Published online Jan 7, 2018. doi: 10.3748/wjg.v24.i1.69
Peer-review started: October 30, 2017
First decision: November 21, 2017
Revised: December 2, 2017
Accepted: December 12, 2017
Article in press: December 12, 2017
Published online: January 7, 2018
Processing time: 69 Days and 6 Hours
To study the safety of insertion of metallic stents in elderly patients with unresectable distal malignant biliary obstruction.
Of 272 patients with unresectable distal malignant biliary obstruction, 184 patients under the age of 80 were classified into Group A, and 88 subjects aged 80 years or more were classified into Group B. The safety of metallic stent insertion, metal stent patency period, and the obstruction rate were examined in each group.
In Group B, patients had a significantly worse performance status, high blood pressure, heart disease, cerebrovascular disease, and dementia; besides the rate of patients orally administered antiplatelet drugs or anticoagulants tended to be higher (P < 0.05). Metallic stents were successfully inserted in all patients. The median patency period was 265.000 ± 26.779 (1-965) d; 252.000 ± 35.998 (1-618) d in Group A and 269.000 ± 47.885 (1-965) d in Group B, with no significant difference between the two groups. Metallic stent obstruction occurred in 82 of the 272 (30.15%) patients; in 53/184 (28.80%) patients in Group A and in 29/88 (32.95%) of those in Group B, showing no significant difference between the two groups. Procedural accidents due to metal stent insertion occurred in 24/272 (8.8%) patients; in 17/184 (9.2%) of patients in Group A and in 7/88 (8.0%) of those in Group B, with no significant difference between the two groups, either.
These results suggested that metallic stents can be safely inserted to treat unresectable distal malignant biliary obstruction even in elderly patients aged 80 years or more.
Core tip: It was suggested that metallic stent insertion for unresectable distal malignant biliary obstruction in the elderly can be conducted safely and with a high success rate, without any significant difference in the occurrence of procedural accidents when compared with the non-elderly group, even though the elderly tend to have more underlying diseases.
- Citation: Sakai Y, Iwai T, Shimura K, Gon K, Koizumi K, Ijima M, Chiba K, Nakatani S, Sugiyama H, Tsuyuguchi T, Kamisawa T, Maetani I, Kida M. Safety and efficacy of metallic stent for unresectable distal malignant biliary obstruction in elderly patients. World J Gastroenterol 2018; 24(1): 69-75
- URL: https://www.wjgnet.com/1007-9327/full/v24/i1/69.htm
- DOI: https://dx.doi.org/10.3748/wjg.v24.i1.69
Endoscopic retrograde cholangiopancreatography (ERCP) related procedure is a minimally invasive diagnostic and therapeutic method for biliary and pancreatic diseases and plays a very important role. As for biliary drainage, endoscopic drainage by ERCP is considered to be noninvasive and the first choice of treatment[1,2]. Either plastic or metallic stents are used in endoscopic drainage for patients with unresectable malignant biliary obstruction. However, it is desirable to use a metallic stent because of its long patency period and low obstruction rate, which reduce the need for retreatment and the total treatment cost[1-4]. It is considered that metallic stents can be safely inserted in patients with unresectable malignant biliary obstruction, they are useful and the drainage effect is excellent[5-8]. Yet, to our knowledge, there are no reports that examined the safety of insertion of metallic stents in the elderly with an unresectable malignant biliary obstruction. Therefore, we studied the safety and usefulness of metallic stents for unresectable distal malignant biliary obstruction in a multicenter, collaborative, retrospective study.
There were 272 patients diagnosed with unresectable distal malignant biliary obstruction, at the 7 institutions participating in this study, from January 2012 to July 2016. Metallic stents were inserted transpapillary using the ERCP route. In all patients, endoscopic sphincterotomy (EST) was performed previous to metal stent insertion. The metallic stent used was BONA stent (Sewoon Medical Co., Ltd. Delivery system, 8Fr., 10 mm diameter, fully covered stent). Inclusion criteria were: (1) written informed consent for the study obtained previous to the endoscopic treatment; (2) patients aged 20 years or more; (3) patients hospitalized on ERCP day who could be followed for one week after ERCP; (4) patients not subjected to stomach reconstruction with Billroth II method or Roux-en Y anastomosis; (5) patients who could orally administered antiplatelet drugs or anticoagulants, and could discontinue drug treatment for one week before and after ERCP or EST; and (6) patients with a platelet count of 50000/mL or more, and PT-INR 1.5 or less. Exclusion criteria were (1) patients whose medical record could not be reviewed after treatment; and (2) other patients who were judged as inappropriate by the investigator. There were 157 men and 115 women, whose mean age was 74.165 ± 11.649 (44-96) years. The disease was pancreatic cancer in 208 patients, bile duct cancer in 30, metastatic biliary obstruction in 16, duodenal papillary carcinoma in 9, gallbladder cancer in 7, hepatocellular carcinoma in 1, and intraductal papillary mucinous carcinoma in 1 patient. Hepatic metastasis was found in 56 patients and ascites retention in 68 patients. Duodenal stenosis was detected in 40 patients and a duodenal stent was inserted in all patients. In 250 patients the diagnosis of malignancy was established by pathological examination, and in the remaining patients imaging techniques and clinical course. The bile duct diameter prior to drainage was 12.093 ± 3.336 (4-23) mm, and the stenosis length prior to the drainage was 27.276 ± 12.683 (5-59) mm. The result of hepatobiliary enzyme tests prior to the drainage was ALT 141.139 ± 105.309 (29-851) IU/L, ALP 1498.163 ± 1248.051 (409-2620) IU/L, and T-Bil 5.388 ± 6.203 (0.4-27.8) mg/dL. Performance status (PS) determined according to the criteria of the Eastern Cooperative Oncology Group was 0 in 80 patients, 1 in 10 patients, 2 in 56 patients, 3 in 66 patients and 4 in 60 patients. Underlying diseases included high blood pressure in 107 patients, diabetes mellitus in 81 patients, hyperlipidemia in 26 patients, chronic lung disease in 43 patients, heart disease in 38 patients, chronic liver disease in 24 patients, chronic kidney disease in 13 patients, cerebrovascular disease in 25 patients, and dementia in 25 patients; and there were 32 patients who were administered antiplatelet drugs or anticoagulants. Chemotherapy was carried out in 121 patients based on judgment by the attending physician. The judgment of therapeutic effect was made after 2 courses of chemotherapy. In patients for whom chemotherapy could not be continued before conducting 2 courses, the effect was judged at that time. Chemotherapy effect was judged using RECIST criteria[9]. At the time of effect judgment, complete response: CR was defined as disappearance of all target lesions, and regarding lymph node involvement, this was defined as reduction of the shorter diameter to less than 10 mm. Partial response: PR was defined as reduction by more than 30% compared to the sum of total target lesion diameter at the baseline. Stable disease: SD was defined as no reduction corresponding to PR and no progress corresponding to PD. Progressive disease: PD was defined as an increase by 20% or more and an increase in absolute value by 5 mm or more when compared with the sum of the minimum diameter of the target lesion during the course. Patients under 80 years of age were classified into Group A and patients aged 80 or more into Group B. The safety of metallic stent insertion, patency period after metallic stent insertion, obstruction rate, and success rate of metallic stent insertion were examined and compared between the two groups. Early procedural accidents occurring in ERCP-related procedures were evaluated using Cotton’s classification[10]. All treatments were carried out with the patient’s or patient’s family informed consent, and a signed consent form was obtained. This study was conducted with the approval of the ethics committee of each participating facility.
Person χ2 test with Yates correction and Fisher’s exact test, when appropriate, were used for statistical analysis of categorical variables. Stent patency and patient survival time were estimated using the Kaplan-Meier method, and the log-rank test was used to access differences between the groups. Data were analyzed using SPSS software version 11 (SPSS, Chicago, IL, United States). Differences with a P value of < 0.05 were considered statistically significant.
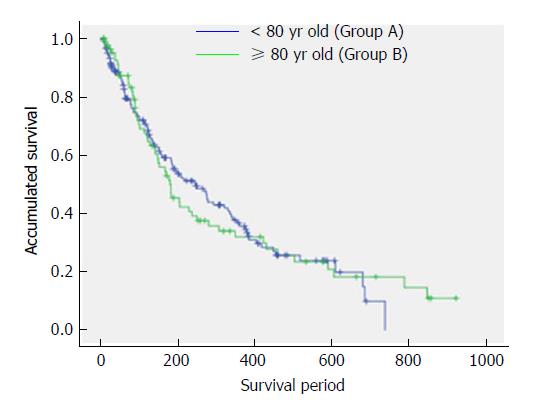
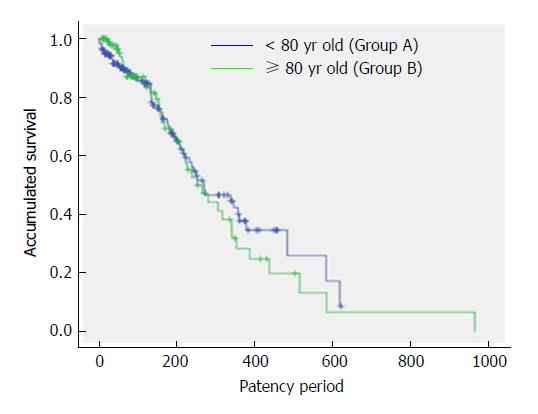
The patient background data is shown in Table 1. In Group B there were significantly more patients with high blood pressure, heart disease, cerebrovascular disease, and dementia, as well as more patients taking antiplatelet drugs or anticoagulants. PS tended to be significantly worse in Group B, and fewer patients were subjected to chemotherapy in this group. Other factors did not show a significant difference between Group A and Group B. The results on treatment are shown in Table 2. The success rate of metallic stent insertion was 100% (272/272). The drainage effect after insertion of the metal stent was ALT 70.375 ± 123.860 (10-278) IU/L, ALP 768.400 ± 70.181 (326-1855) IU/L, and T-Bil 1.944 ± 2.873 (0.4-12.2) mg/dL, showing significant reduction (P < 0.05). There was no significant difference of ALT, ALP and T- Bil values after the drainage between Group A and Group B, and drainage was excellent. Chemotherapy was conducted more frequently in Group A and best supportive care was more frequently employed in Group B. As for the effect of chemotherapy, CR was achieved in 0% (0/121), PR in 13.2% (16/121), SD in 70.2% (85/121), and PD in 16.5% (20/121) of the patients, with a success rate of 13.2% (16/121). Prior to conducting 2 courses of chemotherapy, PD was observed in 8.3% (10/121) of the patients, thus it was not possible to continue with the treatment. In Group A, the number of patients with SD tended to be significantly higher. The median of survival period was 205.000 ± 21.801 (7-999) d. The median of survival period was 246.000 ± 36.056 (7-738) d in Group A and 180.000 ± 25.724 (7-999) d in Group B, showing no significant difference (Figure 1). The median patency period was 265.000 ± 26.779 (1-965) d; 252.000 ± 35.998 (1-618) d in Group A and 269.000 ± 47.885 (1-965) d in Group B, with no significant difference (Figure 2). Stent obstruction occurred in 30.15% (82/272) of the patients during the follow-up period. The cause of stent obstruction included overgrowth in 6.3% (17/272), ingrowth in 2.2% (6/272), sludge in 9.6% (26/272), migration in 8.5% (23/272), food impaction in 2.6% (7/272), and others in 1.1% (3/272). Stent obstruction occurred in 28.80% (53/184) of patients in Group A, and in 32.95% (29/88) of those in Group B with no significant difference between the two groups. There was no significant difference between Group A and Group B regarding the cause-specific obstruction rate (Table 3). Early procedural accidents due to ERCP related procedures were observed in 8.8% (24/272) of the patients. Early procedural accidents included pancreatitis in 2.9% (8/272, mild 8), cholecystitis in 3.7% (10/272, mild 8, moderate 2), cholangitis in 1.1% (3/272 mild 3), stent migration in 0.4% (1/272), and pneumonia in 0.7% (2/272). As shown in Table 4, there was no significant difference in the incidence of procedural accidents between Group A and Group B, whereas the onset of pancreatitis showed a significantly lower tendency in Group B: 0.01% (1/88) when compared with in Group A: 3.8% (7/184). All procedural accidents resolved without requiring a surgical procedure.
| < 80 yr old (Group A) | ≥ 80 yr old (Group B) | P value | |
| Number of patients | 184 | 88 | |
| Male | 105 | 52 | NS |
| Female | 79 | 36 | NS |
| Pancreatic cancer | 136 | 72 | NS |
| Bile duct cancer | 21 | 9 | NS |
| Metastatic biliary obstruction | 13 | 3 | NS |
| Papilla vater cancer | 6 | 3 | NS |
| Gallbladder cancer | 6 | 1 | NS |
| Intraductal papillary mucinous carcinoma | 1 | 0 | NS |
| Hepatocellular carcinoma | 1 | 0 | NS |
| Hepatic metastasis | 40 | 16 | NS |
| Ascites | 45 | 23 | NS |
| Duodenal stent indwelling | 30 | 10 | NS |
| Pathological diagnosis | 161 | 89 | NS |
| Performance status | |||
| 0 | 72 | 8 | 0.0000 |
| 1 | 7 | 3 | NS |
| 2 | 44 | 12 | 0.018 |
| 3 | 29 | 37 | 0.0004 |
| 4 | 32 | 28 | 0.0064 |
| Chemotherapy | 106 | 15 | 0.0000 |
| Hypertension | 55 | 52 | 0.0002 |
| Hyperlipidemia | 20 | 6 | NS |
| Diabetes mellitus | 50 | 31 | NS |
| Chronic respiratory disease | 25 | 18 | NS |
| Cardiac disease | 18 | 20 | 0.0065 |
| Chronic liver disease | 18 | 6 | NS |
| Chronic renal disease | 10 | 3 | NS |
| Cerebrovascular disease | 5 | 20 | 0.0000 |
| Dementia | 5 | 20 | 0.0000 |
| Anticoagulant/antiplatelet | 9 | 23 | 0.0270 |
| Drainage effect | < 80 yr old (Group A; n = 184) | ≥ 80 yr old (Group B; n = 88) | P value |
| Bile duct diameter prior to drainage (mm) | 11.350 ± 3.6310 (4-23) | 12.819 ± 3.3148 (5-22) | NS |
| Stenosis length prior to drainage (mm) | 27.216 ± 12.688 (5-59) | 27.292 ± 12.702(6-52) | NS |
| ALT prior to drainage (IU/L) | 162.767 ± 104.768 (29-851) | 127.567 ± 104.760(30-838) | NS |
| ALT post drainage (IU/L) | 78.875 ± 159.482 (10-278) | 66.039 ± 143.106 (13-270) | NS |
| ALP prior to drainage (IU/L) | 1529.375 ± 1465.465 (409-2620) | 1489.447 ± 1102.192 (432-2512) | NS |
| ALP post drainage (IU/L) | 871.000 ± 803.131 (326-1855) | 665.622 ± 557.643 (331-1811) | NS |
| T-Bil prior to drainage (mg/dl) | 5.438 ± 6.512 (0.4-27.8) | 5.276 ± 5.858 (0.6-27) | NS |
| T-Bil post drainage (mg/dl) | 2.387 ± 3.879 (0.4-12.2) | 1.580 ± 3.943 (0.6-12) | NS |
| Chemotherapeutic effect | |||
| CR | 0 | 0 | NS |
| PR | 12 | 4 | NS |
| SD | 78 | 7 | 0.0000 |
| PD | 16 | 4 | NS |
| Total | 106 | 15 | 0.0000 |
| Best supportive care | 78 | 73 | 0.0000 |
| Related complications | < 80 yr old(Group A; n = 184) | ≥ 80 yr old(Group B; n = 88) | P value |
| Overgrowth | 10 | 7 | NS |
| Ingrowth | 6 | 0 | NS |
| Sludge | 16 | 10 | NS |
| Stent migration | 15 | 8 | NS |
| Food impaction | 3 | 4 | NS |
| Others | 3 | 0 | NS |
| Total | 53 | 29 | NS |
| Related complications | < 80 yr old(Group A; n = 184) | ≥ 80 yr old(Group B; n = 88) | P value |
| Bleeding | 0 | 0 | |
| Perforation | 0 | 0 | NS |
| Pancreatitis | 7 (mild) | 1 (mild) | 0.003 |
| Cholangitis | 1 (mild) | 2 (mild) | NS |
| Cholecystitis | 8 (6 mild, 2 moderate) | 2 (mild) | NS |
| Stent migration | 1 | 0 | NS |
| Pneumoniae | 0 | 2 | NS |
In medical care treatment should be safer and minimally invasive in consideration of the patient’s quality of life. ERCP related procedures can be carried out rather safely as they are minimally invasive and a reasonable treatment method for removal of a calculus from the common bile duct, or drainage in patients with obstructive jaundice. There are many reports indicating that ERCP related procedures can be safely performed even in the elderly[11-14]. However, sufficient attention is necessary because there also are reports describing that procedural accidents easily become serious once they occur[15]. In the present study we assessed the feasibility of metallic stent insertion in elderly patients with unresectable distal malignant biliary obstruction. The study was conducted because there have been no such reports so far. In general, elderly people tend to have various underlying diseases[11-15], and this study also showed that tendency. Although it is obvious that the patient condition is not so good in such a situation, we showed that a metal stent can be safely inserted even in the elderly. In this study, there was no significant difference in the survival period and the metallic stent patency period. In recent years, patient prognosis has improved thanks to advances in chemotherapy for pancreatic cancer and bile duct cancer[16-18]. There is a report showing that not only the survival period but also metal stent patency period is prolonged by chemotherapy for bile duct cancer[19]. However, in this study, no significant difference was found in the survival period and the patency period, though the number of patients who underwent chemotherapy in the elderly group was significantly small. The reason may be that the success rate of chemotherapy was low in this study. The success rate of metal stent insertion was 100% in both groups. Though it is a retrospective study, the success rate of transpapillary metallic stent insertion is generally high even in past reports[5-8]. Therefore, this result seems not to be a particularly good result. There was no significant difference in procedural accidents between the two groups, but the incidence of pancreatitis tended to be lower in Group B. The reason may be that in the elderly, pancreatic function is deteriorated, which lowers the possibility of developing pancreatitis[20]. In addition, pneumonia was observed in Group B but not in Group A. Since elderly people have sometimes reduced sputum excretion capacity, they may suffer from aspiration pneumonia. Therefore, especially for the elderly it was considered necessary to frequently conduct sputum aspiration during and after surgery. This study suggested that metallic stents can be safely inserted and are a useful treatment for unresectable distal malignant biliary obstruction in the elderly. However, since this was a retrospective, multicenter study, a prospective study is considered necessary in the future to further evaluate the feasibility and usefulness of this procedure in elderly patients.
In conclusion, it was suggested that metallic stent insertion for unresectable distal malignant biliary obstruction in the elderly can be conducted safely and with a high success rate, without any significant difference in the occurrence of procedural accidents when compared with the non-elderly group, even though the elderly tend to have more underlying diseases.
The related procedure of endoscopic retrograde cholangiopancreatography (ERCP) is a minimally invasive diagnostic and therapeutic method for biliary and pancreatic diseases and plays a very important role. As for biliary drainage, endoscopic drainage by ERCP is considered to be noninvasive and the first choice of treatment.
To our knowledge, there are no reports that examined the safety of insertion of metallic stents in the elderly with an unresectable malignant biliary obstruction. Therefore, we studied the safety and usefulness of metallic stents for unresectable distal malignant biliary obstruction in a multicenter, collaborative, retrospective study.
This study aims to evaluate the safety of insertion of metallic stents in elderly patients with unresectable distal malignant biliary obstruction.
There are total 272 patients with unresectable distal malignant biliary obstruction in this study. Group A (184 patients under the age of 80) and Group B (88 subjects aged 80 years or more) were examined by the safety of metallic stent insertion, metal stent patency period, and the obstruction rate.
In Group B, patients had a significantly worse performance status, high blood pressure, cerebrovascular disease, heart disease, and dementia; besides the rate of patients orally administered antiplatelet drugs or anticoagulants tended to be higher (P < 0.05). Metallic stents were successfully inserted in all patients. The median patency period was 265.000 ± 26.779 d (1-965); 252.000 ± 35.998 d (1-618) in Group A and 269.000 ± 47.885 d (1-965) in Group B, with no significant difference between the two groups. Metallic stent obstruction occurred in 30.15% (82/272) patients; in 28.80% (53/184) patients in Group A and in 32.95% (29/88) of those in Group B, showing no significant difference between the two groups.
This study suggested that metallic stents can be safely inserted and are a useful treatment for unresectable distal malignant biliary obstruction in the elderly. It was suggested that metallic stent insertion for unresectable distal malignant biliary obstruction in the elderly can be conducted safely and with a high success rate. We should insert metallic stent in unresectable distal malignant biliary obstruction in the elderly patients for improvement of quality of life positively.
A prospective study is considered necessary in the future to further evaluate the feasibility and usefulness of metallic stent for unresectable distal malignant biliary obstruction in elderly patients.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Huang LY, Lleo A S- Editor: Chen K L- Editor: A E- Editor: Huang Y
| 1. | Tsuyuguchi T, Takada T, Miyazaki M, Miyakawa S, Tsukada K, Nagino M, Kondo S, Furuse J, Saito H, Suyama M. Stenting and interventional radiology for obstructive jaundice in patients with unresectable biliary tract carcinomas. J Hepatobiliary Pancreat Surg. 2008;15:69-73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Miyazaki M, Yoshitomi H, Miyakawa S, Uesaka K, Unno M, Endo I, Ota T, Ohtsuka M, Kinoshita H, Shimada K. Clinical practice guidelines for the management of biliary tract cancers 2015: the 2nd English edition. J Hepatobiliary Pancreat Sci. 2015;22:249-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 165] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 3. | Isayama H, Yasuda I, Ryozawa S, Maguchi H, Igarashi Y, Matsuyama Y, Katanuma A, Hasebe O, Irisawa A, Itoi T. Results of a Japanese multicenter, randomized trial of endoscopic stenting for non-resectable pancreatic head cancer (JM-test): Covered Wallstent versus DoubleLayer stent. Dig Endosc. 2011;23:310-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 97] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 4. | Hong WD, Chen XW, Wu WZ, Zhu QH, Chen XR. Metal versus plastic stents for malignant biliary obstruction: an update meta-analysis. Clin Res Hepatol Gastroenterol. 2013;37:496-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 5. | Sakai Y, Tsuyuguchi T, Hirata N, Sugiyama H, Shimura K, Nakaji S, Shiratori T, Fujimoto T, Tsuchiya S, Mikami S. Long-term outcome of the WallFlex partially covered stent for unresectable malignant biliary obstruction: a multicenter single-arm prospective study. Hepatogastroenterology. 2013;60:1854-1860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Costamagna G, Tringali A, Reddy DN, Devière J, Bruno M, Ponchon T, Neuhaus H, Mutignani M, Rao GV, Lakhtakia S. A new partially covered nitinol stent for palliative treatment of malignant bile duct obstruction: a multicenter single-arm prospective study. Endoscopy. 2011;43:317-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Isayama H, Komatsu Y, Tsujino T, Sasahira N, Hirano K, Toda N, Nakai Y, Yamamoto N, Tada M, Yoshida H. A prospective randomised study of “covered” versus “uncovered” diamond stents for the management of distal malignant biliary obstruction. Gut. 2004;53:729-734. [PubMed] |
| 8. | Kullman E, Frozanpor F, Söderlund C, Linder S, Sandström P, Lindhoff-Larsson A, Toth E, Lindell G, Jonas E, Freedman J. Covered versus uncovered self-expandable nitinol stents in the palliative treatment of malignant distal biliary obstruction: results from a randomized, multicenter study. Gastrointest Endosc. 2010;72:915-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 221] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 9. | Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15860] [Cited by in RCA: 21602] [Article Influence: 1350.1] [Reference Citation Analysis (1)] |
| 10. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [PubMed] |
| 11. | Sakai Y, Tsuyuguchi T, Hirata N, Nakaji S, Shimura K, Fujimoto T, Tsuchiya S, Nishino T, Nishikawa T, Sugiyama H. Can endoscopic sphincterotomy be performed safely in elderly patients aged 80 years or older with pancreatic and biliary diseases? Hepatogastroenterology. 2013;60:1251-1256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Ito Y, Tsujino T, Togawa O, Yamamoto N, Isayama H, Nakata R, Kawabe T, Omata M. Endoscopic papillary balloon dilation for the management of bile duct stones in patients 85 years of age and older. Gastrointest Endosc. 2008;68:477-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Sugiyama M, Atomi Y. Endoscopic sphincterotomy for bile duct stones in patients 90 years of age and older. Gastrointest Endosc. 2000;52:187-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 81] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Sakai Y, Tsuyuguchi T, Sugiyama H, Sasaki R, Sakamoto D, Nakamura M, Watanabe Y, Nishikawa T, Yasui S, Mikata R. Endoscopic papillary large balloon dilation for bile duct stones in elderly patients. World J Clin Cases. 2015;3:353-359. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Nishikawa T, Tsuyuguchi T, Sakai Y, Sugiyama H, Sakamoto D, Nakamura M, Yokosuka O. Old age is associated with increased severity of complications in endoscopic biliary stone removal. Dig Endosc. 2014;26:569-576. [PubMed] |
| 16. | Okusaka T, Furuse J, Funakoshi A, Ioka T, Yamao K, Ohkawa S, Boku N, Komatsu Y, Nakamori S, Iguchi H. Phase II study of erlotinib plus gemcitabine in Japanese patients with unresectable pancreatic cancer. Cancer Sci. 2011;102:425-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 17. | Von Hoff DD, Ramanathan RK, Borad MJ, Laheru DA, Smith LS, Wood TE, Korn RL, Desai N, Trieu V, Iglesias JL. Gemcitabine plus nab-paclitaxel is an active regimen in patients with advanced pancreatic cancer: 1 phase I/II trial. J Clin Oncol. 2011;29:4548-4554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 755] [Cited by in RCA: 870] [Article Influence: 62.1] [Reference Citation Analysis (2)] |
| 18. | Sasaki T, Isayama H, Nakai Y, Takahara N, Sasahira N, Kogure H, Mizuno S, Yagioka H, Ito Y, Yamamoto N. Improvement of prognosis for unresectable biliary tract cancer. World J Gastroenterol. 2013;19:72-77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Kawamoto H, Tsutsumi K, Harada R, Fujii M, Kato H, Hirao K, Kurihara N, Nakanishi T, Mizuno O, Ishida E. Endoscopic deployment of multiple JOSTENT SelfX is effective and safe in treatment of malignant hilar biliary strictures. Clin Gastroenterol Hepatol. 2008;6:401-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |