Published online May 28, 2019. doi: 10.3748/wjg.v25.i20.2430
Peer-review started: January 22, 2019
First decision: February 21, 2019
Revised: April 2, 2019
Accepted: April 19, 2019
Article in press: April 20, 2019
Published online: May 28, 2019
Processing time: 126 Days and 21.8 Hours
The objective of this study was to analyze the current evidence for the use of pancreatic enzyme replacement therapy (PERT) in affecting survival and quality of life in patients with pancreatic exocrine insufficiency (PEI). Systematic searches of the literature were performed using the PubMed database. Articles were selected for inclusion if they reported findings from trials assessing the effects of PERT on quality of life, survival, malabsorption, growth parameters (such as height, body weight and body mass index), or gastrointestinal symptoms (such as abdominal pain, stool consistency and flatulence). PERT improved PEI-related malabsorption and weight maintenance in patients with cystic fibrosis, chronic pancreatitis, pancreatic cancer, and post-surgical states. In patients with chronic pancreatitis, PERT improved PEI-related symptoms and quality of life measures. Several small retrospective studies have also suggested that PERT may have a positive impact on survival, but long-term studies assessing this effect were not identified. PERT is effective for treating malnutrition and supporting weight maintenance, and it is associated with improved quality of life and possibly with enhanced survival in patients with PEI. However, there is evidence that not all patients with PEI receive adequate PERT. Future work should aim to assess the long-term effects of PERT on the survival of patients with PEI.
Core tip: Malnutrition associated with pancreatic exocrine insufficiency (PEI) can have serious consequences, leading to increased morbidity and reduced survival. Awareness and education may be needed to ensure that patients with PEI are managed appropriately in order to increase their survival and improve long-term quality of life. There is currently a lack of evidence for the long-term effects of pancreatic enzyme replacement therapy (PERT) on survival in patients with PEI; however, there is substantial evidence supporting its efficacy in improving PEI-related malnutrition. Furthermore, the available evidence indicates that PERT improves PEI-related symptoms and quality of life measures in patients with PEI.
- Citation: Layer P, Kashirskaya N, Gubergrits N. Contribution of pancreatic enzyme replacement therapy to survival and quality of life in patients with pancreatic exocrine insufficiency. World J Gastroenterol 2019; 25(20): 2430-2441
- URL: https://www.wjgnet.com/1007-9327/full/v25/i20/2430.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i20.2430
Effectively understanding the nutritional implications of pancreatic exocrine insufficiency (PEI) is fundamental if physicians are willing to improve the survival and quality of life in patients with compromised pancreatic function[1]. In patients with PEI, secretion of pancreatic enzymes and bicarbonate is insufficient to maintain a normal digestion[2,3]. Impaired food digestion can result in nutrient malabsorption and malnutrition, as well as disturbed regulation of gastrointestinal (GI) motor and secretory functions[2,3]. Thus, patients with PEI frequently complain of steatorrhea, diarrhea, and/or other usually unspecific GI symptoms associated with fat maldigestion[4-8]. PEI may be undiagnosed in some patients who may be suspected to suffer from other GI disorders, such as irritable bowel syndrome[8]. Furthermore, diagnosis may be difficult to establish, particularly with mild or moderate disease[9]. Awareness and education in the management of PEI may be needed to ensure that patients affected by the severe and chronic diseases with which it is associated are managed appropriately, in order to increase their survival and improve long-term quality of life[2,7,10].
Often, patients develop PEI as a result of changes to the pancreas caused by life-limiting or terminal diseases[1]. Conditions such as cystic fibrosis (CF) or chronic pancreatitis (CP) lead to loss of pancreatic parenchyma, while pancreatic cancer may cause obstruction of the pancreatic duct, particularly if the tumor is located in the head of the pancreas. Celiac disease results in decreased pancreatic stimulation, and Zollinger-Ellison syndrome inactivates pancreatic enzymes. Surgical resections, such as gastrectomy or duodenopancreatectomy, may also lead to decreased and delayed pancreatic stimulation and loss of pancreatic parenchyma[11,12]. Overall, the most common causes of PEI are CF, CP, and pancreatic cancer[2].
Malnutrition resulting from PEI is the main clinical manifestation of the disease[12]. It can be associated with serious consequences, leading to increased morbidity and reduced survival[1,7], and it may be associated with a reduced quality of life[13]. Malnutrition resulting from PEI in CF can lead to stunted growth in childhood, weight loss in adults, and deterioration of pulmonary function; PEI can also lead to decreased length of survival compared with pancreatic-sufficient patients[2,14]. In non-CF conditions, e.g., CP and pancreatic cancer, PEI-related malnutrition is associated with weight loss that can lead to the development of comorbidities, and negatively impacts on patient prognosis[15-17].
Pancreatic enzyme replacement therapy (PERT) involves supplementation of pancreatic enzymes in patients with PEI and is effective in reducing the severity of GI symptoms; it also improves GI dysregulation and nutrient absorption, thus preventing malnutrition[7,15]. PERT has the potential to improve the nutritional status of patients suffering from PEI and, therefore, may increase survival and improve quality of life of these patients[1,2,7,16]. Treatment is usually well tolerated, with mild GI symptoms (e.g., stomach pain, nausea, and bloating) reported as major adverse events[7]. Very high doses of PERT have been associated with fibrosing colonopathy in patients with CF; however, such high doses are not recommended by current treatment guidelines[7,17,18].
This review aims to analyze the current evidence for the effectiveness of PERT in increasing survival and improving quality of life in patients with PEI, particularly those with severe and chronic underlying diseases such as CF, CP, or pancreatic cancer (see Supplementary material for literature search details).
No studies directly assessing the link between PERT and increased survival of patients with PEI and CF were identified in the literature, and only one study assessed quality of life. However, a number of randomized, placebo-controlled studies as well as longer-term, open-label studies evaluating various PERT formulations, e.g., pancrelipase (pancreatin) or liprotamase, were identified and are discussed here, as these provide insights on the effects of PERT on nutritional status, growth parameters, or GI symptoms.
In the seven short-term, randomized, double-blind, placebo-controlled studies evaluated, administration of PERT was shown to significantly increase fat and protein absorption compared with placebo in patients ≥ 7 years of age with CF (P < 0.001; Supplementary Table 1)[19-25]. A typical coefficient of fat absorption (CFA) of 40-50% is observed in patients with PEI and CF without treatment[26]. In the short-term studies included here, the CFA ranged from 72.7% to 88.6% in patients treated with PERT vs 47.4% to 62.8% in patients who received placebo, and the coefficient of nitrogen absorption (CNA) from 80.3% to 87.2% in patients treated with PERT vs 45.0% to 65.7% in patients who received placebo (Supplementary Table 1). Greater improve-ments in CFA and CNA were noted in severe disease, which is characterized by a placebo CFA < 40%[19,20] or ≤ 50%[21,22]. Stool consistency, frequency, and mean stool fat were improved in patients receiving PERT compared with placebo, as well as other malnutrition-related symptoms, e.g., bloating, abdominal pain, and flatulence.
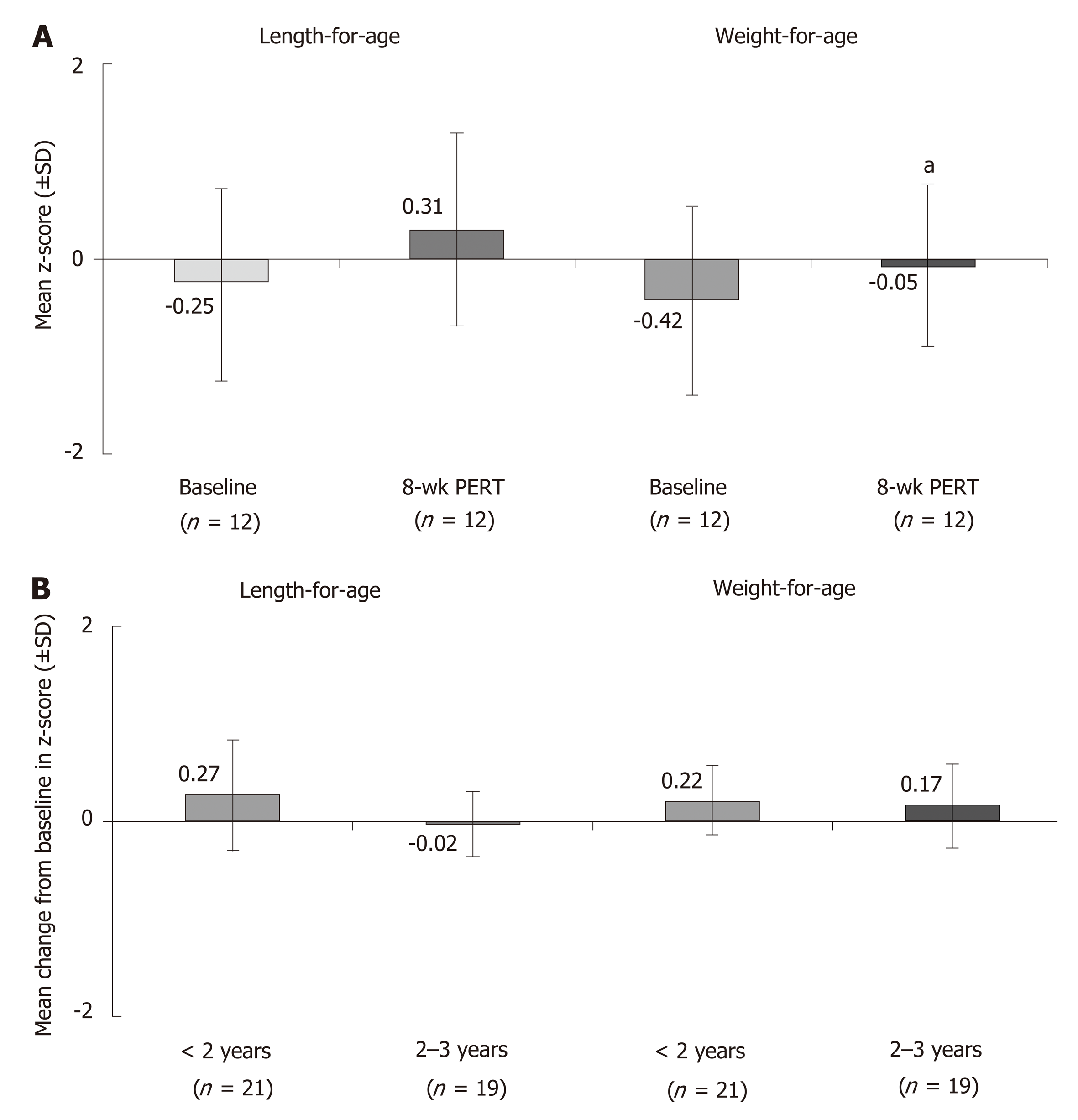
The positive effects of PERT in patients with CF are further supported by findings from open-label studies in different age groups, including an 8-wk study in children < 2 years of age[27], a 12-wk study in children 1 mo to < 4 years of age[28], a 12-mo study in children ≥ 7 years of age[29], and a 14-d study in children 6-36 mo of age[30] (Supplementary Table 2). In addition to improvements in fat and protein absorption, PERT was associated with age-appropriate increases in growth parameters. In children < 2 years of age, significant increases in the weight-for-age z-score were observed after 8 wk of PERT, as well as increases in the length-for-age z-score (Figure 1A)[27]. Similar results were observed over 12 wk of PERT in children 1 mo to < 4 years of age, with marked increases particularly observed in children < 2 years of age (Figure 1B)[28]. In older children ≥ 7 years of age, 12 mo of PERT was shown to lead to and maintain age-appropriate growth and weight gain[29]. During the study in older children ≥ 7 years of age none of the subjects lost > 5% body weight; 67.5% and 62.8% of children 7 to < 12 years of age and 12 to < 17 years of age gained > 5% body weight, respectively[29].
In four short-term, randomized, double-blind, placebo-controlled studies conducted in patients with CP, PERT improved on-treatment CFA and CNA values (Supplementary Table 3)[31-34]. In a trial in 27 patients, fat absorption significantly improved in patients receiving PERT compared with placebo (P = 0.0185)[31]. PERT also led to a significant reduction in fat excretion (P = 0.0181) and stool frequency (P = 0.0015) and improved stool consistency (P = 0.0102). These results are consistent with those obtained in a dose-response, cross-over study evaluating two doses of PERT[32]. Patients were randomized to a low-high or high-low dosing sequence. Following 18-22 d of PERT, fat and protein absorption significantly increased from baseline (P < 0.001). Furthermore, PERT was associated with significant increases in body weight compared with the placebo run-in period (P ≤ 0.021) and in body mass index (BMI)(P ≤ 0.020). PERT also significantly increased high-density lipoprotein cholesterol levels (P < 0.001) compared with the placebo run-in period, while low-density lipoprotein cholesterol and fat-soluble vitamin levels (A, E, and K) remained unchanged over the study duration[32] (Supplementary Table 3).
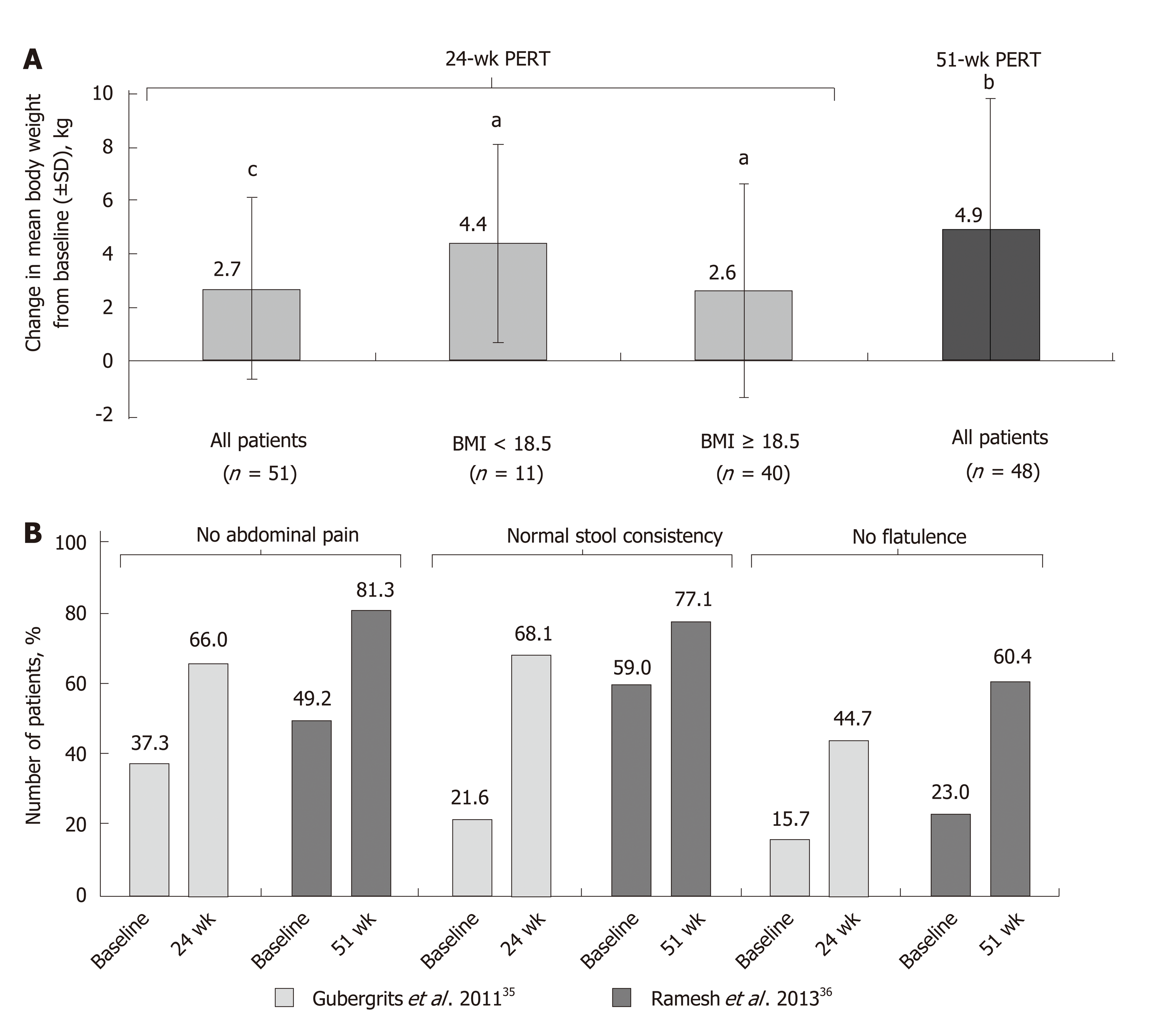
The effects of long-term PERT on nutritional status and body weight of patients with CP were assessed in two open-label studies conducted for up to 1 year (Supplementary Table 4)[35,36]. These were both preceded by a short, randomized phase where the effects of PERT vs placebo on fat and protein absorption were measured. One of these studies was conducted in 54 patients randomized to receive PERT or placebo for 7 d[34], followed by an open-label phase for 6 mo, where all patients in the analysis (n = 48) received PERT[35]. At the end of the randomized phase, fat and protein absorption were greater in patients receiving PERT compared with placebo[34]. A clinically relevant and statistically significant improvement in body weight (P < 0.0001; Figure 2A) was observed at the end of the 24-wk, open-label treatment phase[35]. Stool frequency was significantly reduced (P < 0.001), and improvements in clinical symptoms and the Clinical Global Impression scale of clinical symptoms were reported; the proportion of patients with no symptoms or mild symptoms overall increased (49.1% at baseline to 83.0% at study end)[35]. However, no clinically meaningful changes in quality of life [assessed by the 36-item Short Form (SF-36) Health Survey] were observed at the end of the 24-wk treatment period[35].
In India, a 1-wk, randomized, double-blind, placebo-controlled study was conducted[33] followed by a 51-wk, open-label extension study[36]. PERT was associated with significant improvements in fat and protein absorption (P = 0.001 and P = 0.005, respectively), together with reductions in mean stool frequency, stool weight, stool fat, and stool nitrogen[33,36]. Moreover, significant improvements in body weight (P = 0.001; Figure 2A) and BMI (P = 0.001) were observed after 1 year of PERT[36]. An increase in body weight of ≥ 7% occurred in 61.7% of patients. Overall, the median BMI increased from 19.2 kg/m2 at baseline to 20.9 kg/m2 at the end of the open-label phase[36].
In both the open-label extension studies discussed above, PERT led to improve-ments in PEI-related symptoms, such as abdominal pain, stool consistency, and flatulence (Figure 2B)[35,36]. In the 24-wk study, no clinically meaningful changes in quality of life assessed using the SF-36 were observed at the end of the treatment period[35]. However, in the 51-wk study, quality of life was enhanced with PERT; seven of the eight components of the SF-36 and the two summary scores improved (including significant improvements in bodily pain, general health, vitality, role-emotional, mental health, and the mental component summary)[36].
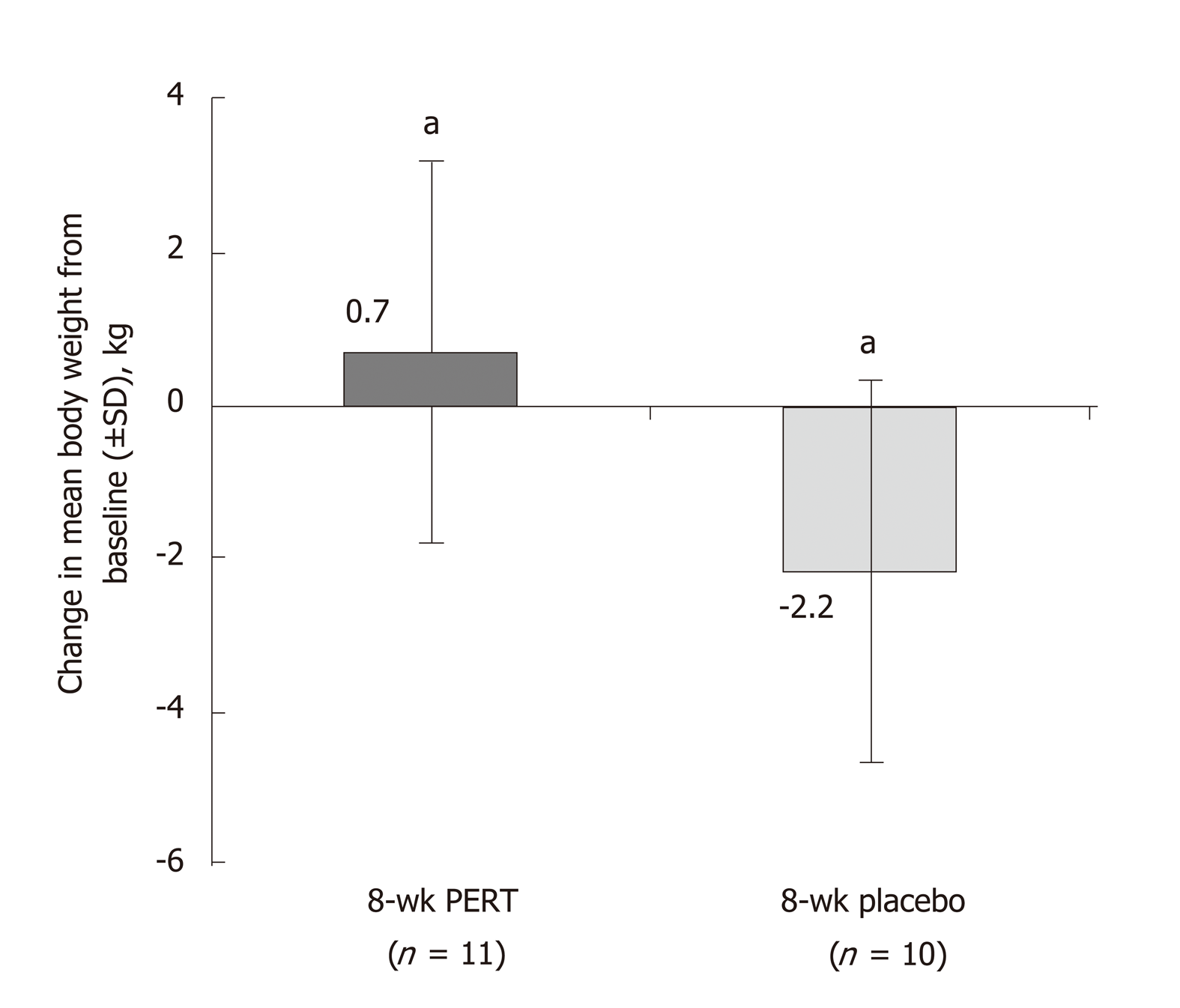
Two studies were identified that described the effects of PERT in patients with unresectable pancreatic cancer. One study in patients with advanced, unresectable cancer of the pancreatic head region and suspected pancreatic duct obstruction reported that PERT prevented weight loss in an 8-wk, randomized, double-blind, placebo-controlled study[37] (Supplementary Table 5). Patients randomized to PERT gained weight, while patients on placebo lost weight over the study duration (Figure 3). Furthermore, fat absorption increased by 12% with PERT, whereas it decreased by 8% in the placebo group[37]. A more recent randomized, double-blind, placebo-controlled study suggested that PERT had no significant effect on weight loss in patients with unresectable pancreatic cancer at 8 wk (P = 0.614; Supplementary Table 5)[38]. There was also no improvement in quality of life with PERT, and no significant difference in overall survival (5.84 mo with PERT vs 8.13 mo with placebo; P = 0.744; Supplementary Table 5 and Table 6)[38].
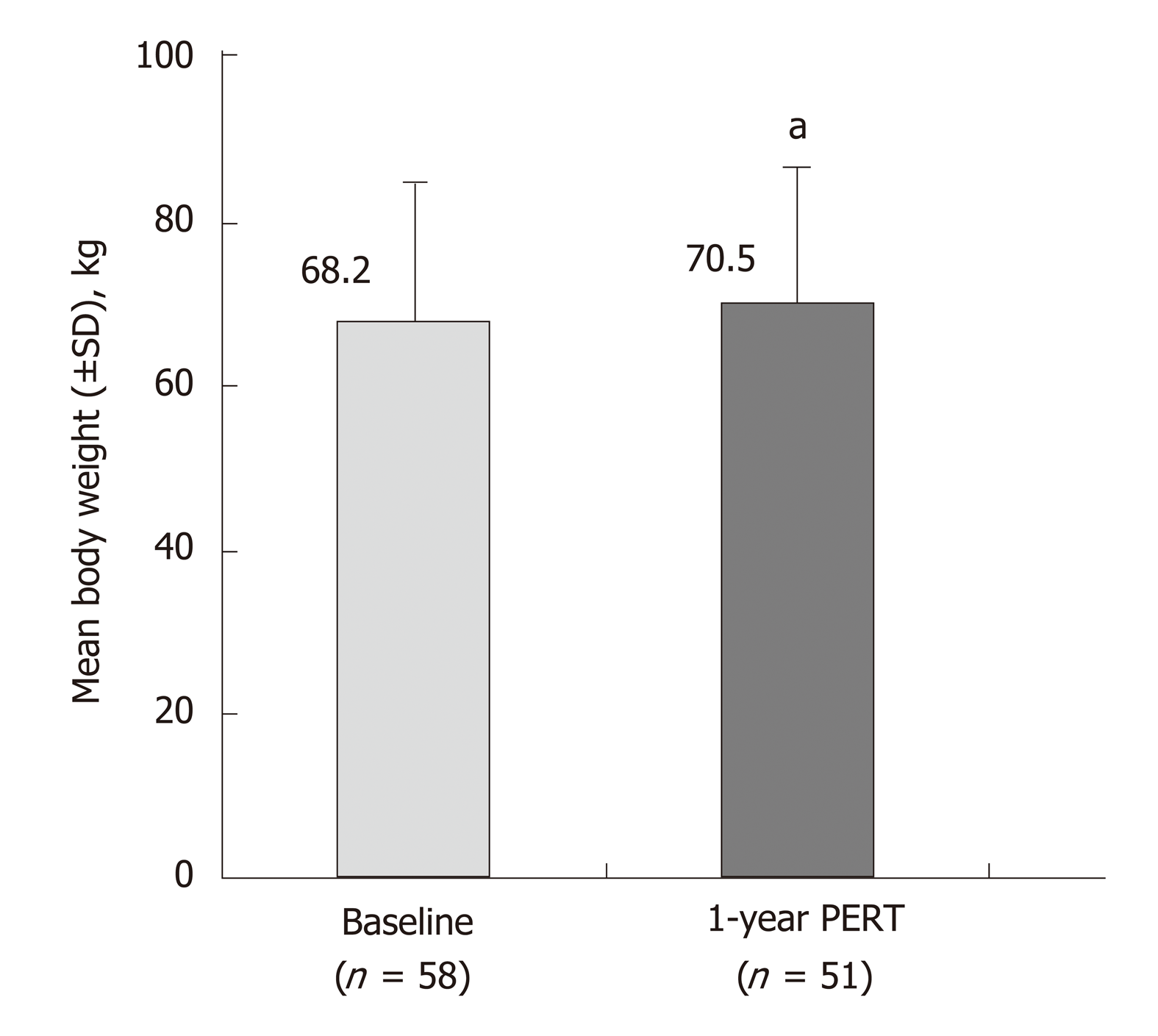
Two studies were identified that described the effects of PERT in patients that had undergone pancreatic surgery; indications for surgery were CP or pancreatic cancer[39,40]. PERT in patients with partial/total pancreatic resection resulted in significant improvements in fat and protein absorption in a 1-wk, randomized, placebo-controlled study (P < 0.001; Supplementary Table 7)[39]. Patients from this study then received PERT for 51 wk in an open-label extension, where improvements in fat and protein digestion were achieved and maintained to the end of follow-up (Supplementary Table 8)[39]. At this time point, body weight had also significantly increased compared with baseline (P < 0.05) (Figure 4)[39]. In a further small, uncontrolled study, PERT was administered for 2.5 years to patients following pancreatic surgery. Significant weight gain and decreased fecal fat excretion were observed during follow-up[40].
The aim of this review was to analyze the current evidence for the effectiveness of PERT in increasing survival and improving quality of life in patients with PEI, particularly those with chronic and severe underlying diseases such as CF, CP, or pancreatic cancer. Evidence from clinical trials supports the efficacy of PERT in treating PEI-related malabsorption and maintenance of a healthy weight in patients with PEI due to these underlying diseases.
CF is caused by mutations in the gene encoding CF transmembrane conductance regulator (CFTR): a protein highly expressed in pancreatic ductal epithelia, responsible for allowing the flow of anions and fluid into the ductal lumen[41]. As a result of these mutations, patients with CF have a decreased flow of anions and fluid into the pancreatic ductal lumen, leading to precipitation of proteins in the ductal lumen and, therefore, obstruction and damage to the pancreas[41]. Consequently, severe PEI is very common in newborns with CF, and is seen in approximately 85% of cases[18,26,42]. Although we identified a lack of studies in the literature explicitly measuring the link between PERT and prolonged survival of patients with CF, randomized, placebo-controlled studies show that PERT increases fat and protein absorption[19-25], while longer, open-label studies show that PERT improves the relevant clinical outcome of age-appropriate growth and weight gain or maintenance[27-29]. A single retrospective study in Moscow identified a potential link between PERT and life expectancy of patients with CF[43]. This study showed that, between 1993 and 2013, improvements in CF management, which included the introduction of PERT, led to an increase in life expectancy from 16 to 39 years[43]. These data suggest a potential link between PERT and life expectancy of patients with CF, although future long-term studies are needed to investigate this further.
The positive effects of PERT on PEI-associated malabsorption in children < 2 years of age with CF is particularly important as the first 2 years of life represent a period of intense growth, with high energy needs[27]. Therefore, addressing PEI-related malabsorption with PERT in those patients may be crucial to maintaining age-appropriate growth. Furthermore, wasting, which is linked with malnutrition, has been shown to be an independent prognosis predictor for survival in patients with CF[16,26,44,45]. The 5-year prognosis is better in patients with > 85% ideal body weight than in patients below that target (survival: 83.8% vs 53.4%, respectively; P < 0.0001)[45]. PEI-related malnutrition and impaired growth correlate with reduced lung function[46], which can ultimately increase mortality. An analysis of the European CF Patient Registry demonstrated that PEI was associated with a statistically significant (P < 0.0001) decrease in the forced expiratory volume (FEV1) vs patients without PEI[47]. Furthermore, patients with PEI were twice as likely to experience severe lung disease (defined as FEV1 < 40%) vs patients without PEI [47]. This indicates that the lack of pancreatic exocrine function is associated with worsening prognosis in CF. Collectively, the evidence suggests that preventing malnutrition and maintaining body weight with PERT may improve the prognosis of patients with PEI due to underlying CF.
CP is characterized by inflammation of the pancreas, leading to fibrosis, atrophy, and irreversible damage to pancreatic tissue[48]; PEI usually develops within 5 to 10 years of disease duration[49]. The presence of PEI in patients with CP is associated with a higher prevalence of diabetes, and lower levels of nutritional markers, e.g., magnesium, hemoglobin, albumin, prealbumin, and retinol binding protein[50]. The resulting malnutrition can lead to weight loss and can increase the morbidity and mortality risk in untreated patients[12,50]. Clinical trials have demonstrated that PERT improves PEI-related malabsorption and importantly increases body weight in patients with CP[31-36]. However, the impact of PERT on patient survival has only been assessed within the context of pancreatic surgery for CP[51]. The absence of PERT following surgery was a significant and independent risk factor for long-term mortality following hospital discharge, according to a retrospective observational study[51].
Relief of PEI-related symptoms, such as abdominal pain, flatulence, or steatorrhea, can improve quality of life in patients with CP and PEI[13,52]. Furthermore, in a 51-wk study PERT has been shown to lead to an improvement in seven of the eight components of the SF-36 and the two summary scores (including improvements in bodily pain, general health, vitality, role-emotional, mental health, and the mental component summary)[36]. The current evidence base, therefore, suggests that PERT may be effective in enhancing quality of life measures as well as addressing PEI-related symptoms, malnutrition, weight loss, and increased mortality risk in patients with CP. However, further long-term studies are needed to establish if any link exists between PERT and survival in these patients.
Diagnosis of pancreatic cancer is typically associated with a poor prognosis, as patients usually present at a late stage of disease progression; the 5-year survival rate was estimated at 7% during the 2004-2010 period[53]. Around 20% of patients are eligible for surgical resection of the tumor[54], and median survival ranges from 23.7-39.5 mo for these patients[55] to 8.5-11.1 mo for those with unresectable cancer and metastatic disease[56,57]. One of the predictive factors of survival in patients with advanced cancer is malnutrition[58]. Weight loss of > 10% of pre-illness stable weight is associated with increased metastases and significantly reduced survival compared with patients without dramatic weight loss[59]. Furthermore, weight stabilization in patients with unresectable pancreatic cancer was found to be associated with improved survival and quality of life[60].
PEI is highly prevalent in patients with resectable or unresectable pancreatic cancer, with an estimated prevalence of 50%-100% and 46%-100% in these patients, respectively[54]. This can be attributable to tumor growth, which may result in a combination of obstruction of the pancreatic duct, destruction of pancreatic parenchyma, and duodenal infiltration[3]. Moreover, relevant postoperative anatomical changes may occur after tumor resection, resulting in profound disturbances of coordinated intraluminal mixing of chyme with biliopancreatic secretions[3,11,61,62]. Of note, in patients with unresectable cancer, PEI may not always manifest with symptoms such as steatorrhea[54]. Severe PEI, i.e., fecal elastase-1 levels ≤ 20 µg/g, is an independent factor associated with poor prognosis in those patients and should, therefore, be addressed[63].
Although limited data on the effects of PERT in patients with pancreatic cancer are available (as most of the evidence comes from evaluation of patients with CP), clinical evidence suggests that PERT can prevent weight loss both in patients with unresectable pancreatic cancer[37] and patients recovering from pancreatic resection[61]. Furthermore, a retrospective analysis conducted in patients with unresectable pancreatic carcinoma found that PERT and nutritional advice were associated with increased survival (301 d [95% confidence interval (CI): 151-451] vs 89 d [95%CI: 30-148]; P = 0.002)[64]. Another retrospective study in patients with unresectable pancreatic cancer similarly reported that PERT resulted in longer survival (189 d [95%CI: 167.0-211.0] vs 95 d [95%CI: 75.4-114.6]; P < 0.001), especially in patients with significant weight loss at diagnosis[65]. The authors concluded that PEI and its treatment should be taken into consideration for optimal patient care, to increase survival and quality of life[65]. Similarly, a recent population-based study in patients with pancreatic cancer found that PERT was associated with an increased medial survival time (274 d vs 140 d; P < 0.001), suggesting a significant benefit for patients[66]. Finally, a review of patients undergoing pancreatoduodenectomy for cancer also found that PERT was independently associated with improved survival on multivariate analysis (33.1 mo vs 26.7 mo; P = 0.046)[67]. These findings support the fact that weight loss in patients with terminal pancreatic cancer is often one of the main factors affecting survival and quality of life. Weight loss is often observed post-surgery, but is also observed in non-surgical patients who suffer from fat and protein malabsorption due to PEI[68].
In contrast to the studies summarized above, a recent open-label, randomized trial evaluating the benefits of PERT in 88 patients with unresectable pancreatic cancer revealed no significant differences in BMI or nutritional status between the PERT and non-PERT groups at 8 wk. Median overall survival was 19.0 mo in the PERT group compared with 12.0 mo in the non-PERT group, but this difference was not statistically significant (P = 0.07)[69].
Despite the suggested beneficial effects of PERT in patients with pancreatic cancer, a recent retrospective analysis conducted between 2010 and 2012 showed that PERT is underused in patients with metastatic pancreatic cancer[68]. Over 70% of the 129 patients with pancreatic cancer referred to specialist palliative care had malabsorption-related symptoms, e.g., abdominal pain, bloating, wind, and steatorrhea, but only 21% were prescribed PERT[68]. Similarly, a recent population-based study reported that only 21.7% of 4554 patients with pancreatic cancer were prescribed PERT[66]. A review of patients undergoing pancreatoduodenectomy for cancer reported that only 43.1% of patients received PERT[67]. Furthermore, a survey conducted in patients following pancreatic surgery (due to CP or pancreatic cancer) and receiving PERT showed that these patients were under-dosed in daily practice[70]. Hence, addressing the symptoms of PEI and the associated malnutrition in patients with pancreatic cancer could be key in reducing the significant burden of this disease. Recent clinical opinion is that PERT should be considered for the management of PEI in patients with pancreatic cancer[65]; however, despite PERT being a relatively simple and inexpensive treatment, it has yet to gain recognition from oncologists[71].
This review of the current literature supports the effectiveness of PERT in addressing PEI-related malabsorption in patients with CF, CP, or pancreatic cancer. However, there is a lack of long-term trials assessing the effect of PERT on patient survival (especially in patients with CF or CP). Despite these limitations, there is substantial evidence to support the hypothesis that PERT allows patients with PEI to improve body weight by preventing malnutrition, a known risk factor for decreased survival[7]. Furthermore, adequate PERT reduces the occurrence of GI symptoms and abdominal pain commonly associated with PEI, thereby improving patients’ quality of life[13,52].
In clinical practice, the absence of PERT, or undertreatment with PERT, may not be uncommon during management of patients with PEI[40,70]. Likely explanations include the variability of clinical PEI manifestations, which are not always suggestive of maldigestion (particularly in the absence of overt steatorrhea), and difficulties in the routine diagnosis of non-severe PEI[9]. Hence, efforts should be made to raise clinical awareness about PEI, both in terms of the correct diagnostic procedures and the optimal management strategies. It can be surmised from the (albeit indirect) evidence presented in this review that in patients with undertreated PEI, adequate PERT may be associated with improved quality of life. The question of whether PERT also affects the long-term survival of patients with PEI should be the subject of future studies.
Editorial assistance was provided to authors by Alpharmaxim Healthcare Commu-nications.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Germany
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aykan NF, Löhr JM S-Editor: Ma RY L-Editor: A E-Editor: Zhang YL
| 1. | Sikkens EC, Cahen DL, Kuipers EJ, Bruno MJ. Pancreatic enzyme replacement therapy in chronic pancreatitis. Best Pract Res Clin Gastroenterol. 2010;24:337-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 84] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 2. | Imrie CW, Connett G, Hall RI, Charnley RM. Review article: enzyme supplementation in cystic fibrosis, chronic pancreatitis, pancreatic and periampullary cancer. Aliment Pharmacol Ther. 2010;32 Suppl 1:1-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Keller J, Layer P. Human pancreatic exocrine response to nutrients in health and disease. Gut. 2005;54 Suppl 6:vi1-v28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 204] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 4. | Gooden HM, White KJ. Pancreatic cancer and supportive care--pancreatic exocrine insufficiency negatively impacts on quality of life. Support Care Cancer. 2013;21:1835-1841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 88] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 5. | Wehler M, Nichterlein R, Fischer B, Farnbacher M, Reulbach U, Hahn EG, Schneider T. Factors associated with health-related quality of life in chronic pancreatitis. Am J Gastroenterol. 2004;99:138-146. [PubMed] |
| 6. | Mokrowiecka A, Pinkowski D, Malecka-Panas E, Johnson CD. Clinical, emotional and social factors associated with quality of life in chronic pancreatitis. Pancreatology. 2010;10:39-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 7. | Nakajima K, Oshida H, Muneyuki T, Kakei M. Pancrelipase: an evidence-based review of its use for treating pancreatic exocrine insufficiency. Core Evid. 2012;7:77-91. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Leeds JS, Hopper AD, Sidhu R, Simmonette A, Azadbakht N, Hoggard N, Morley S, Sanders DS. Some patients with irritable bowel syndrome may have exocrine pancreatic insufficiency. Clin Gastroenterol Hepatol. 2010;8:433-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 80] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 9. | Keller J, Brückel S, Jahr C, Layer P. A modified ¹³C-mixed triglyceride breath test detects moderate pancreatic exocrine insufficiency. Pancreas. 2011;40:1201-1205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Phillips ME. Pancreatic exocrine insufficiency following pancreatic resection. Pancreatology. 2015;15:449-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 66] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 11. | Keim V, Klar E, Poll M, Schoenberg MH. Postoperative care following pancreatic surgery: surveillance and treatment. Dtsch Arztebl Int. 2009;106:789-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Dominguez-Muñoz JE. Diagnosis and treatment of pancreatic exocrine insufficiency. Curr Opin Gastroenterol. 2018;34:349-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 63] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 13. | Czakó L, Takács T, Hegyi P, Prónai L, Tulassay Z, Lakner L, Döbrönte Z, Boda K, Lonovics J. Quality of life assessment after pancreatic enzyme replacement therapy in chronic pancreatitis. Can J Gastroenterol. 2003;17:597-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 50] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Huang NN, Schidlow DV, Szatrowski TH, Palmer J, Laraya-Cuasay LR, Yeung W, Hardy K, Quitell L, Fiel S. Clinical features, survival rate, and prognostic factors in young adults with cystic fibrosis. Am J Med. 1987;82:871-879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 70] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Layer P, von der Ohe MR, Holst JJ, Jansen JB, Grandt D, Holtmann G, Goebell H. Altered postprandial motility in chronic pancreatitis: role of malabsorption. Gastroenterology. 1997;112:1624-1634. [PubMed] |
| 16. | Levy E. Nutrition-related derangements and managements in patients with cystic fibrosis: robust challenges for preventing the development of co-morbidities. Clin Biochem. 2011;44:489-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Borowitz DS, Grand RJ, Durie PR. Use of pancreatic enzyme supplements for patients with cystic fibrosis in the context of fibrosing colonopathy. Consensus Committee. J Pediatr. 1995;127:681-684. [PubMed] |
| 18. | Borowitz D, Gelfond D, Maguiness K, Heubi JE, Ramsey B. Maximal daily dose of pancreatic enzyme replacement therapy in infants with cystic fibrosis: a reconsideration. J Cyst Fibros. 2013;12:784-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Borowitz D, Stevens C, Brettman LR, Campion M, Chatfield B, Cipolli M; Liprotamase 726 Study Group. International phase III trial of liprotamase efficacy and safety in pancreatic-insufficient cystic fibrosis patients. J Cyst Fibros. 2011;10:443-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Heubi JE, Schaeffer D, Ahrens RC, Sollo N, Strausbaugh S, Graff G, Jain R, Witte S, Forssmann K. Safety and Efficacy of a Novel Microbial Lipase in Patients with Exocrine Pancreatic Insufficiency due to Cystic Fibrosis: A Randomized Controlled Clinical Trial. J Pediatr. 2016;176:156-161.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Graff GR, Maguiness K, McNamara J, Morton R, Boyd D, Beckmann K, Bennett D. Efficacy and tolerability of a new formulation of pancrelipase delayed-release capsules in children aged 7 to 11 years with exocrine pancreatic insufficiency and cystic fibrosis: a multicenter, randomized, double-blind, placebo-controlled, two-period crossover, superiority study. Clin Ther. 2010;32:89-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 45] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 22. | Trapnell BC, Maguiness K, Graff GR, Boyd D, Beckmann K, Caras S. Efficacy and safety of Creon 24,000 in subjects with exocrine pancreatic insufficiency due to cystic fibrosis. J Cyst Fibros. 2009;8:370-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 23. | Stern RC, Eisenberg JD, Wagener JS, Ahrens R, Rock M, doPico G, Orenstein DM. A comparison of the efficacy and tolerance of pancrelipase and placebo in the treatment of steatorrhea in cystic fibrosis patients with clinical exocrine pancreatic insufficiency. Am J Gastroenterol. 2000;95:1932-1938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 63] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 24. | Wooldridge JL, Heubi JE, Amaro-Galvez R, Boas SR, Blake KV, Nasr SZ, Chatfield B, McColley SA, Woo MS, Hardy KA, Kravitz RM, Straforini C, Anelli M, Lee C. EUR-1008 pancreatic enzyme replacement is safe and effective in patients with cystic fibrosis and pancreatic insufficiency. J Cyst Fibros. 2009;8:405-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 45] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Trapnell BC, Strausbaugh SD, Woo MS, Tong SY, Silber SA, Mulberg AE, Leitz G. Efficacy and safety of PANCREAZE® for treatment of exocrine pancreatic insufficiency due to cystic fibrosis. J Cyst Fibros. 2011;10:350-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 26. | Sinaasappel M, Stern M, Littlewood J, Wolfe S, Steinkamp G, Heijerman HG, Robberecht E, Döring G. Nutrition in patients with cystic fibrosis: a European Consensus. J Cyst Fibros. 2002;1:51-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 258] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 27. | Colombo C, Fredella C, Russo MC, Faelli N, Motta V, Valmarana L, Longo L, D'Orazio C. Efficacy and tolerability of Creon for Children in infants and toddlers with pancreatic exocrine insufficiency caused by cystic fibrosis: an open-label, single-arm, multicenter study. Pancreas. 2009;38:693-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 28. | Kashirskaya NY, Kapranov NI, Sander-Struckmeier S, Kovalev V. Safety and efficacy of Creon® micro in children with exocrine pancreatic insufficiency due to cystic fibrosis. J Cyst Fibros. 2015;14:275-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Borowitz D, Stevens C, Brettman LR, Campion M, Wilschanski M, Thompson H; Liprotamase 767 Study Group. Liprotamase long-term safety and support of nutritional status in pancreatic-insufficient cystic fibrosis. J Pediatr Gastroenterol Nutr. 2012;54:248-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 30. | Munck A, Duhamel JF, Lamireau T, Le Luyer B, Le Tallec C, Bellon G, Roussey M, Foucaud P, Giniès JL, Houzel A, Marguet C, Guillot M, David V, Kapel N, Dyard F, Henniges F. Pancreatic enzyme replacement therapy for young cystic fibrosis patients. J Cyst Fibros. 2009;8:14-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 31. | Safdi M, Bekal PK, Martin S, Saeed ZA, Burton F, Toskes PP. The effects of oral pancreatic enzymes (Creon 10 capsule) on steatorrhea: a multicenter, placebo-controlled, parallel group trial in subjects with chronic pancreatitis. Pancreas. 2006;33:156-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 73] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 32. | Toskes PP, Secci A, Thieroff-Ekerdt R; ZENPEP Study Group. Efficacy of a novel pancreatic enzyme product, EUR-1008 (Zenpep), in patients with exocrine pancreatic insufficiency due to chronic pancreatitis. Pancreas. 2011;40:376-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 33. | Thorat V, Reddy N, Bhatia S, Bapaye A, Rajkumar JS, Kini DD, Kalla MM, Ramesh H. Randomised clinical trial: the efficacy and safety of pancreatin enteric-coated minimicrospheres (Creon 40000 MMS) in patients with pancreatic exocrine insufficiency due to chronic pancreatitis--a double-blind, placebo-controlled study. Aliment Pharmacol Ther. 2012;36:426-436. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 34. | Whitcomb DC, Lehman GA, Vasileva G, Malecka-Panas E, Gubergrits N, Shen Y, Sander-Struckmeier S, Caras S. Pancrelipase delayed-release capsules (CREON) for exocrine pancreatic insufficiency due to chronic pancreatitis or pancreatic surgery: A double-blind randomized trial. Am J Gastroenterol. 2010;105:2276-2286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 141] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 35. | Gubergrits N, Malecka-Panas E, Lehman GA, Vasileva G, Shen Y, Sander-Struckmeier S, Caras S, Whitcomb DC. A 6-month, open-label clinical trial of pancrelipase delayed-release capsules (Creon) in patients with exocrine pancreatic insufficiency due to chronic pancreatitis or pancreatic surgery. Aliment Pharmacol Ther. 2011;33:1152-1161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 78] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 36. | Ramesh H, Reddy N, Bhatia S, Rajkumar JS, Bapaye A, Kini D, Kalla M, Thorat V. A 51-week, open-label clinical trial in India to assess the efficacy and safety of pancreatin 40000 enteric-coated minimicrospheres in patients with pancreatic exocrine insufficiency due to chronic pancreatitis. Pancreatology. 2013;13:133-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 37. | Bruno MJ, Haverkort EB, Tijssen GP, Tytgat GN, van Leeuwen DJ. Placebo controlled trial of enteric coated pancreatin microsphere treatment in patients with unresectable cancer of the pancreatic head region. Gut. 1998;42:92-96. [PubMed] |
| 38. | Woo SM, Joo J, Kim SY, Park SJ, Han SS, Kim TH, Koh YH, Chung SH, Kim YH, Moon H, Hong EK, Lee WJ. Efficacy of pancreatic exocrine replacement therapy for patients with unresectable pancreatic cancer in a randomized trial. Pancreatology. 2016;16:1099-1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 39. | Seiler CM, Izbicki J, Varga-Szabó L, Czakó L, Fiók J, Sperti C, Lerch MM, Pezzilli R, Vasileva G, Pap A, Varga M, Friess H. Randomised clinical trial: a 1-week, double-blind, placebo-controlled study of pancreatin 25 000 Ph. Eur. minimicrospheres (Creon 25000 MMS) for pancreatic exocrine insufficiency after pancreatic surgery, with a 1-year open-label extension. Aliment Pharmacol Ther. 2013;37:691-702. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 67] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 40. | Braga M, Cristallo M, De Franchis R, Mangiagalli A, Zerbi A, Agape D, Primignani M, Di Carlo V. Pancreatic enzyme replacement therapy in post-pancreatectomy patients. Int J Pancreatol. 1989;5 Suppl:37-44. [PubMed] |
| 41. | Wilschanski M, Novak I. The cystic fibrosis of exocrine pancreas. Cold Spring Harb Perspect Med. 2013;3:a009746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 107] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 42. | Couper RT, Corey M, Moore DJ, Fisher LJ, Forstner GG, Durie PR. Decline of exocrine pancreatic function in cystic fibrosis patients with pancreatic sufficiency. Pediatr Res. 1992;32:179-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 67] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 43. | Kashirskaya NY, Krasovsky SA, Chernyak AV, Sherman VD, Voronkova AY, Shabalova LA, Nikonova VS, Gorinova YV, Simonova OI, Amelina EL, Kondrat'eva EI, Kapranov NI, Petrova NV, Zinchenko RA. Trends in life expectancy of cystic fibrosis patients in Moscow and their connection with the treatment received: retrospective analysis for 1993-2013 [in Russian]. Current Pediatrics. 2015;14:503-508. [RCA] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 44. | Gaskin KJ. Nutritional care in children with cystic fibrosis: are our patients becoming better? Eur J Clin Nutr. 2013;67:558-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 45. | Sharma R, Florea VG, Bolger AP, Doehner W, Florea ND, Coats AJ, Hodson ME, Anker SD, Henein MY. Wasting as an independent predictor of mortality in patients with cystic fibrosis. Thorax. 2001;56:746-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 177] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 46. | Konstan MW, Butler SM, Wohl ME, Stoddard M, Matousek R, Wagener JS, Johnson CA, Morgan WJ; Investigators and Coordinators of the Epidemiologic Study of Cystic Fibrosis. Growth and nutritional indexes in early life predict pulmonary function in cystic fibrosis. J Pediatr. 2003;142:624-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 287] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 47. | Kerem E, Viviani L, Zolin A, MacNeill S, Hatziagorou E, Ellemunter H, Drevinek P, Gulmans V, Krivec U, Olesen H; ECFS Patient Registry Steering Group. Factors associated with FEV1 decline in cystic fibrosis: analysis of the ECFS patient registry. Eur Respir J. 2014;43:125-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 214] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 48. | Forsmark CE. Management of chronic pancreatitis. Gastroenterology. 2013;144:1282-91.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 139] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 49. | Löhr JM, Oliver MR, Frulloni L. Synopsis of recent guidelines on pancreatic exocrine insufficiency. United European Gastroenterol J. 2013;1:79-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 50. | Lindkvist B, Domínguez-Muñoz JE, Luaces-Regueira M, Castiñeiras-Alvariño M, Nieto-Garcia L, Iglesias-Garcia J. Serum nutritional markers for prediction of pancreatic exocrine insufficiency in chronic pancreatitis. Pancreatology. 2012;12:305-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 108] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 51. | Winny M, Paroglou V, Bektas H, Kaltenborn A, Reichert B, Zachau L, Kleine M, Klempnauer J, Schrem H. Insulin dependence and pancreatic enzyme replacement therapy are independent prognostic factors for long-term survival after operation for chronic pancreatitis. Surgery. 2014;155:271-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 52. | D'Haese JG, Ceyhan GO, Demir IE, Layer P, Uhl W, Löhr M, Rychlik R, Pirilis K, Zöllner Y, Gradl B, Foerster D, Möbius J, Henniges F, Friess H. Pancreatic enzyme replacement therapy in patients with exocrine pancreatic insufficiency due to chronic pancreatitis: a 1-year disease management study on symptom control and quality of life. Pancreas. 2014;43:834-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 53. | Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9172] [Cited by in RCA: 9957] [Article Influence: 995.7] [Reference Citation Analysis (0)] |
| 54. | Bartel MJ, Asbun H, Stauffer J, Raimondo M. Pancreatic exocrine insufficiency in pancreatic cancer: A review of the literature. Dig Liver Dis. 2015;47:1013-1020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 62] [Article Influence: 6.2] [Reference Citation Analysis (1)] |
| 55. | Neoptolemos JP, Palmer DH, Ghaneh P, Psarelli EE, Valle JW, Halloran CM, Faluyi O, O'Reilly DA, Cunningham D, Wadsley J, Darby S, Meyer T, Gillmore R, Anthoney A, Lind P, Glimelius B, Falk S, Izbicki JR, Middleton GW, Cummins S, Ross PJ, Wasan H, McDonald A, Crosby T, Ma YT, Patel K, Sherriff D, Soomal R, Borg D, Sothi S, Hammel P, Hackert T, Jackson R, Büchler MW; European Study Group for Pancreatic Cancer. Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): a multicentre, open-label, randomised, phase 3 trial. Lancet. 2017;389:1011-1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1327] [Cited by in RCA: 1394] [Article Influence: 174.3] [Reference Citation Analysis (0)] |
| 56. | Von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, Seay T, Tjulandin SA, Ma WW, Saleh MN, Harris M, Reni M, Dowden S, Laheru D, Bahary N, Ramanathan RK, Tabernero J, Hidalgo M, Goldstein D, Van Cutsem E, Wei X, Iglesias J, Renschler MF. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369:1691-1703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4035] [Cited by in RCA: 4883] [Article Influence: 406.9] [Reference Citation Analysis (0)] |
| 57. | Conroy T, Desseigne F, Ychou M, Bouché O, Guimbaud R, Bécouarn Y, Adenis A, Raoul JL, Gourgou-Bourgade S, de la Fouchardière C, Bennouna J, Bachet JB, Khemissa-Akouz F, Péré-Vergé D, Delbaldo C, Assenat E, Chauffert B, Michel P, Montoto-Grillot C, Ducreux M; Groupe Tumeurs Digestives of Unicancer; PRODIGE Intergroup. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364:1817-1825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4838] [Cited by in RCA: 5634] [Article Influence: 402.4] [Reference Citation Analysis (1)] |
| 58. | Tan CS, Read JA, Phan VH, Beale PJ, Peat JK, Clarke SJ. The relationship between nutritional status, inflammatory markers and survival in patients with advanced cancer: a prospective cohort study. Support Care Cancer. 2015;23:385-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 59. | Bachmann J, Ketterer K, Marsch C, Fechtner K, Krakowski-Roosen H, Büchler MW, Friess H, Martignoni ME. Pancreatic cancer related cachexia: influence on metabolism and correlation to weight loss and pulmonary function. BMC Cancer. 2009;9:255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 97] [Cited by in RCA: 114] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 60. | Davidson W, Ash S, Capra S, Bauer J; Cancer Cachexia Study Group. Weight stabilisation is associated with improved survival duration and quality of life in unresectable pancreatic cancer. Clin Nutr. 2004;23:239-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 134] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 61. | Domínguez-Muñoz JE. Pancreatic enzyme replacement therapy: exocrine pancreatic insufficiency after gastrointestinal surgery. HPB (Oxford). 2009;11 Suppl 3:3-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 45] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 62. | Mössner J, Keim V. Pancreatic enzyme therapy. Dtsch Arztebl Int. 2010;108:578-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 63. | Partelli S, Frulloni L, Minniti C, Bassi C, Barugola G, D'Onofrio M, Crippa S, Falconi M. Faecal elastase-1 is an independent predictor of survival in advanced pancreatic cancer. Dig Liver Dis. 2012;44:945-951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 76] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 64. | Domínguez-Muñoz JE, Nieto-Garcia L, Iglesias-Garcia J. Impact of diagnosis and treatment of pancreatic exocrine insufficiency (PEI) on survival of patients with unresectable pancreatic cancer (PC). Pancreatology. 2013;13:S80. PII-93 Abstract id: 188. [DOI] [Full Text] |
| 65. | Domínguez-Muñoz JE, Nieto-Garcia L, López-Díaz J, Lariño-Noia J, Abdulkader I, Iglesias-Garcia J. Impact of the treatment of pancreatic exocrine insufficiency on survival of patients with unresectable pancreatic cancer: a retrospective analysis. BMC Cancer. 2018;18:534. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 80] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 66. | Roberts KJ, Bannister CA, Schrem H. Enzyme replacement improves survival among patients with pancreatic cancer: Results of a population based study. Pancreatology. 2019;19:114-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 88] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 67. | Roberts KJ, Schrem H, Hodson J, Angelico R, Dasari BVM, Coldham CA, Marudanayagam R, Sutcliffe RP, Muiesan P, Isaac J, Mirza DF. Pancreas exocrine replacement therapy is associated with increased survival following pancreatoduodenectomy for periampullary malignancy. HPB (Oxford). 2017;19:859-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 60] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 68. | Landers A, Muircroft W, Brown H. Pancreatic enzyme replacement therapy (PERT) for malabsorption in patients with metastatic pancreatic cancer. BMJ Support Palliat Care. 2016;6:75-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 69. | Saito T, Nakai Y, Isayama H, Hirano K, Ishigaki K, Hakuta R, Takeda T, Saito K, Umefune G, Akiyama D, Watanabe T, Takagi K, Takahara N, Hamada T, Uchino R, Mizuno S, Mouri D, Yagioka H, Kogure H, Togawa O, Matsubara S, Ito Y, Yamamoto N, Tada M, Koike K. A Multicenter Open-Label Randomized Controlled Trial of Pancreatic Enzyme Replacement Therapy in Unresectable Pancreatic Cancer. Pancreas. 2018;47:800-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 70. | Sikkens EC, Cahen DL, van Eijck C, Kuipers EJ, Bruno MJ. The daily practice of pancreatic enzyme replacement therapy after pancreatic surgery: a northern European survey: enzyme replacement after surgery. J Gastrointest Surg. 2012;16:1487-1492. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 77] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 71. | Damerla V, Gotlieb V, Larson H, Saif MW. Pancreatic enzyme supplementation in pancreatic cancer. J Support Oncol. 2008;6:393-396. [PubMed] |