Published online Dec 28, 2017. doi: 10.3748/wjg.v23.i48.8666
Peer-review started: September 14, 2017
First decision: September 27, 2017
Revised: October 5, 2017
Accepted: October 17, 2017
Article in press: October 17, 2017
Published online: December 28, 2017
Processing time: 104 Days and 21.5 Hours
In the “proton pump inhibitors era”, a penetrating peptic ulcer (PPU) represents an exceptional cause of abdominal pain, and was more frequently observed in the past where there was not an effective antacid treatment. Ulcer-induced pancreatitis is very rare, too, and manifests with persistent, intense pain radiating to the back. A mild to severe pancreatitis with peripancreatic fluid collection can be observed at imaging. However, only a few cases of association between PPU and emphysematous pancreatitis (EP) have been published in the literature. EP is a rare but potentially fatal form of acute necrotizing pancreatitis in which gas grows in and outside the pancreas, and typically involves the whole parenchyma in diabetic individuals.
Here we report an extremely rare case of a duodenal ulcer penetrating the pancreas and complicated with EP. Unlike the classic form of EP, which involves the whole parenchyma and has a poor prognosis, we found that the emphysematous involvement of the pancreas by PPU has a benign course if a conservative therapy is promptly established. Gas is confined to the site of penetration, usually the pancreatic head, and ulcers most often involve the duodenum.
Core tip: Penetrating peptic ulcers (PPU) represent an extremely rare cause of abdominal pain, and can sometimes manifest with mild to severe acute pancreatitis. However, only a few cases of association between PPU and emphysematous pancreatitis (EP) have been published so far in the literature. Here we report an extremely rare case of a duodenal ulcer penetrating the pancreas and complicated with EP. Unlike the classic form of EP, which involves the whole parenchyma and has a poor prognosis, we found that the focal emphysematous involvement of the pancreas by PPU has a benign clinical course if an appropriate therapy is promptly established.
- Citation: Tana C, Silingardi M, Giamberardino MA, Cipollone F, Meschi T, Schiavone C. Emphysematous pancreatitis associated with penetrating duodenal ulcer. World J Gastroenterol 2017; 23(48): 8666-8670
- URL: https://www.wjgnet.com/1007-9327/full/v23/i48/8666.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i48.8666
In the “proton pump inhibitors era”, a penetrating peptic ulcer (PPU) represents an exceptional cause of abdominal pain, and was more frequently observed in the past where there was not an effective antacid treatment. Ulcer-induced pancreatitis is very rare too, and manifests with persistent, intense pain radiating to the back[1-3]. A mild to severe pancreatitis with peripancreatic fluid collection can be observed at imaging[4]. However, only a few cases of association between PPU and emphysematous pancreatitis (EP) have been published in the literature, and complete information regarding epidemiology are unknown. Here we report an extremely rare case of a duodenal ulcer penetrating the pancreas and complicated with EP.
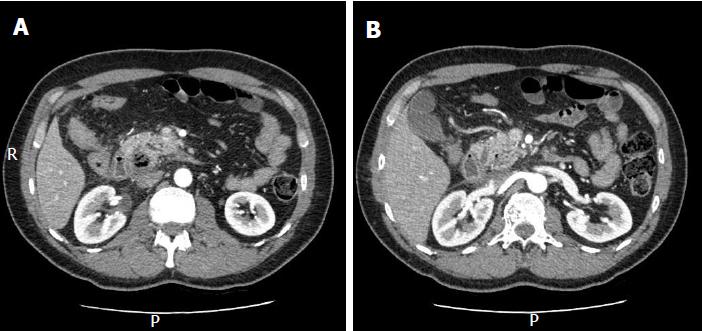
A 49-year-old man presented with an acute complaint of epigastric pain radiating to the back 30 min after an excessive intake of fried, high fat food. He also reported a daily intake of nonsteroidal anti-inflammatory drugs for low back pain for over a year. There was no history of alcohol consumption. Physical examination revealed fever (38 °C), abdominal rigidity, tenderness and torpid peristalsis. Laboratory exams showed an increase in erythrocyte sedimentation rate (46 mm/h), c-reactive protein (27.01 mg/dL), lipase (226 U/L), and leucocytosis with neutrophilia (20.1 and 18.4 × 103/μL, respectively). Hemoglobin, amylase and liver tests were normal. Procalcitonin was 1.45 ng/mL. Abdominal X-ray was negative. Ultrasound (US) did not reveal gallstones or free fluids; bile ducts were not dilated. Pancreas was not evaluable due to meteorism. Blood cultures were collected. Abdominal contrast-enhanced computed tomography (CECT) showed the presence of gas within the pancreatic head, suggestive of focal EP (Figure 1A), and oedema of the duodenum (Figure 1B). There was no free air suggestive of perforation. Clinical examination, laboratory tests and imaging did not reveal signs of obstructive jaundice; there was therefore no indication for an early endoscopic retrograde cholangiopancreatography. The mild oedema of the duodenum in close relation to the damaged pancreas suggested a duodenal origin of the pancreatic gas, we therefore suspected a PPU as the cause of symptoms. Esophagogastroduodenoscopy (EGD) revealed a small duodenal ulcer with the hole at the bottom, confirming the diagnosis of PPU. The surgeon indicated conservative therapy (IV rehydration, bowel rest, proton pump inhibitors, antibiotics), and clinical, laboratory and imaging findings progressively improved. After 4 wk, symptoms resolved and we observed a clear improvement of the pancreatic damage at CECT follow-up.
EP is a rare but potentially fatal form of acute necrotizing pancreatitis in which gas grows in and outside the pancreas, and typically involves the whole parenchyma in diabetic individuals[5]. Acute pancreatitis is classified as oedematous and necrotizing, and most common causes are gallstones and alcohol use. Less frequently, metabolic causes (hypertriglyceridemia, hypercalcemia), drugs, trauma, infections, autoimmune and genetic causes can be found[6-11]. Rarely, peptic ulcers can penetrate the pancreas and cause pancreatitis, which usually manifests with mild to severe pancreatitis with peripancreatic fluid collections. In the last few years, the incidence of complicated peptic ulcers has decreased by one-half and one-third in males and females, respectively. However, complete information regarding epidemiology of association between PPU and EP is still lacking[12]. The overall mortality of EP is high, estimated around 32.8%. The presence of advanced age, hypotension, gas outside the pancreas on CT, multiorgan failure and initial surgical evacuation is associated with higher mortality. Therefore, less invasive approaches have been replacing surgery for their better outcome[13]. Percutaneous or endoscopic aspirations are indeed useful to drain collections and to isolate bacteria by aerobic/anaerobic cultures[5].
The clinical picture is characterized by epigastric pain, nausea, vomiting, and development of multiorgan failure in severe cases[14]. Laboratory tests are non-specific; only a slight elevation of amylase and lipase can be found, and the presence of pancreatic enzyme elevation does not correlate with the severity of the disease[14]. US evaluation can hardly detect a focal emphysematous involvement and, unlike other abdominal inflammatory processes[15-22], cannot be used alone to achieve the correct diagnosis. CECT is useful to reveal the presence and severity of gas in and outside the parenchyma[23], and gas-forming microorganisms may enter from the bowel by haematogenous and lymphatic routes, through the ampulla of Vater or by transmural passage from the adjacent colon. Endoscopy or sphincterotomy can be associated with EP, and a causal relation between EP and PPU has also been hypothesized[24]. Only a few cases have been documented so far, and gas is confined to the site of penetration, usually the pancreatic head, and ulcers most often involve the duodenum[25].
The diagnosis of PPU is made with EGD, which reveals an ulcer with the hole at the bottom[3]. Imaging, such as CECT, is useful to reveal the focal presence of gas within the pancreatic parenchyma but is less useful to reveal peptic ulcers, in particular if they are small and posterior[14,26,27]. In our case, CECT showed focal emphysema of the pancreatic head and also mild oedema of the duodenum, suggesting the intestinal origin of the gas.
Unlike the classic form of EP, which involves the whole parenchyma and has a poor prognosis, we found that the focal involvement of the pancreas by PPU has a benign clinical course if a conservative therapy is promptly established. In view of the clinical and laboratory stability of this patient and the absence of signs of perforation, we in fact preferred to treat him conservatively obtaining a clinical and imaging improvement over time, as documented by CECT follow-up.
In conclusion, the focal presence of gas within the pancreas is a rare condition which should be carefully investigated because it can be associated with an underlying condition not evident on imaging. PPU can be suspected as the cause of EP when the pancreas is involved focally without any other apparent cause of inflammation. A prompt conservative treatment is associated with a good outcome if established promptly, especially if the parenchymal involvement is mild and the patient is hemodynamically stable.
A 49-year-old man presented with an acute complaint of epigastric pain radiating to the back after an excessive intake of fried, high fat food and of nonsteroidal anti-inflammatory drugs for low back pain.
A focal emphysematous pancreatitis due to a penetrating duodenal ulcer was observed.
Perforated ulcer.
Laboratory tests are non-specific; only a slight elevation of amylase and lipase can be found, and the presence of pancreatic enzyme elevation does not correlate with the severity of the disease.
Contrast-enhanced computed tomography is useful to reveal the presence and severity of gas in and outside the pancreatic parenchyma.
A prompt conservative treatment is associated with a good outcome if established promptly, especially if the parenchymal involvement is mild and the patient is hemodynamically stable.
Very few cases of association between penetrating ulcers and emphysematous pancreatitis have been published in the literature. This case shows that the focal presence of gas within the pancreas is a rare condition which should be carefully investigated because it can be associated with an underlying condition not evident on imaging.
A penetrating peptic ulcer represents an exceptional cause of abdominal pain and was more frequently observed in the past where there was not an effective antacid treatment.
Focal emphysematous pancreatitis is a rare condition that could be associated with penetrating ulcers and has a benign clinical course if a conservative therapy is promptly established.
This is a nice case report on a rare case of a duodenal ulcer penetrating the pancreas and complicated with emphysematous pancreatitis. This manuscript is generally of interest. The authors provided the complete review of this issue.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Dambrauskas Z, Gonzalez-Ojeda AG, Liao KF, Zhao JB S- Editor: Chen K L- Editor:A E- Editor: Ma YJ
| 1. | Volwiler W, Mallory TB. Benign gastric ulcer, with penetration into pancreas. N Engl J Med. 1946;235:201. [PubMed] |
| 2. | Merrill JR. Fistulation to the pancreatic duct complicating duodenal peptic ulcer. Gastroenterology. 1984;87:957-959. [PubMed] |
| 3. | Shibukawa N, Ouchi S, Wakamatsu S, Wakahara Y, Tatsumi N, Kaneko A. A Rare Case of Gastric Ulcer Penetrating the Pancreas that was Successfully Managed by Conservative Therapy. Intern Med. 2017;56:2277-2279. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Pyeon SI, Hwang JH, Kim YT, Lee BS, Lee SH, Lee JN, Cheong JH, Oh KJ. Acute pancreatitis due to a duodenal ulcer. Clin Endosc. 2014;47:579-583. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Hamada S, Shime N. Emphysematous pancreatitis. Intensive Care Med. 2016;42:1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, Tsiotos GG, Vege SS; Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4932] [Cited by in RCA: 4328] [Article Influence: 360.7] [Reference Citation Analysis (45)] |
| 7. | Cenci C, Restuccia T, Gnerre P, Chiti I, Betti L, Micati M, Tana C. The management of the patient with acute pancreatitis: from evidence to clinical practice. Ital J Med. 2017;11:220-245. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Tana M, Tana C, Schiavone C, Verdiani V, Palermo C, Alessandri M, Giamberardino MA, Montagnani A. Spontaneous dissection of the celiac artery in the young: a case report and systematic review of the literature. Hosp Pract (1995). 2017;45:258-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Lin HF, Liao KF, Chang CM, Lin CL, Lai SW. Correlation between proton pump inhibitors and risk of pyogenic liver abscess. Eur J Clin Pharmacol. 2017;73:1019-1025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 10. | Liao KF, Huang PT, Lin CC, Lin CL, Lai SW. Fluvastatin use and risk of acute pancreatitis: a population-based case-control study in Taiwan. Biomedicine (Taipei). 2017;7:17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 11. | Liao KF, Cheng KC, Lin CL, Lai SW. Etodolac and the risk of acute pancreatitis. Biomedicine (Taipei). 2017;7:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 12. | Sadic J, Borgström A, Manjer J, Toth E, Lindell G. Bleeding peptic ulcer - time trends in incidence, treatment and mortality in Sweden. Aliment Pharmacol Ther. 2009;30:392-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Bul V, Yazici C, Staudacher JJ, Jung B, Boulay BR. Multiorgan Failure Predicts Mortality in Emphysematous Pancreatitis: A Case Report and Systematic Analysis of the Literature. Pancreas. 2017;46:825-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Okamoto H, Kuriyama A. Emphysematous pancreatitis. Emerg Med J. 2013;30:396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Stoker J, van Randen A, Laméris W, Boermeester MA. Imaging patients with acute abdominal pain. Radiology. 2009;253:31-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 220] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 16. | Tana M, Tana C, Iannetti G, Romano M, Silingardi M, Schiavone C. Role of ultrasonography in acute appendicitis of the elderly. A pictorial essay. Curr Med Imaging Rev. 2017;13:32-37 [DOI 10.2174/1573405612666160606105130]. |
| 17. | Choi HS, Lee YS, Park SB, Yoon Y. Simultaneous emphysematous cholecystitis and emphysematous pancreatitis: a case report. Clin Imaging. 2010;34:239-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Hanbidge AE, Buckler PM, O’Malley ME, Wilson SR. From the RSNA refresher courses: imaging evaluation for acute pain in the right upper quadrant. Radiographics. 2004;24:1117-1135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 72] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 19. | Tana C, Iannetti G, D’Alessandro P, Tana M, Mezzetti A, Schiavone C. Pitfalls of contrast-enhanced ultrasound (CEUS) in the diagnosis of splenic sarcoidosis. J Ultrasound. 2013;16:75-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | van Randen A, Laméris W, van Es HW, van Heesewijk HP, van Ramshorst B, Ten Hove W, Bouma WH, van Leeuwen MS, van Keulen EM, Bossuyt PM. A comparison of the accuracy of ultrasound and computed tomography in common diagnoses causing acute abdominal pain. Eur Radiol. 2011;21:1535-1545. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 161] [Cited by in RCA: 160] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 21. | Atema JJ, Gans SL, Van Randen A, Laméris W, van Es HW, van Heesewijk JP, van Ramshorst B, Bouma WH, Ten Hove W, van Keulen EM. Comparison of Imaging Strategies with Conditional versus Immediate Contrast-Enhanced Computed Tomography in Patients with Clinical Suspicion of Acute Appendicitis. Eur Radiol. 2015;25:2445-2452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Tana C, Dietrich CF, Schiavone C. Hepatosplenic sarcoidosis: contrast-enhanced ultrasound findings and implications for clinical practice. Biomed Res Int. 2014;2014:926203. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 23. | Balani A, Dey AK, Sarjare S, Chatur C. Emphysematous pancreatitis: classic findings. BMJ Case Rep. 2016;2016:pii: bcr2016217445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 24. | Wig JD, Kochhar R, Bharathy KG, Kudari AK, Doley RP, Yadav TD, Kalra N. Emphysematous pancreatitis. Radiological curiosity or a cause for concern? JOP. 2008;9:160-166. [PubMed] |
| 25. | Singh T, Mendelson R. Case report: Confined penetration of a duodenal ulcer causing pancreatitis. J Med Imaging Radiat Oncol. 2010;54:47-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 26. | Allen BC, Tirman P, Tobben JP, Evans JA, Leyendecker JR. Gastroduodenal ulcers on CT: forgotten, but not gone. Abdom Imaging. 2015;40:19-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 27. | Barreda L, Targarona J, Pando E, Reynel M, Portugal J, Barreda C. Medical versus surgical management for emphysematous pancreatic necrosis: is gas within pancreatic necrosis an absolute indication for surgery? Pancreas. 2015;44:808-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |