth II gastrectomy. Prz Gastroenterol. 2016;11:163-169. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 29. | Wang F, Xu B, Li Q, Zhang X, Jiang G, Ge X, Nie J, Zhang X, Wu P, Ji J, Miao L. Endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy: One single center's experience. Medicine (Baltimore). 2016;95:e5743. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 30. | Lee TH, Hwang JC, Choi HJ, Moon JH, Cho YD, Yoo BM, Park SH, Kim JH, Kim SJ. One-Step Transpapillary Balloon Dilation under Cap-Fitted Endoscopy without a Preceding Sphincterotomy for the Removal of Bile Duct Stones in Billroth II Gastrectomy. Gut Liver. 2012;6:113-117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 31. | Hintze RE, Veltzke W, Adler A, Abou-Rebyeh H. Endoscopic sphincterotomy using an S-shaped sphincterotome in patients with a Billroth II or Roux-en-Y gastrojejunostomy. Endoscopy. 1997;29:74-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 48] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 32. | Lin LF, Siauw CP, Ho KS, Tung JC. ERCP in post-Billroth II gastrectomy patients: Emphasis on technique. Am J Gastroenterol. 1999;94:144-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 74] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 33. | Faylona JM, Qadir A, Chan AC, Lau JY, Chung SC. Small-bowel perforations related to endoscopic retrograde cholangiopancreatography (ERCP) in patients with Billroth II gastrectomy. Endoscopy. 1999;31:546-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 94] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 34. | Swarnkar K, Stamatakis JD, Young WT. Diagnostic and therapeutic endoscopic retrograde cholangiopancreaticography after Billroth II gastrectomy--safe provision in a district general hospital. Ann R Coll Surg Engl. 2005;87:274-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 35. | Kikuyama M, Matsubayashi Y, Kageyama F, Sumyoshi S, Kobayashi Y. Oblique-viewing endoscope facilitates endoscopic retrograde cholangiopancreatography and associated procedures in post-Billroth II gastrectomy patients. Digest Endosc. 2005;17:9-12. [RCA] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 36. | Ciçek B, Parlak E, Dişibeyaz S, Koksal AS, Sahin B. Endoscopic retrograde cholangiopancreatography in patients with Billroth II gastroenterostomy. J Gastroenterol Hepatol. 2007;22:1210-1213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 37. | Park CH, Lee WS, Joo YE, Kim HS, Choi SK, Rew JS. Cap-assisted ERCP in patients with a Billroth II gastrectomy. Gastrointest Endosc. 2007;66:612-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 52] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 38. | Dolay K, Soylu A. Easy sphincterotomy in patients with Billroth II gastrectomy: A new technique. Turk J Gastroenterol. 2008;19:109-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 39. | Nakahara K, Horaguchi J, Fujita N, Noda Y, Kobayashi G, Ito K, Obana T, Takasawa O. Therapeutic endoscopic retrograde cholangiopancreatography using an anterior oblique-viewing endoscope for bile duct stones in patients with prior Billroth II gastrectomy. J Gastroenterol. 2009;44:212-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 40. | Shimatani M, Matsushita M, Takaoka M, Koyabu M, Ikeura T, Kato K, Fukui T, Uchida K, Okazaki K. Effective "short" double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy: a large case series. Endoscopy. 2009;41:849-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 161] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 41. | Kikuyama M, Sasada Y, Matsuhashi T, Ota Y, Nakahodo J. ERCP afterRoux-en-Y reconstruction can be carried out using an oblique-viewing endoscope with an overtube. Dig Endosc. 2009;21:180-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 42. | Lin CH, Tang JH, Cheng CL, Tsou YK, Cheng HT, Lee MH, Sung KF, Lee CS, Liu NJ. Double balloon endoscopy increases the ERCP success rate in patients with a history of Billroth II gastrectomy. World J Gastroenterol. 2010;16:4594-4598. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 43. | Byun JW, Kim JW, Sung SY, Jung HY, Jeon HK, Park HJ, Kim MY, Kim HS, Baik SK. Usefulness of Forward-Viewing Endoscope for Endoscopic Retrograde Cholangiopancreatography in Patients with Billroth II Gastrectomy. Clin Endosc. 2012;45:397-403. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 44. | Choi CW, Choi JS, Kang DH, Kim BG, Kim HW, Park SB, Yoon KT, Cho M. Endoscopic papillary large balloon dilation in Billroth II gastrectomy patients with bile duct stones. J Gastroenterol Hepatol. 2012;27:256-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 45. | Kianicka B, Dite P, Piskac P. Pitfalls of pancreatobiliary endoscopy after Billroth II gastrectomy. Hepatogastroenterology. 2012;59:17-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 46. | Sen-Yo M, Kaino S, Suenaga S, Uekitani T, Yoshida K, Harano M, Sakaida I. Utility of the Anterior Oblique-Viewing Endoscope and the Double-Balloon Enteroscope for Endoscopic Retrograde Cholangiopancreatography in Patients with Billroth II Gastrectomy. Gastroenterol Res Pract. 2012;2012:389269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 47. | Jang HW, Lee KJ, Jung MJ, Jung JW, Park JY, Park SW, Song SY, Chung JB, Bang S. Endoscopic papillary large balloon dilatation alone is safe and effective for the treatment of difficult choledocholithiasis in cases of Billroth II gastrectomy: A single center experience. Dig Dis Sci. 2013;58:1737-1743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 48. | Kawamura T, Mandai K, Uno K, Yasuda K. Does single-balloon enteroscopy contribute to successful endoscopic retrograde cholangiopancreatography in patients with surgically altered gastrointestinal anatomy? ISRN Gastroenterol. 2013;2013:214958. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 49. | Kim KH, Kim TN. Endoscopic papillary large balloon dilation for the retrieval of bile duct stones after prior Billroth II gastrectomy. Saudi J Gastroenterol. 2014;20:128-133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 50. | Iwai T, Kida M, Yamauchi H, Imaizumi H, Koizumi W. Short-type and conventional single-balloon enteroscopes for endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy: Single-center experience. Dig Endosc. 2014;26 Suppl 2:156-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 51. | Cheng CL, Liu NJ, Tang JH, Yu MC, Tsui YN, Hsu FY, Lee CS, Lin CH. Double-balloon enteroscopy for ERCP in patients with Billroth II anatomy: Results of a large series of papillary large-balloon dilation for biliary stone removal. Endosc Int Open. 2015;3:E216-E222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 52. | Jang JS, Lee S, Lee HS, Yeon MH, Han JH, Yoon SM, Chae HB, Youn SJ, Park SM. Efficacy and Safety of Endoscopic Papillary Balloon Dilation Using Cap-Fitted Forward-Viewing Endoscope in Patients Who Underwent Billroth II Gastrectomy. Clin Endosc. 2015;48:421-427. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 53. | Ki HS, Park CH, Jun CH, Park SY, Kim HS, Choi SK, Rew JS. Feasibility of cap-assisted endoscopic retrograde cholangiopancreatography in patients with altered gastrointestinal anatomy. Gut Liver. 2015;9:109-112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 54. | Nakahara K, Okuse C, Suetani K, Morita R, Michikawa Y, Ozawa S, Hosoya K, Nomoto M, Kobayashi S, Otsubo T, Itoh F. Endoscopic retrograde cholangiography using an anterior oblique-viewing endoscope in patients with altered gastrointestinal anatomy. Dig Dis Sci. 2015;60:944-950. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 55. | Shimatani M, Tokuhara M, Kato K, Miyamoto S, Masuda M, Sakao M, Fukata N, Miyoshi H, Ikeura T, Takaoka M, Okazaki K. Utility of newly developed short-type double-balloon endoscopy for endoscopic retrograde cholangiography in postoperative patients. J Gastroenterol Hepatol. 2017;32:1348-1354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 56. | Li T, Wen J, Bie LK, Lu Y, Gong B. Long-term outcomes of endoscopic papillary balloon dilation for removal of bile duct stones in Billroth II gastrectomy patients. Hepatobiliary Pancreat Dis Int. 2018;17:257-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 57. | Han MG, Cho E, Park CH, Jun CH, Park SY. Self-expandable metal stents for choledocholithiasis in Billroth II gastrectomy patients. Hepatobiliary Pancreat Dis Int. 2018;17:546-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |