Published online May 7, 2019. doi: 10.3748/wjg.v25.i17.2144
Peer-review started: February 18, 2019
First decision: March 14, 2019
Revised: March 29, 2019
Accepted: April 19, 2019
Article in press: April 20, 2019
Published online: May 7, 2019
Processing time: 79 Days and 10.7 Hours
Esophagomediastinal fistula is a very rare complication of tuberculosis in otherwise healthy adults, and mediastinal bronchial artery aneurysm is even rarer. In this case report, we describe a rare case of tuberculosis complication that presented with acute upper gastrointestinal (GI) bleeding. It also highlights the benefits of chest computed tomography (CT) as an excellent adjunct diagnostic tool to endoscopy and bronchoscopy and the role of trans-arterial embolization as a minimal invasive therapy alternative to surgery.
A 19-year-old medically free male patient presented with acute multiple episodes of hematemesis for 1 d. Upper GI endoscopy, bronchoscopy, and chest CT with IV contrast confirmed esophagomediastinal fistula with mediastinal bronchial artery aneurysm. After resuscitating patient with IV fluid and blood product transfusion, trans catheter embolization was performed for mediastinal bronchial artery aneurysm.
We successfully treated a patient with acute upper GI bleeding due to tuberculous esophagomediastinal fistula and mediastinal bronchial artery aneurysm using transcatheter coil embolization.
Core tip: A 19-year-old medically free male patient presented with acute upper gastrointestinal bleeding. He underwent endoscopy, bronchoscopy, and chest computed tomography with IV contrast. Diagnosis of pulmonary and mediastinal tuberculosis with esophagomediastinal fistula and mediastinal bronchial artery aneurysms was made. Patient was successfully treated with mediastinal bronchial artery aneurysm coil embolization and antitubercular medications.
- Citation: Alharbi SR. Tuberculous esophagomediastinal fistula with concomitant mediastinal bronchial artery aneurysm-acute upper gastrointestinal bleeding: A case report. World J Gastroenterol 2019; 25(17): 2144-2148
- URL: https://www.wjgnet.com/1007-9327/full/v25/i17/2144.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i17.2144
Mediastinal tuberculosis (TB) lymphadenitis is a rare clinical manifestation of TB in adults, and it usually occurs secondary to pulmonary TB. Extrapulmonary lymph node TB was reported to be 17.6% of all TB cases[1]. Esophagomediastinal fistula formation secondary to mediastinal TB lymphadenitis is an unusual complication that develops as a consequence of erosion of adjacent organs[2]. Mediastinal bronchial artery aneurysms are extremely rare and can be idiopathic or secondary. Secondary aneurysms are usually related to an underlying inflammatory process like bronchiectasis, chronic bronchitis, or systemic vascular disease[3,4]. Bronchial artery aneurysm with an esophageal fistula is an extremely rare and potentially fatal diagnosis, and there are few case reports in literature[5].
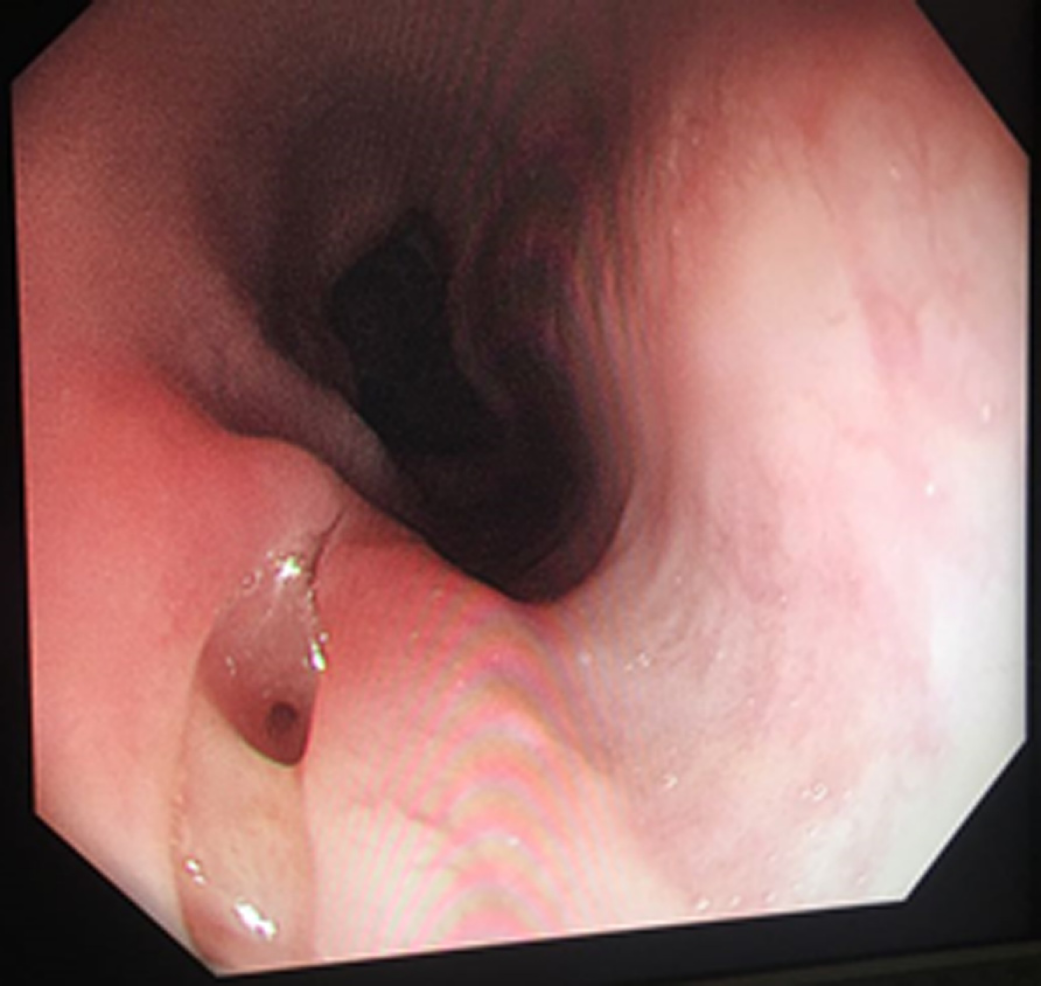
A 19-year-old medically free patient presented to our emergency department with 1-d history of 5 episodes of hematemesis with moderate amount associated with epigastric pain. His medical history is significant for chronic cough with occasional hemoptysis and weight loss for 5 mo. His vital signs are stable. Patient was pale, but there was no jaundice or cyanosis. Chest and abdominal examinations are unremarkable. Laboratory investigations show normal results except low hemoglobin level of 8 g/dL. Two units of packed red blood cells (PRBCs) were transfused. Upper gastrointestinal (GI) endoscopy shows an opening in the mid-esophagus without clot, bleeding, or mucosal lesions, otherwise a normal esophagus, stomach, and duodenum (Figure 1). Tracheoesophageal fistula was suspected, and no definite source of bleeding was identified.
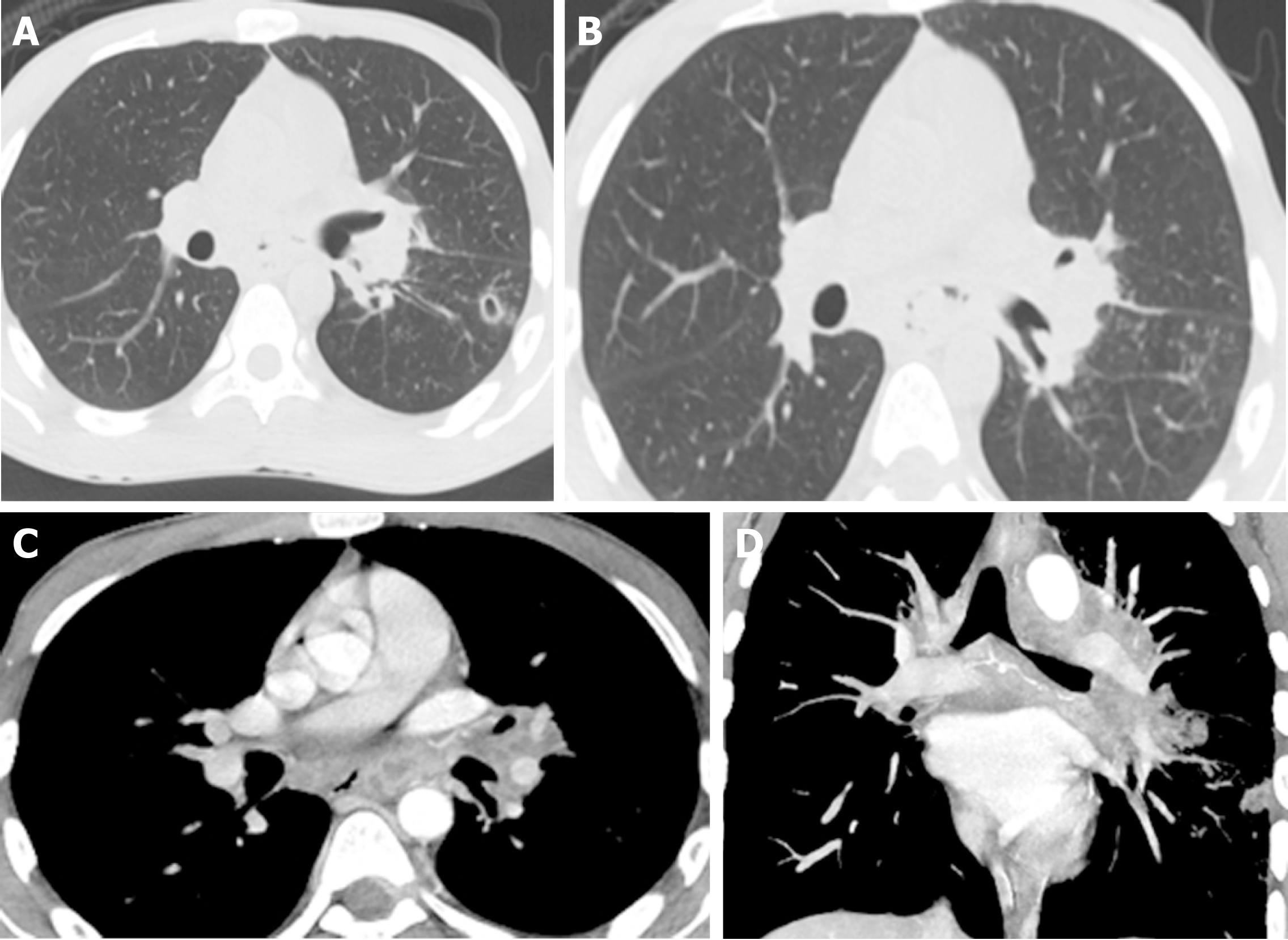
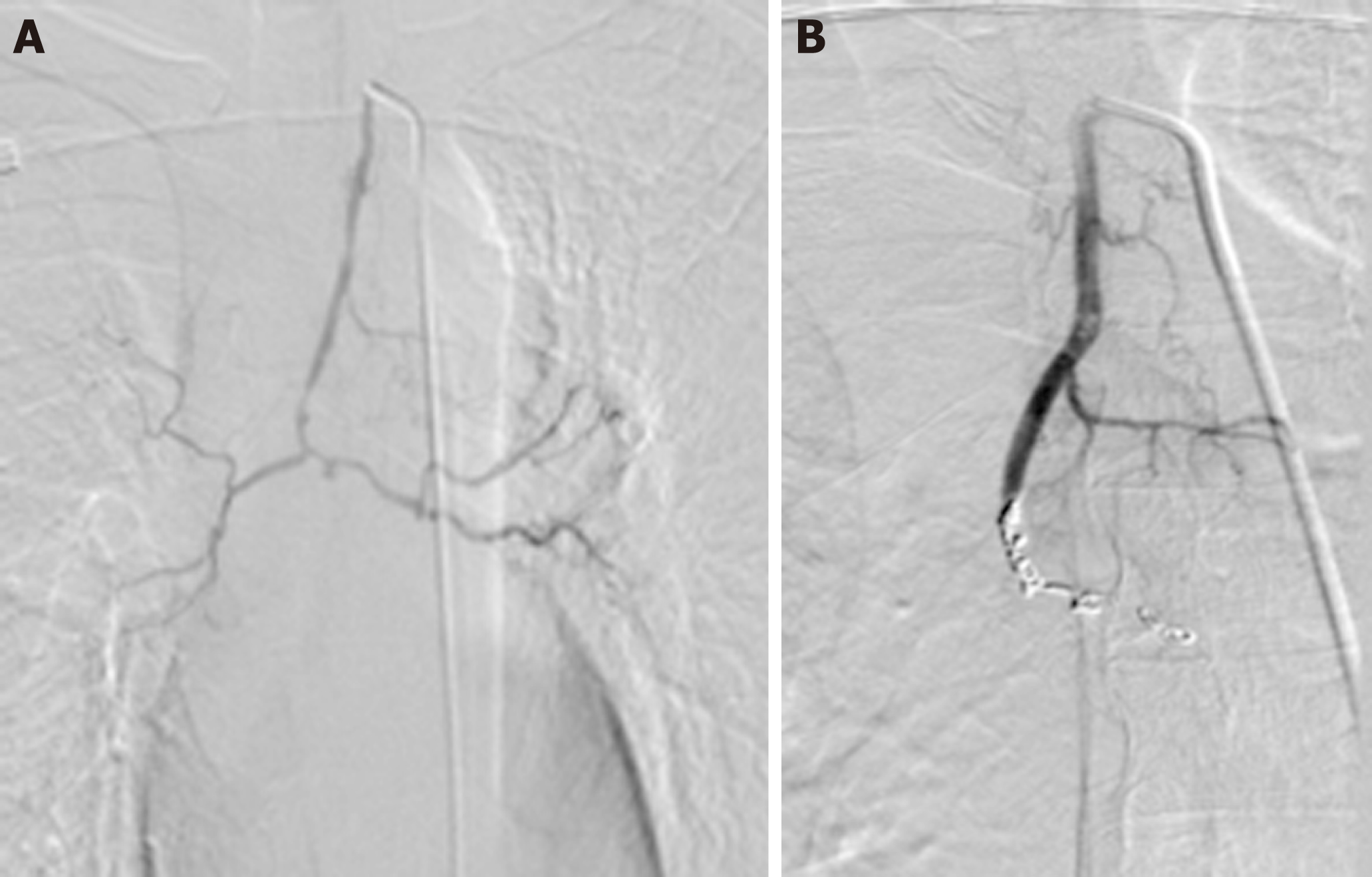
Bronchoscopy was performed and showed no tracheoesophageal fistula but edematous mucosa with nodular lesions in the left lower lobe bronchus. Biopsy was performed. Initial chest X-ray shows cavitary left lung lesion. Three sputum samples were sent for Ziehl-Neelsen (ZN) staining and were negative. Chest computed tomography (CT) with IV contrast was performed and showed evidence of esophagomediastinal fistula, multiple necrotic mediastinal lymph nodes, cavitary lung lesion, and two small mediastinal bronchial artery aneurysms indicating pulmonary and mediastinum TB (Figure 2). Patient had another episode of hematemesis with moderate amount. Upper GI endoscopy was repeated and unremarkable except a small opening in the mid-esophagus. Another two units of PRBC were transfused. Conventional angiography was performed and showed bronchial artery arising from the left subclavian artery with two small mediastinal bronchial artery aneurysms. Embolization was performed using coils (Figure 3). Histopathological results of bronchial biopsy showed necrotizing granulomatous inflammation suggesting TB, and two additional sputum samples were sent for ZN staining and were positive. Anti-TB medication was started. Patient did not have hematemesis or melena after embolization. Patient was discharged in good condition with anti-TB medications. At 3-mo of follow-up, patient was asymptomatic and had no episode of GI bleeding. Follow-up chest X-ray shows interval improvement (Figure 4).
Tuberculous esophagomediastinal fistula with mediastinal bronchial artery aneurysm.
Patient was treated by mediastinal bronchial artery aneurysm trans catheter coil embolization and antitubercular medications.
After 3 mo of mediastinal bronchial artery aneurysm embolization and initiation of antitubercular medication, patient become asymptomatic and no further episode of GI bleeding was encountered. Follow-up chest X-ray shows interval resolution of lung cavity.
Esophageal involvement in TB is extremely rare in otherwise healthy individuals. It mostly affects the mid-esophagus and is secondary to direct extension from the surrounding structures such as mediastinal lymph nodes, lungs, and vertebrae. The usual presenting symptoms are dysphagia or odynophagia[2]. There are several reports on esophageal TB that appeared as submucosal lesions mimicking a mass, ulcer, diverticulum, or only sinus opening[1].
Bronchial artery aneurysm is a rare condition with reported rate of < 1% in selective bronchial arteriogram[6]. It is can be classified according to location as mediastinal or intrapulmonary. Clinical presentation is variable depending on the size, location, concomitant disease and if it is ruptured or not. Although it usually detected incidentally on chest CT, the most frequent symptoms are hemoptysis, chest pain, and hemomediastinum[7]. Chest CT is greatly helpful in detecting TB manifestation in the chest and mediastinal lymph nodes as well as associated fistula formation[8]. CT angiography and conventional angiography are commonly used tools to diagnose mediastinal bronchial aneurysm[3].
Mediastinal bronchial artery aneurysms are fatal and even asymptomatic, requiring treatment regardless of the diameter. Endovascular embolization is the first line of treatment, and surgery is reserved as the last option for some patients with contraindication to endovascular therapy[3,5,7]. Anti-TB medication is the mainstay treatment of mediastinal TB. A large esophageal fistula secondary to TB could be treated by surgery or endoscopic clipping[2,8].
In this case report, although TB was suspected from the beginning, the presence of acute upper GI bleeding made it challenging to determine its source and treat it. Endoscopy and bronchoscopy – the examinations of choice for upper GI bleeding and suspected tracheoesophageal fistula – failed to identify the source. Chest CT with IV contrast and conventional angiography followed by coil embolization were of great value for diagnosis and treatment of such a rare condition. We believe that TB is a primary disease that involves the lung and then extends to the mediastinum and leads to esophageal fistula and mediastinal bronchial artery aneurysm formation. This rare presentation of acute upper GI bleeding is most likely due to mediastinal bronchial artery aneurysm that caused bleeding and drained into the esophagus by the esophagomediastinal fistula.
We successfully treated a patient who presented with acute upper GI bleeding due to tuberculous esophagomediastinal fistula and mediastinal bronchial artery aneurysm using transcatheter coil embolization.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Saudi Arabia
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lu XL, Nagliati C S-Editor: Yan JP L-Editor: A E-Editor: Ma YJ
| 1. | Kim D, Kim J, Lee D, Chang HS, Joh H, Koh WJ, Lee JH. Multidrug-Resistant Tuberculous Mediastinal Lymphadenitis, with an Esophagomediastinal Fistula, Mimicking an Esophageal Submucosal Tumor. Clin Endosc. 2016;49:564-569. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Devarbhavi HC, Alvares JF, Radhikadevi M. Esophageal tuberculosis associated with esophagotracheal or esophagomediastinal fistula: Report of 10 cases. Gastrointest Endosc. 2003;57:588-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 62] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Fukunaga A, Okushiba S, Ohno K, Kitashiro S, Kawarada Y, Shitinohe T, Kondo S, Katoh H. Mediastinal bronchial artery aneurysm with hematemesis. Dis Esophagus. 2003;16:328-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Sakuma K, Takase K, Saito H, Zuguchi M, Tabayashi K. Bronchial artery aneurysm treated with percutaneous transluminal coil embolization. Jpn J Thorac Cardiovasc Surg. 2001;49:330-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Nakada T, Takahashi K, Ito E, Fukushima S, Yamamoto S, Takahashi N, Toya N, Akiba T, Morikawa T, Ohki T. A case of bronchial artery aneurysm with an esophageal fistula as an extremely rare complication after bronchial arterial embolization. J Thorac Dis. 2018;10:E476-E480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Lü PH, Wang LF, Su YS, Lee DH, Wang SX, Sun L, Geng SP, Huang WN. Endovascular therapy of bronchial artery aneurysm: Five cases with six aneurysms. Cardiovasc Intervent Radiol. 2011;34:508-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | San Norberto EM, Urbano García J, Montes JM, Vaquero C. Endovascular treatment of bronchial aneurysms. J Thorac Cardiovasc Surg. 2018;156:e109-e117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Sayeed A, Alqurashi EH, Alzanbagi AB, Ghaleb NAB. Tuberculosis presenting as broncho-oesophageal fistula in a young healthy man. BMJ Case Rep. 2017;2017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |