Published online May 14, 2018. doi: 10.3748/wjg.v24.i18.1978
Peer-review started: April 8, 2018
First decision: April 21, 2018
Revised: April 26, 2018
Accepted: May 6, 2018
Article in press: May 6, 2018
Published online: May 14, 2018
Processing time: 34 Days and 18.4 Hours
The major symptoms of advanced hepatopancreatic-biliary cancer are biliary obstruction, pain and gastric outlet obstruction (GOO). For obstructive jaundice, surgical treatment should de consider in recurrent stent complications. The role of surgery for pain relief is marginal nowadays. On the last, there is no consensus for treatment of malignant GOO. Endoscopic duodenal stents are associated with shorter length of stay and faster relief to oral intake with more recurrent symptoms. Surgical gastrojejunostomy shows better long-term results and lower re-intervention rates, but there are limited data about laparoscopic approach. We performed a systematic review of the literature, according PRISMA guidelines, to search for articles on laparoscopic gastrojejunostomy for malignant GOO treatment. We also report our personal series, from 2009 to 2017. A review of the literature suggests that there is no standardized surgical technique either standardized outcomes to report. Most of the studies are case series, so level of evidence is low. Decision-making must consider medical condition, nutritional status, quality of life and life expectancy. Evaluation of the patient and multidisciplinary expertise are required to select appropriate approach. Given the limited studies and the difficulty to perform prospective controlled trials, no study can answer all the complexities of malignant GOO and more outcome data is needed.
Core tip: Both non-operative endoscopic approach and surgical treatment are available for palliative treatment of gastric outlet obstruction due to advanced hepatopancreatic-biliary cancer. Stent is usually preferred in patients with poor general condition or short life expectancy. Laparoscopic gastrojejunostomy is a feasible, safe and efficient technical option. Given the limited studies, we performed a systematic review of laparoscopic gastrojejunostomy in patients with advanced hepatopancreatic-biliary malignancy. Clinical prospective trials comparing different approaches with adequate sample size are warranted.
- Citation: Manuel-Vázquez A, Latorre-Fragua R, Ramiro-Pérez C, López-Marcano A, De la Plaza-Llamas R, Ramia JM. Laparoscopic gastrojejunostomy for gastric outlet obstruction in patients with unresectable hepatopancreatobiliary cancers: A personal series and systematic review of the literature. World J Gastroenterol 2018; 24(18): 1978-1988
- URL: https://www.wjgnet.com/1007-9327/full/v24/i18/1978.htm
- DOI: https://dx.doi.org/10.3748/wjg.v24.i18.1978
Obstructive jaundice, gastric outlet obstruction (GOO) and tumor-associated pain are the major symptoms of advanced hepatobiliary-pancreatic (HPB) cancer. Usually these cancers are not resected because of infiltration of local structures or disseminated disease. Today, these complications can be managed with endoscopic stenting and percutaneous treatment, which have lower rates of associated morbidity; thus, surgical strategies have decreased.
Around 70% of cases of advanced HPB cancer present obstructive jaundice[1,2], which is the most common symptom[3-5] To resolve jaundice in unresectable or metastatic patients, endoscopic or percutaneous biliary stent is accepted as the gold standard[6]. Surgical treatment of biliary obstruction should be considered in persistent stent-problems, such as recurrent cholangitis or recurrent obstructive jaundice[6]; however laparoscopic surgery for biliary bypass is not a standard procedure[1,7]. Furthermore, the role of surgical pain relief in these patients seems to be marginal nowadays[6].
Finally, there is no consensus about the role of surgery in the management of malignant GOO. This clinical syndrome is characterized by abdominal pain, weight loss, nauseas and vomiting, due to the mechanical obstruction, and may be caused by gastric, duodenal, HPB or extraluminal diseases; therefore, the treatment depends on underlying cause[8]. In recent decades, 50%-80% of cases have been attributed to malignancy. GOO may develop in up to 20% of patients with advanced HPB disease[4,9-14]. The aim of GOO treatment is to reestablish oral intake by restoring gastrointestinal continuity.
Decision-making with regard to palliative treatment of malignant GOO due to advanced HPB cancer has become more complex in recent years. Traditionally, open gastrojejunostomy (OGJ) was the only option[11,15]. In the 1990s, endoscopic duodenal stents were introduced. In the last few years, laparoscopic gastrojejunostomy (LGJ) has emerged as a feasible and safe option that offers improved morbidity and mortality rates compared with the open surgical approach[3]. As can be seen, then, several options are available and there is no current gold standard[9].
The literature on GOO focus on gastric disease and mixes different causes with different prognoses. This means that, the level of evidence in patients with HPB malignant diseases is low and data on the laparoscopic approach to GJ for malignant GOO due to advanced HPB cancers are limited.
Our aim in this paper is to review various aspects of the management of malignant GOO due to advanced HPB cancer. Focusing on the laparoscopic approach for gastroenteroanastomosis, we perform a systematic review of the literature and a retrospective review of our personal series of laparoscopic GJ for the treatment of malignant GOO due to advanced HPB cancer.
A cancer may be found to be unresectable during preoperative staging examinations. Only some 20% of HPB neoplasms are found to be resectable[16-18]. Despite the indications of preoperative staging radiological and endoscopic images, between 8% and 33% of patients are found to be unresectable on laparotomy[19]. This means that surgeons may be encounter this situation intraoperatively and must decide whether to perform prophylactic GJ. This decision should be based on the probability of GOO; between 10%-15% of patients develop GOO at a later stage[3,11,20].
Gurusamy et al[2] report no differences in overall survival, postoperative morbidity and mortality, quality of life (QOL) or length of stay (LOS). This Cochrane review included two RCTs assessing the role of prophylactic GJ in unresectable periampullary cancer[21,22]. The authors reported a long-term GOO incidence of 27.8% in patients with advanced HPB cancer who did not undergo prophylactic GJ and concluded that prophylactic GJ may not be necessary in all patients with advanced HPB malignancy undergoing laparotomy[2].
Physicians may also find a patient with uncontrolled vomiting and a diagnosis of advanced HPB malignancy. Palliative treatment should be offered to relieve the symptoms of GOO and ultimately to improve patient QOL. Palliative treatment is mandatory when the vomiting is uncontrolled.
Traditionally, OGJ was the only option for the treatment of malignant GOO[11,13,15]. Since 1992, several studies have described the use, safety and efficacy of self-expandable metallic stents (SEMS)[10,23-33]. Thus, several options are currently available and there is no established gold standard.
The literature on palliative GJ show good functional outcomes and symptoms relief in up to 70% of patients and reduced re-intervention rates, but it is associated with postoperative complications, such as delayed gastric emptying (DGE)[8,12,14,34,35]. For its part, palliative endoscopic treatment is a well-established procedure today and is considered a valid alternative for avoiding surgery. The endoscopic approach is associated with shorter length of stay (LOS), faster initial relief and shorter time to oral intake, but also with greater symptom recurrences and risk of stent migration[8,12-14,36-39].
The current literature mixes together different etiologies, and even includes benign causes such as superior mesenteric artery syndrome, peptic ulcer stenosis, chronic pancreatitis or annular pancreas, different grades of GOO, and prophylactic and palliative treatments[40-44]. Kohan et al[45] report the results of surgical palliative treatment for pancreatic cancer; but they mixed elective bypass for the treatment of symptomatic malignant GOO together with and prophylactic GJ in advanced HPB cancer patients undergoing surgery for biliary obstruction.
Table 1 shows the results of previous systematic reviews and meta-analysis comparing endoscopic duodenal stent vs GJ for the treatment of malignant GOO, including both gastric and advanced HPB cancers and other metastastic cancers. Minata et al[8], Nagaraja et al[13] and Ly et al[38] have demonstrated shorter LOS and faster oral intake with endoscopic palliative treatment, but lower re-intervention rates with OGJ. No differences in survival or major complications were found. Nagaraja et al[13] concluded that the endoscopic approach minimizes pain, hospitalization, and physiologic stress to the patient, which are the main goals of palliation.
| Ref. | Type of study | GJ studies | Surgery | Endoscopic stent | No differences |
| Minata et al[8], 2016 | Systematic review | LGJ (Mehta 2006, Jeurnink 2010) OGJ (Jeurnink 2010, Fiori 2013) | Lower re-intervention rate | Less invasive COVERED: Higher migration UNCOVERED: Higher obstruction | Technical success Complications |
| Nagaraja et al[13], 2014 | Meta-analisis | Laparoscopic GJ (Mittal 2004, Mehta 2006, Jeurnink 2007, Jeurnink 2010) | Shorter LOS | Technical and clinical outcomes | |
| Ly et al[38], 2010 | Systematic review | Open GJ (Jeurnink 2007, El-Shabrawi 2006, Mehta 2006, Espinal 2006, Mejia 2006, del Piano 2005, Maetani 2005, Fiori 2004, Mittal 2004, Maetani 2004, Johnsson 2004, Wong 2002, Yim 2001) Laparoscopic GJ (Jeurnink 2007, Mehta 2006, Mittal 2004) | More major medical complications | More likely to tolerate an oral intake More likely to tolerate an oral diet earlier Shorter LOS | Survival 30 d-mortality Major complications |
Decisions regarding the best therapeutic strategy for individual patients with malignant GOO due to advanced HPB cancer should be based on the performance and medical condition, the extent of the cancer, the prognosis, their quality of life and expectancy, and the availability and likely success of each treatment option[36,46,47].
Depending on the medical condition, one of the main factors to consider is nutritional status; thus, hypoalbuminemia is considered as a risk factor for GJ whether the disease is benign or malignant[48]. Surgeons should correct this situation if surgical palliation is the aim and at least 1-2 wk of nutritional treatment should be considered in order to decrease the risk of postoperative complications[48]. According Sasaki et al[49], poor performance status should be considered as additional risk factor.
With regard to the extent of the cancer, the presence of carcinomatosis with ascites has been reported as an independent predictive factor for poor clinical success of stent placement, without any differences in stent patency[50].
The choice of palliative GJ or endoscopic enteral stent should consider the life expectancy of patients and the likelihood of recurrent GOO after stenting. As regards the prognosis of malignant disease, in the SUSTENT study, Jeurnink et al[12], concluded that palliative GJ is the treatment of choice in patients expected to live two months or longer, whereas stent is preferable for patients with a life expectancy below this figure. This conclusion is based on the finding that surgery was more effective than endoscopic stent after a follow-up of two months[12]. Recurrent obstruction due to tumor ingrowth into stent or stent migration has been reported in 17%-27% of patients with endoscopic stent[4,51]. Severe complications associated with stenting include bleeding and perforation and have been reported in 1.2% of cases[51]. Comparing stent types, migration rates are higher with covered stents than with uncovered ones; in contrast, uncovered stenting has higher obstruction rates[8,52,53]. In addition, some patients may suffer combined obstructive jaundice and GOO. There are several options for treatment, but biliary endoscopic stenting can pose a challenge if a duodenal stent is in place[54]; patients with stent for biliary obstruction who subsequently have an endoscopic enteral stent are at an increased risk of biliary stent dysfunction[55]. Another option is endoscopic double stenting, a combination of biliary and duodenal stent placement, where different approaches could make it possible[56].
Wilson et al[57] published the first report of LGJ in two patients with malignant GOO due to advanced HPB cancer. Today, LGJ is a feasible option, and presents improved morbidity and mortality rates compared with the open surgical approach[3].
In 2007, Siddiqui et al[58] designed a model for patients with malignant GOO and performed a decision analysis. They concluded that endoscopic enteral stent was a optimal strategy, associated with a 72% success rate and the lowest 1-mo mortality rate (2.1%), one of the drawbacks was recurrent duodenal obstruction, found in up to 25%. They reported a 69% success rate after LGJ (overall 1-mo mortality 2.5% and a cost increase of $10340), and 63% success after open GJ with higher 1-mo mortality (4.5%) and more expensive treatment (a cost increase of $12191)[58].
Given the limited number of controlled trials of the laparoscopic approach in palliative GJ[39,59,60], data available are insufficient to perform an analysis comparing LGJ with OGJ or endoscopic stent[38].
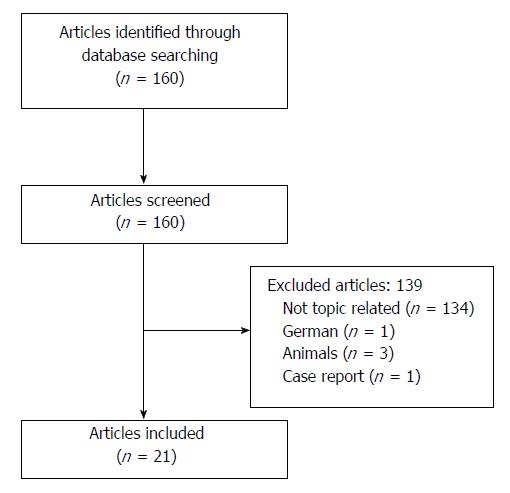
We therefore performed a systematic literature review, in accordance with the PRISMA guidelines, on patients with advanced HPB malignancy who had undergone laparoscopic palliative GJ up to February 2018. The search items were the following MESH terms: [(Gastric outlet obstruction) OR (Gastric Outlet Obstructions) OR (Obstruction, Gastric Outlet) OR (Obstructions, Gastric Outlet) OR (Outlet Obstruction, Gastric) OR (Outlet Obstructions, Gastric) OR (Duodenal obstruction) OR (Duodenal Obstructions) OR (Obstruction, Duodenal) OR (Obstructions, Duodenal)] AND [(Gastric bypass) OR (Bypass, Gastric) OR (Gastrojejunostomy) OR (Gastrojejunostomies) OR (Gastroenterostomy) OR (Gastroenterostomies)] AND [(Laparoscopy) OR (Laparoscopies) OR (Surgical Procedures, Laparoscopic) OR (Laparoscopic Surgical Procedure) OR (Procedure, Laparoscopic Surgical) OR (Procedures, Laparoscopic Surgical) OR (Surgery, Laparoscopic) OR (Laparoscopic Surgical Procedures) OR (Laparoscopic Surgery) OR (Laparoscopic Surgeries) OR (Surgeries, Laparoscopic) OR (Surgical Procedure, Laparoscopic)]. Eligibility criteria were any type of article that included patients with advanced HPB malignancy who had undergone laparoscopic palliative GJ, excluding case reports or reports of prophylactic GJ.
The articles were included or rejected based on the information in the title and summary, and in case of doubt, after reading the complete article.
Figure 1 presents a flowchart of systematic review of patients with advanced HPB malignancy who had undergone laparoscopic palliative GJ. The initial search yielded, 160 articles, but only 21 (13.12%) met the search criteria.
The outcomes and surgical techniques of LGJ for malignant GOO are displayed in Tables 2 and 3[3-5,9,15,37,39,57,60-72]. Most studies were case series (12/21)[5,9,15,57,61-64,66,69,72], five were cohort series[3,4,37,60,68], two case/control studies[70,71] and only two studies were randomized controlled trials (RCT)[39,67]. The studies included different etiologies for GOO, among them benign disease[66] and only nine publications recorded all patients with advanced HPB malignancy[4,5,9,61-65].The systematic review included 495 patients, of whom 55 (11.11%) had advanced HPB cancer and had undergone LGJ. There was a mix of associated treatments for biliary obstruction, including endoscopic stent (ES), percutaneous drainage (PD), and biliary bypass (choledochojejunostomy, CJ; cholecystojejunostomy, CCJ). The results displayed in Table 2, show that there are no standardized outcomes for reporting results after LGJ. Regarding the surgical technique (Table 3), most LGJ were antecolic-isoperistaltic stapler plus manual suture, but there was no standardized approach for LGJ.
| Ref. | n | Type of study | HPB Etiology | Biliary obstruction | Operating time | Perioperative morbidity | Time to initiate intake | Time to solid food | LOS | Duration of food intake | Comment |
| All HPB Malignancy | |||||||||||
| Jeurnink et al[60], 2007 | 95 | Cohort: GJ (42) vs duodenal stent (53) | GJ: All patients (laparoscopy: 10) | GJ: 17 previous treatment | ND | GJ: 4 major (hemorrhage, severe pain, cholangitis, respiratory failure); 13 minor (mild pain, wound infection, nausea and vomiting) | ND | GJ: 10.1 ± 4.8 d | GJ: 18d (4-55) | ND | |
| Hamade et al[4], 2005 | 21 | Cohort: laparoscopic GJ/CJ/GJ+CJ | All patients | 5 biliary bypass, 8 GJ+biliary bypass | gastric bypass 75 min, GJ+CJ 130 min | 1 pneumonia, 1 central line sepsis, 1 wound abscess | ND | ND | 4 d (1-14) | 9 patients untill death | Includes pre-treatment, profilactic and terapeutic GJ |
| Denley et al[9], 2005 | 18 | Case series: LGJ | All patients | ND | ND | 2 reconversions, 1 leak, 1 sepsis, 1 DGE | ND | ND | 6 (3-22) | 15 patients untill death | |
| Kazanjian et al[5], 2004 | 9 | Case series: LGJ | All patients | ND | 116 min (75-300) | 1 DGE, 1 Cholangitis | ND | 4 d (3-6) | 7 d (5-18) | ND | 4 patient previous stent |
| Alam et al[61], 2003 | 8 | Case series: LGJ | All patients | ND | 135 min | Pneumonia (1) | ND | 4 (2-7) | 7 (5-13) | 7 patients untill death | |
| Kuriansky et al[62], 2000 | 12 | Case series: LGJ+biliary bypass | All patients | 12 CCJ | 89.16 min (35-150) | 2 wound infection, 1 pneumonia, 2 DGE, 1 reintervention (bleeding) | ND | ND | 6.4 (5-17) | All patients untill death | |
| Casaccia et al[63], 1999 | 6 | Case series: LGJ | All patients | 4 ES. 2 Laparoscopic CCJ | 82 min (60-135) | 1 Bleeding (transfusion) | ND | ND | 4.5 (4-6) | ND | |
| Casaccia et al[64], 1998 | 5 | Case series: LGJ | All patients | 4 ES. 1 laparoscopic CCJ | ND | 1 Bleeding (transfusion) | ND | ND | 4 (4-6) | ND | |
| Rhodes et al[65], 1995 | 16 | Case series: laparoscopic CCJ ± GJ (5GJ, 3 both, 9CCJ) | All patients | ND | 75 min | 1 DGE, 1 ictus | ND | ND | 4 d (3-33) | ND | Results of the entire data series |
| Wilson et al[57], 1992 | 2 | Case series: LGJ | All patients | ND | 120 min | None | 2d | 3 d, 4 d | 4-5 d | 1 patient untill death | |
| Mixed malignancies | |||||||||||
| Zhang et al[66], 2011 | 28 | Case series: LGJ for benign/malignant disease | 7 HPB malignancy | ND | 170 min | 2 reinterventions (anastomotic leak, trocar site hemorrhage), 2 bleeding controlled by endoscopy, 1 ileus, 5 DGE | 3d | 5 d | 8 d (2-83) | ND | Results of the entire data series |
| Guzman et al[3], 2009 | 20 | Cohort: LGJ AND OGJ | Laparoscopy: 8 HPB malignancy | ND | 116 min | 2 DGE | ND | 7 d | 8 d | ND | |
| Navarra et al[67], 2006 | 24 | RCT: 12 LGJ vs 12 OGJ | Laparoscopy: 5 HPB malignancy | ND | 150 min | None | ND | 4.08 d | 11 d | ND | |
| Mehta et al[39], 2006 | 27 | RCT: 14 LGJ vs 13 SEMS | ND | 6 patients (ES, PD) | ND | 2 bleeding, 1 wound infection, 1 pneumonia, 3 DGE. 3 mortality (sepsis, pneumonia, carcinomatosis) | ND | ND | 11.4 D | ND | |
| Al-Rashedy et al[68], 2005 | 26 | Cohort: LGJ and OGJ | Laparoscopy: 7 HPB malignancy | ND | ND | 2 (13.3%) | ND | ND | 3 (3-8) | ND | |
| Khan et al[69], 2005 | 19 | Case series: laparoscopic CCJ ± GJ (16 GJ, 1 CCJ, 2 both) | 7 HPB malignancy | 2 CCJ | 164 min single bypass, 245 min double bypass | ND | 3d | ND | ND | ND | |
| Mittal et al[37], 2004 | 56 | Cohort: 16 OGJ, 14 LGJ, 16 ES. | Laparoscopy: 9 HPB malignancy | None patient | ND | 4 pneumonia, 1 ileus, 1 wound infection | ND | 5 d (4-8) | 13.5 d (6-36) (after procedure 7d) | ND | |
| Bergamaschi et al[70], 2002 | 55 | Case/control: antiperistaltic vs isoperistaltic LGJ | AP-LGJ: 29 HPB malignancy, IP-LGJ 14 HPB malignancy | ND | 100min (AP) vs 99min (IP) | 14 (II: 1, III: 9, IV: 3) | ND | 5.1d (AP) vs 5.3 d (IP) | 8.4 d (AP) vs 8.1 d (IP) | ND | |
| Bergamaschi et al[71],1998 | 22 | Case /control: OGJ (prophylactic and GOO treatment) vs LGJ (GOO treatment) | Laparoscopy: 9 HPB malignancy | 1 ES, 3 PD | 94 min | Pneumonia (1), SSI (1), delayed gastric emptying (1) | ND | 8.4 (media) | 18.4 (media) | ND | |
| Brune et al[15], 1997 | 16 | Case series: LGJ | 13 HPB malignancy | ES/PD | 126 min (70-210) | 1 reintervention (hemorrhage), 3 delayed gastric emptying | ND | ND | 4.7 (2-8) | 16 patients untill death | |
| Nagy et al[72], 1995 | 10 | Case series: LGJ | 9 HPB malignancy | 8 ES/1 PD/ 2 simultaneous CJ | ND | 2 reconversions, 1 CCF, 1 pneumonia, 1 CD infection | ND | 10 d (4-15) | ND | All patients untill death | |
| Ref. | Peristalsis | Location | Type |
| All HPB malignancy | |||
| Jeurnink et al[60], 2007 | ND | Antecolic | Completely stapler |
| Hamade et al[4], 2005 | IP | Antecolic | Stapler + manual suture |
| Denley et al[9], 2005 | IP | Antecolic | Stapler + manual suture |
| Kazanjian et al[5], 2004 | ND | Antecolic | Completely stapler |
| Alam et al[61], 2003 | IP | ND | Completely stapler |
| Kuriansky et al[62], 2000 | ND | Retrocolic | Completely stapler |
| Casaccia et al[63], 1999 | ND | Antecolic | Completely stapler/stapler+ manual suture |
| Casaccia et al[64], 1998 | ND | Antecolic | Completely stapler/stapler+ manual suture |
| Rhodes et al[65], 1995 | ND | ND | Stapler + manual suture |
| Wilson et al[57], 1992 | ND | Antecolic | Stapler + manual suture |
| Mixed malignancies | |||
| Zhang et al[66], 2011 | ND | Antecolic (majority) | Stapler + manual suture |
| Guzman et al[3], 2009 | ND | ND | Stapler + manual suture |
| Navarra et al[67], 2006 | IP | Antecolic | Stapler + manual suture |
| Mehta et al[39], 2006 | ND | Antecolic | Stapler + manual suture |
| Al-Rashedy et al[68], 2005 | ND | Antecolic | Hand-sutured or stapler |
| Khan et al[69], 2005 | ND | Antecolic | Stapler + manual suture |
| Mittal et al[37], 2004 | ND | ND | ND |
| Bergamaschi et al[70], 2002 | 29 AP vs 14 IP | Antecolic | 17 completely stapled/38 stapler+ manual suture |
| Bergamaschi et al[71],1998 | ND | ND | 7 completely stapled/2 stapler+ manual suture |
| Brune et al[15], 1997 | IP | Antecolic | Stapler + manual suture |
| Nagy et al[72], 1995 | ND | Antecolic | Stapler + manual suture |
We also performed a retrospective study at the Department of General Surgery and Digestive of the University Hospital of Guadalajara. The period analyzed was January 2009-March 2018. We included all consecutive patients who underwent laparoscopic palliative GJ for malignant GOO due to advanced HPB cancer, excluding prophylactic GJ and OGJ. All patients had histological diagnosis of HPB cancer. For this purpose, the Mambrino XXI® electronic medical history was used.
Our results are shown in Table 4. All GJ were performed by the same surgeon using the same approach (IP, antecolic and stapler plus manual suture). Three patients had previous biliary stent, and another patient needed a percutaneous biliary stent after laparoscopic GJ due to obstructive jaundice. The clinical success rate was 100%, with all patients maintaining oral intake until death. The median time from surgery to hospital discharge was 12 d (range 5-13), excluding hospital stay prior surgery attributable to GOO. One patient died due to sepsis caused by a hepatic abscess on postoperative (PO) day 78, and another died due to carcinomatosis and tumor progression on PO day 82. Median overall-survival was 214.67 d.
| Age/sex | Biliary obstruction | Surgical technique | Clinical success | Time to initiate intake | Surgery-discharge (d) | 90-d morbidity | Duration of food intake | Survival (d) |
| 87/F | No | IP antecolic, stapler + manual suture | Yes | 4 | 12 | CD infection | Until death | 402 |
| 76/M | Biliary stent | IP antecolic, stapler + manual suture | Yes | 3 | 12 | No | Until death | 228 |
| 91/F | No | IP antecolic, stapler + manual suture | Yes | 1 | 5 | No | Until death | 278 |
| 78/F | No | IP antecolic, stapler + manual suture | Yes | 3 | 10 | Readmission: Sepsis due to hepatic abscess (death) | 78 | 78 |
| 68/F | Biliary stent | IP antecolic, stapler + manual suture | Yes | 3 | 12 | Readmission: Intestinal obstruction due to carcinomatosis (death) | 82 | 82 |
| 76/M | Biliary stent | IP antecolic, stapler + manual suture | Yes | 3 | 13 | Catheter-related bacteriemia. Readmission: Biliary stent due to jaundice. | Until death | 220 |
| 76/F | No | IP antecolic, stapler + manual suture | Yes | 3 | 5 | No | Until death | ND |
Several surgical procedures for GJ have been reported since Devine et al’s first description in 1925, which introduced a procedure consisting of transection of the stomach and anastomosis between the jejunal loop-and the proximal stump of the stomach[73]. But GJ may be not fully effective due to of DGE or tumor bleeding; so a modified Devine procedure has been developed, in which the stomach is partially divided into proximal and distal parts, and the proximal part of the stomach is anastomosed to the proximal part of the jejunum[74,75]. This technique, stomach-partitioning GJ (SP-GJ), minimizes contact between food and the tumor and allows endoscopic examination[74]. The first laparoscopic approach for SP-GJ was described by Matsumoto et al[76] in 2005. This surgical technique is associated with lower incidence of bleeding and delayed gastric emptying, with no increase in anastomotic leakage[74-78].
Other surgical approaches reported in the literature for the management of malignant GOO include natural orifice transumbilical surgery[79] or a laparoscopic-assisted approach for a circular mechanical GJ, in which the proximal jejunum is exteriorized by laparoscopy via an epigastric trocar-site incision[80].
EUS-gastroenteroanastomosis (EUS-GE) was first described by Fritscher-Ravens et al[81,82] in 2002. It is produced by anatomical puncture from the stomach into the third part of the duodenum (-EUS-guided gastroduodenostomy), or into the jejunum (EUS-guided gastrojejunostomy)[83].
This new EUS technique involves the placement of a lumen-apposing metal stent (LAMS). Data regarding its use are limited[84-87]. In 2017, Pérez-Miranda et al[87] reported the results of a multicenter cohort study comparing EUS-GJ and LGJ. All patients in the EUS-GJ group had symptomatic GOO, compared with only 34% of patients in LGJ group. The clinical success rates in the two groups were 84% vs 90%, LOS was 9.4 d vs 8.9 d and adverse events were 12% vs 41%, with the EUS-GJ group presenting better results in all cases. This is a new EUS technique and it should be reserved for use at experienced centers.
Palliative treatment of GOO due to advanced HPB cancer may improve QOL and resolve symptoms. Both a non-operative endoscopic approach and surgical treatment are available (Table 5) and an estimation of probable survival is essential for the choice of treatment. Evaluation of the patient and multidisciplinary expertise are required to select the appropriate approach.
| Procedure | Advantages | Disadvantages |
| Open GJ | Bypass of tumor | Most invasive procedure |
| Established surgical procedure | Longer LOS | |
| Lower re-intervention rate | Nutritional status | |
| Good long-term results | Critically ill patients | |
| Laparoscopic GJ | Bypass of tumor | Invasive procedure |
| Lower re-intervention rate | Longer LOS | |
| Established surgical procedure | Nutritional status | |
| Less invasive than open GJ | Critically ill patients | |
| Good long-term results | ||
| Endoscopic enteral stent | Short procedure time | Stent migration |
| Established endoscopic procedure | Patency | |
| Broad indication regardless patient condition | ||
| Short LOS | ||
| Good short-term results | ||
| EUS-GJ | Bypass of tumor | Special device |
| Short procedure time | Non-establish endoscopic procedure | |
| Short LOS | Serious adverse events | |
| Less invasive |
Stent is usually preferred in patients with poor general condition or short life expectancy. LGJ is a feasible, safe and efficient technical option. Given the limited studies and the difficulty of performing prospective controlled trials due to patient heterogeneity, no study can cover all the complexities of malignant GOO and more outcome data are needed. Prospective clinical trials with adequate sample sizes comparing different approaches size are warranted.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Spain
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Fiori E, Nakai Y S- Editor: Gong ZM L- Editor: A E- Editor: Huang Y
| 1. | Gentileschi P, Kini S, Gagner M. Palliative laparoscopic hepatico- and gastrojejunostomy for advanced pancreatic cancer. JSLS. 2002;6:331-338. [PubMed] |
| 2. | Gurusamy KS, Kumar S, Davidson BR. Prophylactic gastrojejunostomy for unresectable periampullary carcinoma. Cochrane Database Syst Rev. 2013;2:CD008533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Guzman EA, Dagis A, Bening L, Pigazzi A. Laparoscopic gastrojejunostomy in patients with obstruction of the gastric outlet secondary to advanced malignancies. Am Surg. 2009;75:129-132. [PubMed] |
| 4. | Hamade AM, Al-Bahrani AZ, Owera AM, Hamoodi AA, Abid GH, Bani Hani OI, O’Shea S, Lee SH, Ammori BJ. Therapeutic, prophylactic, and preresection applications of laparoscopic gastric and biliary bypass for patients with periampullary malignancy. Surg Endosc. 2005;19:1333-1340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Kazanjian KK, Reber HA, Hines OJ. Laparoscopic gastrojejunostomy for gastric outlet obstruction in pancreatic cancer. Am Surg. 2004;70:910-913. [PubMed] |
| 6. | Bahra M, Jacob D. Surgical palliation of advanced pancreatic cancer. Recent Results Cancer Res. 2008;177:111-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Moss AC, Morris E, Mac Mathuna P. Palliative biliary stents for obstructing pancreatic carcinoma. Cochrane Database Syst Rev. 2006;2:CD004200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Minata MK, Bernardo WM, Rocha RS, Morita FH, Aquino JC, Cheng S, Zilberstein B, Sakai P, de Moura EG. Stents and surgical interventions in the palliation of gastric outlet obstruction: a systematic review. Endosc Int Open. 2016;4:E1158-E1170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Denley SM, Moug SJ, Carter CR, McKay CJ. The outcome of laparoscopic gastrojejunostomy in malignant gastric outlet obstruction. Int J Gastrointest Cancer. 2005;35:165-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Del Piano M, Ballarè M, Montino F, Todesco A, Orsello M, Magnani C, Garello E. Endoscopy or surgery for malignant GI outlet obstruction? Gastrointest Endosc. 2005;61:421-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 126] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 11. | Watanapa P, Williamson RC. Surgical palliation for pancreatic cancer: developments during the past two decades. Br J Surg. 1992;79:8-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 240] [Cited by in RCA: 213] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 12. | Jeurnink SM, Steyerberg EW, van Hooft JE, van Eijck CH, Schwartz MP, Vleggaar FP, Kuipers EJ, Siersema PD; Dutch SUSTENT Study Group. Surgical gastrojejunostomy or endoscopic stent placement for the palliation of malignant gastric outlet obstruction (SUSTENT study): a multicenter randomized trial. Gastrointest Endosc. 2010;71:490-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 358] [Cited by in RCA: 358] [Article Influence: 23.9] [Reference Citation Analysis (2)] |
| 13. | Nagaraja V, Eslick GD, Cox MR. Endoscopic stenting versus operative gastrojejunostomy for malignant gastric outlet obstruction-a systematic review and meta-analysis of randomized and non-randomized trials. J Gastrointest Oncol. 2014;5:92-98. [PubMed] |
| 14. | Yoshida Y, Fukutomi A, Tanaka M, Sugiura T, Kawata N, Kawai S, Kito Y, Hamauchi S, Tsushima T, Yokota T. Gastrojejunostomy versus duodenal stent placement for gastric outlet obstruction in patients with unresectable pancreatic cancer. Pancreatology. 2017;17:983-989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 15. | Brune IB, Feussner H, Neuhaus H, Classen M, Siewert JR. Laparoscopic gastrojejunostomy and endoscopic biliary stent placement for palliation of incurable gastric outlet obstruction with cholestasis. Surg Endosc. 1997;11:834-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Engelken FJ, Bettschart V, Rahman MQ, Parks RW, Garden OJ. Prognostic factors in the palliation of pancreatic cancer. Eur J Surg Oncol. 2003;29:368-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 85] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 17. | Michelassi F, Erroi F, Dawson PJ, Pietrabissa A, Noda S, Handcock M, Block GE. Experience with 647 consecutive tumors of the duodenum, ampulla, head of the pancreas, and distal common bile duct. Ann Surg. 1989;210:544-554; discussion 554-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 161] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 18. | Smith RA, Bosonnet L, Ghaneh P, Sutton R, Evans J, Healey P, Garvey C, Hughes M, Raraty M, Campbell F. The platelet-lymphocyte ratio improves the predictive value of serum CA19-9 levels in determining patient selection for staging laparoscopy in suspected periampullary cancer. Surgery. 2008;143:658-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 82] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 19. | Mayo SC, Austin DF, Sheppard BC, Mori M, Shipley DK, Billingsley KG. Evolving preoperative evaluation of patients with pancreatic cancer: does laparoscopy have a role in the current era? J Am Coll Surg. 2009;208:87-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 20. | Wong YT, Brams DM, Munson L, Sanders L, Heiss F, Chase M, Birkett DH. Gastric outlet obstruction secondary to pancreatic cancer: surgical vs endoscopic palliation. Surg Endosc. 2002;16:310-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 141] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 21. | Lillemoe KD, Cameron JL, Hardacre JM, Sohn TA, Sauter PK, Coleman J, Pitt HA, Yeo CJ. Is prophylactic gastrojejunostomy indicated for unresectable periampullary cancer? A prospective randomized trial. Ann Surg. 1999;230:322-328; discussion 328-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 293] [Cited by in RCA: 243] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 22. | Van Heek NT, De Castro SM, van Eijck CH, van Geenen RC, Hesselink EJ, Breslau PJ, Tran TC, Kazemier G, Visser MR, Busch OR. The need for a prophylactic gastrojejunostomy for unresectable periampullary cancer: a prospective randomized multicenter trial with special focus on assessment of quality of life. Ann Surg. 2003;238:894-902; discussion 902-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 117] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 23. | Topazian M, Ring E, Grendell J. Palliation of obstructing gastric cancer with steel mesh, self-expanding endoprostheses. Gastrointest Endosc. 1992;38:58-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 72] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 24. | Solt J, Papp Z. Strecker stent implantation in malignant gastric outlet stenosis. Gastrointest Endosc. 1993;39:442-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Song HY, Yang DH, Kuh JH, Choi KC. Obstructing cancer of the gastric antrum: palliative treatment with covered metallic stents. Radiology. 1993;187:357-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 59] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Maetani I, Ogawa S, Hoshi H, Sato M, Yoshioka H, Igarashi Y, Sakai Y. Self-expanding metal stents for palliative treatment of malignant biliary and duodenal stenoses. Endoscopy. 1994;26:701-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 27. | Strecker EP, Boos I, Husfeldt KJ. Malignant duodenal stenosis: palliation with peroral implantation of a self-expanding nitinol stent. Radiology. 1995;196:349-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 39] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 28. | Maetani I, Inoue H, Sato M, Ohashi S, Igarashi Y, Sakai Y. Peroral insertion techniques of self-expanding metal stents for malignant gastric outlet and duodenal stenoses. Gastrointest Endosc. 1996;44:468-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 29. | Feretis C, Benakis P, Dimopoulos C, Manouras A, Tsimbloulis B, Apostolidis N. Duodenal obstruction caused by pancreatic head carcinoma: palliation with self-expandable endoprostheses. Gastrointest Endosc. 1997;46:161-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 63] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 30. | Nevitt AW, Vida F, Kozarek RA, Traverso LW, Raltz SL. Expandable metallic prostheses for malignant obstructions of gastric outlet and proximal small bowel. Gastrointest Endosc. 1998;47:271-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 73] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 31. | Yates MR 3rd, Morgan DE, Baron TH. Palliation of malignant gastric and small intestinal strictures with self-expandable metal stents. Endoscopy. 1998;30:266-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 82] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 32. | Soetikno RM, Carr-Locke DL. Expandable metal stents for gastric-outlet, duodenal, and small intestinal obstruction. Gastrointest Endosc Clin N Am. 1999;9:447-458. [PubMed] |
| 33. | Park HS, Do YS, Suh SW, Choo SW, Lim HK, Kim SH, Shim YM, Park KC, Choo IW. Upper gastrointestinal tract malignant obstruction: initial results of palliation with a flexible covered stent. Radiology. 1999;210:865-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 34. | Fiori E, Lamazza A, Volpino P, Burza A, Paparelli C, Cavallaro G, Schillaci A, Cangemi V. Palliative management of malignant antro-pyloric strictures. Gastroenterostomy vs. endoscopic stenting. A randomized prospective trial. Anticancer Res. 2004;24:269-271. [PubMed] |
| 35. | Maetani I, Tada T, Ukita T, Inoue H, Sakai Y, Nagao J. Comparison of duodenal stent placement with surgical gastrojejunostomy for palliation in patients with duodenal obstructions caused by pancreaticobiliary malignancies. Endoscopy. 2004;36:73-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 133] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 36. | Potz BA, Miner TJ. Surgical palliation of gastric outlet obstruction in advanced malignancy. World J Gastrointest Surg. 2016;8:545-555. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 19] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (1)] |
| 37. | Mittal A, Windsor J, Woodfield J, Casey P, Lane M. Matched study of three methods for palliation of malignant pyloroduodenal obstruction. Br J Surg. 2004;91:205-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 127] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 38. | Ly J, O’Grady G, Mittal A, Plank L, Windsor JA. A systematic review of methods to palliate malignant gastric outlet obstruction. Surg Endosc. 2010;24:290-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 120] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 39. | Mehta S, Hindmarsh A, Cheong E, Cockburn J, Saada J, Tighe R, Lewis MP, Rhodes M. Prospective randomized trial of laparoscopic gastrojejunostomy versus duodenal stenting for malignant gastric outflow obstruction. Surg Endosc. 2006;20:239-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 155] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 40. | Levenick JM, Gordon SR, Sutton JE, Suriawinata A, Gardner TB. A comprehensive, case-based review of groove pancreatitis. Pancreas. 2009;38:e169-e175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 41. | Kirby GC, Faulconer ER, Robinson SJ, Perry A, Downing R. Superior mesenteric artery syndrome: a single centre experience of laparoscopic duodenojejunostomy as the operation of choice. Ann R Coll Surg Engl. 2017;99:472-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 42. | Pottorf BJ, Husain FA, Hollis HW Jr, Lin E. Laparoscopic management of duodenal obstruction resulting from superior mesenteric artery syndrome. JAMA Surg. 2014;149:1319-1322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (1)] |
| 43. | Zilberstein B, Sorbello MP, Orso IR, Cecconello I. Laparoscopic duodenal-jejunal bypass for the treatment of duodenal obstruction caused by annular pancreas: description of a surgical technique. Surg Laparosc Endosc Percutan Tech. 2011;21:e60-e64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 44. | De Ugarte DA, Dutson EP, Hiyama DT. Annular pancreas in the adult: management with laparoscopic gastrojejunostomy. Am Surg. 2006;72:71-73. [PubMed] |
| 45. | Kohan G, Ocampo CG, Zandalazini HI, Klappenbach R, Yazyi F, Ditulio O, Coturel A, Canullán C, Porras LT, Rodriguez JA. Laparoscopic hepaticojejunostomy and gastrojejunostomy for palliative treatment of pancreatic head cancer in 48 patients. Surg Endosc. 2015;29:1970-1975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 46. | Miner TJ. Palliative surgery for advanced cancer: lessons learned in patient selection and outcome assessment. Am J Clin Oncol. 2005;28:411-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 42] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 47. | Miner TJ, Cohen J, Charpentier K, McPhillips J, Marvell L, Cioffi WG. The palliative triangle: improved patient selection and outcomes associated with palliative operations. Arch Surg. 2011;146:517-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 48. | Poulsen M, Trezza M, Atimash GH, Sorensen LT, Kallehave F, Hemmingsen U, Jorgensen LN. Risk factors for morbidity and mortality following gastroenterostomy. J Gastrointest Surg. 2009;13:1238-1244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 49. | Sasaki T, Isayama H, Nakai Y, Togawa O, Kogure H, Kawakubo K, Mizuno S, Yashima Y, Ito Y, Yamamoto N. Predictive factors of solid food intake in patients with malignant gastric outlet obstruction receiving self-expandable metallic stents for palliation. Dig Endosc. 2012;24:226-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 50. | Jeon HH, Park CH, Park JC, Shim CN, Kim S, Lee HJ, Lee H, Shin SK, Lee SK, Lee YC. Carcinomatosis matters: clinical outcomes and prognostic factors for clinical success of stent placement in malignant gastric outlet obstruction. Surg Endosc. 2014;28:988-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 51. | Dormann A, Meisner S, Verin N, Wenk Lang A. Self-expanding metal stents for gastroduodenal malignancies: systematic review of their clinical effectiveness. Endoscopy. 2004;36:543-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 290] [Article Influence: 13.8] [Reference Citation Analysis (1)] |
| 52. | Chandrasegaram MD, Eslick GD, Mansfield CO, Liem H, Richardson M, Ahmed S, Cox MR. Endoscopic stenting versus operative gastrojejunostomy for malignant gastric outlet obstruction. Surg Endosc. 2012;26:323-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 66] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 53. | Hamada T, Nakai Y, Isayama H, Sasaki T, Kogure H, Kawakubo K, Sasahira N, Yamamoto N, Togawa O, Mizuno S. Duodenal metal stent placement is a risk factor for biliary metal stent dysfunction: an analysis using a time-dependent covariate. Surg Endosc. 2013;27:1243-1248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 54. | Woo SM, Kim DH, Lee WJ, Park KW, Park SJ, Han SS, Kim TH, Koh YH, Kim HB, Hong EK. Comparison of uncovered and covered stents for the treatment of malignant duodenal obstruction caused by pancreaticobiliary cancer. Surg Endosc. 2013;27:2031-2039. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 55. | Hamada T, Hakuta R, Takahara N, Sasaki T, Nakai Y, Isayama H, Koike K. Covered versus uncovered metal stents for malignant gastric outlet obstruction: Systematic review and meta-analysis. Dig Endosc. 2017;29:259-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 56. | Nakai Y, Hamada T, Isayama H, Itoi T, Koike K. Endoscopic management of combined malignant biliary and gastric outlet obstruction. Dig Endosc. 2017;29:16-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (1)] |
| 57. | Wilson RG, Varma JS. Laparoscopic gastroenterostomy for malignant duodenal obstruction. Br J Surg. 1992;79:1348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 58. | Siddiqui A, Spechler SJ, Huerta S. Surgical bypass versus endoscopic stenting for malignant gastroduodenal obstruction: a decision analysis. Dig Dis Sci. 2007;52:276-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 54] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 59. | Fiori E, Lamazza A, Demasi E, Decesare A, Schillaci A, Sterpetti AV. Endoscopic stenting for gastric outlet obstruction in patients with unresectable antro pyloric cancer. Systematic review of the literature and final results of a prospective study. The point of view of a surgical group. Am J Surg. 2013;206:210-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 60. | Jeurnink SM, Steyerberg EW, Hof Gv, van Eijck CH, Kuipers EJ, Siersema PD. Gastrojejunostomy versus stent placement in patients with malignant gastric outlet obstruction: a comparison in 95 patients. J Surg Oncol. 2007;96:389-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 105] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 61. | Alam TA, Baines M, Parker MC. The management of gastric outlet obstruction secondary to inoperable cancer. Surg Endosc. 2003;17:320-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 62. | Kuriansky J, Sáenz A, Astudillo E, Cardona V, Fernández-Cruz L. Simultaneous laparoscopic biliary and retrocolic gastric bypass in patients with unresectable carcinoma of the pancreas. Surg Endosc. 2000;14:179-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 63. | Casaccia M, Diviacco P, Molinello P, Danovaro L, Casaccia M. Laparoscopic palliation of unresectable pancreatic cancers: preliminary results. Eur J Surg. 1999;165:556-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 64. | Casaccia M, Diviacco P, Molinello P, Danovaro L, Casaccia M. Laparoscopic gastrojejunostomy in the palliation of pancreatic cancer: reflections on the preliminary results. Surg Laparosc Endosc. 1998;8:331-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 65. | Rhodes M, Nathanson L, Fielding G. Laparoscopic biliary and gastric bypass: a useful adjunct in the treatment of carcinoma of the pancreas. Gut. 1995;36:778-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 75] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 66. | Zhang LP, Tabrizian P, Nguyen S, Telem D, Divino C. Laparoscopic gastrojejunostomy for the treatment of gastric outlet obstruction. JSLS. 2011;15:169-173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 67. | Navarra G, Musolino C, Venneri A, De Marco ML, Bartolotta M. Palliative antecolic isoperistaltic gastrojejunostomy: a randomized controlled trial comparing open and laparoscopic approaches. Surg Endosc. 2006;20:1831-1834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 47] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 68. | Al-Rashedy M, Dadibhai M, Shareif A, Khandelwal MI, Ballester P, Abid G, McCloy RF, Ammori BJ. Laparoscopic gastric bypass for gastric outlet obstruction is associated with smoother, faster recovery and shorter hospital stay compared with open surgery. J Hepatobiliary Pancreat Surg. 2005;12:474-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 69. | Khan AZ, Miles WF, Singh KK. Initial experience with laparoscopic bypass for upper gastrointestinal malignancy: a new option for palliation of patients with advanced upper gastrointestinal tumors. J Laparoendosc Adv Surg Tech A. 2005;15:374-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 70. | Bergamaschi R, Arnaud JP, Mårvik R, Myrvold HE. Laparoscopic antiperistaltic versus isoperistaltic gastrojejunostomy for palliation of gastric outlet obstruction in advanced cancer. Surg Laparosc Endosc Percutan Tech. 2002;12:393-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 71. | Bergamaschi R, Mårvik R, Thoresen JE, Ystgaard B, Johnsen G, Myrvold HE. Open versus laparoscopic gastrojejunostomy for palliation in advanced pancreatic cancer. Surg Laparosc Endosc. 1998;8:92-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 48] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 72. | Nagy A, Brosseuk D, Hemming A, Scudamore C, Mamazza J. Laparoscopic gastroenterostomy for duodenal obstruction. Am J Surg. 1995;169:539-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 53] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 73. | Devine HB. Basic principles and supreme difficulties in gastric surgery. Surg Gynecol obstet. 1925;40:1-16. |
| 74. | Schantz SP, Schickler W, Evans TK, Coffey RJ. Palliative gastroenterostomy for pancreatic cancer. Am J Surg. 1989;76:793-796. |
| 75. | Kaminishi M, Yamaguchi H, Shimizu N, Nomura S, Yoshikawa A, Hashimoto M, Sakai S, Oohara T. Stomach-partitioning gastrojejunostomy for unresectable gastric carcinoma. Arch Surg. 1997;132:184-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 76. | Matsumoto T, Izumi K, Shiromizu A, Shibata K, Ohta M, Kitano S. Laparoscopic gastric partitioning gastrojejunostomy for an unresectable duodenal malignant tumor. J Minim Access Surg. 2005;1:129-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 77. | Kushibiki T, Ebihara Y, Hontani K, Tanaka K, Nakanishi Y, Asano T, Noji T, Kurashima Y, Murakami S, Nakamura T. The Surgical Outcomes of Totally Laparoscopic Stomach-partitioning Gastrojejunostomy for Gastric Outlet Obstruction: A Retrospective, Cohort Study. Surg Laparosc Endosc Percutan Tech. 2018;28:e49-e53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 78. | Eguchi H, Yada K, Shibata K, Matsumoto T, Etoh T, Yasuda K, Inomata M, Shiraishi N, Ohta M, Kitano S. Laparoscopic stomach-partitioning gastrojejunostomy is an effective palliative procedure to improve quality of life in patients with malignant gastroduodenal outlet obstruction. Asian J Endosc Surg. 2012;5:153-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 79. | Nguyen NT, Slone J, Reavis KM, Woolridge J, Smith BR, Chang K. Laparoscopic transumbilical gastrojejunostomy: an advanced anastomotic procedure performed through a single site. J Laparoendosc Adv Surg Tech A. 2009;19:199-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 80. | Chung RS, Li P. Palliative gastrojejunostomy. A minimally invasive approach. Surg Endosc. 1997;11:676-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 81. | Fritscher-Ravens A, Mosse CA, Mills TN, Mukherjee D, Park PO, Swain P. A through-the-scope device for suturing and tissue approximation under EUS control. Gastrointest Endosc. 2002;56:737-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 82. | Fritscher-Ravens A, Mosse CA, Mukherjee D, Mills T, Park PO, Swain CP. Transluminal endosurgery: single lumen access anastomotic device for flexible endoscopy. Gastrointest Endosc. 2003;58:585-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 61] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 83. | Itoi T, Baron TH, Khashab MA, Tsuchiya T, Irani S, Dhir V, Bun Teoh AY. Technical review of endoscopic ultrasonography-guided gastroenterostomy in 2017. Dig Endosc. 2017;29:495-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 86] [Article Influence: 10.8] [Reference Citation Analysis (35)] |
| 84. | Khashab MA, Kumbhari V, Grimm IS, Ngamruengphong S, Aguila G, El Zein M, Kalloo AN, Baron TH. EUS-guided gastroenterostomy: the first U.S. clinical experience (with video). Gastrointest Endosc. 2015;82:932-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 144] [Article Influence: 14.4] [Reference Citation Analysis (3)] |
| 85. | Tyberg A, Perez-Miranda M, Sanchez-Ocaña R, Peñas I, de la Serna C, Shah J, Binmoeller K, Gaidhane M, Grimm I, Baron T. Endoscopic ultrasound-guided gastrojejunostomy with a lumen-apposing metal stent: a multicenter, international experience. Endosc Int Open. 2016;4:E276-E281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 174] [Cited by in RCA: 178] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 86. | Itoi T, Tsuchiya T, Tonozuka R, Ijima M, Kusano C. Novel EUS-guided double-balloon-occluded gastrojejunostomy bypass. Gastrointest Endosc. 2016;83:461-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 87. | Perez-Miranda M, Tyberg A, Poletto D, Toscano E, Gaidhane M, Desai AP, Kumta NA, Fayad L, Nieto J, Barthet M. EUS-guided Gastrojejunostomy Versus Laparoscopic Gastrojejunostomy: An International Collaborative Study. J Clin Gastroenterol. 2017;51:896-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 170] [Article Influence: 21.3] [Reference Citation Analysis (1)] |