Published online Dec 7, 2017. doi: 10.3748/wjg.v23.i45.8104
Peer-review started: June 30, 2017
First decision: July 13, 2017
Revised: August 27, 2017
Accepted: September 13, 2017
Article in press: September 13, 2017
Published online: December 7, 2017
Processing time: 158 Days and 23 Hours
Simultaneous liver, pancreas-duodenum, and kidney transplantation has been rarely reported in the literature. Here we present a new and more efficient en bloc technique that combines classic orthotopic liver and pancreas-duodenum transplantation and heterotopic kidney transplantation for a male patient aged 44 years who had hepatitis B related cirrhosis, renal failure, and insulin dependent diabetes mellitus (IDDM). A quadruple immunosuppressive regimen including induction with basiliximab and maintenance therapy with tacrolimus, mycophenolate mofetil, and steroids was used in the early stage post-transplant. Postoperative recovery was uneventful and the patient was discharged on the 15th postoperative day with normal liver and kidney function. The insulin treatment was completely withdrawn 3 wk after operation, and the blood glucose level remained normal. The case findings support that abdominal organ cluster and kidney transplantation is an effective method for the treatment of end-stage liver disease combined with uremia and IDDM.
Core tip: Combined orthotopic liver and heterotopic pancreas transplant has been usually reported in the literature. Here we present a new and more efficient en bloc technique for combined liver-pancreas transplant. Hepatectomy was performed in the standard fashion with caval cross-clamping. The liver, along with the en bloc duodenopancreatic graft, was then transplanted orthotopically without using veno-venous bypass. Graft kidney was implanted in right iliac fossa in accordance with the traditional classical manner. Postoperative recovery was uneventful and the patient was discharged on the 15th postoperative day with normal liver and kidney function. The insulin treatment was completely withdrawn 3 wk after operation, and the blood glucose level remained normal. The case findings support that abdominal organ cluster and kidney transplantation is an effective method for the treatment of end-stage liver disease combined with uremia and insulin dependent diabetes mellitus.
- Citation: Li J, Guo QJ, Cai JZ, Pan C, Shen ZY, Jiang WT. Simultaneous liver, pancreas-duodenum and kidney transplantation in a patient with hepatitis B cirrhosis, uremia and insulin dependent diabetes mellitus. World J Gastroenterol 2017; 23(45): 8104-8108
- URL: https://www.wjgnet.com/1007-9327/full/v23/i45/8104.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i45.8104
Combined liver-pancreas transplantation was formerly used as a salvage procedure for non-resectable upper abdominal malignancies, but the procedure was almost abandoned due to poor outcome[1]. Recently, the indication for combined liver-pancreas transplantation has been changed and transplant surgeons have started using this technique for patients with insulin dependent diabetes mellitus (IDDM) who are candidates for liver transplantation at the same time. There are several advantages to using simultaneous liver-pancreas transplant such as insulin independence after transplantation, improving patient management, and decreasing the risk of post-transplant cardiovascular diseases[2]. Diabetic patients who receive only liver graft are not only at increased risk of developing cardiovascular diseases but also remain diabetic after transplantation which may itself negatively affect the long-term graft survival[3-5]. Although there are so many advantages to combined liver pancreas transplantation, surprisingly only few cases have been reported in the literature[6]. We hereby report about our experience with en bloc liver-pancreas and kidney transplantation in one patient with end-stage liver disease, chronic renal failure, and IDDM, with some detail aspects about the surgical procedures and immunosuppressive regimens discussed.
A 44-year-old male complaining of abdominal distension and anorexia more than one year was referred to our center in April 2016. The patient was infected with hepatitis B virus for more than 30 years, and he developed abdominal distension and anorexia one year ago and suffered with melena two months ago. His past medical history was significant for IDDM for more than 10 years. Additionally, the patient suffered with chronic renal failure relying on regular dialysis (three times per week). He was on insulin therapy (60 units/d) and had a history of recurrent hypoglycemic episodes recently. At the time of admission, the laboratory parameters were as follows: total bilirubin 2.5 mg/dL, aspartate aminotransferase 106 U/L, alanine aminotransferase 50 U/L, alkaline phosphatase 683 U/L, albumin 33.1 g/L, blood urea nitrogen 22 mg/dL, serum creatinine 8.2 mg/dL, and hemoglobin 7.7 g/dL. Bleeding profile was within normal limits. Enhanced abdominal computed tomography indicated liver cirrhosis, splenomegaly, mild ascites, and esophageal varices. After much clinical testing and deliberation, the multi-disciplinary care management concluded that transplantation would offer the greatest survival benefit. The patient was listed for a combined liver, pancreas, and kidney transplant.
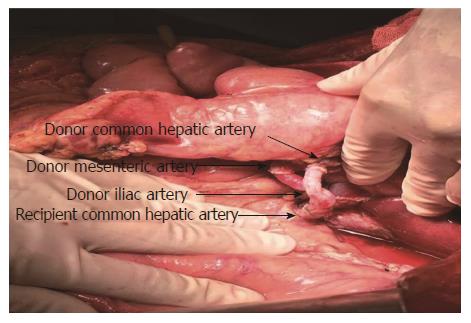
He received en bloc liver-pancreas and kidney graft from an ABO identical deceased donor aged 28 years. Liver biopsy of the graft showed no macro- or microsteatosis. Liver, pancreas, duodenum, and both kidneys were retrieved en bloc without disturbing the hepatoduodenal ligament. The superior mesenteric artery and celiac arteries were then anastomosed to a Y graft of the internal iliac artery and external iliac artery from the same donor on the back table so as to allow a single vascular anastomosis. Bile was washed out through the gallbladder as the bile duct was left intact. The superior mesenteric vein beyond the neck of the pancreas was closed (Figure 1).
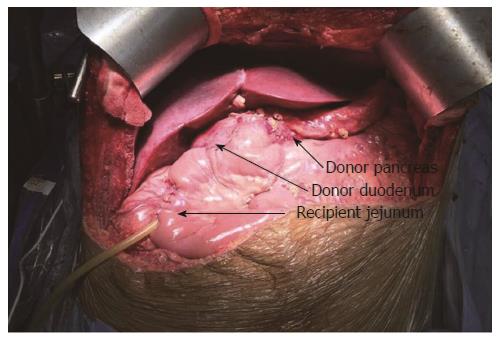
Hepatectomy was performed in the standard fashion with caval cross-clamping. The liver, along with the en bloc duodenopancreatic graft, was then transplanted orthotopically without using veno-venous bypass. This was followed by the suprahepatic and infrahepatic inferior vena caval anastomoses. The recipient portal vein was then anastomosed to the back side of the donor portal vein between the superior border of pancreas and the liver. The innominate artery Y graft was anastomosed to the infrarenal aorta (Figure 2). After reperfusion, graft liver and pancreas were well perfused with normal color (Figure 1). Finally, a Roux-en-y enteroenteric anastomosis was performed between the recipient’s jejunum and graft duodenum for exocrine pancreatic and biliary drainage. Graft kidney was implanted in right iliac fossa in accordance with the traditional classical manner. Total duration of the operation was 480 min and 10 units of packed cells were transfused. Total cold ischemic time was 1 h and 15 min with a warm ischemic time of 5 min.
Initial immunosuppression included induction with basiliximab (Simulect) and maintenance therapy with tacrolimus (target trough level 8-10 ng/mL) and mycophenolate mofetil (MMF) 1.5 g/d. Steroids were tapered down and completely withdrawn within 3 mo post transplantation. In addition, anti-infection, anticoagulation, inhibition of gastric acid and pancreatic enzyme secretion, and intravenous nutritional support treatment were provided.
Postoperative recovery was uneventful and the patient was discharged on the 15th postoperative day with normal liver and kidney function. The insulin treatment was completely withdrawn 3 wk after operation, and the blood glucose level remained normal.
The most accepted indication for combined liver-pancreas transplantation is chronic liver disease in patients who concomitantly suffer from IDDM. This approach not only corrects liver disease but also allows the patient to have insulin independence at the same time[7]. Multivisceral transplants have usually been in the form of kidney-pancreas, liver-kidney, and sometimes liver-pancreas transplant, with combined liver, pancreas, and kidney transplant being comparatively rare. Until now, there have been only three cases of combined liver, pancreas, and kidney transplant reported[8-10]. Certain liver diseases have strong association with diabetes mellitus; primary sclerosing cholangitis is one of the diseases which has been described in association with diabetes mellitus type 1[11,12]. Other diseases of the liver which have direct association with diabetes mellitus are NASH[13,14] and systic fibrosis[15]. In selected cases, these diseases justify combined liver-pancreas transplantation.
Technically, combined liver-pancreas transplantation can be performed in two ways. The first pattern is to perform a standard orthotopic liver transplantation followed by a standard heterotopic transplantation of the pancreas allograft onto the iliac vessels in the right lower quadrant. The separate transplantation of the liver and pancreas offers the advantage that if a complication occurs in one of the organ grafts, the other organ theoretically is less likely to become affected. The second technique described by Starzl et al[16] is to perform an orthotopic organ cluster of graft liver and pancreas with their entire arterial blood supply including the donor celiac axis and superior mesenteric artery. The recipient portal vein was anastomosed to graft portal vein in an end-to-side manner. A good metabolic control can be achieved for the en bloc technique, which provided the physiological position of the pancreas with a natural venous drainage on to graft liver[17]. Additionally, this technique greatly reduced the surgical difficulty since it involved only three or four large vascular anastomoses and one duodeno-jejunostomy without biliary anastomosis compared to the separate transplantation.
Preexisting IDDM is a major risk factor for poor outcome after liver transplantation[4,18-20]. For patients with end-stage liver disease and type 1 diabetes mellitus, there seems to be a strong rationale for replacing the pancreas in addition to the liver[6]. Adequate glycemic control without the need for endogenous insulin was achieved in our patient after combined liver and pancreas transplant, which indicated that combined liver and pancreas transplantation is an effective method for the treatment of end-stage liver disease and IDDM.
Liver transplant has also been combined with simultaneous islet cell transplant with some success dating back to the cluster operations[21] and again more recently[22]. Although islet transplantation is much easier to operate with fewer complications and can be repeated several times, long-term (> 5 years) islet survival is not ideal and patients usually return to insulin dependence. Compared with islet transplantation, separated pancreas transplantation is accompanied by more postoperative complications such as splenic vein thrombosis, anastomotic leakage, and pancreatic fistula. However, combined liver and pancreas transplantation greatly reduces the difficulty of surgery and risk of complications. Additionally, the pancreas transplantation can also solve the problem of insufficient islet.
Combined liver-pancreas transplantation may have an immunologic advantage. Unlike the liver, the pancreas is considered a highly immunogenic organ[23] and when liver transplant is combined with other organ transplants such as pancreas or multiple organs, the liver can protect these organs from severe rejection episodes[24-26]. We applied the same immunosuppressive regimen (induction with basiliximab and maintenance therapy with tacrolimus, mycophenolate mofetil, and steroids) for liver transplantation in this case, and at the time of this writing, no liver, pancreatic, or kidney rejection was seen in our case. Despite the advantages of combined liver-pancreas transplantation, only few centers have reported this kind of transplantation. The establishment of more effective immunosuppressive regimen has to be based on the accumulation of more multi-organ transplantation cases.
Multivisceral transplants have usually been in the form of kidney-pancreas, liver- pancreas, or sometimes liver-kidney transplant, however, combined liver-pancreas and kidney transplant was rarely reported. More recently, the authors have successfully performed en bloc liver-pancreas and kidney transplant in one patient with end-stage liver disease, uremia, and insulin dependent diabetes mellitus (IDDM), although the follow-up period was shorter.
The patient was infected with hepatitis B virus for more than 30 years, and he developed abdominal distension and anorexia one year ago, and suffered with melena two months ago. Upon physical examination, he had a mild abdominal tenderness and palpable enlarged spleen. His past medical history was significant for IDDM for more than 10 years. Additionally, the patient suffered with chronic renal failure relying on regular dialysis (three times per week).
Liver cirrhosis can be divided into viral hepatitis cirrhosis, alcoholic cirrhosis, metabolic cirrhosis, cholestatic cirrhosis, portal cirrhosis, autoimmune cirrhosis, toxic and drug-induced cirrhosis, malnutritional liver cirrhosis, and cryptogenic cirrhosis.
At the time of admission, the laboratory parameters were as follows: total bilirubin 2.5 mg/dL, aspartate aminotransferase 106 U/L, alanine aminotransferase 50 U/L, alkaline phosphatase 683 U/L, albumin 33.1 g/L, blood urea nitrogen 22 mg/dL, serum creatinine 8.2 mg/dL, and hemoglobin 7.7 g/dL. Bleeding profile was within normal limits.
Enhanced abdominal computed tomography indicated liver cirrhosis, splenomegaly, mild ascites, and esophageal varices.
Histological examination showed diffuse nodular sclerosis which was in line with the performance of hepatitis B cirrhosis.
A quadruple immunosuppressive regimen including induction with basiliximab and maintenance therapy with tacrolimus, mycophenolate mofetil, and steroids was used in the early stage post-transplant. In addition, anti-infection, anticoagulation, inhibition of gastric acid and pancreatic enzyme secretion, and intravenous nutritional support treatment were provided.
Very few cases of simultaneous liver, pancreas-duodenum, and kidney transplantation have been reported in the literature. Additionally, combined liver- pancreas transplant was usually reported in the manner of separate transplantation, however, we performed orthotopic en bloc transplantation of the liver and pancreas grafts.
This case report presents a new surgical type of the upper abdominal organ cluster transplant. Compared to the traditional separate transplantation, the main advantage of this technique is its rapidity and simplicity since it involves only three or four large vascular anastomoses and one duodeno-jejunostomy with no separate biliary anastomosis. Additional advantage of the en bloc technique is the physiological position of the pancreas with a natural venous drainage into the donor liver graft.
The author has described one case of simultaneous liver, pancreas-duodenum, and kidney transplantation. The article highlights surgical advantages of abdominal organ cluster transplant compared with traditional separate multivisceral transplants.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Acevedo JG, Taheri S, Yorioka N S- Editor: Ma YJ L- Editor: Wang TQ E- Editor: Huang Y
| 1. | Mieles L, Todo S, Tzakis A, Starzl TE. Treatment of upper abdominal malignancies with organ cluster procedures. Clin Transplant. 1990;4:63-67. [PubMed] |
| 2. | Aguirrezabalaga J, Gómez M, Novás S, Fernández C, Corbal G, Fraguela J, Bueno J, Suarez F, Otero A. Combined liver-pancreas transplantation: contribution of five cases. Transplant Proc. 2002;34:211-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Haydon G, Neuberger J. Liver transplantation in cirrhotic patients with diabetes mellitus. Liver Transpl. 2001;7:234-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Shields PL, Tang H, Neuberger JM, Gunson BK, McMaster P, Pirenne J. Poor outcome in patients with diabetes mellitus undergoing liver transplantation. Transplantation. 1999;68:530-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 59] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Yoo HY, Thuluvath PJ. The effect of insulin-dependent diabetes mellitus on outcome of liver transplantation. Transplantation. 2002;74:1007-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Trotter JF, Bak TE, Wachs ME, Everson GT, Kam I. Combined liver-pancreas transplantation in a patient with primary sclerosing cholangitis and insulin-dependent diabetes mellitus. Transplantation. 2000;70:1469-1471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Pirenne J, Deloose K, Coosemans W, Aerts R, Van Gelder F, Kuypers D, Maes B, Verslype C, Yap P, Van Steenbergen W. Combined ‘en bloc’ liver and pancreas transplantation in patients with liver disease and type 1 diabetes mellitus. Am J Transplant. 2004;4:1921-1927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Wang H, Dou KF, Yang XJ, Qin WJ, Zhang G, Yu L, Kang FX, Chen SY, Xiong LZ, Song ZS. [A case report of simultaneous liver, pancreas-duodenum, and kidney transplantation in a patient with post-hepatitic cirrhosis combined with uremia and insulin-dependent diabetes related to chronic pancreatitis]. Zhonghua Yi Xue Za Zhi. 2006;86:2421-2424. [PubMed] |
| 9. | Tzakis AG, Nunnelley MJ, Tekin A, Buccini LD, Garcia J, Uchida K, Neville HL, Nares MA, Ruiz P, Bodamer O. Liver, pancreas and kidney transplantation for the treatment of Wolcott-Rallison syndrome. Am J Transplant. 2015;15:565-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Rivera E, Gupta S, Chavers B, Quinones L, Berger MR, Schwarzenberg SJ, Pruett T, Verghese P, Chinnakotla S. En bloc multiorgan transplant (liver, pancreas, and kidney) for acute liver and renal failure in a patient with Wolcott-Rallison syndrome. Liver Transpl. 2016;22:371-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Kay M, Wyllie R, Michener W, Caulfield M, Steffen R. Associated ulcerative colitis, sclerosing cholangitis, and insulin-dependent diabetes mellitus. Cleve Clin J Med. 1993;60:473-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Thompson HH, Pitt HA, Tompkins RK, Longmire WP Jr. Primary sclerosing cholangitis: a heterogenous disease. Ann Surg. 1982;196:127-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Day CP. Non-alcoholic steatohepatitis (NASH): where are we now and where are we going? Gut. 2002;50:585-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 122] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 14. | James O, Day C. Non-alcoholic steatohepatitis: another disease of affluence. Lancet. 1999;353:1634-1636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 180] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 15. | Stern RC, Mayes JT, Weber FL Jr, Blades EW, Schulak JA. Restoration of exocrine pancreatic function following pancreas-liver-kidney transplantation in a cystic fibrosis patient. Clin Transplant. 1994;8:1-4. [PubMed] |
| 16. | Starzl TE, Rowe MI, Todo S, Jaffe R, Tzakis A, Hoffman AL, Esquivel C, Porter KA, Venkataramanan R, Makowka L. Transplantation of multiple abdominal viscera. JAMA. 1989;261:1449-1457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 160] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 17. | Gaber AO, Shokouh-Amiri H, Hathaway DK, Gaber LW, Elmer D, Kitabchi A, Stentz F, Hughes T. Pancreas transplantation with portal venous and enteric drainage eliminates hyperinsulinemia and reduces postoperative complications. Transplant Proc. 1993;25:1176-1178. [PubMed] |
| 18. | Blanco JJ, Herrero JI, Quiroga J, Sangro B, Gómez-Manero N, Pardo F, Cienfuegos JA, Prieto J. Liver transplantation in cirrhotic patients with diabetes mellitus: midterm results, survival, and adverse events. Liver Transpl. 2001;7:226-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | John PR, Thuluvath PJ. Outcome of liver transplantation in patients with diabetes mellitus: a case-control study. Hepatology. 2001;34:889-895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 114] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 20. | Trail KC, Stratta RJ, Larsen JL, Ruby EI, Patil KD, Langnas AN, Donovan JP, Sorrell MF, Zetterman RK, Pillen TJ. Results of liver transplantation in diabetic recipients. Surgery. 1993;114:650-656; discussion 656-658. [PubMed] |
| 21. | Tzakis AG, Ricordi C, Alejandro R, Zeng Y, Fung JJ, Todo S, Demetris AJ, Mintz DH, Starzl TE. Pancreatic islet transplantation after upper abdominal exenteration and liver replacement. Lancet. 1990;336:402-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 202] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 22. | Angelico MC, Alejandro R, Nery J, Webb M, Bottino R, Kong SS, Karatzas T, Olson L, Tzakis AG, Ricordi C. Transplantation of islets of Langerhans in patients with insulin-requiring diabetes mellitus undergoing orthotopic liver transplantation--the Miami experience. J Mol Med (Berl). 1999;77:144-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 23. | Humar A, Khwaja K, Ramcharan T, Asolati M, Kandaswamy R, Gruessner RW, Sutherland DE, Gruessner AC. Chronic rejection: the next major challenge for pancreas transplant recipients. Transplantation. 2003;76:918-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 66] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 24. | Johnston TD, Ranjan D. Transplantation of the liver combined with other organs. Hepatogastroenterology. 1998;45:1387-1390. [PubMed] |
| 25. | Benedetti E, Pirenne J, Troppmann C, Hakim N, Moon C, Gruessner RW, Sharp H, Matas AJ, Payne WD, Najarian JS. Combined liver and kidney transplantation. Transpl Int. 1996;9:486-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 26. | Calne RY, Sells RA, Pena JR, Davis DR, Millard PR, Herbertson BM, Binns RM, Davies DA. Induction of immunological tolerance by porcine liver allografts. Nature. 1969;223:472-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 642] [Cited by in RCA: 613] [Article Influence: 10.9] [Reference Citation Analysis (0)] |