Published online Mar 28, 2019. doi: 10.3748/wjg.v25.i12.1457
Peer-review started: January 23, 2019
First decision: February 21, 2019
Revised: February 28, 2019
Accepted: March 11, 2019
Article in press: March 12, 2019
Published online: March 28, 2019
Processing time: 64 Days and 23.5 Hours
Esophageal diverticula are rare conditions that cause esophageal symptoms, such as dysphagia, regurgitation, and chest pain. They are classified according to their location and characteristic pathophysiology into three types: epiphrenic diverticulum, Zenker’s diverticulum, and Rokitansky diverticulum. The former two disorders take the form of protrusions, and symptomatic cases require interventional treatment. However, the esophageal anatomy presents distinct challenges to surgical resection of the diverticulum, particularly when it is located closer to the oral orifice. Since the condition itself is not malignant, minimally invasive endoscopic approaches have been developed with a focus on alleviation of symptoms. Several types of endoscopic devices and techniques are currently employed, including peroral endoscopic myotomy (POEM). However, the use of minimally invasive endoscopic approaches, like POEM, has allowed the development of new disorder called iatrogenic esophageal diverticula. In this paper, we review the pathophysiology of each type of diverticulum and the current state-of-the-art treatment based on our experience.
Core tip: Esophageal diverticula are rare but can cause difficulty in swallowing. They are classified into three major categories according to their pathophysiology and location: epiphrenic diverticulum, Zenker’s diverticulum, and Rokitansky diverticulum, with the former two presenting as clinically significant protrusions and symptomatic cases requiring interventional treatment. However, the esophageal anatomy presents challenges to surgical resection, and the condition itself is not malignant. Therefore, minimally invasive endoscopic treatments have been developed. In this paper, we review the pathophysiology and up-to-date treatment of each diverticulum.
- Citation: Sato H, Takeuchi M, Hashimoto S, Mizuno KI, Furukawa K, Sato A, Yokoyama J, Terai S. Esophageal diverticulum: New perspectives in the era of minimally invasive endoscopic treatment. World J Gastroenterol 2019; 25(12): 1457-1464
- URL: https://www.wjgnet.com/1007-9327/full/v25/i12/1457.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i12.1457
Esophageal diverticula comprise a rare condition that causes dysphagia, regurgitation, and chest pain as they progress. The pathophysiology of the diverticula varies according to their location in the esophagus (i.e., epiphrenic, Zenker’s, and Rokitansky).
Interventional treatment should be considered for symptomatic cases. Although surgical resection of the diverticulum has traditionally been considered to be the only curative option, esophageal anatomy presents several challenges to surgery, particularly when the diverticulum is near the oral orifice. Some of the issues associated with surgery include the extensive invasiveness and risk of adverse events. Esophageal diverticula themselves are not malignant; hence, minimally invasive endoscopic treatment that avoids surgery is preferred. The primary purpose of interventions for esophageal diverticulum is to alleviate the patients’ symptoms and improve their quality of life; therefore, we do not have to singularly focus on achieving complete excision of the diverticulum. However, the development of minimally invasive endoscopic approaches for the esophagus has led to a new kind of disorder called iatrogenic diverticula. Caution must be exercised to avoid the incidence of such diverticula.
In this paper, we review the pathophysiology and up-to-date treatment options for esophageal diverticulum based on our experience.
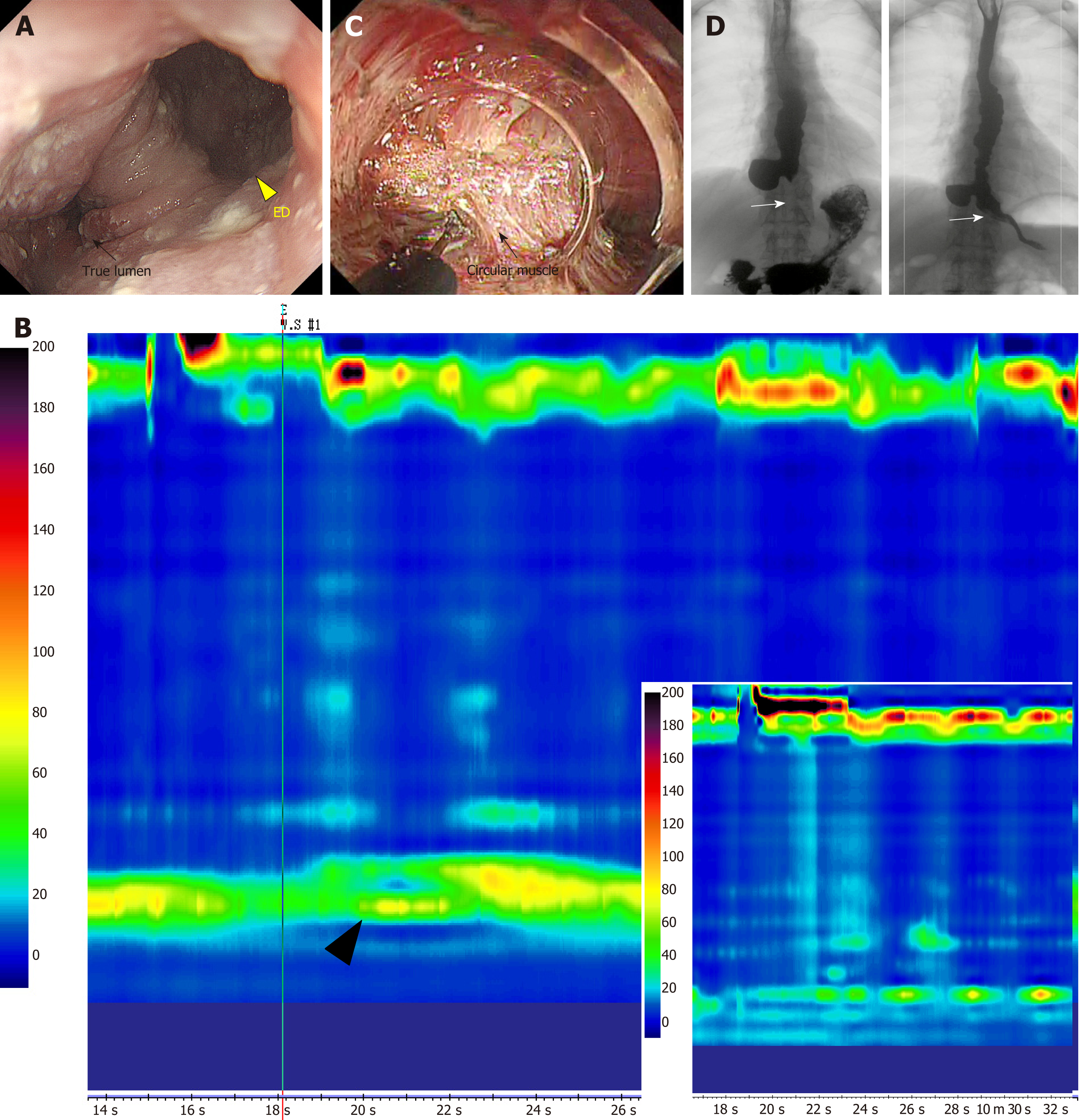
Epiphrenic diverticula are pulsion-type diverticula that are usually located in the distal esophagus (Figure 1A and D). Histologically, they appear as pseudodiverticula lacking a muscle layer. Their pathogenesis is considered to be secondary to esophageal motility disorders and is associated with congenital weakness of the esophageal wall[1].
Recent studies have reported that more than 75% of epiphrenic diverticula occur concomitantly with esophageal motility disorders[2-8]. Therefore, evaluation of esophageal motility using high resolution manometry (HRM) is recommended before deciding on the intervention (Figure 1B)[9,10]. The right esophageal wall is more susceptible to epiphrenic diverticula[2,11], although the reason for this is still unclear. In contrast, spontaneous esophageal rupture tends to occur through the left wall (Table 1)[12].
| Diverticulum | Characteristics | Treatment |
| Epiphrenic diverticulum | The right wall of the distal esophagus is the most common site. Pulsion-type pseudodiverticulum. Generally detected after middle-age. No difference in incidence between the sexes. More than 75% of cases occur concomitantly with esophageal motility disorders. Symptoms: dysphagia, regurgitation, chest pain | Surgical treatment; Removal of the diverticulum with myotomy through the LES and fundoplication |
| Endoscopic treatment (flexible endoscope); s-POEM (myotomy through the LES); D-POEM (POEM diverticulectomy) | ||
| Zenker’s diverticulum | Arises from Killian’s triangle in the pharyngoesophagus. Pulsion-type pseudodiverticulum. Incidence: 2 per 100000 person-years, Prevalence: 0.01%-0.11% (United States, Europe > Asia)[42,43]. Common in the 7th-8th decade, male predominance[44]. Symptoms: dysphagia, regurgitation | Surgical treatment; Transcervical diverticulectomy, diverticuloplexy, or diverticular inversion. |
| Diverticulectomy with rigid endoscope; Harmonic scalpel, CO2 laser, endostapler, etc. | ||
| Diverticulectomy with flexible endoscope | ||
| Clutch Cutter, Stag Beetle knife, D-POEM, etc. |
The classical indications for surgery are continued growth of the diverticulum, the presence of symptoms, and concomitant malignancy in the diverticulum.
The laparoscopic approach is the less invasive surgical choice. As described above, associated motility disorders of the esophagus are found in most cases; therefore, a myotomy through the lower esophageal sphincter (LES) and an anti-reflux procedure should be added to treat the primary problem and avoid gastroesophageal reflux[13]. The long-term outcomes of surgical management are satisfactory[7,14,15]. However, Michael et al’s[16] study using a United States nationally representative database showed that the mortality rate associated with surgery for non-Zenker’s diverticulum (ZD) was 1.6% and that the most common complication was air leakage (3.1%). Furthermore, the risk of postoperative morbidity was greater after thoracotomy than after laparoscopy (odds ratio: 7.45).
In 2010, Inoue et al[17] first reported a case series of achalasia successfully treated with peroral endoscopic myotomy (POEM). It is an innovative approach for endoscopic myotomy of the esophageal muscle layer through the mouth. POEM has been gaining attention due to its minimally invasive nature and equivalent efficacy for achalasia compared to that of conventional surgical approaches, such as Heller’s myotomy[18,19]. We previously reported the first case of epiphrenic diverticulum successfully treated by salvage POEM (s-POEM)[20]. In s-POEM, endoscopic myotomy of the side opposite to the diverticulum was performed longitudinally, from the oral to the gastric terminus, and a thick muscle layer, including the LES, was completely dissected (Figure 1C). The patient’s severe dysphagia and regurgitation subsequently resolved. Follow-up endoscopy showed no food remnants in the diverticulum or esophageal lumen, and a post-barium swallow test indicated smooth passage through the esophago-gastric junction (Figure 1D). One interesting aspect in this case was that the HRM showed no specific esophageal abnormalities, although the patient was suspected to have an esophageal motility disorder-related diverticulum based on the findings of the endoscopic and barium swallow examinations. Similarly, patients with disparate manometry (normal), and barium swallow (corkscrew esophagus) findings have been previously reported[2]. Based on this successful experience, we proceeded to perform s-POEM for cases, such as epiphrenic diverticulum with achalasia and esophagogastric junction outflow obstruction[21], which were, without exception, effective in ameliorating symptoms and clearing remnant food from the diverticulum (Figure 1). Therefore, s-POEM could be a promising treatment alternative for epiphrenic diverticulum[22,23]. Diverticular peroral endoscopic myotomy (D-POEM), which is a septotomy of the diverticulum using the POEM technique, has also been reported to be effective[24]. The procedure involves exposing the septal wall after creation of a submucosal tunnel.
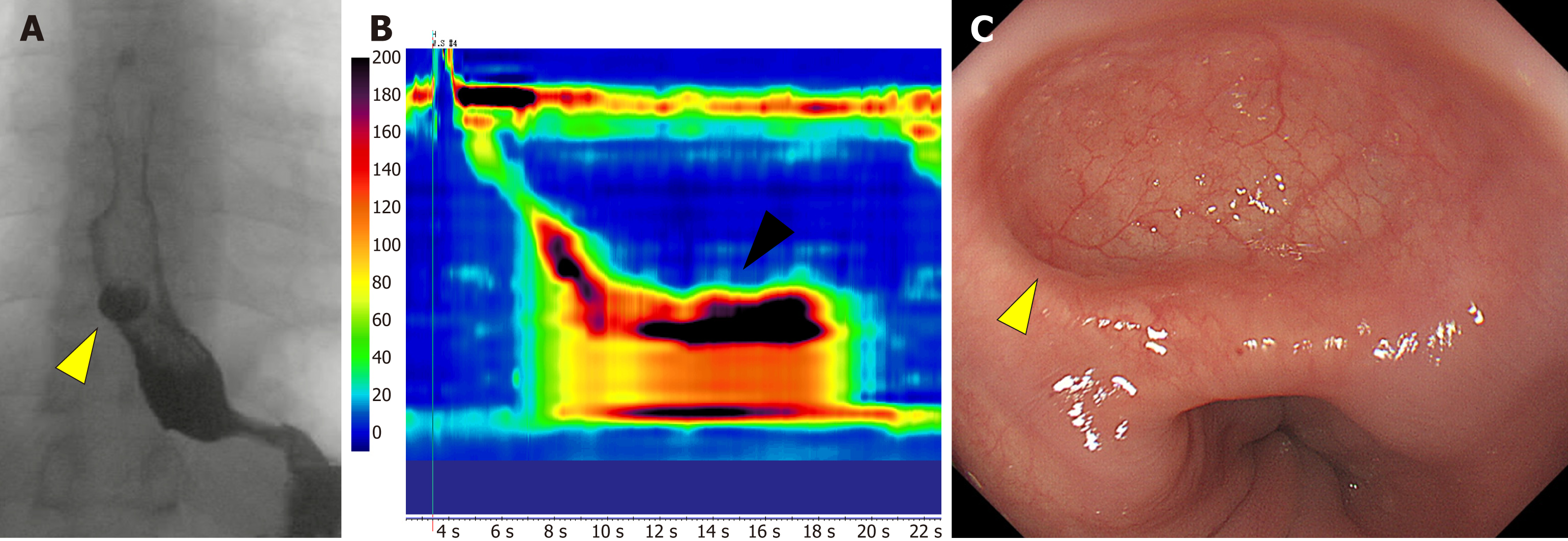
The development and adoption of minimally invasive endoscopic treatments, such as POEM have led to reports of iatrogenic diverticulum (Figure 2A)[25,26], although it has not been recognized as a major problem in POEM[27,28]. Based on our experience with epiphrenic diverticula, the right wall of the distal esophagus is anatomically vulnerable and predisposed to diverticulum formation. Furthermore, remnant abnormal contractions of the esophageal body post-POEM (Figure 2B) exert significant pressure on the weak wall of the distal esophagus. Thus, clinicians need to take extra care when using POEM in esophageal motility disorders, such as jackhammer esophagus (hypercontractile esophagus) or type II (with pan-esophageal pressurization) and III (with spastic pressurization in the distal esophagus) achalasia. A pre-procedural HRM examination is essential to the decision-making process. A long myotomy that targets the esophageal body contraction as well, or a posterior myotomy that avoids the weak segments of the esophagus may prevent post-POEM diverticulum formation (Figure 2C).
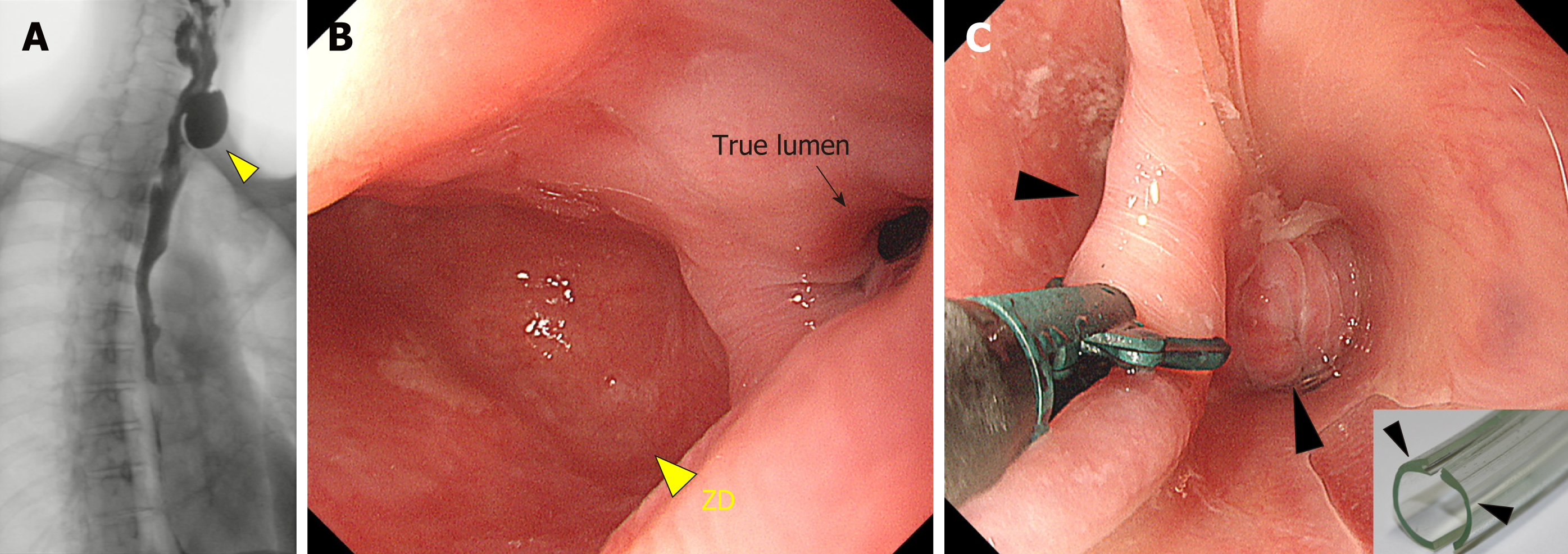
ZD is also called pharyngoesophageal diverticulum or pharyngeal pouch (Figure 3A and B). As the synonyms suggest, ZD is an acquired pulsion-type pseudo-diverticulum in the pharyngoesophagus. Increased intraluminal pressure leads to posterior outpouching between two strong pharyngoesophageal muscles: the cricopharyngeus and inferior pharyngeal constrictor. This area has a decreased hypopharyngeal wall tone and increased intraluminal pressure can present with posterior pouch formation. The location with the anatomical weakness is known as the Killian’s triangle[29].
ZD is a rare condition with a yearly incidence rate of 2 per 100000 adults. Geographical variation in the incidence has been observed with a significantly lower incidence in Asian than in Western countries[30]. It occurs predominantly in men, and is most common in the seventh and eight decades of life (Table 1)[31].
Several surgical options are available for the management of ZD. Diverticulectomy, diverticulopexy, diverticular inversion with or without myotomy, and myotomy alone have been reported[32]. Conventionally, an open left cervical incision under general anesthesia has been employed. However, as mentioned above, symptoms of ZD generally appear in the seventh and- eight decades of life, debilitating the patients and leading to increased surgical morbidity and mortality rates. Thus, minimally invasive endoscopic approaches have gained popularity in the recent years[33].
Endoscopic treatment generally involves diverticulectomy, using several devices originally developed for endoscopic submucosal dissection, and the POEM technique. The septal wall is dissected using a rigid endoscope with a CO2 laser or endostapler, while a flexible endoscope uses devices such as a stag beetle knife and clutch cutter knife. Two approaches to the dissection have been reported: direct incision of the septal wall along with the mucosa using the rigid or flexible endoscope[34] (Figure 3C), or myotomy of the exposed septal wall using the POEM technique with a flexible endoscope (D-POEM)[33]. Yuan et al[32] reviewed their entire experience from 1990 to 2011 and reported that the overall morbidity and mortality rates for the endoscopic approach were 8.7% and 0.2%, respectively, while they were 10.5% and 0.6%, respectively for open surgery. Studies on endoscopic treatment and open surgery for ZD performed from 1990 to 2002 also found that the endoscopic stapling technique was associated with lower major complications and mortality rates than open surgery (2.6% vs 11.8% and 0.3% vs 1.6%, respectively). It is understandable that the endoscopic technique carries a lesser risk of nerve injury and wound infection due to the minimally invasive nature of the endoluminal approach[35]. In addition, the hospital costs for endoscopic treatment are slightly lower than those for open surgery[36]. The recurrence rate varies from 0% to 35%[37-39].
Classically, diverticula of the middle esophagus were classified as Rokitansky diverticula, which generally occur in the thoracic esophagus. They are formed by cicatricial contraction due to a chronic inflammatory and fibrotic state that draws the wall of the esophagus outward; therefore, they involve the entire wall of the esophagus (true diverticulum). The apex of the pouch is generally located at a higher point than its entry point; therefore, it rarely attains an appreciable size or produces any symptoms. Their association with pulmonary tuberculosis is well characterized[40,41]. Cases of uncontrolled pulmonary tuberculosis are rare in the current era; therefore, Rokitansky diverticula presenting with clinical problems are even rarer.
Pulsion-type diverticula in the middle esophagus should be treated similarly to epiphrenic diverticula.
At present, the relative proportion of pulsion-type esophageal diverticula (epiphrenic and ZD) is increasing, while that of the traction-type (Rokitansky) is decreasing. Minimally invasive endoscopic treatment is indicated for pulsion-type diverticula and is being increasingly adopted owing to lower complication rates and equivalent efficacy to surgery. However, no randomized controlled trials comparing the difference between endoscopic treatment and surgery, or among the different endoscopic techniques have been performed. Furthermore, such studies of long-term follow-up results, including esophageal motility outcomes, are required to decide the best intervention modality for esophageal diverticulum. Another issue is the risk of esophageal carcinoma in the remnant diverticulum. Although the absolute risk of esophageal carcinoma is rather low, surveillance endoscopy is necessary after treatment. Minimally invasive endoscopic treatment should be performed after careful consideration of its advantages and drawbacks.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cicala M, Di Mitri R S-Editor: Ma RY L-Editor: A E-Editor: Song H
| 1. | Soares R, Herbella FA, Prachand VN, Ferguson MK, Patti MG. Epiphrenic diverticulum of the esophagus. From pathophysiology to treatment. J Gastrointest Surg. 2010;14:2009-2015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 2. | Tedesco P, Fisichella PM, Way LW, Patti MG. Cause and treatment of epiphrenic diverticula. Am J Surg. 2005;190:891-894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 85] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 3. | Nehra D, Lord RV, DeMeester TR, Theisen J, Peters JH, Crookes PF, Bremner CG. Physiologic basis for the treatment of epiphrenic diverticulum. Ann Surg. 2002;235:346-354. [PubMed] |
| 4. | Melman L, Quinlan J, Robertson B, Brunt LM, Halpin VJ, Eagon JC, Frisella MM, Matthews BD. Esophageal manometric characteristics and outcomes for laparoscopic esophageal diverticulectomy, myotomy, and partial fundoplication for epiphrenic diverticula. Surg Endosc. 2009;23:1337-1341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 60] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Del Genio A, Rossetti G, Maffetton V, Renzi A, Brusciano L, Limongelli P, Cuttitta D, Russo G, Del Genio G. Laparoscopic approach in the treatment of epiphrenic diverticula: long-term results. Surg Endosc. 2004;18:741-745. [PubMed] |
| 6. | Fernando HC, Luketich JD, Samphire J, Alvelo-Rivera M, Christie NA, Buenaventura PO, Landreneau RJ. Minimally invasive operation for esophageal diverticula. Ann Thorac Surg. 2005;80:2076-2080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 82] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 7. | Varghese TK, Marshall B, Chang AC, Pickens A, Lau CL, Orringer MB. Surgical treatment of epiphrenic diverticula: a 30-year experience. Ann Thorac Surg. 2007;84:1801-1809; discussion 1801-1809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 57] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 8. | D'Journo XB, Ferraro P, Martin J, Chen LQ, Duranceau A. Lower oesophageal sphincter dysfunction is part of the functional abnormality in epiphrenic diverticulum. Br J Surg. 2009;96:892-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Bredenoord AJ, Fox M, Kahrilas PJ, Pandolfino JE, Schwizer W, Smout AJ; International High Resolution Manometry Working Group. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24 Suppl 1:57-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 608] [Cited by in RCA: 607] [Article Influence: 46.7] [Reference Citation Analysis (0)] |
| 10. | Sato H, Takahashi K, Mizuno KI, Hashimoto S, Yokoyama J, Hasegawa G, Terai S. Esophageal motility disorders: new perspectives from high-resolution manometry and histopathology. J Gastroenterol. 2018;53:484-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 11. | Fasano NC, Levine MS, Rubesin SE, Redfern RO, Laufer I. Epiphrenic diverticulum: clinical and radiographic findings in 27 patients. Dysphagia. 2003;18:9-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 39] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | de Schipper JP, Pull ter Gunne AF, Oostvogel HJ, van Laarhoven CJ. Spontaneous rupture of the oesophagus: Boerhaave's syndrome in 2008. Literature review and treatment algorithm. Dig Surg. 2009;26:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 105] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 13. | Klaus A, Hinder RA, Swain J, Achem SR. Management of epiphrenic diverticula. J Gastrointest Surg. 2003;7:906-911. [PubMed] |
| 14. | Rosati R, Fumagalli U, Elmore U, de Pascale S, Massaron S, Peracchia A. Long-term results of minimally invasive surgery for symptomatic epiphrenic diverticulum. Am J Surg. 2011;201:132-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Brandeis AE, Singhal S, Lee TH, Mittal SK. Surgical management of epiphrenic diverticulum: A single-center experience and brief review of literature. Am J Surg. 2018;216:280-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Onwugbufor MT, Obirieze AC, Ortega G, Allen D, Cornwell EE, Fullum TM. Surgical management of esophageal diverticulum: a review of the Nationwide Inpatient Sample database. J Surg Res. 2013;184:120-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1168] [Cited by in RCA: 1235] [Article Influence: 82.3] [Reference Citation Analysis (1)] |
| 18. | Inoue H, Sato H, Ikeda H, Onimaru M, Sato C, Minami H, Yokomichi H, Kobayashi Y, Grimes KL, Kudo SE. Per-Oral Endoscopic Myotomy: A Series of 500 Patients. J Am Coll Surg. 2015;221:256-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 349] [Article Influence: 34.9] [Reference Citation Analysis (0)] |
| 19. | Inoue H, Shiwaku H, Iwakiri K, Onimaru M, Kobayashi Y, Minami H, Sato H, Kitano S, Iwakiri R, Omura N, Murakami K, Fukami N, Fujimoto K, Tajiri H. Clinical practice guidelines for peroral endoscopic myotomy. Dig Endosc. 2018;30:563-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 126] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 20. | Sato H, Sato Y, Takeuchi M, Takahashi K, Takeda SR, Inoue H, Kobayashi M. Salvage peroral endoscopic myotomy for esophageal diverticulum. Endoscopy. 2015;47 Suppl 1 UCTN:E14-E15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Sato H, Sato Y, Hashimoto S, Mizuno K, Nakajima N, Terai S. Gastrointestinal: Salvage peroral endoscopic myotomy for outflow obstruction with growing esophageal diverticulum. J Gastroenterol Hepatol. 2016;31:1237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Otani K, Tanaka S, Kawara F, Fujikawa J, Sawada A, Uemura R, Tanigawa T, Watanabe T, Azuma T, Fujiwara Y. Distal esophageal spasm with multiple esophageal diverticula successfully treated by peroral endoscopic myotomy. Clin J Gastroenterol. 2017;10:442-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Demeter M, Bánovčin P, Ďuriček M, Kunda R, Hyrdel R. Peroral endoscopic myotomy in achalasia and large epiphrenic diverticulum. Dig Endosc. 2018;30:260-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 24. | Yang J, Zeng X, Yuan X, Chang K, Sanaei O, Fayad L, Kumbhari V, Singh V, Kalloo AN, Hu B, Khashab MA. An international study on the use of peroral endoscopic myotomy (POEM) in the management of esophageal diverticula: the first multicenter D-POEM experience. Endoscopy. 2019;51:346-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 81] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 25. | Sato H, Takahashi K, Takeuchi M, Sato Y, Hashimoto S, Mizuno K, Terai S. Epiphrenic diverticulum of the esophagus after peroral endoscopic myotomy. Endoscopy. 2015;47 Suppl 1 UCTN:E509-E510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Badillo R, Francis D, DeVault K. Formation of large esophageal diverticulum after peroral endoscopic myotomy. Gastrointest Endosc. 2015;82:962; discussion 963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Akintoye E, Kumar N, Obaitan I, Alayo QA, Thompson CC. Peroral endoscopic myotomy: a meta-analysis. Endoscopy. 2016;48:1059-1068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 173] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 28. | Talukdar R, Inoue H, Nageshwar Reddy D. Efficacy of peroral endoscopic myotomy (POEM) in the treatment of achalasia: a systematic review and meta-analysis. Surg Endosc. 2015;29:3030-3046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 121] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 29. | Law R, Katzka DA, Baron TH. Zenker's Diverticulum. Clin Gastroenterol Hepatol. 2014;12:1773-1782; quiz e111-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 90] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 30. | Beard K, Swanström LL. Zenker's diverticulum: flexible versus rigid repair. J Thorac Dis. 2017;9:S154-S162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 31. | Watemberg S, Landau O, Avrahami R. Zenker's diverticulum: reappraisal. Am J Gastroenterol. 1996;91:1494-1498. [PubMed] |
| 32. | Yuan Y, Zhao YF, Hu Y, Chen LQ. Surgical treatment of Zenker's diverticulum. Dig Surg. 2013;30:207-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 104] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 33. | Ishaq S, Sultan H, Siau K, Kuwai T, Mulder CJ, Neumann H. New and emerging techniques for endoscopic treatment of Zenker's diverticulum: State-of-the-art review. Dig Endosc. 2018;30:449-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (1)] |
| 34. | Sato H, Takeuchi M, Terai S. Gastrointestinal: Endoscopic diverticulectomy for the treatment of Zenker's diverticulum with a unique "tip": A first case report in Japan. J Gastroenterol Hepatol. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 35. | Chang CY, Payyapilli RJ, Scher RL. Endoscopic staple diverticulostomy for Zenker's diverticulum: review of literature and experience in 159 consecutive cases. Laryngoscope. 2003;113:957-965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 115] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 36. | Smith SR, Genden EM, Urken ML. Endoscopic stapling technique for the treatment of Zenker diverticulum vs standard open-neck technique: a direct comparison and charge analysis. Arch Otolaryngol Head Neck Surg. 2002;128:141-144. [PubMed] |
| 37. | Baldwin DL, Toma AG. Endoscopic stapled diverticulotomy: a real advance in the treatment of hypopharyngeal diverticulum. Clin Otolaryngol Allied Sci. 1998;23:244-247. [PubMed] |
| 38. | Counter PR, Hilton ML, Baldwin DL. Long-term follow-up of endoscopic stapled diverticulotomy. Ann R Coll Surg Engl. 2002;84:89-92. [PubMed] |
| 39. | Vogelsang A, Preiss C, Neuhaus H, Schumacher B. Endotherapy of Zenker's diverticulum using the needle-knife technique: long-term follow-up. Endoscopy. 2007;39:131-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 69] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 40. | Charles T, Sturgeon MD. Esophageal diverticula. JAMA. 1929;92:379-385. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 41. | SCHICK A, YESNER R. Traction diverticulum of esophagus with exsanguination: report of a case. Ann Intern Med. 1953;39:345-349. [PubMed] |
| 42. | Ferreira LE, Simmons DT, Baron TH. Zenker's diverticula: pathophysiology, clinical presentation, and flexible endoscopic management. Dis Esophagus. 2008;21:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 136] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 43. | Siddiq MA, Sood S, Strachan D. Pharyngeal pouch (Zenker's diverticulum). Postgrad Med J. 2001;77:506-511. [PubMed] |
| 44. | Bizzotto A, Iacopini F, Landi R, Costamagna G. Zenker's diverticulum: exploring treatment options. Acta Otorhinolaryngol Ital. 2013;33:219-229. [PubMed] |