Published online Nov 21, 2017. doi: 10.3748/wjg.v23.i43.7785
Peer-review started: September 4, 2017
First decision: September 20, 2017
Revised: October 1, 2017
Accepted: November 1, 2017
Article in press: November 1, 2017
Published online: November 21, 2017
Processing time: 78 Days and 11.6 Hours
To explore the outcomes and the appropriate treatment for patients with moderately severe acute pancreatitis (AP).
Statistical analysis was performed on data from the prospectively collected database of 103 AP patients admitted to the Department of Surgery, Hospital of Lithuanian University of Health Sciences in 2008-2013. All patients were confirmed to have the diagnosis of AP during the first 24 h following admission. The severity of pancreatitis was assessed by MODS and APACHE II scale. Clinical course was re-evaluated after 24, 48 and 72 h. All patients were categorized into 3 groups based on Atlanta 2012 classification: Mild, moderately severe, and severe. Outcomes and management in moderately severe group were also compared to mild and severe cases according to Atlanta 1992 and 2012 classification.
Fifty-three-point four percent of patients had edematous while 46.6 % were diagnosed with necrotic AP. The most common cause of AP was alcohol (42.7%) followed by alimentary (26.2%), biliary (26.2%) and idiopathic (4.9%). Under Atlanta 1992 classification 56 (54.4%) cases were classified as “mild” and 47 (45.6%) as “severe”. Using the revised classification (Atlanta 2012), the patient stratification was different: 49 (47.6%) mild, 27 (26.2%) moderately severe and 27 (26.2%) severe AP cases. The two severe groups (Atlanta 1992 and Revised Atlanta 2012) did not show statistically significant differences in clinical parameters, including ICU stay, need for interventional treatment, infected pancreatic necrosis or mortality rates. The moderately severe group of 27 patients (according to Atlanta 2012) had significantly better outcomes when compared to those 47 patients classified as severe form of AP (according to Atlanta 1992) with lower incidence of necrosis and sepsis, lower APACHE II (P = 0.002) and MODS (P = 0.001) scores, shorter ICU stay, decreased need for interventional and surgical treatment.
Study shows that Atlanta 2012 criteria are more accurate, reduce unnecessary treatments for patients with mild and moderate severe pancreatitis, potentially resulting in health costs savings.
Core tip: The revised (2012) Atlanta classification proved to be superior to the former classic (1992) Atlanta classification. The results of this study support the use of Atlanta 2012 classification in clinical setting and suggest that “moderately” severe AP cases could be treated as “mild” AP once temporary organ failure is controlled, and should result in significant health costs savings without compromising the patient’s outcomes.
- Citation: Ignatavicius P, Gulla A, Cernauskis K, Barauskas G, Dambrauskas Z. How severe is moderately severe acute pancreatitis? Clinical validation of revised 2012 Atlanta Classification. World J Gastroenterol 2017; 23(43): 7785-7790
- URL: https://www.wjgnet.com/1007-9327/full/v23/i43/7785.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i43.7785
Acute pancreatitis (AP) encompasses a wide spectrum of disease severity from a brief, self-limited presentation to a fulminant progression to multi-organ failure and death[1,2]. In response to the need for a comprehensive classification system in the treatment of AP, the 1992 Atlanta classification was established. The 1992 Atlanta Classifications identified two categories of AP, “mild” and “severe” and recommended the clinical treatment for each type[3,4]. However, a subgroup of AP patients who fell in-between the two 1992 severity categories were often observed to have relatively good outcomes and respond positively to less aggressive treatment protocols than those with severe disease, thus calling for the revision of the existing classification system. In 2012 the Atlanta classification was revised by adding a third category defined as “moderately severe”.
To the best of our knowledge, no studies have evaluated the outcomes and clinical course of “moderately severe” pancreatitis to test their true value in clinical setting. No studies have focused on complications, mortality and outcomes of patients with moderately severe AP. It raises the question if the recommended aggressive treatment and expensive interventions are necessary in moderately severe category patients.
The main aim of this study was to stratify the same cohort of patients into the mild and severe categories using Atlanta 1992 classification and into mild, moderate and severe categories according to the Atlanta 2012 revised version to highlight the severity of moderate AP and to assess the outcomes of these patients. We also aimed to ascertain whether this new category aids predicting the outcomes and complications while optimizing the use of medical resources and interventional procedures.
Since 2008 data of patients with acute pancreatitis, admitted to the Department of Surgery, Hospital of Lithuanian University of Health Sciences were prospectively collected and entered into a specially designed database (The Regional Ethics Committee and IRB approval No. BE-2-47 and P1-113/2005, all patients provided a written informed consent). Statistical analysis was performed on data from the prospectively collected database of 103 AP patients. All patients were confirmed to have diagnosis of AP during the first 24 h since admission according to Atlanta 2012 classification (acute abdominal pain, localized in epigastrium, commonly radiating to the back, 3-fold elevated serum levels of lipase/amylase content, typical findings on abdominal computed tomography (CT) scan with intravenous enhancement).
In addition, the severity of pancreatitis was assessed by MODS and APACHE II scale. Clinical course was reevaluated after 24, 48 and 72 h. A contrast enhanced CT scan performed on Days 5-7 after the onset of the disease to confirm the presence and extent of pancreatic/peripancreatic necrosis. Clinical data relating to the severity of the disease, development of organ dysfunction and/or septic complications were prospectively collected in standardized fashion. All patients were re-categorized into 3 groups based on severity: Mild (no organ failure, no local or systemic complications), moderately severe (organ failure that resolves within 48 h (transient organ failure) and/or local or systemic complications without persistent organ failure), severe [persistent organ (single/multiple) failure (> 48 h)] (Atlanta 2012) and mild (minimal organ dysfunction and an uneventful recovery, absence of the described features of severe acute pancreatitis) and severe (organ failure and/or local complications, such as necrosis, abscess, or pseudocyst) acute pancreatitis groups (Atlanta 1992).
Severe AP groups according to Atlanta 1992 and Atlanta 2012 were compared with each other. Moderately severe (Atlanta 2012) cases were compared to mild and severe cases according to Atlanta 1992 classification. Outcomes and management were re-assessed in all groups.
Data are expressed as mean ± SD of the number of replicate. Differences between two groups are evaluated with t-test. Differences among three or more groups are evaluated using the nonparametric one-way ANOVA test. Differences are considered significant when P < 0.05. SPSS 20.0 (SPSS Inc., Chicago, IL, United States) was employed to analyze the data.
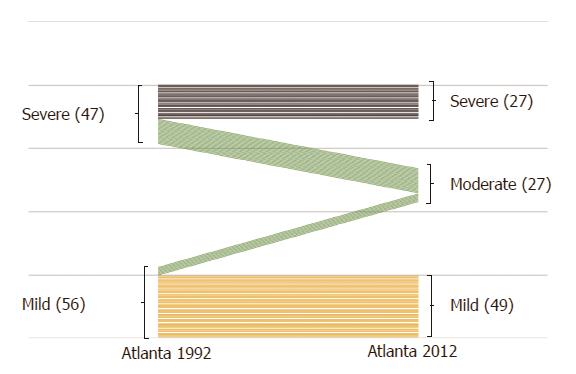
There were a total of 103 patients with acute pancreatitis included in the study. Alcohol abuse was the most common cause of the disease 42.7%, while biliary etiology was obvious in less than 30% of patients. According to the Atlanta 1992 classification mild AP was diagnosed in 56 (54.4%) and severe AP in 47 (45.6%) cases. The group of moderately severe acute pancreatitis (Atlanta 2012) was mainly derived from the severe AP group (Atlanta 1992), while only 7 patients moved from the mild AP group (Atlanta 1992). Overall mortality reached 12.6 % (Table 1).
| Variable | All patients (n = 103) |
| Male | 54 (52.4) |
| Necrotic | 48 (46.6) |
| Edematous | 55 (53.4) |
| Etiology | |
| Alcohol | 44 (42.7) |
| Alimentary | 27 (26.2) |
| Biliary | 27 (26.2) |
| Idiopathic | 5 (4.9) |
| Atlanta 1992 | |
| Mild | 56 (54.4) |
| Severe | 47 (45.6) |
| Atlanta 2012 | |
| Mild | 49 (47.6) |
| Moderately severe | 27 (26.2) |
| Severe | 27 (26.2) |
| Interventions | |
| US guided drainage | 6 (5.8) |
| Fasciotomy | 1 (1) |
| Necrosectomy | 5 (4.9) |
| APACHE II (mean ± SD) | 7.1 ± 5.32 |
| MODS (mean ± SD) | 2.6 ± 2.91 |
| Sepsis | 6 (5.8) |
| Mortality | 13 (12.6) |
While comparing the disease course and outcomes of severe AP according to 1992 and 2012 classifications, there were no statistically significant differences in clinical outcomes, including intensive care unit (ICU) stay, need for ultrasound (US) guided drainage, occurrence of infected necrosis or mortality rates (Table 2).
| Atlanta 1992 | Atlanta 2012 | P value | |
| ICU admission (n) | 5 | 6 | 0.32 |
| US drainage (n) | 5 | 4 | 0.71 |
| Infected necrosis (n) | 12 | 11 | 0.19 |
| Deaths (n) | 13 | 13 | 0.75 |
According to the severity of disease, organ failure, complication rates and treatment outcomes, majority of moderately severe acute pancreatitis cases according to Atlanta 2012 classification matched to being “severe” according to Atlanta 1992 classification, as only 7 patients according to Atlanta 1992 classification would have been classified as “mild” and the rest 20 patients as “severe” category, if the former criteria were followed. Both mild and severe acute pancreatitis patients according to Atlanta 2012 classification matched the groups identically to Atlanta 1992 classification (Figure 1).
When comparing mild AP to severe AP according to Atlanta 1992 classification, there were more patients who had SIRS and MODS (confirmed by APACHE II and MODS scores). Incidence of pancreatic and extrapancreatic necrosis, infected necrosis, number of surgical interventions was also significantly higher. In severe AP group, there were 13 (27.7%) deaths, while there was none in the mild AP group (Table 3).
| Mild | Severe | P value | |
| Male | 29 (51.8) | 25 (53.2) | 1.000 |
| Necrosis | |||
| Sterile | 55 (98.2) | 41 (87.2) | 0.343 |
| Infected | 1 (1.8) | 6 (12.8) | 0.054 |
| Sepsis | 0 (0) | 6 (12.8) | 0.011 |
| Interventions | |||
| Fine needle aspiration | 1 (1.8) | 12 (25.5) | 0.002 |
| US guided drainage | 1 (1.8) | 5 (10.6) | 0.101 |
| Necrosectomy | 0 (0) | 6 (12.7) | 0.011 |
| APACHE II, mean ± SD | 3.51 ± 1.94 | 11.48 ± 4.79 | < 0.001 |
| MODS, mean ± SD | 1.17 ± 1.28 | 4.29 ± 3.38 | < 0.001 |
| Deaths | 0 (0) | 13 (27.7) | < 0.001 |
Comparison of moderately severe and severe AP groups according to Atlanta 2012 classification is presented in Table 4. In moderately severe AP group rate of surgical interventions [FNA 2 (7.4%), US-guided drainage 1 (3.7%), surgical treatment 0 (0%), mortality rate, deaths 0 (0%)] and disease severity (APACHE II 7.7 ± 3.07, MODS scores 2.9 ± 1.78) was significantly lower when comparing to severe AP accordingly: [FNA 10 (37%), US-guided drainage 4 (14.8%), surgical treatment 6 (22.2%), mortality rate, deaths 13(48.1%)] and disease severity (APACHE II 13.2 ± 5.43, MODS scores 5.2 ± 3.90).
| Moderately severe | Severe | P value | |
| Male | 15 (55.6) | 16 (59.3) | 1.000 |
| Necrosis | |||
| Sterile | 26 (96.3) | 22 (81.5) | 0.696 |
| Infected | 1 (3.7) | 5 (18.5) | 0.201 |
| Sepsis | 0 (0) | 6 (22.2) | 0.028 |
| Interventions | |||
| Fine needle aspiration | 2 (7.4) | 10 (37.0) | 0.053 |
| US guided drainage | 1 (3.7) | 4 (14.8) | 0.356 |
| Necrosectomy | 0 (0) | 6 (22.2) | 0.028 |
| APACHE II, mean ± SD | 7.7 ± 3.07 | 13.2 ± 5.43 | 0.002 |
| MODS, mean ± SD | 2.9 ± 1.78 | 5.2 ± 3.90 | < 0.001 |
| ICU admission | 5 (18.5) | 24 (88.9) | 0.004 |
| Deaths | 0 (0) | 13 (27.7) | 0.001 |
Since the Atlanta conference established a classification system in the early 1990s, it has been criticized for being overly simplistic in categorizing acute pancreatitis into only “mild” and “severe” disease[5-8]. As a result, a heterogeneous group of patients were categorized as having severe AP, making it difficult to appropriately stratify patients therapeutically and compare research outcomes in this disease[4,9-11].
Our study supports the literature finding that Atlanta 1992 classification (mild and severe AP) is not sufficient because patients may experience transitory organ failure and/or have local pancreas and peripancreatic complications and were categorized as being “severe” AP[4-13]. The updated Atlanta 2012 classification addresses this missing group and “moderately severe” category is introduced[9,10]. While performing analysis of our clinical database, patients who had less than 48 hours transitory one organ system failure and previously categorized as “severe” pancreatitis (“moderately severe” according to Atlanta 2012), usually had self-limited disease, little risk of local and systemic complications, and the course of AP was like “mild” AP[2,3,14-18]. As a result, these patients require shorter ICU stay if any at all, less frequently develop infected pancreatic necrosis and/or sepsis, furthermore, require little or no US guided or surgical interventions. There were no deaths reported in moderately severe AP group. Failure to categorize precisely patient’s according to disease severity and initiation of aggressive treatment results in increased costs.
Our study compared the accuracy of two AP severity classifications for predicting important outcomes using a prospective clinical database. In addition, we evaluated different course (mild, moderately severe, severe) of the disease, treatment outcomes and compared among the groups while applying the most recent classification. Both classifications (Atlanta 1992, Atlanta 2012) were accurate for predicting “severe” group of the patients. They both were essentially equivalent in predicting mortality, need for ICU stay and surgical interventional procedure for “severe” AP group. Our study also demonstrates that all patients with persistent organ failure do not have the same risk of mortality and should be further stratified.
Like previously reported by Kadiyala et al[11] that those with multisystem persistent organ failure experienced a significantly higher mortality than those with single-system persistent organ failure (7.4% vs 56.3%, respectively, P = 0.001). Furthermore, the study by Kadiyala et al[11]. reports that multisystem persistent organ failure was a stronger predictor of mortality than single-system persistent organ failure, sterile necrosis, or infected necrosis. The same study suggested that patient classified as having severe AP based on persistent organ failure should be further stratified by the presence or absence of multisystem persistent organ failure. Therefore, our study results suggest that patients classified as “severe” based on organ failure should be further evaluated for the presence or absence of multiple persistent organ failure.
The biggest advantage of the Revised Atlanta 2012 classification is that patients with transitory organ failure previously classified as severe AP are now allocated to the moderately severe AP group. Our findings suggest that “moderately severe” AP has a clinical course similar to “mild AP” and often is self-limited or if the treatment is initiated they have less complications and they rarely need intervention (drainage, surgical, etc.). Furthermore, if organ insufficiency regresses within the first 48 hours, antibiotic usage may be limited or not even started, no need for enteric or parenteral feeding or use of catheterization (central vein, urinary) while aiming to limit complications related to interventions and treatment costs.
The present study has several important strengths. The primary strength of this study is that the data were collected prospectively. This minimized missing data and selection bias. Also, our study explicatively analyzed patient outcomes and economic impact while comparing two versions (1992 and 2012) of Atlanta classification. All patients had a CT scan performed at regular intervals according to the protocol
According to our data, moderately severe AP (Atlanta 2012) group has similar disease course to mild AP (Atlanta 1992 and 2012). As a result, the disease often resolves without any adverse events and temporary organ failure is overcome by the timely treatment, patients tend to have less complications and interventional treatment is rarely needed.
In conclusion, the revised (2012) Atlanta classification proved to be superior to the former classic (1992) Atlanta classification. The results of the study support the use of Atlanta 2012 classification and suggest that “moderately” severe AP cases should be treated as “mild” AP once temporary organ failure is controlled. Use of the classification system in this way will result in significant costs savings with improved outcomes of the patients.
The 1992 Atlanta Classifications identified two categories of acute pancreatitis (AP), “mild” and “severe”. However, a subgroup of AP patients who fell in-between the two 1992 severity categories were often observed to have relatively good outcomes and respond positively to less aggressive treatment protocols than those with severe disease. In 2012 the Atlanta classification of AP was revised by adding a third category defined as “moderately severe”.
To the best of authors’ knowledge, there are no studies have evaluated the outcomes and clinical course of “moderately severe” pancreatitis to test their true value in clinical setting. There are no studies have focused on complications, mortality and outcomes of patients with moderately severe AP. The question if the recommended aggressive treatment and expensive interventions are necessary in moderately severe category patients is raises.
The main objectives of this study were to explore the outcomes and the appropriate treatment for patients with moderately severe AP. These objectives were achieved and to the best of our knowledge, no studies have evaluated the outcomes and clinical course of “moderately severe” pancreatitis to test their true value in clinical setting.
The study is based on the data from specially designed database. Since 2008 data of patients with AP, admitted to the Department of Surgery, Hospital of Lithuanian University of Health Sciences were prospectively collected and entered into this database. Statistical analysis was performed on data of 103 AP patients. After stratifying patients into different categories, severe AP groups according to Atlanta 1992 and Atlanta 2012 were compared with each other. Moderately severe (Atlanta 2012) cases were compared to mild and severe cases according to Atlanta 1992 classification and the outcomes and management were re-assessed in all groups.
Both classifications (Atlanta 1992, Atlanta 2012) are accurate for predicting “severe” group of the patients. They both are essentially equivalent in predicting mortality, need for ICU stay and surgical interventional procedure for “severe” AP group. The study also demonstrates that all patients with persistent organ failure do not have the same risk of mortality and should be further stratified. Findings suggest that “moderately severe” AP has a clinical course similar to “mild AP” and often is self-limited or if the treatment is initiated they have less complications and they rarely need intervention (drainage, surgical, etc.).
The revised (2012) Atlanta classification proved to be superior to the former classic (1992) Atlanta classification. Use of the classification system in this way will result in significant costs savings with improved outcomes of the patients.
Similar validation studies could be performed with larger patient cohorts in multicenter setting. The focus of such studies in the future should be on “severe” group of AP patients as the patients of this group require the most intensive treatment and the mortality rate is high.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Lithuania
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Kikuyama M, Xu CF S- Editor: Gong ZM L- Editor: A E- Editor: Lu YJ
| 1. | Kwong WT, Ondrejková A, Vege SS. Predictors and outcomes of moderately severe acute pancreatitis - Evidence to reclassify. Pancreatology. 2016;16:940-945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Bradley EL 3rd. A clinically based classification system for acute pancreatitis. Summary of the International Symposium on Acute Pancreatitis, Atlanta, Ga, September 11 through 13, 1992. Arch Surg. 1993;128:586-590. [PubMed] |
| 3. | Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, Tsiotos GG, Vege SS; Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4932] [Cited by in RCA: 4304] [Article Influence: 358.7] [Reference Citation Analysis (44)] |
| 4. | Vege SS, Gardner TB, Chari ST, Munukuti P, Pearson RK, Clain JE, Petersen BT, Baron TH, Farnell MB, Sarr MG. Low mortality and high morbidity in severe acute pancreatitis without organ failure: a case for revising the Atlanta classification to include “moderately severe acute pancreatitis”. Am J Gastroenterol. 2009;104:710-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 101] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 5. | Banks PA, Freeman ML; Practice Parameters Committee of the American College of Gastroenterology. Practice guidelines in acute pancreatitis. Am J Gastroenterol. 2006;101:2379-2400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1181] [Cited by in RCA: 1148] [Article Influence: 60.4] [Reference Citation Analysis (0)] |
| 6. | Bollen TL, Besselink MG, van Santvoort HC, Gooszen HG, van Leeuwen MS. Toward an update of the atlanta classification on acute pancreatitis: review of new and abandoned terms. Pancreas. 2007;35:107-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Bollen TL, van Santvoort HC, Besselink MG, van Leeuwen MS, Horvath KD, Freeny PC, Gooszen HG; Dutch Acute Pancreatitis Study Group. The Atlanta Classification of acute pancreatitis revisited. Br J Surg. 2008;95:6-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 162] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 8. | Pandol SJ, Saluja AK, Imrie CW, Banks PA. Acute pancreatitis: bench to the bedside. Gastroenterology. 2007;132:1127-1151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 433] [Cited by in RCA: 447] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 9. | Pintado MC, Trascasa M, Arenillas C, de Zárate YO, Pardo A, Blandino Ortiz A, de Pablo R. New Atlanta Classification of acute pancreatitis in intensive care unit: Complications and prognosis. Eur J Intern Med. 2016;30:82-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Chen Y, Ke L, Tong Z, Li W, Li J. Association between severity and the determinant-based classification, Atlanta 2012 and Atlanta 1992, in acute pancreatitis: a clinical retrospective study. Medicine (Baltimore). 2015;94:e638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Kadiyala V, Suleiman SL, McNabb-Baltar J, Wu BU, Banks PA, Singh VK. The Atlanta Classification, Revised Atlanta Classification, and Determinant-Based Classification of Acute Pancreatitis: Which Is Best at Stratifying Outcomes? Pancreas. 2016;45:510-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 12. | Singh RK, Poddar B, Baronia AK, Azim A, Gurjar M, Singhal S, Srivastava S, Saigal S. Audit of patients with severe acute pancreatitis admitted to an intensive care unit. Indian J Gastroenterol. 2012;31:243-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Petrov MS, Shanbhag S, Chakraborty M, Phillips AR, Windsor JA. Organ failure and infection of pancreatic necrosis as determinants of mortality in patients with acute pancreatitis. Gastroenterology. 2010;139:813-820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 517] [Cited by in RCA: 557] [Article Influence: 37.1] [Reference Citation Analysis (0)] |
| 14. | Cacopardo B, Pinzone M, Berretta S, Fisichella R, Di Vita M, Zanghì G, Cappellani A, Nunnari G, Zanghì A. Localized and systemic bacterial infections in necrotizing pancreatitis submitted to surgical necrosectomy or percutaneous drainage of necrotic secretions. BMC Surg. 2013;13 Suppl 2:S50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Harrison DA, D’Amico G, Singer M. Case mix, outcome, and activity for admissions to UK critical care units with severe acute pancreatitis: a secondary analysis of the ICNARC Case Mix Programme Database. Crit Care. 2007;11 Suppl 1:S1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Halonen KI, Pettilä V, Leppäniemi AK, Kemppainen EA, Puolakkainen PA, Haapiainen RK. Multiple organ dysfunction associated with severe acute pancreatitis. Crit Care Med. 2002;30:1274-1279. [PubMed] |
| 17. | Arroyo-Sánchez AS, García Ventura J, Aguirre Mejía RY. [Acute pancreatitis in intensive care unit: review and evolution of 36 cases Víctor Lazarte E. Hospital. Trujillo, Perú]. Rev Gastroenterol Peru. 2008;28:133-139. [PubMed] |
| 18. | De Waele JJ, Rello J, Anzueto A, Moreno R, Lipman J, Sakr Y, Pickkers P, Leone M, Ferguson A, Oud L. Infections and use of antibiotics in patients admitted for severe acute pancreatitis: data from the EPIC II study. Surg Infect (Larchmt). 2014;15:394-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |