Published online May 7, 2018. doi: 10.3748/wjg.v24.i17.1859
Peer-review started: March 11, 2018
First decision: March 29, 2018
Revised: April 14, 2018
Accepted: April 23, 2018
Article in press: April 23, 2018
Published online: May 7, 2018
Processing time: 57 Days and 9.4 Hours
Symptomatic intestinal strictures develop in more than one third of patients with Crohn’s disease (CD) within 10 years of disease onset. Strictures can be inflammatory, fibrotic or mixed and result in a significant decline in quality of life, frequently requiring surgery for palliation of symptoms. Patients under the age of 40 with perianal disease are more likely to suffer from disabling ileocolonic disease thus may have a greater risk for fibrostenotic strictures. Treatment options for fibrostenotic strictures are limited to endoscopic and surgical therapy. Endoscopic balloon dilatation (EBD) appears to be a safe, less invasive and effective alternative modality to replace or defer surgery. Serious complications are rare and occur in less than 3% of procedures. For non-complex strictures without adjacent fistulizaation or perforation that are less than 5 cm in length, EBD should be considered as first-line therapy. The aim of this review is to present the current literature on the endoscopic management of small bowel and colonic strictures in CD, which includes balloon dilatation, adjuvant techniques of intralesional injection of steroids and anti-tumor necrosis factor, and metal stent insertion. Short and long-term outcomes, complications and safety of EBD will be discussed.
Core tip: Endoscopic balloon dilation (EBD) for Crohn’s disease-related fibrostenotic strictures has been recognized as a safe, and less invasive intervention with rare complications that occur in less than 3% of procedures. EBD can replace or defer surgery and help avoid frequent intestinal resections, which result in short bowel syndrome and impair quality of life. For non-complex strictures without adjacent fistulization or perforation that are less than 5 cm in length, EBD should be considered as first-line therapy. In this review we discuss safety, short and long-term outcomes, as well as adjuvant techniques of intralesional injection of steroids, anti-tumor necrosis factor, and metal stent insertion.
- Citation: Bessissow T, Reinglas J, Aruljothy A, Lakatos PL, Van Assche G. Endoscopic management of Crohn’s strictures. World J Gastroenterol 2018; 24(17): 1859-1867
- URL: https://www.wjgnet.com/1007-9327/full/v24/i17/1859.htm
- DOI: https://dx.doi.org/10.3748/wjg.v24.i17.1859
Intestinal strictures are a common complication of Crohn’s disease (CD) affecting one-third of the patient population within 10 years of disease onset. This number, however, is likely under-reported[1,2]. In general, CD strictures are classified into inflammatory, fibrotic or mixed, although all symptomatic inflammatory strictures likely have some component of fibrosis and vice-versa[2,3]. Risk factors and predictors of intestinal strictures to date are clinical, environmental, genetic or endoscopic parameters[4] (Table 1). Although no clinical factors exist which can accurately predict the stricturing phenotype of CD, there do exist factors which may predict the likelihood of small bowel disease and a disabling disease course thus indirectly may suggest an increased risk for the development of fibrostenotic disease. These factors include the presence of perianal disease, age of CD diagnosis less than 40 years old and the need for steroids during the first flare[4,5]. Patients frequently complain of progressive post-prandial abdominal pain, bloating, nausea, vomiting and weight loss. The diagnosis of intestinal strictures usually coincides with a spiraling decline in quality of life and results in surgery in 75% of patients at least once during their lifetime[1]. CD patients will frequently undergo multiple bowel resections over their lifetime that repeatedly exposes them to immediate and long-term post-operative complications such as anastomotic leaks with intra-abdominal sepsis, short bowel syndrome, and adhesions with recurrent bowel obstructions[2,6].
| Clinical[4] | Age at diagnosis < 40 yr |
| Perianal disease at diagnosis | |
| Need for steroids during first flare | |
| Small bowel disease location | |
| Prior appendectomy | |
| Environmental[4] | Smoking |
| Endoscopic[4] | Deep mucosal ulcerations |
| Genetic[4] | Nucleotide oligomerisation domain 2 (NOD2) variants |
| Janus-associated kinase 2 (JAK2) | |
| Caspase-recruitment domain 15 (CARD15) | |
| NOD2/CARD15 mutations on both chromosomes | |
| TNF superfamily 15 (TNFSF15) in Asians | |
| 5T5T in the MMP3 gene | |
| rs1363670 | |
| Serological[4] | Antimicrobial antibodies |
| anti-Saccharomyces cerevisiae antibodies (ASCA) IgA in Asians |
The pathogenesis of CD complications develops from chronic accumulation of inflammatory bowel damage variably leading to stricture, fistula and/or abscess formation[2]. Stricture development, although not fully understood, involves the progressive deposition of extracellular matrix protein (ECM) produced by myofibroblasts at variable sites of the bowel being injured by chronically uncontrolled relapsing and remitting transmural inflammation[7]. During chronic intestinal inflammation, the baseline release of profibrotic cytokines (e.g., IL-4 and IL-13) increases over time further accelerating the process of excessive matrix deposition[7,8]. There may also exist a point where inflammation is no longer required to trigger fibrosis. As ECM is deposited during chronic inflammation, the bowel wall becomes stiffer. Bowel wall stiffness acts independently as a mesenchymal cell activator, resulting in ongoing myofibroblast stimulation, thus progressive fibrotic stenosis[9].
Treatment options for fibrostenotic strictures are limited to endoscopic and surgical therapy (i.e., stricturoplasty and small bowel resection)[10]. Fortunately, most de novo strictures form in the ileum and ileocolic regions, which are accessible by ileocolonoscopy or balloon-assisted enteroscopy[11]. Although pharmacotherapy may delay the time before operative management, it has not been shown to prevent it[12]. Approximately 80% of patients will have their first bowel resection 10 years following their diagnosis of CD[2]. To date no specific intestinal anti-fibrotic therapy exists, nor has any immunosuppressant or biologic therapy been shown to prevent stricture formation.
The following review presents the current data on the endoscopic management of small bowel and colonic strictures in CD. Short and long-term outcomes, complications and a description of the procedure will be discussed.
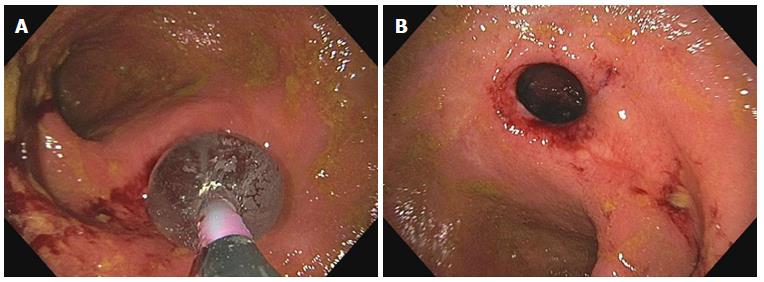
Endoscopic balloon dilation (EBD) is a minimally invasive bowel-length preserving mean of managing symptomatic CD patients with short fibrotic strictures (Figure 1). EBD has become an established modality of therapy and often plays an important role in delaying or acting as a bridge to surgery[10,13]. The most common location of the small bowel to undergo EBD using a colonoscope is the distal ileum or at the ileocolonic anastomosis of a patient following a small bowel resection[14]. Strictures located in the distal duodenum to proximal jejunum or distal jejunum to proximal ileum may be accessed with ante- or retrograde enteroscopy, respectively[15].
Short- and long-term efficacy has been inconsistently defined in studies[13]. In general, short-term efficacy has been described as the technical success of the procedure or the ability to traverse the dilated area freely with the endoscope immediately after dilatation[13,16]. Long-term efficacy, in most studies, has been described as the time elapsed until another intervention (either surgical or endoscopic) is required[2,13,16]. Despite the lack of a formal definition, excellent short- and moderate long-term efficacy of EBD for CD strictures has been documented in many studies[14,16,17]. Table 2 shows a summary of published studies on EBD using conventional colonoscopy in CD patients. In a systematic review and descriptive pooled analysis of 12 studies conducted between 1991 to 2013 evaluating 1463 CD patients who underwent 3213 EBD procedures, the technical success rate was 89% with an associated relief of clinical symptoms in 81% of patients[14]. The majority of strictures were ileal (98.6%) at anastomotic sites (62%), which were 2 cm or less. However, the recurrence rate of strictures was high. At the 36.6 mo median follow-up, 47.5% of patients had symptomatic recurrence and 28.6% of all patients had required surgical intervention. This study concluded that the chance of requiring repeat EBD or surgical intervention at 2 years was 73.5% and 42.9%, respectively[14]. Another large recent systematic review with meta-analysis involving 1089 patients (2664 EBDs) across 25 studies revealed similar results[17]. The technical success rate was 92.3% with a reported symptomatic response rate of 70.4%. The proportion of patients requiring a repeat dilation after 1 and 2 years was 31.6% (160/506) and 25.9% (117/451), respectively. Most patients within 5 years required recurrent dilations (80%) and/or surgical interventions (75%)[17]. Of interest is the lower symptomatic success rate as compared to the technical success rate across studies. This likely occurred due to a lack of a standardized means of reporting technical and clinical efficacy and/or a superimposed process existing that contributed to the patient’s symptoms (e.g., ongoing inflammation, intestinal bacterial overgrowth, IBS, etc.)[10]. Despite this discrepancy, the short-term clinical success rate remains high.
| Authors | Pubished year | No. of patients | Anastomotic strictures (%) | Maximum balloon caliber (mm) | Technical success (%) | Clinical efficacy (%) | Major complication (%) |
| Blomberg et al[52] | 1991 | 27 | 100 | 25 | 100 | 67 | 0 |
| Williams et al[53] | 1991 | 7 | 71 | 20 | 71 | 71 | 0 |
| Breysem et al[54] | 1992 | 18 | 78 | 18 | 89 | 50 | 0 |
| Cockuyt et al[55] | 1995 | 55 | 67 | 20 | 85 | 62 | 8 |
| Ramboer et al[56] | 1995 | 13 | 69 | 18 | 100 | 100 | 0 |
| Matsui et al[57] | 2000 | 55 | 43 | 20 | 86 | 78 | 2 |
| Dear et al[58] | 2001 | 22 | 95 | 18 | 100 | 73 | 0 |
| Brooker et al[59] | 2003 | 14 | 79 | 20 | 100 | 79 | 0 |
| Morini et al[60] | 2003 | 43 | 67 | 18 | 79 | 42 | 0 |
| Sabate et al[61] | 2003 | 38 | 68 | 25 | 84 | 53 | 3 |
| Thomas-Gibson et al[62] | 2003 | 59 | 90 | 18 | 73 | 41 | 3 |
| Singh et al[63] | 2005 | 17 | 35 | 20 | 100 | 76 | 18 |
| Aljouni et al[64] | 2006 | 37 | 37 | 20 | 90 | 87 | 3 |
| Ferlitsch et al[65] | 2006 | 46 | 59 | 20 | 85 | 66 | 4 |
| Nomura et al[66] | 2006 | 16 | 35 | 20 | 94 | 65 | 6 |
| Foster et al[67] | 2008 | 24 | 41 | 20 | 92 | NA | 13 |
| Hoffman et al[68] | 2008 | 25 | 57 | 20 | 100 | 52 | 16 |
| Stienecker et al[69] | 2009 | 25 | 42 | 18 | 97 | 94 | 3 |
| Mueller et al[70] | 2010 | 55 | 23 | 18 | 95 | 76 | 2 |
| Thienpont et al[71] | 2010` | 138 | 84 | 18 | 97 | 76 | 3 |
| Scimeca et al[72] | 2011 | 37 | 90 | 20 | 84 | 89 | 0 |
| Gustavsson et al[51] | 2012 | 178 | 80 | 25 | 89 | 64 | 11 |
| Karstensen et al[73] | 2012 | 23 | 24 | 15 | 83 | 74 | 1.9 |
| De’Angelis et al[74] | 2013 | 26 | 52 | 18 | 100 | 93 | 2 |
| Endo et al[75] | 2013 | 30 | 36 | 20 | 94 | 64 | 10 |
| Honzawa et al[76] | 2013 | 25 | 21 | 20 | 88 | 62 | 12 |
| Nanda et al[77] | 2013 | 31 | 100 | 18 | 100 | 45 | 0 |
| Atreja et al[78] | 2014 | 128 | 48 | 20 | 83 | 67 | 3 |
| Bhalme et al[79] | 2014 | 79 | 61 | 20 | 95 | 77 | 0 |
| Hagel et al[80] | 2014 | 77 | 57 | 20 | 55 | 65 | 10 |
| Krauss et al[81] | 2014 | 20 | 25 | 18 | 100 | NA | 14 |
| Ding et al[82] | 2016 | 54 | 100 | 20 | 89 | 82 | 2 |
In the setting of small bowel strictures not in reach of the enteroscope or colonoscope, the double balloon enteroscope can be used in an antegrade or retrograde fashion for diagnostic and/or therapeutic intervention[15]. Although there are only a few small studies which have evaluated its use in dilating small bowel CD strictures, the results were positive[18,19]. Nishida et al[20] performed a retrospective review on their center’s experience with dilating small bowel strictures between 2006 to 2015. Overall, small bowel dilation using the double balloon enteroscope was found to be successful but there was a greater risk for requiring surgery in patients with multiple strictures as compared to those with a single stricture (adjusted hazard ratio, 14.94; 95%CI: 1.91-117.12; P = 0.010)[20]. As such, a single stricture but not necessarily multiple strictures may be a good indication for considering dilation using the double balloon enteroscope.
Factors that are predictive of a successful EBD include short straight strictures in-line with the bowel lumen distal to the duodenum, which are non-ulcerated in a location without any adjacent abscess and at least 5 cm from a fistula orifice[21,22]. Strictures located in the duodenum were found to have a 5 fold increased hazard for time to shorter surgery as compared to strictures located in the jejunum/ileum or colon (HR = 4.7, P = 0.038; HR = 5.6, P = 0.03; respectively)[23]. Additionally, a stricture length ≤ 5 cm was associated with a lower chance of requiring surgical intervention following EBD (HR = 2.5, 95%CI: 1.4-4.4; P = 0.002). For every 1 cm increase in stricture length, the risk for surgery increased by 8% (P = 0.005)[23]. In contrast to popular belief, anastomotic strictures have been associated with poorer short-term outcomes than de novo strictures[23,24]. This was highlighted in the aforementioned review by Bettenworth et al[14] which documented a lower technical success rate for post-surgical strictures as compared to native strictures (OR = 2.3, P < 0.001). Similarly, a recent study published by the Cleveland Clinic group after performing a retrospective review on 307 patients who had undergone either EBD or surgical resection for an ileocolonic anastomotic stricture had worse short-term outcomes (i.e., technical success) but similar long-term outcomes as compared to the aforementioned studies evaluating EBD of de novo strictures[24]. Of the 176 patients who had undergone EBD, the technical success rate was 86% (range 71% to 100%) with a long-term clinical efficacy, defined as an avoidance of surgery, of 58% over a follow-up period of 33 mo[24]. The presence of active inflammation identified on endoscopy, elevated CRP, medical treatment after dilation, cigarette smoking and intralesional steroid injection have demonstrated conflicting results with respect to the need for surgery and successful EBD[2,17,23,24].
Intralesional injection of steroids has been demonstrated to be effective for peptic, corrosive, anastomotic or post-radiotherapy fibrotic strictures[25]. However, strong evidence for the use of intralesional injection of steroids in CD is lacking[25-28]. Studies that have evaluated its use in CD have used the formulation triamcinolone due to its rapid onset of action and long-lasting duration of effectiveness of 3-4 wk[29]. Only two small randomized placebo controlled studies have been performed evaluating the use of intralesional steroids versus saline injection after failing medical therapy and EBD. The first study conducted in 2007, included 13 adult patients with short (≤ 5 cm) ileocolonic anastomotic strictures[30]. Five of the seven patients in the intervention group required re-dilation after the procedure and one patient had a complication versus one of six in the placebo group required re-dilation. There was no significant difference with respect to success of the procedure between groups[30]. This trial was stopped early due to the trend toward harm and remains the influential study behind the current American College of Gastroenterology and British Society of Gastroenterology position statements against the routine use of intralesional steroids[31,32]. The second study published in 2010 included 29 pediatric patients with short ileal or colonic strictures (12 anastomotic, 17 de novo)[33]. In contrast, this study did demonstrate a reduction in time to re-dilation and surgery in the intervention group. Within the sub-group of patients evaluated in a recent large systematic review evaluating the management of CD strictures, intralesional steroid injection did not improve outcomes[33]. Similarly, a review conducted in 2013 summarizing the findings from five retrospective case-series evaluating the use of intralesional steroids in CD patients concluded the data to be contradictory and limited[34].
Although controversial, intralesional injection of anti-tumor necrosis factor has been evaluated in patients with small bowel and colonic CD strictures with promising results, but concerns related to immunization may limit its potential as a therapeutic option[35,36]. One small case series evaluated the effect of a 90-120 mg intralesional injection of infliximab in three symptomatic patients with colonic CD strictures. All three patients had an improved endoscopic appearance of the stricture as well as relief of their obstructive symptoms for at least four months following the injection[35]. Similarly, another small case series evaluating intralesional injections of 40 mg of infliximab into small bowel CD strictures combined with EBD in six patients was associated with improved symptoms and a reduction in their modified simple endoscopic score for Crohn’s disease (SES-CD)[37]. The results of a larger randomized controlled trial evaluating the efficacy of performing intralesional injections of adalimumab into intestinal CD strictures are awaited[38].
Endoscopic metal stent insertion has been attempted in few patients with CD strictures. Although the technical success rate has been reportedly high, major complications such as bowel perforation, stent migration and fistulization was reported in 67% of patients[39]. Additionally, in order to avoid stent impaction, most studies suggest removing the stent after one month[40-42]. One small prospective cohort study concluded the risk for complications was too high to suggest the use of endoscopic metal stents as a treatment option for CD strictures after evaluating the data from 11 patients at their center[40]. The use of biodegradable instead of metal stents has been evaluated recently in a case-series last year involving six patients with intestinal and colonic CD strictures. Although technical success was good, premature stent failure occurred in all of the patients[43].
Although EBD is a minimally invasive procedure, bowel perforation and severe bleeding has been reported in most large studies[17,23,24]. In the aforementioned review by Bettenworth et al[14], major complications requiring hospitalization occurred in 2.8% of patients. Similarly, another large systematic review evaluating 24 non-randomized studies including 1163 patients found the rate of iatrogenic perforation to be 3%[44]. The rate for major complications including infection and hemorrhage in this study was 4%[44]. In a study directly comparing EBD to surgical intervention for the management of intestinal CD strictures, perforation occurred in 1.1% of the patients in the EBD group whereas the post-operative complication rate (e.g., intra-abdominal sepsis) was 8.8%[24]. Despite these significant complications, no deaths have been reported to date. Since benign or inflammatory intestinal strictures are indistinguishable from early adenocarcinoma on imaging, there exists a risk that malignancy may be missed when EBD is performed instead of surgical excision[3]. Population based studies have suggested a greater risk for small bowel malignancy in patients with longstanding CD. Several case reports exist documenting the development of small bowel malignancy following stricturoplasty and bypassed loops[45-51]. As such, biopsies of the stricture should occur prior to dilation[22]. There has been no evidence to suggest obtaining biopsies prior to EBD increases the risk for perforation.
EBD remains a safe and effective modality of treating CD strictures in appropriately selected patients. Although it may not be able to prevent operative management in all patients, it can significantly delay it. For an isolated intestinal fibrostenotic CD stricture less than or equal to 5 cm in length without adjacent fistulization or perforation, EBD should be considered as first-line therapy (Table 3).
| Predictors favoring successful dilation[11,22-25] | Symptomatic predominantly fibrotic stricture |
| Short (≤ 5 cm) stricture | |
| Single straight stricture | |
| Stricture distal to the duodenum | |
| Anastomotic stricture more favorable than de novo stricture | |
| First dilation | |
| Lack of a superimposed process contributing to symptoms (e.g., SIBO or IBS) | |
| Risk factors for complications[22-25] | Predominantly inflammatory stricture without medical optimization |
| Stricture greater than 5 cm | |
| Multiple small bowel strictures | |
| Strictures caused by extrinsic compression (e.g., adhesions) | |
| Fistulization within 5 cm of the area to be dilated | |
| Adjacent perforation or intra-abdominal collection | |
| Complete small bowel obstruction | |
| Tortuous or tethered small bowel or significant stricture angulation | |
| Duodenal stricture | |
| 1Short term outcome[15,18] | 85%-95% (technical success), 70%-80% (clinical response) |
| 2Long term outcome[15,18] | 32% (year 1 post dilation), 80% (year 5 post dilation) |
| 3Complication rate[25,45] | 1%-4% |
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Canada
Peer-review report classification
Grade A (Excellent): A, A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Gangl A, M’Koma A, Souza JL, Wittmann T S- Editor: Gong ZM L- Editor: A E- Editor: Huang Y
| 1. | Cosnes J, Cattan S, Blain A, Beaugerie L, Carbonnel F, Parc R, Gendre JP. Long-term evolution of disease behavior of Crohn’s disease. Inflamm Bowel Dis. 2002;8:244-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 981] [Cited by in RCA: 979] [Article Influence: 42.6] [Reference Citation Analysis (0)] |
| 2. | Rieder F, Zimmermann EM, Remzi FH, Sandborn WJ. Crohn’s disease complicated by strictures: a systematic review. Gut. 2013;62:1072-1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 388] [Article Influence: 32.3] [Reference Citation Analysis (0)] |
| 3. | Bettenworth D, Nowacki TM, Cordes F, Buerke B, Lenze F. Assessment of stricturing Crohn’s disease: Current clinical practice and future avenues. World J Gastroenterol. 2016;22:1008-1016. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 37] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 4. | Rieder F, Lawrance IC, Leite A, Sans M. Predictors of fibrostenotic Crohn’s disease. Inflamm Bowel Dis. 2011;17:2000-2007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 57] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 5. | Burke JP, Mulsow JJ, O’Keane C, Docherty NG, Watson RW, O’Connell PR. Fibrogenesis in Crohn’s disease. Am J Gastroenterol. 2007;102:439-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 219] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 6. | Shivananda S, Hordijk ML, Pena AS, Mayberry JF. Crohn’s disease: risk of recurrence and reoperation in a defined population. Gut. 1989;30:990-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 56] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Fiocchi C, Lund PK. Themes in fibrosis and gastrointestinal inflammation. Am J Physiol Gastrointest Liver Physiol. 2011;300:G677-G683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 87] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 8. | Graham MF, Diegelmann RF, Elson CO, Lindblad WJ, Gotschalk N, Gay S, Gay R. Collagen content and types in the intestinal strictures of Crohn’s disease. Gastroenterology. 1988;94:257-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 222] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 9. | Wells RG. The role of matrix stiffness in regulating cell behavior. Hepatology. 2008;47:1394-1400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 764] [Cited by in RCA: 761] [Article Influence: 44.8] [Reference Citation Analysis (0)] |
| 10. | Gionchetti P, Dignass A, Danese S, Magro Dias FJ, Rogler G, Lakatos PL, Adamina M, Ardizzone S, Buskens CJ, Sebastian S. 3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn’s Disease 2016: Part 2: Surgical Management and Special Situations. J Crohns Colitis. 2017;11:135-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 594] [Cited by in RCA: 530] [Article Influence: 66.3] [Reference Citation Analysis (0)] |
| 11. | Louis E, Collard A, Oger AF, Degroote E, Aboul Nasr El Yafi FA, Belaiche J. Behaviour of Crohn’s disease according to the Vienna classification: changing pattern over the course of the disease. Gut. 2001;49:777-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 684] [Cited by in RCA: 705] [Article Influence: 29.4] [Reference Citation Analysis (0)] |
| 12. | Cosnes J, Nion-Larmurier I, Beaugerie L, Afchain P, Tiret E, Gendre JP. Impact of the increasing use of immunosuppressants in Crohn’s disease on the need for intestinal surgery. Gut. 2005;54:237-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 499] [Cited by in RCA: 490] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 13. | Klag T, Wehkamp J, Goetz M. Endoscopic Balloon Dilation for Crohn’s Disease-Associated Strictures. Clin Endosc. 2017;50:429-436. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 14. | Bettenworth D, Gustavsson A, Atreja A, Lopez R, Tysk C, van Assche G, Rieder F. A Pooled Analysis of Efficacy, Safety, and Long-term Outcome of Endoscopic Balloon Dilation Therapy for Patients with Stricturing Crohn’s Disease. Inflamm Bowel Dis. 2017;23:133-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 177] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 15. | Tharian B, Caddy G, Tham TC. Enteroscopy in small bowel Crohn’s disease: A review. World J Gastrointest Endosc. 2013;5:476-486. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Hirai F. Current status of endoscopic balloon dilation for Crohn’s disease. Intest Res. 2017;15:166-173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Morar PS, Faiz O, Warusavitarne J, Brown S, Cohen R, Hind D, Abercrombie J, Ragunath K, Sanders DS, Arnott I, Wilson G, Bloom S, Arebi N; Crohn’s Stricture Study (CroSS) Group. Systematic review with meta-analysis: endoscopic balloon dilatation for Crohn’s disease strictures. Aliment Pharmacol Ther. 2015;42:1137-1148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 83] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 18. | Gill RS, Kaffes AJ. Small bowel stricture characterization and outcomes of dilatation by double-balloon enteroscopy: a single-centre experience. Therap Adv Gastroenterol. 2014;7:108-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 19. | Fukumoto A, Tanaka S, Yamamoto H, Yao T, Matsui T, Iida M, Goto H, Sakamoto C, Chiba T, Sugano K. Diagnosis and treatment of small-bowel stricture by double balloon endoscopy. Gastrointest Endosc. 2007;66:S108-S112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 88] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 20. | Nishida Y, Hosomi S, Yamagami H, Yukawa T, Nagami Y, Tanaka F, Kamata N, Tanigawa T, Shiba M, Watanabe T. Analysis of the Risk Factors of Surgery after Endoscopic Balloon Dilation for Small Intestinal Strictures in Crohn’s Disease Using Double-balloon Endoscopy. Intern Med. 2017;56:2245-2252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Chen M, Shen B. Endoscopic Therapy in Crohn’s Disease: Principle, Preparation, and Technique. Inflamm Bowel Dis. 2015;21:2222-2240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 55] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 22. | Rieder F, Latella G, Magro F, Yuksel ES, Higgins PD, Di Sabatino A, de Bruyn JR, Rimola J, Brito J, Bettenworth D. European Crohn’s and Colitis Organisation Topical Review on Prediction, Diagnosis and Management of Fibrostenosing Crohn’s Disease. J Crohns Colitis. 2016;10:873-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 197] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 23. | Bettenworth D, Rieder F. Medical therapy of stricturing Crohn’s disease: what the gut can learn from other organs - a systematic review. Fibrogenesis Tissue Repair. 2014;7:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 64] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 24. | Lian L, Stocchi L, Remzi FH, Shen B. Comparison of Endoscopic Dilation vs Surgery for Anastomotic Stricture in Patients With Crohn’s Disease Following Ileocolonic Resection. Clin Gastroenterol Hepatol. 2017;15:1226-1231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 59] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 25. | Nelson RS, Hernandez AJ, Goldstein HM, Saca A. Treatment of irradiation esophagitis. Value of hydrocortisone injection. Am J Gastroenterol. 1979;71:17-23. [PubMed] |
| 26. | Kochhar R, Poornachandra KS. Intralesional steroid injection therapy in the management of resistant gastrointestinal strictures. World J Gastrointest Endosc. 2010;2:61-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 54] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (1)] |
| 27. | Kochhar R, Makharia GK. Usefulness of intralesional triamcinolone in treatment of benign esophageal strictures. Gastrointest Endosc. 2002;56:829-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 120] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 28. | Ramage JI Jr, Rumalla A, Baron TH, Pochron NL, Zinsmeister AR, Murray JA, Norton ID, Diehl N, Romero Y. A prospective, randomized, double-blind, placebo-controlled trial of endoscopic steroid injection therapy for recalcitrant esophageal peptic strictures. Am J Gastroenterol. 2005;100:2419-2425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 160] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 29. | Roques C, Téot L. The use of corticosteroids to treat keloids: a review. Int J Low Extrem Wounds. 2008;7:137-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 105] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 30. | East JE, Brooker JC, Rutter MD, Saunders BP. A pilot study of intrastricture steroid versus placebo injection after balloon dilatation of Crohn’s strictures. Clin Gastroenterol Hepatol. 2007;5:1065-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 116] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 31. | Lichtenstein GR, Hanauer SB, Sandborn WJ; Practice Parameters Committee of American College of Gastroenterology. Management of Crohn’s disease in adults. Am J Gastroenterol. 2009;104:465-83; quiz 464, 484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 619] [Cited by in RCA: 591] [Article Influence: 36.9] [Reference Citation Analysis (0)] |
| 32. | Carter MJ, Lobo AJ, Travis SP; IBD Section, British Society of Gastroenterology. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2004;53 Suppl 5:V1-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 746] [Cited by in RCA: 772] [Article Influence: 36.8] [Reference Citation Analysis (0)] |
| 33. | Di Nardo G, Oliva S, Passariello M, Pallotta N, Civitelli F, Frediani S, Gualdi G, Gandullia P, Mallardo S, Cucchiara S. Intralesional steroid injection after endoscopic balloon dilation in pediatric Crohn’s disease with stricture: a prospective, randomized, double-blind, controlled trial. Gastrointest Endosc. 2010;72:1201-1208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 92] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 34. | Bevan R, Rees CJ, Rutter MD, Macafee DAL. Review of the use of intralesional steroid injections in the management of ileocolonic Crohn’s strictures. Frontline Gastroenterol. 2013;4:238-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 35. | Swaminath A, Lichtiger S. Dilation of colonic strictures by intralesional injection of infliximab in patients with Crohn’s colitis. Inflamm Bowel Dis. 2008;14:213-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 74] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 36. | Sorrentino D, Avellini C, Beltrami CA, Pasqual E, Zearo E. Selective effect of infliximab on the inflammatory component of a colonic stricture in Crohn’s disease. Int J Colorectal Dis. 2006;21:276-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 37. | Hendel J, Karstensen JG, Vilmann P. Serial intralesional injections of infliximab in small bowel Crohn’s strictures are feasible and might lower inflammation. United European Gastroenterol J. 2014;2:406-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 38. | ClinicalTrials. gov [Internet]. Bethesda (MD): National Library of Medicine (US) 2013; NCT01986127, A Randomized, Double-blinded, Placebo-controlled Study on the Effects of Adalimumab Intralesional Intestinal Strictures of Crohn's Disease Patients; [cited Dec 29, 2017] Available from: https://clinicaltrials.gov/ct2/show/study/NCT01986127 ClinicalTrials.gov. |
| 39. | Levine RA, Wasvary H, Kadro O. Endoprosthetic management of refractory ileocolonic anastomotic strictures after resection for Crohn’s disease: report of nine-year follow-up and review of the literature. Inflamm Bowel Dis. 2012;18:506-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 40. | Attar A, Maunoury V, Vahedi K, Vernier-Massouille G, Vida S, Bulois P, Colombel JF, Bouhnik Y; GETAID. Safety and efficacy of extractible self-expandable metal stents in the treatment of Crohn’s disease intestinal strictures: a prospective pilot study. Inflamm Bowel Dis. 2012;18:1849-1854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 66] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 41. | Branche J, Attar A, Vernier-Massouille G, Bulois P, Colombel JF, Bouhnik Y, Maunoury V. Extractible self-expandable metal stent in the treatment of Crohn’s disease anastomotic strictures. Endoscopy. 2012;44 Suppl 2 UCTN:E325-E326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 42. | Loras C, Pérez-Roldan F, Gornals JB, Barrio J, Igea F, González-Huix F, González-Carro P, Pérez-Miranda M, Espinós JC, Fernández-Bañares F. Endoscopic treatment with self-expanding metal stents for Crohn’s disease strictures. Aliment Pharmacol Ther. 2012;36:833-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 72] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 43. | Karstensen JG, Christensen KR, Brynskov J, Rønholt C, Vilmann P, Hendel J. Biodegradable stents for the treatment of bowel strictures in Crohn’s disease: technical results and challenges. Endosc Int Open. 2016;4:E296-E300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 44. | Navaneethan U, Lourdusamy V, Njei B, Shen B. Endoscopic balloon dilation in the management of strictures in Crohn’s disease: a systematic review and meta-analysis of non-randomized trials. Surg Endosc. 2016;30:5434-5443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 100] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 45. | Menon AM, Mirza AH, Moolla S, Morton DG. Adenocarcinoma of the small bowel arising from a previous strictureplasty for Crohn’s disease: report of a case. Dis Colon Rectum. 2007;50:257-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 46. | Partridge SK, Hodin RA. Small bowel adenocarcinoma at a strictureplasty site in a patient with Crohn’s disease: report of a case. Dis Colon Rectum. 2004;47:778-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 47. | Barwood N, Platell C. Case report: adenocarcinoma arising in a Crohn’s stricture of the jejunum. J Gastroenterol Hepatol. 1999;14:1132-1134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 48. | Jaskowiak NT, Michelassi F. Adenocarcinoma at a strictureplasty site in Crohn’s disease: report of a case. Dis Colon Rectum. 2001;44:284-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 46] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 49. | Collier PE, Turowski P, Diamond DL. Small intestinal adenocarcinoma complicating regional enteritis. Cancer. 1985;55:516-521. [PubMed] |
| 50. | Ribeiro MB, Greenstein AJ, Heimann TM, Yamazaki Y, Aufses AH Jr. Adenocarcinoma of the small intestine in Crohn’s disease. Surg Gynecol Obstet. 1991;173:343-349. [PubMed] |
| 51. | Gustavsson A, Magnuson A, Blomberg B, Andersson M, Halfvarson J, Tysk C. Endoscopic dilation is an efficacious and safe treatment of intestinal strictures in Crohn’s disease. Aliment Pharmacol Ther. 2012;36:151-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 100] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 52. | Blomberg B, Rolny P, Järnerot G. Endoscopic treatment of anastomotic strictures in Crohn’s disease. Endoscopy. 1991;23:195-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 95] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 53. | Williams AJ, Palmer KR. Endoscopic balloon dilatation as a therapeutic option in the management of intestinal strictures resulting from Crohn’s disease. Br J Surg. 1991;78:453-454. [PubMed] |
| 54. | Breysem Y, Janssens JF, Coremans G, Vantrappen G, Hendrickx G, Rutgeerts P. Endoscopic balloon dilation of colonic and ileo-colonic Crohn’s strictures: long-term results. Gastrointest Endosc. 1992;38:142-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 80] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 55. | Couckuyt H, Gevers AM, Coremans G, Hiele M, Rutgeerts P. Efficacy and safety of hydrostatic balloon dilatation of ileocolonic Crohn’s strictures: a prospective longterm analysis. Gut. 1995;36:577-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 143] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 56. | Ramboer C, Verhamme M, Dhondt E, Huys S, Van Eygen K, Vermeire L. Endoscopic treatment of stenosis in recurrent Crohn’s disease with balloon dilation combined with local corticosteroid injection. Gastrointest Endosc. 1995;42:252-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 83] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 57. | Matsui T, Ikeda K, Tsuda S, Yao K, Sou S, Satoh S, Hatakeyama S, Matake H, Sakurai T, Yao T. Long-term outcome of endoscopic balloon dilation in obstructive gastrointestinal Crohn’s disease: a prospective long-term study. Diagn Ther Endosc. 2000;6:67-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 58. | Dear KL, Hunter JO. Colonoscopic hydrostatic balloon dilatation of Crohn’s strictures. J Clin Gastroenterol. 2001;33:315-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 60] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 59. | Brooker JC, Beckett CG, Saunders BP, Benson MJ. Long-acting steroid injection after endoscopic dilation of anastomotic Crohn’s strictures may improve the outcome: a retrospective case series. Endoscopy. 2003;35:333-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 107] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 60. | Morini S, Hassan C, Lorenzetti R, Zullo A, Cerro P, Winn S, Giustini M, Taggi F. Long-term outcome of endoscopic pneumatic dilatation in Crohn’s disease. Dig Liver Dis. 2003;35:893-897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 49] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 61. | Sabaté JM, Villarejo J, Bouhnik Y, Allez M, Gornet JM, Vahedi K, Modigliani R, Lémann M. Hydrostatic balloon dilatation of Crohn’s strictures. Aliment Pharmacol Ther. 2003;18:409-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 73] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 62. | Thomas-Gibson S, Brooker JC, Hayward CM, Shah SG, Williams CB, Saunders BP. Colonoscopic balloon dilation of Crohn’s strictures: a review of long-term outcomes. Eur J Gastroenterol Hepatol. 2003;15:485-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 63. | Singh VV, Draganov P, Valentine J. Efficacy and safety of endoscopic balloon dilation of symptomatic upper and lower gastrointestinal Crohn’s disease strictures. J Clin Gastroenterol. 2005;39:284-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 113] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 64. | Ajlouni Y, Iser JH, Gibson PR. Endoscopic balloon dilatation of intestinal strictures in Crohn’s disease: safe alternative to surgery. J Gastroenterol Hepatol. 2007;22:486-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 65. | Ferlitsch A, Reinisch W, Püspök A, Dejaco C, Schillinger M, Schöfl R, Pötzi R, Gangl A, Vogelsang H. Safety and efficacy of endoscopic balloon dilation for treatment of Crohn’s disease strictures. Endoscopy. 2006;38:483-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 79] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 66. | Nomura E, Takagi S, Kikuchi T, Negoro K, Takahashi S, Kinouchi Y, Hiwatashi N, Shimosegawa T. Efficacy and safety of endoscopic balloon dilation for Crohn’s strictures. Dis Colon Rectum. 2006;49:S59-S67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 67. | Foster EN, Quiros JA, Prindiville TP. Long-term follow-up of the endoscopic treatment of strictures in pediatric and adult patients with inflammatory bowel disease. J Clin Gastroenterol. 2008;42:880-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 68. | Hoffmann JC, Heller F, Faiss S, von Lampe B, Kroesen AJ, Wahnschaffe U, Schulzke JD, Zeitz M, Bojarski C. Through the endoscope balloon dilation of ileocolonic strictures: prognostic factors, complications, and effectiveness. Int J Colorectal Dis. 2008;23:689-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 58] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 69. | Stienecker K, Gleichmann D, Neumayer U, Glaser HJ, Tonus C. Long-term results of endoscopic balloon dilatation of lower gastrointestinal tract strictures in Crohn’s disease: a prospective study. World J Gastroenterol. 2009;15:2623-2627. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 47] [Cited by in RCA: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 70. | Mueller T, Rieder B, Bechtner G, Pfeiffer A. The response of Crohn’s strictures to endoscopic balloon dilation. Aliment Pharmacol Ther. 2010;31:634-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 72] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 71. | Thienpont C, D’Hoore A, Vermeire S, Demedts I, Bisschops R, Coremans G, Rutgeerts P, Van Assche G. Long-term outcome of endoscopic dilatation in patients with Crohn’s disease is not affected by disease activity or medical therapy. Gut. 2010;59:320-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 129] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 72. | Scimeca D, Mocciaro F, Cottone M, Montalbano LM, D’Amico G, Olivo M, Orlando R, Orlando A. Efficacy and safety of endoscopic balloon dilation of symptomatic intestinal Crohn’s disease strictures. Dig Liver Dis. 2011;43:121-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 64] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 73. | Karstensen JG, Hendel J, Vilmann P. Endoscopic balloon dilatation for Crohn’s strictures of the gastrointestinal tract is feasible. Dan Med J. 2012;59:A4471. [PubMed] |
| 74. | de’Angelis N, Carra MC, Borrelli O, Bizzarri B, Vincenzi F, Fornaroli F, De Caro G, de’Angelis GL. Short- and long-term efficacy of endoscopic balloon dilation in Crohn’s disease strictures. World J Gastroenterol. 2013;19:2660-2667. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 39] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 75. | Endo K, Takahashi S, Shiga H, Kakuta Y, Kinouchi Y, Shimosegawa T. Short and long-term outcomes of endoscopic balloon dilatation for Crohn’s disease strictures. World J Gastroenterol. 2013;19:86-91. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 53] [Cited by in RCA: 51] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 76. | Honzawa Y, Nakase H, Matsuura M, Higuchi H, Toyonaga T, Matsumura K, Yoshino T, Okazaki K, Chiba T. Prior use of immunomodulatory drugs improves the clinical outcome of endoscopic balloon dilation for intestinal stricture in patients with Crohn’s disease. Dig Endosc. 2013;25:535-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 77. | Nanda K, Courtney W, Keegan D, Byrne K, Nolan B, O’Donoghue D, Mulcahy H, Doherty G. Prolonged avoidance of repeat surgery with endoscopic balloon dilatation of anastomotic strictures in Crohn’s disease. J Crohns Colitis. 2013;7:474-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 78. | Atreja A, Aggarwal A, Dwivedi S, Rieder F, Lopez R, Lashner BA, Brzezinski A, Vargo JJ, Shen B. Safety and efficacy of endoscopic dilation for primary and anastomotic Crohn’s disease strictures. J Crohns Colitis. 2014;8:392-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 77] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 79. | Bhalme M, Sarkar S, Lal S, Bodger K, Baker R, Willert RP. Endoscopic balloon dilatation of Crohn’s disease strictures: results from a large United kingdom series. Inflamm Bowel Dis. 2014;20:265-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 80. | Hagel AF, Hahn A, Dauth W, Matzel K, Konturek PC, Neurath MF, Raithel M. Outcome and complications of endoscopic balloon dilatations in various types of ileocaecal and colonic stenosis in patients with Crohn’s disease. Surg Endosc. 2014;28:2966-2972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 81. | Krauss E, Agaimy A, Gottfried A, Maiss J, Weidinger T, Albrecht H, Hartmann A, Hohenberger W, Neurath MF, Kessler H. Long term follow up of through-the-scope balloon dilation as compared to strictureplasty and bowel resection of intestinal strictures in crohn’s disease. Int J Clin Exp Pathol. 2014;7:7419-7431. [PubMed] |
| 82. | Ding NS, Yip WM, Choi CH, Saunders B, Thomas-Gibson S, Arebi N, Humphries A, Hart A. Endoscopic Dilatation of Crohn’s Anastomotic Strictures is Effective in the Long Term, and Escalation of Medical Therapy Improves Outcomes in the Biologic Era. J Crohns Colitis. 2016;10:1172-1178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |